Dermatology Blueprint PANCE Blueprint Eczematous Eruptions Contact Dermatitis

Dermatology Blueprint PANCE Blueprint
Eczematous Eruptions
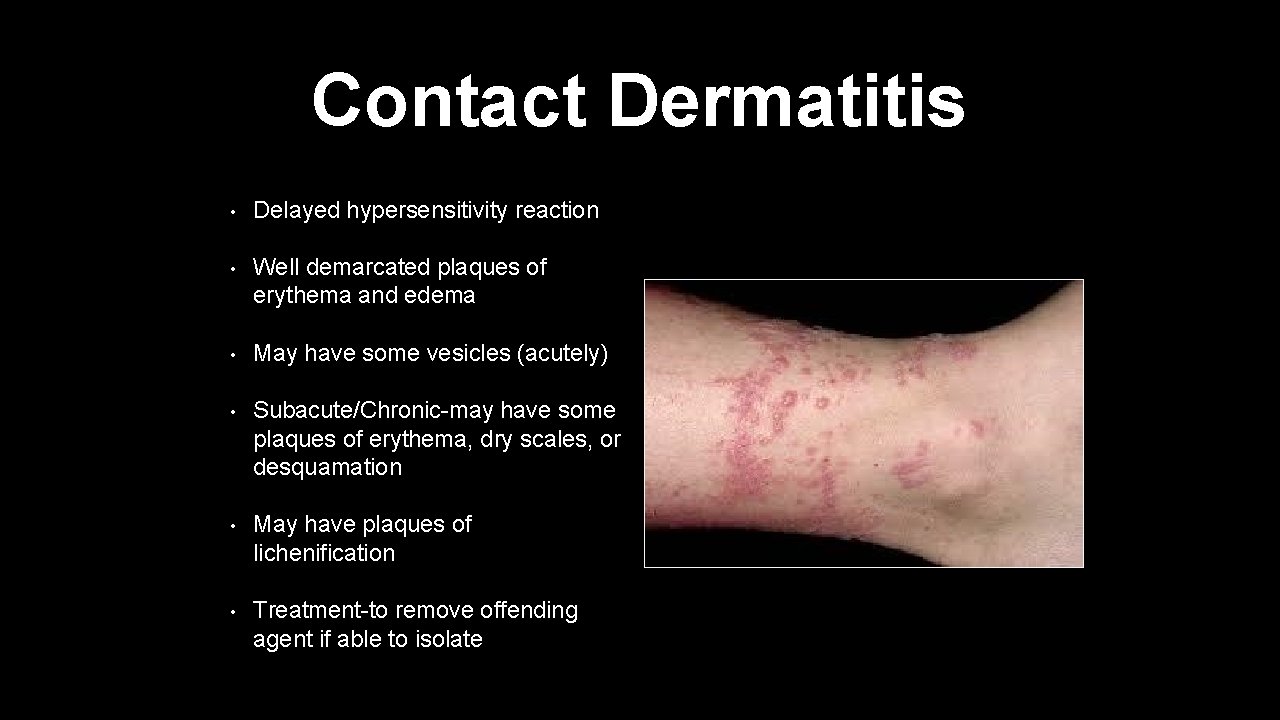
Contact Dermatitis • Delayed hypersensitivity reaction • Well demarcated plaques of erythema and edema • May have some vesicles (acutely) • Subacute/Chronic-may have some plaques of erythema, dry scales, or desquamation • May have plaques of lichenification • Treatment-to remove offending agent if able to isolate
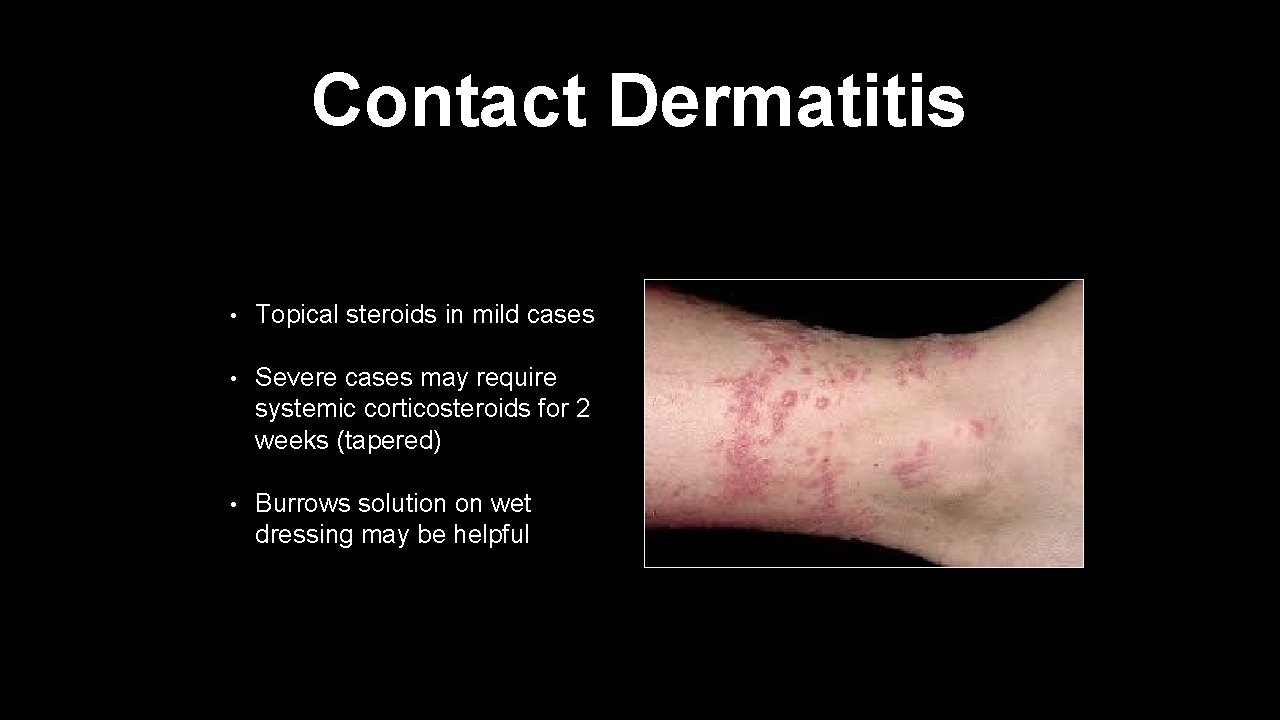
Contact Dermatitis • Topical steroids in mild cases • Severe cases may require systemic corticosteroids for 2 weeks (tapered) • Burrows solution on wet dressing may be helpful
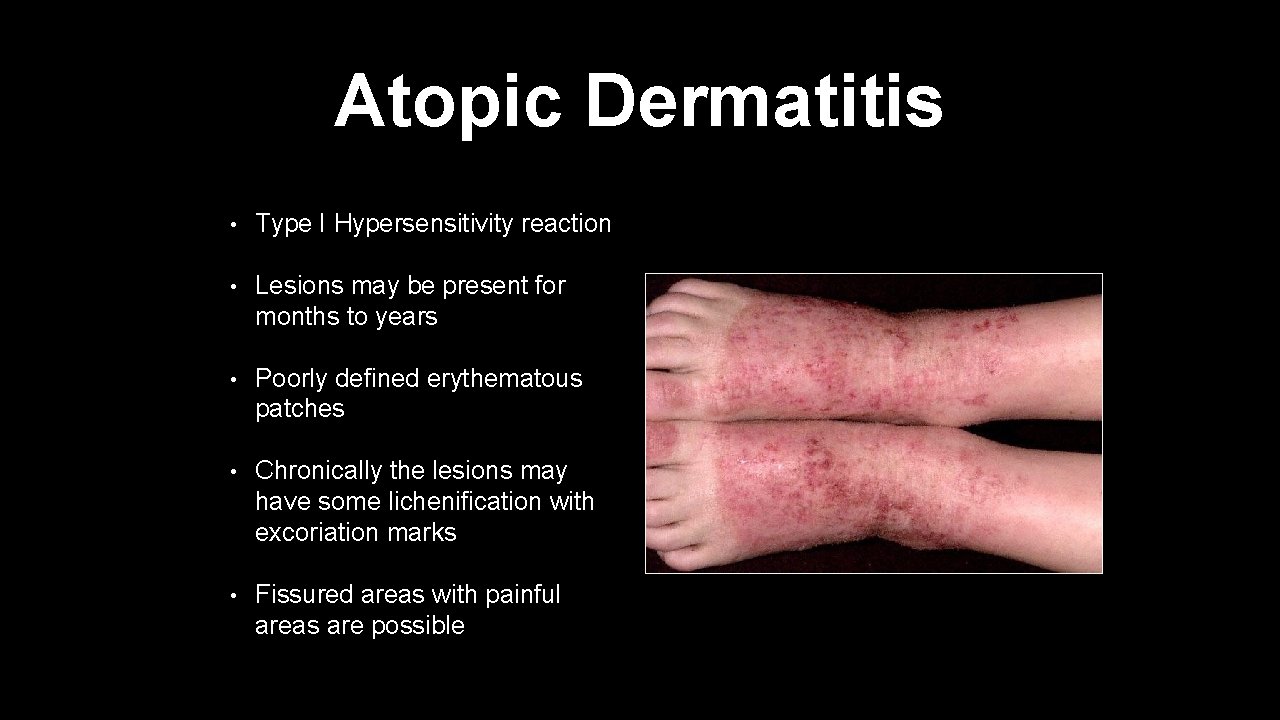
Atopic Dermatitis • Type I Hypersensitivity reaction • Lesions may be present for months to years • Poorly defined erythematous patches • Chronically the lesions may have some lichenification with excoriation marks • Fissured areas with painful areas are possible
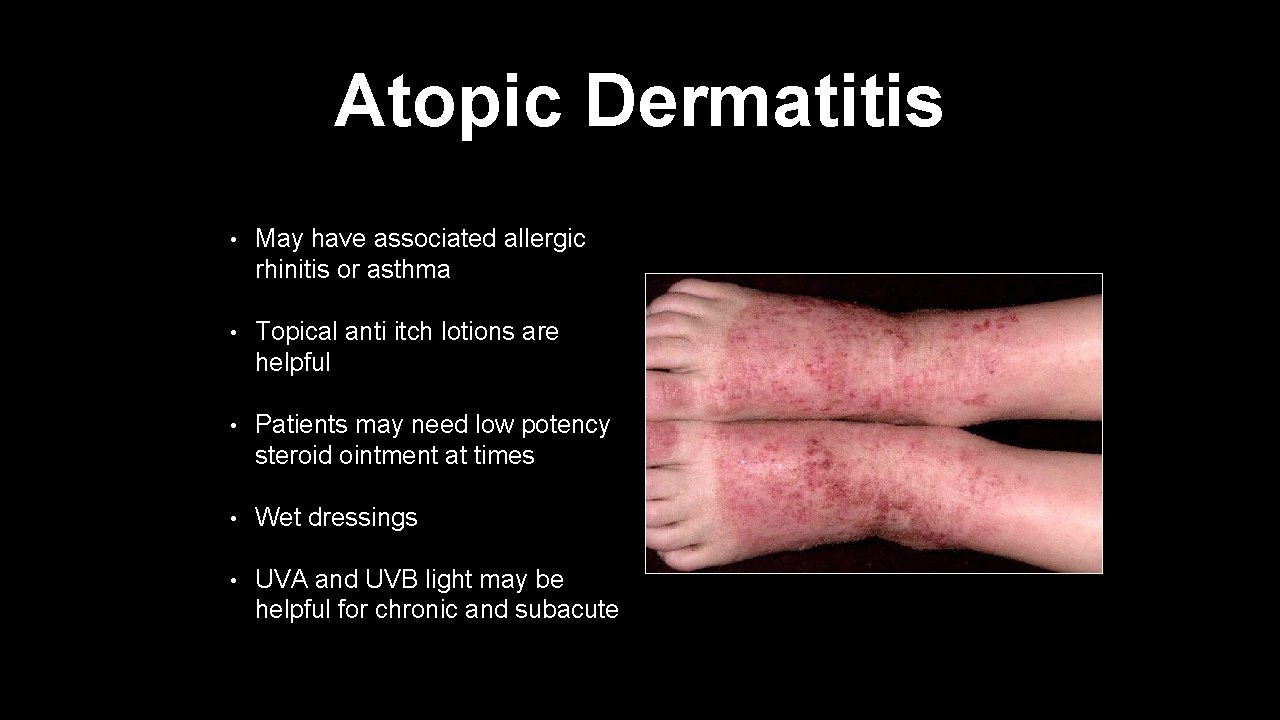
Atopic Dermatitis • May have associated allergic rhinitis or asthma • Topical anti itch lotions are helpful • Patients may need low potency steroid ointment at times • Wet dressings • UVA and UVB light may be helpful for chronic and subacute
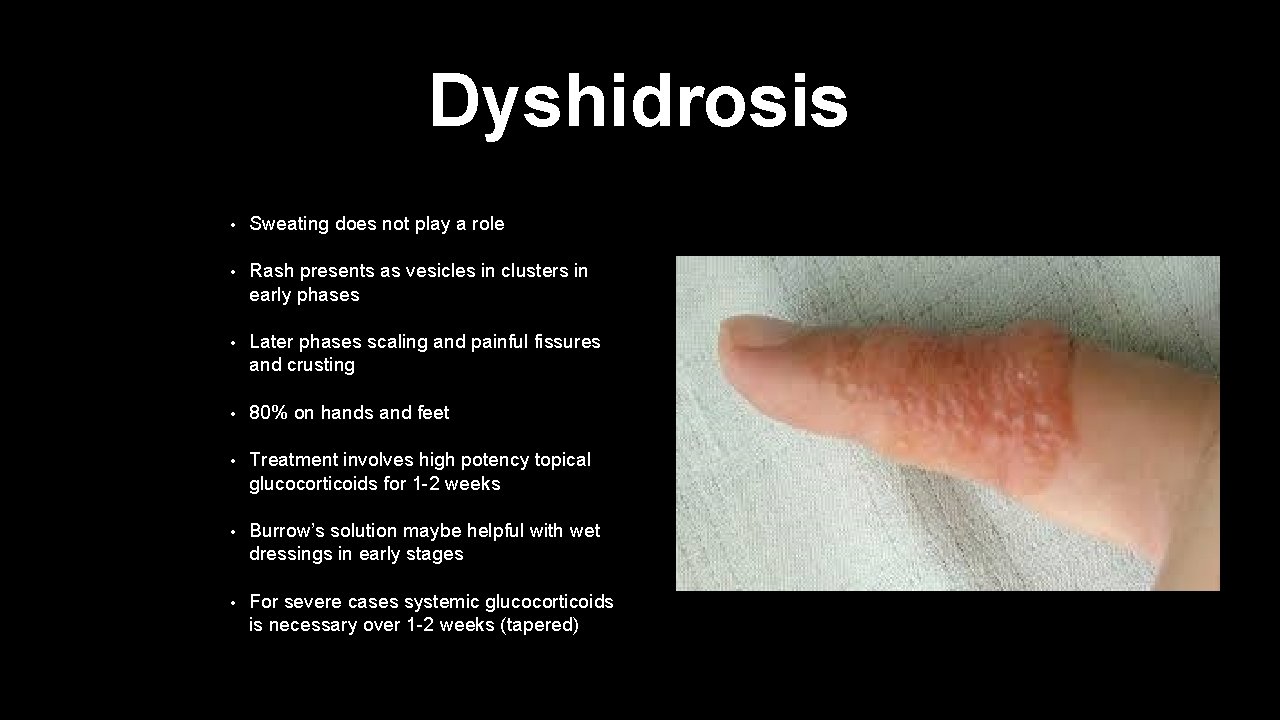
Dyshidrosis • Sweating does not play a role • Rash presents as vesicles in clusters in early phases • Later phases scaling and painful fissures and crusting • 80% on hands and feet • Treatment involves high potency topical glucocorticoids for 1 -2 weeks • Burrow’s solution maybe helpful with wet dressings in early stages • For severe cases systemic glucocorticoids is necessary over 1 -2 weeks (tapered)
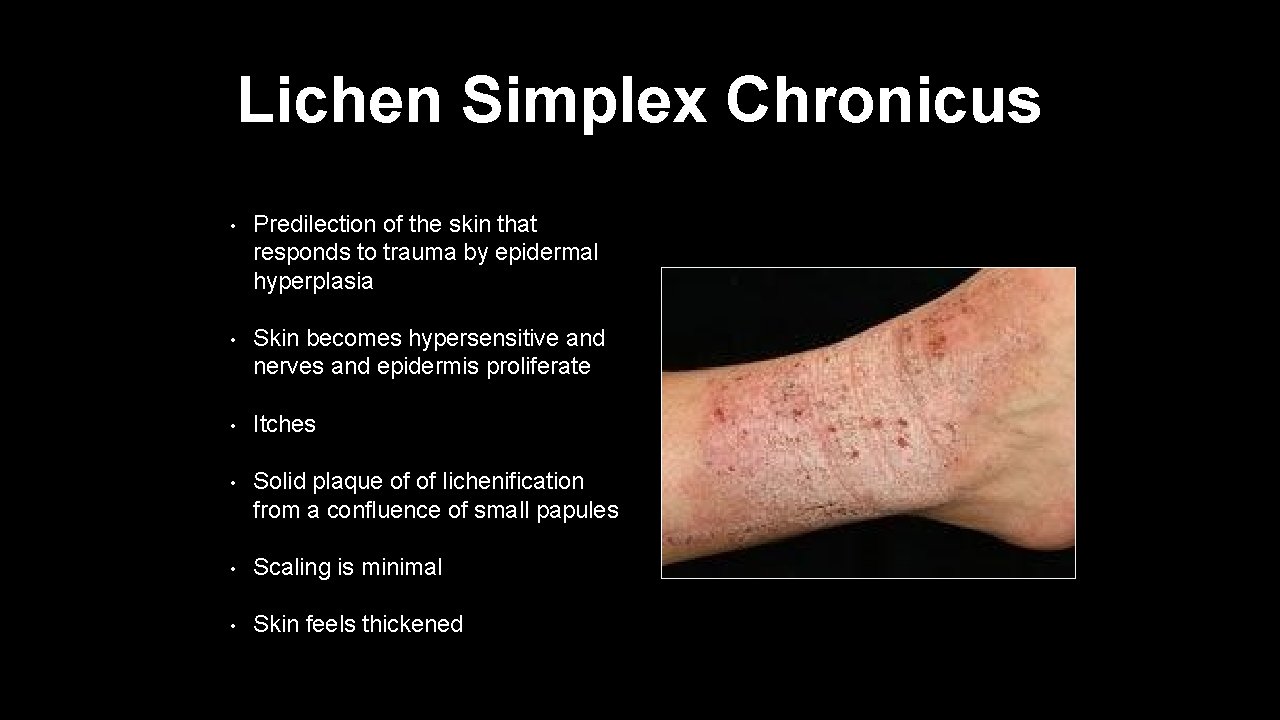
Lichen Simplex Chronicus • Predilection of the skin that responds to trauma by epidermal hyperplasia • Skin becomes hypersensitive and nerves and epidermis proliferate • Itches • Solid plaque of of lichenification from a confluence of small papules • Scaling is minimal • Skin feels thickened
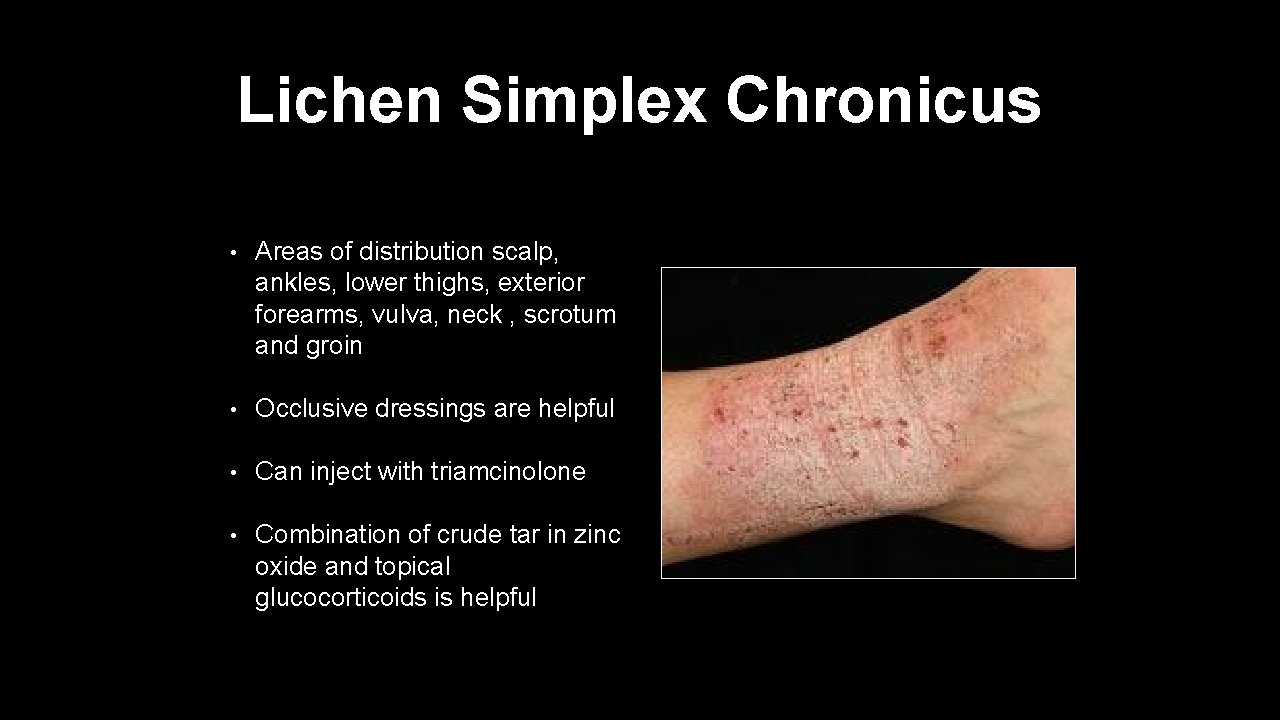
Lichen Simplex Chronicus • Areas of distribution scalp, ankles, lower thighs, exterior forearms, vulva, neck , scrotum and groin • Occlusive dressings are helpful • Can inject with triamcinolone • Combination of crude tar in zinc oxide and topical glucocorticoids is helpful
Papulosquamous Diseases
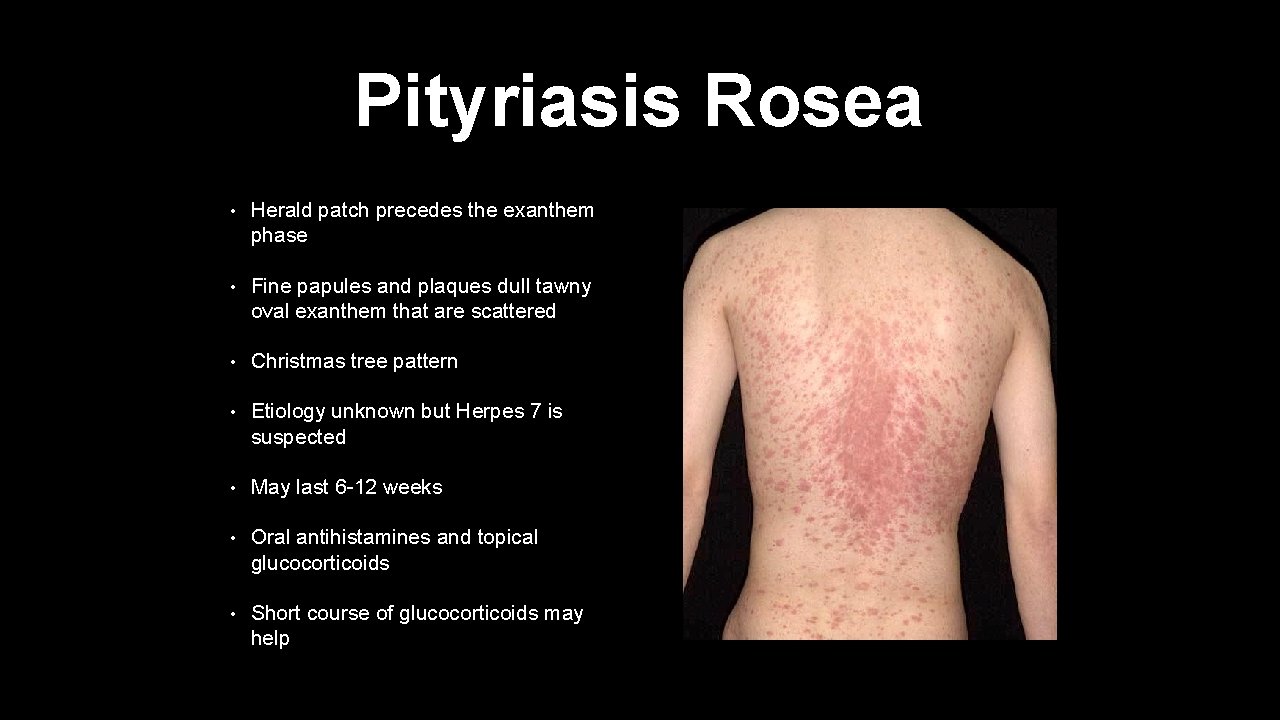
Pityriasis Rosea • Herald patch precedes the exanthem phase • Fine papules and plaques dull tawny oval exanthem that are scattered • Christmas tree pattern • Etiology unknown but Herpes 7 is suspected • May last 6 -12 weeks • Oral antihistamines and topical glucocorticoids • Short course of glucocorticoids may help
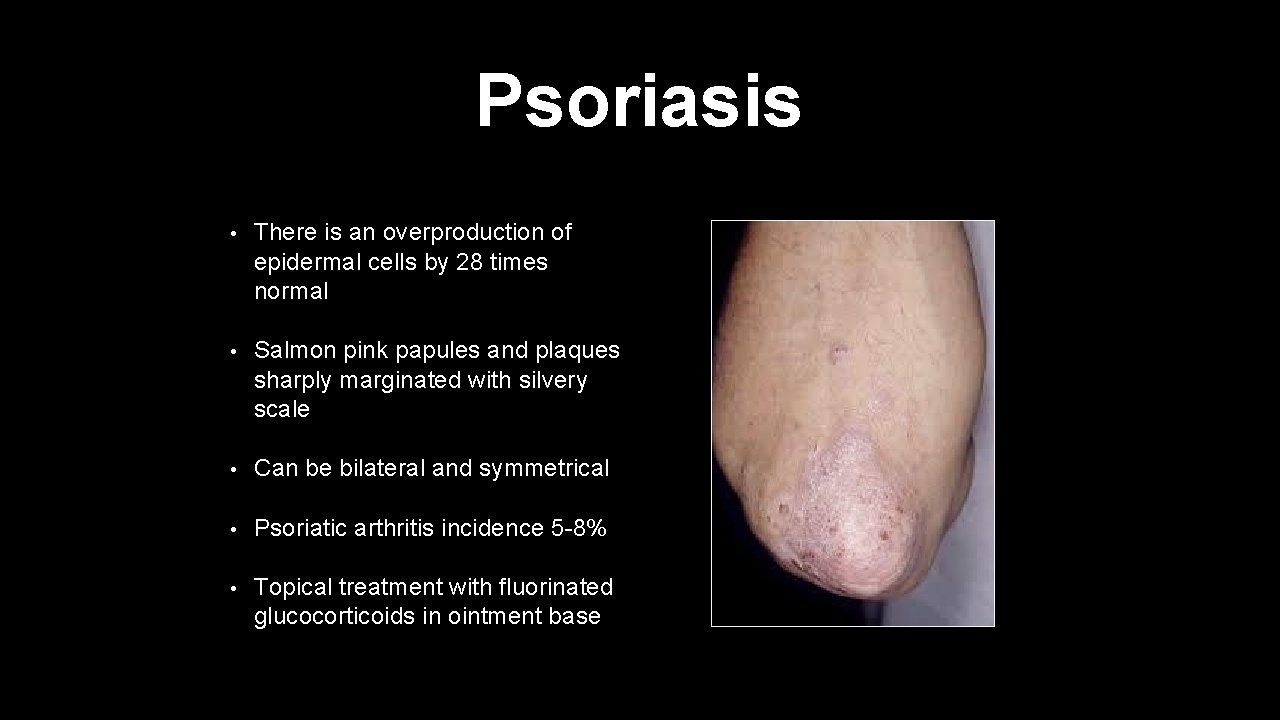
Psoriasis • There is an overproduction of epidermal cells by 28 times normal • Salmon pink papules and plaques sharply marginated with silvery scale • Can be bilateral and symmetrical • Psoriatic arthritis incidence 5 -8% • Topical treatment with fluorinated glucocorticoids in ointment base
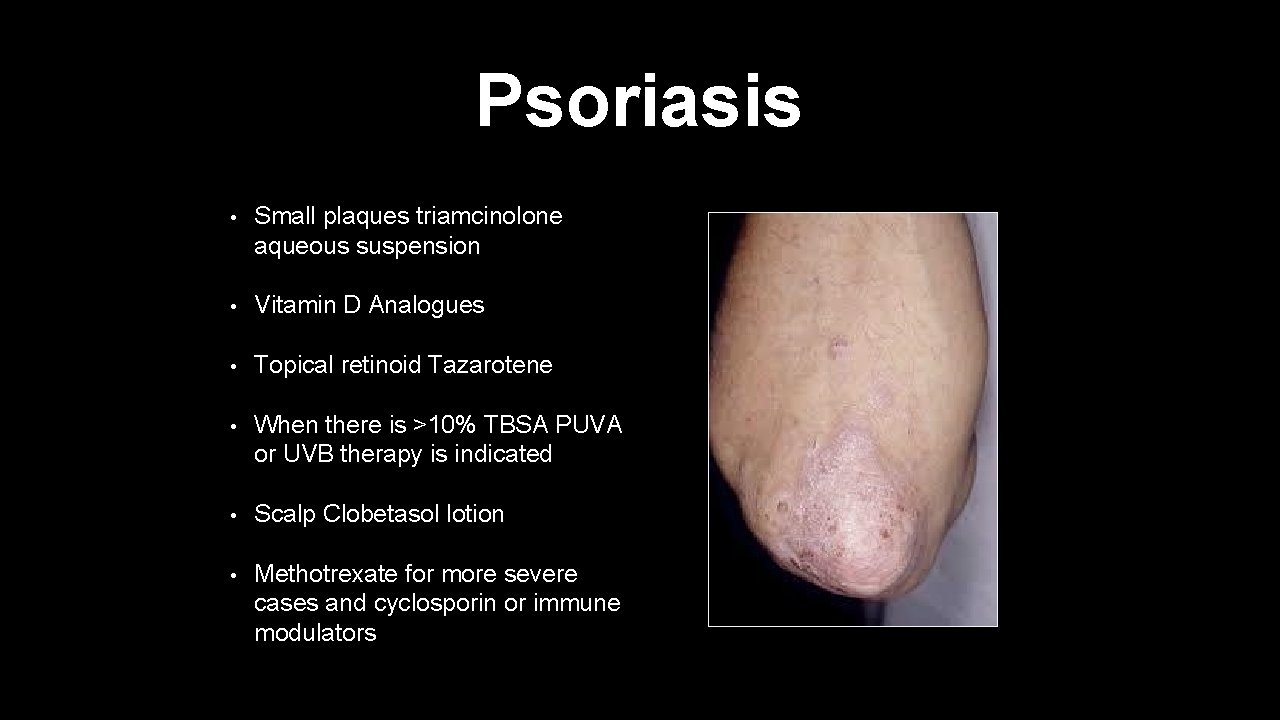
Psoriasis • Small plaques triamcinolone aqueous suspension • Vitamin D Analogues • Topical retinoid Tazarotene • When there is >10% TBSA PUVA or UVB therapy is indicated • Scalp Clobetasol lotion • Methotrexate for more severe cases and cyclosporin or immune modulators
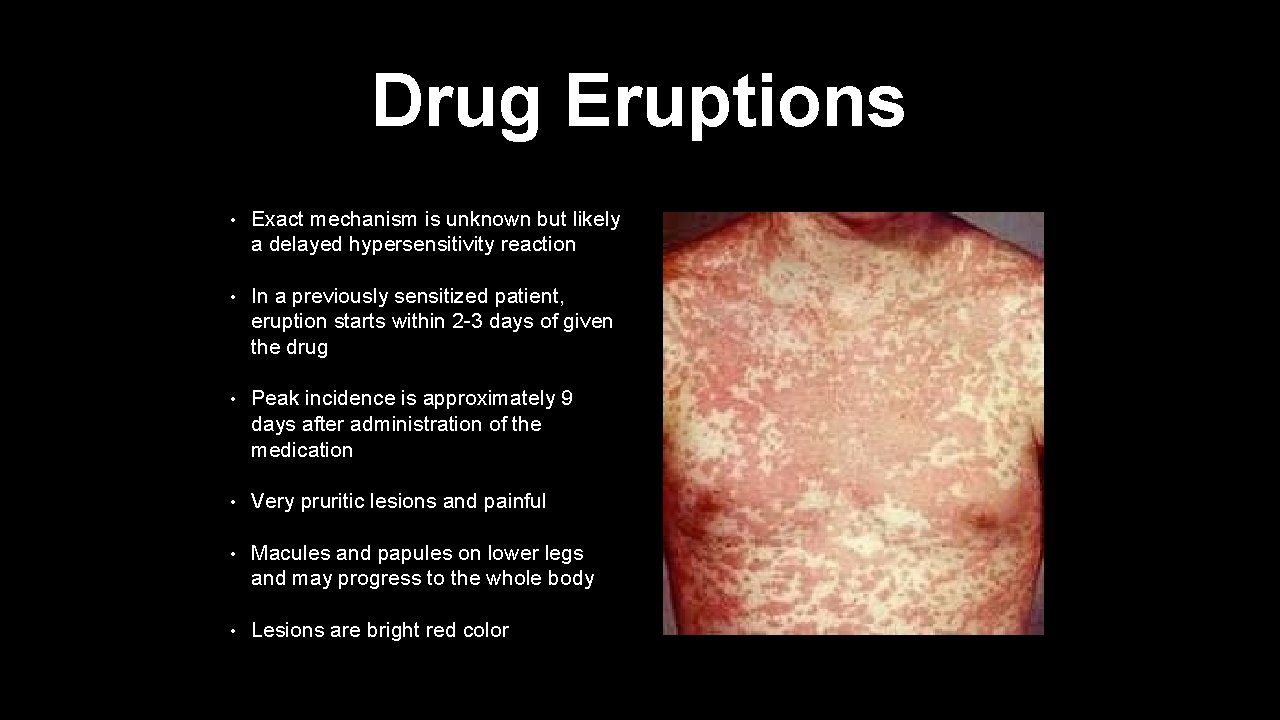
Drug Eruptions • Exact mechanism is unknown but likely a delayed hypersensitivity reaction • In a previously sensitized patient, eruption starts within 2 -3 days of given the drug • Peak incidence is approximately 9 days after administration of the medication • Very pruritic lesions and painful • Macules and papules on lower legs and may progress to the whole body • Lesions are bright red color
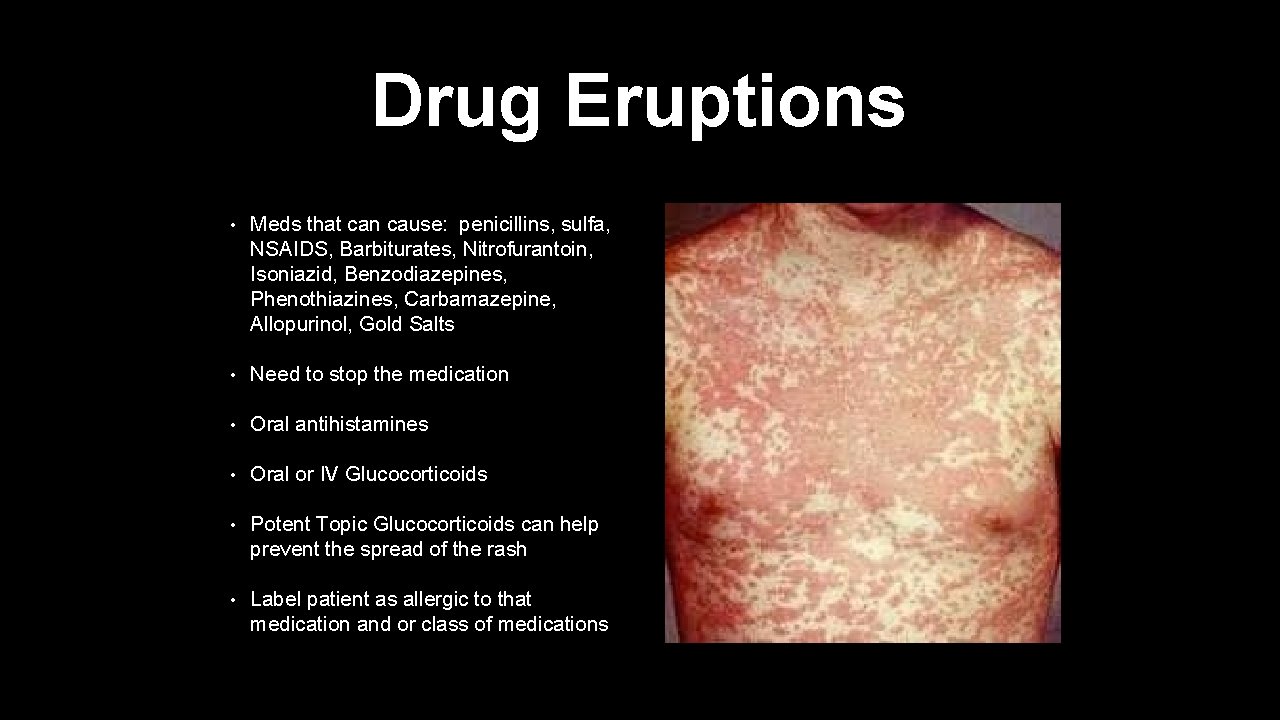
Drug Eruptions • Meds that can cause: penicillins, sulfa, NSAIDS, Barbiturates, Nitrofurantoin, Isoniazid, Benzodiazepines, Phenothiazines, Carbamazepine, Allopurinol, Gold Salts • Need to stop the medication • Oral antihistamines • Oral or IV Glucocorticoids • Potent Topic Glucocorticoids can help prevent the spread of the rash • Label patient as allergic to that medication and or class of medications
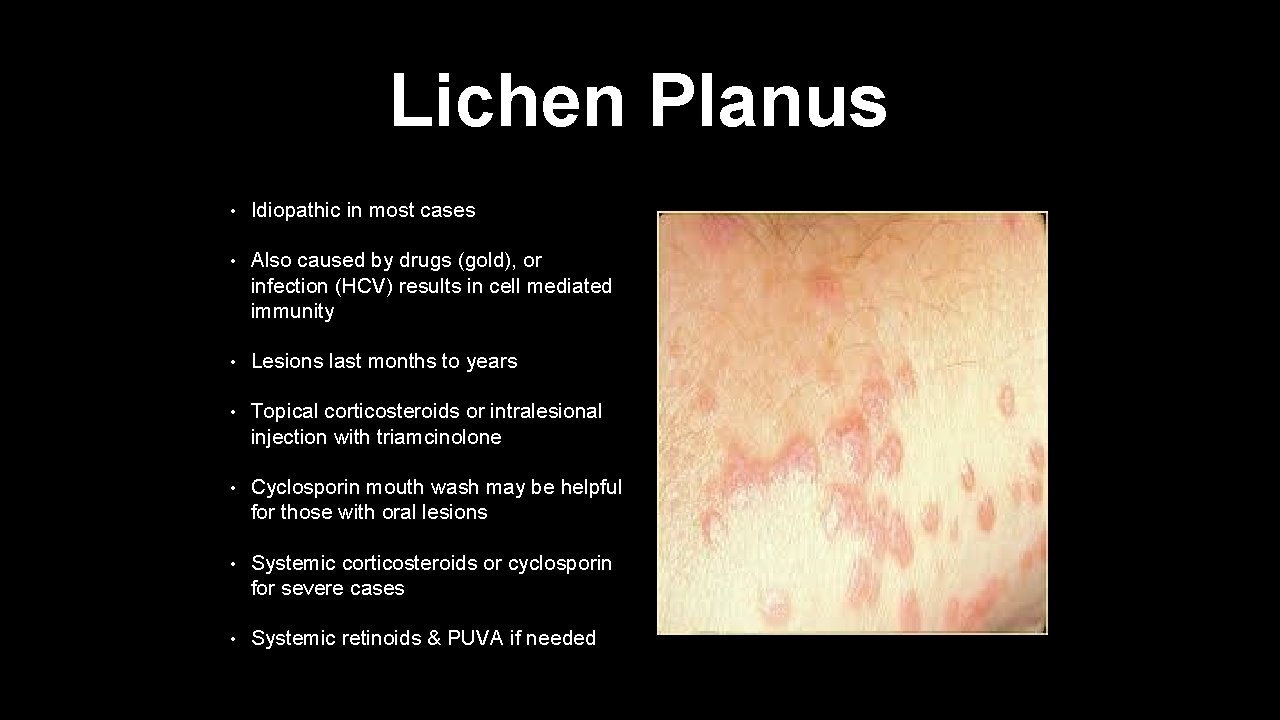
Lichen Planus • Idiopathic in most cases • Also caused by drugs (gold), or infection (HCV) results in cell mediated immunity • Lesions last months to years • Topical corticosteroids or intralesional injection with triamcinolone • Cyclosporin mouth wash may be helpful for those with oral lesions • Systemic corticosteroids or cyclosporin for severe cases • Systemic retinoids & PUVA if needed

Lichen Planus • Lesions last months to years • The 5 P’s of Lichen Planus- • -Purple • -Polygonal • -Papules • -Pruritic • -Planar
Desquamation
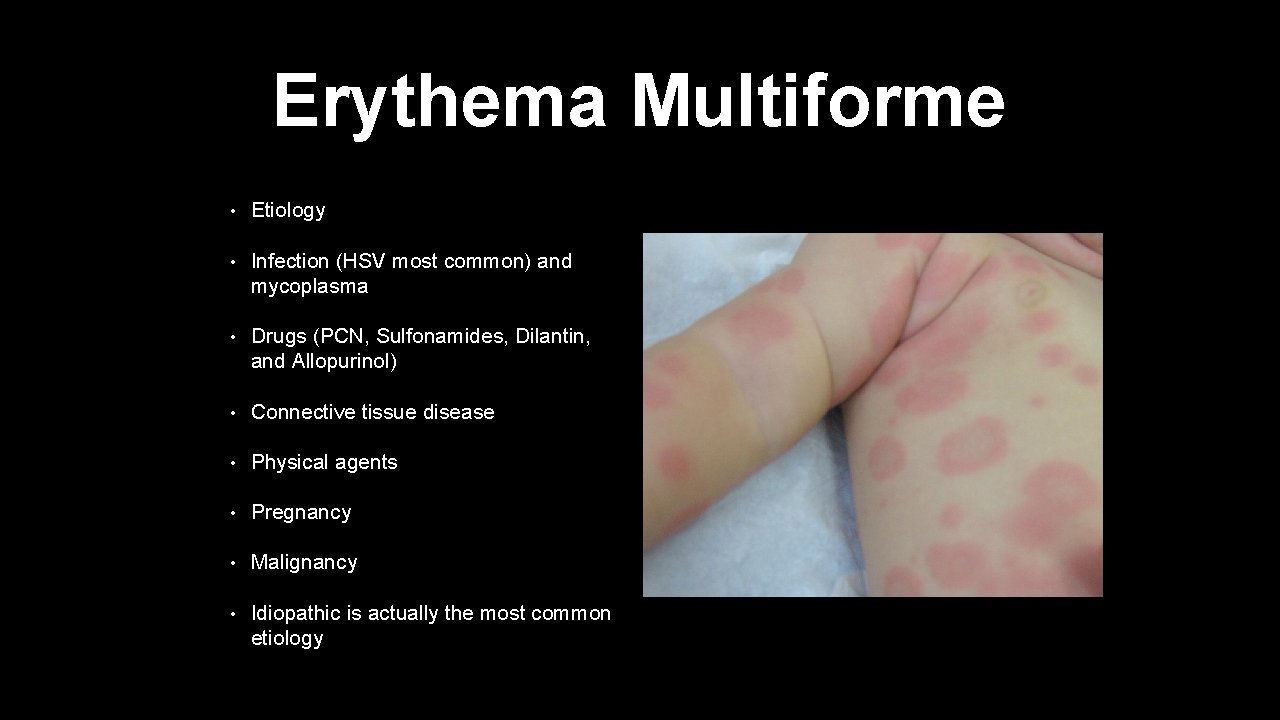
Erythema Multiforme • Etiology • Infection (HSV most common) and mycoplasma • Drugs (PCN, Sulfonamides, Dilantin, and Allopurinol) • Connective tissue disease • Physical agents • Pregnancy • Malignancy • Idiopathic is actually the most common etiology
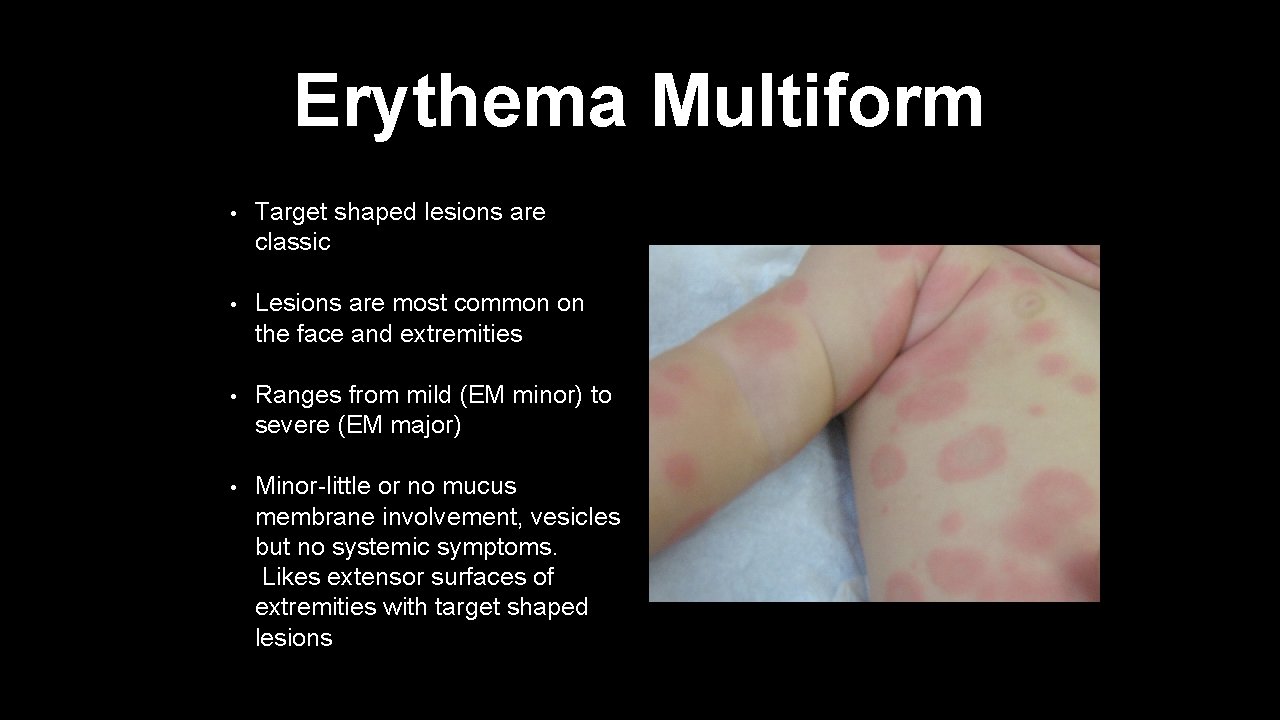
Erythema Multiform • Target shaped lesions are classic • Lesions are most common on the face and extremities • Ranges from mild (EM minor) to severe (EM major) • Minor-little or no mucus membrane involvement, vesicles but no systemic symptoms. Likes extensor surfaces of extremities with target shaped lesions
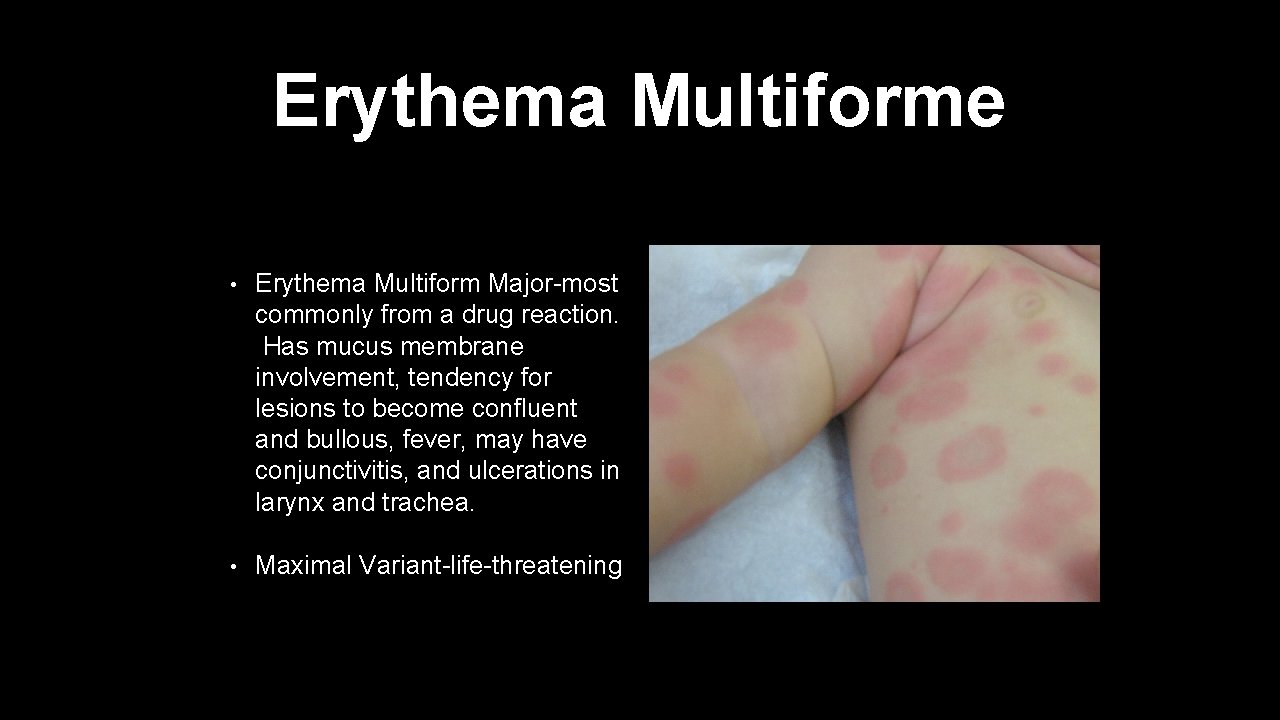
Erythema Multiforme • Erythema Multiform Major-most commonly from a drug reaction. Has mucus membrane involvement, tendency for lesions to become confluent and bullous, fever, may have conjunctivitis, and ulcerations in larynx and trachea. • Maximal Variant-life-threatening
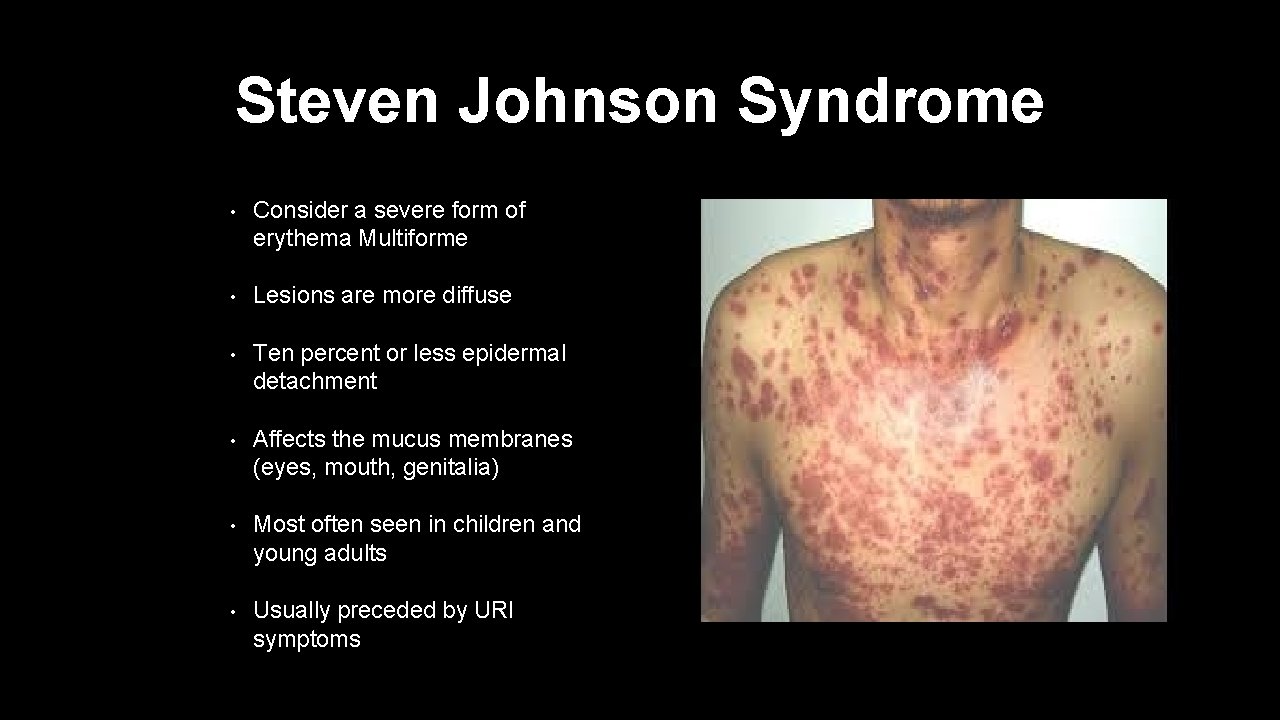
Steven Johnson Syndrome • Consider a severe form of erythema Multiforme • Lesions are more diffuse • Ten percent or less epidermal detachment • Affects the mucus membranes (eyes, mouth, genitalia) • Most often seen in children and young adults • Usually preceded by URI symptoms
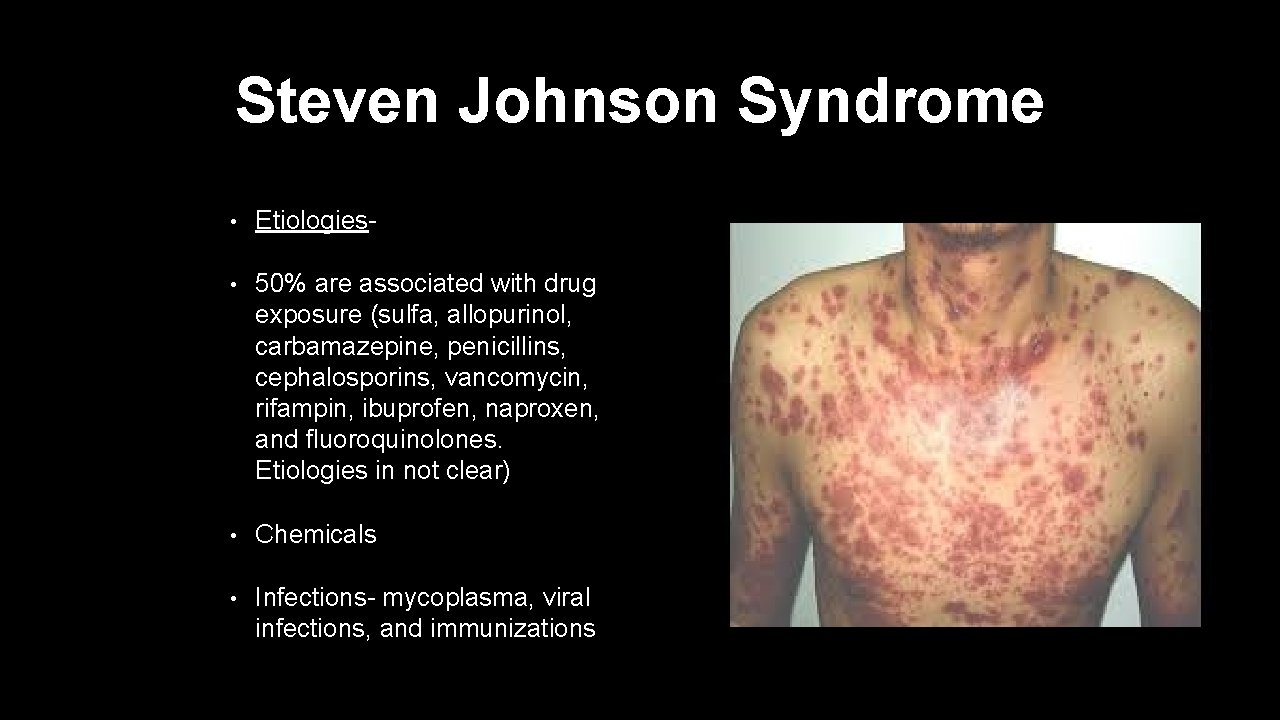
Steven Johnson Syndrome • Etiologies- • 50% are associated with drug exposure (sulfa, allopurinol, carbamazepine, penicillins, cephalosporins, vancomycin, rifampin, ibuprofen, naproxen, and fluoroquinolones. Etiologies in not clear) • Chemicals • Infections- mycoplasma, viral infections, and immunizations
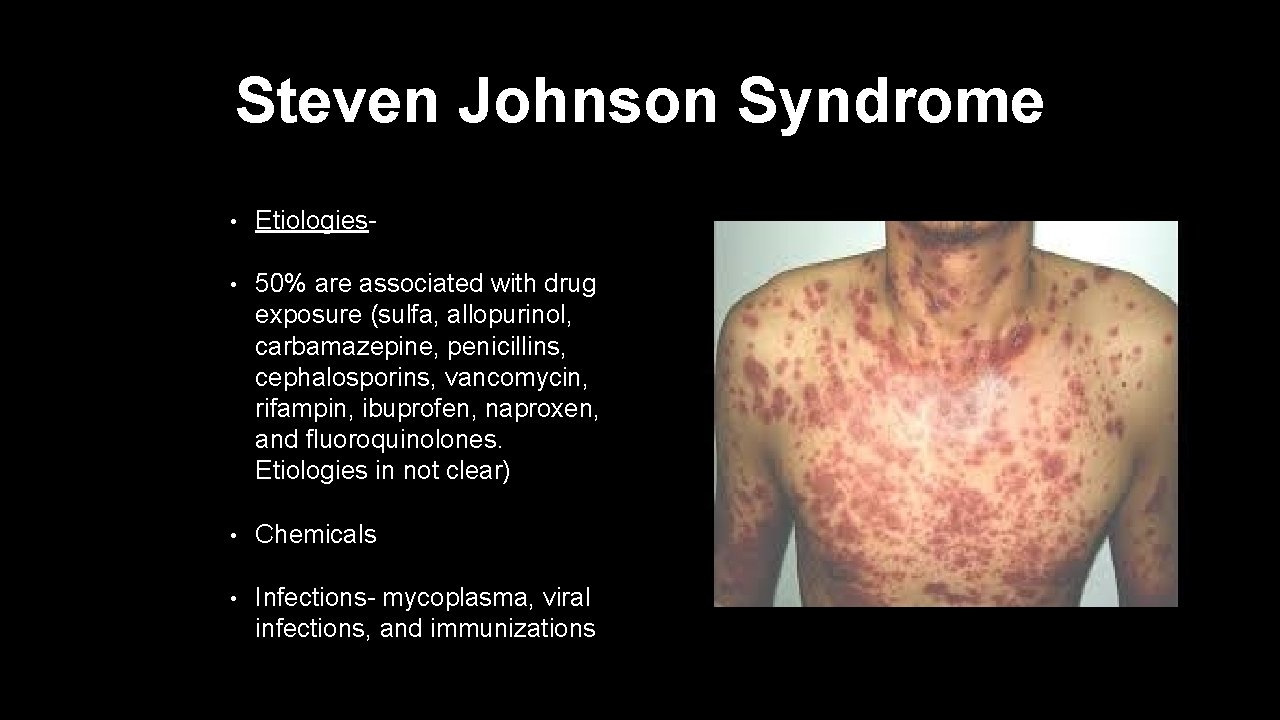
Steven Johnson Syndrome • Etiologies- • 50% are associated with drug exposure (sulfa, allopurinol, carbamazepine, penicillins, cephalosporins, vancomycin, rifampin, ibuprofen, naproxen, and fluoroquinolones. Etiologies in not clear) • Chemicals • Infections- mycoplasma, viral infections, and immunizations
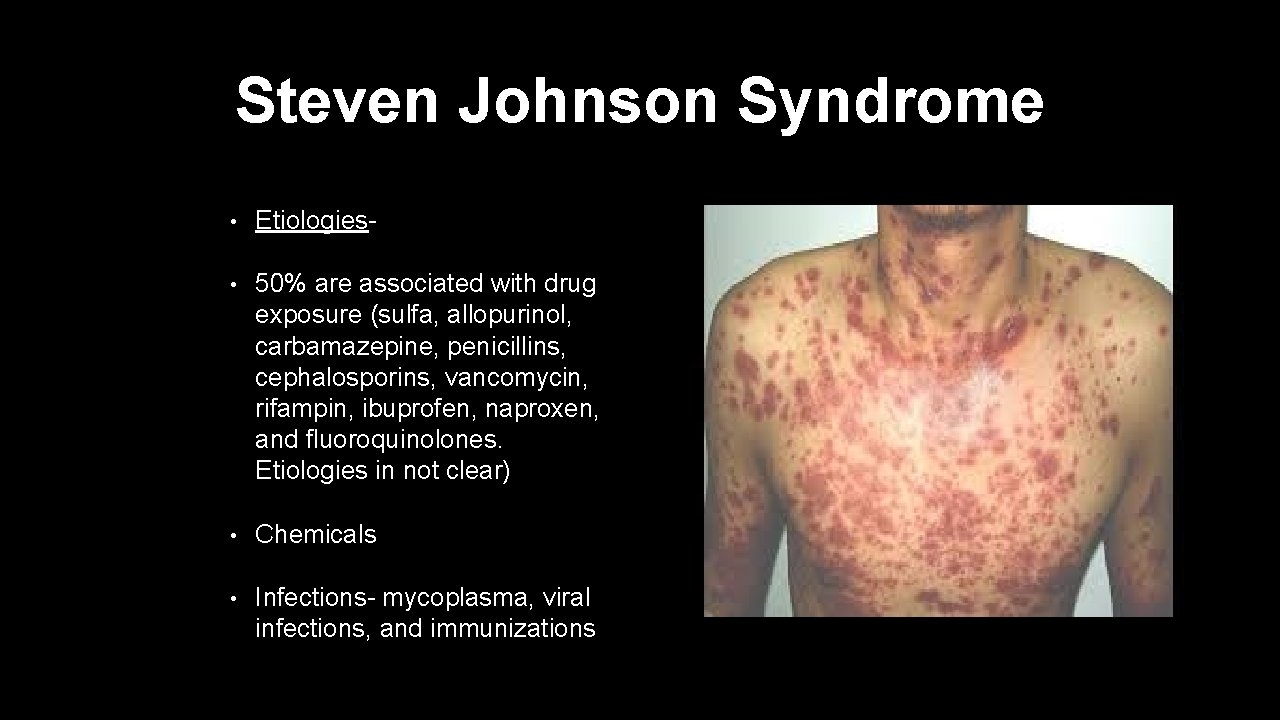
Steven Johnson Syndrome • Etiologies- • 50% are associated with drug exposure (sulfa, allopurinol, carbamazepine, penicillins, cephalosporins, vancomycin, rifampin, ibuprofen, naproxen, and fluoroquinolones. Etiologies in not clear) • Chemicals • Infections- mycoplasma, viral infections, and immunizations
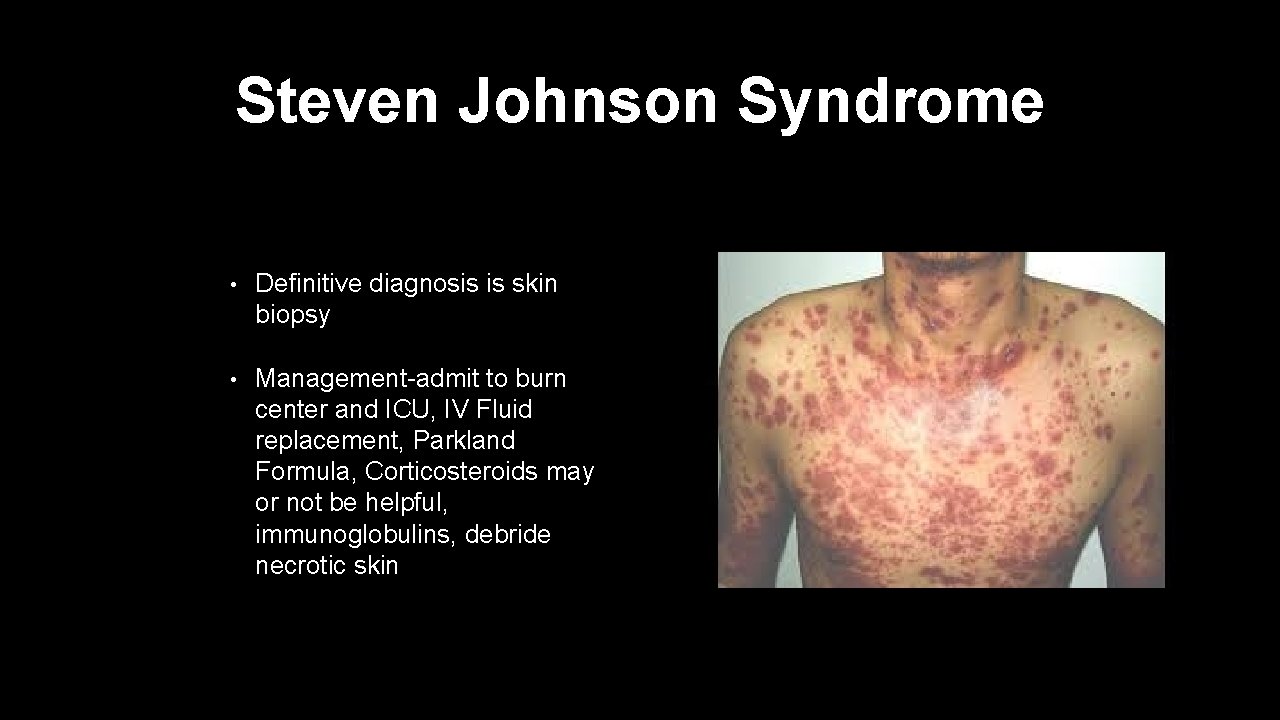
Steven Johnson Syndrome • Definitive diagnosis is skin biopsy • Management-admit to burn center and ICU, IV Fluid replacement, Parkland Formula, Corticosteroids may or not be helpful, immunoglobulins, debride necrotic skin
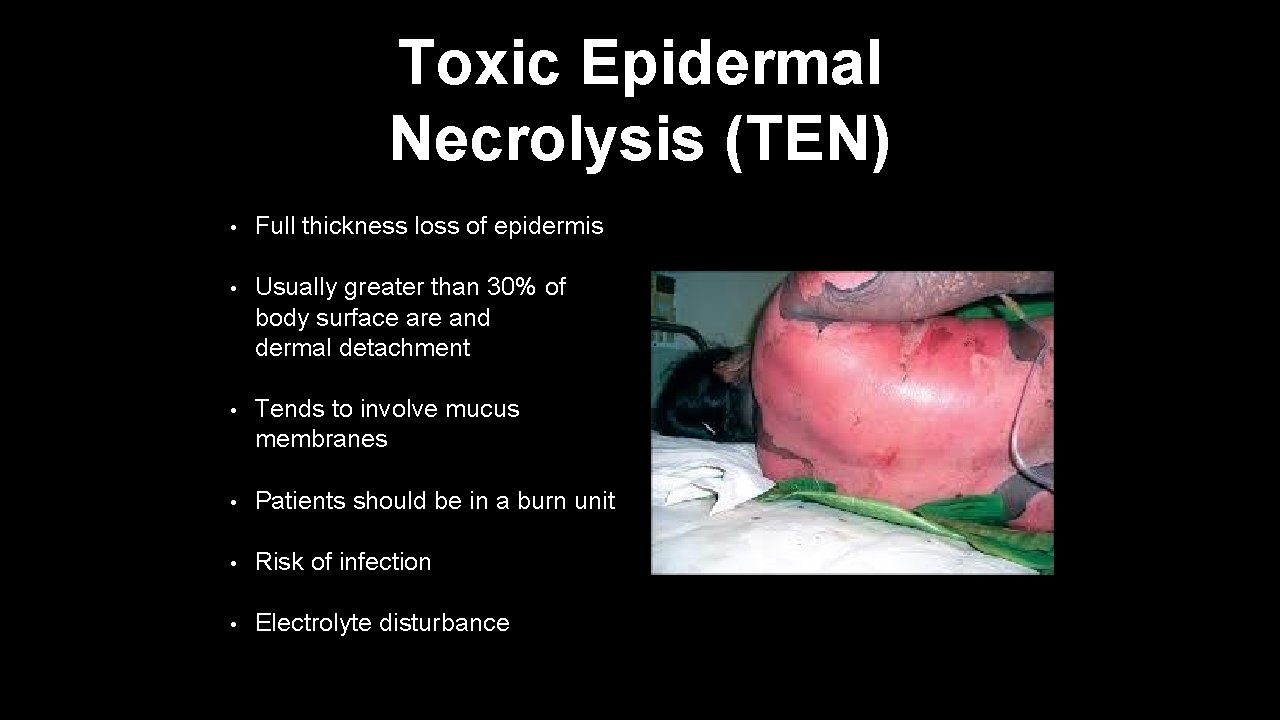
Toxic Epidermal Necrolysis (TEN) • Full thickness loss of epidermis • Usually greater than 30% of body surface are and dermal detachment • Tends to involve mucus membranes • Patients should be in a burn unit • Risk of infection • Electrolyte disturbance
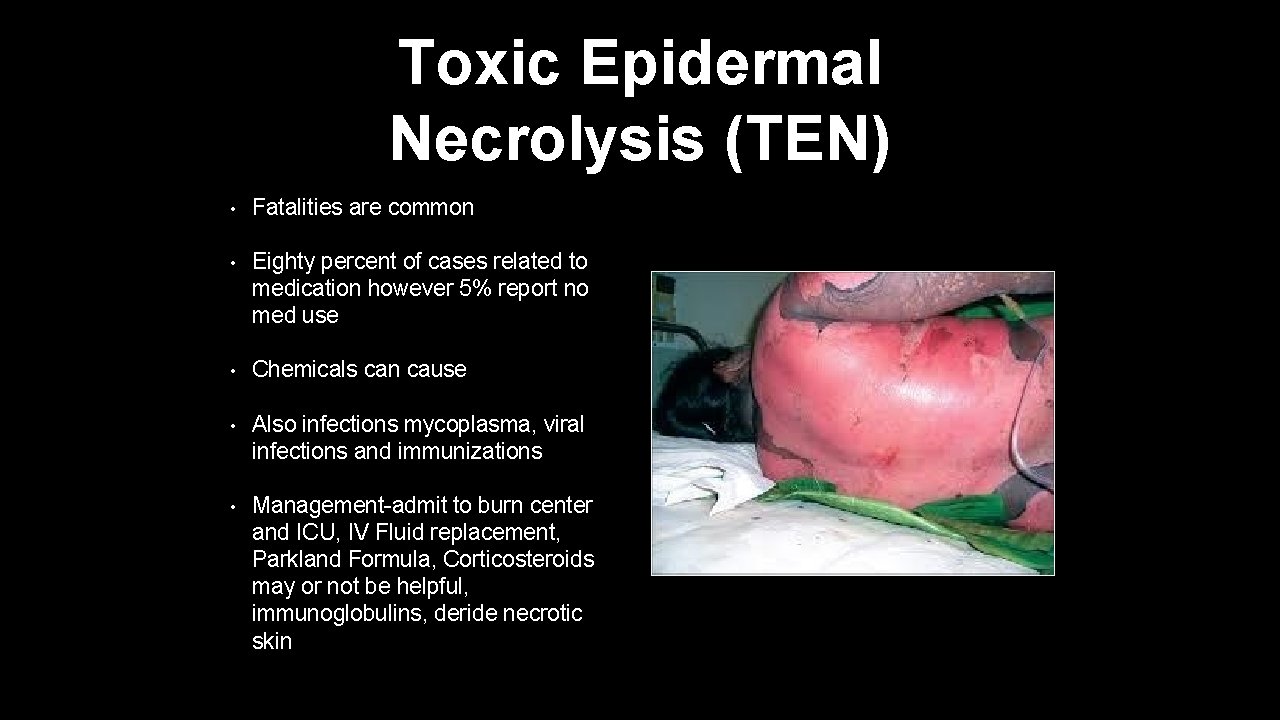
Toxic Epidermal Necrolysis (TEN) • Fatalities are common • Eighty percent of cases related to medication however 5% report no med use • Chemicals can cause • Also infections mycoplasma, viral infections and immunizations • Management-admit to burn center and ICU, IV Fluid replacement, Parkland Formula, Corticosteroids may or not be helpful, immunoglobulins, deride necrotic skin
Vesicular Bullae
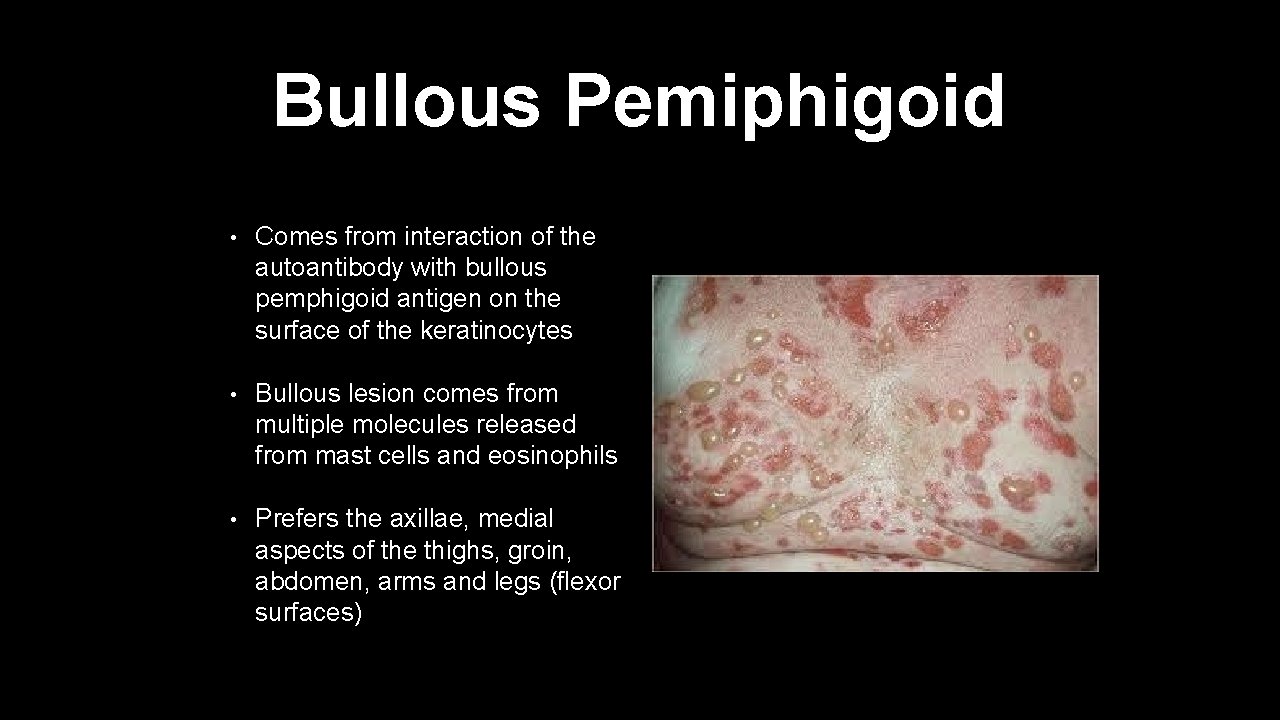
Bullous Pemiphigoid • Comes from interaction of the autoantibody with bullous pemphigoid antigen on the surface of the keratinocytes • Bullous lesion comes from multiple molecules released from mast cells and eosinophils • Prefers the axillae, medial aspects of the thighs, groin, abdomen, arms and legs (flexor surfaces)
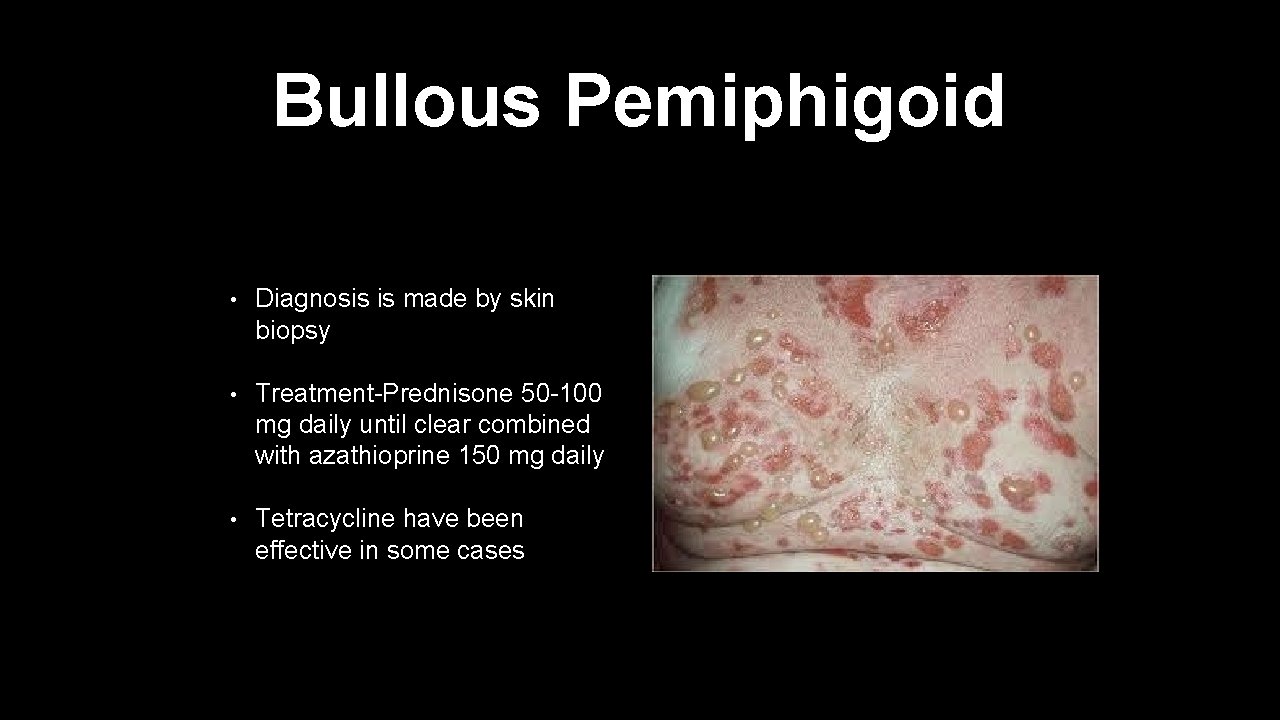
Bullous Pemiphigoid • Diagnosis is made by skin biopsy • Treatment-Prednisone 50 -100 mg daily until clear combined with azathioprine 150 mg daily • Tetracycline have been effective in some cases
Acneiform Lesions
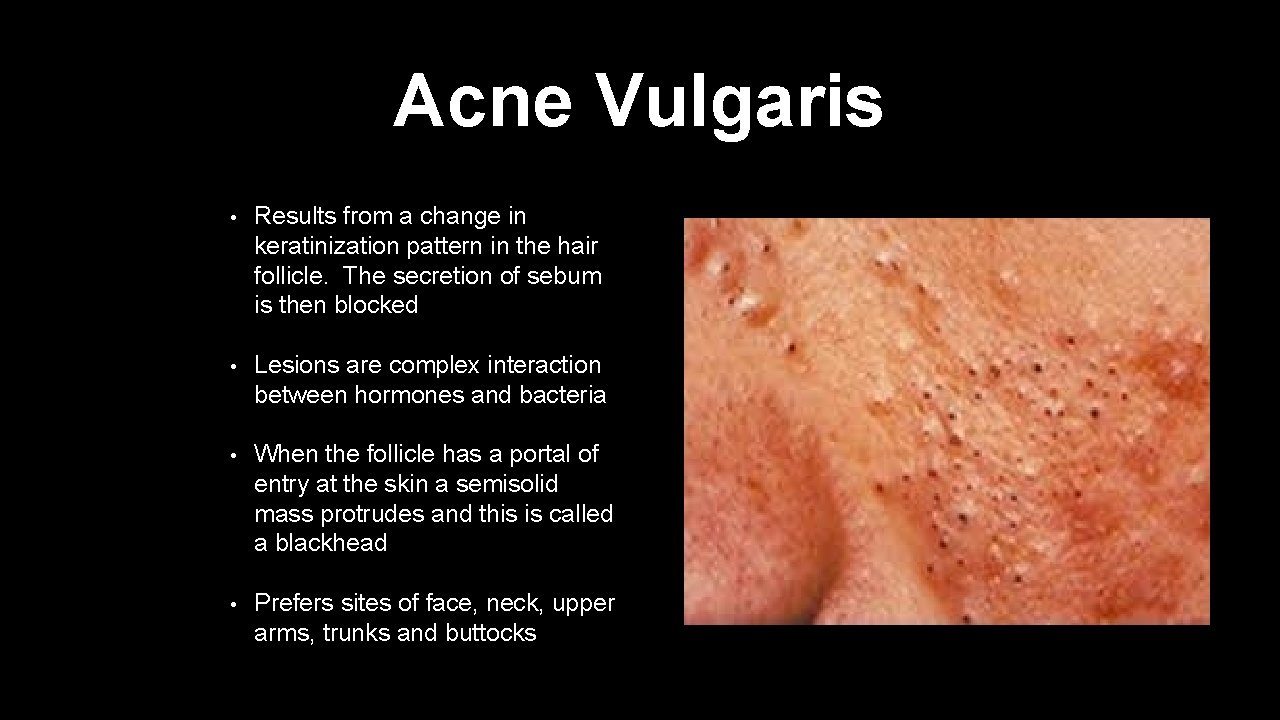
Acne Vulgaris • Results from a change in keratinization pattern in the hair follicle. The secretion of sebum is then blocked • Lesions are complex interaction between hormones and bacteria • When the follicle has a portal of entry at the skin a semisolid mass protrudes and this is called a blackhead • Prefers sites of face, neck, upper arms, trunks and buttocks
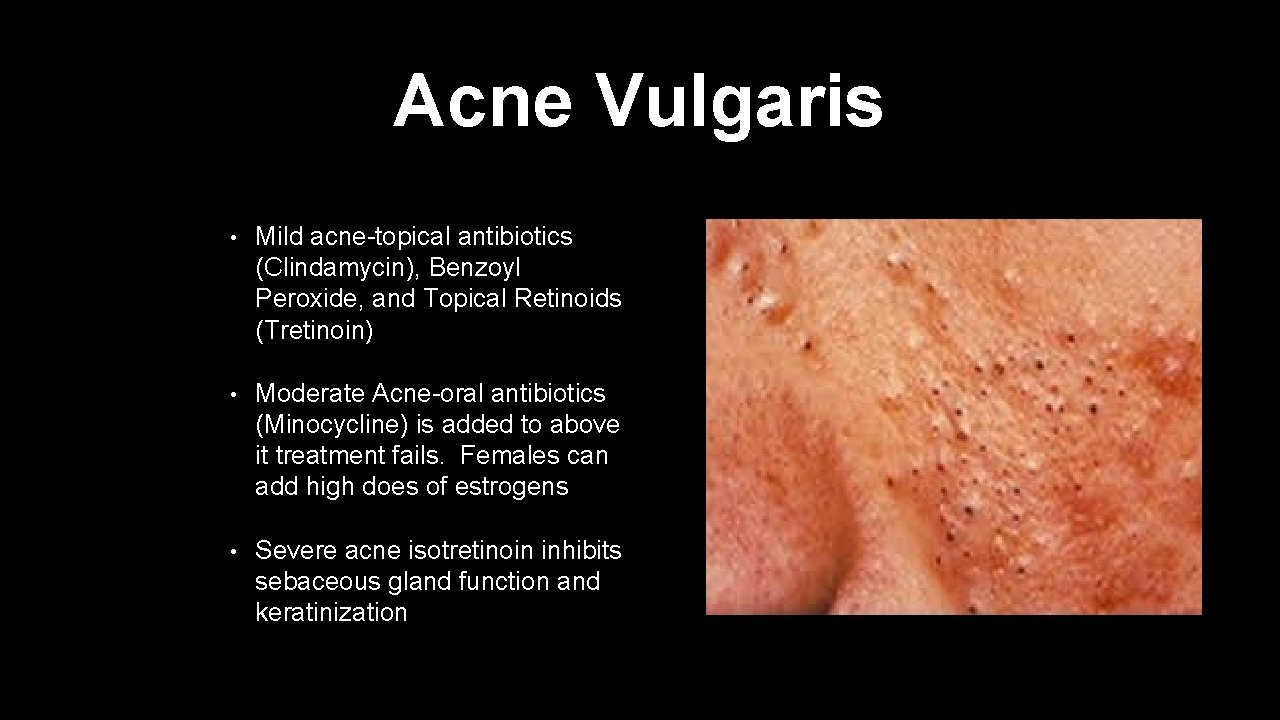
Acne Vulgaris • Mild acne-topical antibiotics (Clindamycin), Benzoyl Peroxide, and Topical Retinoids (Tretinoin) • Moderate Acne-oral antibiotics (Minocycline) is added to above it treatment fails. Females can add high does of estrogens • Severe acne isotretinoin inhibits sebaceous gland function and keratinization
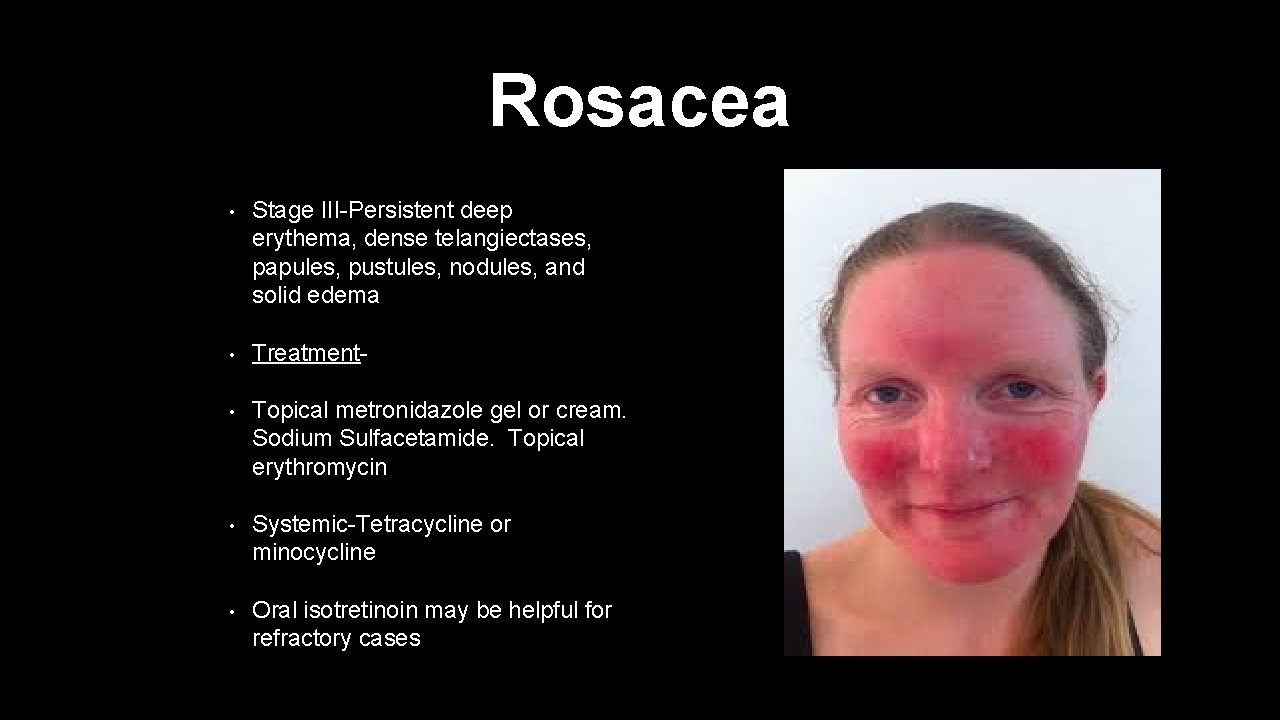
Rosacea • Stage III-Persistent deep erythema, dense telangiectases, papules, pustules, nodules, and solid edema • Treatment- • Topical metronidazole gel or cream. Sodium Sulfacetamide. Topical erythromycin • Systemic-Tetracycline or minocycline • Oral isotretinoin may be helpful for refractory cases
Verrucous Lesions
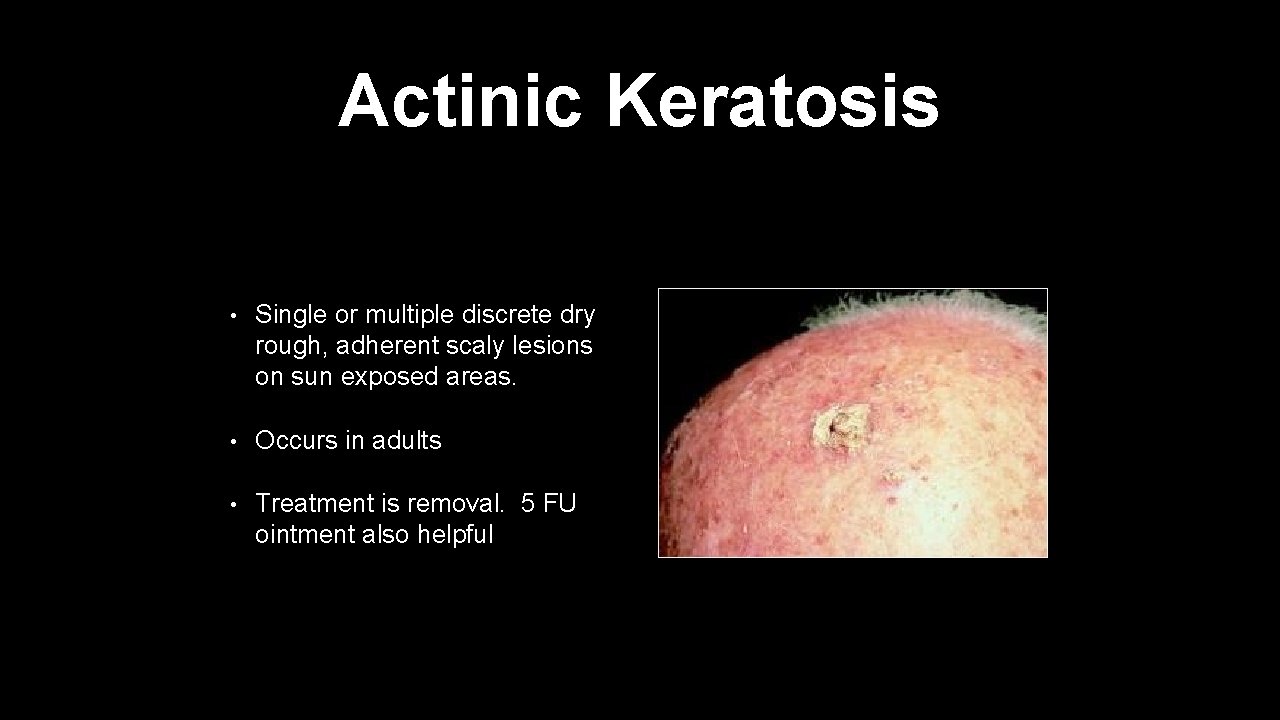
Actinic Keratosis • Single or multiple discrete dry rough, adherent scaly lesions on sun exposed areas. • Occurs in adults • Treatment is removal. 5 FU ointment also helpful
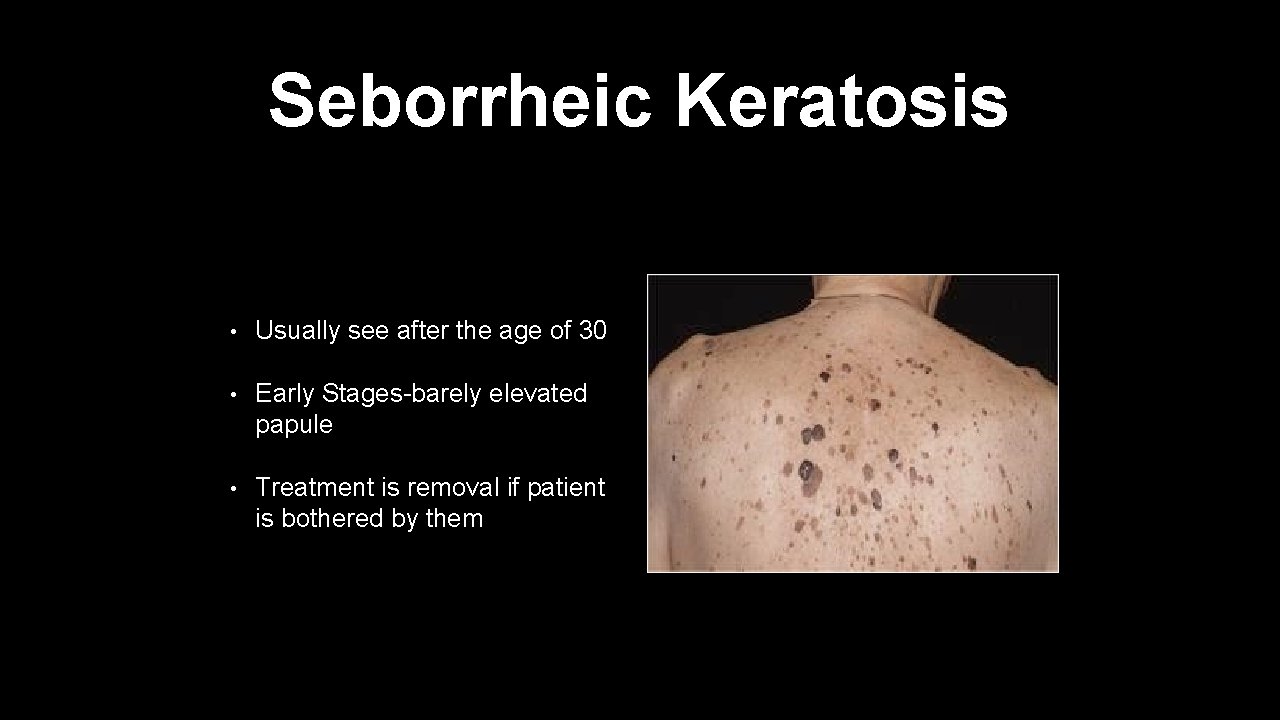
Seborrheic Keratosis • Usually see after the age of 30 • Early Stages-barely elevated papule • Treatment is removal if patient is bothered by them
Insects/Parasites
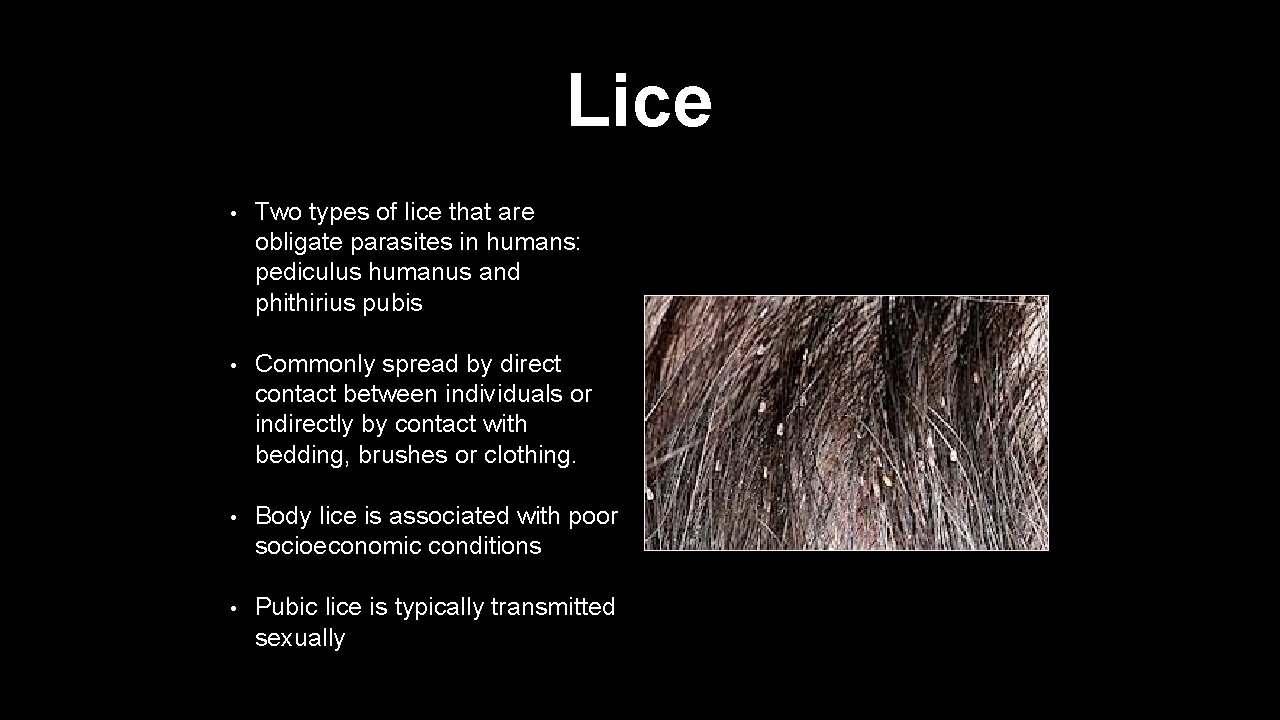
Lice • Two types of lice that are obligate parasites in humans: pediculus humanus and phithirius pubis • Commonly spread by direct contact between individuals or indirectly by contact with bedding, brushes or clothing. • Body lice is associated with poor socioeconomic conditions • Pubic lice is typically transmitted sexually

Lice • Pubic lice may not be transmitted sexually also. Transmitted from pubic lice in hair on head and back • Itches and excoriations can get infected. • Pediculosis Capitis- lice infection of the scalp • Pediculosis Pubis-pubic lice • Treatment avoid contact with contaminated items, environment should be vacuumed. Permethrin, Malathion, Lindane
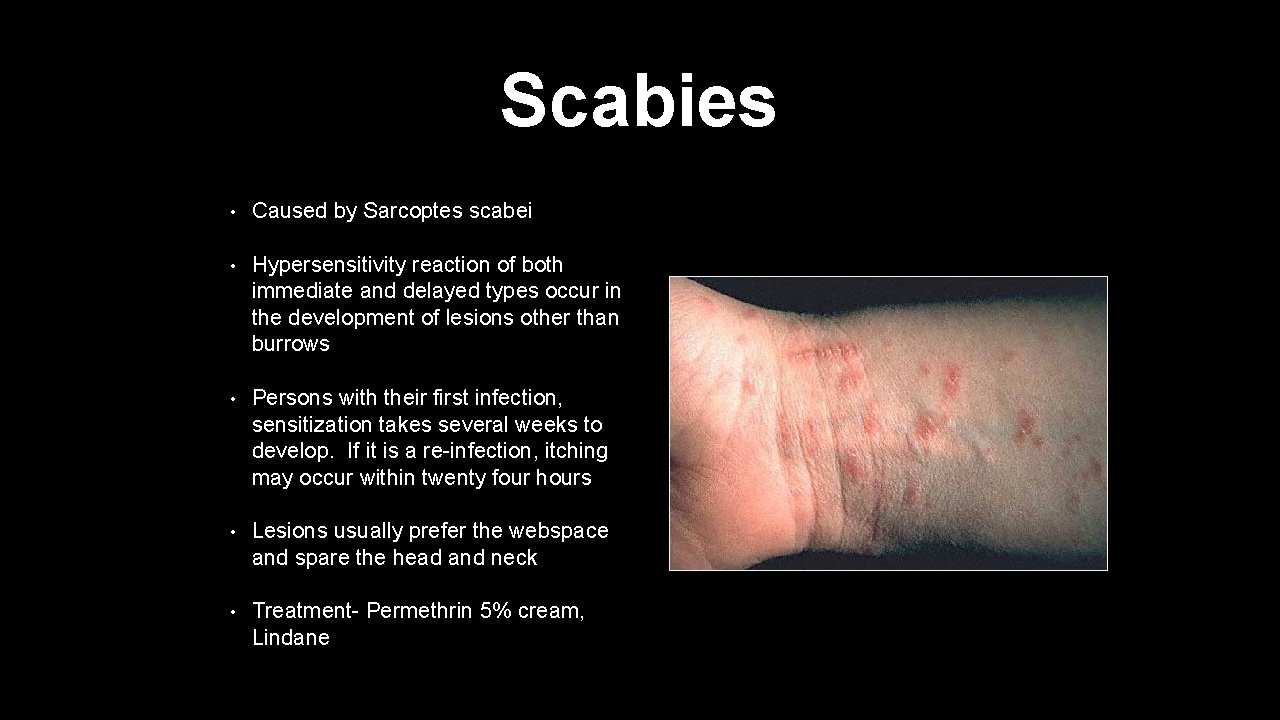
Scabies • Caused by Sarcoptes scabei • Hypersensitivity reaction of both immediate and delayed types occur in the development of lesions other than burrows • Persons with their first infection, sensitization takes several weeks to develop. If it is a re-infection, itching may occur within twenty four hours • Lesions usually prefer the webspace and spare the head and neck • Treatment- Permethrin 5% cream, Lindane
Spider Bites • Can easily be confused with a MRSA infection • Most spiders are harmless except brown recluse spider and the black widow spider • Can cause rashes from mild urticaria to full blown necrosis • The black widow spider venom has a neurotoxin producing reactions at the bite site to varying degrees of systemic reactions
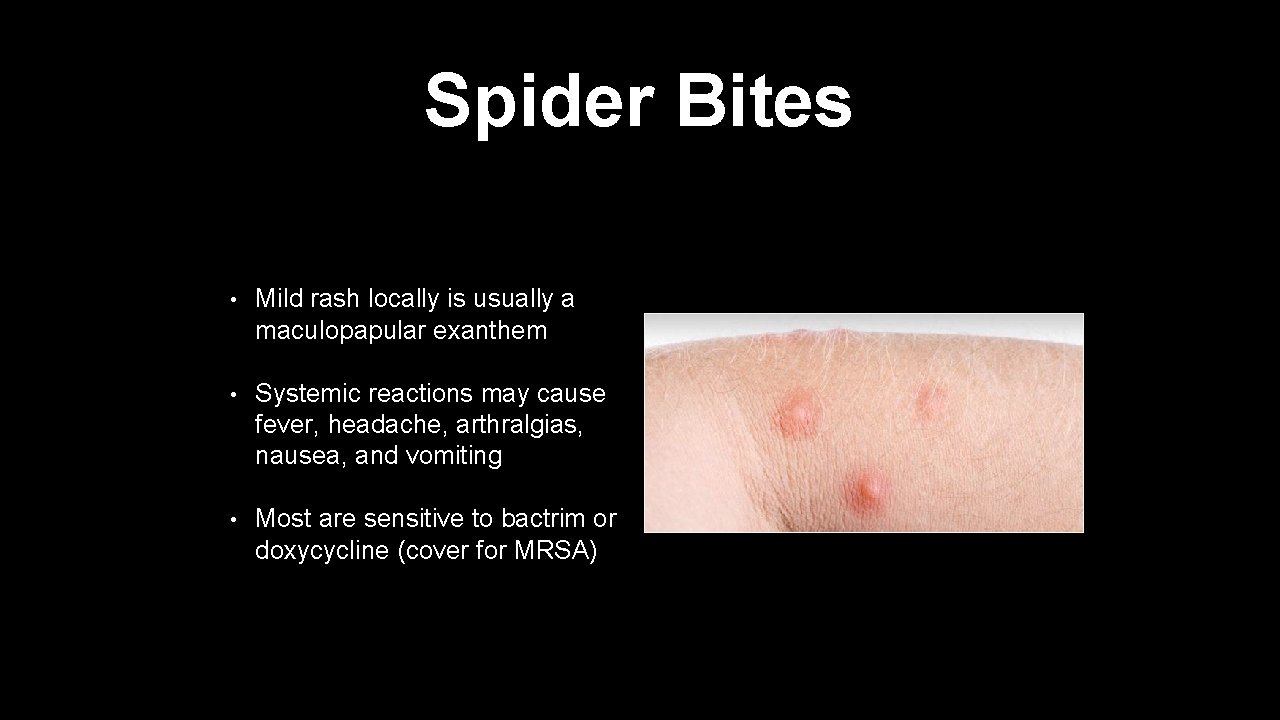
Spider Bites • Mild rash locally is usually a maculopapular exanthem • Systemic reactions may cause fever, headache, arthralgias, nausea, and vomiting • Most are sensitive to bactrim or doxycycline (cover for MRSA)
Neoplasms
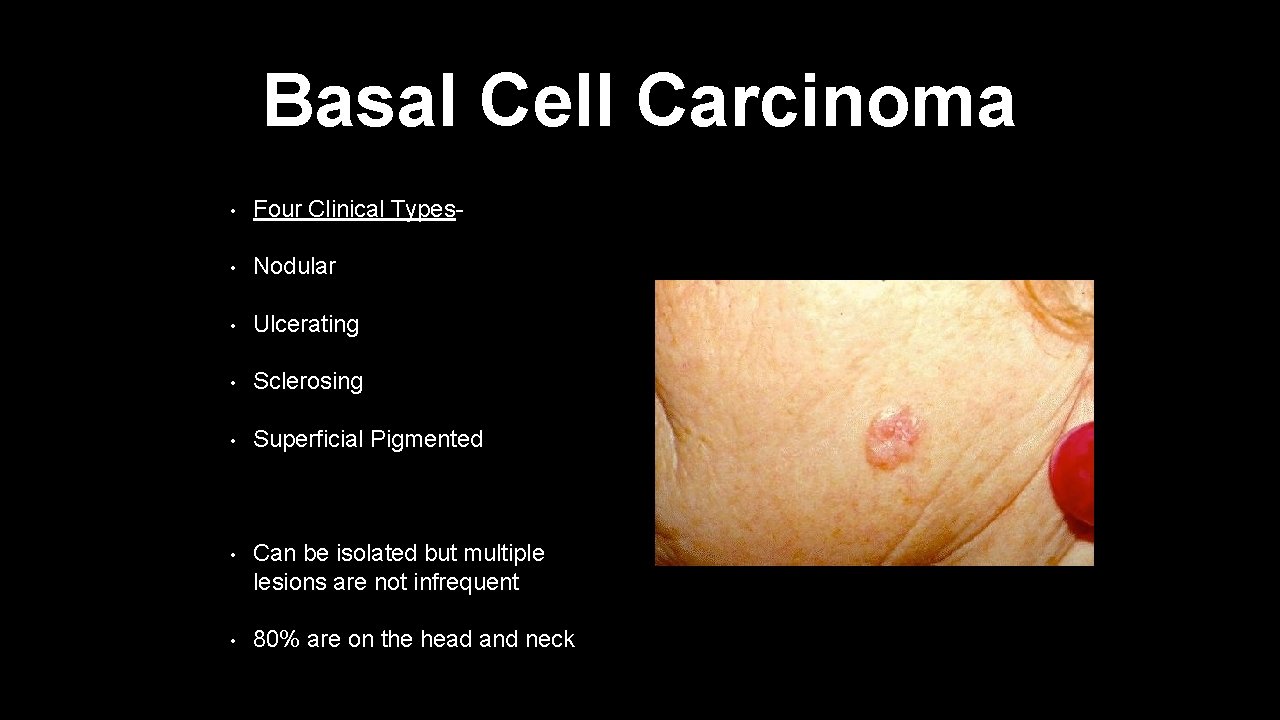
Basal Cell Carcinoma • Four Clinical Types- • Nodular • Ulcerating • Sclerosing • Superficial Pigmented • Can be isolated but multiple lesions are not infrequent • 80% are on the head and neck
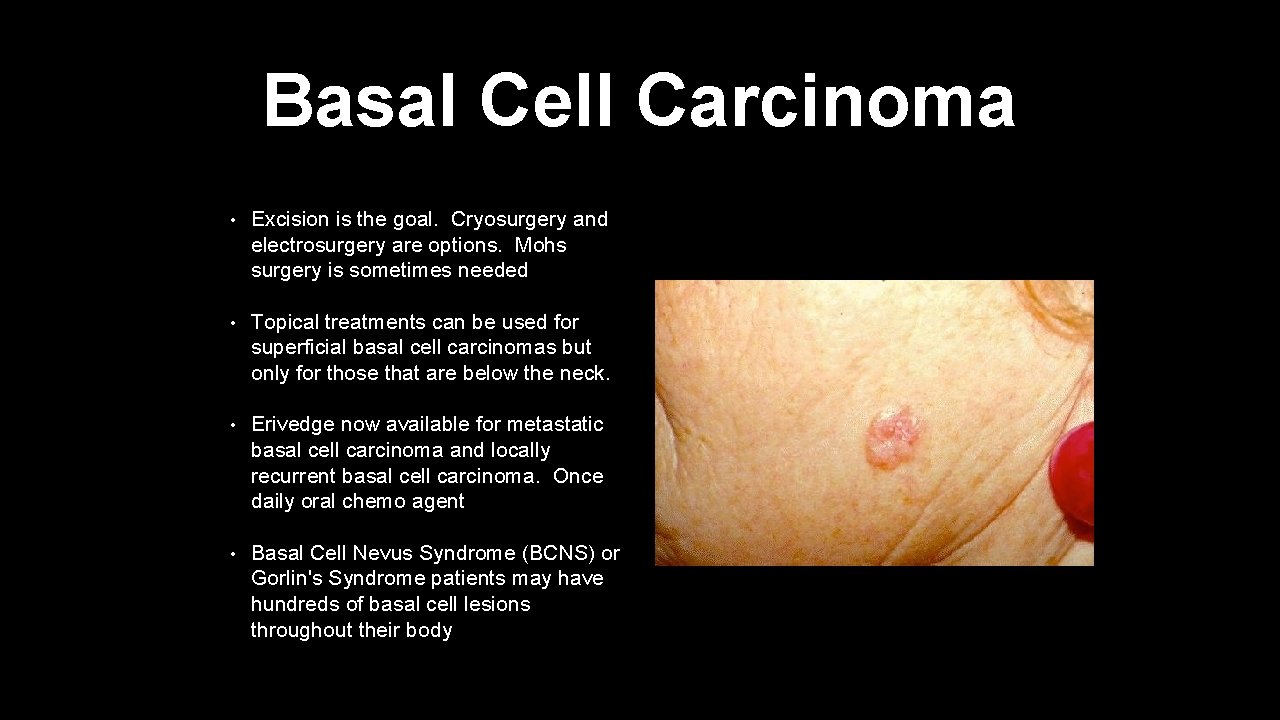
Basal Cell Carcinoma • Excision is the goal. Cryosurgery and electrosurgery are options. Mohs surgery is sometimes needed • Topical treatments can be used for superficial basal cell carcinomas but only for those that are below the neck. • Erivedge now available for metastatic basal cell carcinoma and locally recurrent basal cell carcinoma. Once daily oral chemo agent • Basal Cell Nevus Syndrome (BCNS) or Gorlin's Syndrome patients may have hundreds of basal cell lesions throughout their body
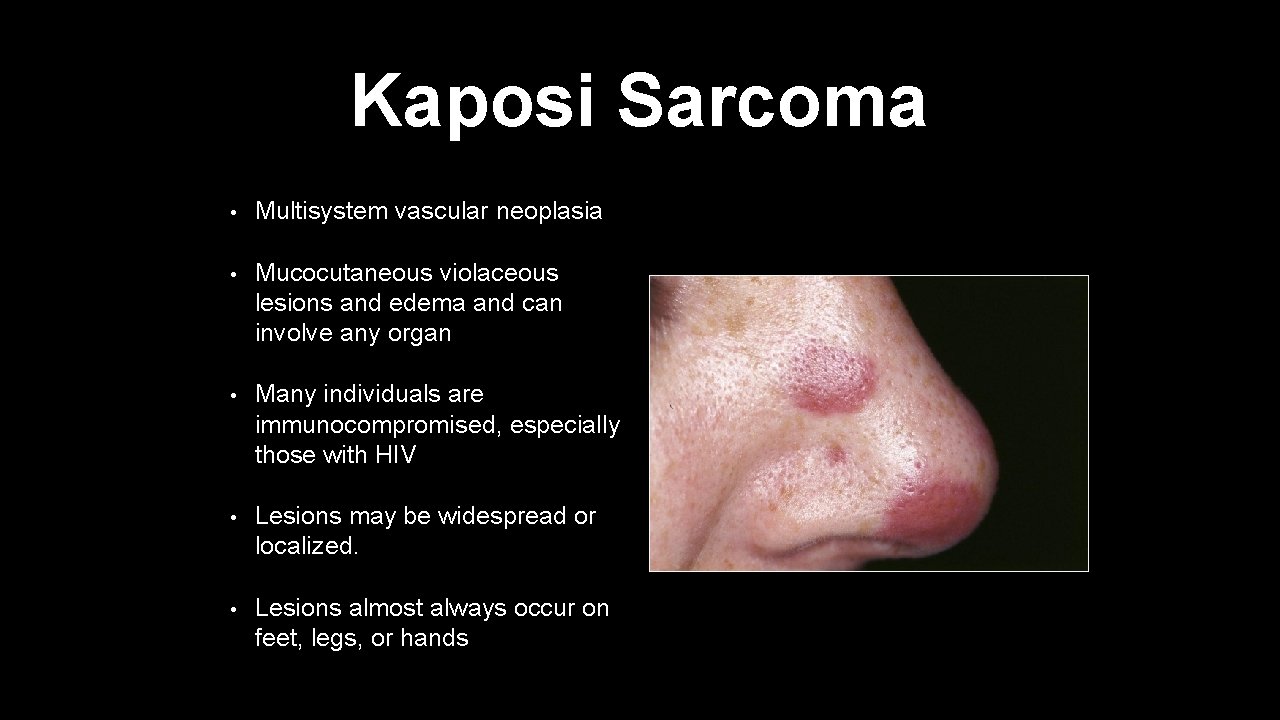
Kaposi Sarcoma • Multisystem vascular neoplasia • Mucocutaneous violaceous lesions and edema and can involve any organ • Many individuals are immunocompromised, especially those with HIV • Lesions may be widespread or localized. • Lesions almost always occur on feet, legs, or hands
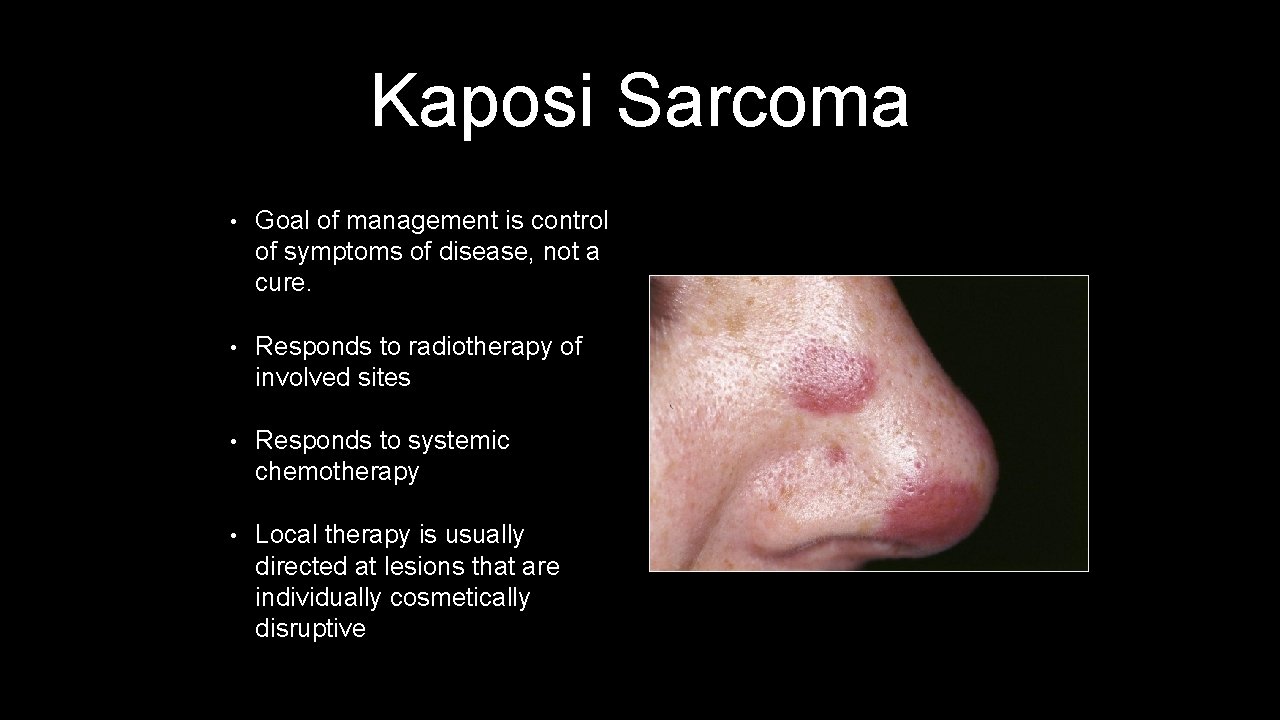
Kaposi Sarcoma • Goal of management is control of symptoms of disease, not a cure. • Responds to radiotherapy of involved sites • Responds to systemic chemotherapy • Local therapy is usually directed at lesions that are individually cosmetically disruptive
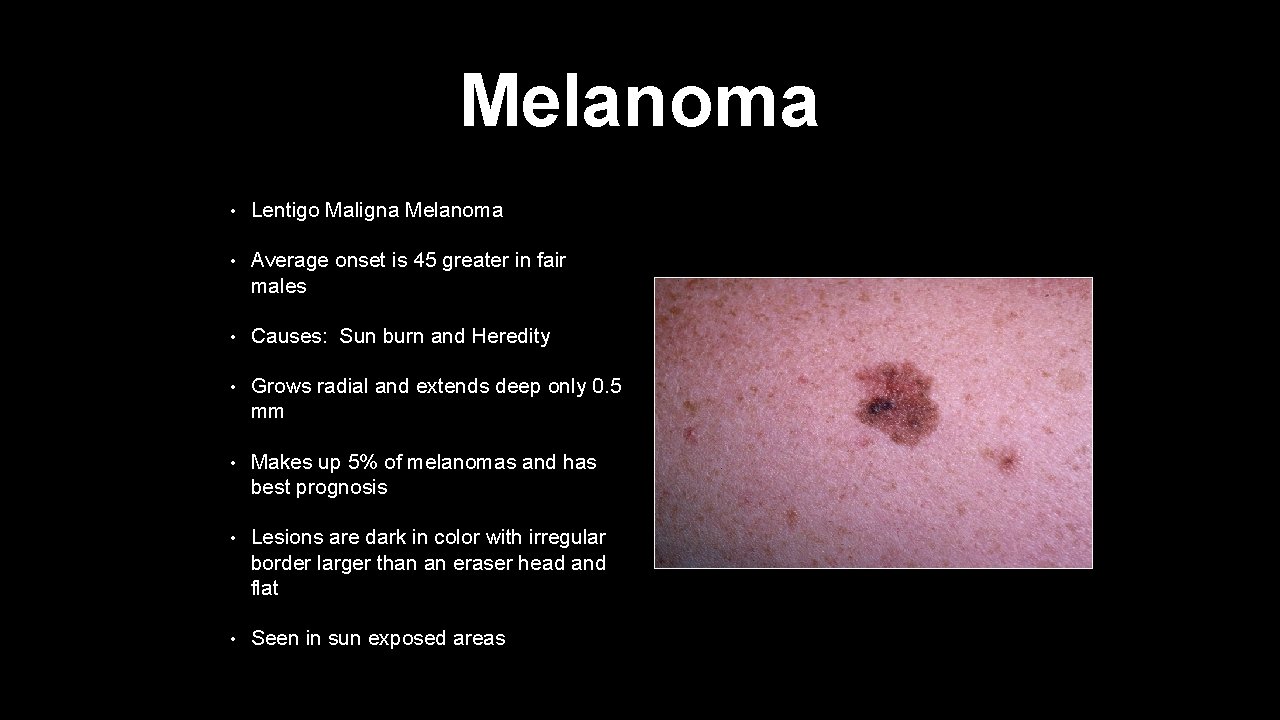
Melanoma • Lentigo Maligna Melanoma • Average onset is 45 greater in fair males • Causes: Sun burn and Heredity • Grows radial and extends deep only 0. 5 mm • Makes up 5% of melanomas and has best prognosis • Lesions are dark in color with irregular border larger than an eraser head and flat • Seen in sun exposed areas
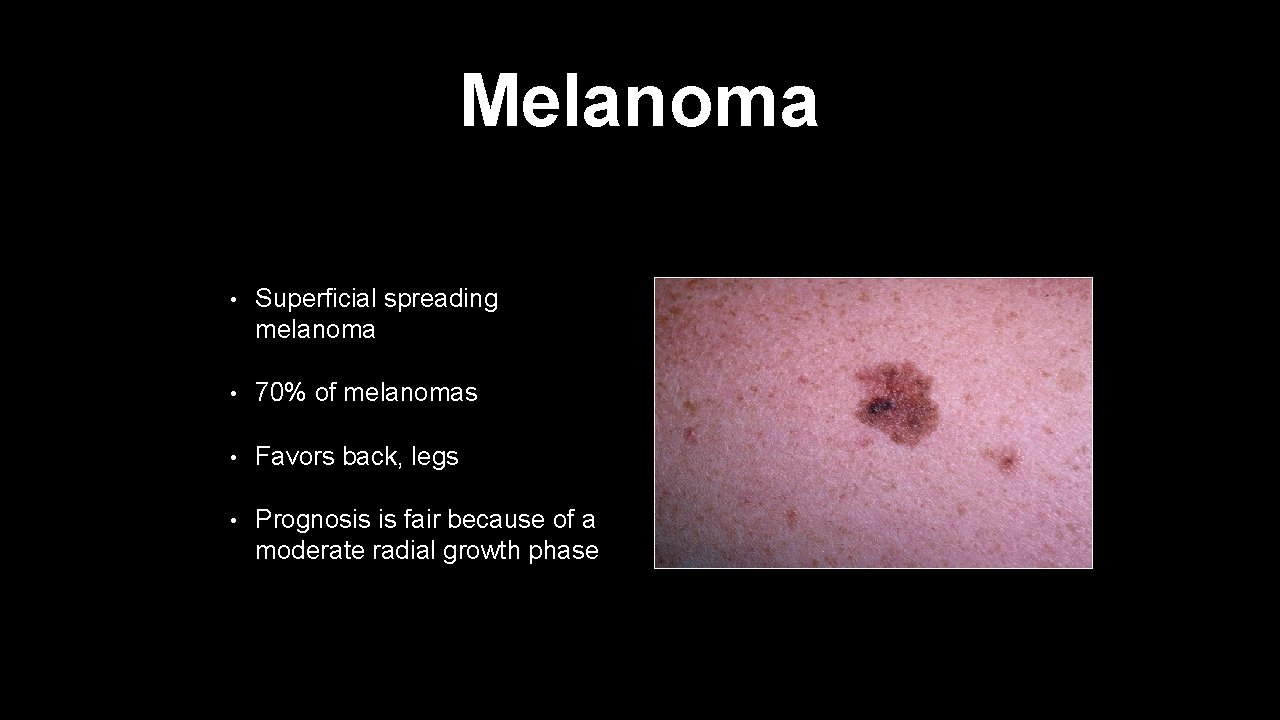
Melanoma • Superficial spreading melanoma • 70% of melanomas • Favors back, legs • Prognosis is fair because of a moderate radial growth phase
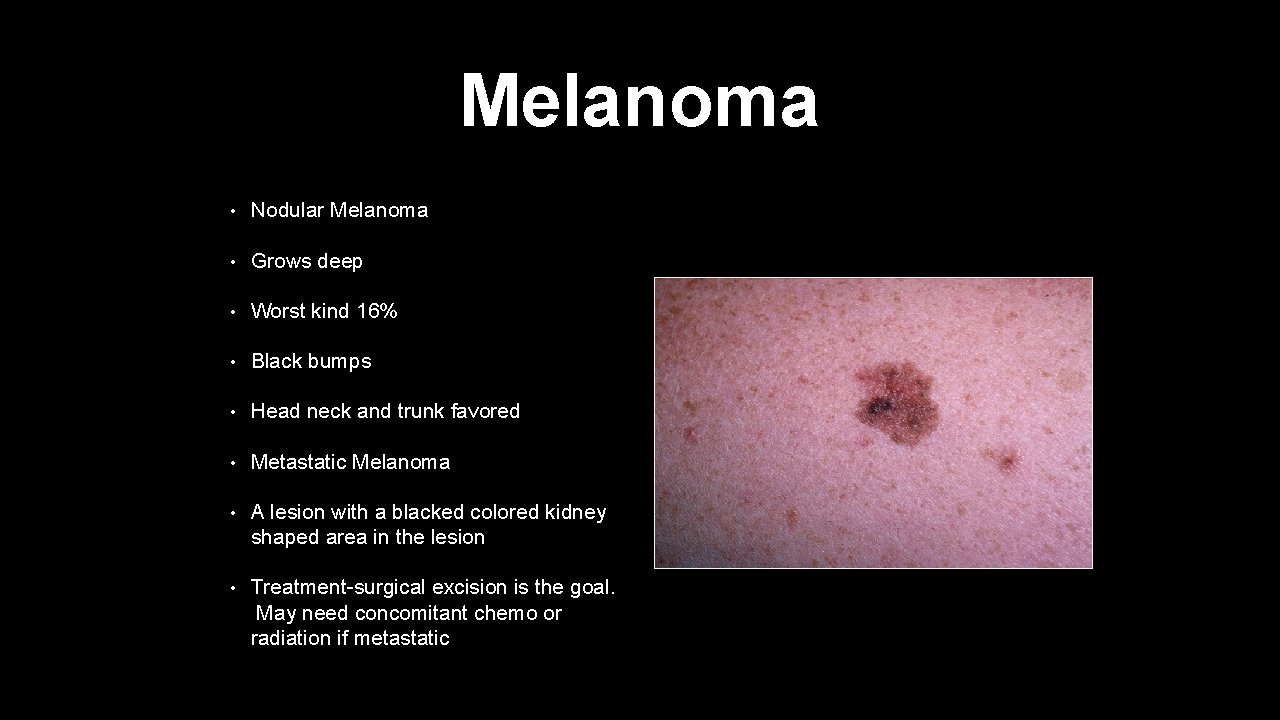
Melanoma • Nodular Melanoma • Grows deep • Worst kind 16% • Black bumps • Head neck and trunk favored • Metastatic Melanoma • A lesion with a blacked colored kidney shaped area in the lesion • Treatment-surgical excision is the goal. May need concomitant chemo or radiation if metastatic
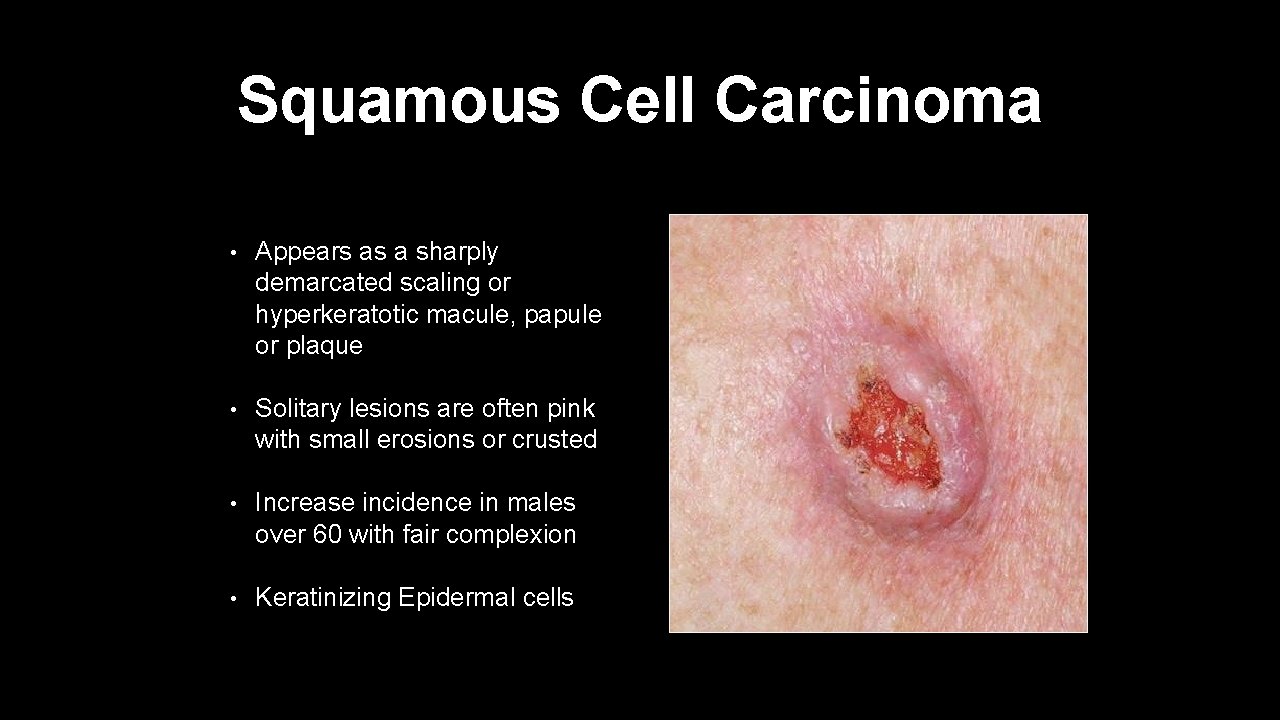
Squamous Cell Carcinoma • Appears as a sharply demarcated scaling or hyperkeratotic macule, papule or plaque • Solitary lesions are often pink with small erosions or crusted • Increase incidence in males over 60 with fair complexion • Keratinizing Epidermal cells

Squamous Cell Carcinoma • Ultraviolet rays cause cancer. HPV can also cause • Sun exposed areas rolled border with crust in the center • Can form cutaneous horn • Surgical excision is the goal. Cryotherapy or 5 FU topically can also be used
Hair and Nails

Alopecia • Several different types- • Alopecia Areata is considered an autoimmune disease. Causes patches of hair loss over weeks to months. Some may have spontaneous regrowth • Alopecia Universalis is global loss of hair, eyebrows, lashes, beard and all body hair.

Alopecia • Androgenic Alopecia-the most common progressive hairless that occurs through the combined effect of genetic predisposition and the action of androgen on the hair follicles of the scalp. • Treatment for androgenic alopecia involves oral finasteride, topical minoxidil, and anti androgens
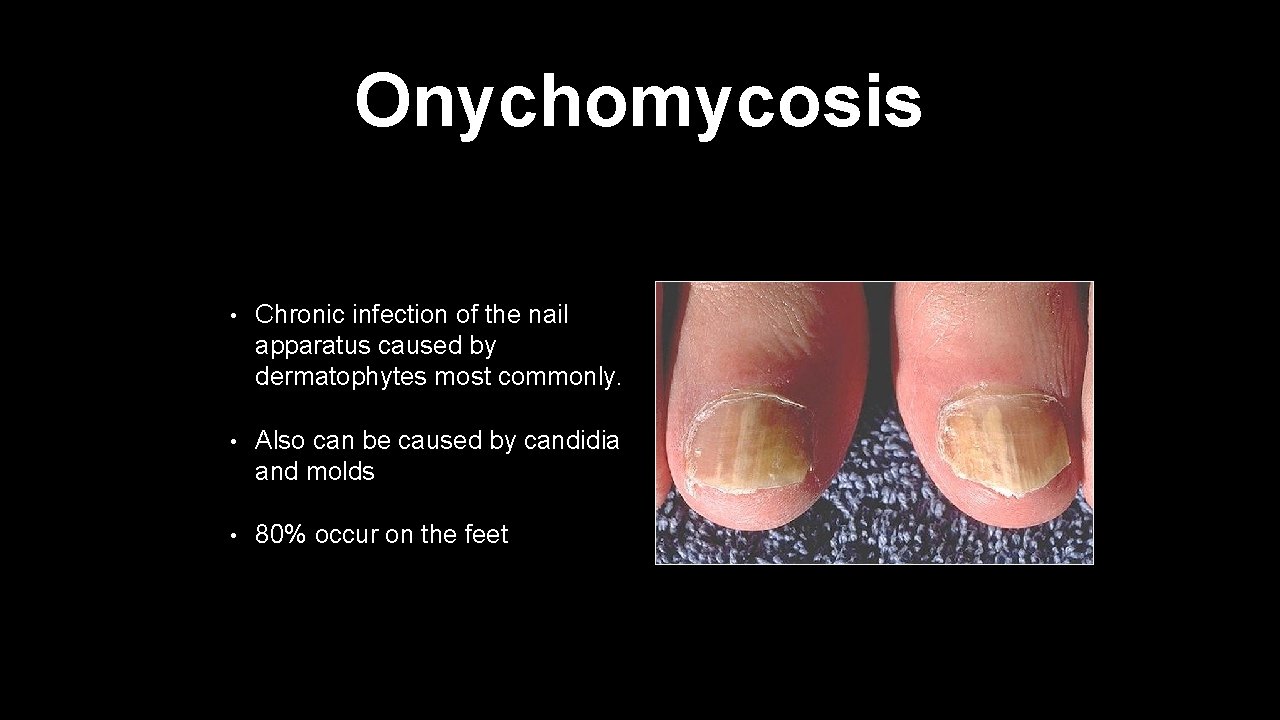
Onychomycosis • Chronic infection of the nail apparatus caused by dermatophytes most commonly. • Also can be caused by candidia and molds • 80% occur on the feet
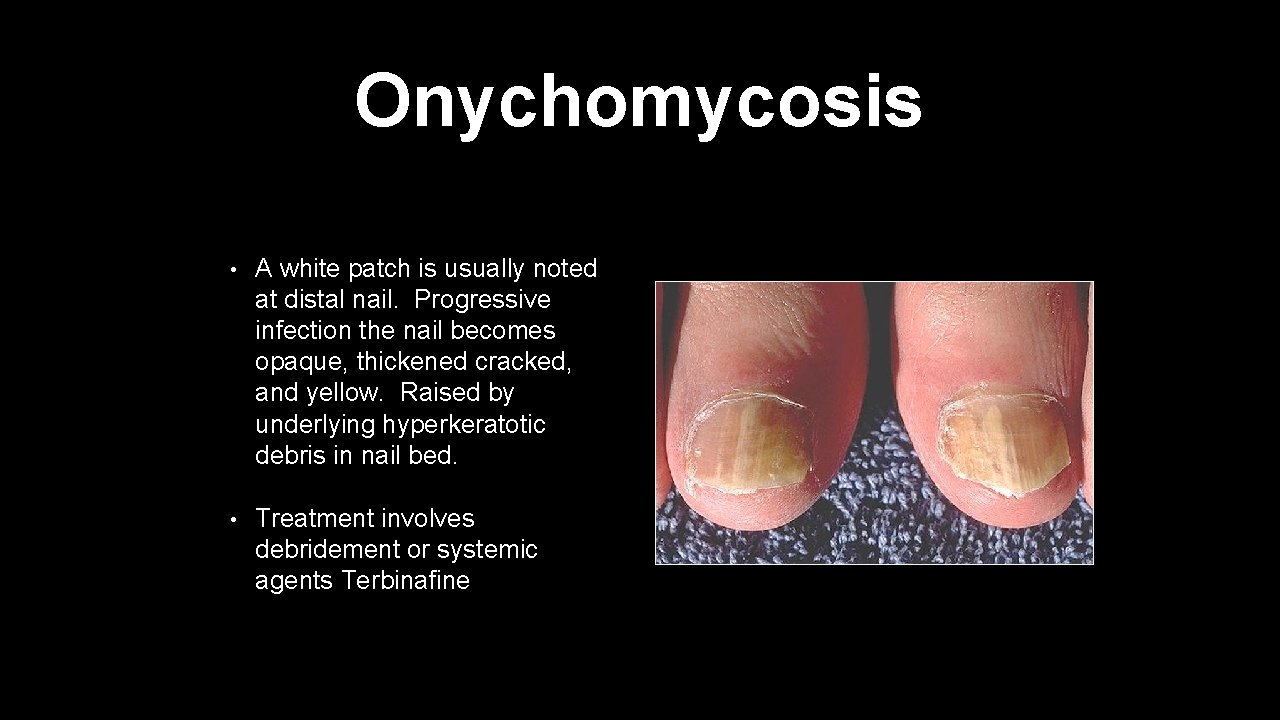
Onychomycosis • A white patch is usually noted at distal nail. Progressive infection the nail becomes opaque, thickened cracked, and yellow. Raised by underlying hyperkeratotic debris in nail bed. • Treatment involves debridement or systemic agents Terbinafine

Paronychia • Inflammation of the nail fold produces erythema, swelling, and throbbing pain and extend into the proximal nail fold and the eponychium • Purulent material accumulates and often requires surgical incision and drainage • Antimicrobial coverage with bactrim and cephalexin is necessary

Viral Diseases
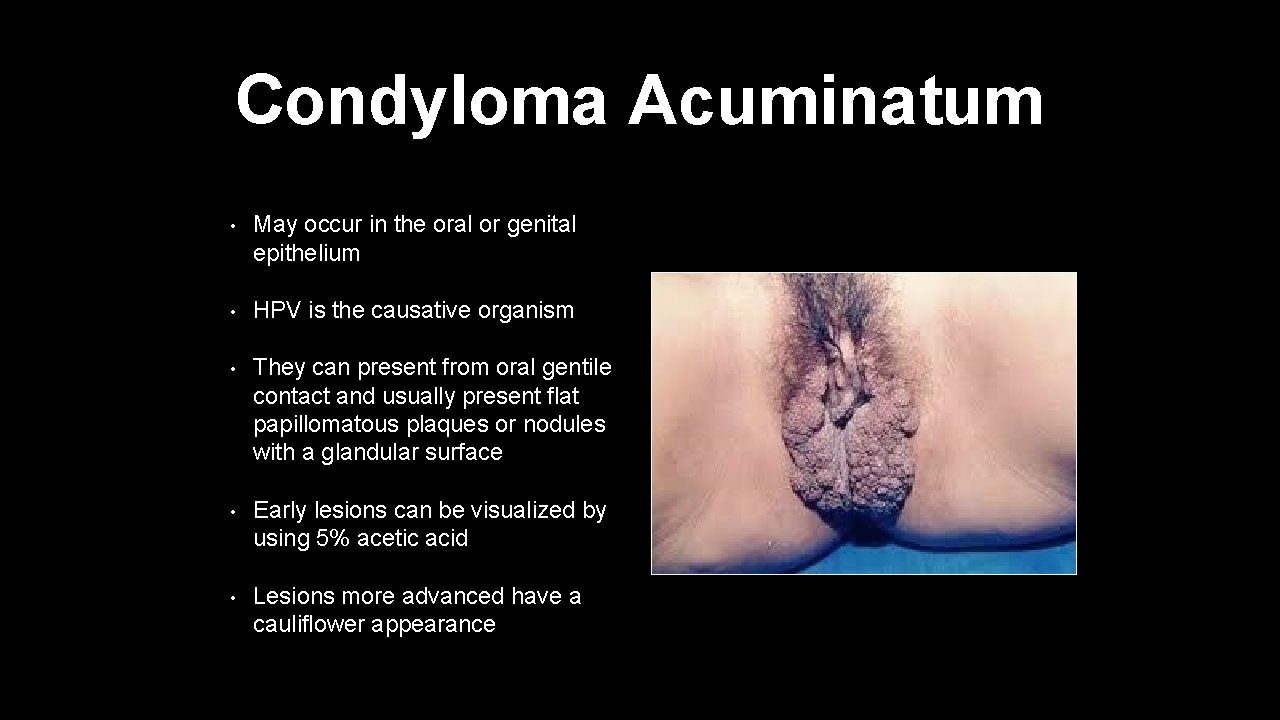
Condyloma Acuminatum • May occur in the oral or genital epithelium • HPV is the causative organism • They can present from oral gentile contact and usually present flat papillomatous plaques or nodules with a glandular surface • Early lesions can be visualized by using 5% acetic acid • Lesions more advanced have a cauliflower appearance
Exanthems • An infections generalized skin eruption associated with a primary systemic infection. • Most common they are viral in nature, but can be associated with bacteria and parasites. • Examples of Exanthems- • Rubella • Measles • Hand Foot and Mouth Disease • Erythema Infectiosum
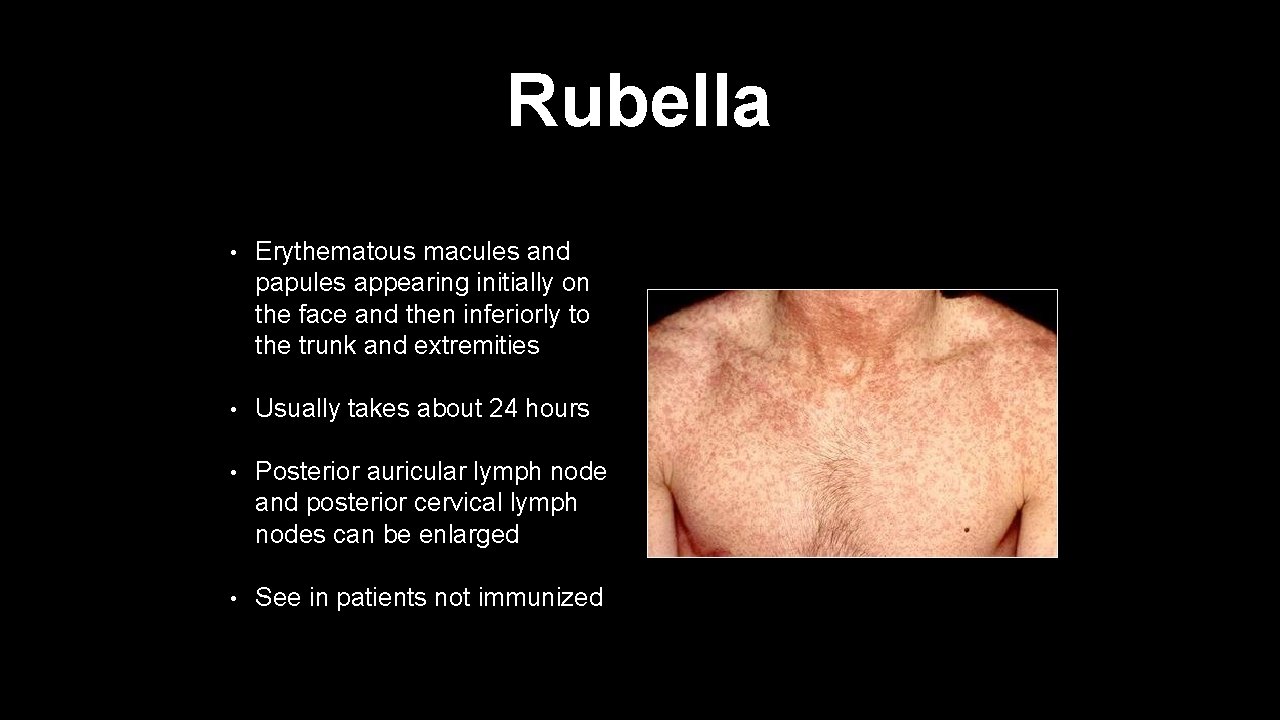
Rubella • Erythematous macules and papules appearing initially on the face and then inferiorly to the trunk and extremities • Usually takes about 24 hours • Posterior auricular lymph node and posterior cervical lymph nodes can be enlarged • See in patients not immunized
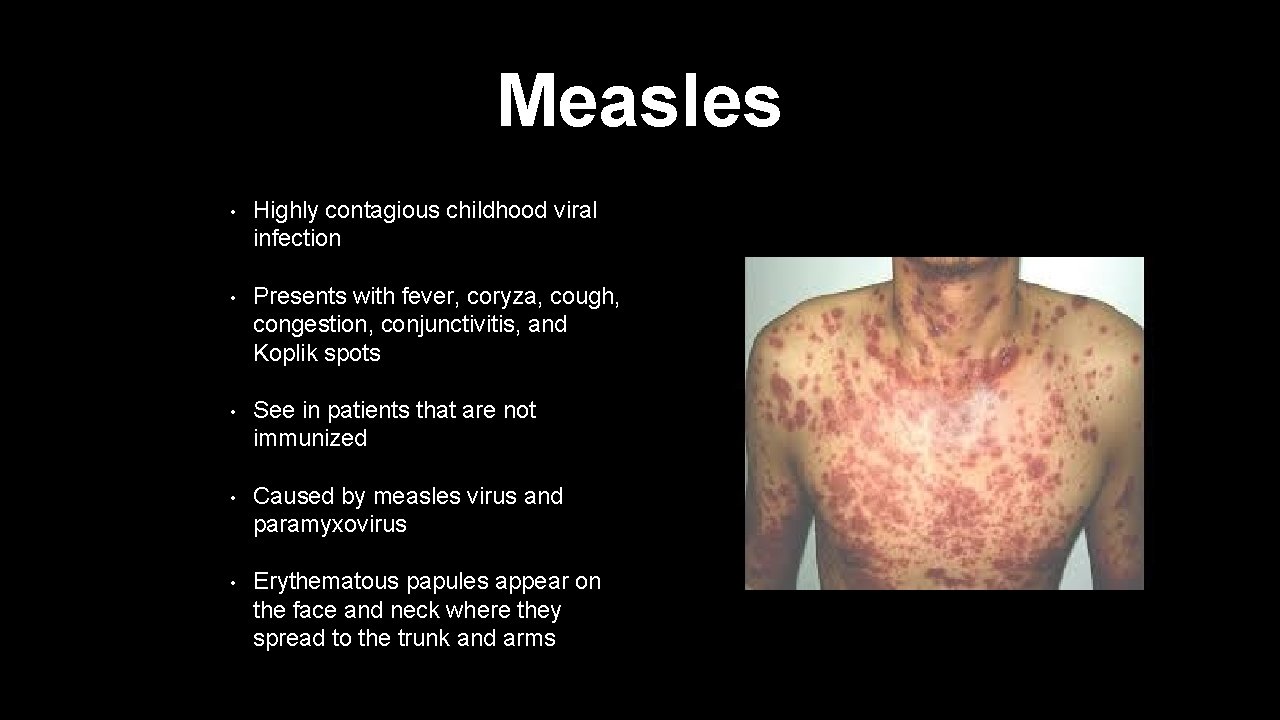
Measles • Highly contagious childhood viral infection • Presents with fever, coryza, cough, congestion, conjunctivitis, and Koplik spots • See in patients that are not immunized • Caused by measles virus and paramyxovirus • Erythematous papules appear on the face and neck where they spread to the trunk and arms
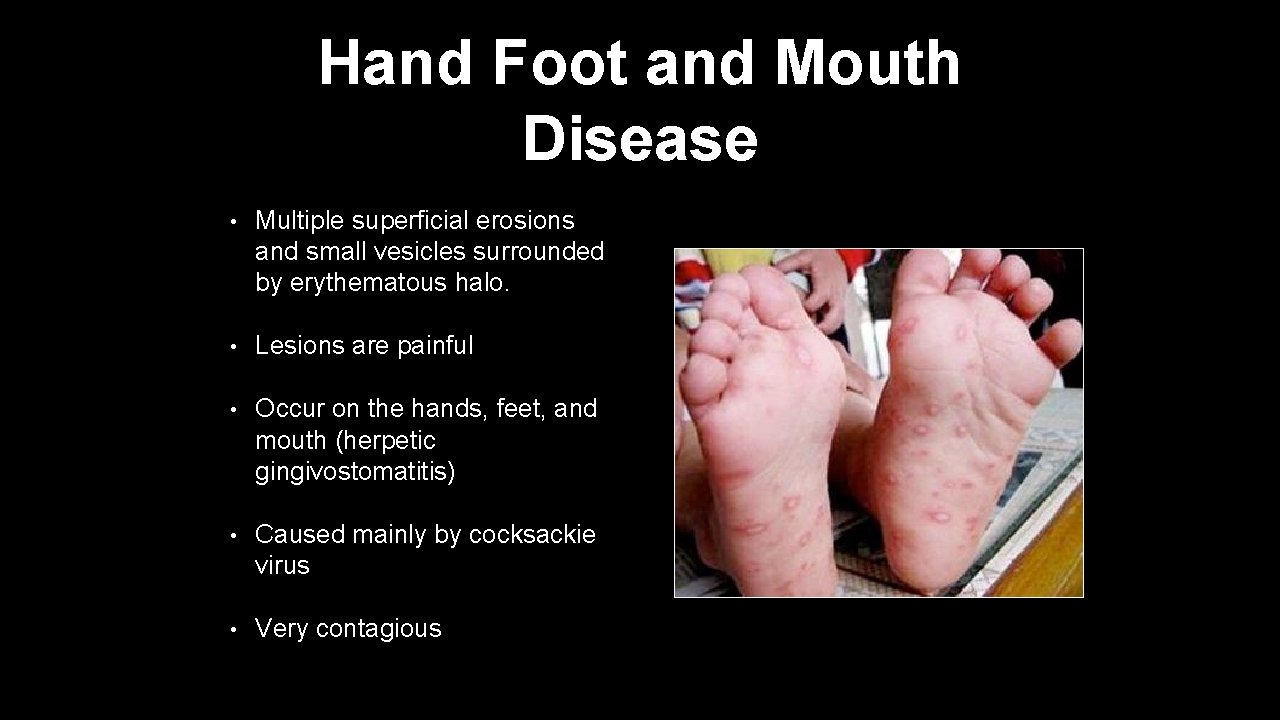
Hand Foot and Mouth Disease • Multiple superficial erosions and small vesicles surrounded by erythematous halo. • Lesions are painful • Occur on the hands, feet, and mouth (herpetic gingivostomatitis) • Caused mainly by cocksackie virus • Very contagious
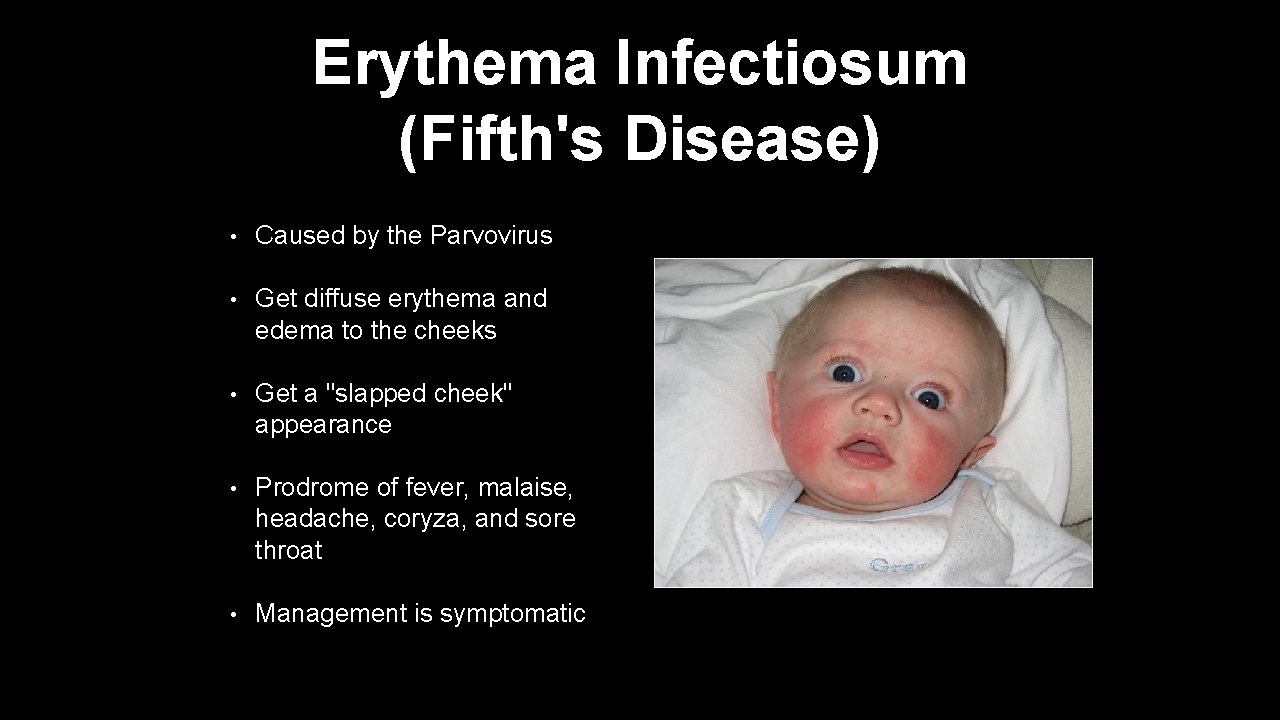
Erythema Infectiosum (Fifth's Disease) • Caused by the Parvovirus • Get diffuse erythema and edema to the cheeks • Get a "slapped cheek" appearance • Prodrome of fever, malaise, headache, coryza, and sore throat • Management is symptomatic
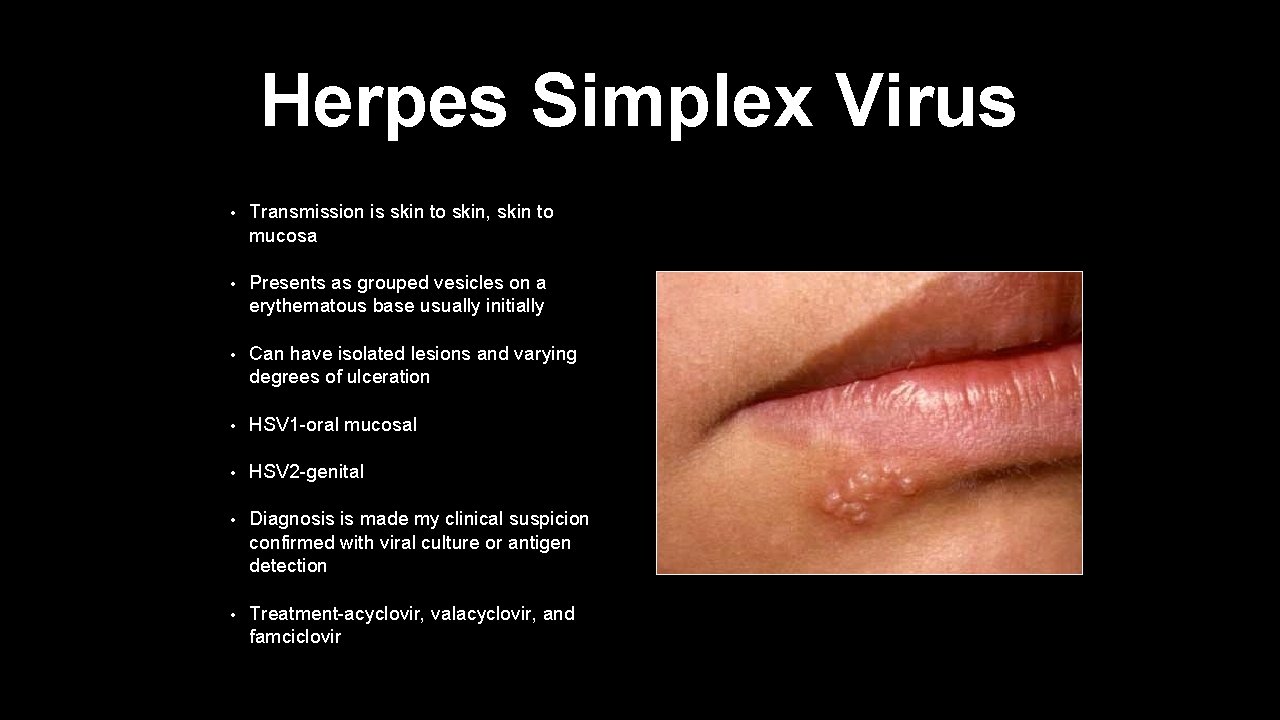
Herpes Simplex Virus • Transmission is skin to skin, skin to mucosa • Presents as grouped vesicles on a erythematous base usually initially • Can have isolated lesions and varying degrees of ulceration • HSV 1 -oral mucosal • HSV 2 -genital • Diagnosis is made my clinical suspicion confirmed with viral culture or antigen detection • Treatment-acyclovir, valacyclovir, and famciclovir
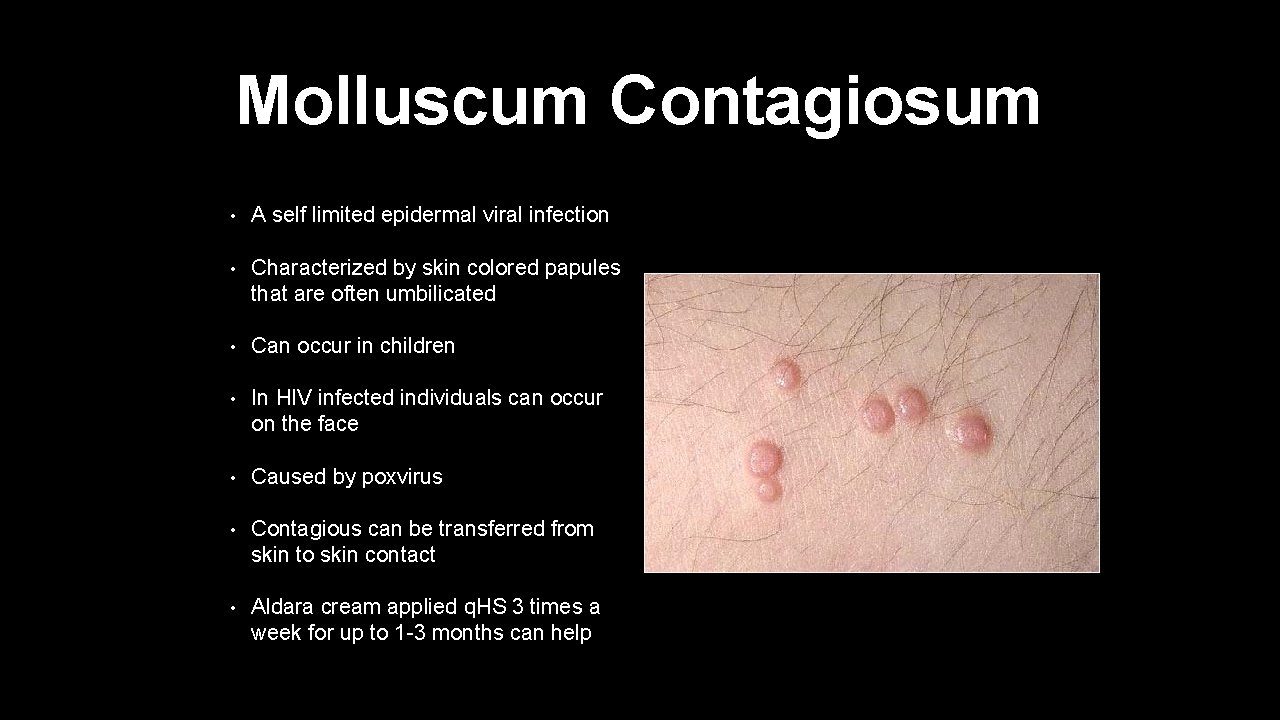
Molluscum Contagiosum • A self limited epidermal viral infection • Characterized by skin colored papules that are often umbilicated • Can occur in children • In HIV infected individuals can occur on the face • Caused by poxvirus • Contagious can be transferred from skin to skin contact • Aldara cream applied q. HS 3 times a week for up to 1 -3 months can help
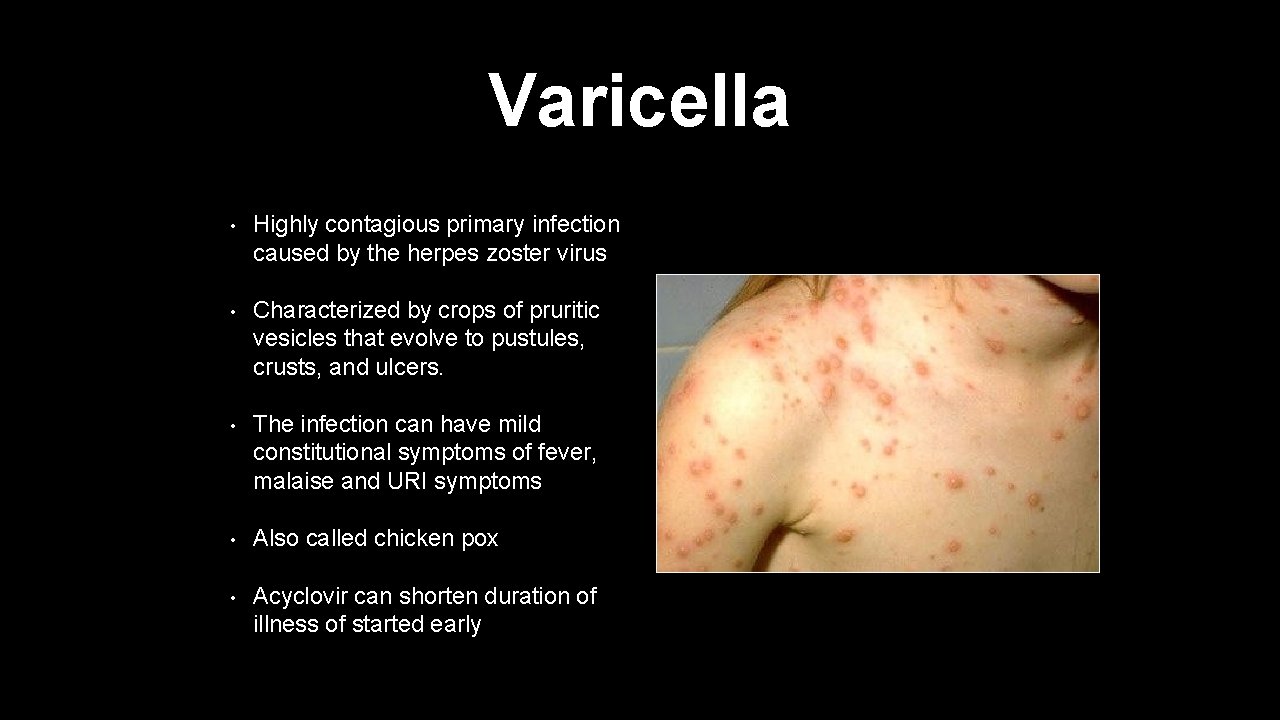
Varicella • Highly contagious primary infection caused by the herpes zoster virus • Characterized by crops of pruritic vesicles that evolve to pustules, crusts, and ulcers. • The infection can have mild constitutional symptoms of fever, malaise and URI symptoms • Also called chicken pox • Acyclovir can shorten duration of illness of started early
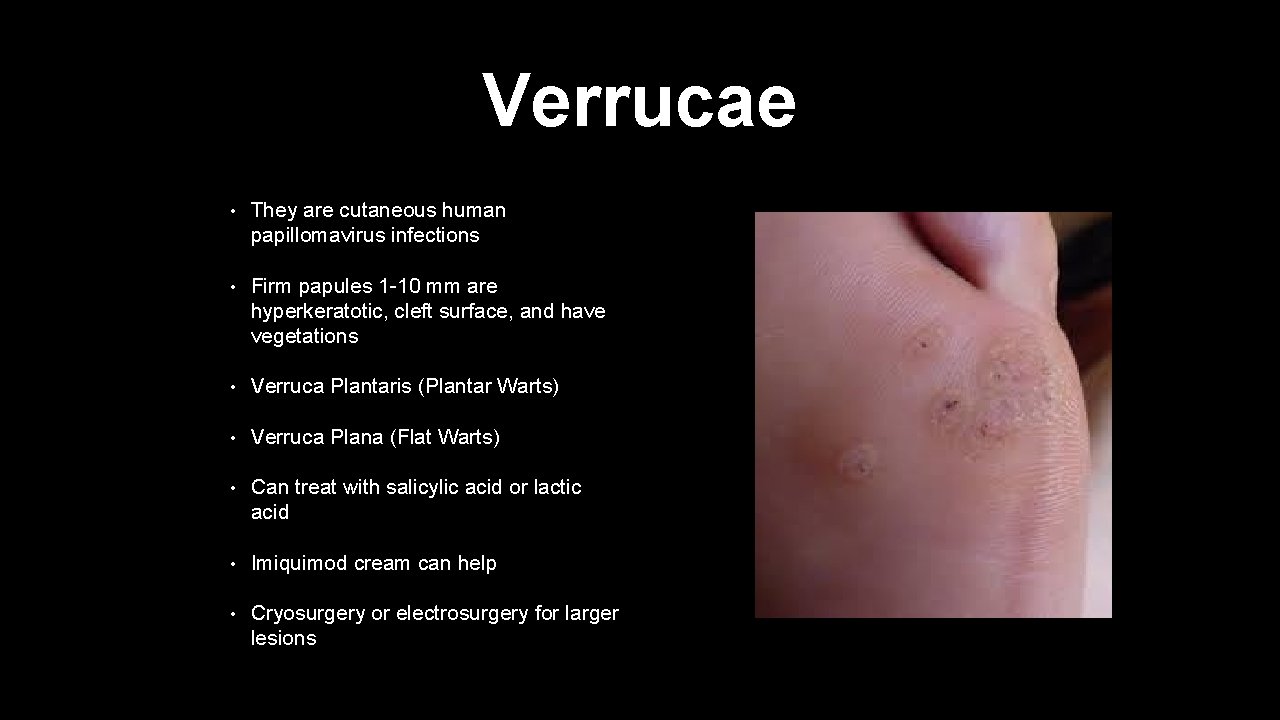
Verrucae • They are cutaneous human papillomavirus infections • Firm papules 1 -10 mm are hyperkeratotic, cleft surface, and have vegetations • Verruca Plantaris (Plantar Warts) • Verruca Plana (Flat Warts) • Can treat with salicylic acid or lactic acid • Imiquimod cream can help • Cryosurgery or electrosurgery for larger lesions
Bacterial Infections
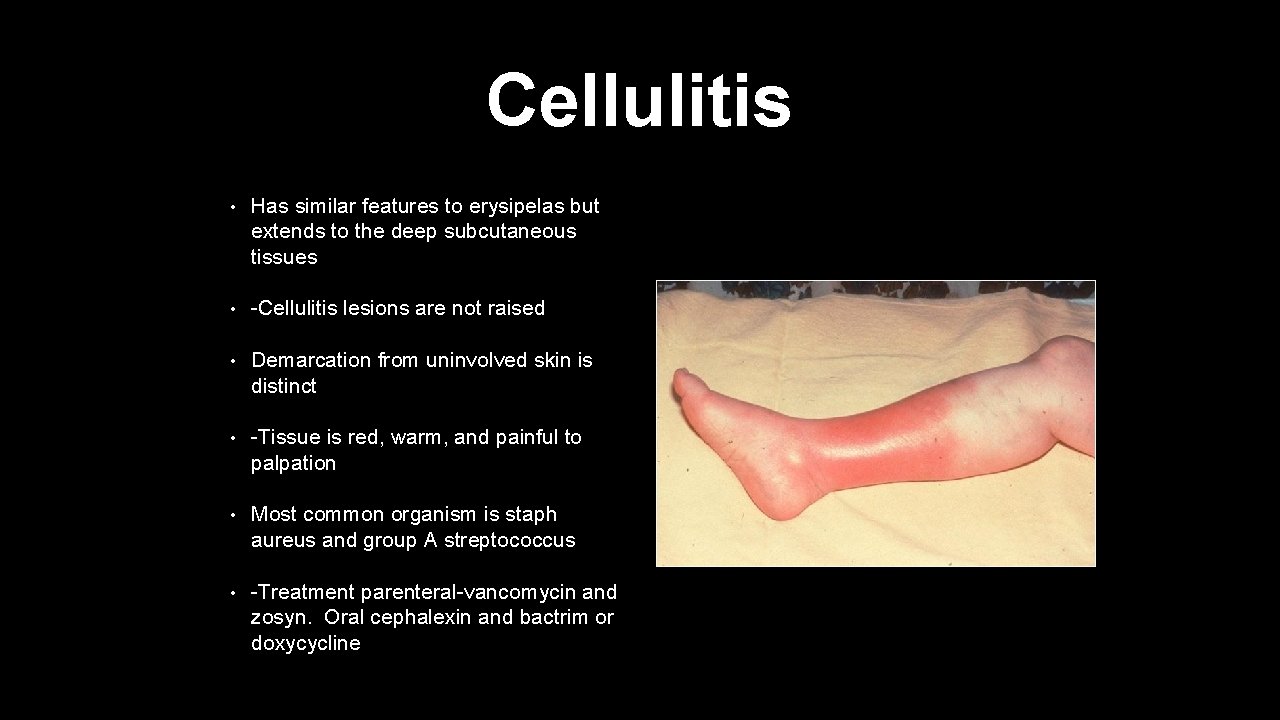
Cellulitis • Has similar features to erysipelas but extends to the deep subcutaneous tissues • -Cellulitis lesions are not raised • Demarcation from uninvolved skin is distinct • -Tissue is red, warm, and painful to palpation • Most common organism is staph aureus and group A streptococcus • -Treatment parenteral-vancomycin and zosyn. Oral cephalexin and bactrim or doxycycline
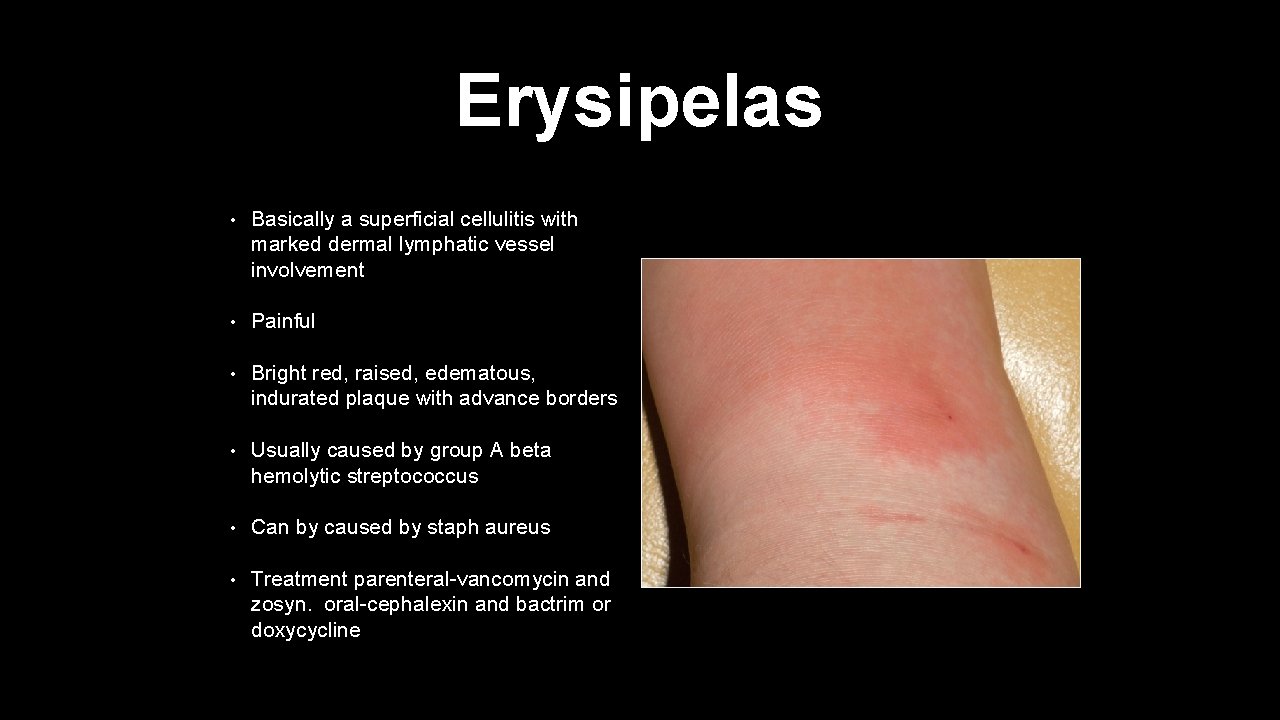
Erysipelas • Basically a superficial cellulitis with marked dermal lymphatic vessel involvement • Painful • Bright red, raised, edematous, indurated plaque with advance borders • Usually caused by group A beta hemolytic streptococcus • Can by caused by staph aureus • Treatment parenteral-vancomycin and zosyn. oral-cephalexin and bactrim or doxycycline
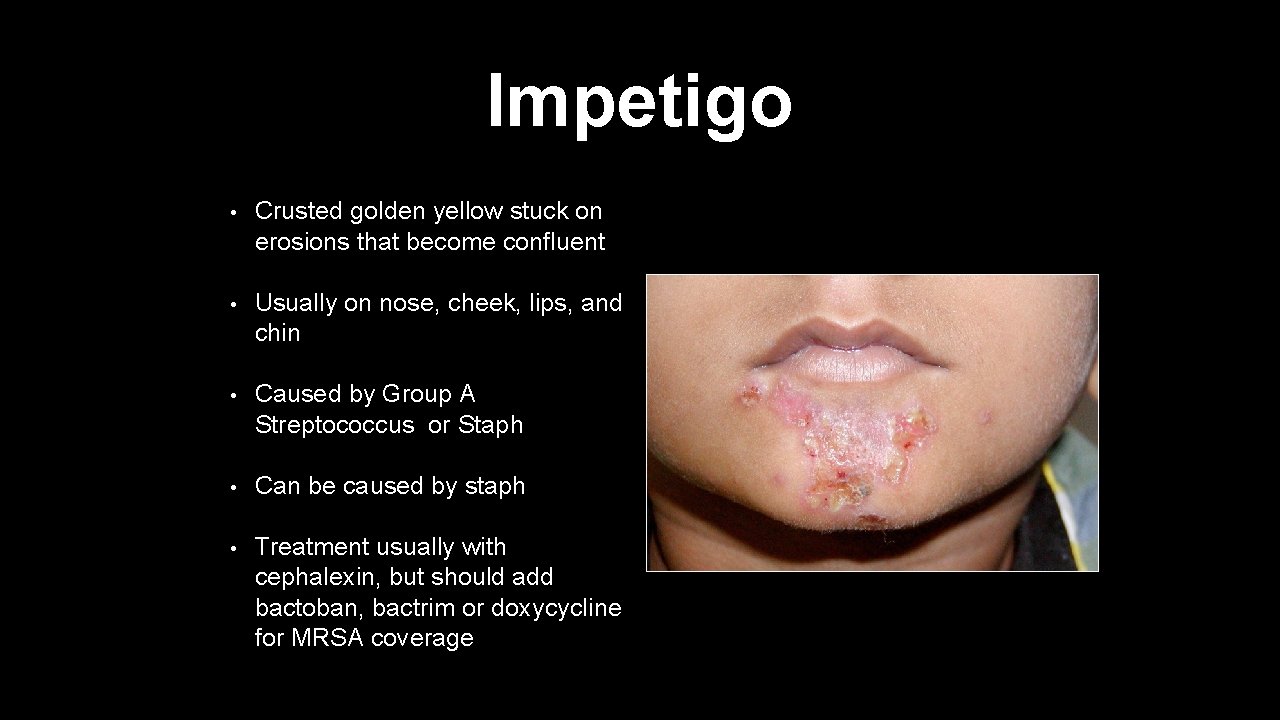
Impetigo • Crusted golden yellow stuck on erosions that become confluent • Usually on nose, cheek, lips, and chin • Caused by Group A Streptococcus or Staph • Can be caused by staph • Treatment usually with cephalexin, but should add bactoban, bactrim or doxycycline for MRSA coverage

Fungal Infections
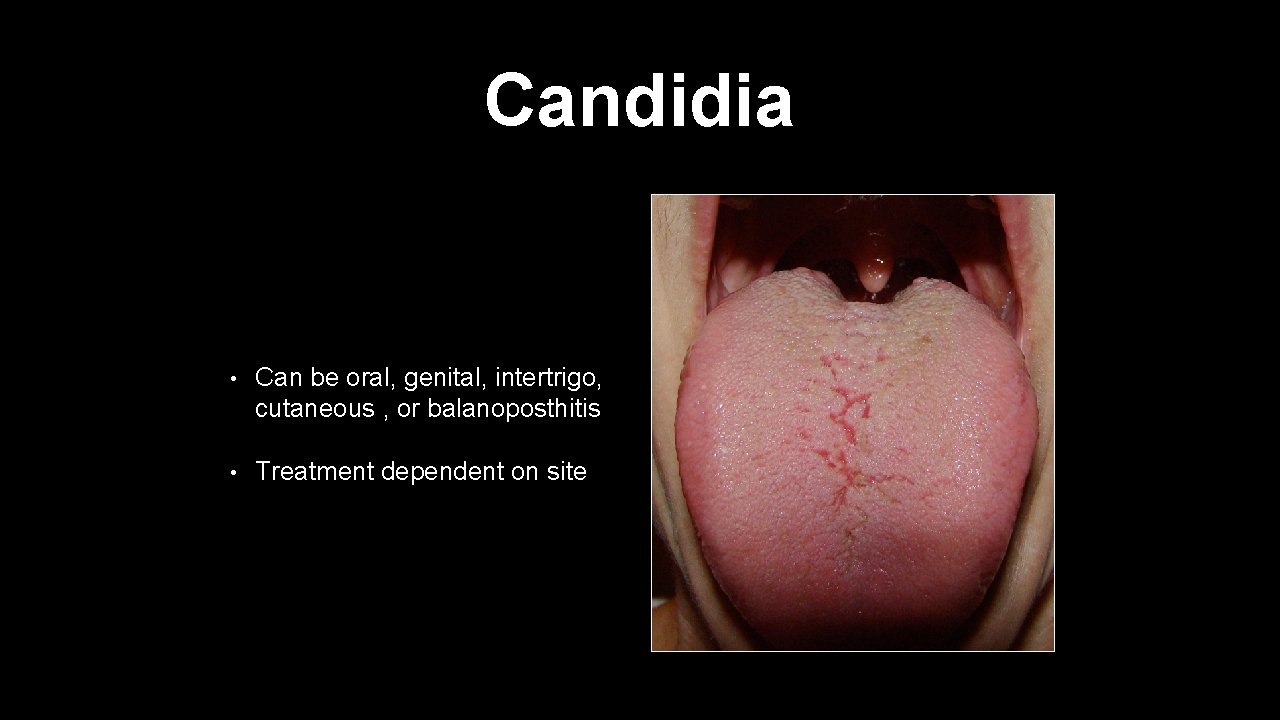
Candidia • Can be oral, genital, intertrigo, cutaneous , or balanoposthitis • Treatment dependent on site
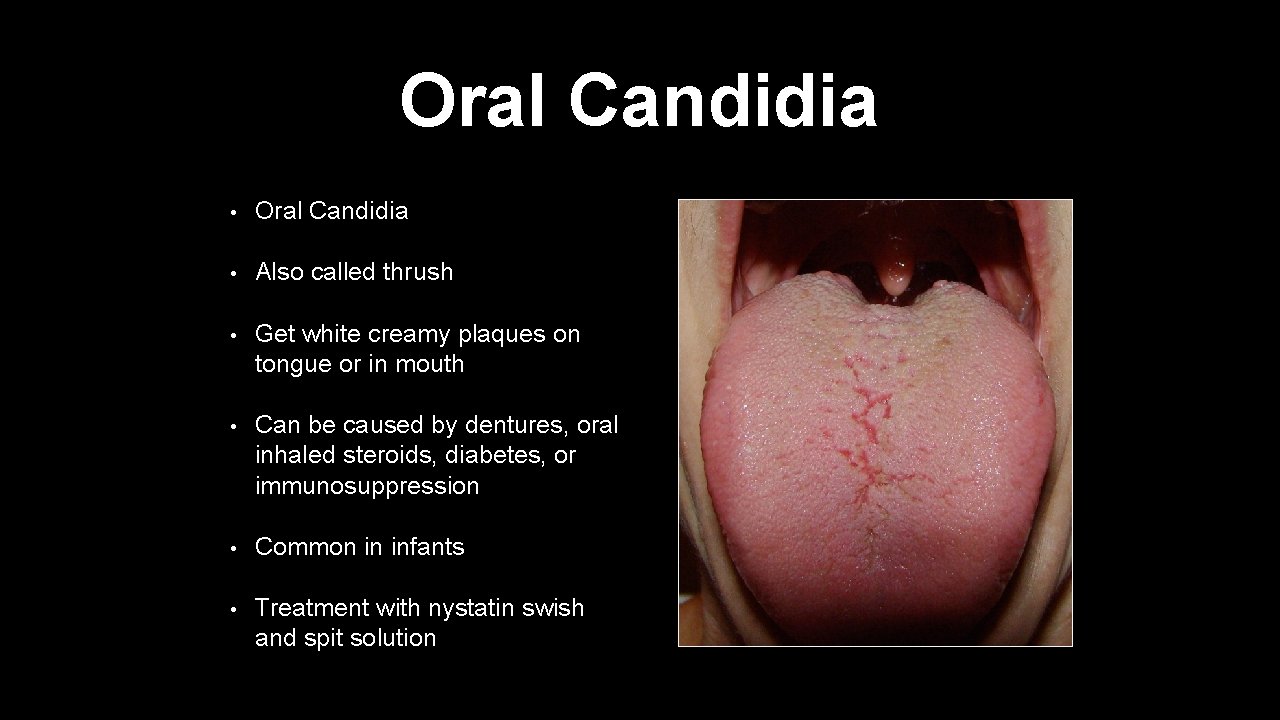
Oral Candidia • Oral Candidia • Also called thrush • Get white creamy plaques on tongue or in mouth • Can be caused by dentures, oral inhaled steroids, diabetes, or immunosuppression • Common in infants • Treatment with nystatin swish and spit solution
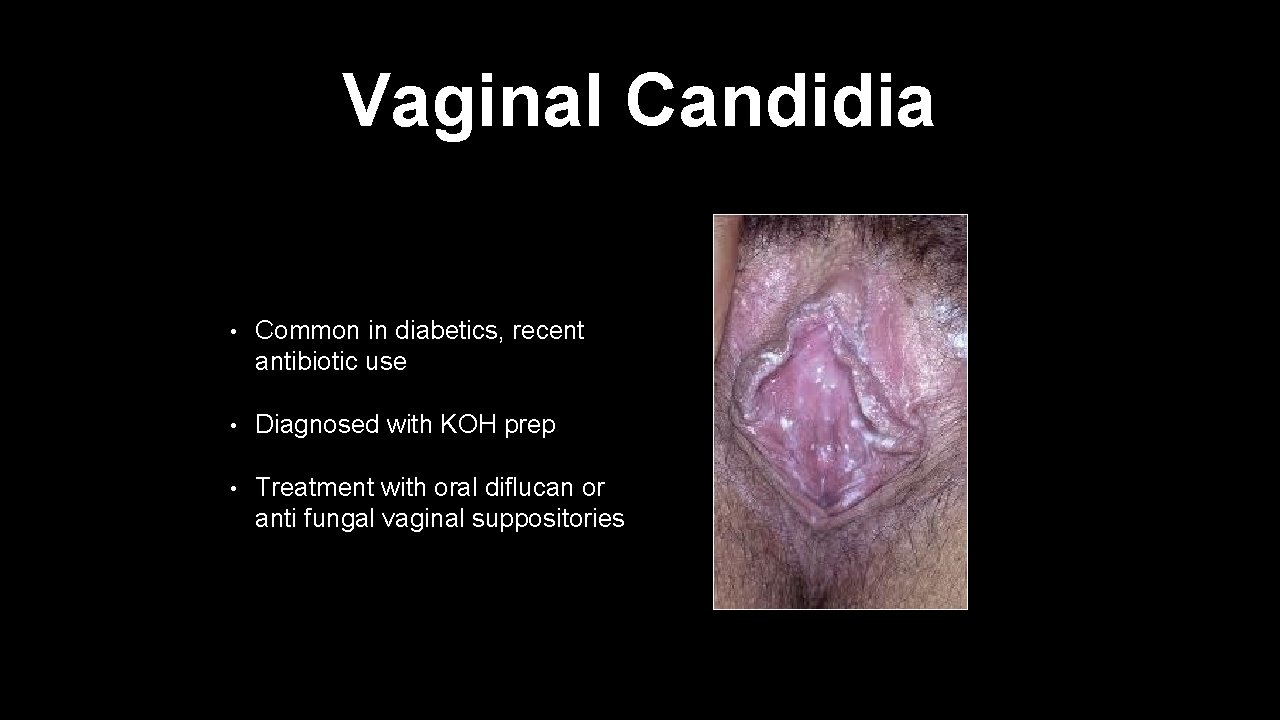
Vaginal Candidia • Common in diabetics, recent antibiotic use • Diagnosed with KOH prep • Treatment with oral diflucan or anti fungal vaginal suppositories
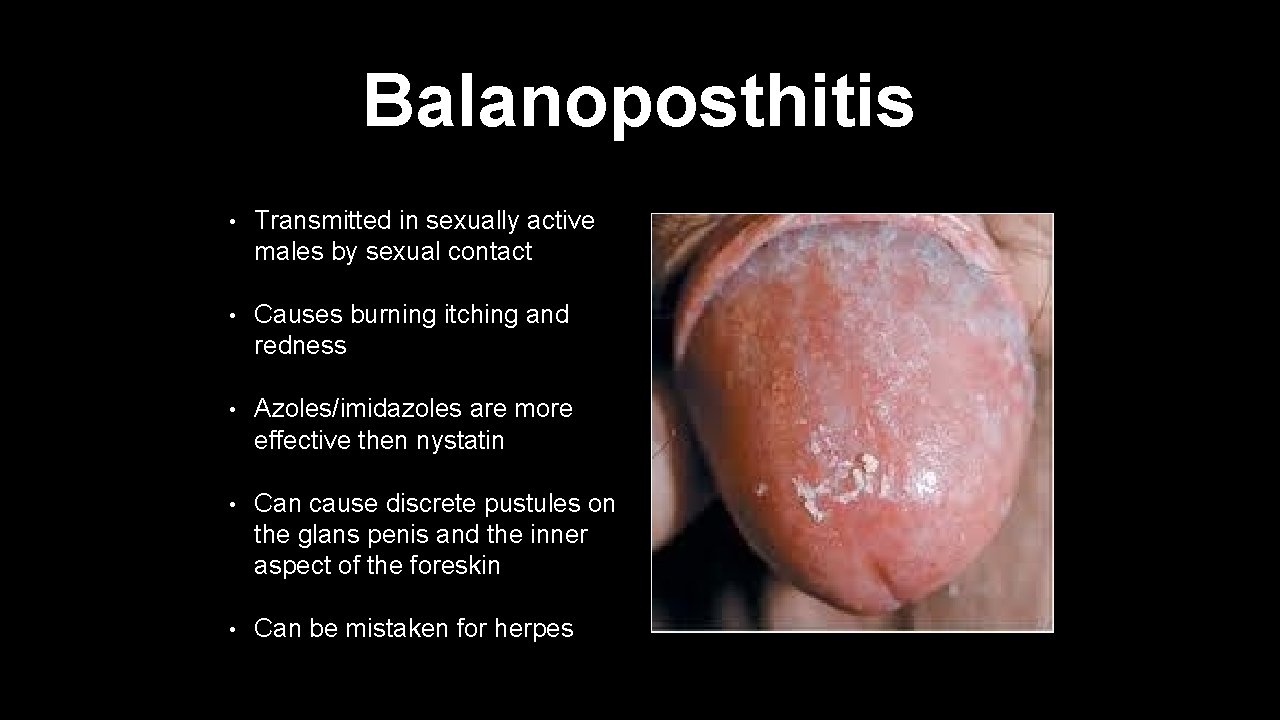
Balanoposthitis • Transmitted in sexually active males by sexual contact • Causes burning itching and redness • Azoles/imidazoles are more effective then nystatin • Can cause discrete pustules on the glans penis and the inner aspect of the foreskin • Can be mistaken for herpes
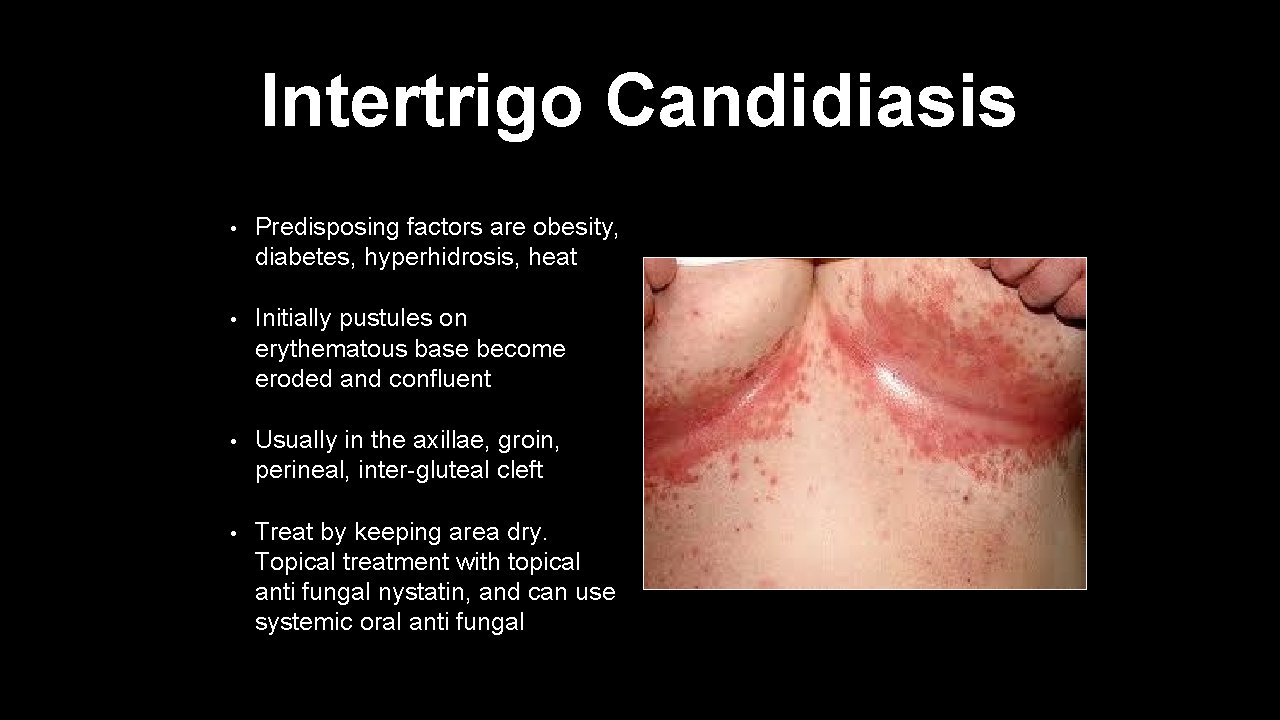
Intertrigo Candidiasis • Predisposing factors are obesity, diabetes, hyperhidrosis, heat • Initially pustules on erythematous base become eroded and confluent • Usually in the axillae, groin, perineal, inter-gluteal cleft • Treat by keeping area dry. Topical treatment with topical anti fungal nystatin, and can use systemic oral anti fungal
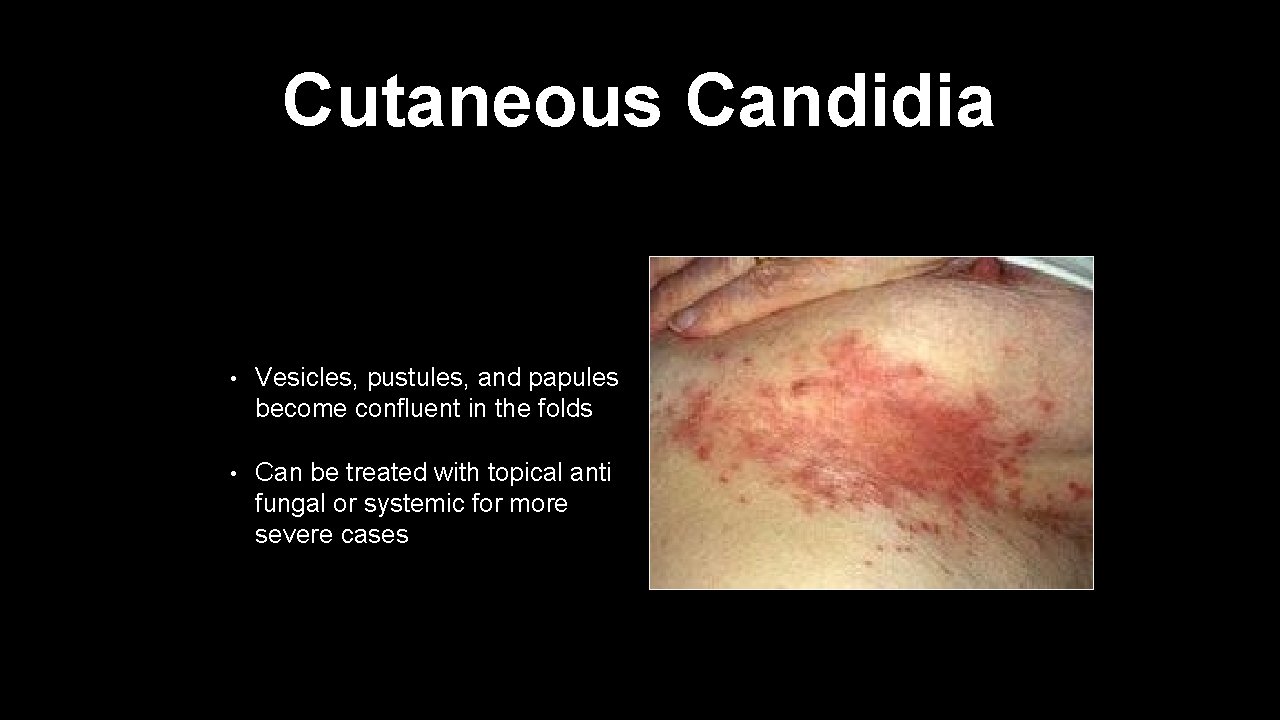
Cutaneous Candidia • Vesicles, pustules, and papules become confluent in the folds • Can be treated with topical anti fungal or systemic for more severe cases

Dermatophyte Infections • Dermatophyte infection of the feet • Causes redness, scaling, and maceration and or bullae formation • Often breaks up the integrity of the epidermis • Also known as athletes foot • Management use shoes while bathing. Topical anti fungal for mild to moderate infections. Oral anti fungal for more severe infection
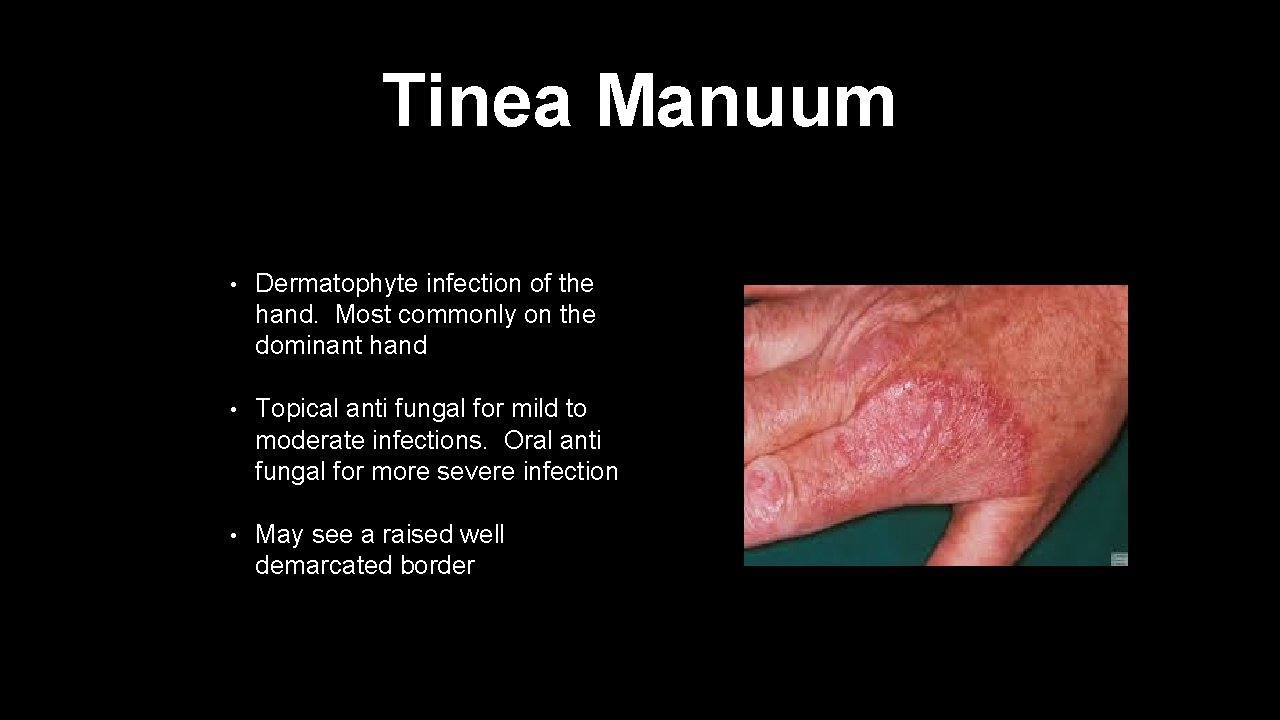
Tinea Manuum • Dermatophyte infection of the hand. Most commonly on the dominant hand • Topical anti fungal for mild to moderate infections. Oral anti fungal for more severe infection • May see a raised well demarcated border
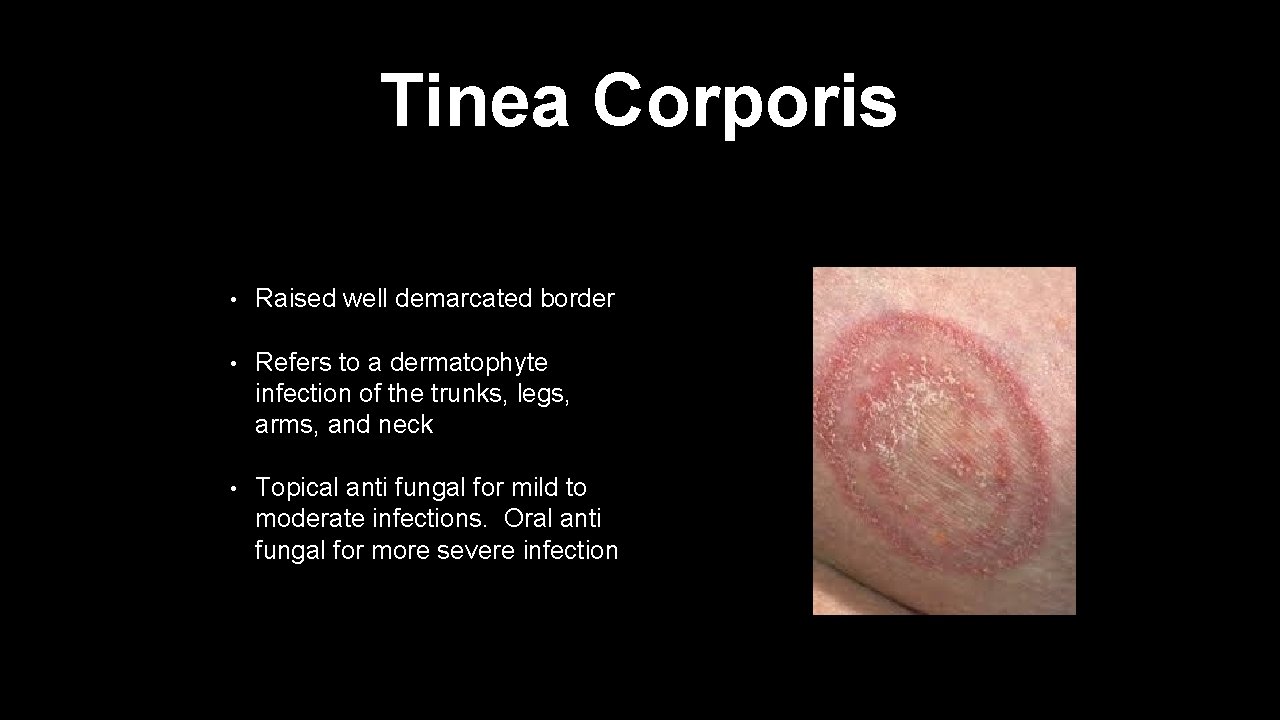
Tinea Corporis • Raised well demarcated border • Refers to a dermatophyte infection of the trunks, legs, arms, and neck • Topical anti fungal for mild to moderate infections. Oral anti fungal for more severe infection

Tinea Capitis • Dermatophyte infection involving the hair follicles • Get a large circular area of missing patch of hair • Topical antifungals are ineffective • Oral anti-fungal necessary for several weeks. Griseofulvin • Tinea Barbae is a tinea infection of the beard
Other Category
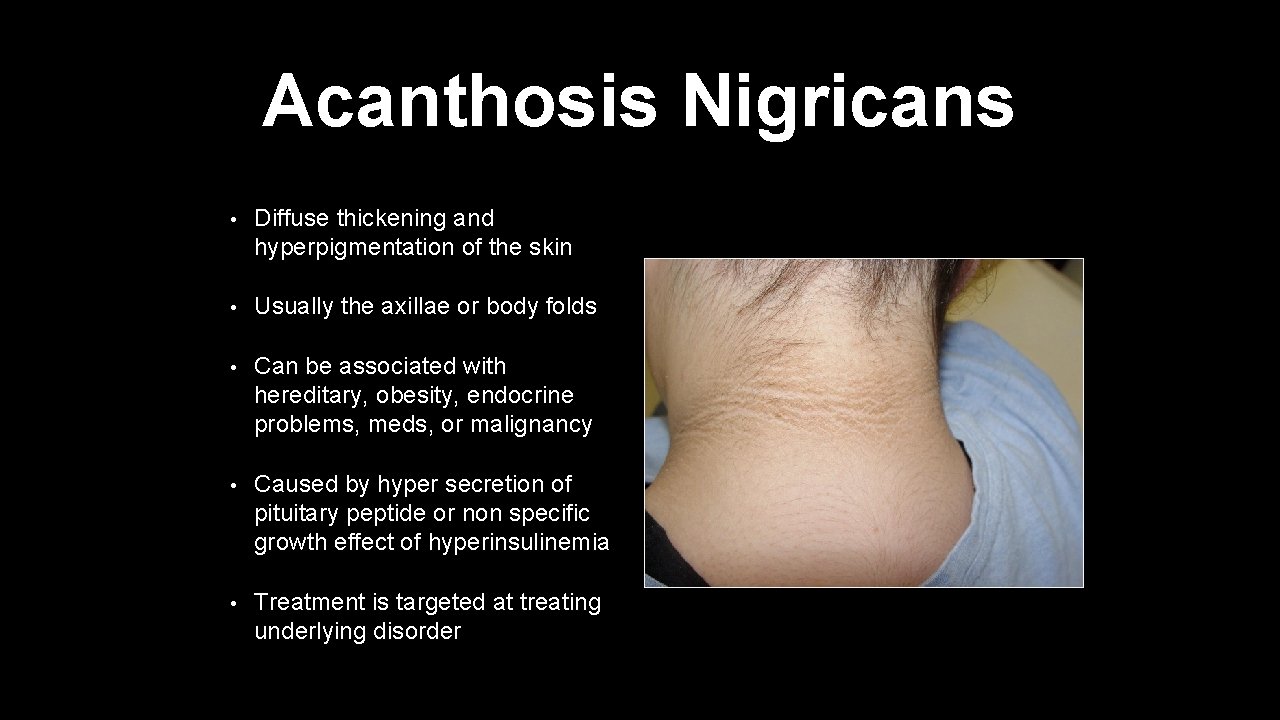
Acanthosis Nigricans • Diffuse thickening and hyperpigmentation of the skin • Usually the axillae or body folds • Can be associated with hereditary, obesity, endocrine problems, meds, or malignancy • Caused by hyper secretion of pituitary peptide or non specific growth effect of hyperinsulinemia • Treatment is targeted at treating underlying disorder
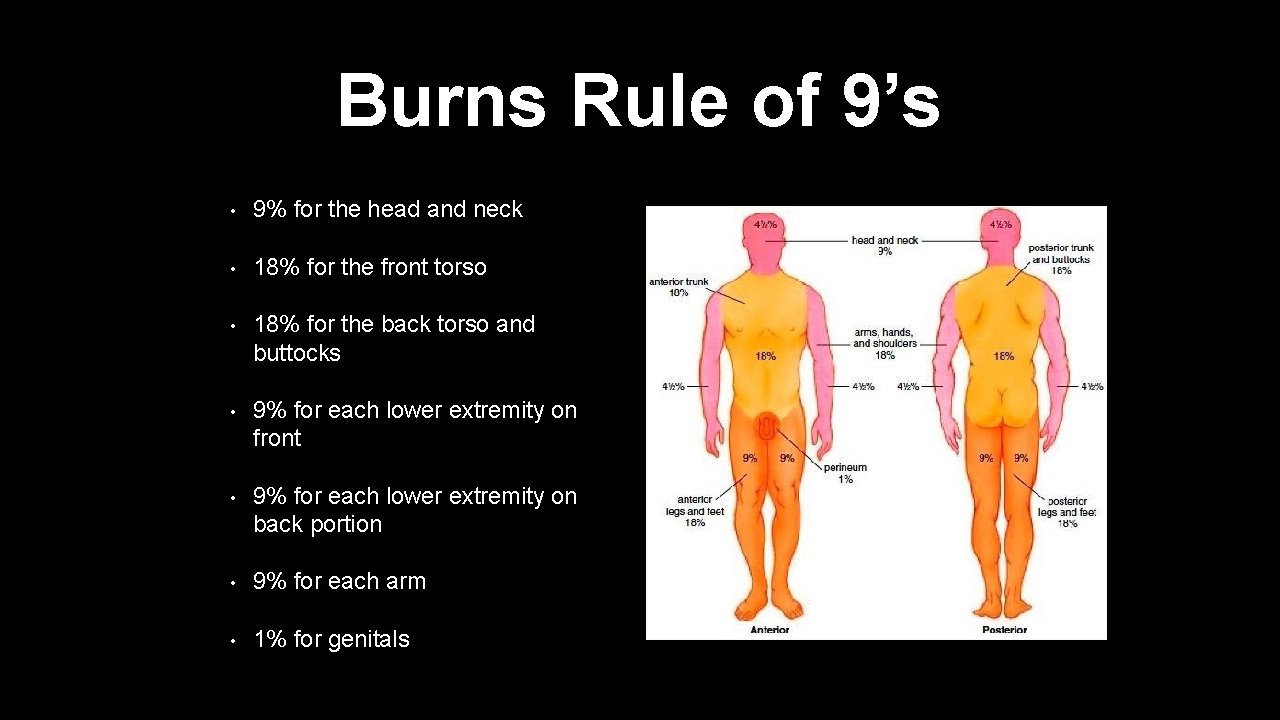
Burns Rule of 9’s • 9% for the head and neck • 18% for the front torso • 18% for the back torso and buttocks • 9% for each lower extremity on front • 9% for each lower extremity on back portion • 9% for each arm • 1% for genitals

Burns • Parkland Formula- to determine fluid needs for the first 24 hours in a burn victim • 4 x weight in kg x TBSA burn = fluid requirements for the first 24 hours. • Give first half over the first 8 hours and give the second half over the last 16 hours. Simple divide the total over the amount of hours necessary to give the fluids and that gives you the hourly rate.
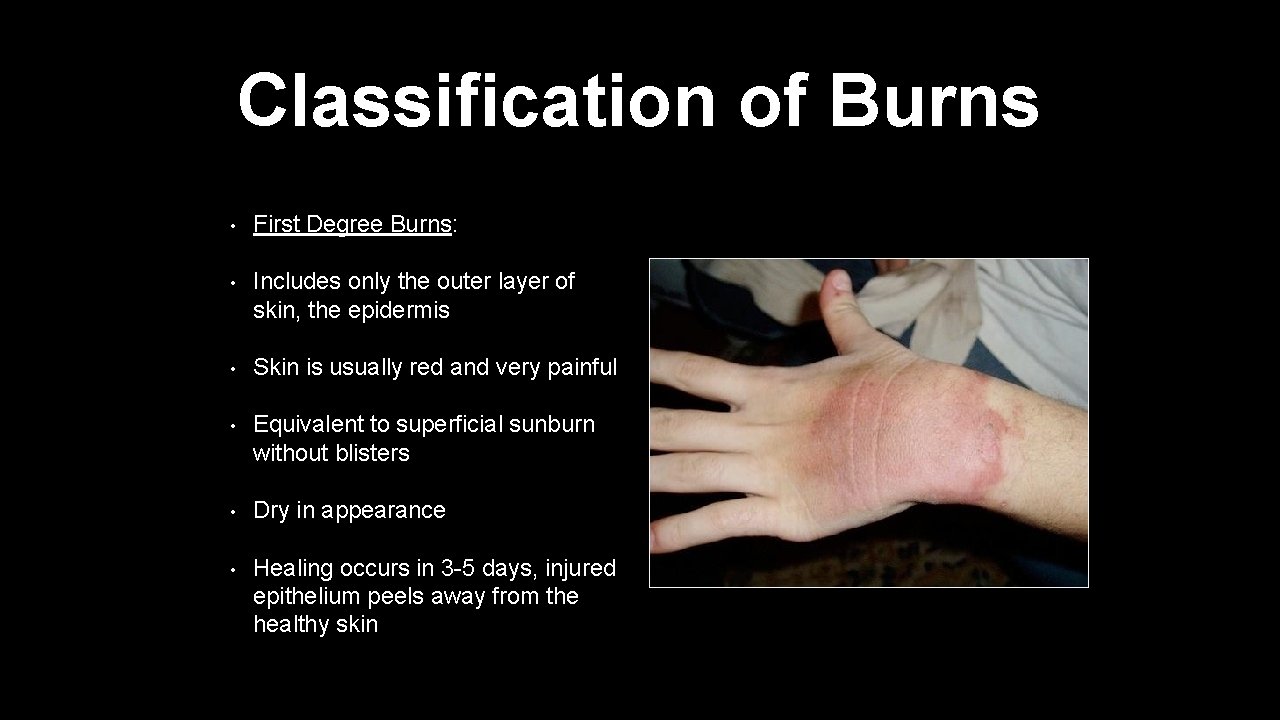
Classification of Burns • First Degree Burns: • Includes only the outer layer of skin, the epidermis • Skin is usually red and very painful • Equivalent to superficial sunburn without blisters • Dry in appearance • Healing occurs in 3 -5 days, injured epithelium peels away from the healthy skin
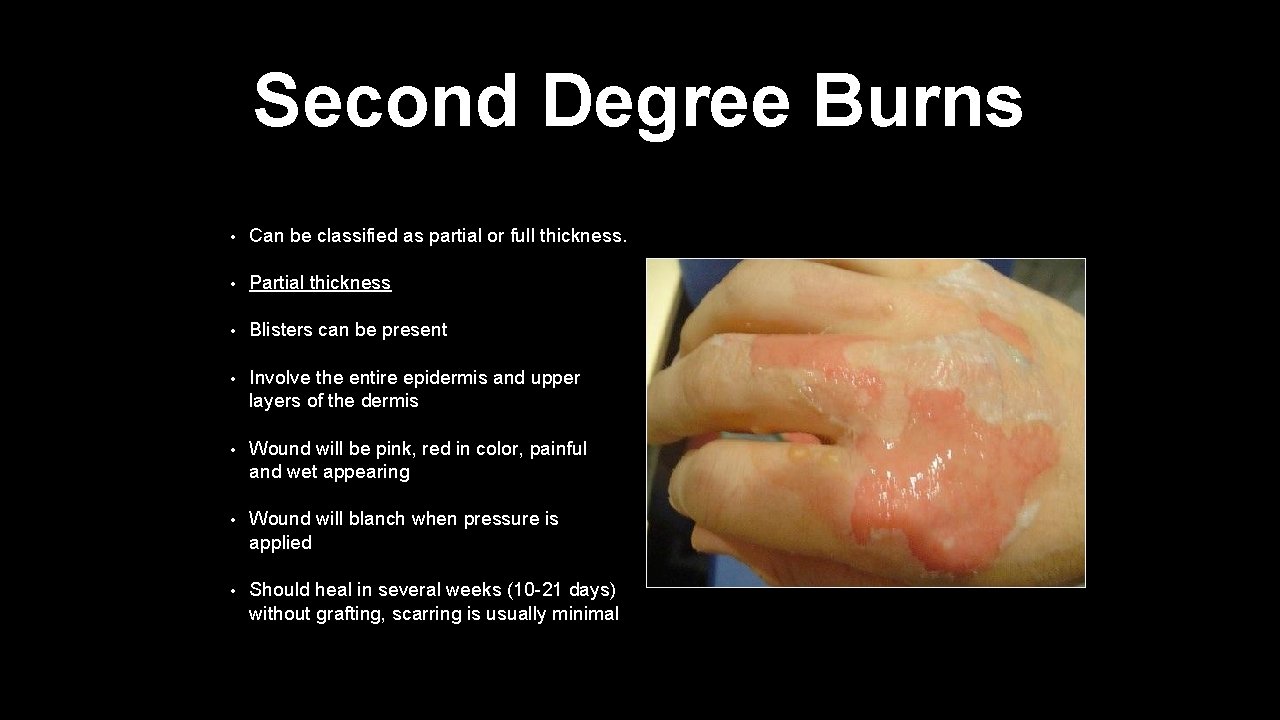
Second Degree Burns • Can be classified as partial or full thickness. • Partial thickness • Blisters can be present • Involve the entire epidermis and upper layers of the dermis • Wound will be pink, red in color, painful and wet appearing • Wound will blanch when pressure is applied • Should heal in several weeks (10 -21 days) without grafting, scarring is usually minimal
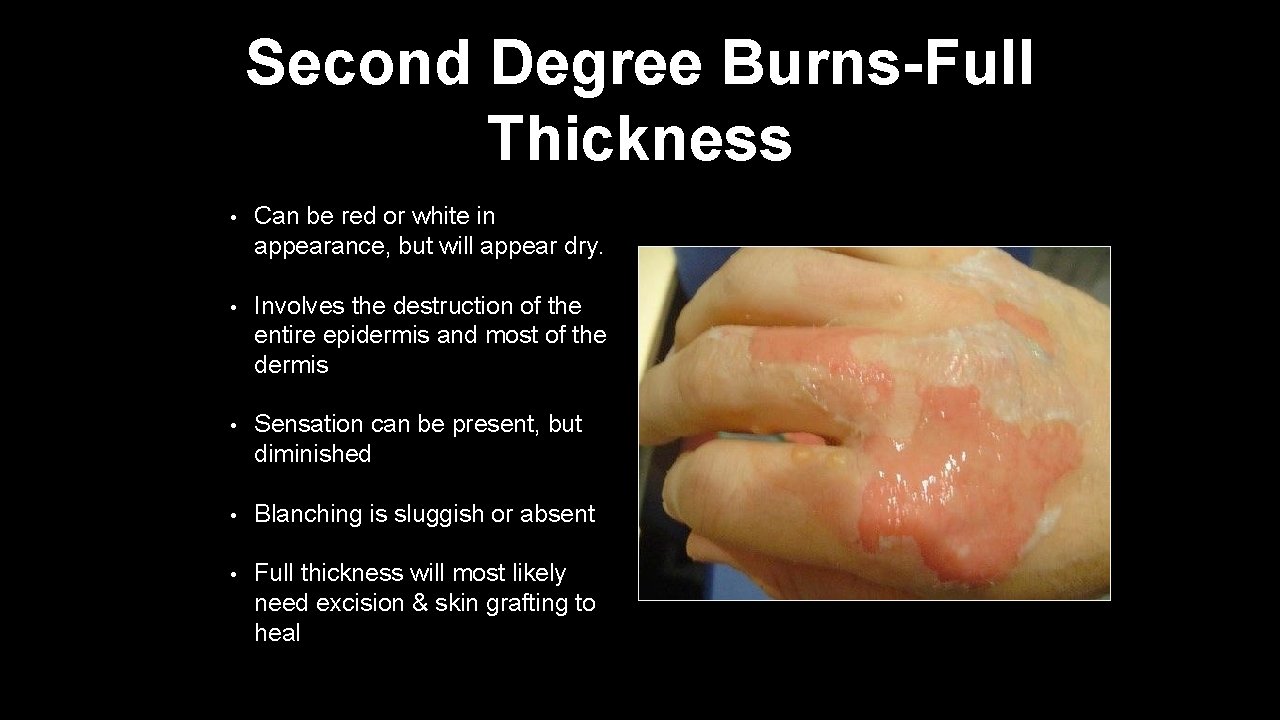
Second Degree Burns-Full Thickness • Can be red or white in appearance, but will appear dry. • Involves the destruction of the entire epidermis and most of the dermis • Sensation can be present, but diminished • Blanching is sluggish or absent • Full thickness will most likely need excision & skin grafting to heal
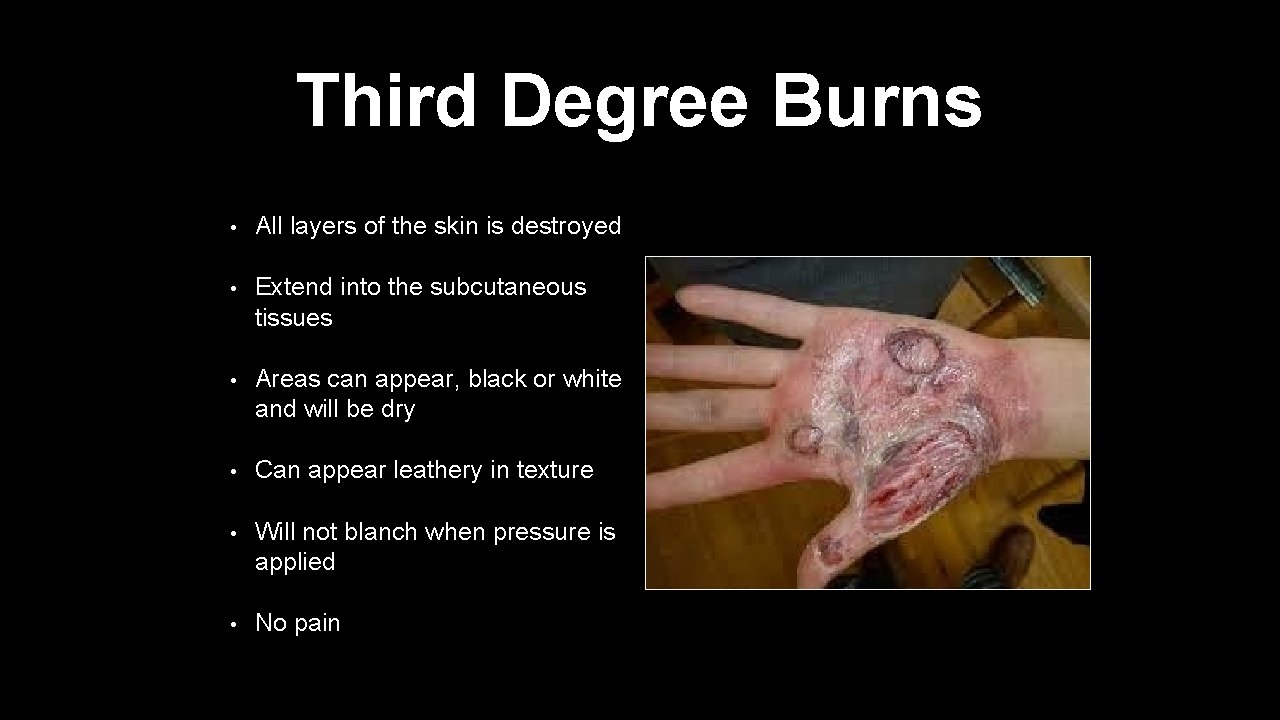
Third Degree Burns • All layers of the skin is destroyed • Extend into the subcutaneous tissues • Areas can appear, black or white and will be dry • Can appear leathery in texture • Will not blanch when pressure is applied • No pain
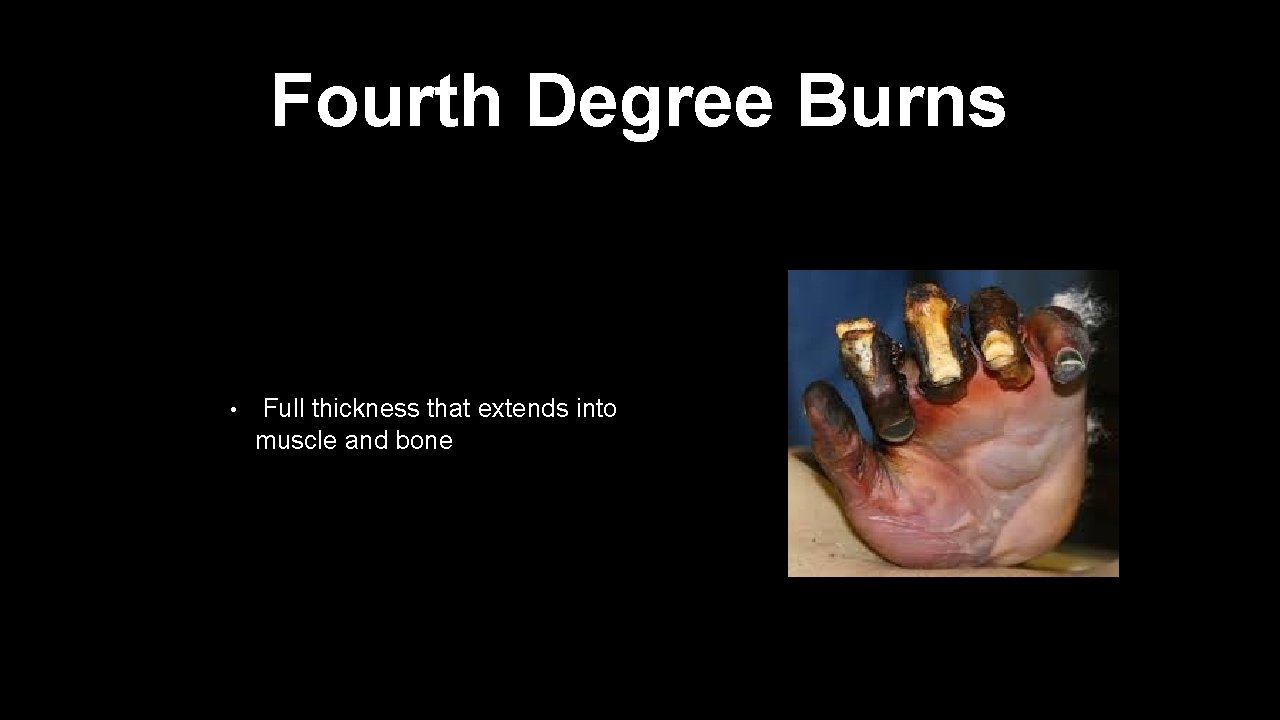
Fourth Degree Burns • Full thickness that extends into muscle and bone
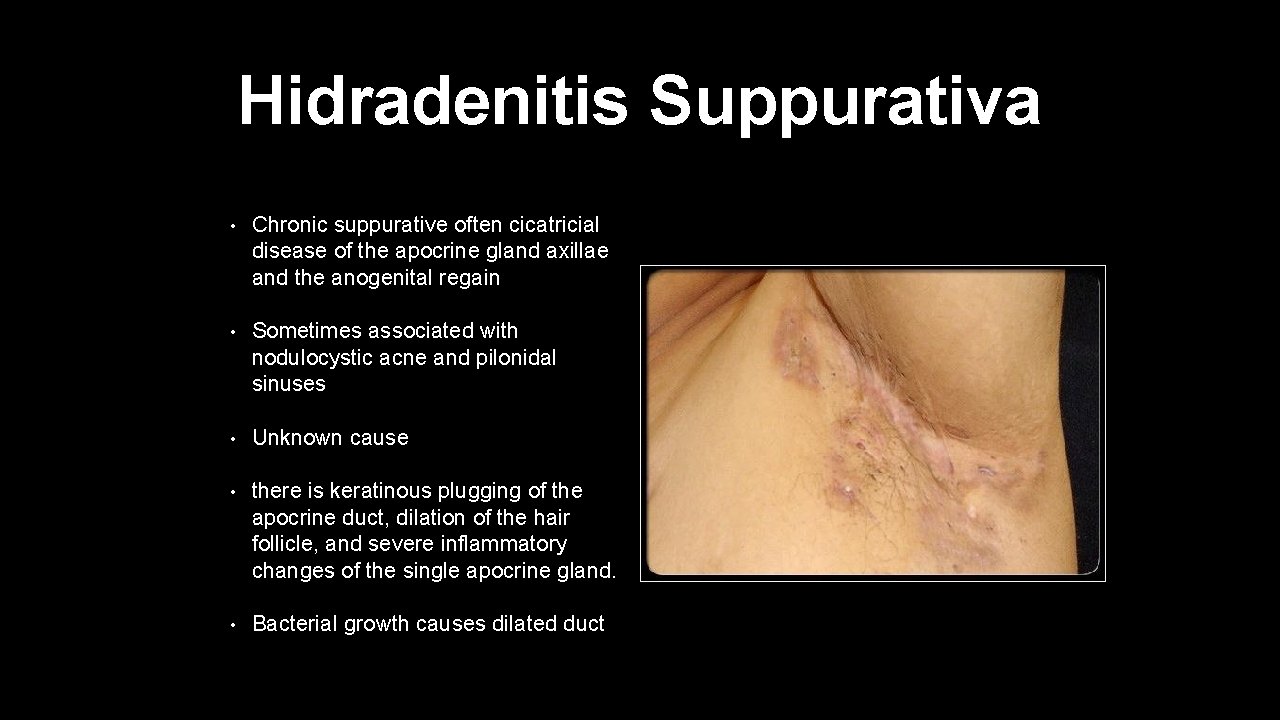
Hidradenitis Suppurativa • Chronic suppurative often cicatricial disease of the apocrine gland axillae and the anogenital regain • Sometimes associated with nodulocystic acne and pilonidal sinuses • Unknown cause • there is keratinous plugging of the apocrine duct, dilation of the hair follicle, and severe inflammatory changes of the single apocrine gland. • Bacterial growth causes dilated duct

Hidradenitis Suppurativa • Ruptured duct or gland causes extension of inflammation or infection which cause tissue destruction and then this leads to ulceration, fibrosis and sinus tract formation • Treatment is incision and drainage and to excise recurrent fibrotic nodules and tracts
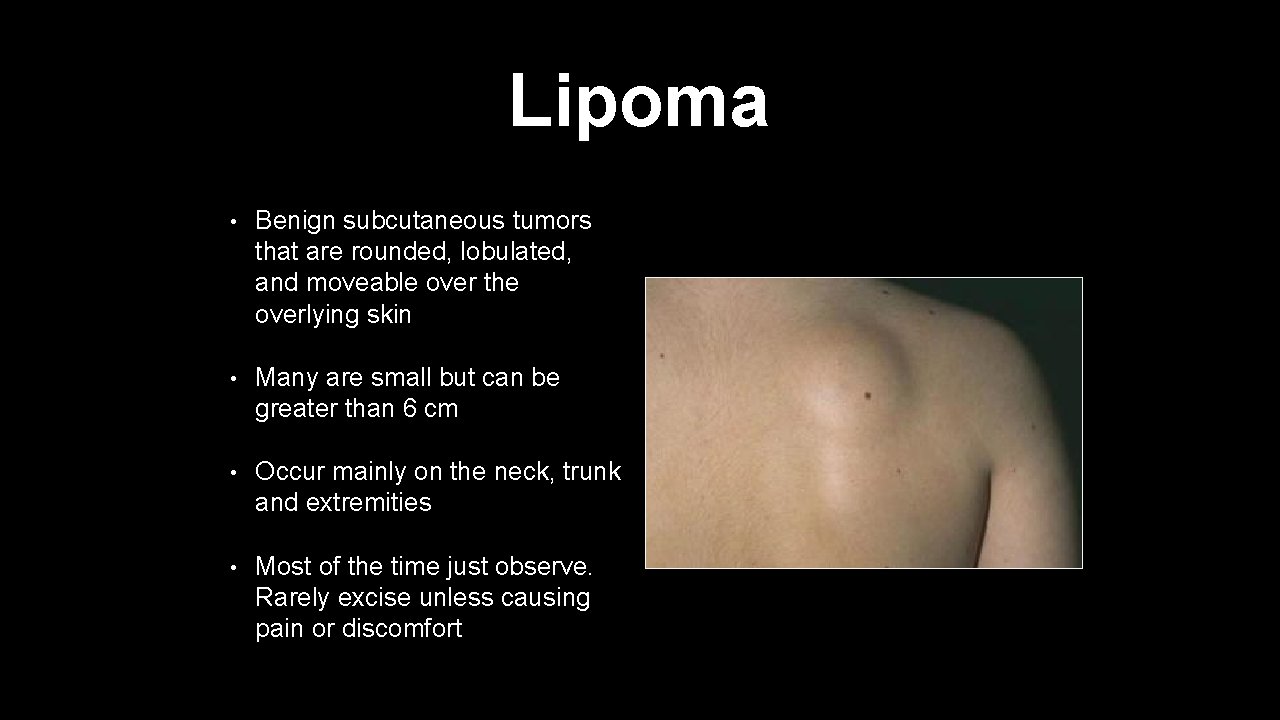
Lipoma • Benign subcutaneous tumors that are rounded, lobulated, and moveable over the overlying skin • Many are small but can be greater than 6 cm • Occur mainly on the neck, trunk and extremities • Most of the time just observe. Rarely excise unless causing pain or discomfort
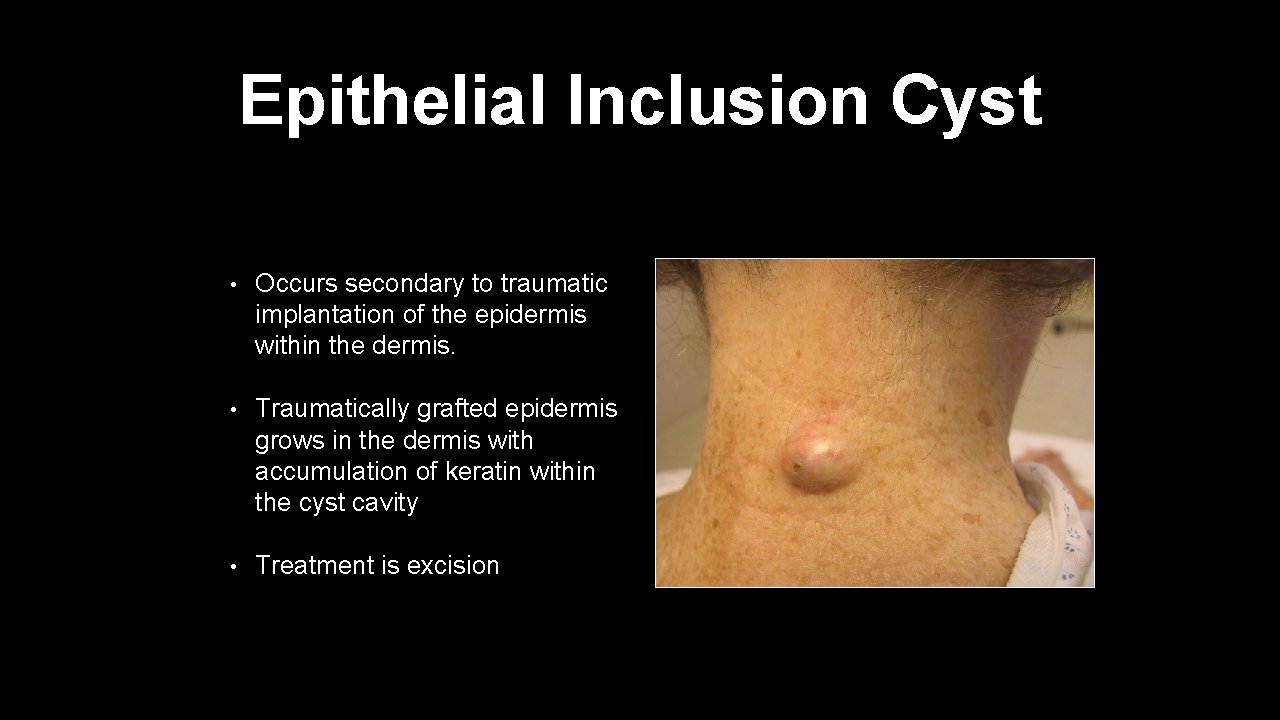
Epithelial Inclusion Cyst • Occurs secondary to traumatic implantation of the epidermis within the dermis. • Traumatically grafted epidermis grows in the dermis with accumulation of keratin within the cyst cavity • Treatment is excision
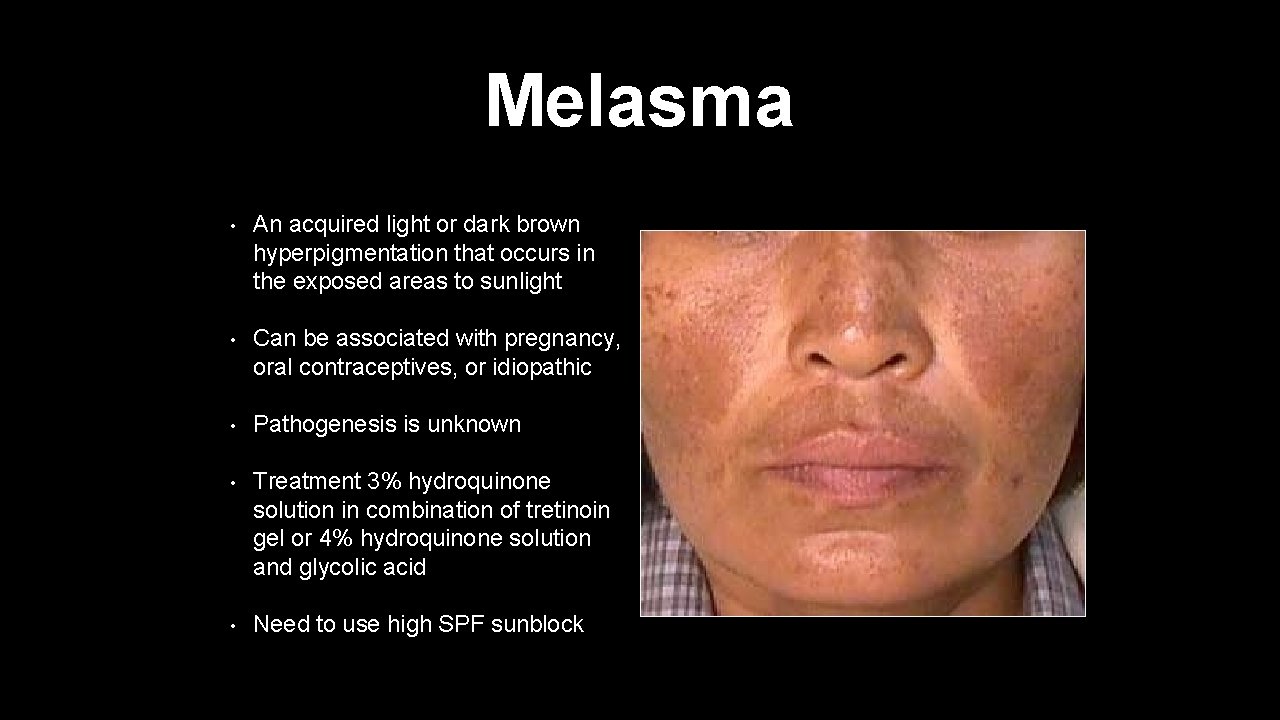
Melasma • An acquired light or dark brown hyperpigmentation that occurs in the exposed areas to sunlight • Can be associated with pregnancy, oral contraceptives, or idiopathic • Pathogenesis is unknown • Treatment 3% hydroquinone solution in combination of tretinoin gel or 4% hydroquinone solution and glycolic acid • Need to use high SPF sunblock
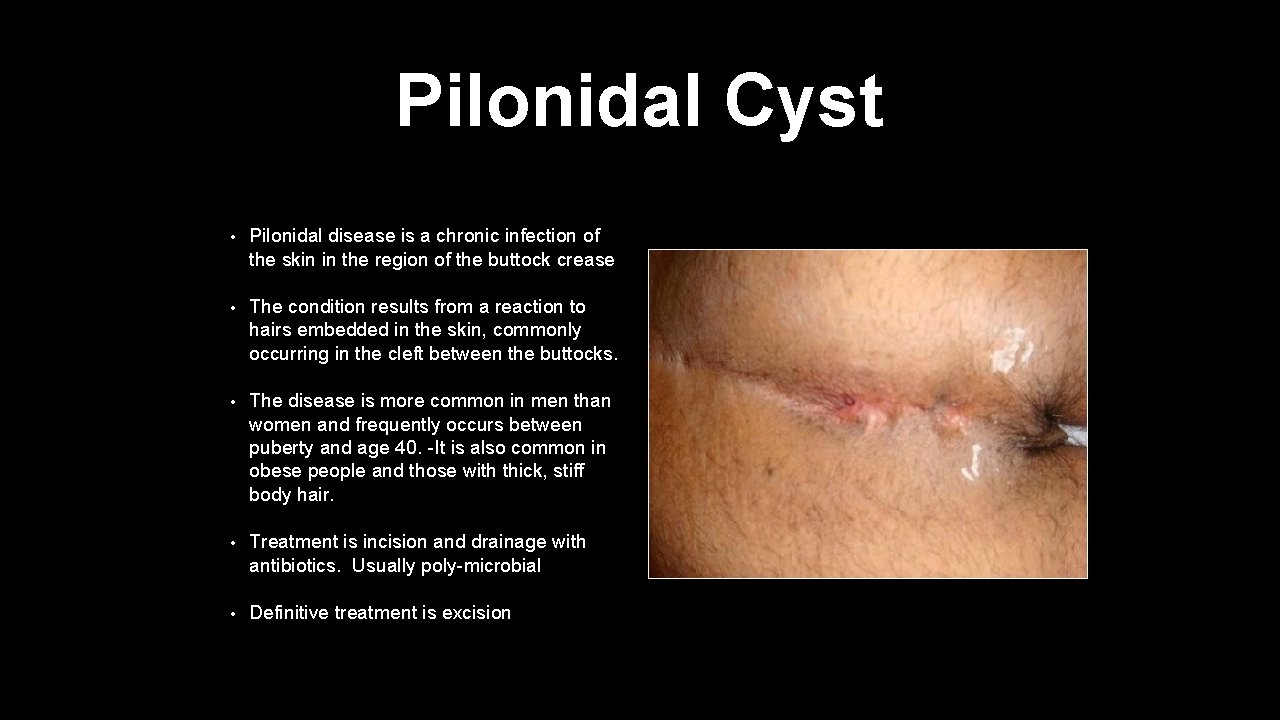
Pilonidal Cyst • Pilonidal disease is a chronic infection of the skin in the region of the buttock crease • The condition results from a reaction to hairs embedded in the skin, commonly occurring in the cleft between the buttocks. • The disease is more common in men than women and frequently occurs between puberty and age 40. -It is also common in obese people and those with thick, stiff body hair. • Treatment is incision and drainage with antibiotics. Usually poly-microbial • Definitive treatment is excision
Pressure Ulcers • Develop over body support surfaces over bony prominences as a result of the external compression of the skin, shear forces, or friction which produce ischemic changes or necrosis • Treatment is prevention. Reposition patient every 2 hours. Pad ulcer prone areas and massage them • Clean areas and keep free of urine and feces • Mobilize patient if possible
Pressure Ulcers Stage I • Stage I: Non blanchable erythema • Intact skin with non blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area. The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Category I may be difficult to detect in individuals with dark skin tones.
Pressure Ulcer Stage II Partial Thickness • Stage II: Partial thickness • Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled or serosanginous filled blister. Presents as a shiny or dry shallow ulcer without slough or bruising. This category should not be used to describe skin tears, tape burns, incontinence associated dermatitis, maceration or excoriation.
Pressure Ulcer Stage III Full Thickness • Stage III: Full thickness skin loss • Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling. The depth of a Stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and Stage III ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep Stage III pressure ulcers. Bone/tendon is not visible or directly palpable.
Pressure Ulcer Stage IV Full Thickness • Stage IV: Full thickness tissue loss • Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. Often includes undermining and tunneling. The depth of a Stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and these ulcers can be shallow. Stage IV ulcers can extend into muscle and/or supporting structures (e. g. , fascia, tendon or joint capsule) making osteomyelitis or osteitis likely to occur. Exposed bone/muscle is visible or directly palpable.
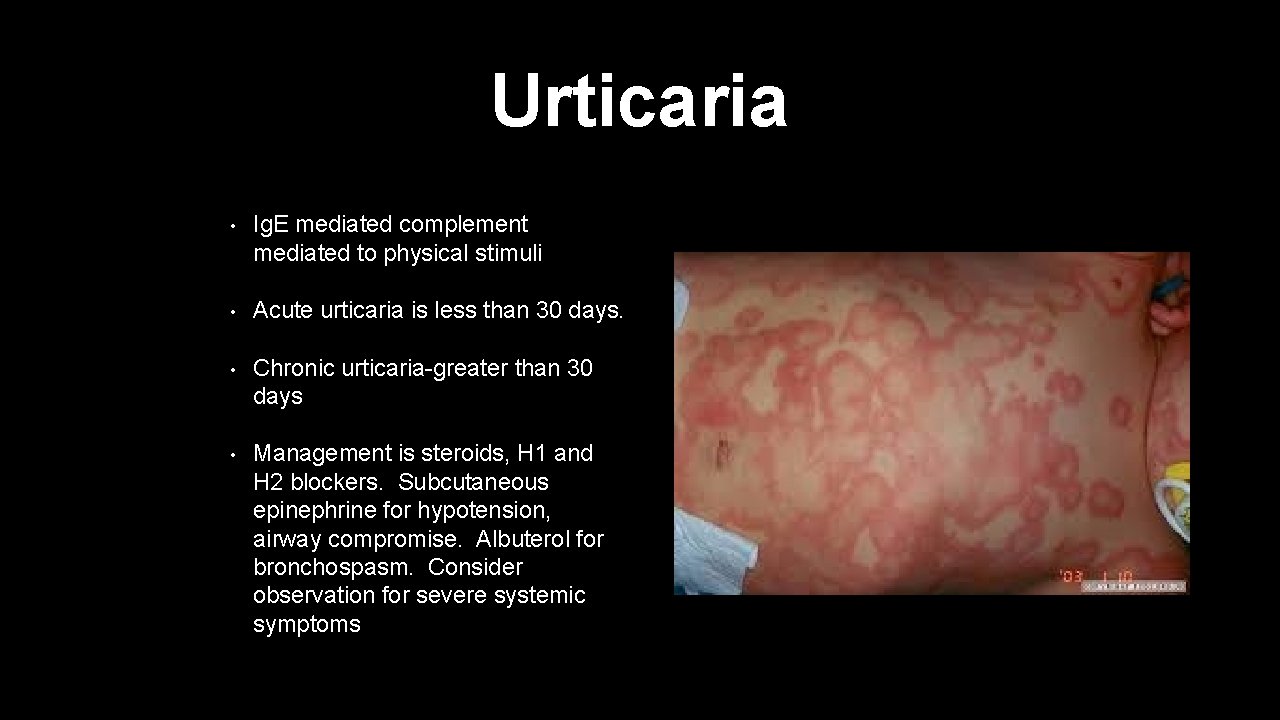
Urticaria • Ig. E mediated complement mediated to physical stimuli • Acute urticaria is less than 30 days. • Chronic urticaria-greater than 30 days • Management is steroids, H 1 and H 2 blockers. Subcutaneous epinephrine for hypotension, airway compromise. Albuterol for bronchospasm. Consider observation for severe systemic symptoms
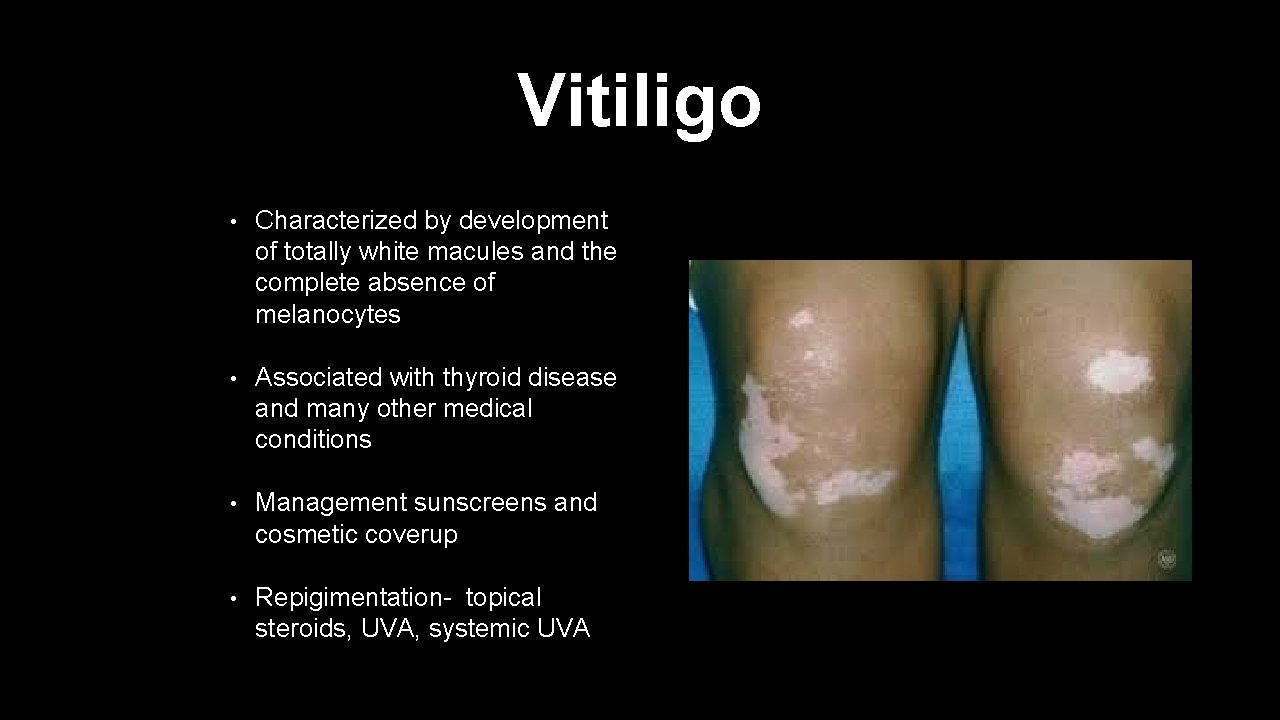
Vitiligo • Characterized by development of totally white macules and the complete absence of melanocytes • Associated with thyroid disease and many other medical conditions • Management sunscreens and cosmetic coverup • Repigimentation- topical steroids, UVA, systemic UVA
References • J. Tintinalli et al, Emergency Medicine: A Comprehensive Study Guide, 6 th Ed. 2014 • Currrent Medical: Diagnosis and Treatment 2013, 44 th ed. • Essentials of Musculoskeletal Care, Greene, 2 nd Ed. • www. medscape. com • Nelson's Essentials of Pediatrics, 5 th ed. • www. uptodate. com • Current Pediatric Diagnosis & Treatment, 16 th ed.
• Current Obstetric & Gynecologic Diagnosis & Treatment, 9 th Ed. • Schwartz’s Principles of Surgery, 2005 • Habif, Clinical Dermatology, 4 th ed. • 2014 CURRENT Medical Diagnosis and Treatment
- Slides: 110