Dermatology and HIV HAIVN Harvard Medical School AIDS










- Slides: 41
Dermatology and HIV HAIVN Harvard Medical School AIDS Initiative in Vietnam
Learning Objectives By the end of this session, participants should be able to: n Describe the most common skin diseases among PLHIV in Vietnam n Explain how to treat these skin conditions 2
What are Common Skin Conditions Among PLHIV in Vietnam? n n n Pruritis Drug allergy rash Varicella-Zoster Herpes Simplex Seborrheic dermatitis n n Scabies Molluscum contagiosum Penicillium Marneffei PPE (Papulo. Pruritic Eruption) 3
Pruritis - Itchy Skin (1) Causes: n Dry scaly skin: • Seborrheic dermatitis • Fungal infection • Eczema • Xerosis n Papules: • Scabies • Insect bites • Eosinophilic folliculitis • Papulopruritic eruption • Infections 4
Pruritis - Itchy Skin (2) Treatment: n Oral antihistamines n Topical moisturizers n Topical steroids n Avoid excessive bathing, soap, or hot water 5
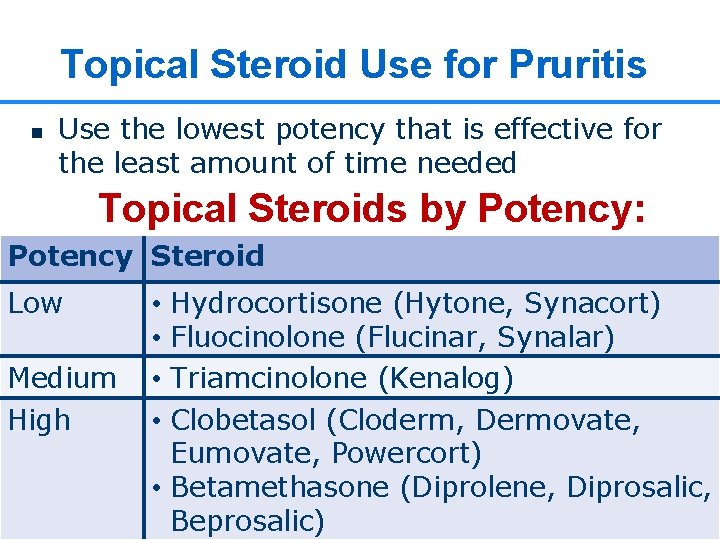
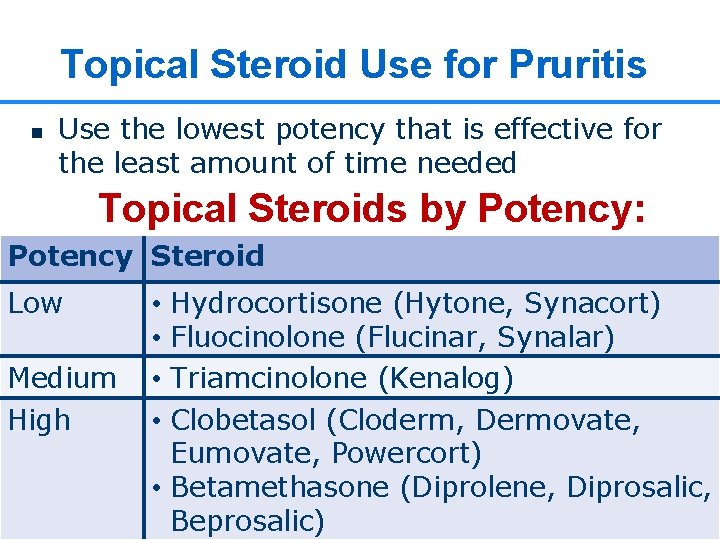
Topical Steroid Use for Pruritis n Use the lowest potency that is effective for the least amount of time needed Topical Steroids by Potency: Potency Steroid Low Medium High Hydrocortisone (Hytone, Synacort) Fluocinolone (Flucinar, Synalar) Triamcinolone (Kenalog) Clobetasol (Cloderm, Dermovate, Eumovate, Powercort) • Betamethasone (Diprolene, Diprosalic, 6 Beprosalic) • •
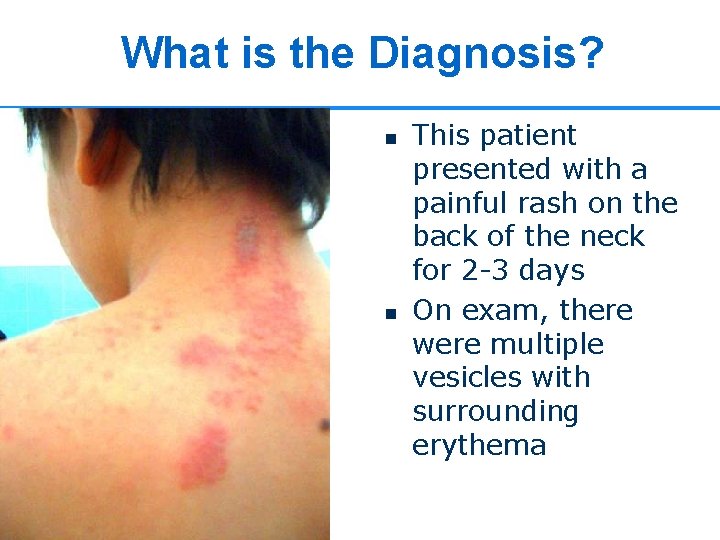
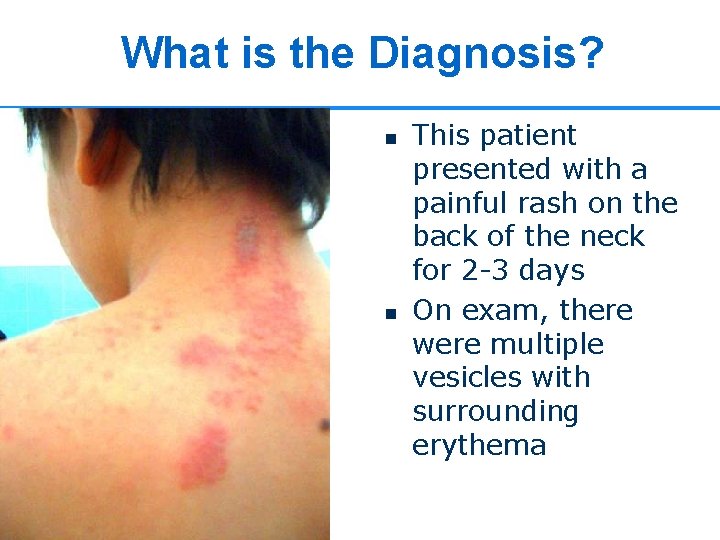
What is the Diagnosis? n n This patient presented with a painful rash on the back of the neck for 2 -3 days On exam, there were multiple vesicles with surrounding erythema 7
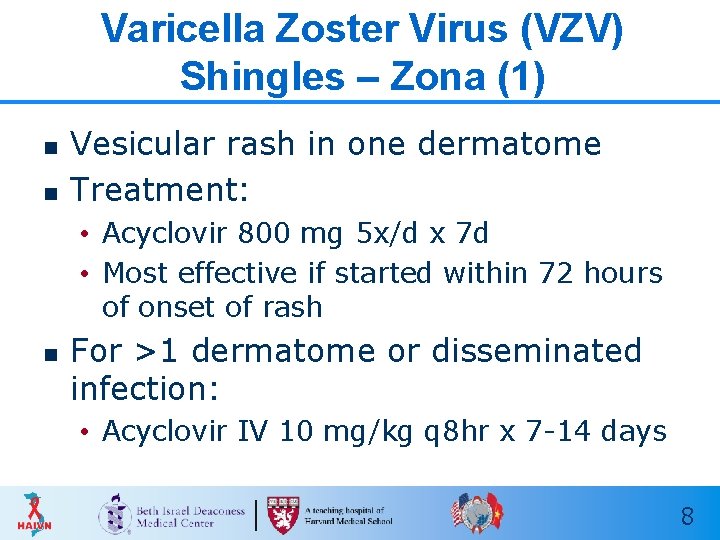
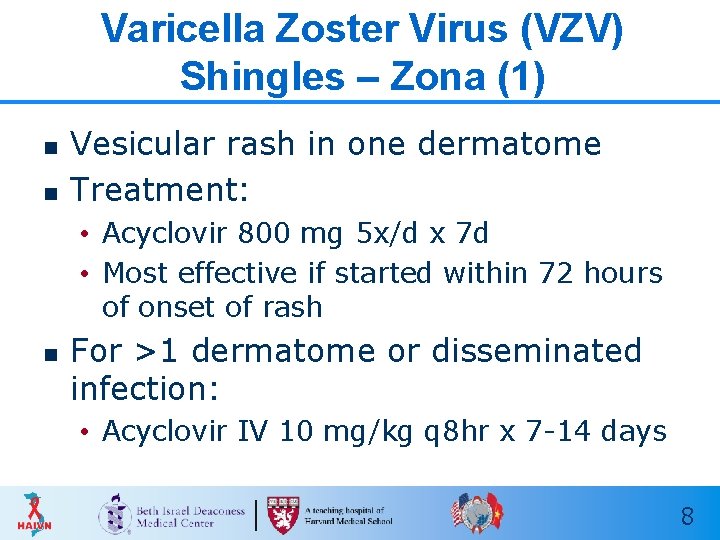
Varicella Zoster Virus (VZV) Shingles – Zona (1) n n Vesicular rash in one dermatome Treatment: • Acyclovir 800 mg 5 x/d x 7 d • Most effective if started within 72 hours of onset of rash n For >1 dermatome or disseminated infection: • Acyclovir IV 10 mg/kg q 8 hr x 7 -14 days 8

Varicella Zoster Virus (VZV) Shingles – “Zona” (2) 9
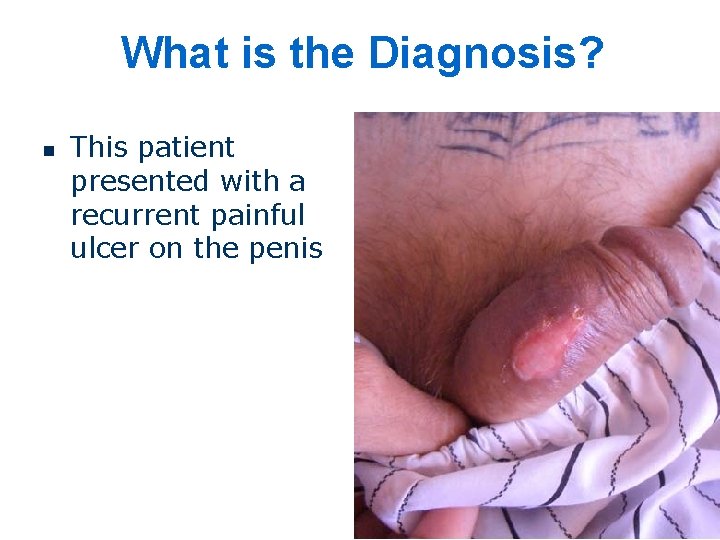
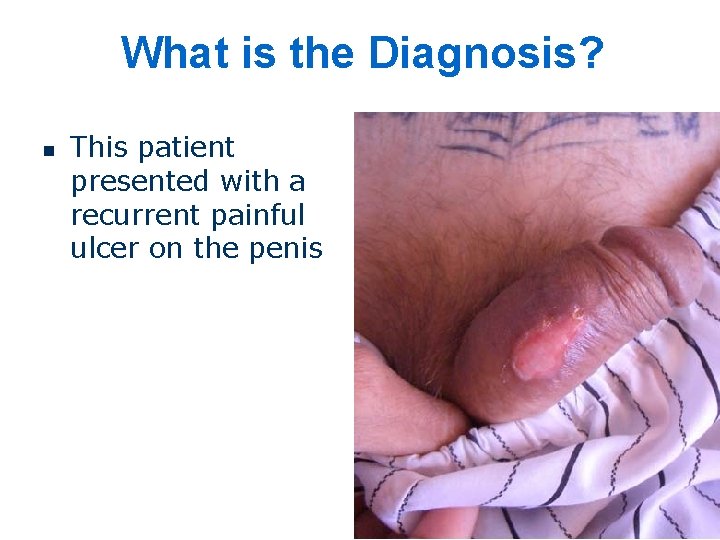
What is the Diagnosis? n This patient presented with a recurrent painful ulcer on the penis
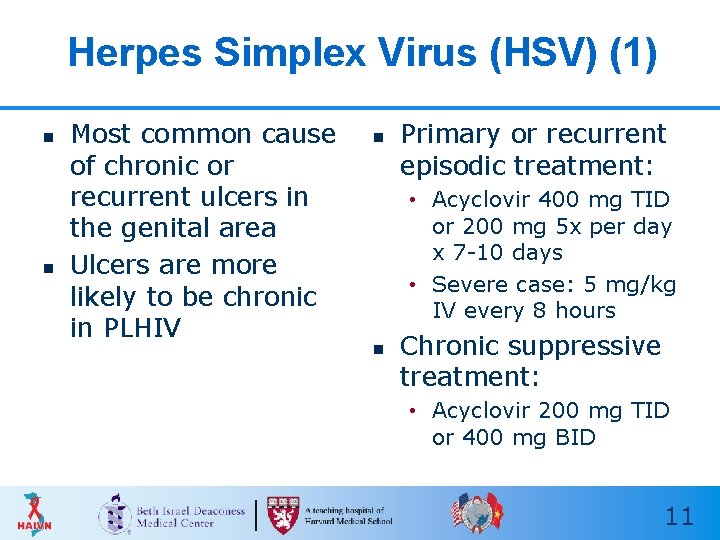
Herpes Simplex Virus (HSV) (1) n n Most common cause of chronic or recurrent ulcers in the genital area Ulcers are more likely to be chronic in PLHIV n Primary or recurrent episodic treatment: • Acyclovir 400 mg TID or 200 mg 5 x per day x 7 -10 days • Severe case: 5 mg/kg IV every 8 hours n Chronic suppressive treatment: • Acyclovir 200 mg TID or 400 mg BID 11

Herpes Simplex Virus (HSV) (2) Chronic ulcer on scrotum Chronic ulcer on hand
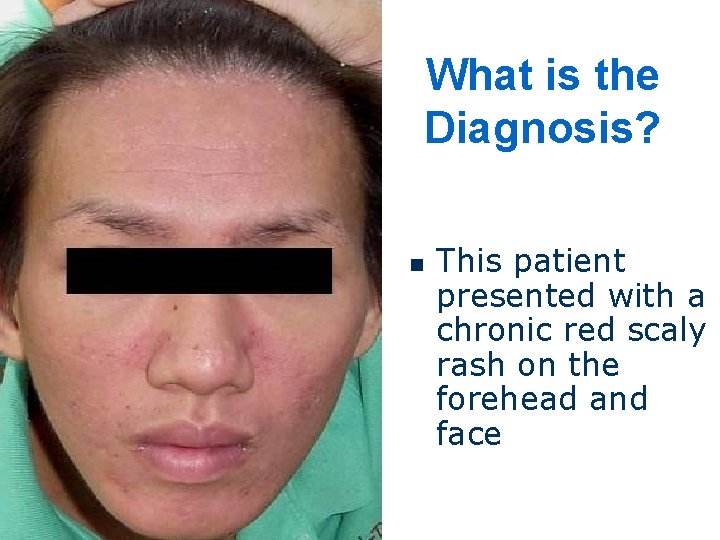
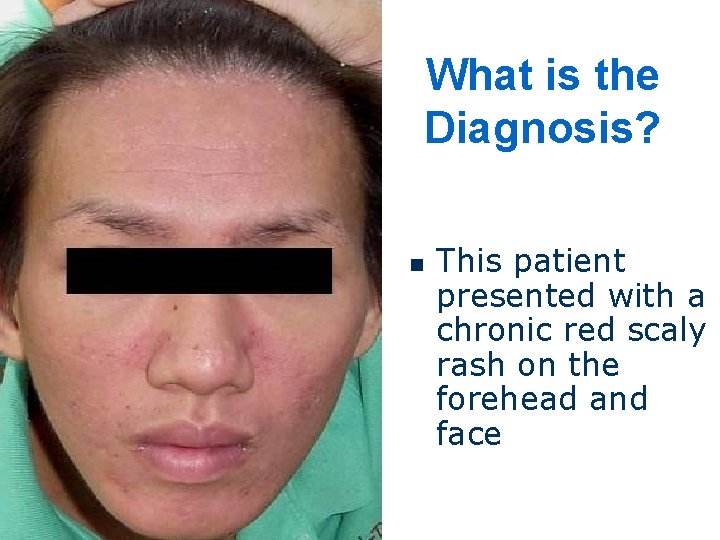
What is the Diagnosis? n This patient presented with a chronic red scaly rash on the forehead and face

Seborrheic Dermatitis (1) n n Cause: Dermatophyte (fungal) Erythematous, papular to scaly rash CD 4 < 500 Nasolabial fold, beard, hairlines

Seborrheic Dermatitis (2) Treatment: n Ketoconazole cream or shampoo n Shampoos (tar, selenium sulfide) n Low potency steroid cream (hydrocortisone or antifungal) n Antiretroviral Therapy 15
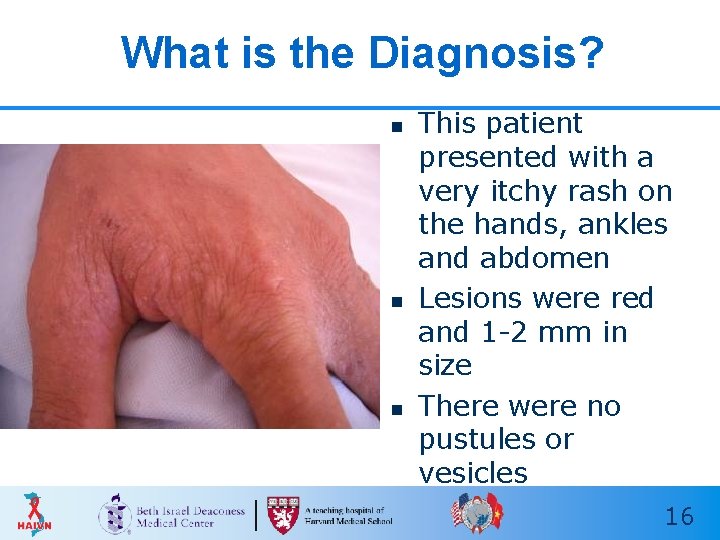
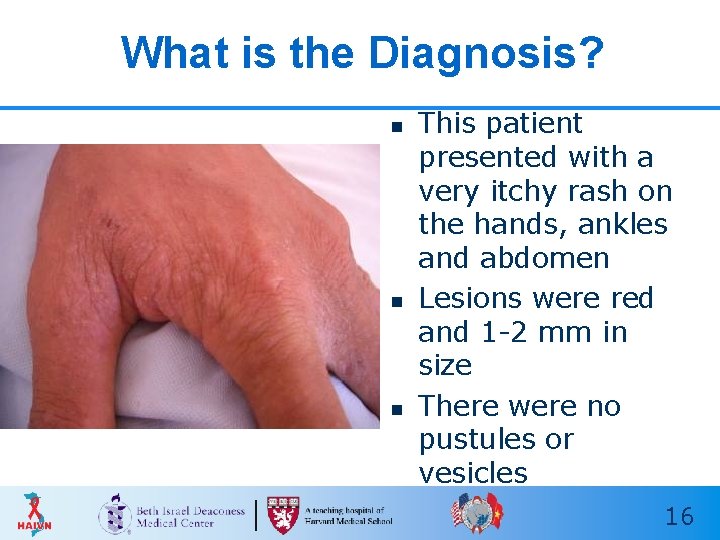
What is the Diagnosis? n n n This patient presented with a very itchy rash on the hands, ankles and abdomen Lesions were red and 1 -2 mm in size There were no pustules or vesicles 16
Scabies (1) n n Cause: Sarcoptes Scabiei (mites) Symptoms: • Itchy, red, papular lesions • Linear “burrows”, often between fingers n n Commonly located on hands, wrists and ankles, and groin Norwegian Scabies • Severe form in PLHIV • Hyperkeratotic lesions 17

Scabies (2)
Scabies (3) Treatment: n Benzyl benzoate, DEP n Permethrin 5%- safe for children >2 months n Lindane 1%- not safe in young children or pregnancy n Ivermectin 19
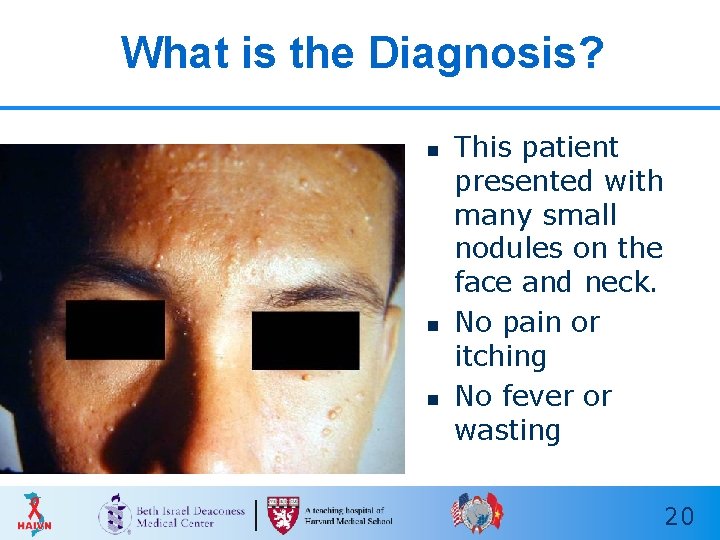
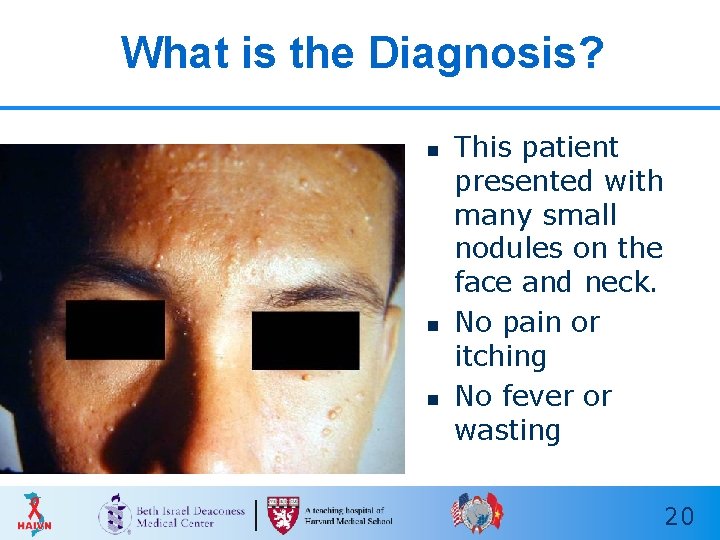
What is the Diagnosis? n n n This patient presented with many small nodules on the face and neck. No pain or itching No fever or wasting 20
Molluscum Contagiosum (MC) (1) n n n Caused by a viral infection (MC virus) Spread by direct skin-to-skin contact Lesions: • Chronic, dome shaped papules (2 to 5 mm) • Shiny surface and central umbilication • Must differentiate from Penicillium and Cryptococcus n Lesions can be found anywhere on the body except the palms and soles 21

Molluscum Contagiosum (2)
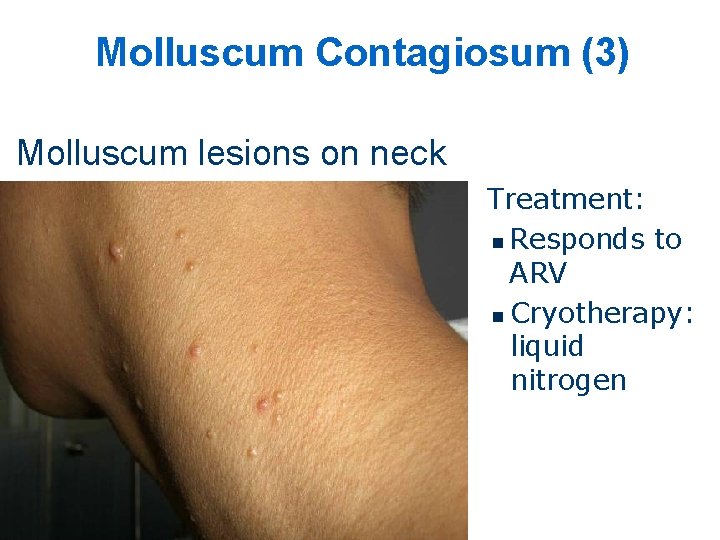
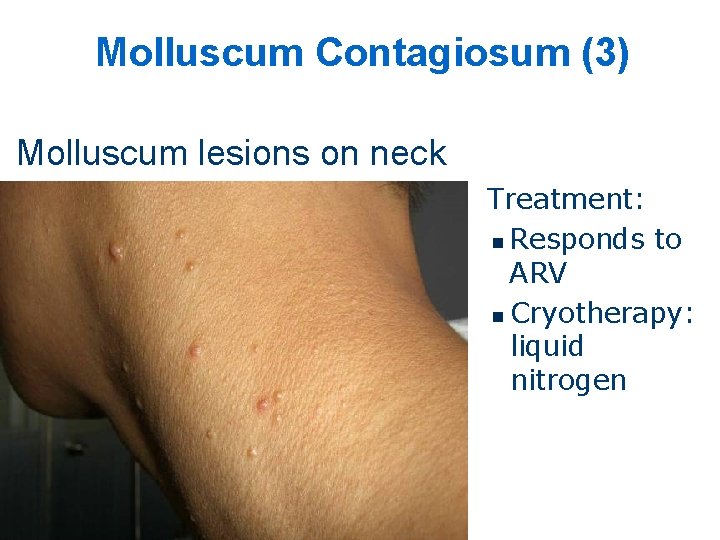
Molluscum Contagiosum (3) Molluscum lesions on neck Treatment: n Responds to ARV n Cryotherapy: liquid nitrogen
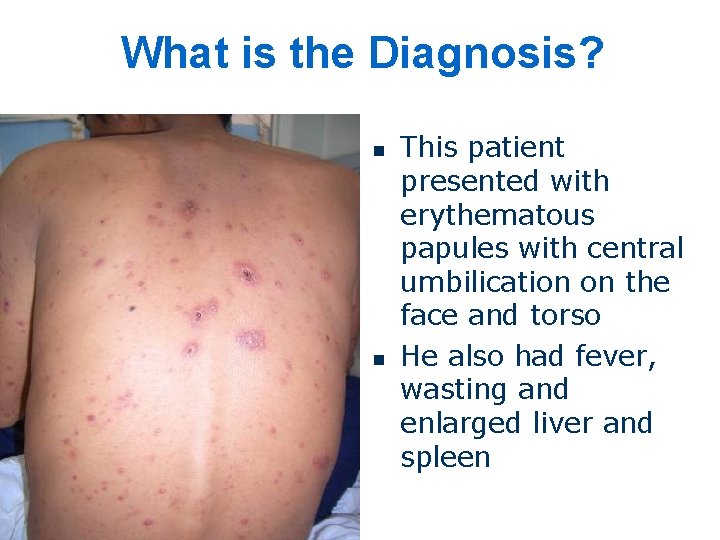
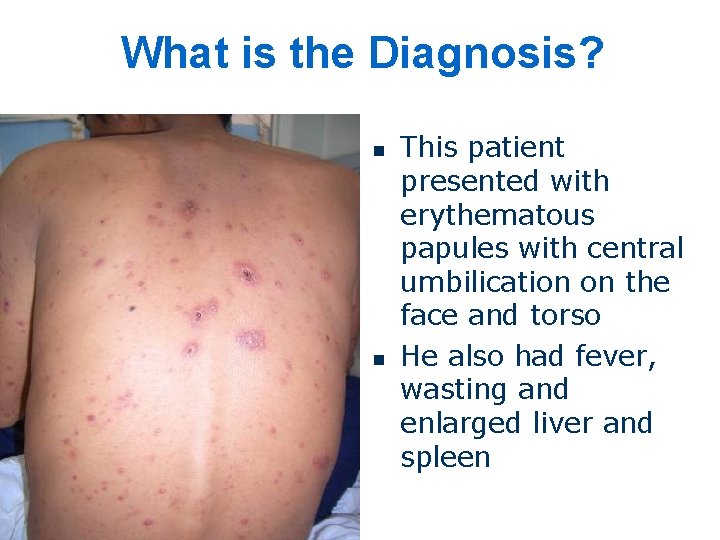
What is the Diagnosis? n n This patient presented with erythematous papules with central umbilication on the face and torso He also had fever, wasting and enlarged liver and spleen
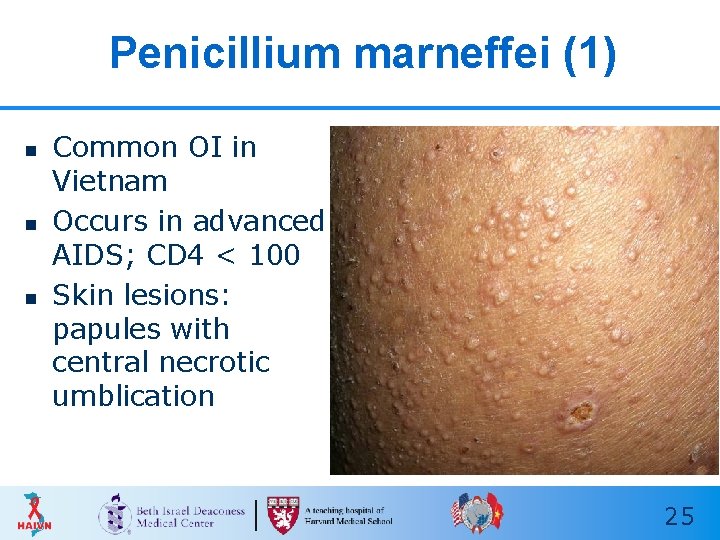
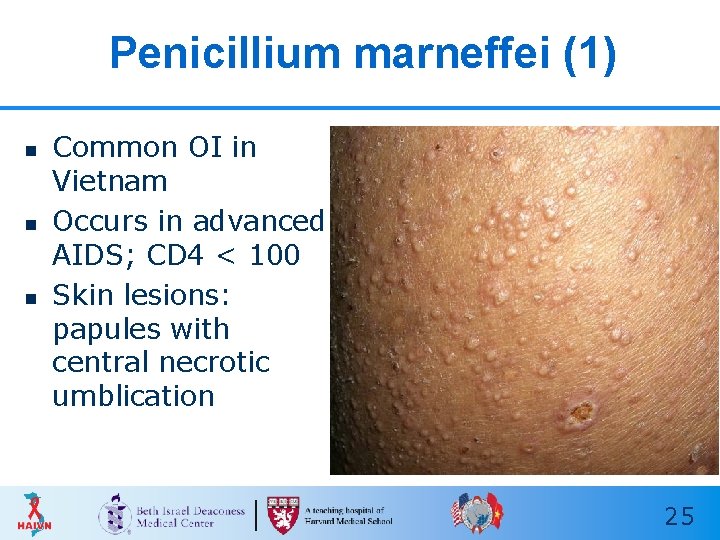
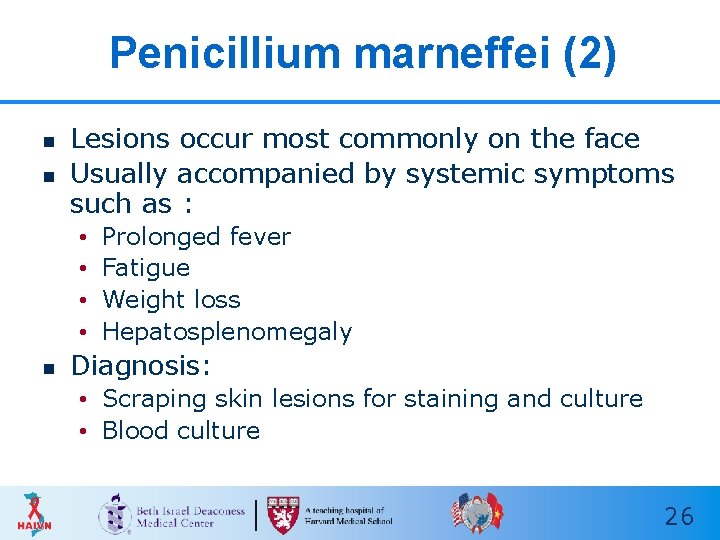
Penicillium marneffei (1) n n n Common OI in Vietnam Occurs in advanced AIDS; CD 4 < 100 Skin lesions: papules with central necrotic umblication 25
Penicillium marneffei (2) n n Lesions occur most commonly on the face Usually accompanied by systemic symptoms such as : • • n Prolonged fever Fatigue Weight loss Hepatosplenomegaly Diagnosis: • Scraping skin lesions for staining and culture • Blood culture 26

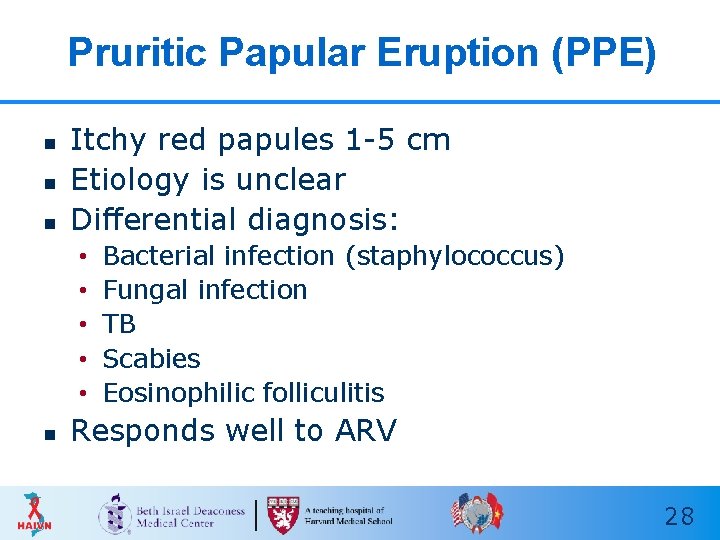
What is the Diagnosis? n n This patient presented with a very itchy papular rash on the legs No fever or other symptoms
Pruritic Papular Eruption (PPE) n n n Itchy red papules 1 -5 cm Etiology is unclear Differential diagnosis: • • • n Bacterial infection (staphylococcus) Fungal infection TB Scabies Eosinophilic folliculitis Responds well to ARV 28

A B Identify the Skin Condition (1) C D

Oral Mucosal Lesions
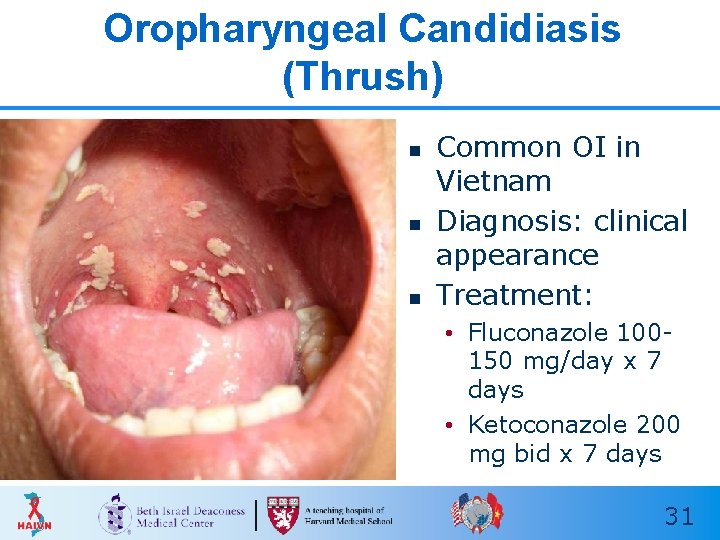
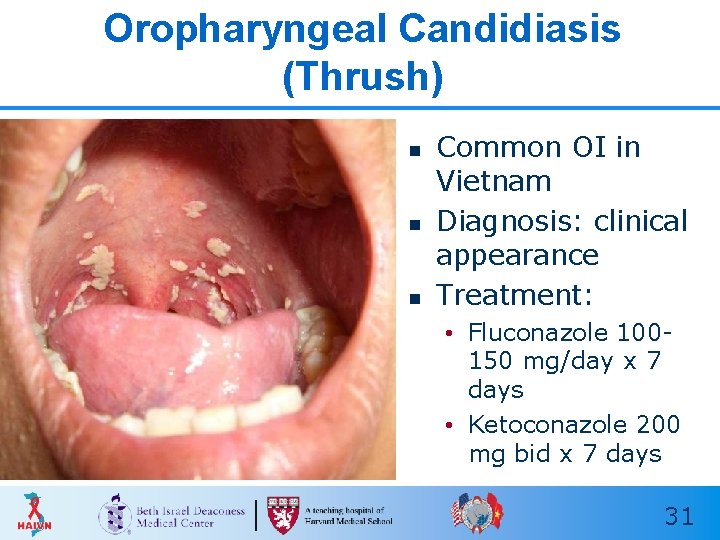
Oropharyngeal Candidiasis (Thrush) n n n Common OI in Vietnam Diagnosis: clinical appearance Treatment: • Fluconazole 100150 mg/day x 7 days • Ketoconazole 200 mg bid x 7 days 31
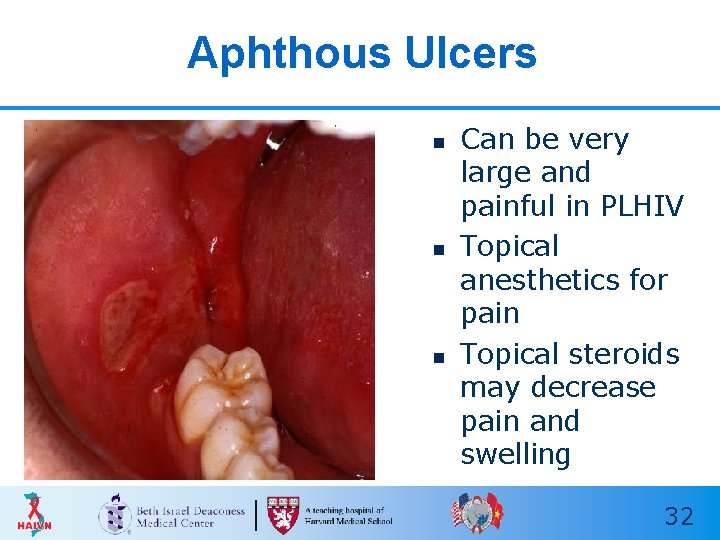
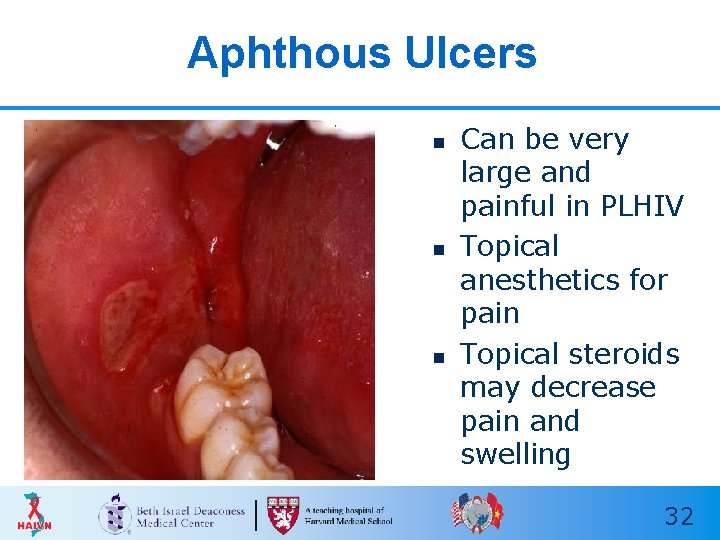
Aphthous Ulcers n n n Can be very large and painful in PLHIV Topical anesthetics for pain Topical steroids may decrease pain and swelling 32
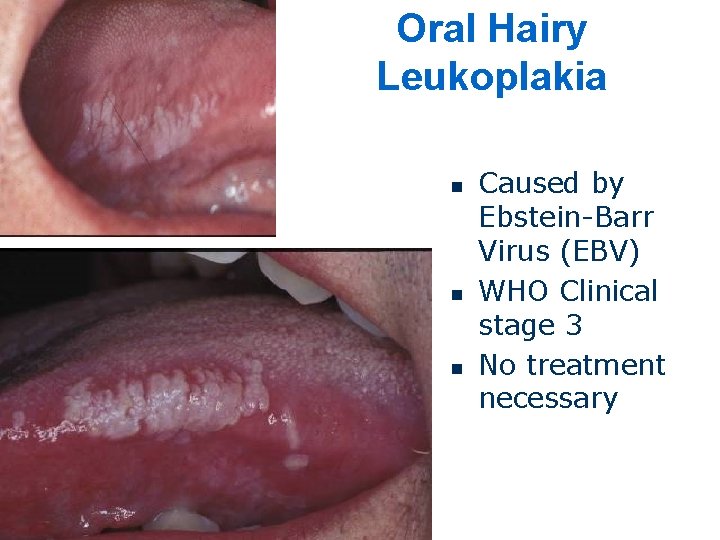
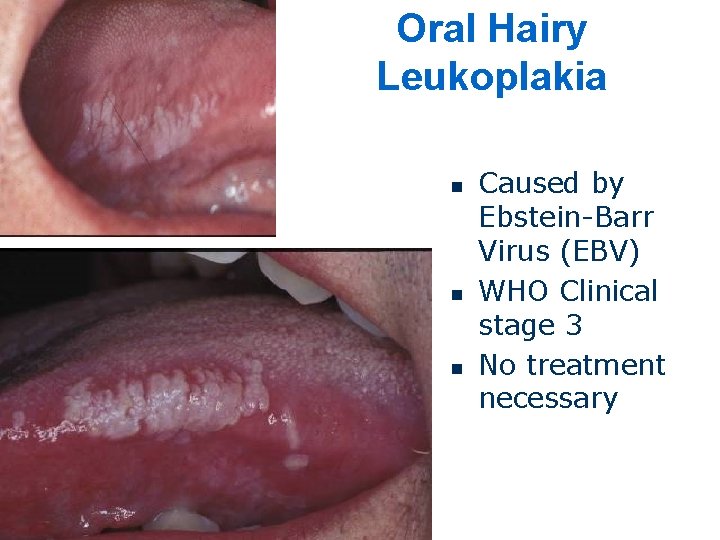
Oral Hairy Leukoplakia n n n Caused by Ebstein-Barr Virus (EBV) WHO Clinical stage 3 No treatment necessary
Less Common Skin Conditions n Eosinophilic Folliculitis n Cryptococcal Infection n Bacillary Angiomatosis n Kaposi’s Sarcoma 34
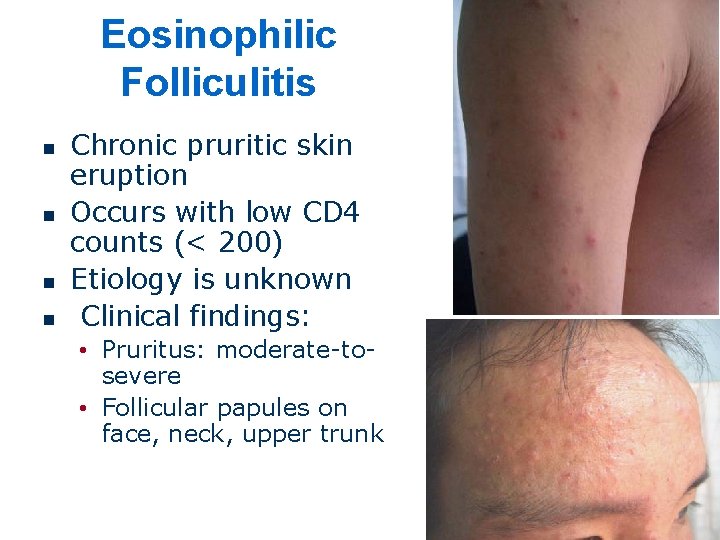
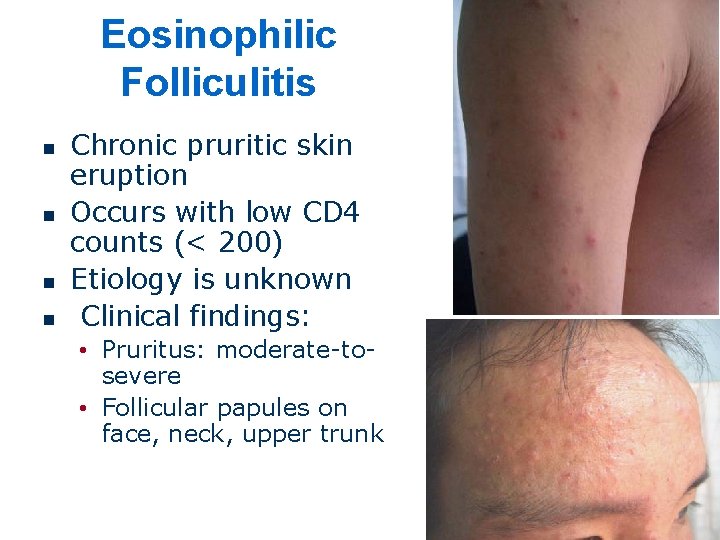
Eosinophilic Folliculitis n n Chronic pruritic skin eruption Occurs with low CD 4 counts (< 200) Etiology is unknown Clinical findings: • Pruritus: moderate-tosevere • Follicular papules on face, neck, upper trunk
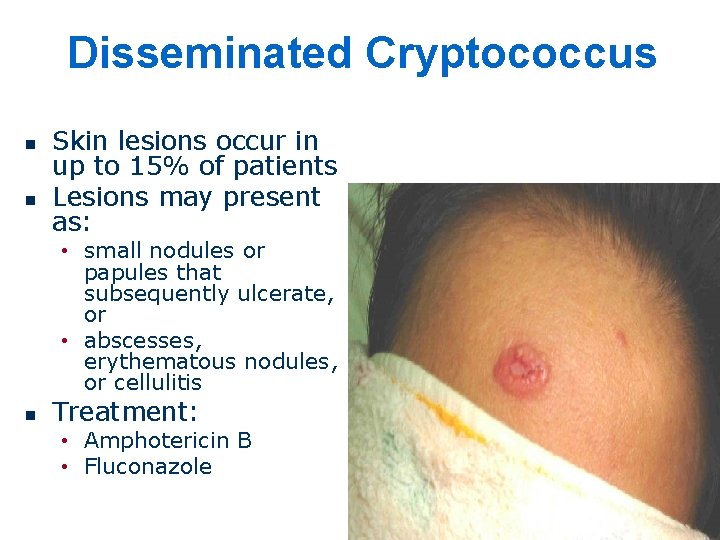
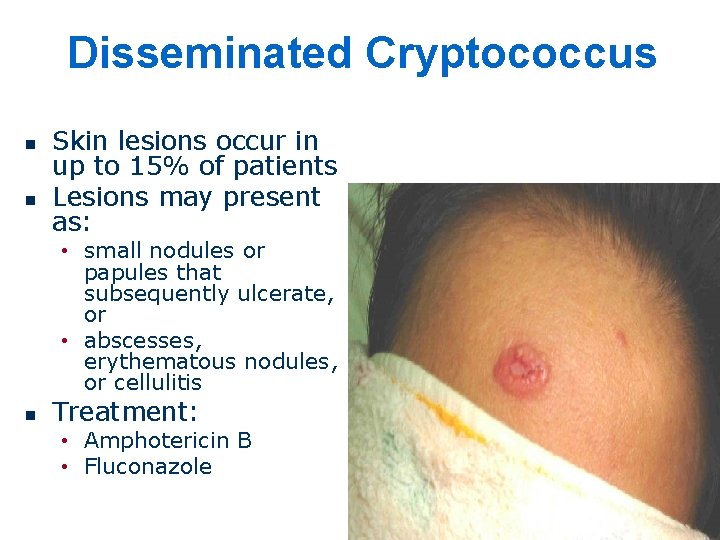
Disseminated Cryptococcus n n Skin lesions occur in up to 15% of patients Lesions may present as: • small nodules or papules that subsequently ulcerate, or • abscesses, erythematous nodules, or cellulitis n Treatment: • Amphotericin B • Fluconazole
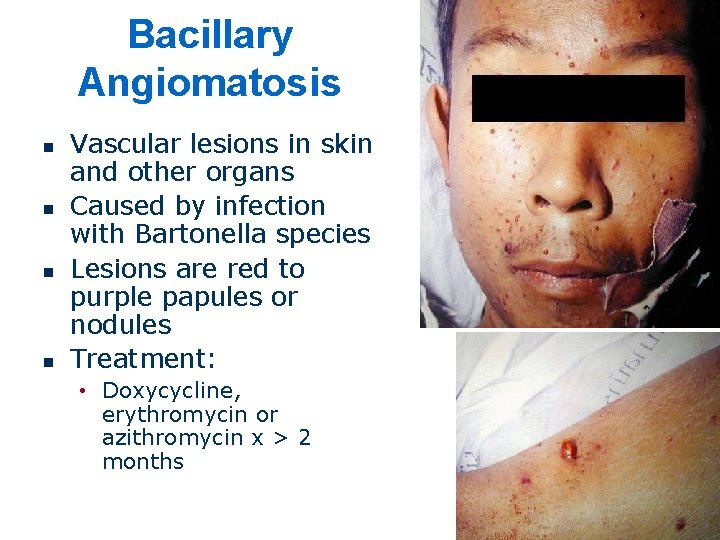
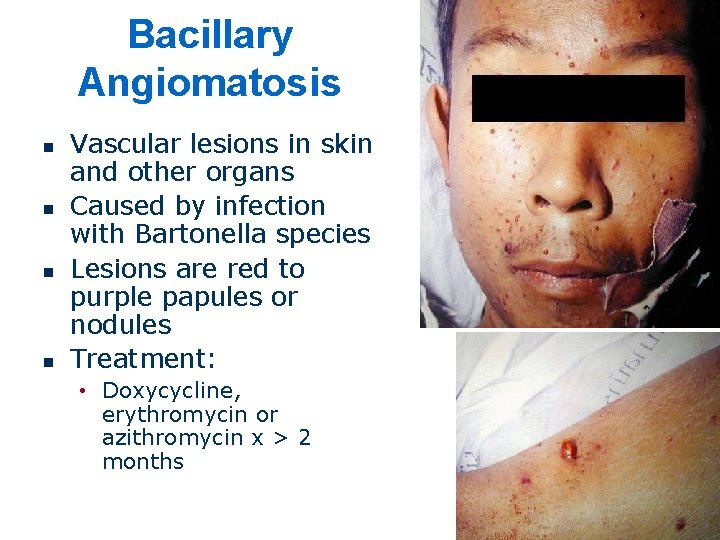
Bacillary Angiomatosis n n Vascular lesions in skin and other organs Caused by infection with Bartonella species Lesions are red to purple papules or nodules Treatment: • Doxycycline, erythromycin or azithromycin x > 2 months
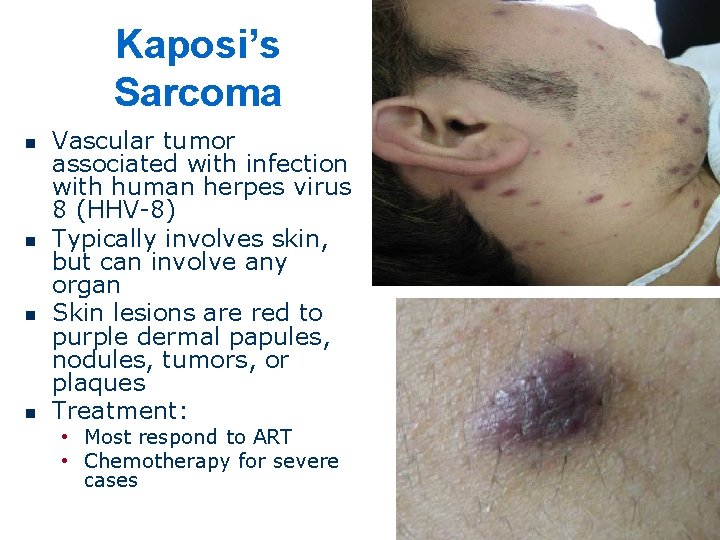
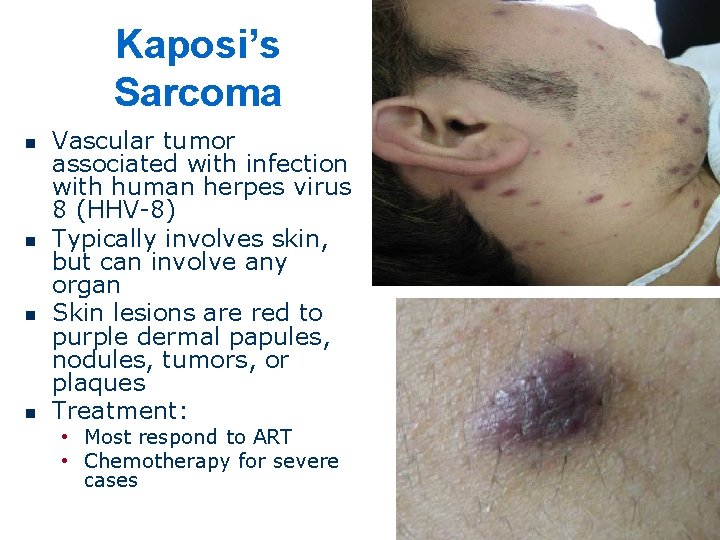
Kaposi’s Sarcoma n n Vascular tumor associated with infection with human herpes virus 8 (HHV-8) Typically involves skin, but can involve any organ Skin lesions are red to purple dermal papules, nodules, tumors, or plaques Treatment: • Most respond to ART • Chemotherapy for severe cases

E F Identify the Skin Condition (2) G H
Key Points n n n Skin conditions are very common in PLHIV, but can be difficult to diagnose If treatment is not effective, biopsy may be necessary to make a diagnosis Most skin conditions will improve with ART 40
Thank you! Questions?