Depression In adults NICE Clinical Guidelines 90 91


- Slides: 50
Depression (In adults) NICE Clinical Guidelines 90 & 91 2009 & KTT 8 2015 Durham and Tees Valley VTS Sept 2017 Dr Rachel Lunney Dr Steven Rowan
Learning outcomes • By the end of this session GPRs will be able to: • Recall key elements of the NICE guideline on depression (CG 90+91), regarding diagnosis, assessment and stepped care management • Relate the NICE guideline to clinical cases of patients with depression Curriculum coverage (2012) • 3. 10 Care of People with Mental Health Problems
Depression Why do I need to know this? Why the need for a NICE guideline? (NB Updated NICE guidance on Depression in children & young people not covered here: QS 48 Sept 13 + update Aug 15)
Depression – In context • • Common: 2. 6% Dep’n prevalence UK 16 -74 yr 11. 4% prevalence Anxiety & Depression F>M Under-diagnosed, treatable More common in chronic disease patients Often over-treated with medication Under-resourced for psychological therapies Rewarding to treat Close to your experience?
Your knowledge: starting point • 1) Key symptoms of depression? • 3) First line psychological treatment? • 2) How do you assess patients? • 4) First choice drug?
Lawrence’s story “It could happen to anyone” http: //www. nhs. uk/video/Pages/Clinicaldepress ion. aspx
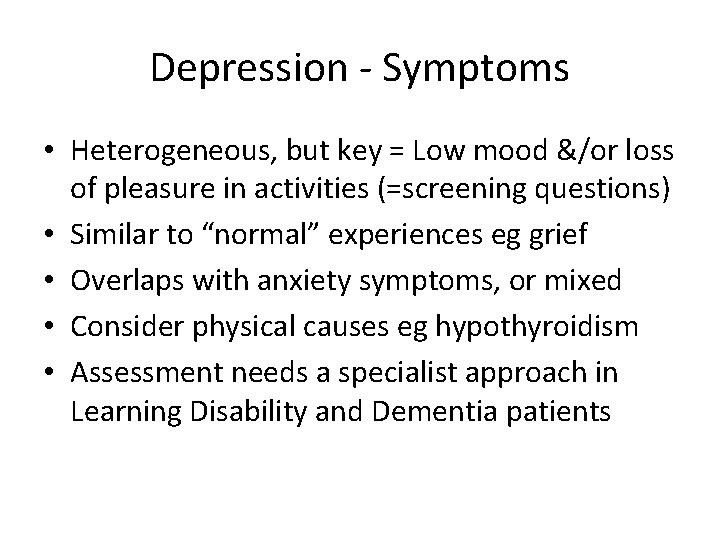
Depression - Symptoms • Heterogeneous, but key = Low mood &/or loss of pleasure in activities (=screening questions) • Similar to “normal” experiences eg grief • Overlaps with anxiety symptoms, or mixed • Consider physical causes eg hypothyroidism • Assessment needs a specialist approach in Learning Disability and Dementia patients
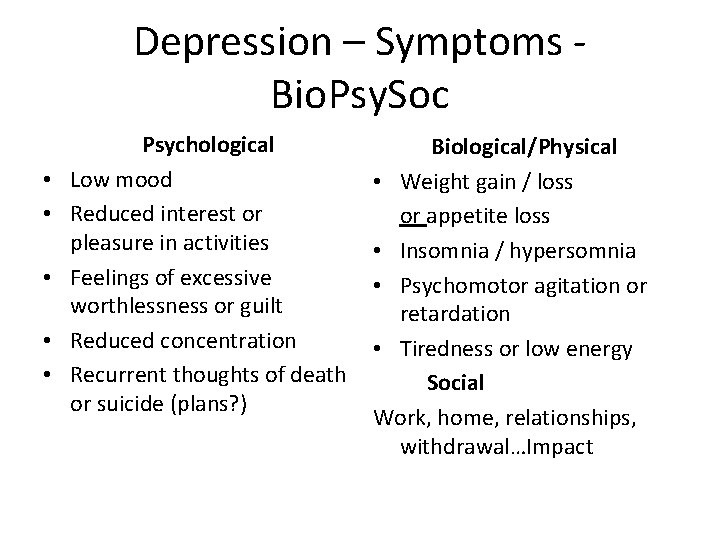
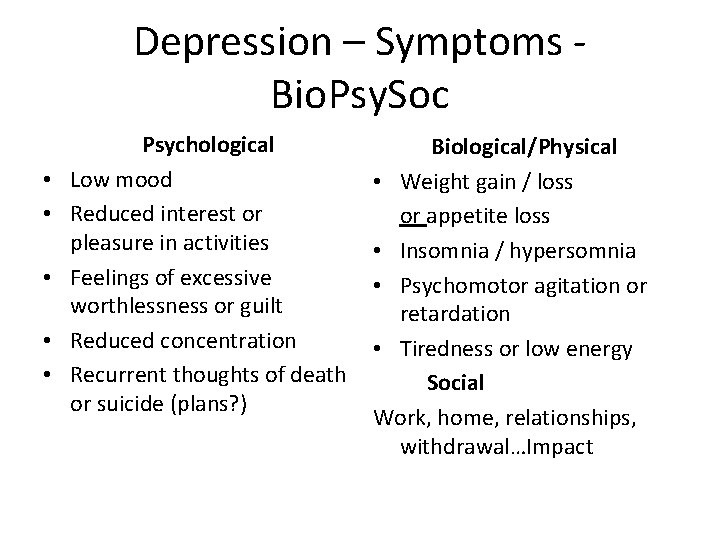
Depression – Symptoms - Bio. Psy. Soc • • • Psychological Low mood Reduced interest or pleasure in activities Feelings of excessive worthlessness or guilt Reduced concentration Recurrent thoughts of death or suicide (plans? ) Biological/Physical • Weight gain / loss or appetite loss • Insomnia / hypersomnia • Psychomotor agitation or retardation • Tiredness or low energy Social Work, home, relationships, withdrawal…Impact
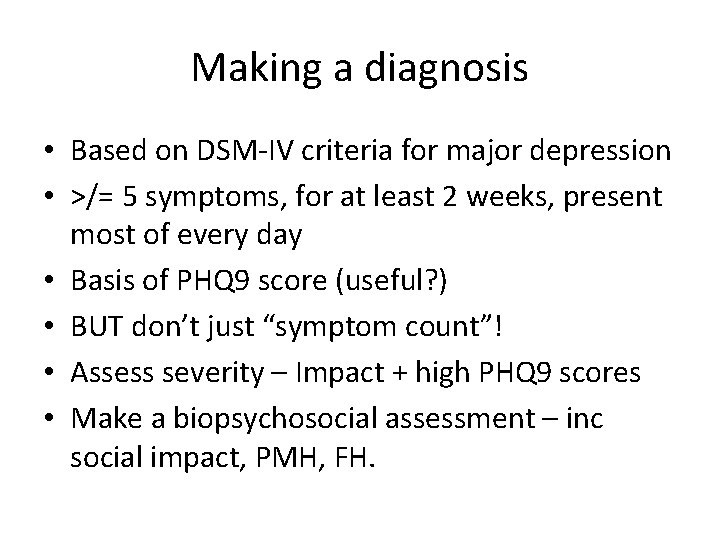
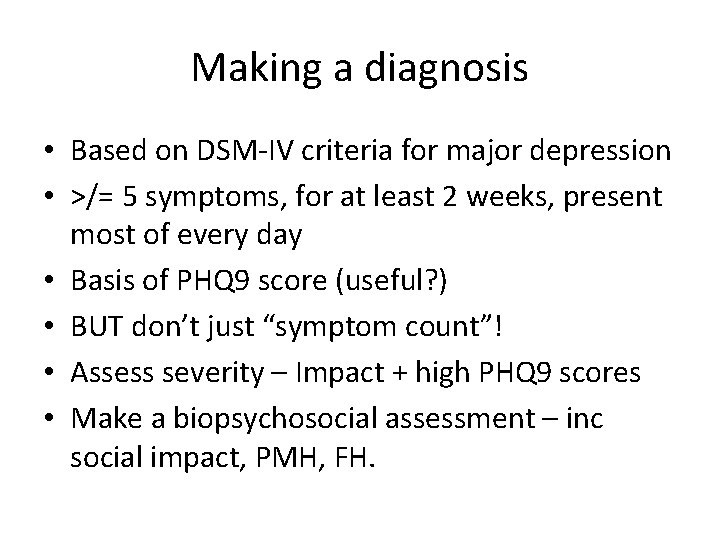
Making a diagnosis • Based on DSM-IV criteria for major depression • >/= 5 symptoms, for at least 2 weeks, present most of every day • Basis of PHQ 9 score (useful? ) • BUT don’t just “symptom count”! • Assess severity – Impact + high PHQ 9 scores • Make a biopsychosocial assessment – inc social impact, PMH, FH.
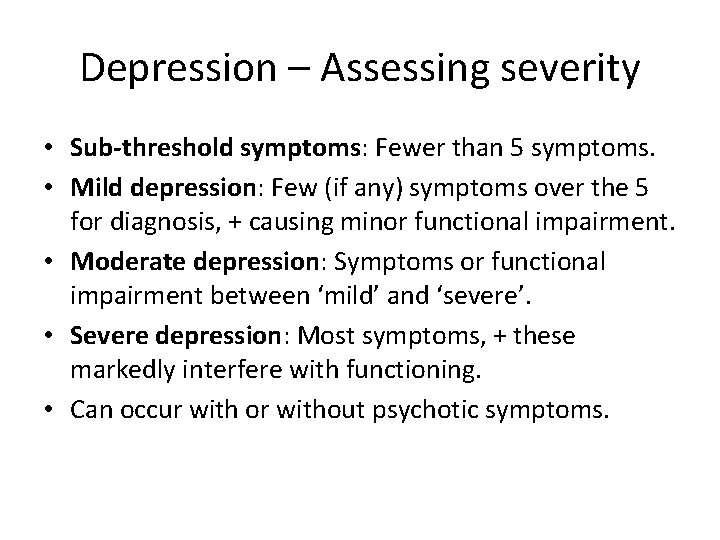
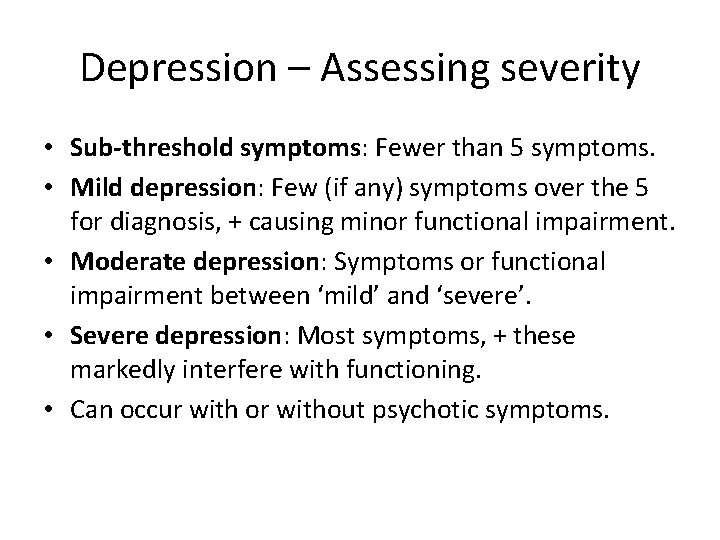
Depression – Assessing severity • Sub-threshold symptoms: Fewer than 5 symptoms. • Mild depression: Few (if any) symptoms over the 5 for diagnosis, + causing minor functional impairment. • Moderate depression: Symptoms or functional impairment between ‘mild’ and ‘severe’. • Severe depression: Most symptoms, + these markedly interfere with functioning. • Can occur with or without psychotic symptoms.
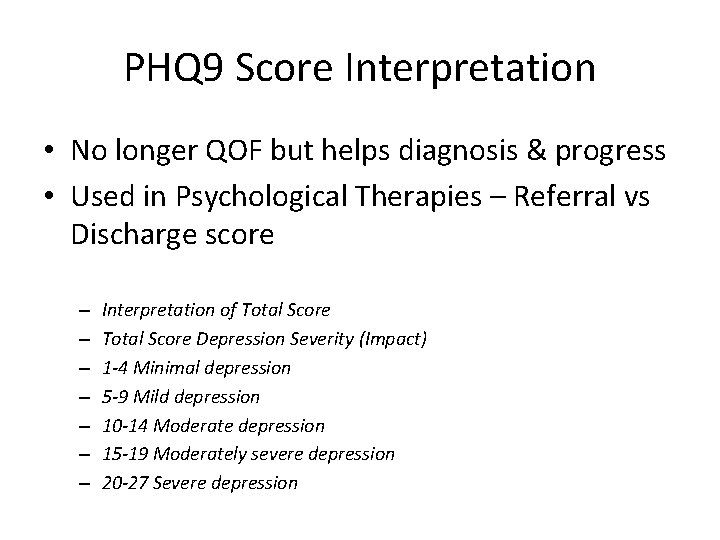
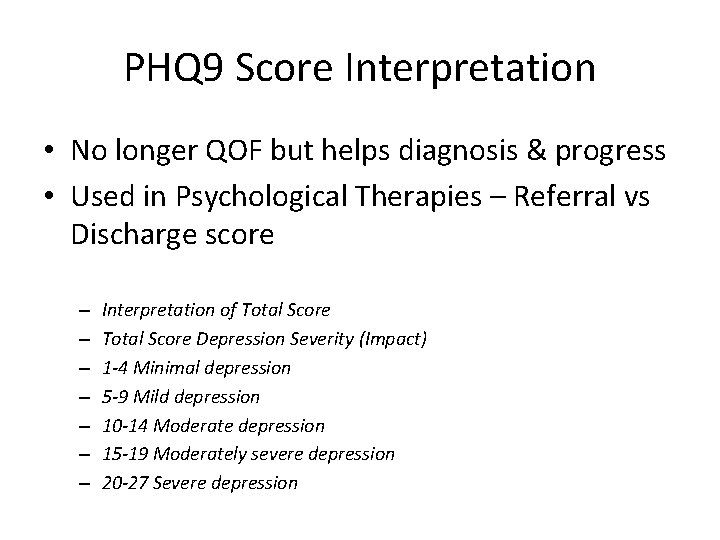
PHQ 9 Score Interpretation • No longer QOF but helps diagnosis & progress • Used in Psychological Therapies – Referral vs Discharge score – – – – Interpretation of Total Score Depression Severity (Impact) 1 -4 Minimal depression 5 -9 Mild depression 10 -14 Moderate depression 15 -19 Moderately severe depression 20 -27 Severe depression
Previous Qo. F 2013/14 (Not NICE) Qo. F removed this 2014/15 Biopsychosocial Assessment “Newly diagnosed depression >/= 18 y should have a biopsychosocial assessment completed on the day of diagnosis. ” Relevant now? Good holistic care Still valuable as a structure for considering impact, resources, challenges for patient?
What was in the BPS Assessment? • • Current symptoms, duration & severity Past history and Family History of MH probs Relationships (partner, children) & support Living conditions Employment & finances (Time off: pros/cons? ) Drug & alcohol use, present & past Suicidal ideation Treatment options, past Rx & responses
Depression in Older People
Depression in Older People Not NICE: BMJ 2011: 343: d 5219 • • Dep’n >65 y ass’d w physical illness & disability Dep’n worsens outcomes in those conditions Prevalence of dep’n 4. 6 -9. 3% of all adults >75 y Higher - Parkinson’s, Dementia, CVA, DM, CVD Social factors influence dep: eg bereavement More functional impact than in younger pts May present differently: somatisation, anxiety, cognitive impairment, psychomotor symptoms
Depression in Older People Not NICE: BMJ 2011: 343: d 5219 Management should be adapted to older pt’s PHQ 9 the only validated GP tool for older pt’s Exclude physical conditions: routine bloods Highest completed suicide risk by age: ask pt Psychosocial interventions are key e. g. groups, meaningful activities, structured exercise • Drugs: SSRIs first line, & safest • • •
Depression So how should we manage it? NICE advice: Stepped Care Psychological therapies Medications
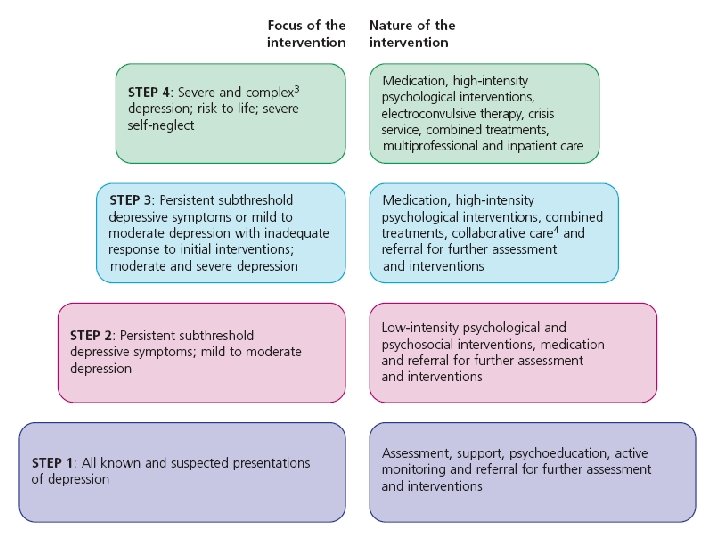
NICE 90 +91 - Key messages • Patient-centred, culturally appropriate • Severity inc impact are key to assessment: BPS • Intervention should reflect severity (stepped care model) and patient preference • Offer Psychological therapies for mild • Add medication for moderate and severe: effective • Consider chronic health problems – Psych’l therapies first. Offer med’n if dep’n affecting their condition • Treat for at least 6/12 from resolution • Consider relapse prevention
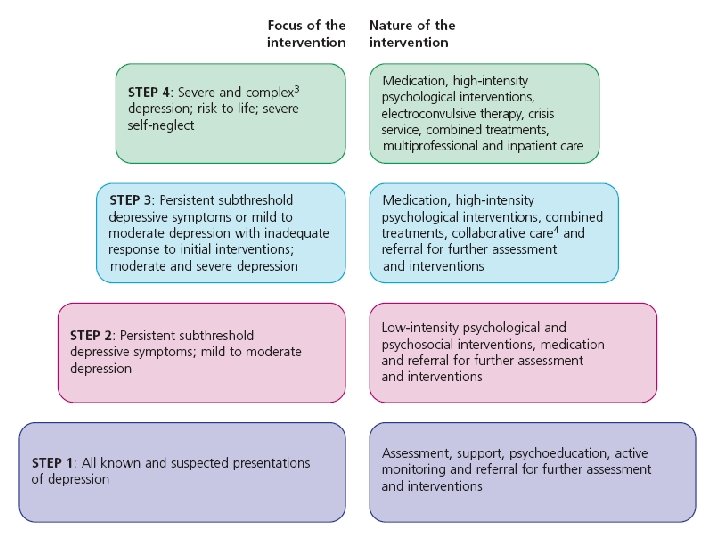
NICE 90 +91 – Stepped care • Consider depression esp in chronic conditions • Low intensity psychosocial intervention for mild-moderate or “sub-threshold” symptoms • Meds only help mild depression if past modsevere episode, no response to psy’social interv’n , or 2 years sub-threshold symptoms • Moderate to severe – Meds effective* + highintensity psychological support (eg CBT) • *Meta-analysis of 234 studies: Ann Int Med 2011; 155: 772
• Identify depression - esp in chronic conditions. Consider using Whooley screening questions: “During the last month, have you often been bothered by: Feeling down, depressed or hopeless? Having little interest or pleasure in doing things? ” • Then make a comprehensive assessment inc: – Symptoms - Duration – Degree of functional impairment PHQ 9 may help – Exclude other explanations / causes
• Explore history & severity : – Past Hx of depression & chronic conditions – Hx of mood elevation (Bipolar under-diagnosed)* – Response to previous treatments – Interpersonal relationships – Support? Impact? – Living conditions & social isolation * - Not in NICE 90. Hot Topics 2011. Bipolar is covered in VTS separately.
• Ask directly about suicidal ideation and intent. If at risk: – Adequate social support & aware of sources of help? eg Samaritans 08457 90 90 90 – Arrange help appropriate to level of risk • Immediate risk: urgent referral to specialist services • Risk of suicide: increased support & referral to MHT – Advise to seek help if the situation deteriorates • Psychoeducation – inc self help booklets, wesbites eg Mood. Gym, Mood Juice, NHS Choices Moodzone • Monitoring – watchful waiting, consider review
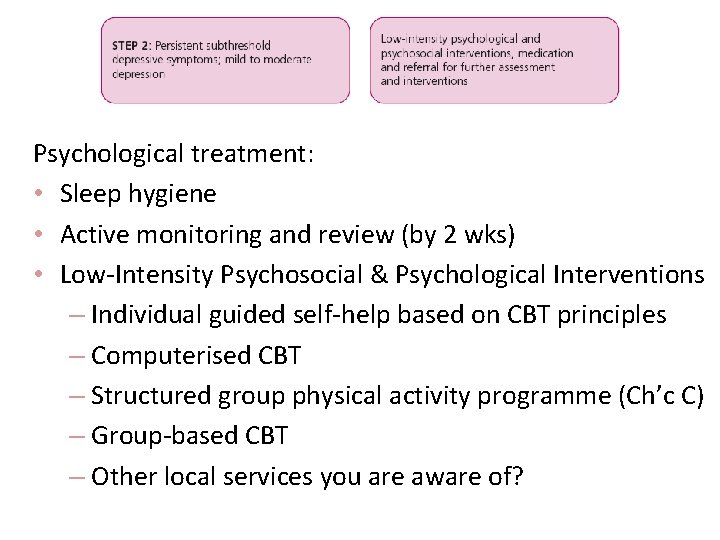
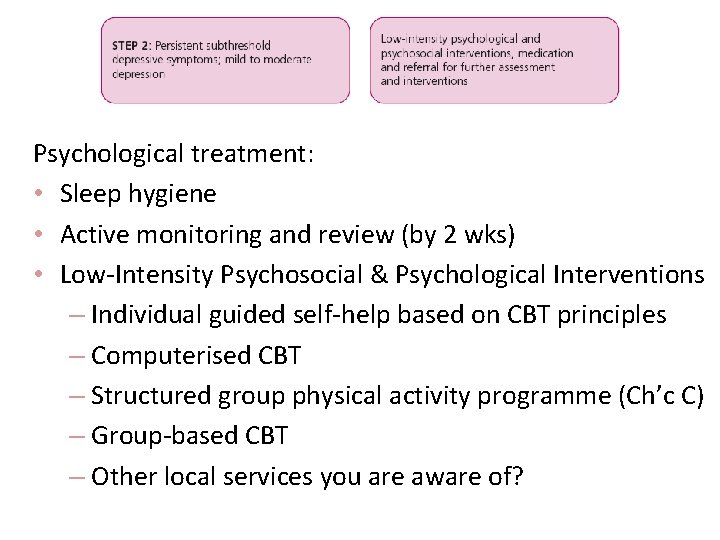
Psychological treatment: • Sleep hygiene • Active monitoring and review (by 2 wks) • Low-Intensity Psychosocial & Psychological Interventions – Individual guided self-help based on CBT principles – Computerised CBT – Structured group physical activity programme (Ch’c C) – Group-based CBT – Other local services you are aware of?
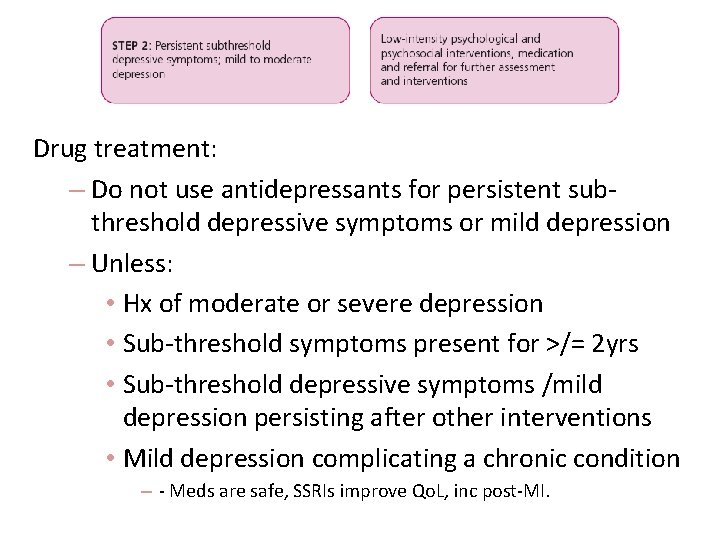
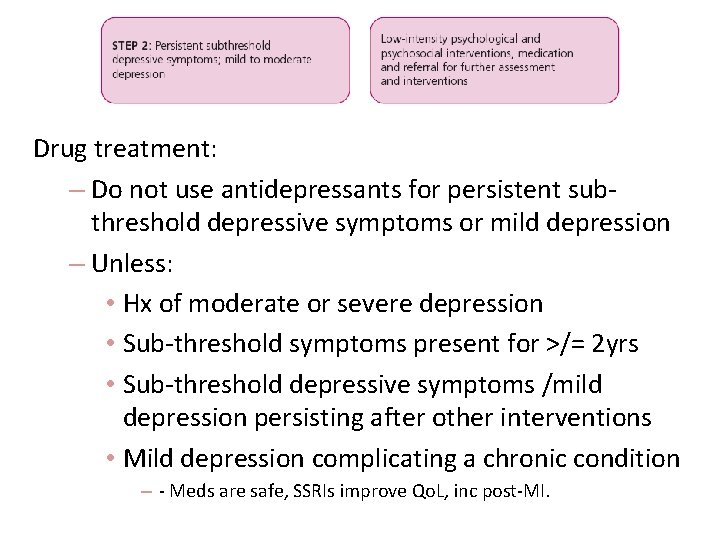
Drug treatment: – Do not use antidepressants for persistent subthreshold depressive symptoms or mild depression – Unless: • Hx of moderate or severe depression • Sub-threshold symptoms present for >/= 2 yrs • Sub-threshold depressive symptoms /mild depression persisting after other interventions • Mild depression complicating a chronic condition – - Meds are safe, SSRIs improve Qo. L, inc post-MI.
Step 2 summary • Low intensity psychological interventions inc self help • Watchful waiting & review • No medication unless sig’t history or 2 yr low Step 3: Mild-moderate Depression What do we offer when more is needed?
Choice of intervention should be influenced by: • Duration of episode & trajectory of symptoms • Hx depression & response to treatment • Likely concordance & potential adverse effects • Patient preference • Patients with moderate or severe depression: • Combine antidepressants with high-intensity psychological intervention
Psychological Intervention: High-Intensity – Individual or group-based CBT (inc Ch’c Cond’n) – Interpersonal psychotherapy (IPT) – Behavioural activation – Behavioural couples therapy – Counselling (can family help/join in? ) – Short-term psychodynamic psychotherapy

Psychological Intervention What’s available? How to “sell it” to patients? http: //www. nhs. uk/video/Pages/Talk ingtherapies. aspx
Antidepressants
Antidepressant drug choice. Consider: • Side effects & interactions Citalopram & Sertraline safest; caution w NSAIDS or Aspirin Citalopram contraind’d w meds prolonging QT interval eg Amiodarone TCAs contraind’d with Warfarin – use Mirtazapine
Antidepressant drug choice. Consider: • Patient’s perception / experience • Toxicity in overdose (eg TCAs, Venlafaxine) • Discuss choice of antidepressant & give information: 1. Gradual development of full effect (from 2 weeks) 2. Concordance, inc 6/12 (or longer) after remission 3. Discontinuation symptoms

Review and ongoing care: – No risk suicide: 2 wks then every 2 -4 wks for 3 mths, then at longer intervals – Risk of suicide / <30 yrs: 1 wk then frequently until lower risk Absent / minimal response at 3 -4 wks: – Concordance? – Consider increasing dose &/or support – Consider switching antidepressant (if SEs or patient prefers. ) See Switching Chart on VTS site
Review and ongoing care: – Inadequate response at 3 -4 wks : Up dose or swap drug (KTT 8 2015; past advice was do so at 4 -6 wks: NICE CG 90/91) – 1 week gap – Some response at 3 -4 wk? Continue 2 -4 wk more before switching drug/amending dose – Follow guidance on withdrawal – Continue meds for 6 months after resolution High risk of relapse (or past severe or recurrent): – Treat for 2 years – Add post-resolution CBT or Mindfulness Therapy
Mindfulness
Mindfulness Evidence shows that Mindfulness-Based Cognitive Therapy can, on average, reduce the risk of relapse for people who experience recurrent depression by 43%. Research also suggests that it’s particularly effective for vulnerable groups who are more likely to relapse (J Williams et al, “Mindfulness -Based Cognitive Therapy for Preventing Relapse in Recurrent Depression: A Randomized Dismantling Trial”, 2013. ). As a psycho-social approach to staying well, it’s a cost-effective and accessible treatment for individuals and providers (M Williams and W Kuyken, “Mindfulness-based cognitive therapy: a promising new approach to preventing depressive relapse”, 2012). http: //www. mentalhealth. org. uk/help-information/mental-health-az/M/mindfulness/
Mindfulness • NICE: >/= 3 episodes, chronic, relapsing dep – 50% reduction in relapse rate • Klyken 2015: RCT Mindfulness (MBCT) vs maintenance antidepressants in chronic dep’n – 55% reduction in antidepressant use • MYRIAD study – Adolescents, 7 yr study of primay prevention in shcools. MBCT helps children more adversely affected in childhood
Completing antidepressant drugs: • • • Patients may be unconfident to try Agree a time; share the plan Reassure pts about transient withdrawal effects Reduce over 4 weeks usually Slower withdrawal with Paroxetine and Venlafaxine Warn about relapse – plan ahead, to reduce the risk
Not NICE: Do drugs really work? BMJ 2012; 344: e 1014/Ann Int Med 2011; 155: 772 • BMJ editorial of meta-analysis of 234 studies inc unpublished evidence & head-to-head drug trials • Antidepressants work in major depression • 2/3 of patients respond to treatment by 12 weeks • This counters claims of low effect sizes in past studies • No clinically important differences between drugs in efficacy, maintenance or relapse prevention • Some differences in speed of onset & side effects: e. g. Mirtazapine has highest risk of weight gain
Step 3 summary • High intensity psychological interventions • Medication tailored to other conditions, preference, side effects • Maintenance phase then slow reduction • Relapse prevention Step 4: When step 3 treatment is not enough, depression is severe or patient at risk
When step 1 -3 interventions do not help? • Do not start combined antidepressants in primary care • Refer to specialist mental health services for oversight • High-intensity psychological interventions – Increased intensity & duration of the interventions • Develop a multidisciplinary care plan with the patient : – Include a crisis plan – Identify crisis triggers & strategies to manage these – Shared with the patient & others eg Ch’c Cond’n Team
When step 1 -3 interventions do not help? • Use crisis resolution & home treatment teams for crises • Consider advance decisions & advance statements if appropriate • Consider inpatient treatment if significant risk of suicide, self-harm or neglect • Consider ECT for severe, life-threatening depression, when a rapid response is required, or other treatments have failed
NICE Clinical Guidelines 90 & 91 Depression Summary: • Identify depression esp in longterm conditions • Diagnose it carefully - >/= 5 symptoms • Assess severity, impact + suicide risk: BPS assessment • Treat in a stepped care approach –Psychological intervention first, + med’s later usually • Tailor the approach in chronic conditions • Review and end treatment carefully • You can make a difference!
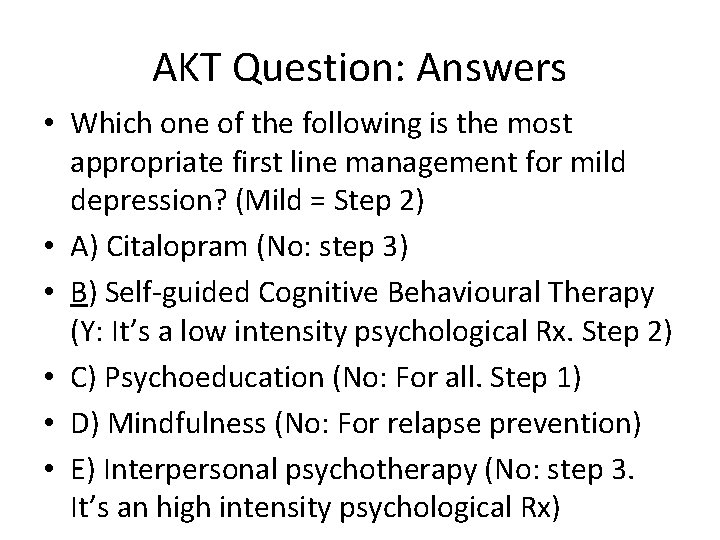
AKT Question • Which one of the following is the most appropriate first line management for mild depression? • A) Citalopram • B) Self-guided Cognitive Behavioural Therapy • C) Psychoeducation • D) Mindfulness • E) Interpersonal psychotherapy
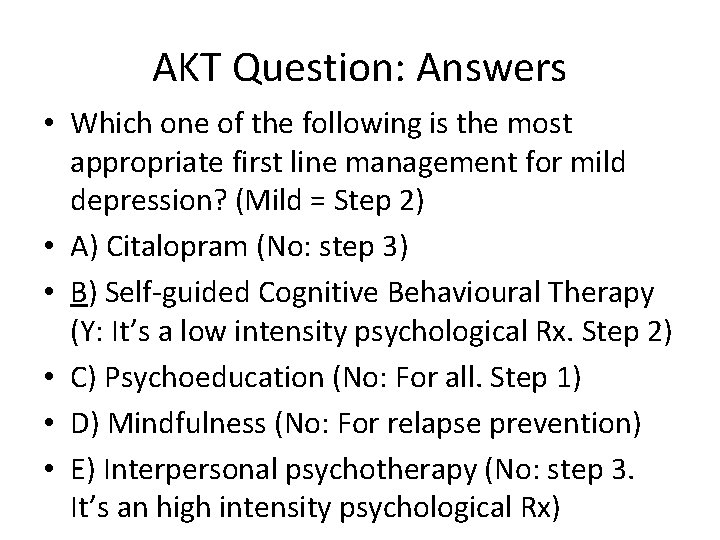
AKT Question: Answers • Which one of the following is the most appropriate first line management for mild depression? (Mild = Step 2) • A) Citalopram (No: step 3) • B) Self-guided Cognitive Behavioural Therapy (Y: It’s a low intensity psychological Rx. Step 2) • C) Psychoeducation (No: For all. Step 1) • D) Mindfulness (No: For relapse prevention) • E) Interpersonal psychotherapy (No: step 3. It’s an high intensity psychological Rx)
NICE Clinical Guidelines 90 & 91 Depression Small groups: Relate the guidance to patient cases – Diagnosis, severity, treatment Consider and discuss your learning needs
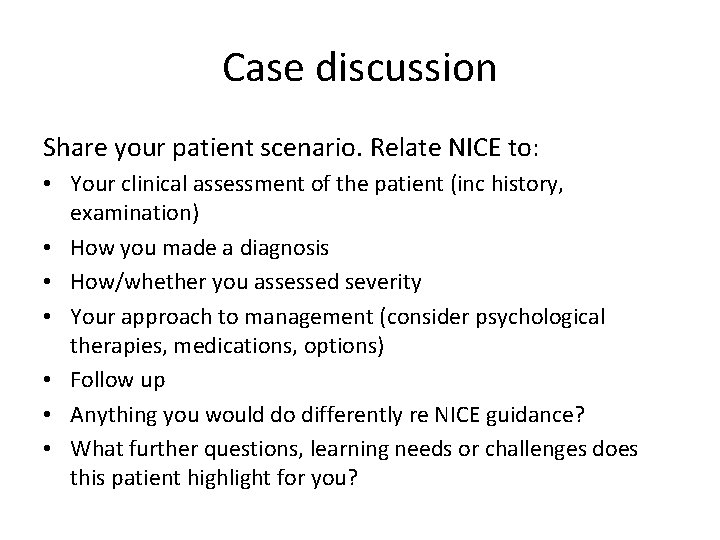
Case discussion Share your patient scenario. Relate NICE to: • Your clinical assessment of the patient (inc history, examination) • How you made a diagnosis • How/whether you assessed severity • Your approach to management (consider psychological therapies, medications, options) • Follow up • Anything you would do differently re NICE guidance? • What further questions, learning needs or challenges does this patient highlight for you?