DepersonalizationDerealization Disorder WHAT IS DEPERSONALIZATION AND DEREALIZATION DEPERSONALIZATION
- Slides: 1
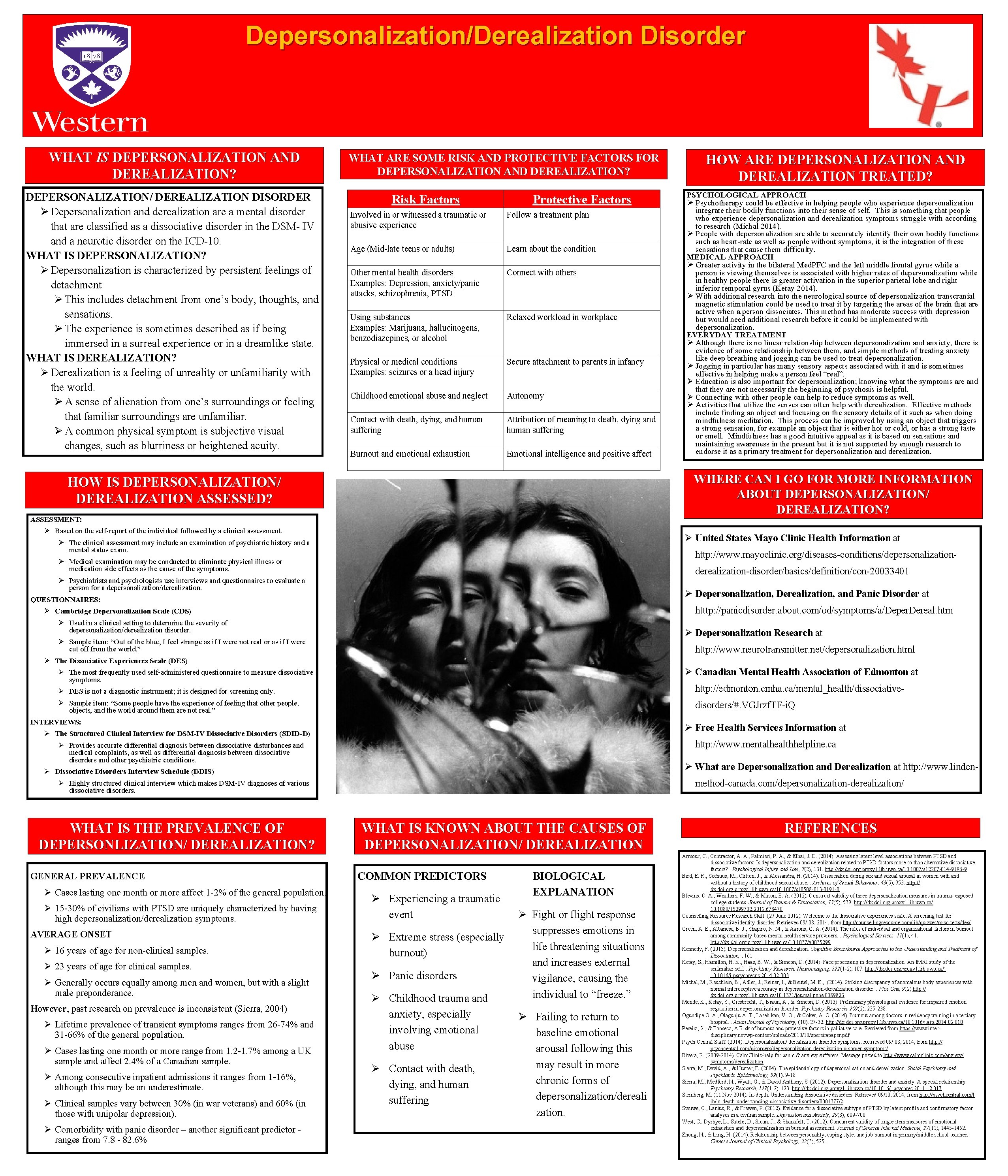
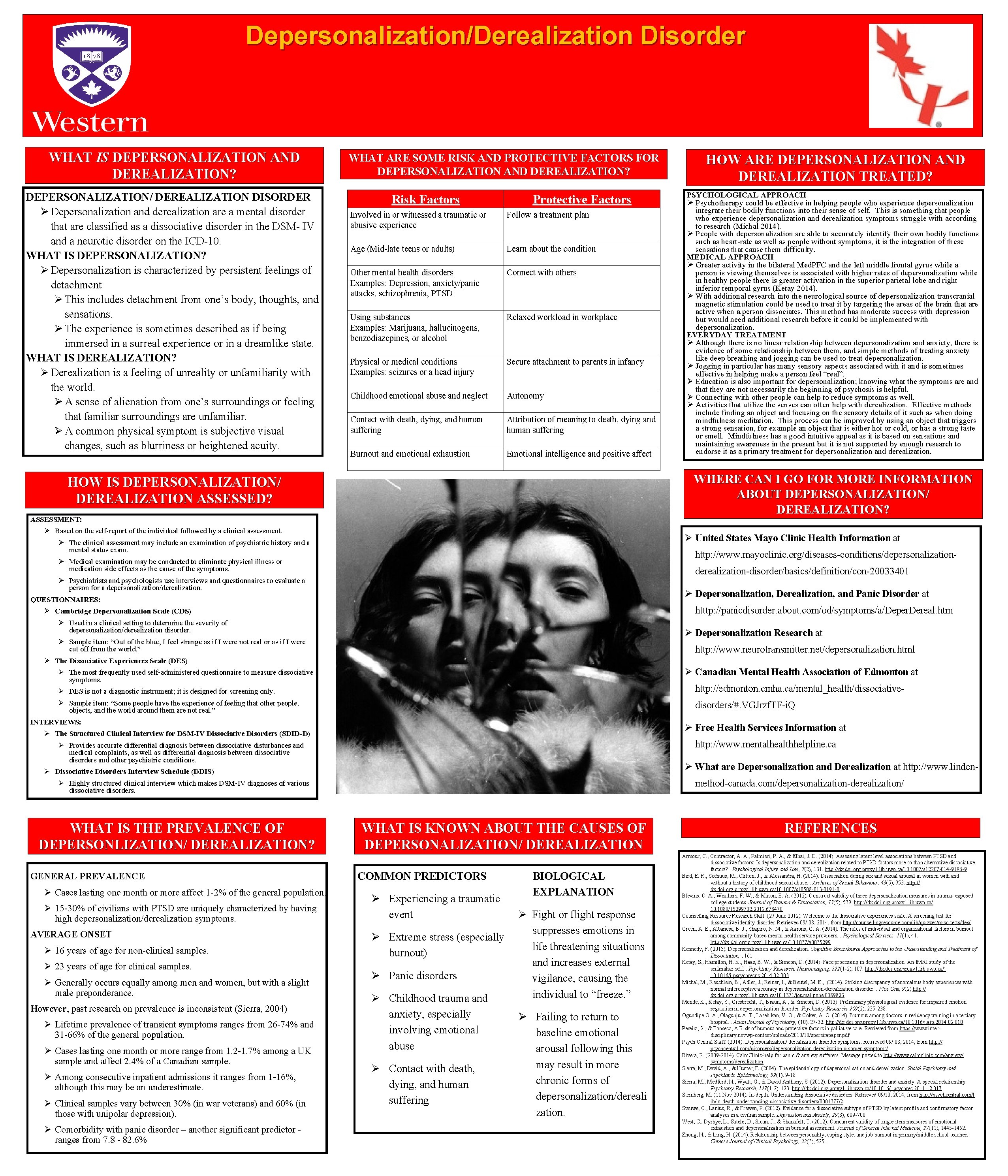
Depersonalization/Derealization Disorder WHAT IS DEPERSONALIZATION AND DEREALIZATION? DEPERSONALIZATION/ DEREALIZATION DISORDER Ø Depersonalization and derealization are a mental disorder that are classified as a dissociative disorder in the DSM- IV and a neurotic disorder on the ICD-10. WHAT IS DEPERSONALIZATION? Ø Depersonalization is characterized by persistent feelings of detachment Ø This includes detachment from one’s body, thoughts, and sensations. Ø The experience is sometimes described as if being immersed in a surreal experience or in a dreamlike state. WHAT IS DEREALIZATION? Ø Derealization is a feeling of unreality or unfamiliarity with the world. Ø A sense of alienation from one’s surroundings or feeling that familiar surroundings are unfamiliar. Ø A common physical symptom is subjective visual changes, such as blurriness or heightened acuity. WHAT ARE SOME RISK AND PROTECTIVE FACTORS FOR DEPERSONALIZATION AND DEREALIZATION? Risk Factors Protective Factors Involved in or witnessed a traumatic or abusive experience Follow a treatment plan Age (Mid-late teens or adults) Learn about the condition Other mental health disorders Examples: Depression, anxiety/panic attacks, schizophrenia, PTSD Connect with others Using substances Examples: Marijuana, hallucinogens, benzodiazepines, or alcohol Relaxed workload in workplace Physical or medical conditions Examples: seizures or a head injury Secure attachment to parents in infancy Childhood emotional abuse and neglect Autonomy Contact with death, dying, and human suffering Attribution of meaning to death, dying and human suffering Burnout and emotional exhaustion Emotional intelligence and positive affect HOW ARE DEPERSONALIZATION AND DEREALIZATION TREATED? PSYCHOLOGICAL APPROACH Ø Psychotherapy could be effective in helping people who experience depersonalization integrate their bodily functions into their sense of self. This is something that people who experience depersonalization and derealization symptoms struggle with according to research (Michal 2014). Ø People with depersonalization are able to accurately identify their own bodily functions such as heart-rate as well as people without symptoms, it is the integration of these sensations that cause them difficulty. MEDICAL APPROACH Ø Greater activity in the bilateral Med. PFC and the left middle frontal gyrus while a person is viewing themselves is associated with higher rates of depersonalization while in healthy people there is greater activation in the superior parietal lobe and right inferior temporal gyrus (Ketay 2014). Ø With additional research into the neurological source of depersonalization transcranial magnetic stimulation could be used to treat it by targeting the areas of the brain that are active when a person dissociates. This method has moderate success with depression but would need additional research before it could be implemented with depersonalization. EVERYDAY TREATMENT Ø Although there is no linear relationship between depersonalization and anxiety, there is evidence of some relationship between them, and simple methods of treating anxiety like deep breathing and jogging can be used to treat depersonalization. Ø Jogging in particular has many sensory aspects associated with it and is sometimes effective in helping make a person feel “real”. Ø Education is also important for depersonalization; knowing what the symptoms are and that they are not necessarily the beginning of psychosis is helpful. Ø Connecting with other people can help to reduce symptoms as well. Ø Activities that utilize the senses can often help with derealization. Effective methods include finding an object and focusing on the sensory details of it such as when doing mindfulness meditation. This process can be improved by using an object that triggers a strong sensation, for example an object that is either hot or cold, or has a strong taste or smell. Mindfulness has a good intuitive appeal as it is based on sensations and maintaining awareness in the present but it is not supported by enough research to endorse it as a primary treatment for depersonalization and derealization. WHERE CAN I GO FOR MORE INFORMATION ABOUT DEPERSONALIZATION/ DEREALIZATION? HOW IS DEPERSONALIZATION/ DEREALIZATION ASSESSED? ASSESSMENT: Ø Based on the self-report of the individual followed by a clinical assessment. Ø United States Mayo Clinic Health Information at Ø The clinical assessment may include an examination of psychiatric history and a mental status exam. http: //www. mayoclinic. org/diseases-conditions/depersonalization- Ø Medical examination may be conducted to eliminate physical illness or medication side effects as the cause of the symptoms. derealization-disorder/basics/definition/con-20033401 Ø Psychiatrists and psychologists use interviews and questionnaires to evaluate a person for a depersonalization/derealization. Ø Depersonalization, Derealization, and Panic Disorder at QUESTIONNAIRES: htttp: //panicdisorder. about. com/od/symptoms/a/Deper. Dereal. htm Ø Cambridge Depersonalization Scale (CDS) Ø Used in a clinical setting to determine the severity of depersonalization/derealization disorder. Ø Depersonalization Research at Ø Sample item: “Out of the blue, I feel strange as if I were not real or as if I were cut off from the world. ” http: //www. neurotransmitter. net/depersonalization. html Ø The Dissociative Experiences Scale (DES) Ø Canadian Mental Health Association of Edmonton at Ø The most frequently used self-administered questionnaire to measure dissociative symptoms. Ø DES is not a diagnostic instrument; it is designed for screening only. http: //edmonton. cmha. ca/mental_health/dissociative- Ø Sample item: “Some people have the experience of feeling that other people, objects, and the world around them are not real. ” disorders/#. VGJrzf. TF-i. Q INTERVIEWS: Ø Free Health Services Information at Ø The Structured Clinical Interview for DSM-IV Dissociative Disorders (SDID-D) http: //www. mentalhealthhelpline. ca Ø Provides accurate differential diagnosis between dissociative disturbances and medical complaints, as well as differential diagnosis between dissociative disorders and other psychiatric conditions. Ø What are Depersonalization and Derealization at http: //www. linden- Ø Dissociative Disorders Interview Schedule (DDIS) method-canada. com/depersonalization-derealization/ Ø Highly structured clinical interview which makes DSM-IV diagnoses of various dissociative disorders. WHAT IS THE PREVALENCE OF DEPERSONLIZATION/ DEREALIZATION? GENERAL PREVALENCE Ø Cases lasting one month or more affect 1 -2% of the general population. Ø 15 -30% of civilians with PTSD are uniquely characterized by having high depersonalization/derealization symptoms. AVERAGE ONSET Ø 16 years of age for non-clinical samples. Ø 23 years of age for clinical samples. Ø Generally occurs equally among men and women, but with a slight male preponderance. However, past research on prevalence is inconsistent (Sierra, 2004) Ø Lifetime prevalence of transient symptoms ranges from 26 -74% and 31 -66% of the general population. Ø Cases lasting one month or more range from 1. 2 -1. 7% among a UK sample and affect 2. 4% of a Canadian sample. Ø Among consecutive inpatient admissions it ranges from 1 -16%, although this may be an underestimate. Ø Clinical samples vary between 30% (in war veterans) and 60% (in those with unipolar depression). Ø Comorbidity with panic disorder – another significant predictor - ranges from 7. 8 - 82. 6% WHAT IS KNOWN ABOUT THE CAUSES OF DEPERSONALIZATION/ DEREALIZATION COMMON PREDICTORS Ø Experiencing a traumatic event BIOLOGICAL EXPLANATION Ø Fight or flight response suppresses emotions in Ø Extreme stress (especially life threatening situations burnout) and increases external Ø Panic disorders vigilance, causing the individual to “freeze. ” Ø Childhood trauma and anxiety, especially Ø Failing to return to involving emotional baseline emotional abuse arousal following this Ø Contact with death, dying, and human suffering may result in more chronic forms of depersonalization/dereali zation. REFERENCES Armour, C. , Contractor, A. A. , Palmieri, P. A. , & Elhai, J. D. (2014). Assessing latent level associations between PTSD and dissociative factors: Is depersonalization and derealization related to PTSD factors more so than alternative dissociative factors? . Psychological Injury and Law, 7(2), 131. http: //dx. doi. org. proxy 1. lib. uwo. ca/10. 1007/s 12207 -014 -9196 -9 Bird, E. R. , Seehuus, M. , Clifton, J. , & Alessandra, H. (2014). Dissociation during sex and sexual arousal in women with and without a history of childhood sexual abuse. . Archives of Sexual Behaviour, 43(5), 953. http: // dx. doi. org. proxy 1. lib. uwo. ca/10. 1007/s 10508 -013 -0191 -0 Blevins, C. A. , Weathers, F. W. , & Mason, E. A. (2012). Construct validity of three depersonalization measures in trauma- exposed college students. Journal of Trauma & Dissociation, 13(5), 539. http: //dx. doi. org. proxy 1. lib. uwo. ca/ 10. 1080/15299732. 2012. 678470 Counselling Resource Research Staff. (27 June 2012). Welcome to the dissociative experiences scale, A screening test for dissociative identity disorder. Retrieved 09/ 08, 2014, from http: //counsellingresource. com/lib/quizzes/misc-tests/des/ Green, A. E. , Albanese, B. J. , Shapiro, N. M. , & Aarons, G. A. (2014). The roles of individual and organizational factors in burnout among community-based mental health service providers. . Psychological Services, 11(1), 41. http: //dx. doi. org. proxy 1. lib. uwo. ca/10. 1037/a 0035299 Kennedy, F. (2013). Depersonalization and derealization. Cognitive Behavioural Approaches to the Understanding and Treatment of Dissociation, , 161. Ketay, S. , Hamilton, H. K. , Haas, B. W. , & Simeon, D. (2014). Face processing in depersonalization: An f. MRI study of the unfamiliar self. . Psychiatry Research: Neuroimaging, 222(1 -2), 107. http: //dx. doi. org. proxy 1. lib. uwo. ca/` 10. 1016/j. pscychresns. 2014. 02. 003 Michal, M. , Reuchlein, B. , Adler, J. , Reiner, I. , & Beutel, M. E. , . (2014). Striking discrepancy of anomalous body experiences with normal interoceptive accuracy in depersonalization-derealization disorder. . Plos One, 9(2) http: // dx. doi. org. proxy 1. lib. uwo. ca/10. 1371/journal. pone. 0089823 Monde, K. , Ketay, S. , Giesbrecht, T. , Braun, A. , & Simeon, D. (2013). Preliminary physiological evidence for impaired emotion regulation in depersonalization disorder. Psychiatry Research, 209(2), 235 -238. Ogundipe O. A. , Olagunju A. T. , Lasebikan, V. O. , & Coker, A. O. (2014). Burnout among doctors in residency training in a tertiary hospital. . Asian Journal of Psychiatry, (10), 27 -32. http: //dx. doi. org. proxy 1. lib. uwo. ca/10. 1016/j. ajp. 2014. 02. 010 Pereira, S. , & Fonseca, A. Risk of burnout and protective factors in palliative care. Retrieved from https: //www. interdisciplinary. net/wp-content/uploads/2010/10/spereirapaper. pdf Psych Central Staff. (2014). Depersonalization/ derealization disorder symptoms. Retrieved 09/ 08, 2014, from http: // psychcentral. com/disorders/depersonalization-derealization-disorder-symptoms/ Rivera, R. (2009 -2014). Calm. Clinic-help for panic & anxiety sufferers. Message posted to http: //www. calmclinic. com/anxiety/ symptoms/derealization Sierra, M. , David, A. , & Hunter, E. (2004). The epidemiology of depersonalisation and derealization. Social Psychiatry and Psychiatric Epidemiology, 39(1), 9 -18. Sierra, M. , Medford, N. , Wyatt, G. , & David Anthony, S. (2012). Depersonalization disorder and anxiety: A special relationship. Psychiatry Research, 197(1 -2), 123. http: //dx. doi. org. proxy 1. lib. uwo. ca/10. 1016/j. psychres. 2011. 12. 017 Steinberg, M. (11 Nov 2014). In-depth: Understanding dissociative disorders. Retrieved 09/10, 2014, from http: //psychcentral. com/l ib/in-depth-understanding-dissociative-disorders/0001377/2 Steuwe, C. , Lanius, R. , & Frewen, P. (2012). Evidence for a dissociative subtype of PTSD by latent profile and confirmatory factor analyses in a civilian sample. Depression and Anxiety, 29(8), 689 -700. West, C. , Dyrbye, L. , Satele, D. , Sloan, J. , & Shanafelt, T. (2012). Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. Journal of General Internal Medicine, 27(11), 1445 -1452. Zhong, N. , & Ling, H. (2014). Relationship between personality, coping style, and job burnout in primary/middle school teachers. Chinese Journal of Clinical Psychology, 22(3), 525. Template provided by: “posters 4 research. com”