Depression and PTSD Treatments Improve HIV Treatment Outcome





















- Slides: 60
Depression and PTSD Treatments Improve HIV Treatment Outcome Eric Avery, MD Assistant Clinical Professor of Psychiatry Director, HIV Psychiatry Services The University of Texas Medical Branch Galveston, Texas
Objectives 1. To understand the relationship between the increasing prevalence of psychiatric disorders in HIV patients and the changing epidemiology of the epidemic. 2. To review Depression and Post Traumatic Stress Disorder (PTSD): Prevalence Diagnosis Impact on adherance and mortality Treatment of Depression and PTSD 3. To review HIV and psychiatric drug/drug interactions.
HIV is a Psychiatric Epidemic • Psychiatric illness increases risk for HIV. • HIV increases risk for psychiatric illness. • Effective treatment for psychiatric illness can improve patient outcome. • Effective treatment for psychiatric can decrease HIV transmission.
Psychiatric Illness Increases Risk of HIV Infection • Substance Abuse. • Mood Disorders (Major Depression, Bipolor D/O) • Post Traumatic Stress Disorder (PTSD) • Psychotic Disorders • Impulsive behavior and personality factors
HIV Increases Risk for Psychiatric Illness • Increased major depression. • Increased mania. • HIV dementia (AIDS Dementia Complex). • Increased psychosocial stressors.

Depression 1. Prevalence 2. Diagnosis 3. Impact on ARV Treatment: • Initiation • Discontinuation • Adherance 4. Impact on HIV Mortality 5. Treatment of Depression
100 Patients with HIV How many are depressed?

Depressed Mood and HIV: Name the 11 types: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Why is the diagnosis important?

Differential Diagnosis of Depressed Moods in HIV Patients • Despondency/demoralization. • Dysthymia (chronic low mood). • Adjustment disorder/minor depression. • Major depression, recurrent major depression. • General anxiety disorder. • Bipolar disorder -- depressed phase. • Organic mood disorder “secondary depression” (infections, medication sideeffects, and mass lesions of CNS). • Malnourishment/weight loss associated with HIV. • Sleep disorder. • Psychoactive substance abuse. • Bereavement.
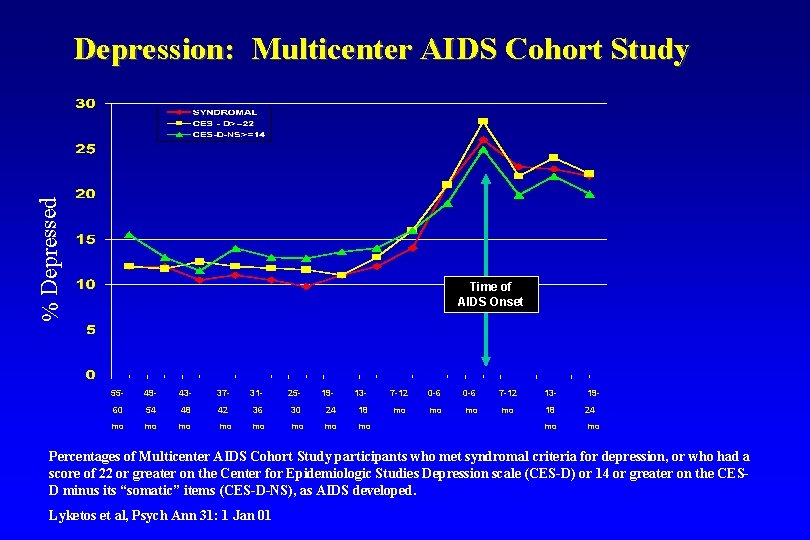
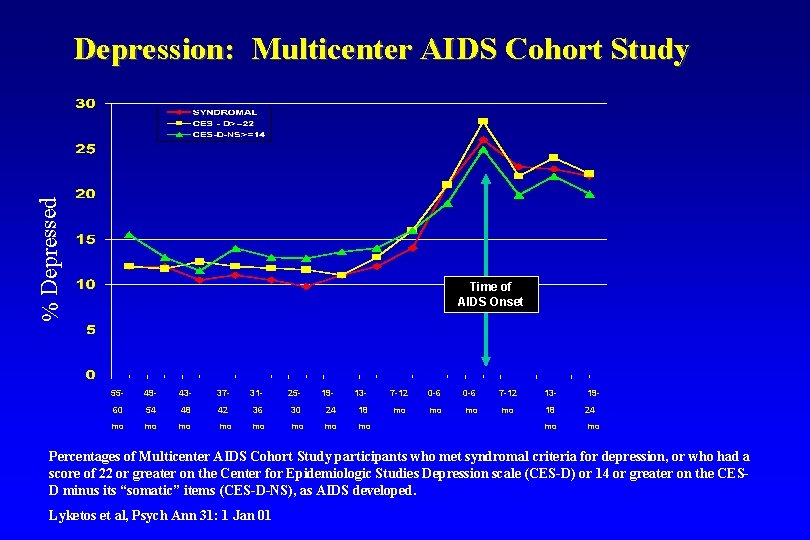
% Depressed Depression: Multicenter AIDS Cohort Study Time of AIDS Onset 55 - 49 - 43 - 37 - 31 - 25 - 19 - 13 - 7 -12 0 -6 7 -12 13 - 19 - 60 54 48 42 36 30 24 18 mo mo 18 24 mo mo mo Percentages of Multicenter AIDS Cohort Study participants who met syndromal criteria for depression, or who had a score of 22 or greater on the Center for Epidemiologic Studies Depression scale (CES-D) or 14 or greater on the CESD minus its “somatic” items (CES-D-NS), as AIDS developed. Lyketos et al, Psych Ann 31: 1 Jan 01
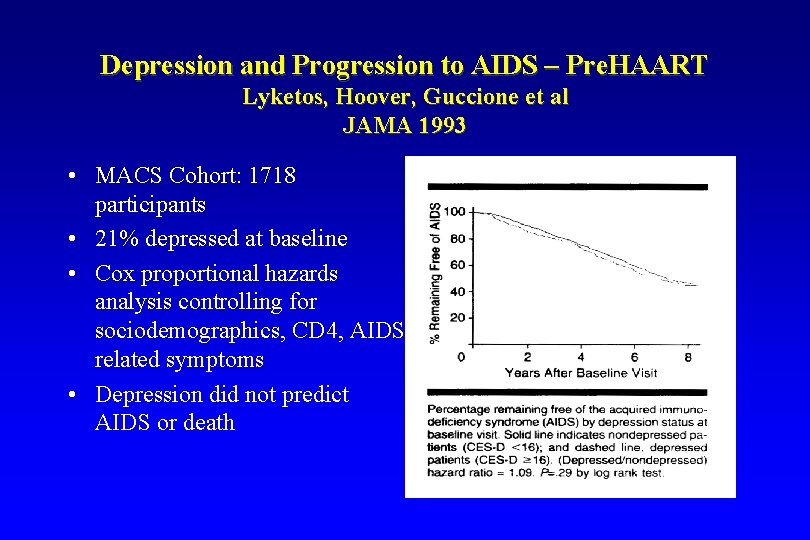
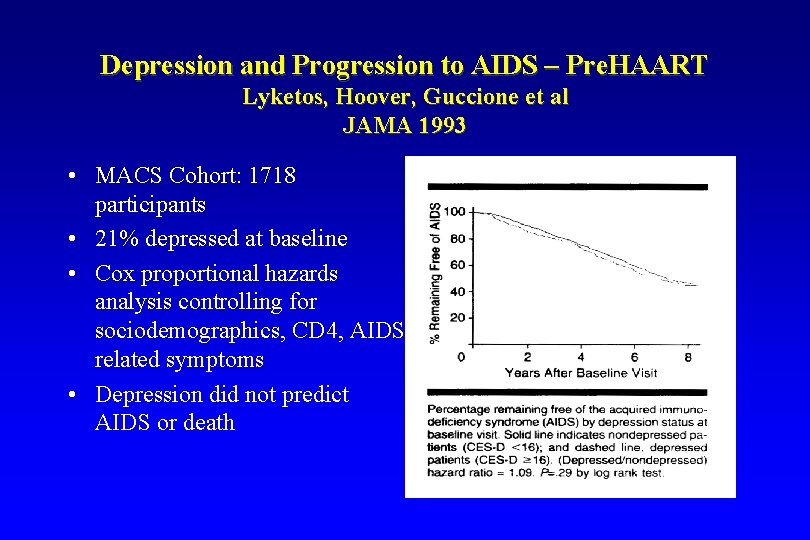
Depression and Progression to AIDS – Pre. HAART Lyketos, Hoover, Guccione et al JAMA 1993 • MACS Cohort: 1718 participants • 21% depressed at baseline • Cox proportional hazards analysis controlling for sociodemographics, CD 4, AIDS related symptoms • Depression did not predict AIDS or death
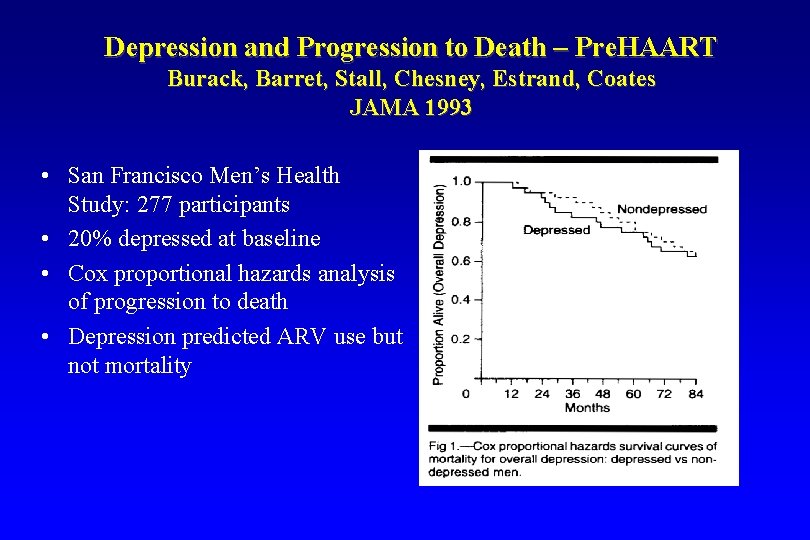
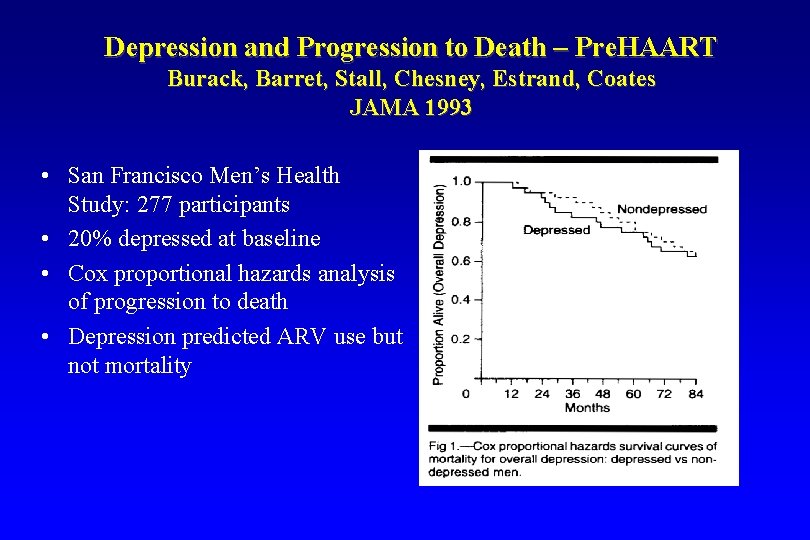
Depression and Progression to Death – Pre. HAART Burack, Barret, Stall, Chesney, Estrand, Coates JAMA 1993 • San Francisco Men’s Health Study: 277 participants • 20% depressed at baseline • Cox proportional hazards analysis of progression to death • Depression predicted ARV use but not mortality

Depression and Progression to AIDS – Pre. HAART Mayne, Vittinghoff, Chesney, Barrett, Coates Arch Int Med 1996 • • • SF Men’s Cohort: 1032 participants over 102 months Cox proportional hazards with time dependent variables 58% had significant depressive symptoms (CES-D) Longitudinal measurement of depression every 6 months Predictors of Mortality – CD 4 cell count – B 2 microglobulin – P 24 antigen – WHO HIV stage – Depression (RR=1. 67 P<0. 05)
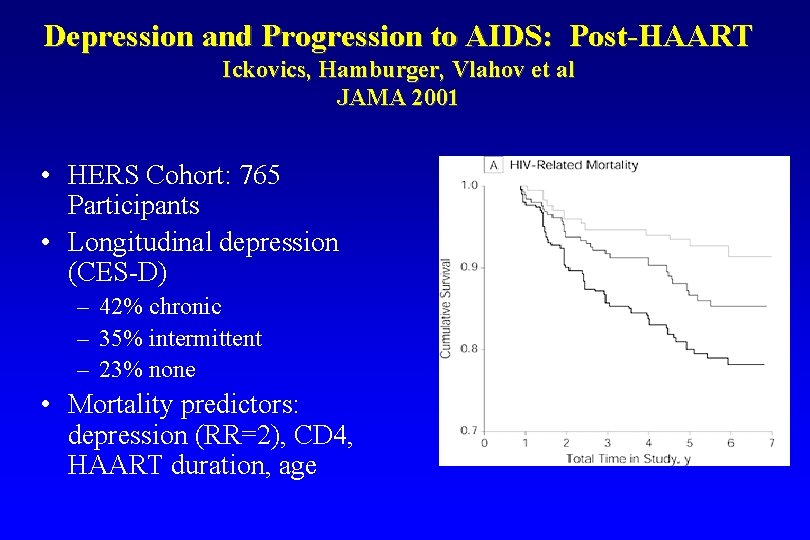
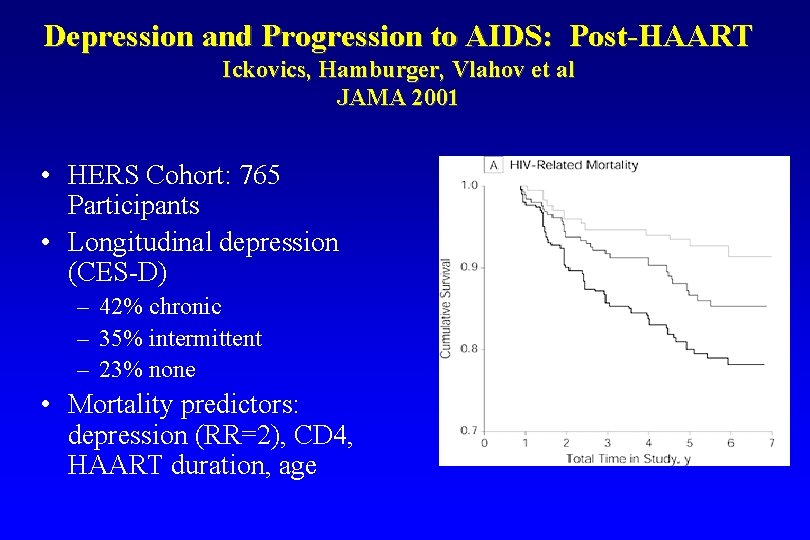
Depression and Progression to AIDS: Post-HAART Ickovics, Hamburger, Vlahov et al JAMA 2001 • HERS Cohort: 765 Participants • Longitudinal depression (CES-D) – 42% chronic – 35% intermittent – 23% none • Mortality predictors: depression (RR=2), CD 4, HAART duration, age
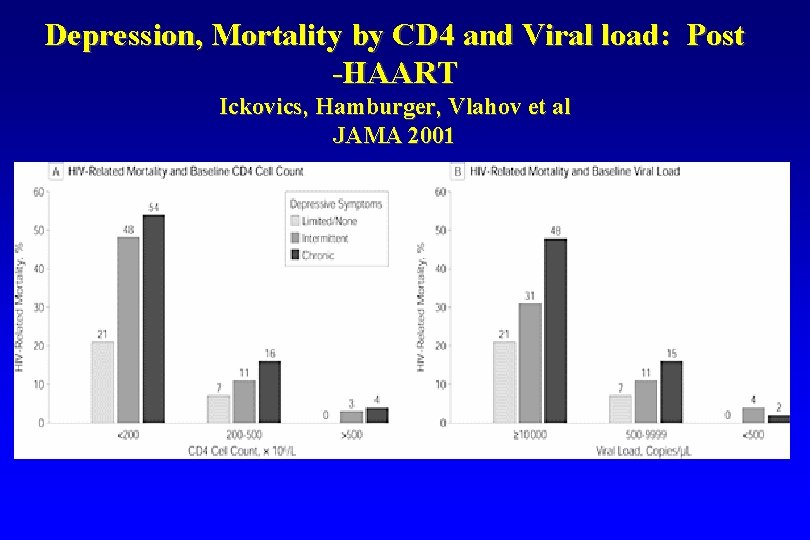
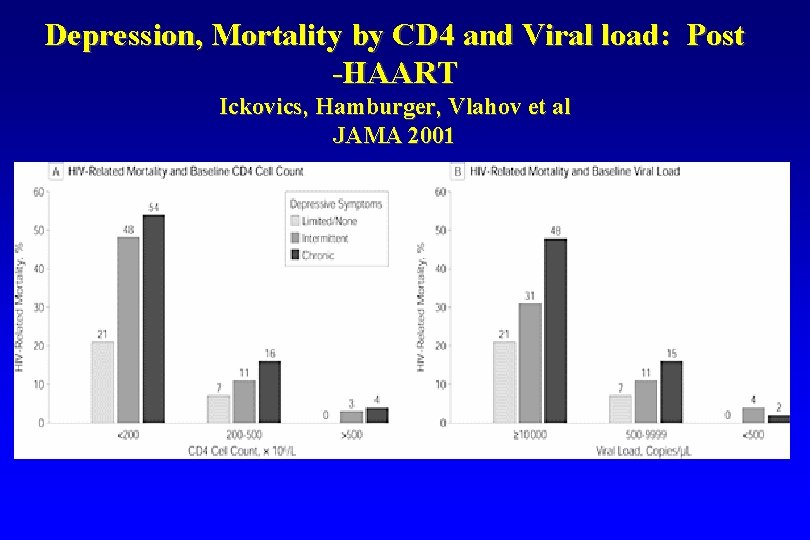
Depression, Mortality by CD 4 and Viral load: Post -HAART Ickovics, Hamburger, Vlahov et al JAMA 2001

Why Does Depression Speed Progression to AIDS and Death? • Stress alters cellular and humoral immune response • • • Kieclot-Glaser Proc Nat Acad Sci 1996 Vedhara Lancet 1999 Glaser Psychosom Med 1992 Jabaaij J Psychosom Res 1993 Glaser Ann NY Acad Sci 1998 Azciati Psychosomatics 2001 • Delay in HAART initiation • Early HAART Discontinuation • Sub-optimal adherence to HAART
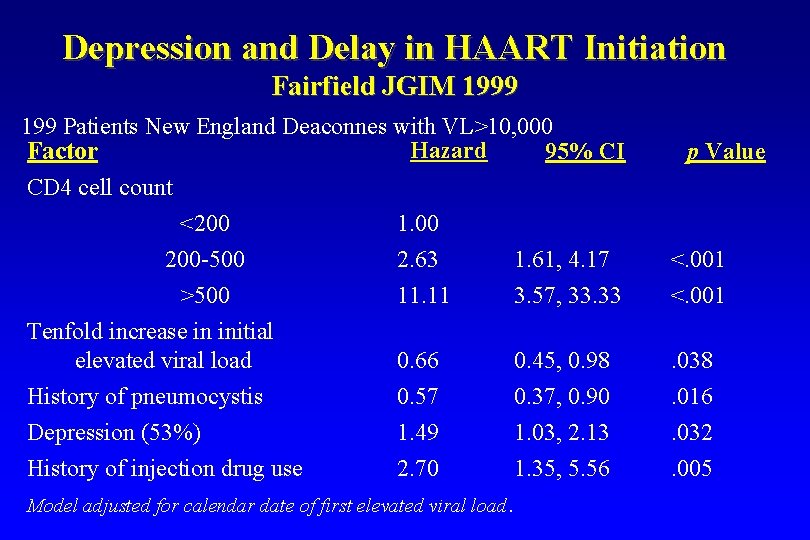
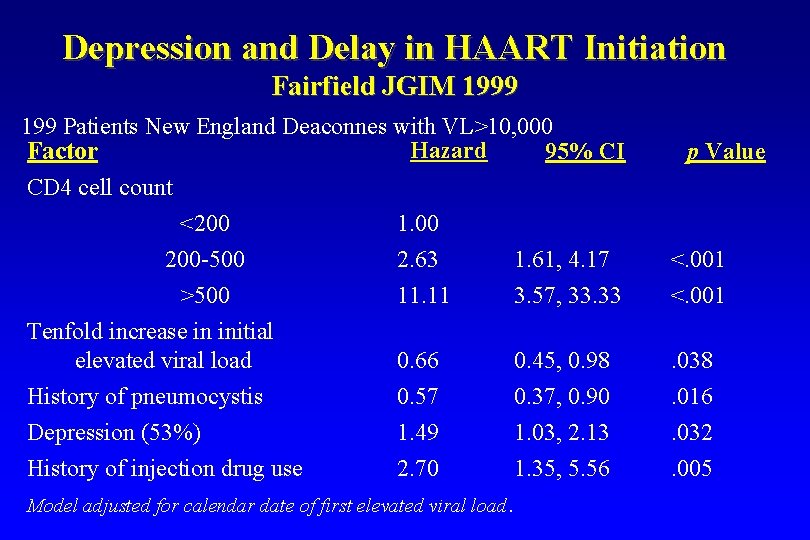
Depression and Delay in HAART Initiation Fairfield JGIM 1999 199 Patients New England Deaconnes with VL>10, 000 Hazard Factor 95% CI p Value CD 4 cell count <200 200 -500 >500 Tenfold increase in initial elevated viral load History of pneumocystis 1. 00 2. 63 11. 11 1. 61, 4. 17 3. 57, 33. 33 <. 001 0. 66 0. 57 0. 45, 0. 98 0. 37, 0. 90 . 038. 016 Depression (53%) 1. 49 1. 03, 2. 13 . 032 History of injection drug use 2. 70 1. 35, 5. 56 Model adjusted for calendar date of first elevated viral load. . 005
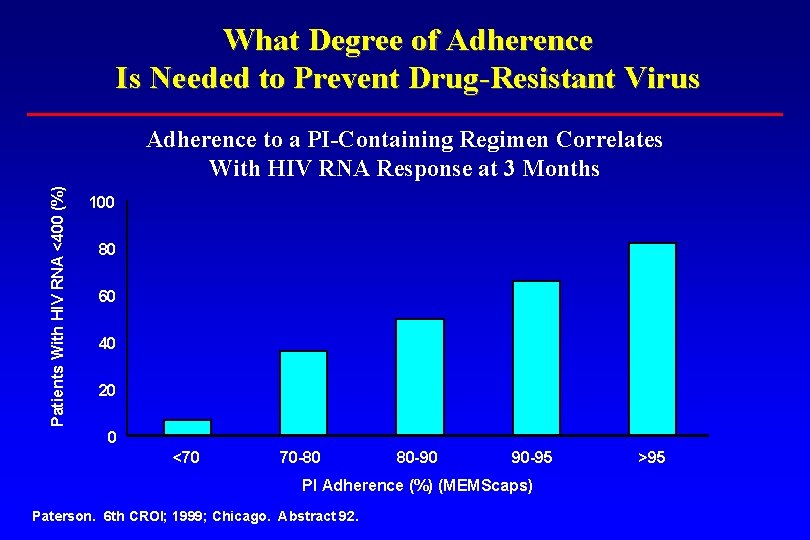
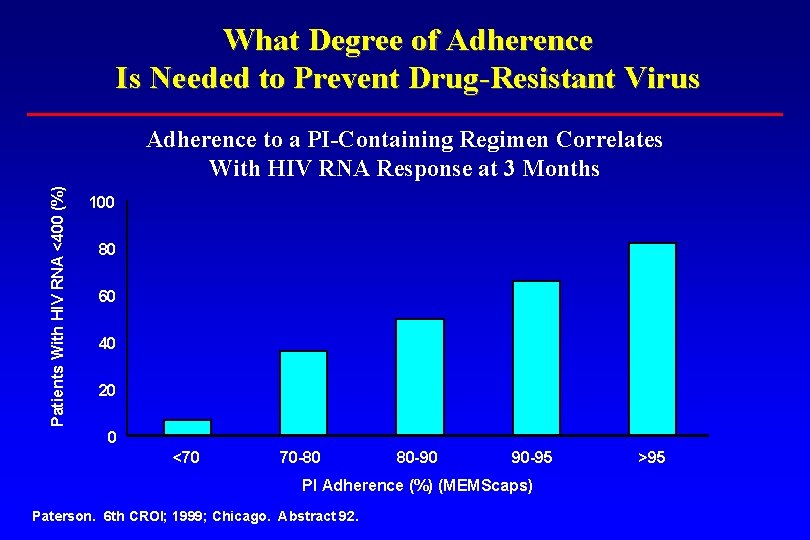
What Degree of Adherence Is Needed to Prevent Drug-Resistant Virus Patients With HIV RNA <400 (%) Adherence to a PI-Containing Regimen Correlates With HIV RNA Response at 3 Months 100 80 60 40 20 0 <70 70 -80 80 -90 90 -95 PI Adherence (%) (MEMScaps) Paterson. 6 th CROI; 1999; Chicago. Abstract 92. >95

Depression Predicts Adherence to Non-HIV Treatment Amiodarone Irvine Psychosom Med 1999 General medicine Botelho J Fam Pract 1992 Aspirin for angina Carney Behavioral Med 1998 Renal diet De-Nour Transplantation 1993 ESRD Diet Katz Psychol Reports 1998 ESRD Diet Schnieder Health psychol 1991 ESRD Medical Regimen Brownbridge Ped Neph 1994 Cyclosporine Renal Transplant Kiley Transplantation 1993 Cyclosporine Renal Transplant Rodriguez Trans Proc 1991 Rheum arthritis treatment plan Taal Pt Ed Counsel 1992 Oral cytoxan Lebovits Cancer 1990 Asthma Cochrane Drugs 1996

Depression and HIV Medication Adherence • • • Singh AIDS Care 1996 Holzmer AIDS Patient Care STDs 1999 Peterson Annals Int Med 2000 Schulz 38 th ICAAC 1998 Bangsberg #1721 41 st ICAAC 2001
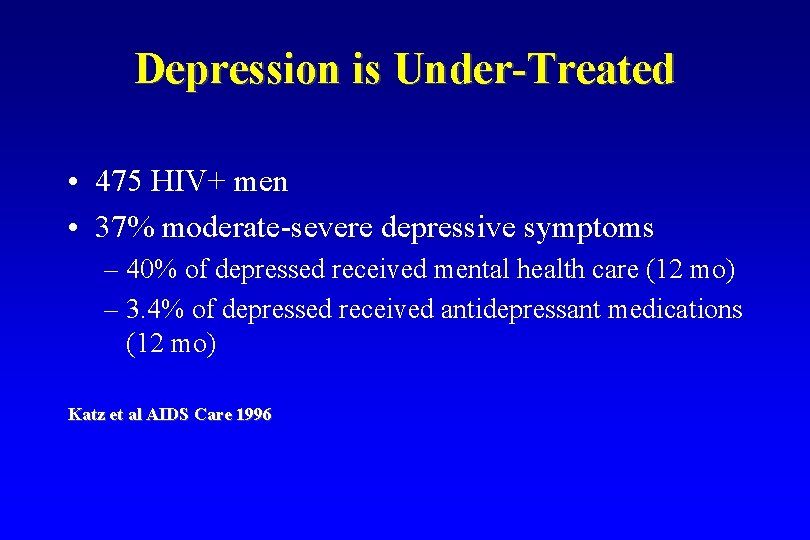
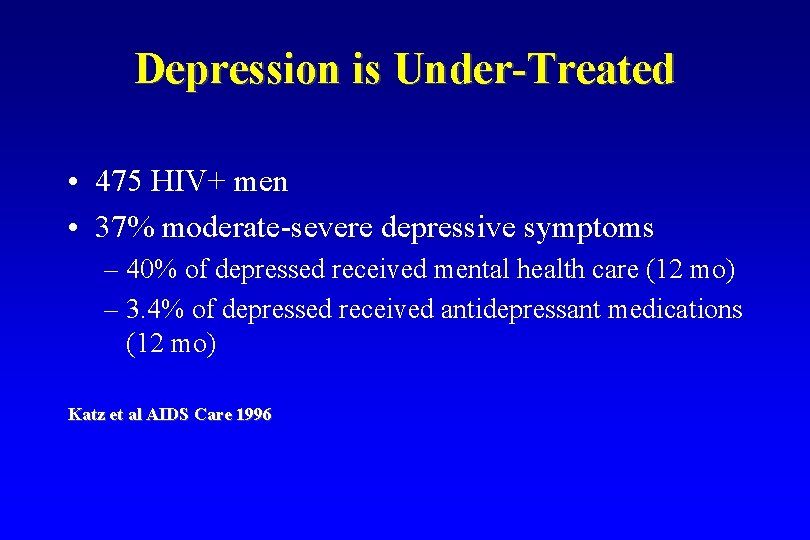
Depression is Under-Treated • 475 HIV+ men • 37% moderate-severe depressive symptoms – 40% of depressed received mental health care (12 mo) – 3. 4% of depressed received antidepressant medications (12 mo) Katz et al AIDS Care 1996

Depression: Diagnosis
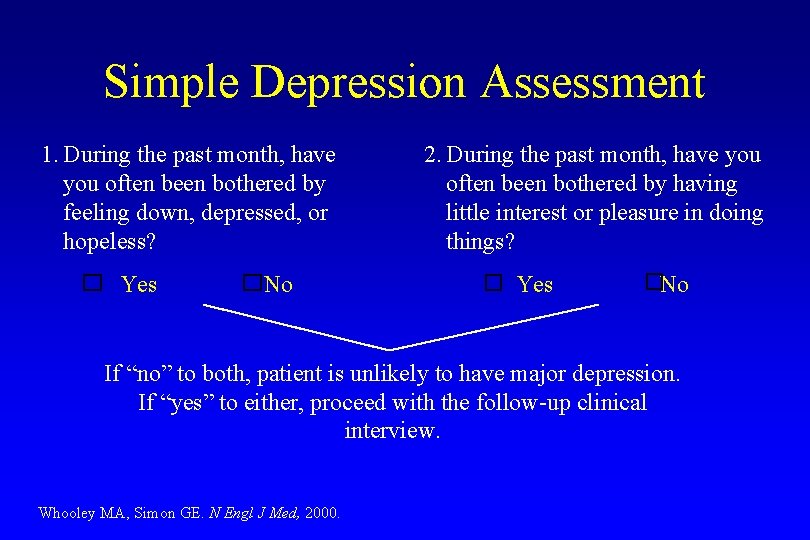
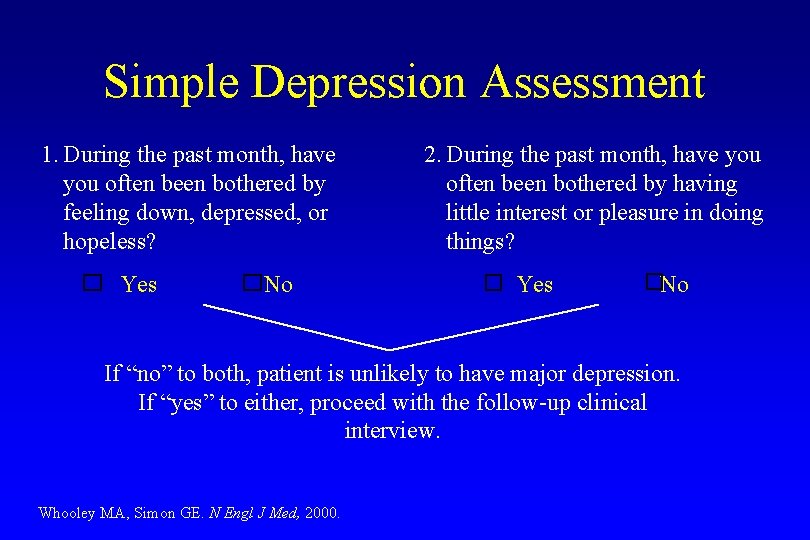
Simple Depression Assessment 1. During the past month, have you often been bothered by feeling down, depressed, or hopeless? Yes No 2. During the past month, have you often been bothered by having little interest or pleasure in doing things? Yes No If “no” to both, patient is unlikely to have major depression. If “yes” to either, proceed with the follow-up clinical interview. Whooley MA, Simon GE. N Engl J Med, 2000.
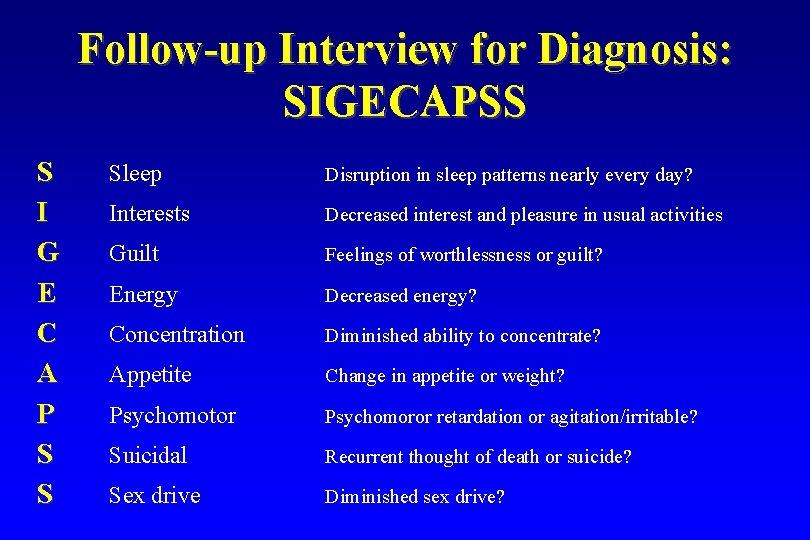
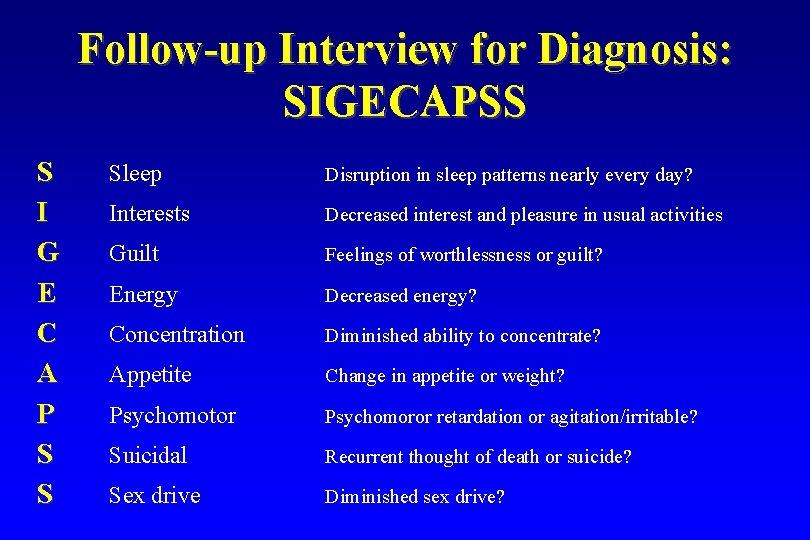
Follow-up Interview for Diagnosis: SIGECAPSS S I G E C A P S S Sleep Disruption in sleep patterns nearly every day? Interests Decreased interest and pleasure in usual activities Guilt Feelings of worthlessness or guilt? Energy Decreased energy? Concentration Diminished ability to concentrate? Appetite Change in appetite or weight? Psychomotor Psychomoror retardation or agitation/irritable? Suicidal Recurrent thought of death or suicide? Sex drive Diminished sex drive?
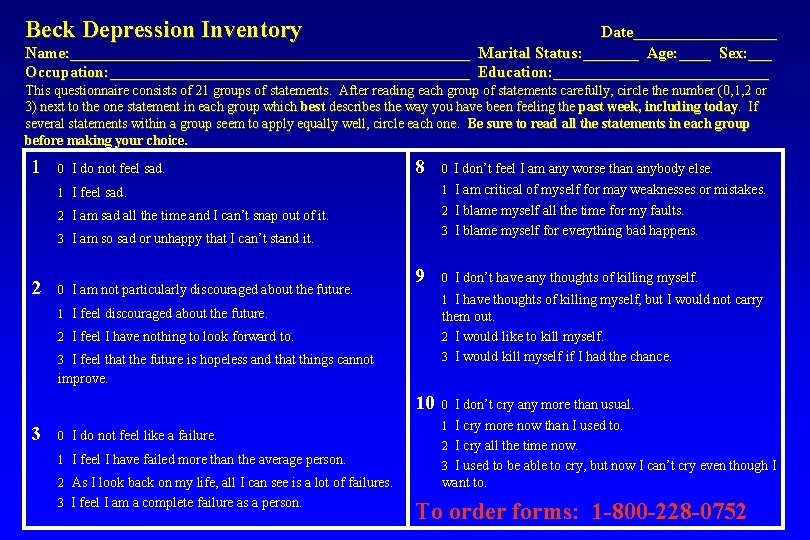
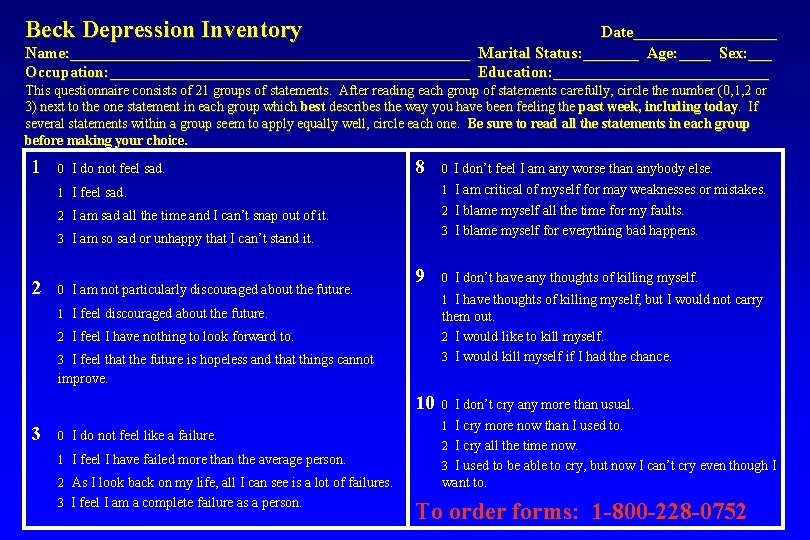
Beck Depression Inventory Date_________ Name: _________________________ Marital Status: _______ Age: ____ Sex: ___ Occupation: _______________________ Education: ______________ This questionnaire consists of 21 groups of statements. After reading each group of statements carefully, circle the number (0, 1, 2 or 3) next to the one statement in each group which best describes the way you have been feeling the past week, including today. If several statements within a group seem to apply equally well, circle each one. Be sure to read all the statements in each group before making your choice. 1 0 I do not feel sad. 8 1 I feel sad. 1 I am critical of myself for may weaknesses or mistakes. 2 I am sad all the time and I can’t snap out of it. 2 I blame myself all the time for my faults. 3 I blame myself for everything bad happens. 3 I am so sad or unhappy that I can’t stand it. 2 0 I don’t feel I am any worse than anybody else. 0 I am not particularly discouraged about the future. 9 0 I don’t have any thoughts of killing myself. 1 I have thoughts of killing myself, but I would not carry 1 I feel discouraged about the future. them out. 2 I would like to kill myself. 3 I would kill myself if I had the chance. 2 I feel I have nothing to look forward to. 3 I feel that the future is hopeless and that things cannot improve. 10 3 0 I do not feel like a failure. 1 I feel I have failed more than the average person. 2 As I look back on my life, all I can see is a lot of failures. 3 I feel I am a complete failure as a person. 0 I don’t cry any more than usual. 1 I cry more now than I used to. 2 I cry all the time now. 3 I used to be able to cry, but now I can’t cry even though I want to. To order forms: 1 -800 -228 -0752
Depression: Treatment
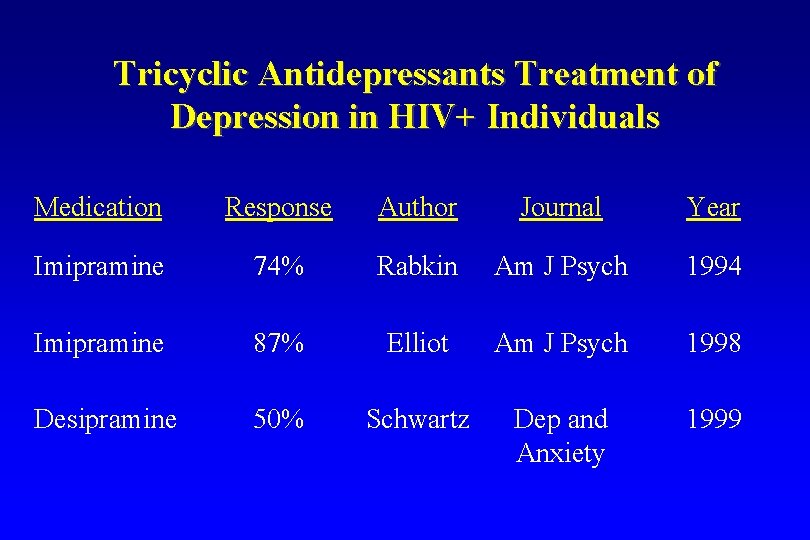
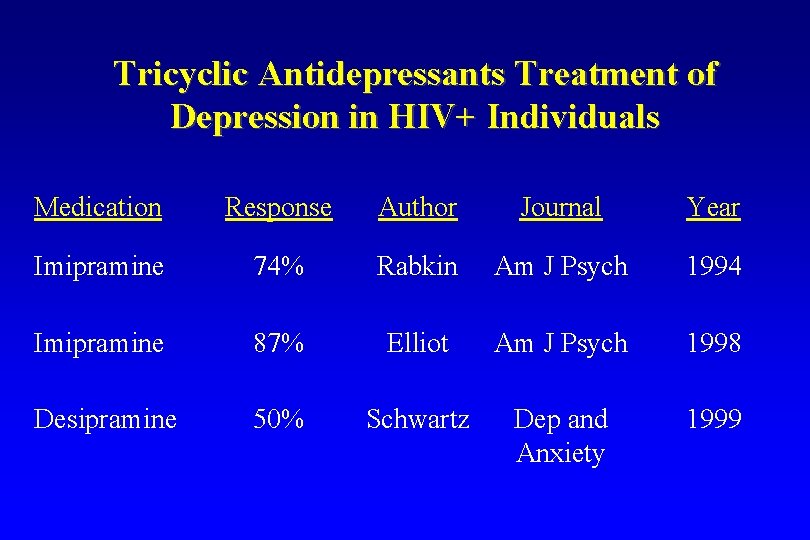
Tricyclic Antidepressants Treatment of Depression in HIV+ Individuals Medication Response Author Journal Year Imipramine 74% Rabkin Am J Psych 1994 Imipramine 87% Elliot Am J Psych 1998 Desipramine 50% Schwartz Dep and Anxiety 1999
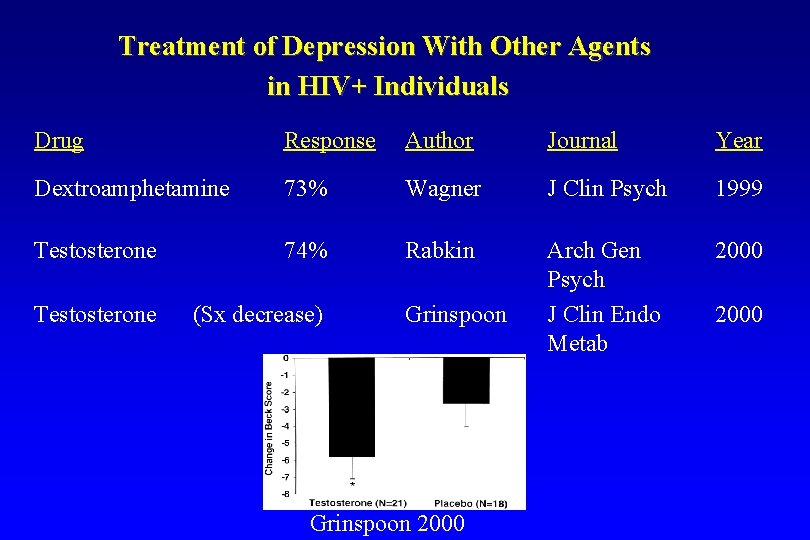
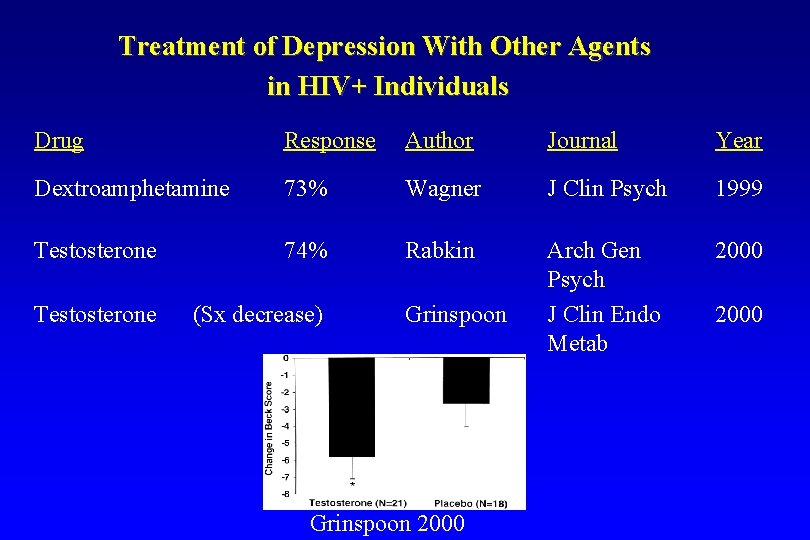
Treatment of Depression With Other Agents in HIV+ Individuals Drug Response Author Journal Year Dextroamphetamine 73% Wagner J Clin Psych 1999 Testosterone 74% Rabkin Arch Gen Psych J Clin Endo Metab 2000 Testosterone (Sx decrease) Grinspoon 2000

SSRI Treatment of Depression in HIV+ Individuals Medication Response Author Journal Year Fluoxetine 83% Rabkin J Clin Psych 1994 Fluoxetine 64% Zisook J Clin Psych 1998 Fluoxetine 67% Elliot Am J Psych 1998 Fluoxetine 90% Ferrando Gen Hosp Psych 1997 Fluoxetine 75% Schwartz Dep and Anxiety 1999 Fluoxetine/ Sertraline 78% Ferrando J Clin Psych 1999 Sertraline 86% Ferrando Gen Hosp Psyh 1997 Nefazodone 73% Elliot J Clin Psych 1999 Paroxetine 86% Ferrando Gen Hosp Psych 1997

Side Effect/Toxicity Profile TCA vs SSRI TCA SSRI • Narrow therapeutic window • Mild side effects – Requires drug monitoring • Anticholinergic effects – Dry mouth, Constipation, dizziness, hypotension – 41% discontinue at 6 months • (Rabkin Amer J Psych 1994) • Pill burden – Anticholinergic, agitation/sedation, sexual dysfunction • Drug interactions (Rx + ritonavir) • Bupropion - seizures
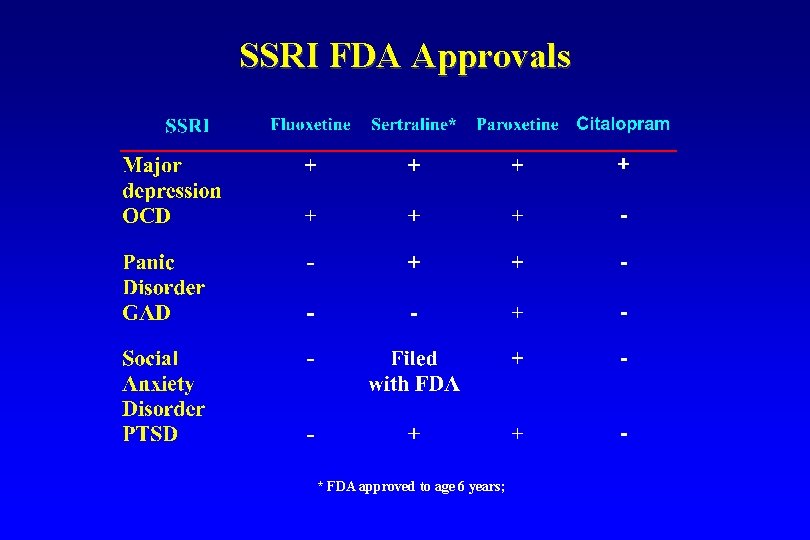
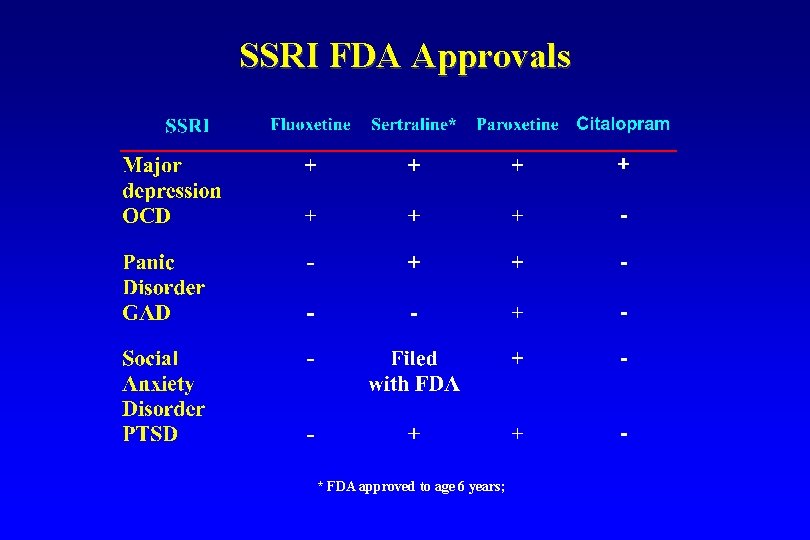
SSRI FDA Approvals * FDA approved to age 6 years;
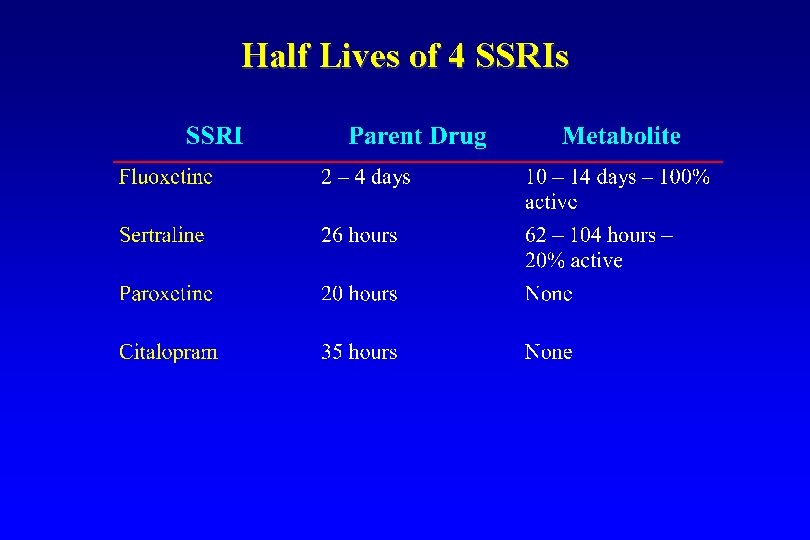
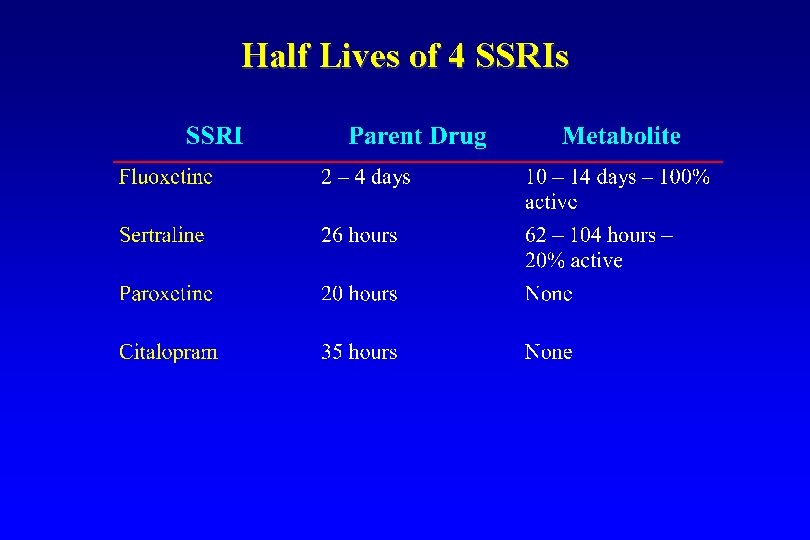
Half Lives of 4 SSRIs
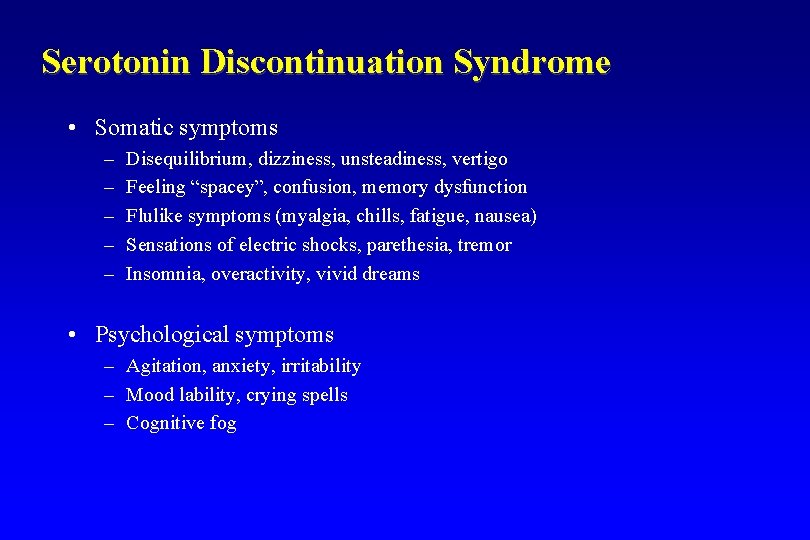
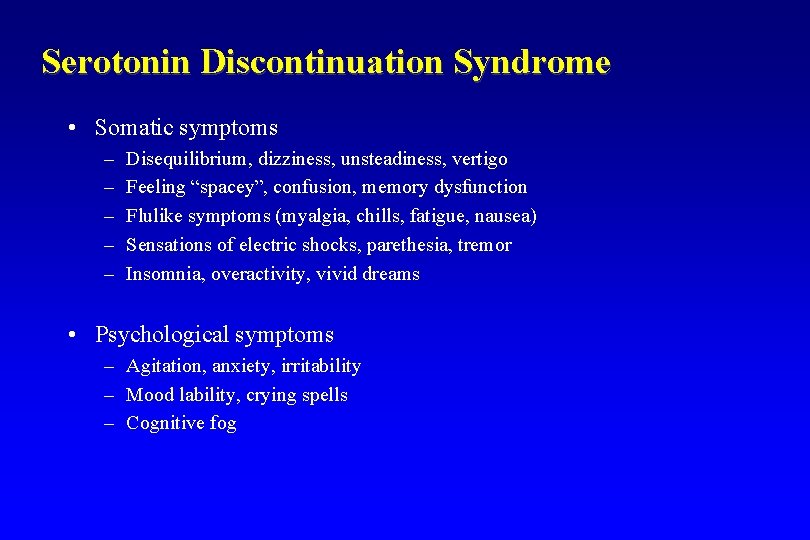
Serotonin Discontinuation Syndrome • Somatic symptoms – – – Disequilibrium, dizziness, unsteadiness, vertigo Feeling “spacey”, confusion, memory dysfunction Flulike symptoms (myalgia, chills, fatigue, nausea) Sensations of electric shocks, parethesia, tremor Insomnia, overactivity, vivid dreams • Psychological symptoms – Agitation, anxiety, irritability – Mood lability, crying spells – Cognitive fog

Hepatic Isoenzyme Inhibition of the SSRIs (Cytochrome P 450)
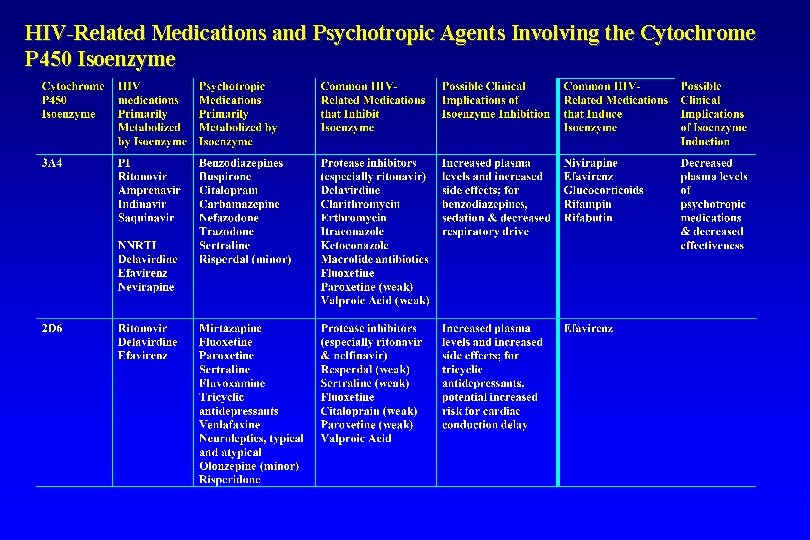
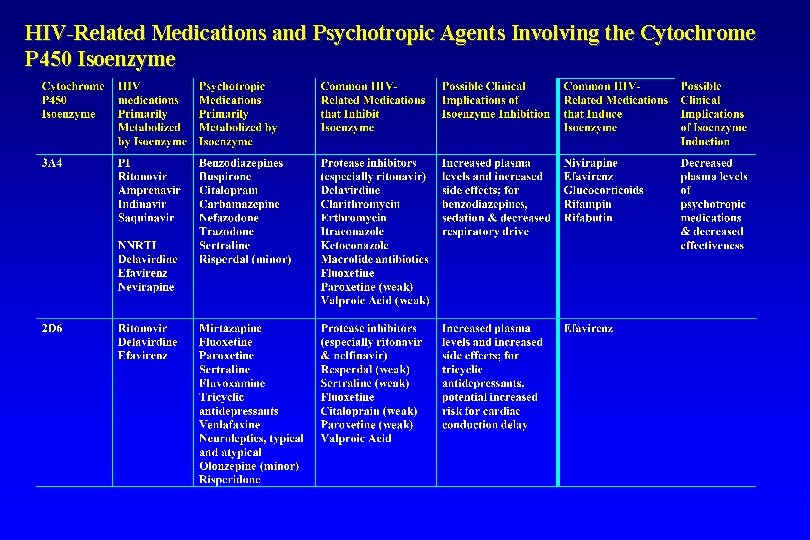
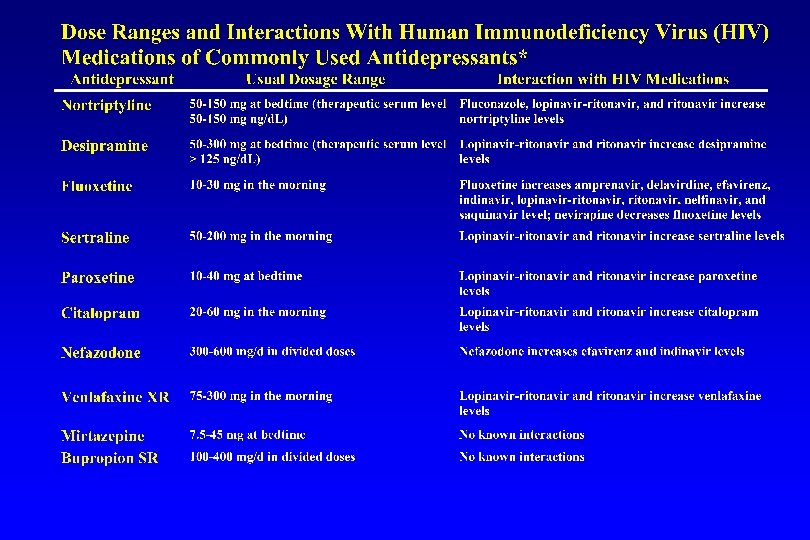
HIV-Related Medications and Psychotropic Agents Involving the Cytochrome P 450 Isoenzyme
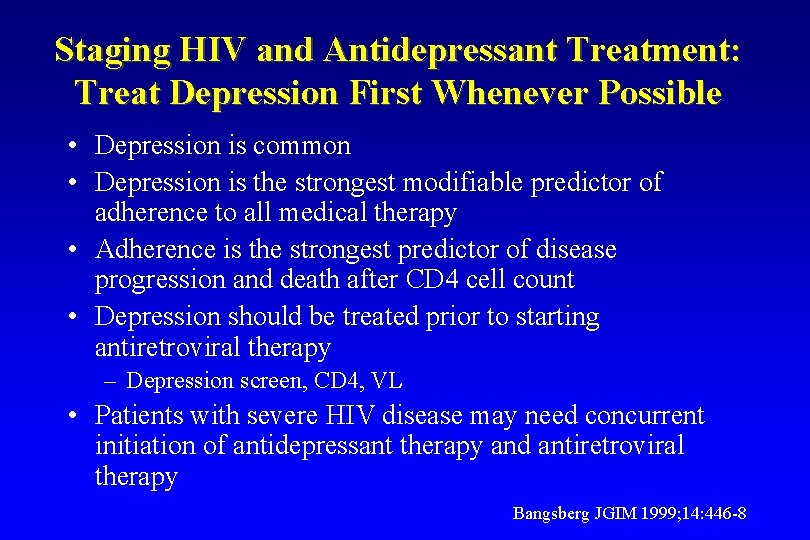
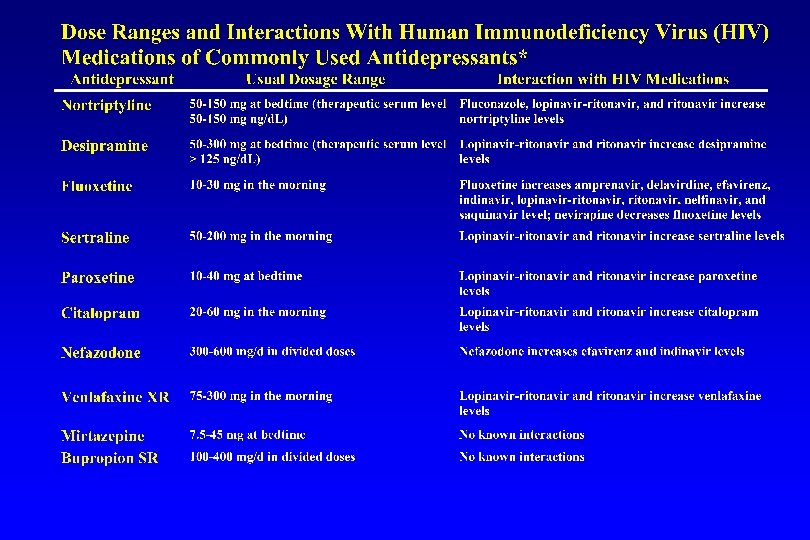
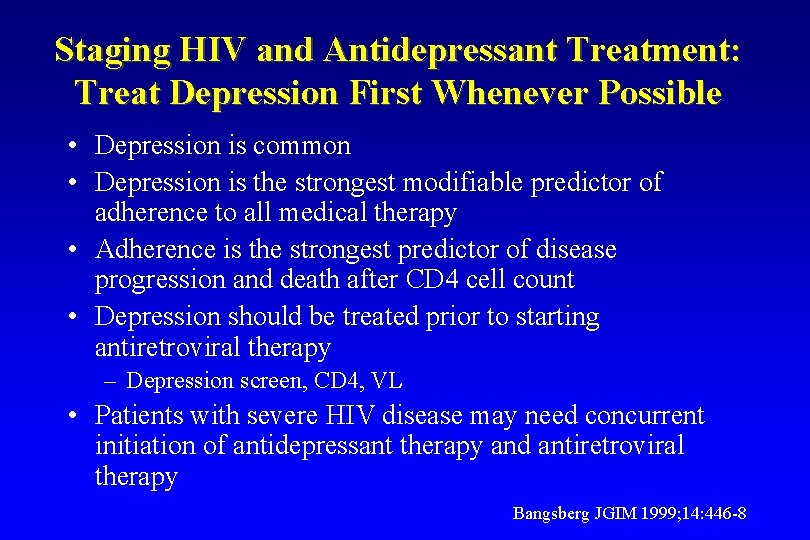
Staging HIV and Antidepressant Treatment: Treat Depression First Whenever Possible • Depression is common • Depression is the strongest modifiable predictor of adherence to all medical therapy • Adherence is the strongest predictor of disease progression and death after CD 4 cell count • Depression should be treated prior to starting antiretroviral therapy – Depression screen, CD 4, VL • Patients with severe HIV disease may need concurrent initiation of antidepressant therapy and antiretroviral therapy Bangsberg JGIM 1999; 14: 446 -8
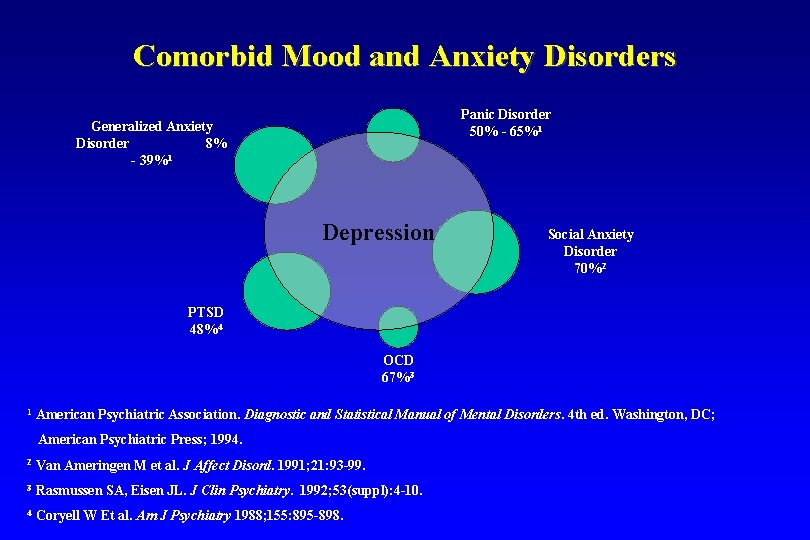
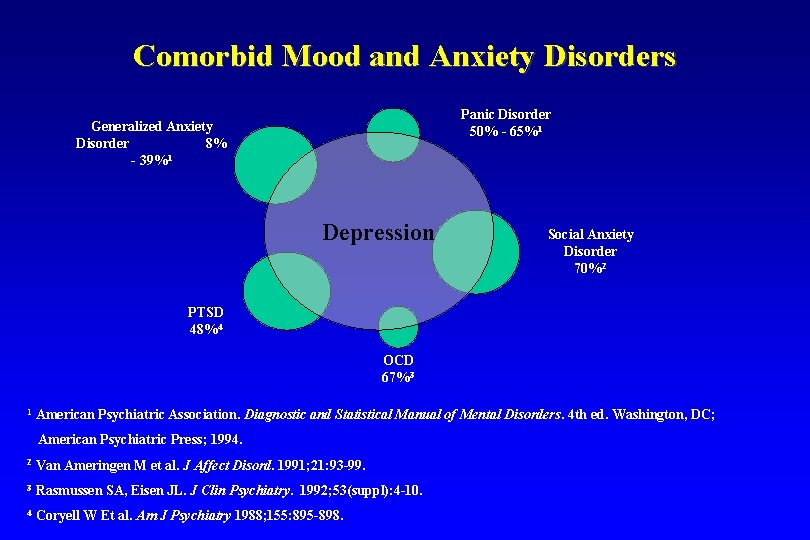
Comorbid Mood and Anxiety Disorders Panic Disorder 50% - 65%1 Generalized Anxiety Disorder 8% - 39%1 Depression Social Anxiety Disorder 70%2 PTSD 48%4 OCD 67%3 1 American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4 th ed. Washington, DC; American Psychiatric Press; 1994. 2 Van Ameringen M et al. J Affect Disord. 1991; 21: 93 -99. 3 Rasmussen SA, Eisen JL. J Clin Psychiatry. 1992; 53(suppl): 4 -10. 4 Coryell W Et al. Am J Psychiatry 1988; 155: 895 -898.

Post Traumatic Stress Disorder • Prevalence • Childhood abuse, PTSD and HIV risk behaviors • Proposed association between PTSD and HIV treatment nonadherance • Treatment of PTSD

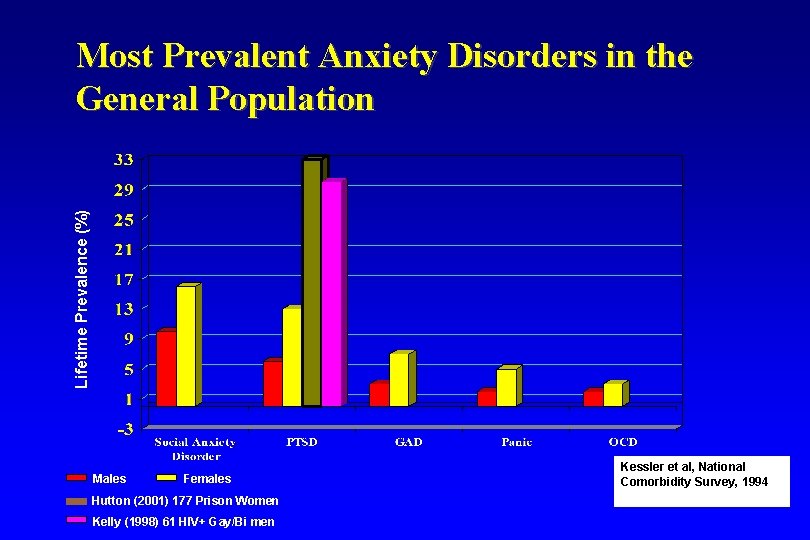
PTSD Prevalence • Over half the U. S. population has been exposed to a severe trauma • 10 -20% of trauma survivors will develop PTSD • Lifetime prevalence 8% overall. 12% in women (Kessler 1995) – Increased rates in HIV +, incarcerated – Limited studies: • HIV + 30% (1/3 after HIV dx) (Kelly 1998) • Incarcerated women lifetime 33%, current 15 -22% (Hutton 2001) • PTSD is the 5 th most prevalent major psychiatric illness
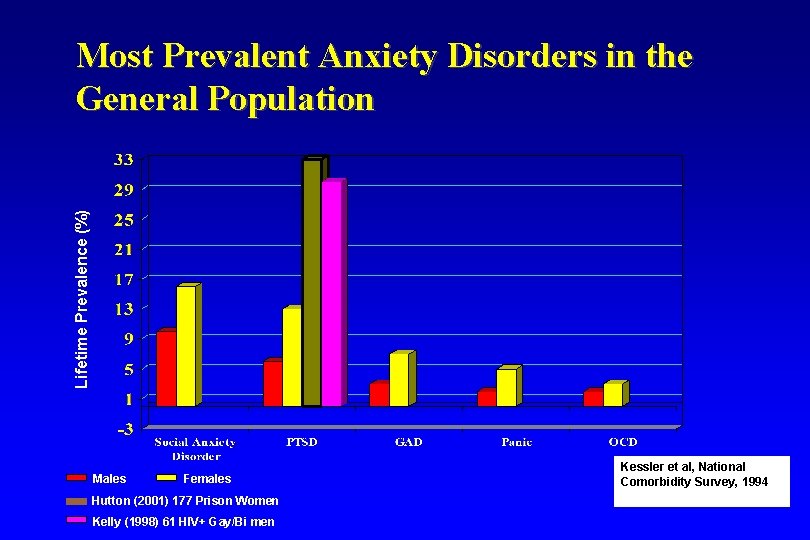
Lifetime Prevalence (%) Most Prevalent Anxiety Disorders in the General Population Males Females Hutton (2001) 177 Prison Women Kelly (1998) 61 HIV+ Gay/Bi men Kessler et al, National Comorbidity Survey, 1994

Comorbidity • Comorbid psychiatric illness is about 80% • Patients with PTSD are 2 - 4 X more likely to have depression, anxiety disorders or substance abuse • They are 90 X more likely to have a somatization disorder

Common Traumatic Events • Witnessing injury/death • Sexual molestation/rape • Natural disaster/fire • Physical attack or abuse/threatened with a weapon • Life threatening accident • Combat
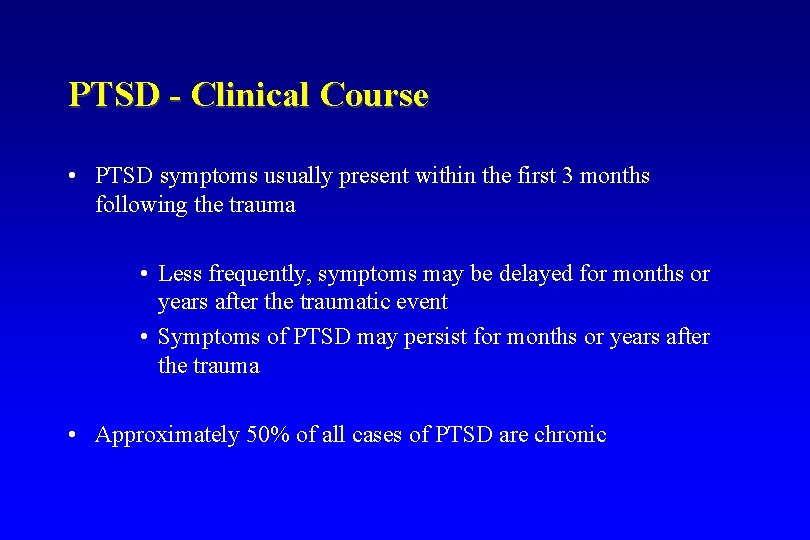
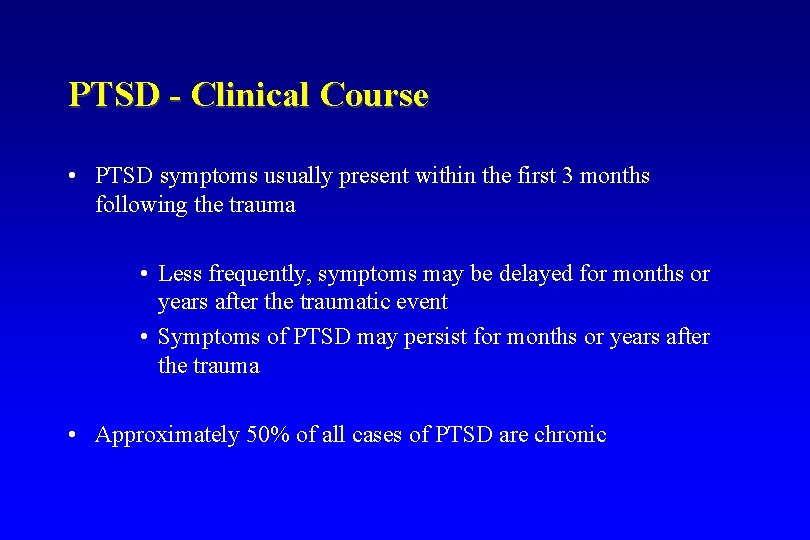
PTSD - Clinical Course • PTSD symptoms usually present within the first 3 months following the trauma • Less frequently, symptoms may be delayed for months or years after the traumatic event • Symptoms of PTSD may persist for months or years after the trauma • Approximately 50% of all cases of PTSD are chronic
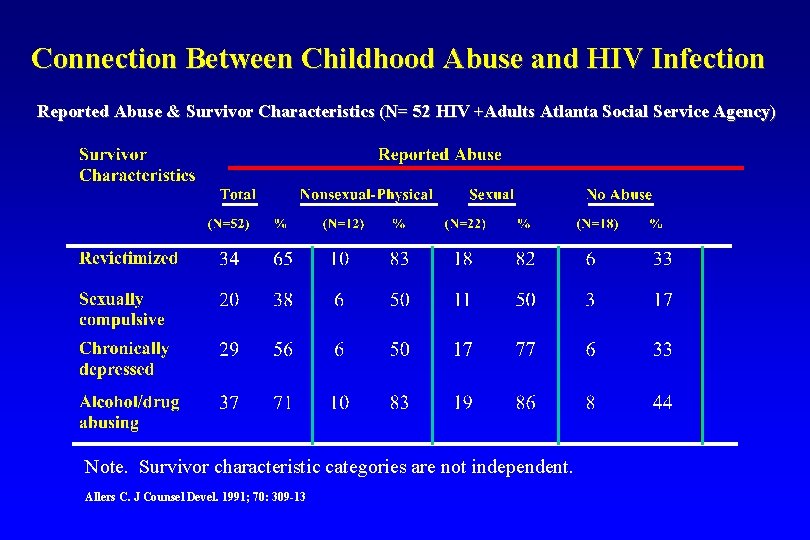
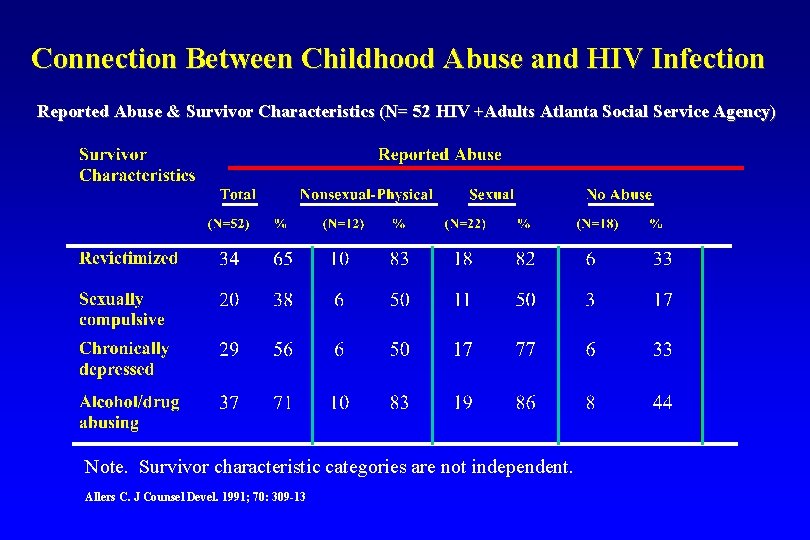
Connection Between Childhood Abuse and HIV Infection Reported Abuse & Survivor Characteristics (N= 52 HIV +Adults Atlanta Social Service Agency) Note. Survivor characteristic categories are not independent. Allers C. J Counsel Devel. 1991; 70: 309 -13

Frequency of PTSD Disorders Among 177 Women Prisoners in an HIV Risk Behavior Study Compared with participants who did not have PTSD, those with lifetime diagnosis of PTSD were 71% more likely to have engaged in anal sex and 56% more likely to have engaged in prostitution. The association between lifetime PTSD and other HIV risk behaviors were not significant in this study. Hutton, Psych Services 2001, 52/4: 508 -13
PTSD Predicts Adherence to Non-HIV Treatment Survivors of Myocardial Infarction • 102 s/p MI • 10% PTSD (intrusion/avoidance) – significant association with decreased adherence Shemesh Gen. Hosp. Psych 2000

PTSD is Under-Treated 47 HIV+ women • 42% full, current PTSD – 59% not receiving mental health care • 22% partial PTSD – 78% not receiving mental health care Martinez AIDS Patient Care and STDs 2002
PTSD: Diagnosis
Screening questions • Have you ever had anything happen to you where you thought you would be seriously injured or might die? • Have you ever been in a life threatening accident? Fire? Disaster? • Have you ever been attacked or raped? • Have you ever seen these things happen to someone else?
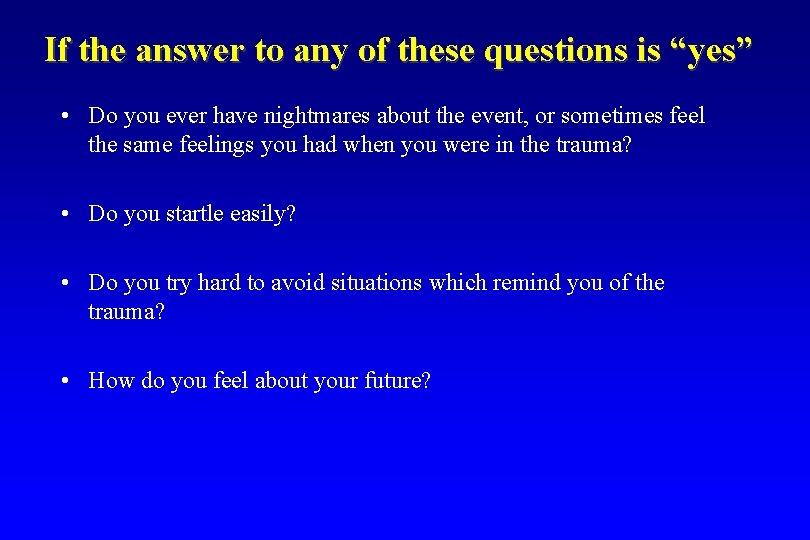
If the answer to any of these questions is “yes” • Do you ever have nightmares about the event, or sometimes feel the same feelings you had when you were in the trauma? • Do you startle easily? • Do you try hard to avoid situations which remind you of the trauma? • How do you feel about your future?
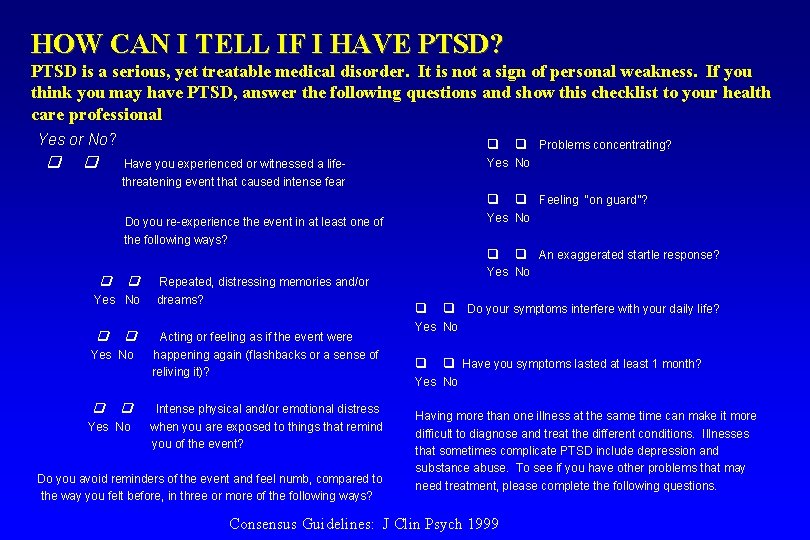
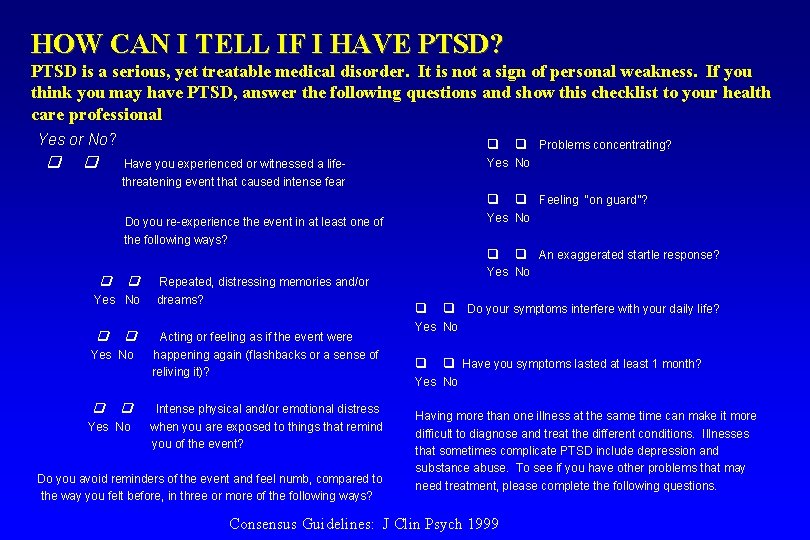
HOW CAN I TELL IF I HAVE PTSD? PTSD is a serious, yet treatable medical disorder. It is not a sign of personal weakness. If you think you may have PTSD, answer the following questions and show this checklist to your health care professional Yes or No? Problems concentrating? Yes No Have you experienced or witnessed a lifethreatening event that caused intense fear Yes No Do you re-experience the event in at least one of the following ways? Yes No Acting or feeling as if the event were happening again (flashbacks or a sense of reliving it)? Intense physical and/or emotional distress when you are exposed to things that remind you of the event? Do you avoid reminders of the event and feel numb, compared to the way you felt before, in three or more of the following ways? An exaggerated startle response? Yes No Repeated, distressing memories and/or dreams? Feeling “on guard”? Do your symptoms interfere with your daily life? Yes No Have you symptoms lasted at least 1 month? Yes No Having more than one illness at the same time can make it more difficult to diagnose and treat the different conditions. Illnesses that sometimes complicate PTSD include depression and substance abuse. To see if you have other problems that may need treatment, please complete the following questions. Consensus Guidelines: J Clin Psych 1999
PTSD: Treatment

Psychotherapeutic Interventions • Acute PTSD – mild: – severe: Psychotherapy Psycho therapy and medication • Chronic PTSD – mild: – severe: Psychotherapy first or + medication If comorbid (eg: depression / bipolor / other anxiety DO) – medication plus psychotherapy • Most effective: cognitive behavioral therapy (CBT) and exposure therapy • Patients are encouraged to confront anxiety provoking triggers, decrease avoidance, and practice stress reducing strategies • When referring patients, seek therapists with expertise in CBT and BT Consensus Guidelines J. Clin. Psychiatry 1999
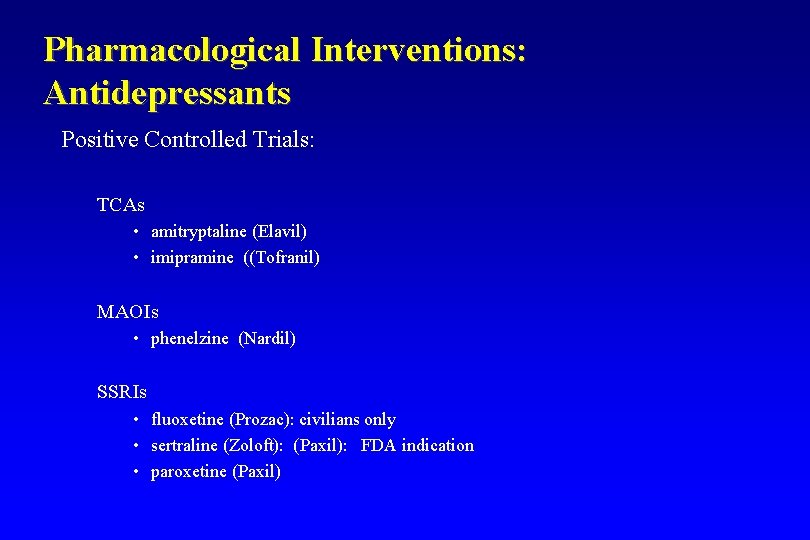
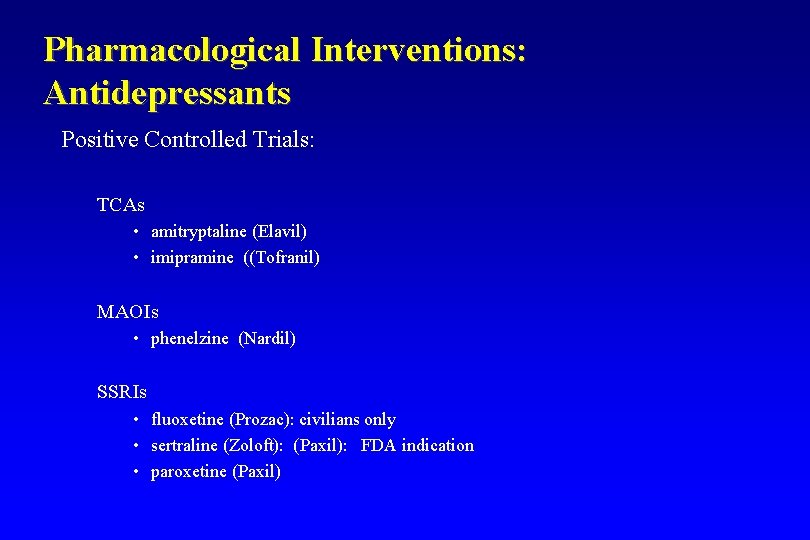
Pharmacological Interventions: Antidepressants Positive Controlled Trials: TCAs • amitryptaline (Elavil) • imipramine ((Tofranil) MAOIs • phenelzine (Nardil) SSRIs • fluoxetine (Prozac): civilians only • sertraline (Zoloft): (Paxil): FDA indication • paroxetine (Paxil)
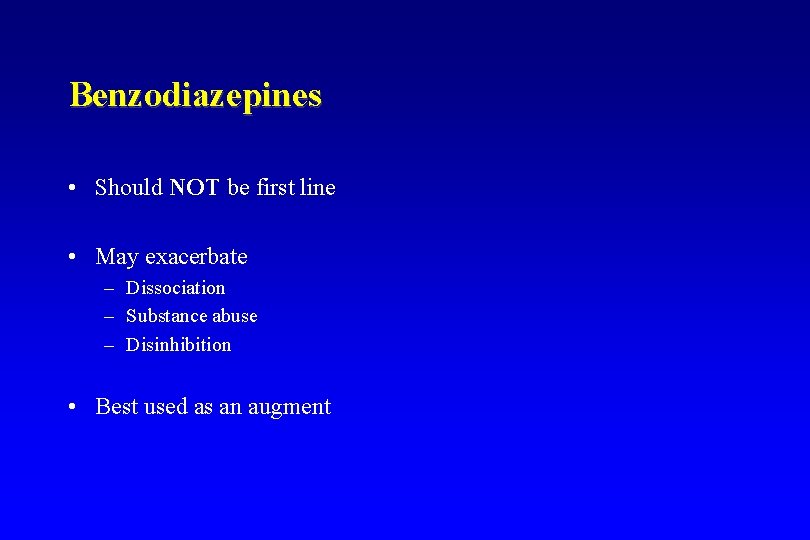
Benzodiazepines • Should NOT be first line • May exacerbate – Dissociation – Substance abuse – Disinhibition • Best used as an augment

Pharmacological Steps for PTSD • Start with and SSRI • Initiate with a low dose, half of what would start for depression • Titrate to a high dose • Once patient improves, maintain dosage for at least a year
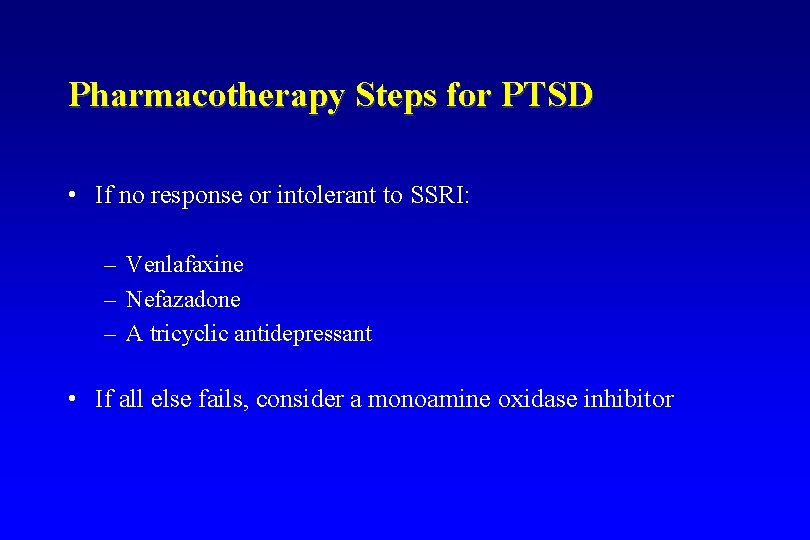
Pharmacotherapy Steps for PTSD • If no response or intolerant to SSRI: – Venlafaxine – Nefazadone – A tricyclic antidepressant • If all else fails, consider a monoamine oxidase inhibitor

Reasonable augmentations • Anticonvulsants: for dissociation, explosiveness, mood lability • Autonomic blockers: for SNS overactivity • Benzodiazepines or Buspirone: for excessive anxiety • Neuroleptics: for poor impulse control • Sedating antidepressants (Trazadone): for insomnia

Summary 1. Psychiatric disorders, especially depression and PTSD are common in HIV patients. 2. Depression is the strongest modifiable predictor of adherence to all medical therapy. 3. Adherence is the strongest predictor of disease progression and death after CD 4 count. 4. Depression should be treated prior to starting antiretroviral therapy. When in doubt, treat. 5. The behavioral manifestations of PTSD contribute to problems of HIV treatment adherance. • • Difficulty recognizing harm Difficulty developing self protective mechanism Compulsive need to repeat the trauma Sense of foreshortened future
 Hiv treatments
Hiv treatments Psychosis and ptsd
Psychosis and ptsd Ptsd model ehlers and clark
Ptsd model ehlers and clark Ptsd symptomer
Ptsd symptomer Macbeth nihilism quote
Macbeth nihilism quote Psykoedukation ptsd
Psykoedukation ptsd Va ptsd rating scale pdf
Va ptsd rating scale pdf Ptsd seizures
Ptsd seizures Dual representation theory ptsd
Dual representation theory ptsd Ptsd spiritual warfare
Ptsd spiritual warfare Cpt trust star worksheet
Cpt trust star worksheet Remains poem armitage
Remains poem armitage Ptsd violent behavior
Ptsd violent behavior Toleransfönstret
Toleransfönstret Evolution of ptsd
Evolution of ptsd Ptsd
Ptsd Jamal and deborah therapy
Jamal and deborah therapy What is complex post traumatic stress disorder
What is complex post traumatic stress disorder Causes of ptsd
Causes of ptsd Ptsd stages
Ptsd stages Toleransevinduet
Toleransevinduet Ptsd circumcision
Ptsd circumcision Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Treatments for acute renal failure
Treatments for acute renal failure Facial electrical treatments level 3
Facial electrical treatments level 3 Simultaneous treatment design
Simultaneous treatment design Diabetes treatments
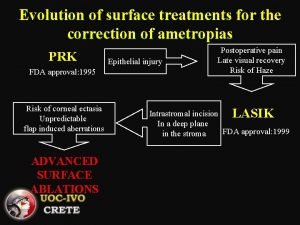
Diabetes treatments Advanced surface treatments
Advanced surface treatments Insomnia treatments
Insomnia treatments A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Compare and contrast hoover and roosevelt
Compare and contrast hoover and roosevelt The reformation outcome martin luther and the reformation
The reformation outcome martin luther and the reformation Dpgt cover sheet
Dpgt cover sheet Veyldf learning and development outcome descriptors
Veyldf learning and development outcome descriptors Counseling outcome research and evaluation
Counseling outcome research and evaluation The age of exploration outcome china and japan's reactions
The age of exploration outcome china and japan's reactions What was the outcome of china's age of exploration?
What was the outcome of china's age of exploration? Rapid access clinic london ontario
Rapid access clinic london ontario Content and learning outcome examples
Content and learning outcome examples The reformation outcome martin luther and the reformation
The reformation outcome martin luther and the reformation Ancient egypt and judaism outcome the new kingdom
Ancient egypt and judaism outcome the new kingdom Who won battle of lexington and concord
Who won battle of lexington and concord Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Hiv reverse transcription
Hiv reverse transcription Test wiedzy o hiv i aids z odpowiedziami
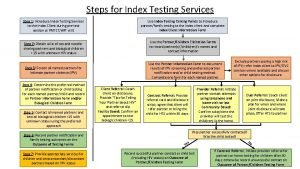
Test wiedzy o hiv i aids z odpowiedziami 10 steps of index testing
10 steps of index testing Elemen penilaian prognas snars edisi 1.1
Elemen penilaian prognas snars edisi 1.1 Phdp in hiv
Phdp in hiv Kuchecheudzwa
Kuchecheudzwa Window period hiv
Window period hiv Why do the bodys antibodies fail to protect people from hiv
Why do the bodys antibodies fail to protect people from hiv Iris hiv
Iris hiv Where did hiv come from
Where did hiv come from Hiv risk factors
Hiv risk factors Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Fiebig hiv
Fiebig hiv Ephi ethiopia
Ephi ethiopia Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Basic hiv course
Basic hiv course Stakeholders in hiv prevention
Stakeholders in hiv prevention