Descending pathways Motor Neurons Motor neurons are split

- Slides: 33
Descending pathways

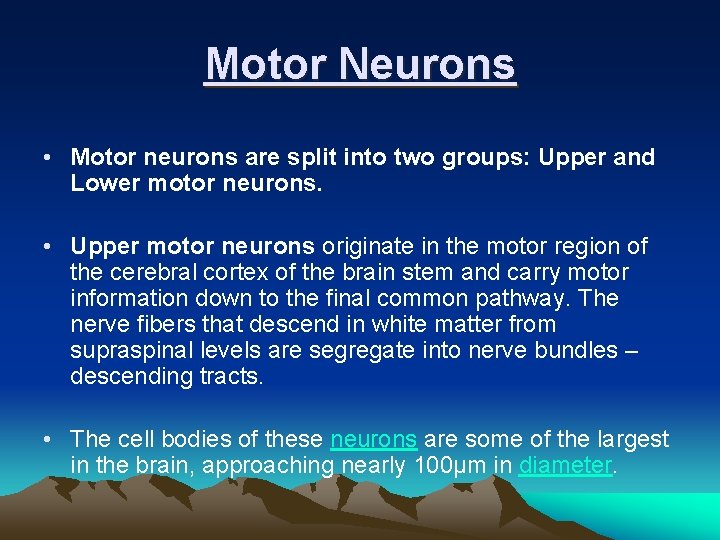
Motor Neurons • Motor neurons are split into two groups: Upper and Lower motor neurons. • Upper motor neurons originate in the motor region of the cerebral cortex of the brain stem and carry motor information down to the final common pathway. The nerve fibers that descend in white matter from supraspinal levels are segregate into nerve bundles – descending tracts. • The cell bodies of these neurons are some of the largest in the brain, approaching nearly 100μm in diameter.
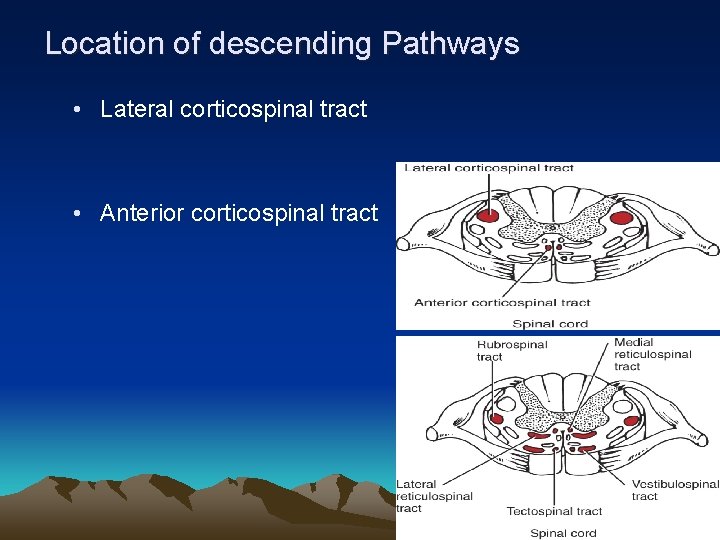
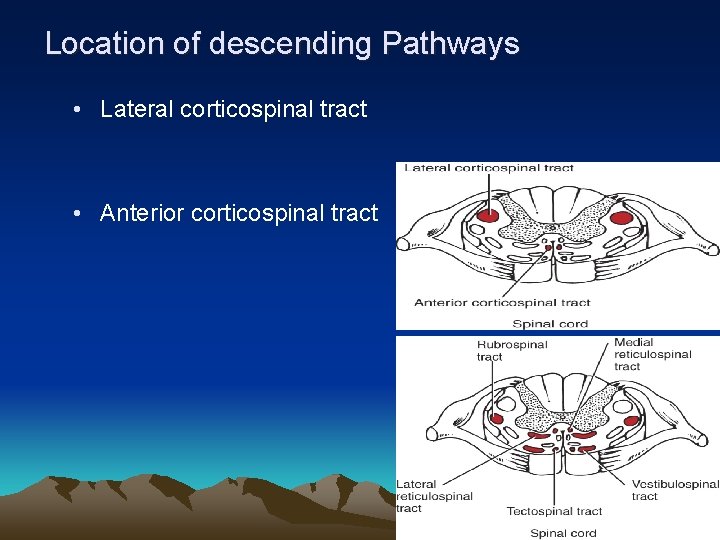
Location of descending Pathways • Lateral corticospinal tract • Anterior corticospinal tract
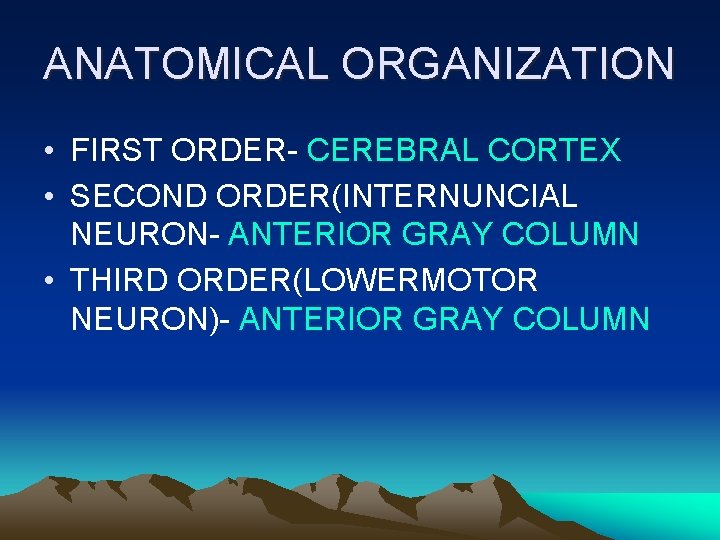
ANATOMICAL ORGANIZATION • FIRST ORDER- CEREBRAL CORTEX • SECOND ORDER(INTERNUNCIAL NEURON- ANTERIOR GRAY COLUMN • THIRD ORDER(LOWERMOTOR NEURON)- ANTERIOR GRAY COLUMN
Nerve pathways Descending Tracts Signal function Tract Corticospinal (pyramidal) Fine voluntary motor control of the limbs. The pathway also controls voluntary body posture adjustments. Rubrospinal Involved in involuntary adjustment of arm position in response to balance information; support of the body. Reticulospinal (1) Pontine Regulates various involuntary motor activities and assists in balance (leg extensors). Some pattern movements e. g. stepping (2) Medullary Inhibits firing of spinal and cranial motor neurons, control of antigravity muscles. Vestibulospinal (1) Medial It is responsible for adjusting posture to maintain balance (neck muscles). (2) Lateral It is responsible for adjusting posture to maintain balance (body/lower limb). Tectospinal Controls head and eye movements, Involved in involuntary adjustment of head position in response to visual information.
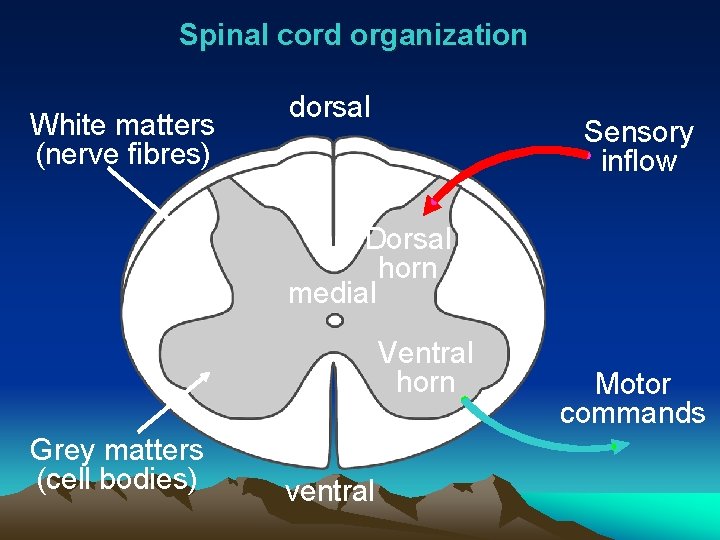
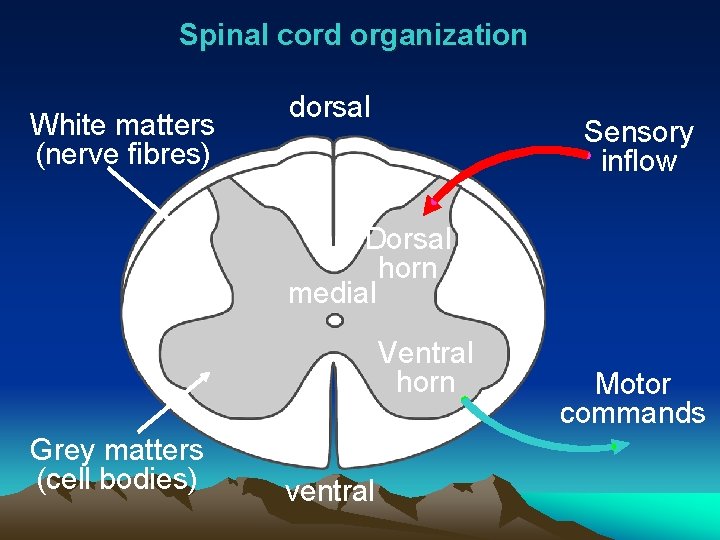
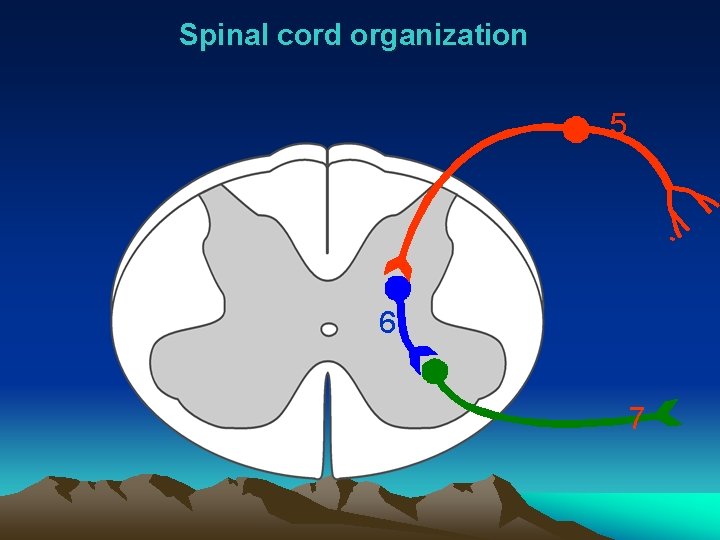
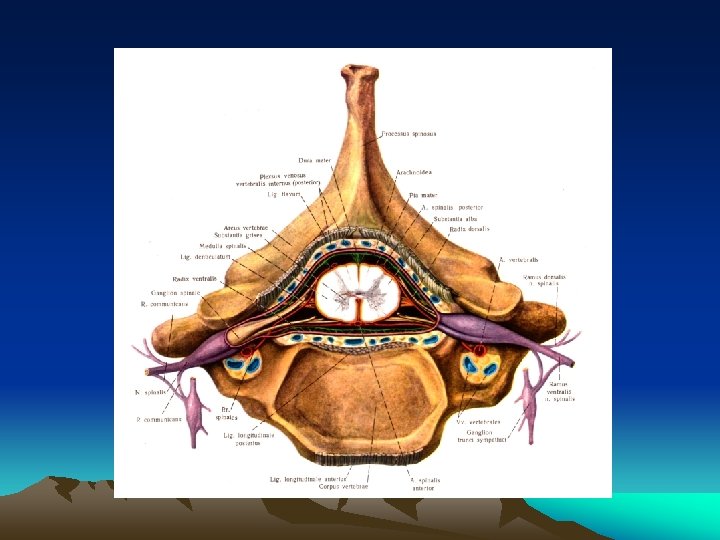
Spinal cord organization White matters (nerve fibres) lateral dorsal Sensory inflow Dorsal horn medial Ventral horn Grey matters (cell bodies) ventral Motor commands
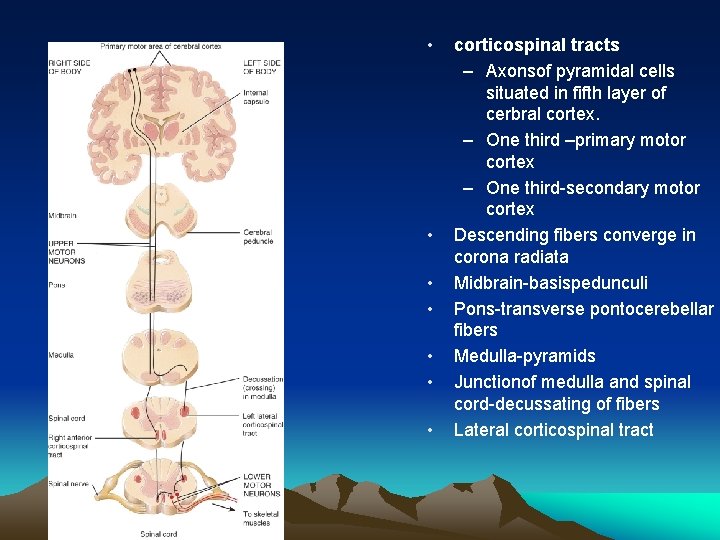
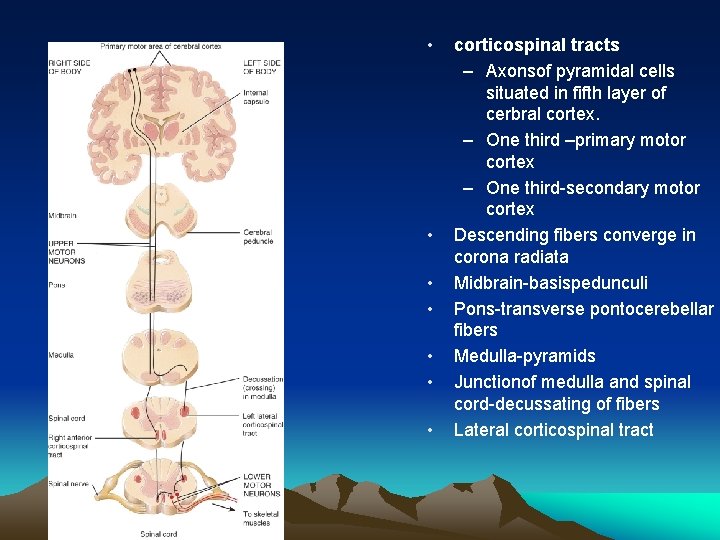
• • corticospinal tracts – Axonsof pyramidal cells situated in fifth layer of cerbral cortex. – One third –primary motor cortex – One third-secondary motor cortex Descending fibers converge in corona radiata Midbrain-basispedunculi Pons-transverse pontocerebellar fibers Medulla-pyramids Junctionof medulla and spinal cord-decussating of fibers Lateral corticospinal tract
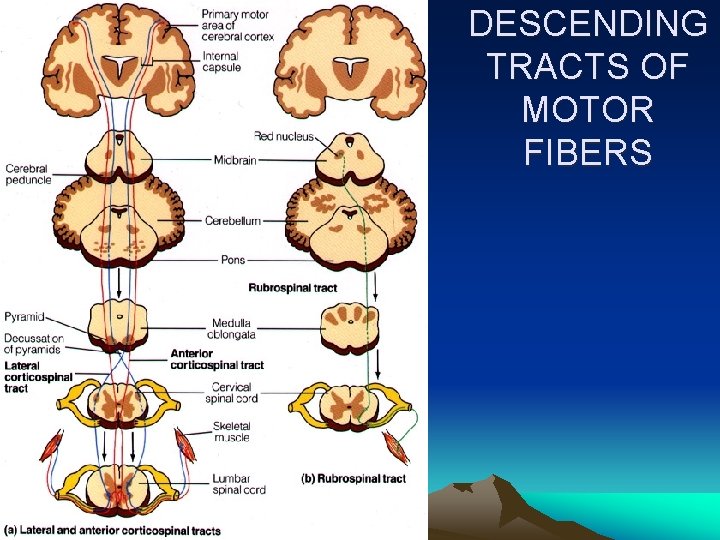
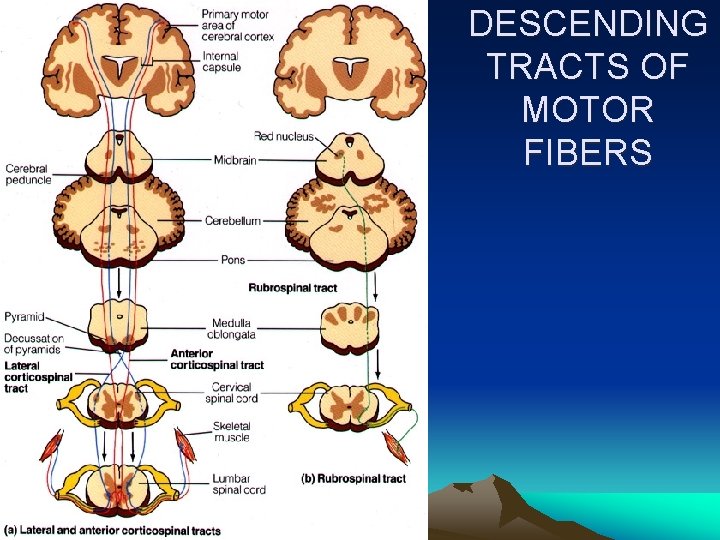
DESCENDING TRACTS OF MOTOR FIBERS
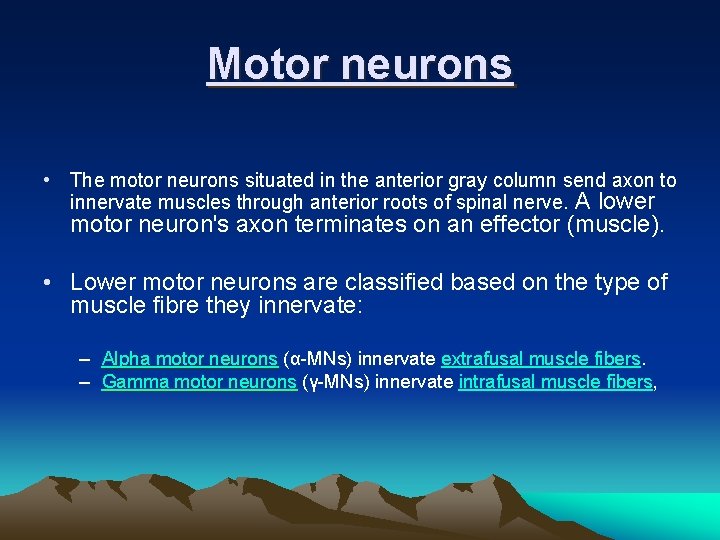
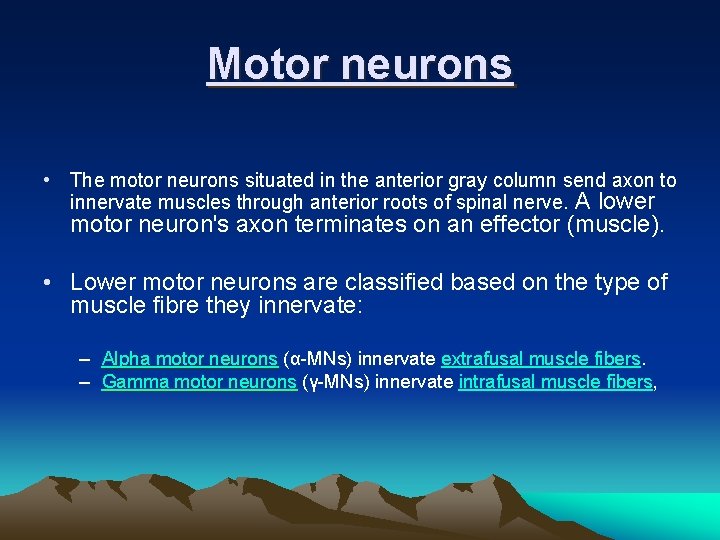
Motor neurons • The motor neurons situated in the anterior gray column send axon to innervate muscles through anterior roots of spinal nerve. A lower motor neuron's axon terminates on an effector (muscle). • Lower motor neurons are classified based on the type of muscle fibre they innervate: – Alpha motor neurons (α-MNs) innervate extrafusal muscle fibers. – Gamma motor neurons (γ-MNs) innervate intrafusal muscle fibers,
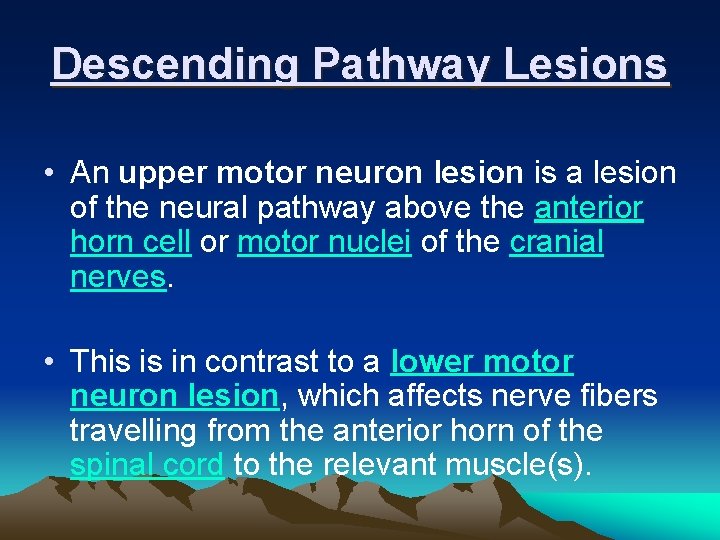
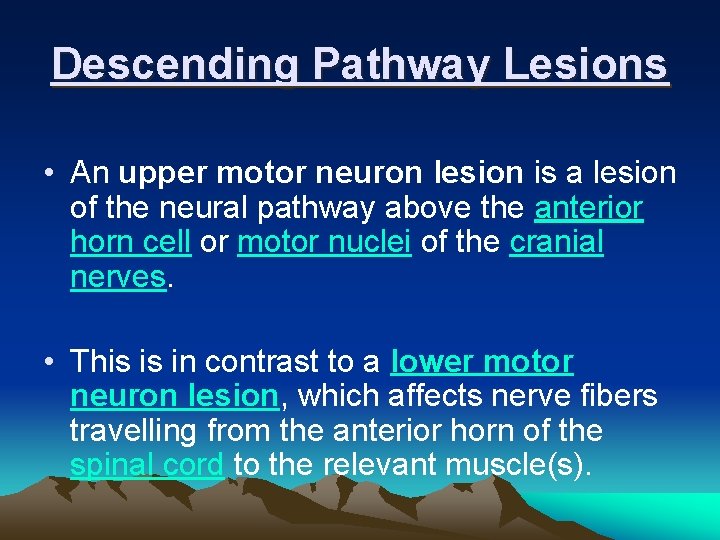
Descending Pathway Lesions • An upper motor neuron lesion is a lesion of the neural pathway above the anterior horn cell or motor nuclei of the cranial nerves. • This is in contrast to a lower motor neuron lesion, which affects nerve fibers travelling from the anterior horn of the spinal cord to the relevant muscle(s).
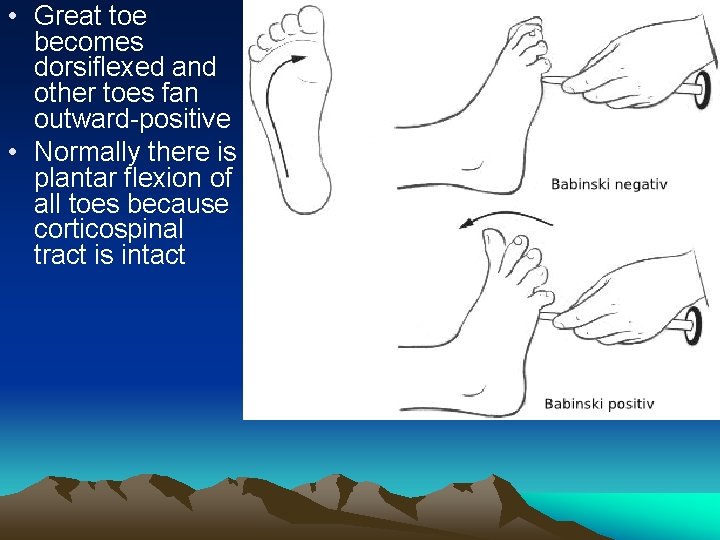
Corticospinal tract leisons • Babinski s sign is present • Superfficial abdominal reflexes absent • Loss of fine skilled movements
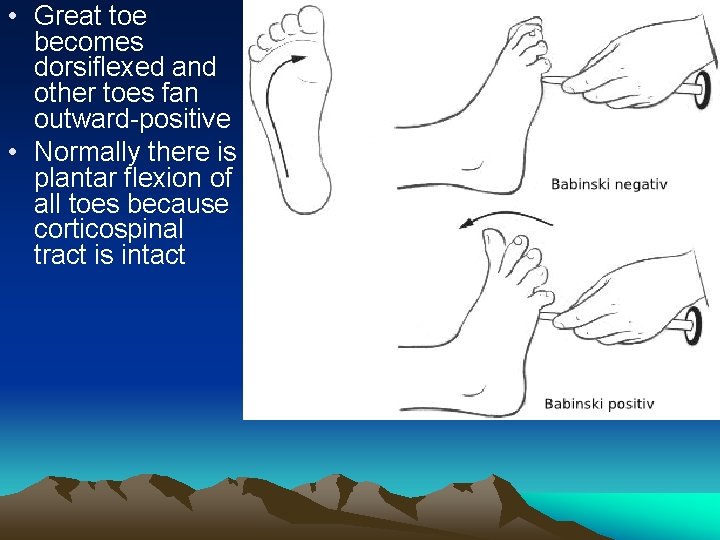
• Great toe becomes dorsiflexed and other toes fan outward-positive • Normally there is plantar flexion of all toes because corticospinal tract is intact
Upper motor neuron lesions (extra pyramidal tract) are indicated by: – Spasticity, increase in tone in the extensor muscles (lower limbs) or flexor muscles (upper limbs). As a result upperlimb is maintained in flexion and lower limb in extension
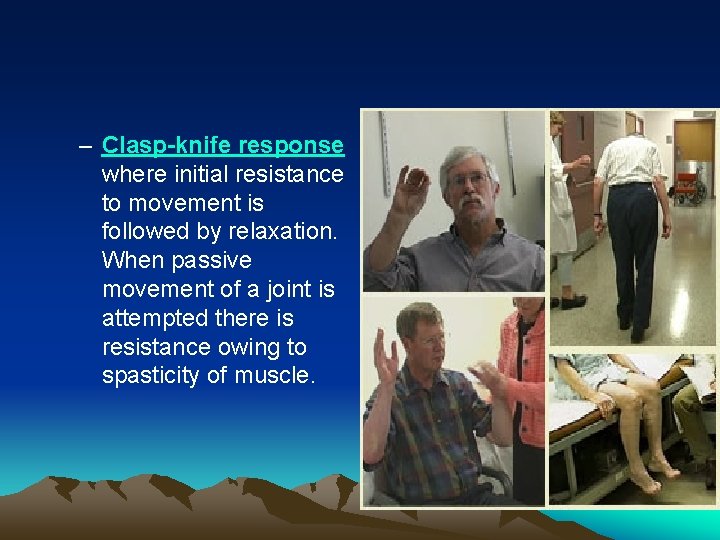
– Clasp-knife response where initial resistance to movement is followed by relaxation. When passive movement of a joint is attempted there is resistance owing to spasticity of muscle.
– Weakness in the flexors (lower limbs) or extensors (upper limbs), but no muscle wasting
• Exaggerated abdominal reflexes
Lower motor neuron leison • • Flaccid paralysis Atrophy of muscles Muscular fasiculations Muscular contracture
• Overall, upper • lower motor neuron lesions result in hypotonia, no hypertonia, reflexes, flaccid hyperreflexia, paralysis, muscle spastic paralysis, atrophy revival of the Babinski reflex (stroke lateral sole)
Indirect (Extrapyramidal) System • Includes the brain stem, motor nuclei, and all motor pathways not part of the pyramidal system • This system includes the rubrospinal, vestibulospinal, reticulospinal, and tectospinal tracts • These motor pathways are complex and multisynaptic, and regulate: – Axial muscles that maintain balance and posture – Muscles controlling coarse movement of the proximal portions of limbs – Head, neck, and eye movement
• LMN are known as the ‘final common pathway’ because despite all the descending tracts they are the only neurons that actually physically contact the muscle fibers • LMN’s get stimulated by corticospinal, vestibulospinal, reticulospinal, rubrospinal and tectospinal tracts, among others. The cerebellum exerts a substantial influence on many of them.
Ascending Pathway Lesions • Loss of sensory input from relevant pathway – E. g. Spinothalamic tract • Unilateral lesion usually causes contralateral anaesthesia (loss of sensation (pain and temperature)). Anaesthesia will normally begin 1 -2 segments below the level of lesion, affecting all caudal body areas. This is clinically tested by using pin pricks.
– If lesion is hemisection (halfway across the spinal cord) (causing hemiplegia)) it is known as Brown. Séquard syndrome. • Brown-Séquard syndrome may be caused by a spinal cord tumour, trauma (such as a gunshot wound or puncture wound to the neck or back), ischemia (obstruction of a blood vessel), or infectious or inflammatory diseases such as tuberculosis, or multiple sclerosis. – Any presentation of spinal injury which is an incomplete lesion can be called a partial Brown. Séquard or incomplete Brown-Séquard syndrome, so long as it has characterized by features of a motor loss on the same side of the spinal injury and loss of sensation on the opposite side.
Questions?
• Draw labelled diagram showing ascending tracts in spinal cord.
• What will happen in leison of spinal leminiscus in medulla oblongata.
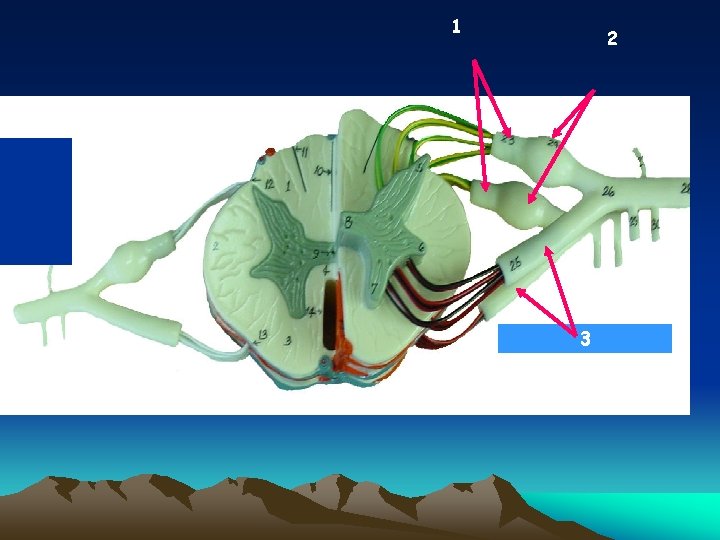
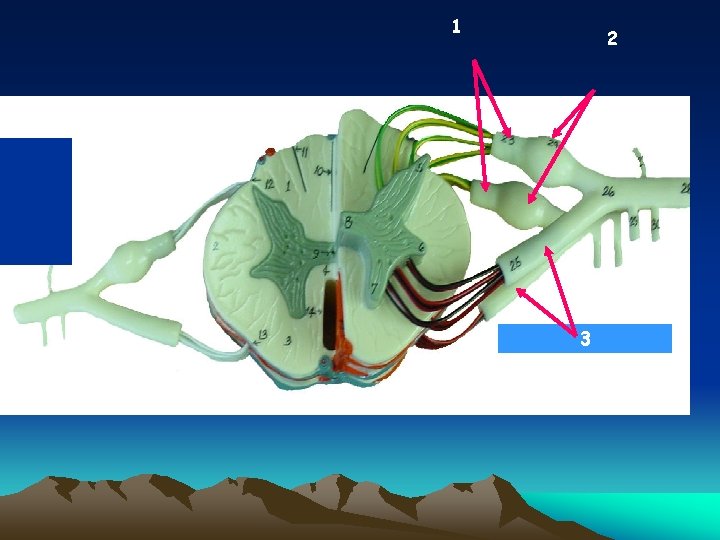
1 2 Dorsal root 4 3 3
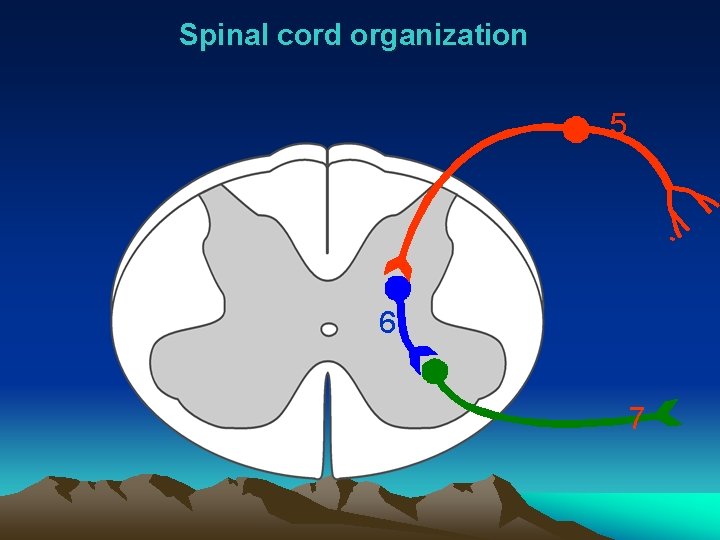
Spinal cord organization 5 6 7
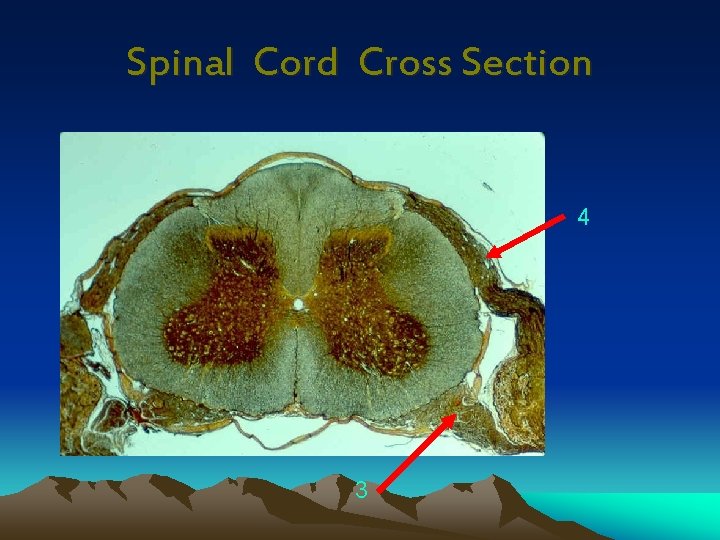
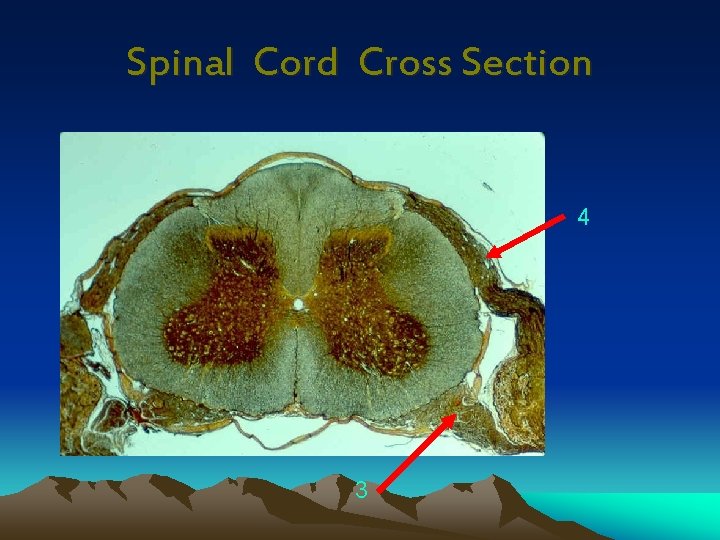
Spinal Cord Cross Section 4 3
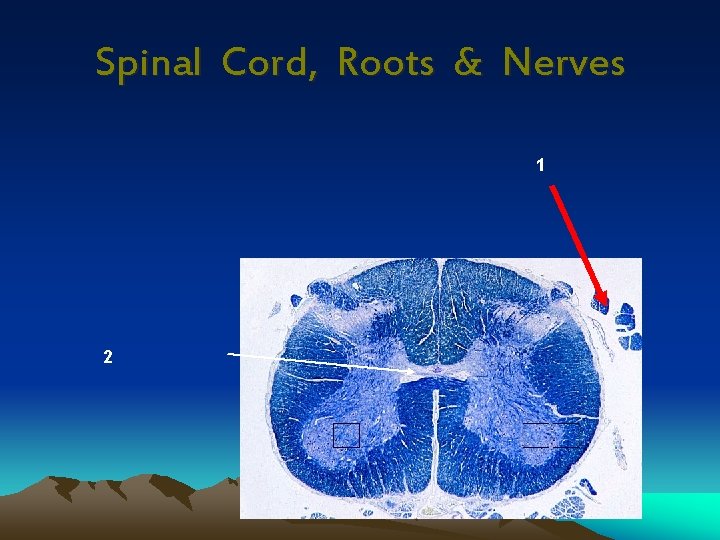
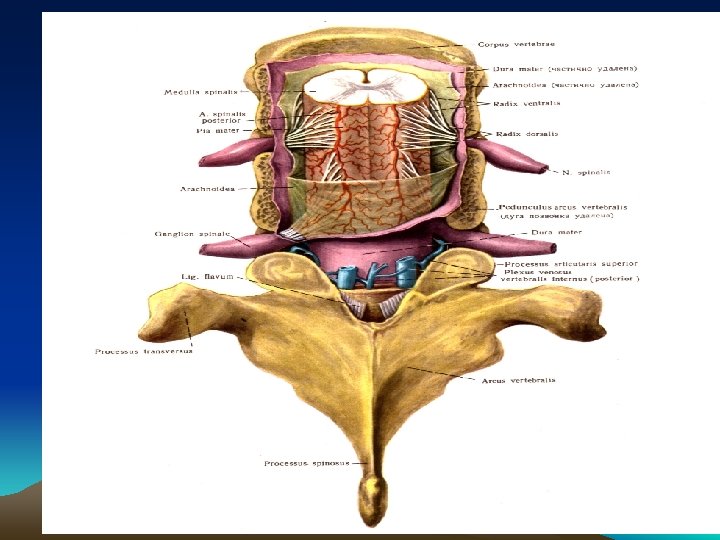
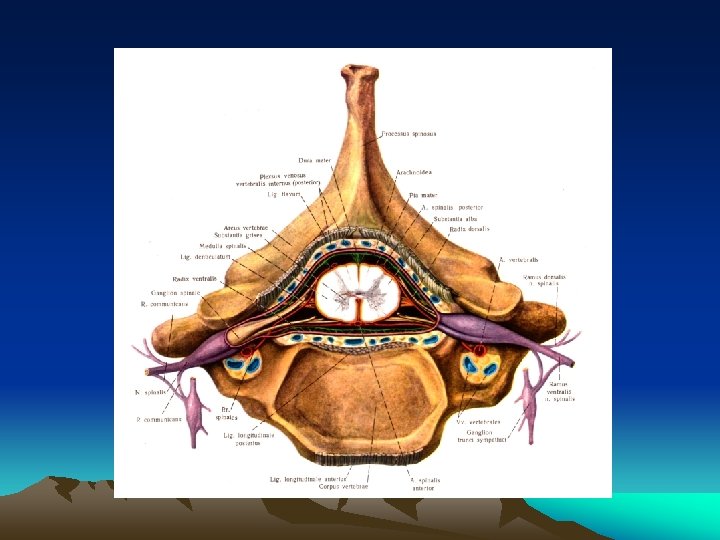
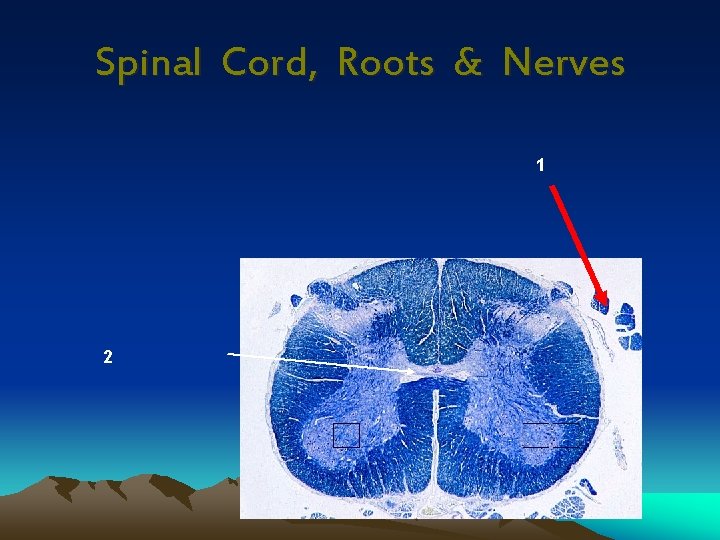
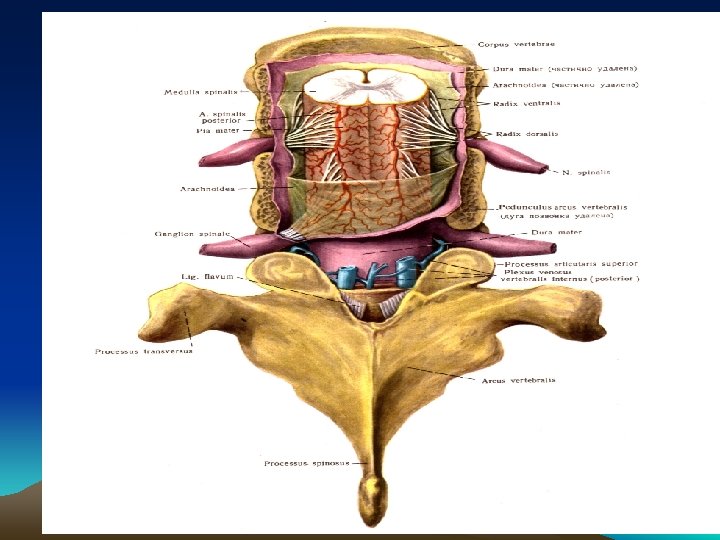
Spinal Cord, Roots & Nerves 1 2