Deploying digital health interventions in the NHS He


- Slides: 22
Deploying digital health interventions in the NHS: He. LP-Diabetes Case study Elizabeth Murray 3 October 2017.
Outline • • • What is He. LP-Diabetes? Why did we want to deploy it in the NHS? How did we approach this? Setting up a Community Interest Company Lessons learnt
Background • Diabetes an NHS priority; c. 4 million people in UK • Self-management improves outcomes • Uptake of structured education remains low (c. 5%), despite incentivisation in the QOF • Partly due to problems of group-based education • Could a web-based self-management programme help?
He. LP-Diabetes • Funded by the NIHR Programme for Applied Health Research • £ 2 million over 5 years • Aim: to develop, evaluate and implement a webbased self-management programme for people with type 2 diabetes.
What is He. LP-Diabetes? • • Theoretically informed Evidence based Strong user input Interactive Videos, graphics Reading age of 12 QISMET certified www. helpdiabetes. org. uk/
Evidence of effectiveness and use • RCT in primary care (n = 374): – He. LP-Diabetes + TAU vs. information only website + TAU – He. LP-Diabetes improves diabetes control @ 12 months – Cost-effective • Implementation study in primary care (1 CCG) – – Adopted by 22/34 practices; 18 actually referred patients Adopted by hospital and intermediate care clinic Wide demographic of patients registering / using H-D Some evidence that HCP facilitation helped overcome digital divide
Why deploy He. LP-Diabetes across the NHS? • NIHR funding – explicit aim to improve patient care and health outcomes; • Explicit commitment to implementation in our grant application • Enormous PPI enthusiasm and pressure; • Effective, cost-effective and crossed digital divide; • Surely everybody would want it?
Approach to implementation (planning) 1. Thought about implementation from the conception of the grant. 2. Use of Normalisation Process Theory to guide development 3. Appropriate stakeholders recruited for steering group (NHS Direct, NHS Choices, CCG leads)
Approach to implementation (during grant) • Ensure intervention could be easily implemented • Discussions with UCL Business, UCL Enterprise, NHS Choices, NIHR • Preferred model was a commercial partner • Developed criteria for working with partners, e. g. – Free at the point of delivery – Commitment to holistic approach – Understanding of socio-technical aspects of implementation. • (Endless) meetings with potential partners …. .
Approach to implementation (as grant ended) • Dawning realisation that a satisfactory commercial partnership was unlikely • Increasing interest from CCGs outside the study area • Exploration of alternative ways forward • Decision to set up a not-for-profit Community Interest Company (June 2015) • He. LP-Digital (2 members – UCL and the Whittington NHS Trust)

Awards • Health and Social Innovator Programme – £ 40, 000 investment; incubator programme • UCL Social Enterprise Project of the Year Award 2015 (received honourable mention) • People Driven Digital un. Awards 2015 – Finalist (most impressive digitally-enabled health/social care service)
Current status • Business model = flat fee license for whole CCG (not per user); CCG takes responsibility for uptake • Commissioned by 5 London CCGs and 1 in Northumbria • Approximately 1, 000 registered users • Around 130 new registrations per month, but very variable between CCGs
Lessons learnt • Running a company is very different to being an academic – need a completely different skill set and outlook. • The NHS model of commissioning by CCG is not suited to digital health interventions, as their key advantage is scalability • Needing to negotiate individual contracts puts up costs ++++, undermining cost-effectiveness • CCGs vary in encouraging uptake and use; low uptake undermines perceived value.
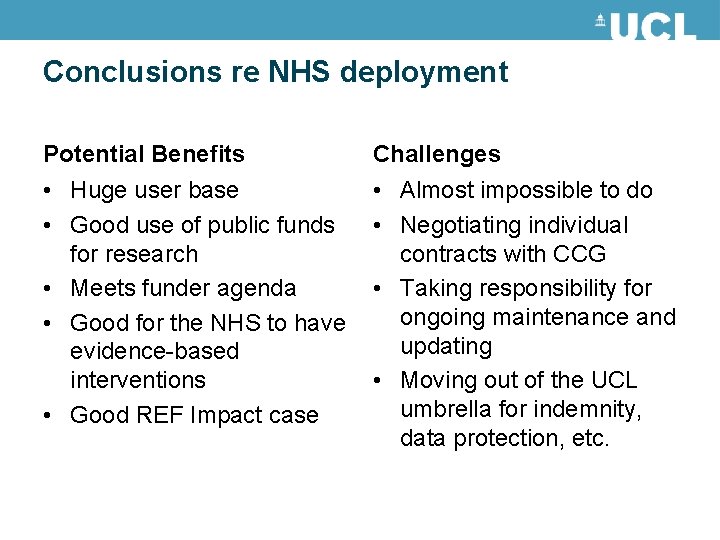
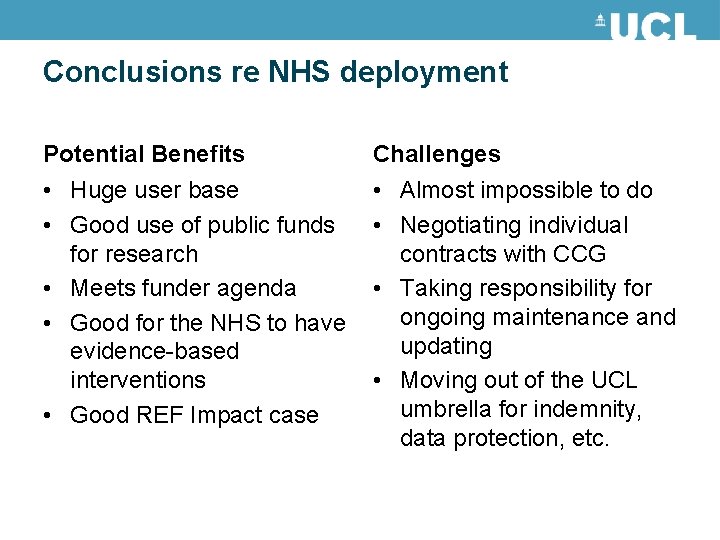
Conclusions re NHS deployment Potential Benefits Challenges • Huge user base • Good use of public funds for research • Meets funder agenda • Good for the NHS to have evidence-based interventions • Good REF Impact case • Almost impossible to do • Negotiating individual contracts with CCG • Taking responsibility for ongoing maintenance and updating • Moving out of the UCL umbrella for indemnity, data protection, etc.
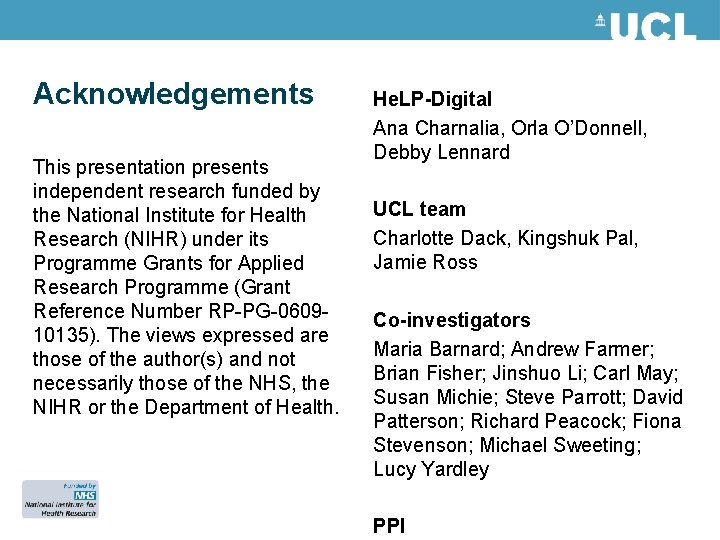
Acknowledgements This presentation presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (Grant Reference Number RP-PG-060910135). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. He. LP-Digital Ana Charnalia, Orla O’Donnell, Debby Lennard UCL team Charlotte Dack, Kingshuk Pal, Jamie Ross Co-investigators Maria Barnard; Andrew Farmer; Brian Fisher; Jinshuo Li; Carl May; Susan Michie; Steve Parrott; David Patterson; Richard Peacock; Fiona Stevenson; Michael Sweeting; Lucy Yardley PPI
Questions?
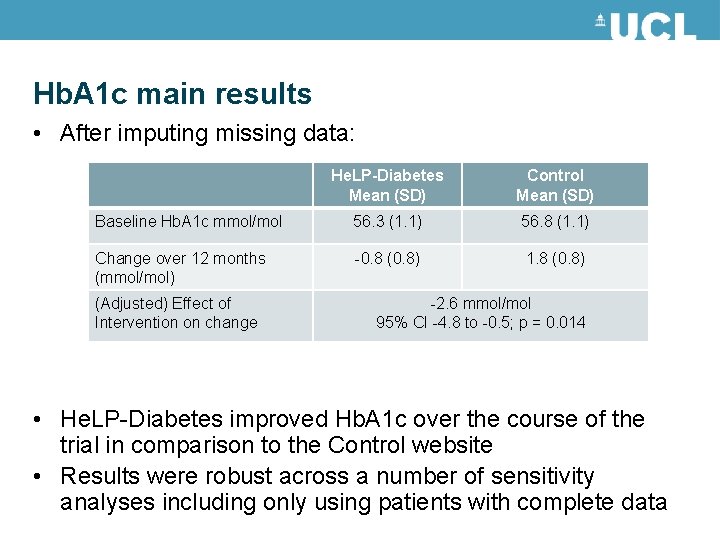
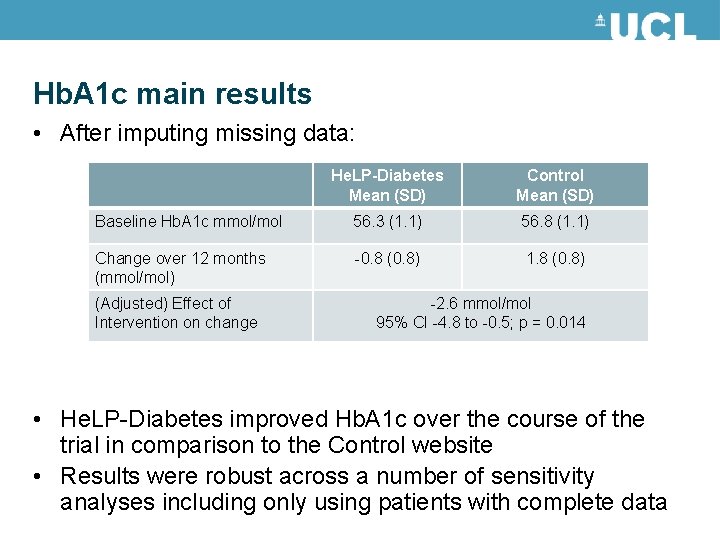
Hb. A 1 c main results • After imputing missing data: He. LP-Diabetes Mean (SD) Control Mean (SD) Baseline Hb. A 1 c mmol/mol 56. 3 (1. 1) 56. 8 (1. 1) Change over 12 months (mmol/mol) -0. 8 (0. 8) 1. 8 (0. 8) (Adjusted) Effect of Intervention on change -2. 6 mmol/mol 95% CI -4. 8 to -0. 5; p = 0. 014 • He. LP-Diabetes improved Hb. A 1 c over the course of the trial in comparison to the Control website • Results were robust across a number of sensitivity analyses including only using patients with complete data

Within trial cost-effectiveness data £ 50 000 £ 45 000 £ 40 000 N = 58 ICER = £ 30, 281/QA LYN = 81 ICER = £ 20, 050/QA LY ICER £ 35 000 £ 30 000 £ 25 000 £ 20 000 £ 15 000 £ 10 000 £ 5 000 £ 0 40 90 140 190 240 Number of users 290 340
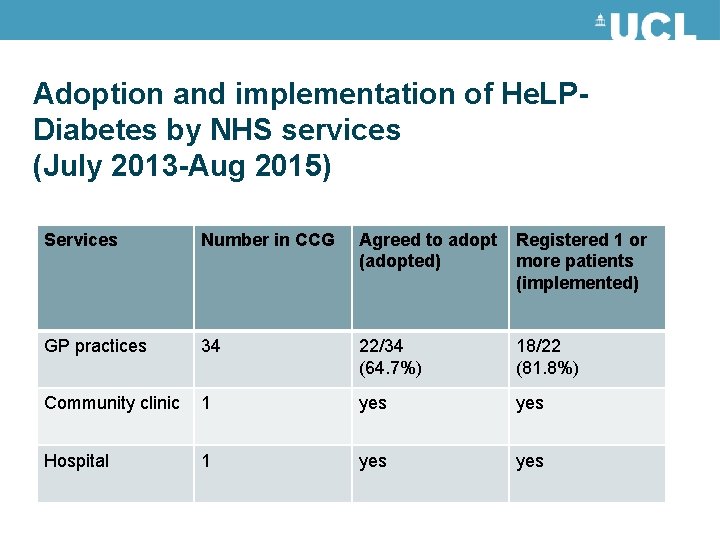
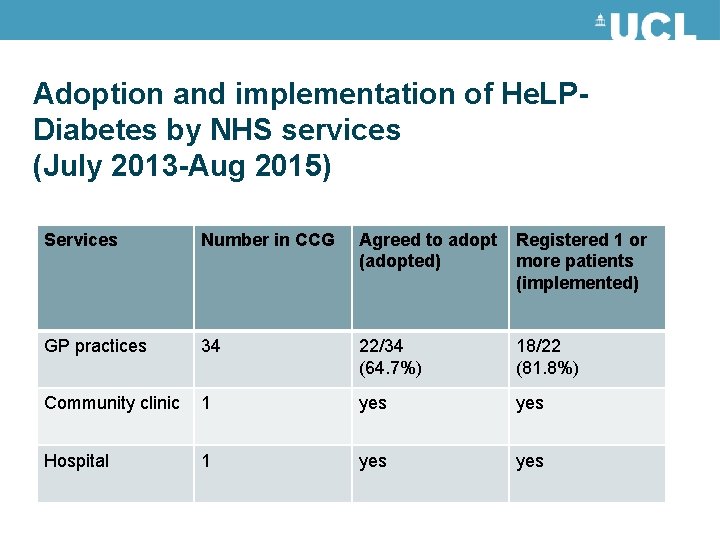
Adoption and implementation of He. LPDiabetes by NHS services (July 2013 -Aug 2015) Services Number in CCG Agreed to adopt (adopted) Registered 1 or more patients (implemented) GP practices 34 22/34 (64. 7%) 18/22 (81. 8%) Community clinic 1 yes Hospital 1 yes
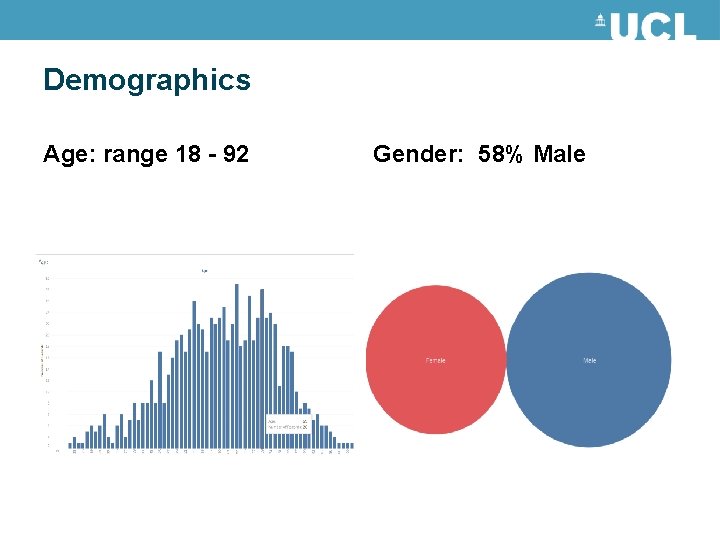
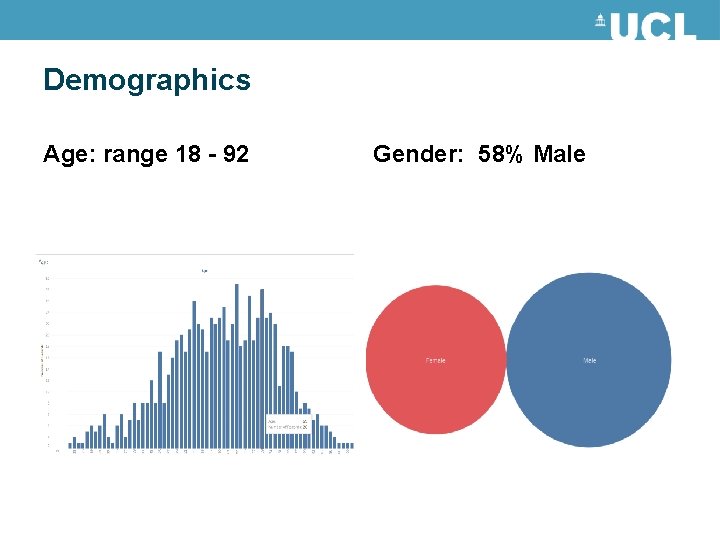
Demographics Age: range 18 - 92 Gender: 58% Male
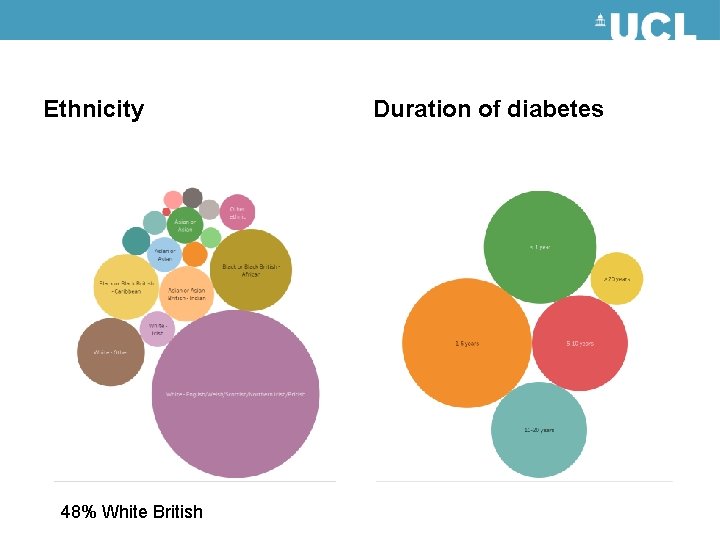
Ethnicity 48% White British Duration of diabetes
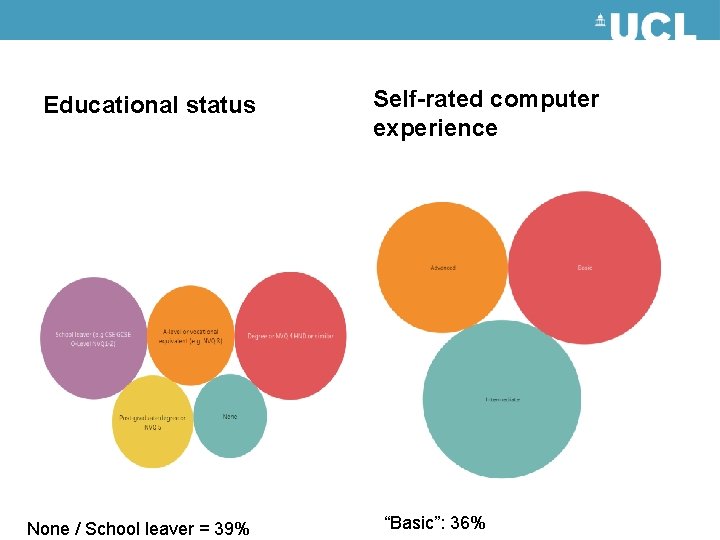
Educational status None / School leaver = 39% Self-rated computer experience “Basic”: 36%