DEPARTMENT OF NEUROLOGY OSMANIA MEDICAL COLLEGE Dr kiran





































- Slides: 92
DEPARTMENT OF NEUROLOGY OSMANIA MEDICAL COLLEGE Dr kiran Resident in Neurology
American Academy of Neurology Guideline Update 2010 Determining BRAIN DEATH in Adult
Coma, from the Greek ‘‘deep sleep or trance, ’’ is a state of unresponsiveness in which the patient lies with eyes closed and cannot be aroused to respond appropriately to stimuli even with vigorous stimulation.

• Three medical considerations emphasize the importance of the concept of brain death: (1) Transplant programs require the donation of healthy peripheral organs for success. The early diagnosis of brain death before the systemic circulation fails allows the salvage of such organs. However, ethical and legal considerations demand that if one is to declare the brain dead, the criteria must be clear and unassailable

(2) Even if there were no transplant programs, the ability of modern medicine to keep a body functioning for extended periods often leads to prolonged, expensive, and futile procedures accompanied by great emotional strain on family and medical staff.

(3) Critical care facilities; are limited and expensive and inevitably place a drain on other medical resources. Their best use demands that one identify and select patients who are most likely to benefit from intensive techniques, so that these units are not overloaded with individuals who can never recover cerebral function.
The THREE clinical findings necessary to confirm irreversible cessation of all functions of the entire brain, including the brain stem: 1. coma (with a known cause) 2. absence of brainstem reflexes, and 3. apnea.
4 Steps in Determining Brain Death The Clinical Evaluation The Neurologic Assessment Ancillary Test Documentation
The Clinical Evaluation A. Establish irreversible and proximate cause of coma. Exclude the presence of a CNS-depressant drug effect There should be no recent administration or continued presence of neuromuscular blocking agents There should be no severe electrolyte, acid-base, or endocrine disturbance

The Clinical Evaluation B. Achieve normal core temperature. Raise the body temperature and maintain a normal or nearnormal temperature-36°C
The Clinical Evaluation C. Achieve normal systolic blood pressure. Neurologic examination is usually reliable with a systolic blood pressure 100 mm Hg.
The Clinical Evaluation D. Perform 1 neurologic examination If a certain period of time has passed since the onset of the brain insult to exclude the possibility of recovery, 1 neurologic examination should be sufficient to pronounce brain death.

4 Steps in Determining Brain Death The Clinical Evaluation The Neurologic Assessment

The Neurologic Assessment A. Coma Patients must lack all evidence of responsiveness. Eye opening or eye movement to noxious stimuli is absent. Noxious stimuli should not produce a motor response other than spinally mediated reflexes.
The Neurologic Assessment B. Absence of Brain Stem Reflex Absence of pupillary response to a bright light is documented in both eyes. Absence of ocular movements using oculocephalic testing and oculovestibular reflex testing. Absence of corneal reflex. Absence of facial muscle movement to a noxious stimulus. Absence of the pharyngeal and tracheal reflexes.

The Neurologic Assessment C. Apnea Absence of a breathing drive. Breathing drive is tested with CO 2 Challenge. Prerequisites: 1) normotension 2) normothermia, 3) euvolemia 4) eucapnia (Pa. CO 2 35– 45 mm Hg) 5) absence of hypoxia 6) no prior evidence of CO 2 retention

The CO 2 Challenge Adjust vasopressors to a systolic blood pressure 100 mm Hg. Preoxygenate for at least 10 minutes with 100% oxygen to a Pa. O 2 200 mm Hg. Reduce ventilation frequency to 10 breaths per minute to eucapnia. Reduce positive end-expiratory pressure (PEEP) to 5 cm H 2 O If pulse oximetry oxygen saturation remains 95%, obtain a baseline blood gas
The CO 2 Challenge Disconnect the patient from the ventilator. Preserve oxygenation(e. g. , place an insufflation catheter through the endotracheal tube and close to the level of the carina and deliver 100% O 2 at 6 L/min). Look closely for respiratory movements for 8– 10 minutes. Abort if systolic blood pressure decreases to 90 mm Hg. Abort if oxygen saturation measured by pulse oximetry is 85% for 30 seconds.
The CO 2 Challenge If no respiratory drive is observed, repeat blood gas after 8 minutes. If respiratory movements are absent and arterial PCO 2 is 60 mm Hg (or 20 mm Hg increase in arterial PCO 2 over a baseline normal arterial PCO 2), the apnea test result is POSITIVE. If the test is inconclusive but the patient is hemodynamically stable during the procedure, it may be repeated for a longer period of time (10– 15 minutes) after the patient is again adequately preoxygenated.

4 Steps in Determining Brain Death The Clinical Evaluation The Neurologic Assessment Ancillary Test
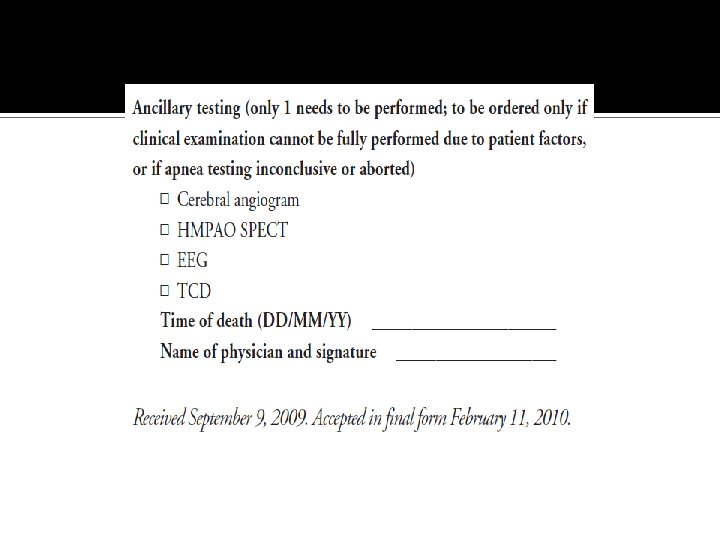
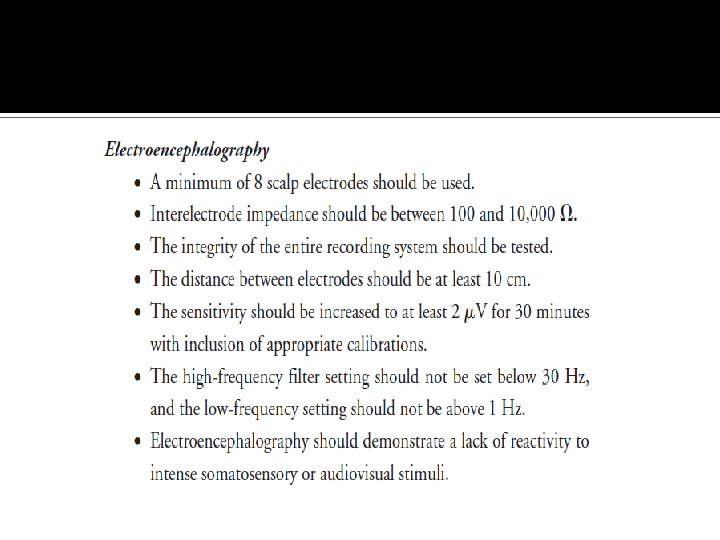
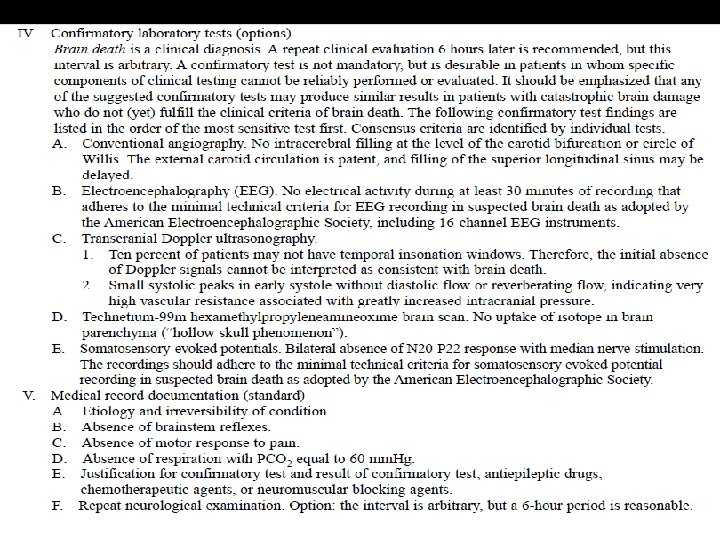
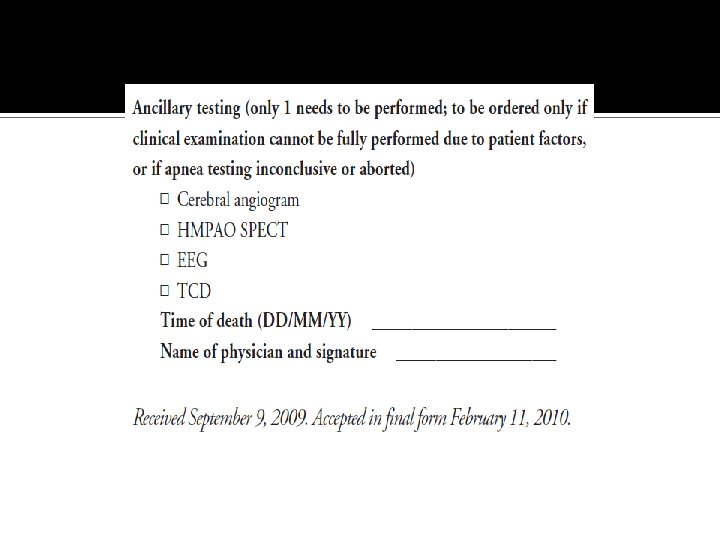
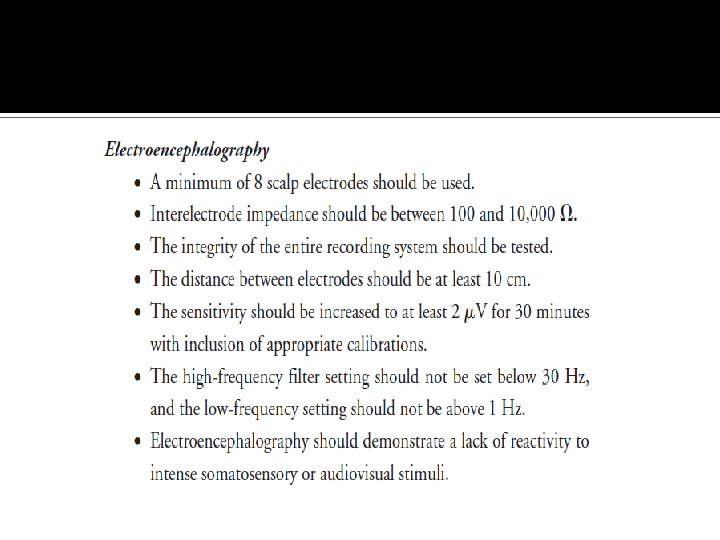
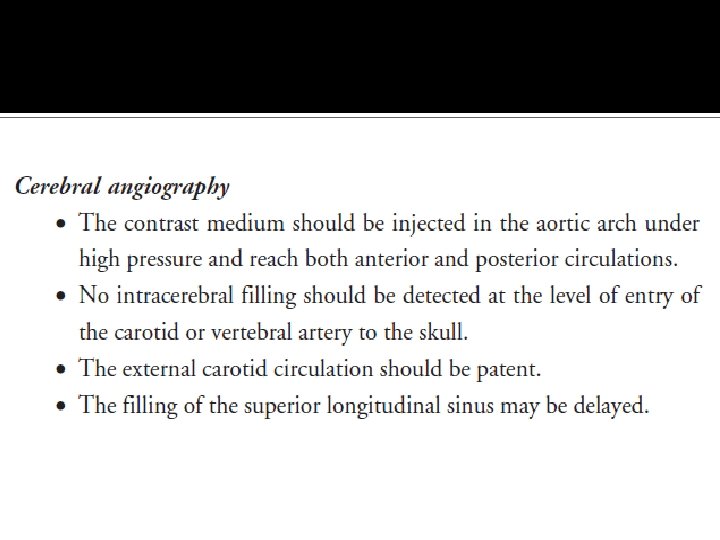
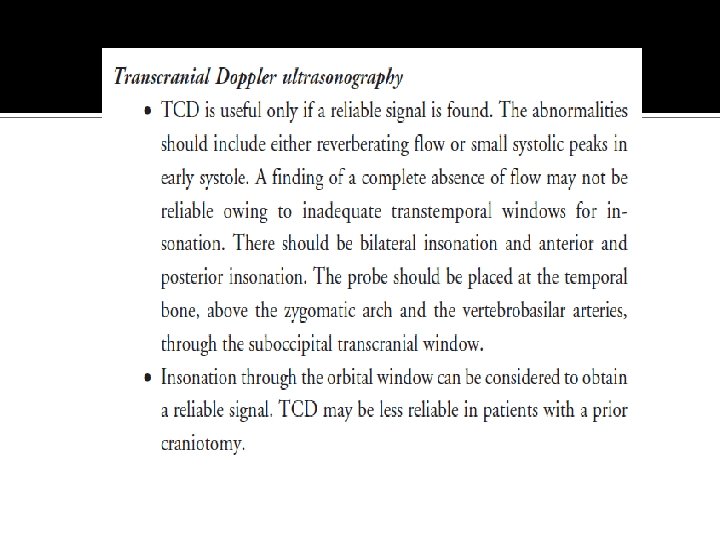
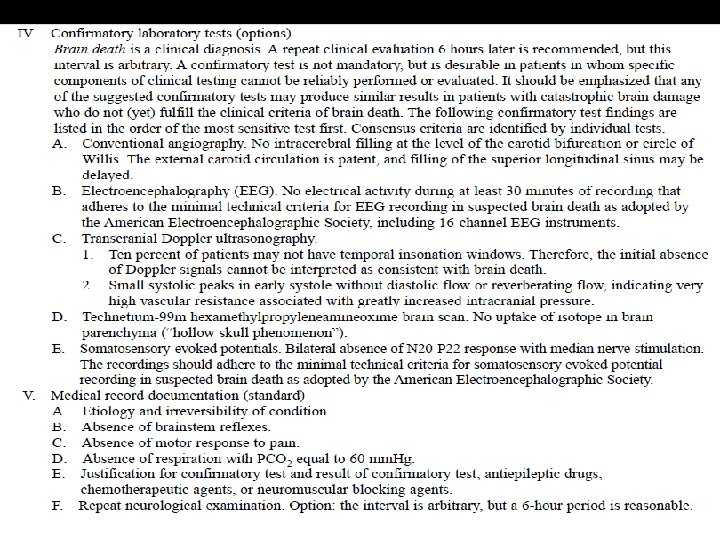
Ancillary Tests In clinical practice, EEG, cerebral angiography, nuclear scan, TCD, CTA, and MRI/MRA are currently used ancillary tests in adults. Ancillary tests can be used when uncertainty exists about the reliability of parts of the neurologic examination or when the apnea test cannot be performed.

“In adults, ancillary tests are not needed for the clinical diagnosis of brain death and cannot replace a neurologic examination. ”

4 Steps in Determining Brain Death The Clinical Evaluation The Neurologic Assessment Ancillary Test Documentation
Documentation Time of death is the time the arterial PCO 2 reached the target value (60). In patients with an aborted apnea test, the time of death is when the ancillary test has been officially interpreted.
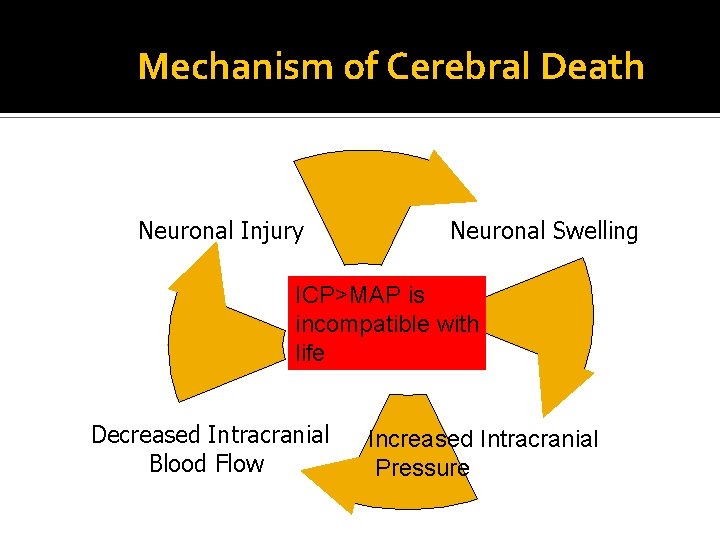
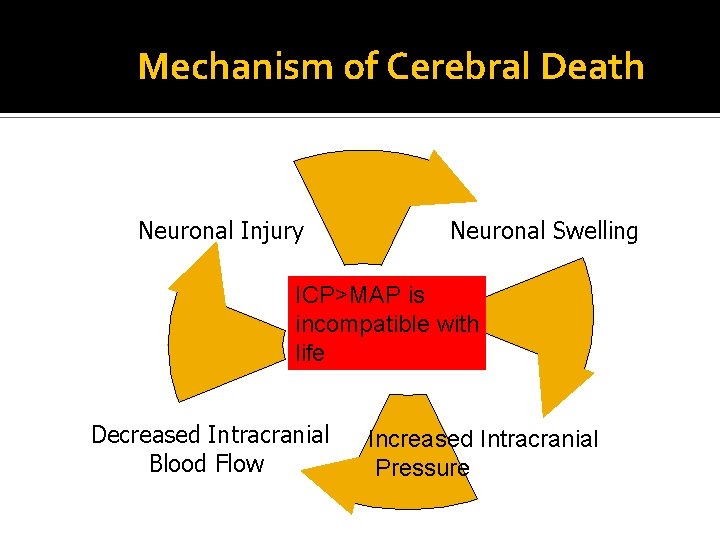
Mechanism of Cerebral Death Neuronal Injury Neuronal Swelling ICP>MAP is incompatible with life Decreased Intracranial Blood Flow Increased Intracranial Pressure


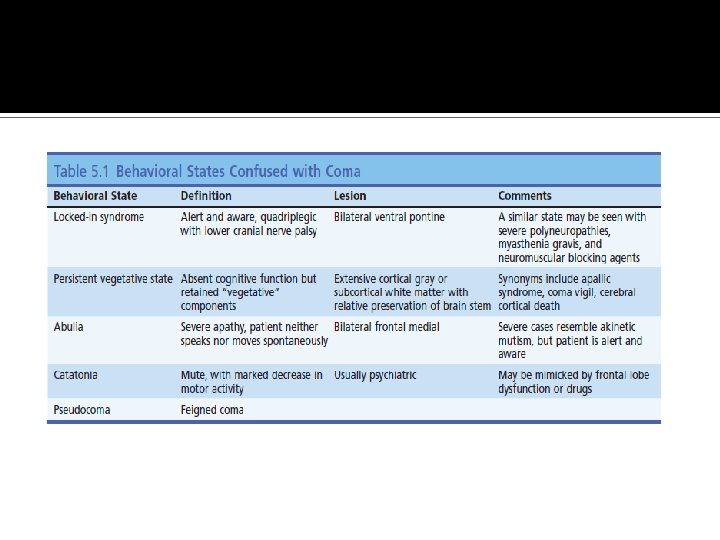
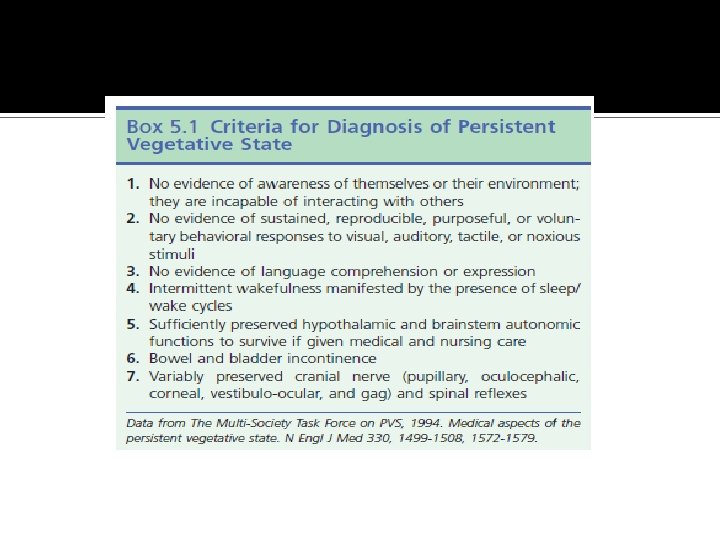
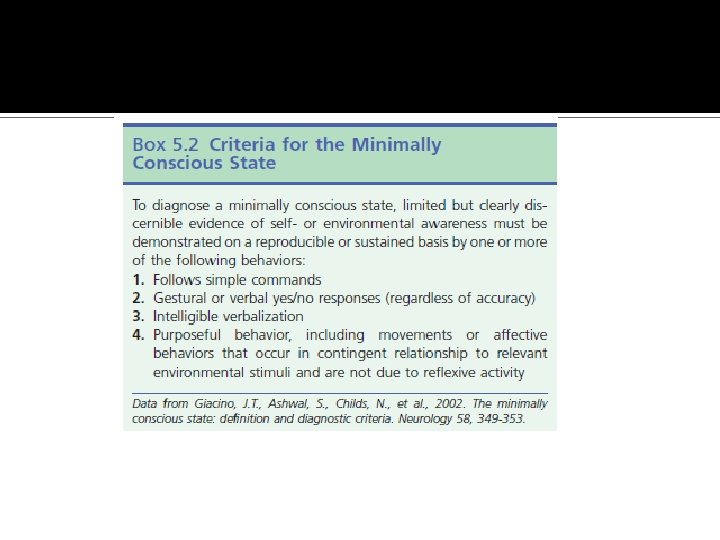
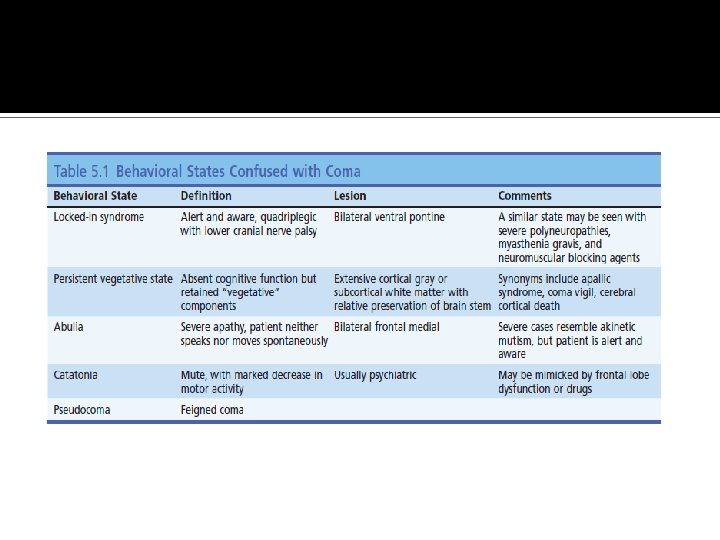
Conditions Distinct From Brain Death Persistent Vegetative State Locked-in Syndrome Minimally Responsive State

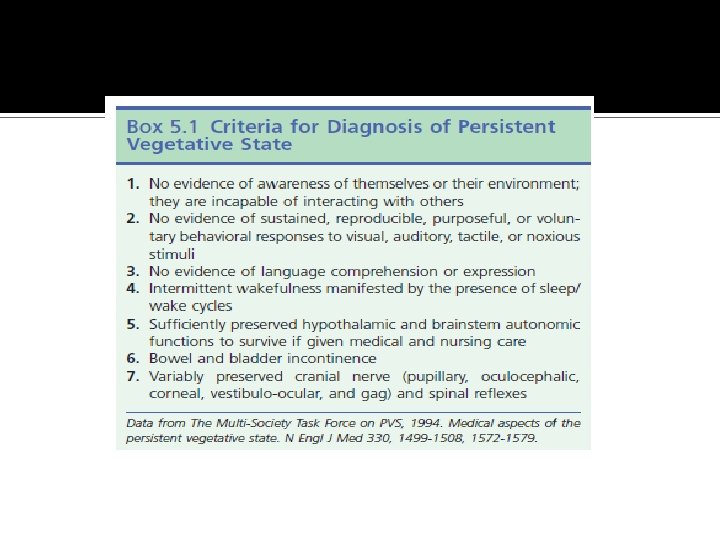
Persistent Vegetative State Normal Sleep-Wake Cycles No Response to Environmental Stimuli Diffuse Brain Injury with Preservation of Brain Stem Function
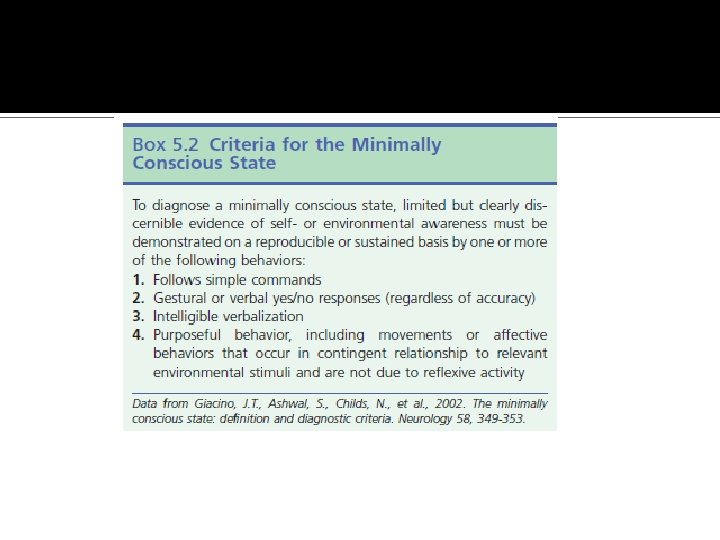
Minimally Responsive Static Encephalopathy Diffuse or Multi-Focal Brain Injury Preserved Brain Stem Function Variable Interaction with Environmental Stimuli
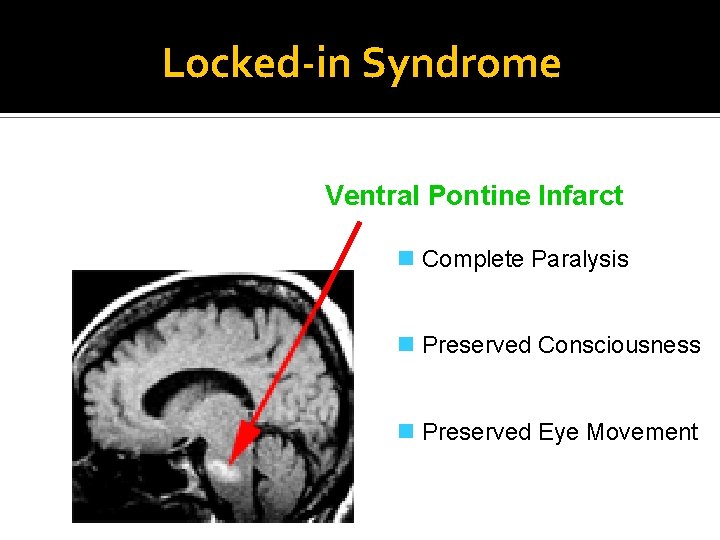
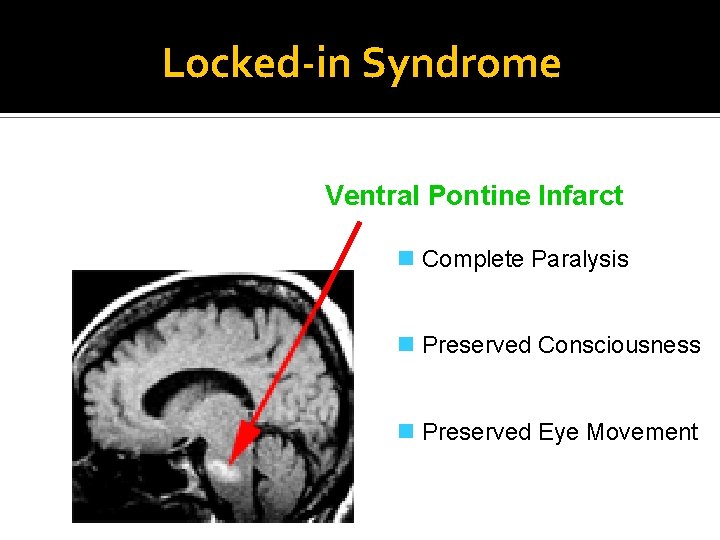
Locked-in Syndrome Ventral Pontine Infarct n Complete Paralysis n Preserved Consciousness n Preserved Eye Movement

Brain Death Neurological Examination Clinical Prerequisites: n Known Irreversible Cause n Exclusion of Potentially Reversible Conditions ▪ Drug Intoxication or Poisoning ▪ Electrolyte or Acid-Base Imbalance ▪ Endocrine Disturbances n Core Body temperature > 32° C
Brain Death Neurological Examination Coma Absent Brain Stem Reflexes Apnea
Coma No Response to Noxious Stimuli ▪ Nail Bed Pressure ▪ Sternal Rub ▪ Supra-Orbital Ridge Pressure
Absence of Brain Stem Reflexes Pupillary Reflex Eye Movements Facial Sensation and Motor Response Pharyngeal (Gag) Reflex Tracheal (Cough) Reflex
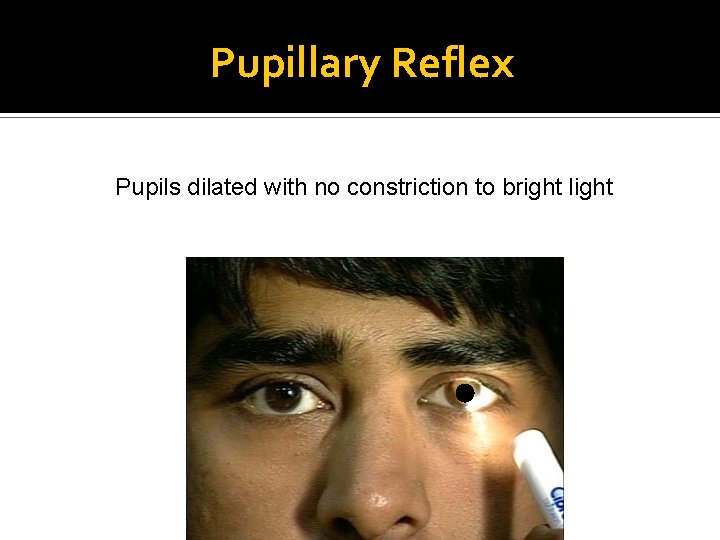
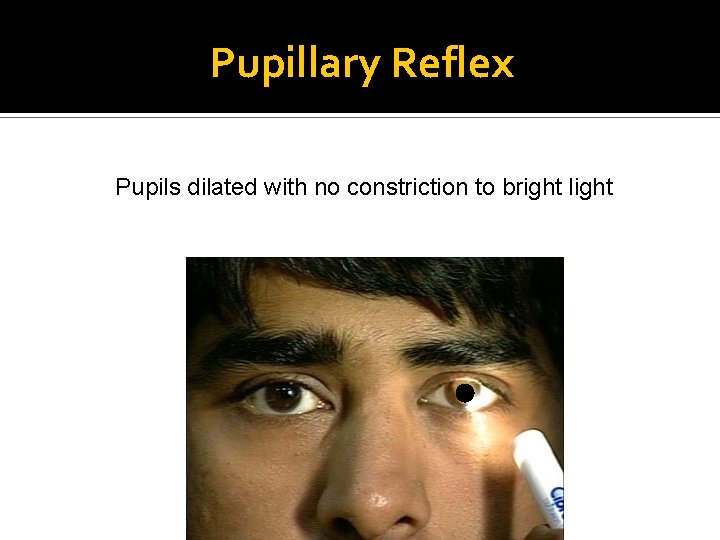
Pupillary Reflex Pupils dilated with no constriction to bright light
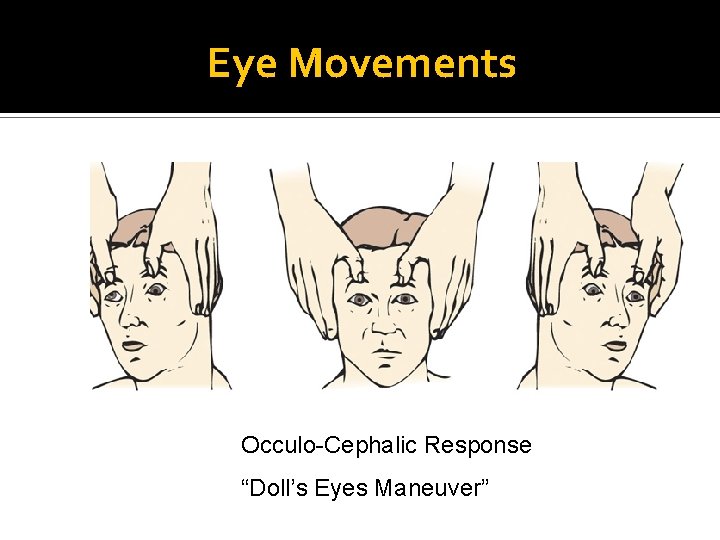
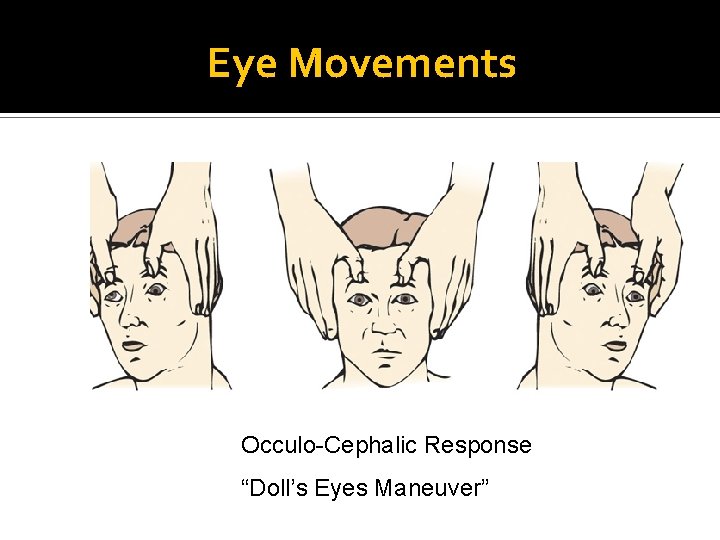
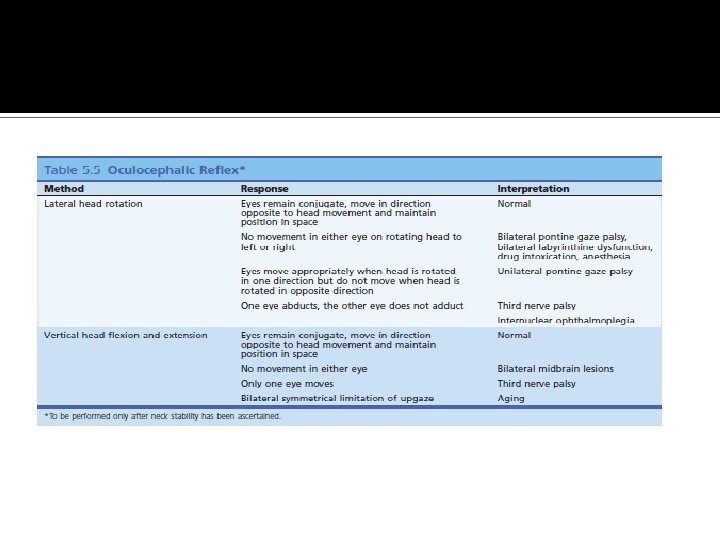
Eye Movements Occulo-Cephalic Response “Doll’s Eyes Maneuver”
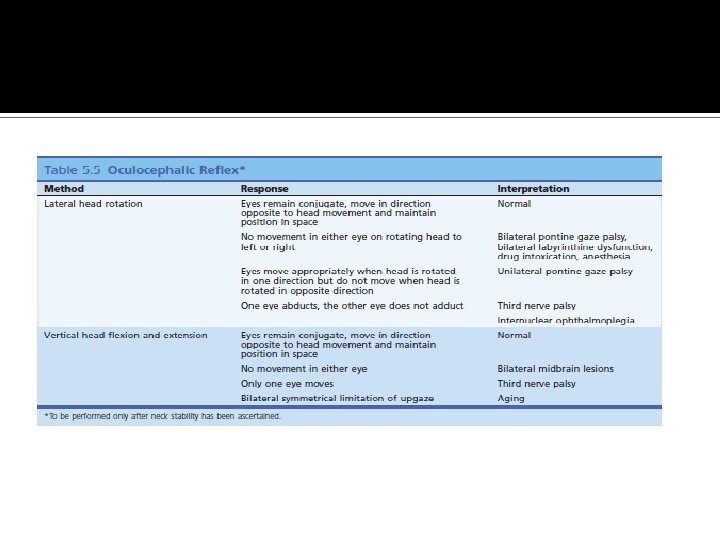

Eye Movements Oculo-Vestibular Response “Cold Caloric Testing”

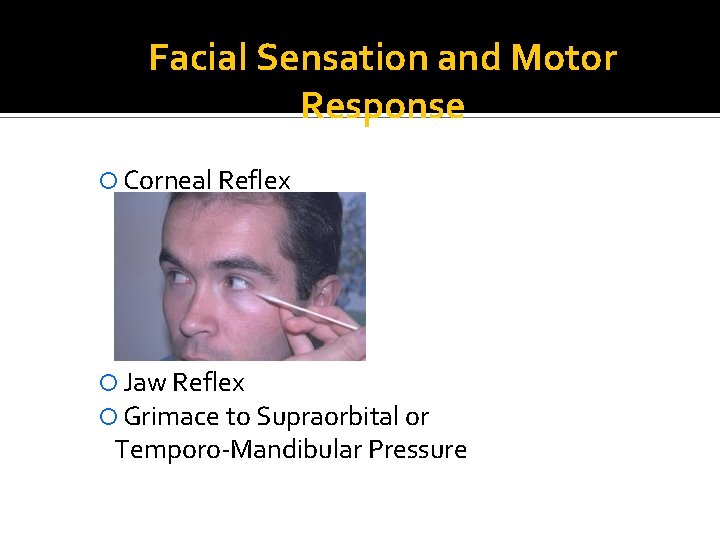
Facial Sensation and Motor Response Corneal Reflex Jaw Reflex Grimace to Supraorbital or Temporo-Mandibular Pressure

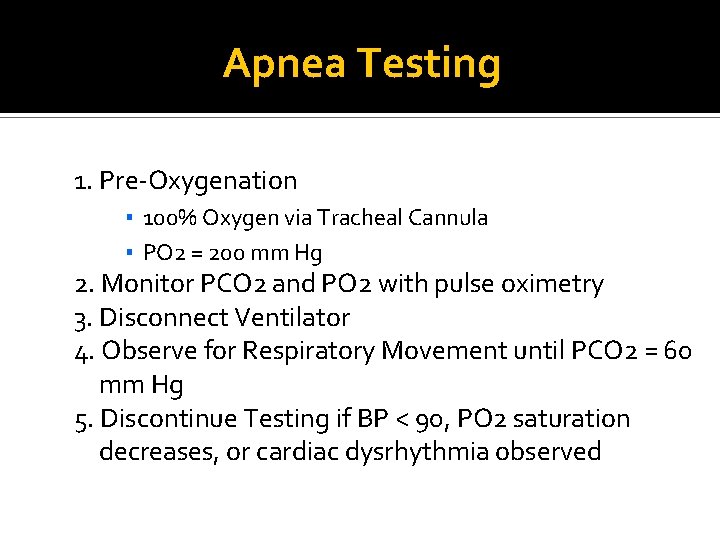
Apnea Testing Prerequisites ▪ Core Body Temperature > 32° C ▪ Systolic Blood Pressure ≥ 100 mm Hg ▪ Normal Electrolytes ▪ Normal PCO 2
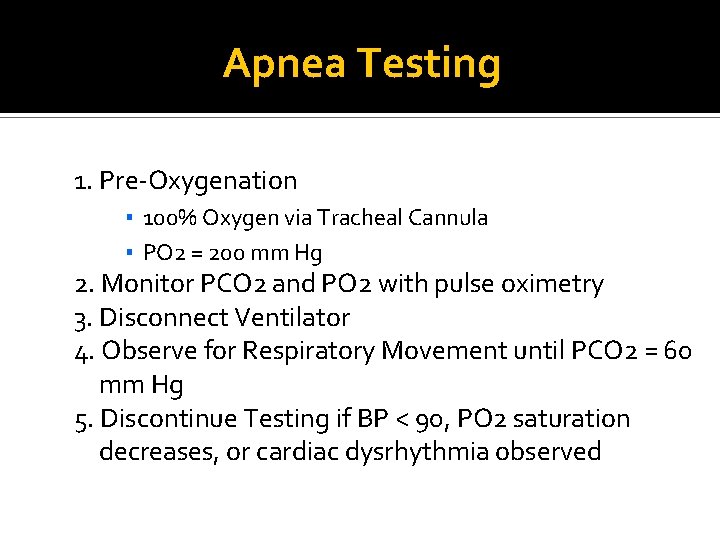
Apnea Testing 1. Pre-Oxygenation ▪ 100% Oxygen via Tracheal Cannula ▪ PO 2 = 200 mm Hg 2. Monitor PCO 2 and PO 2 with pulse oximetry 3. Disconnect Ventilator 4. Observe for Respiratory Movement until PCO 2 = 60 mm Hg 5. Discontinue Testing if BP < 90, PO 2 saturation decreases, or cardiac dysrhythmia observed
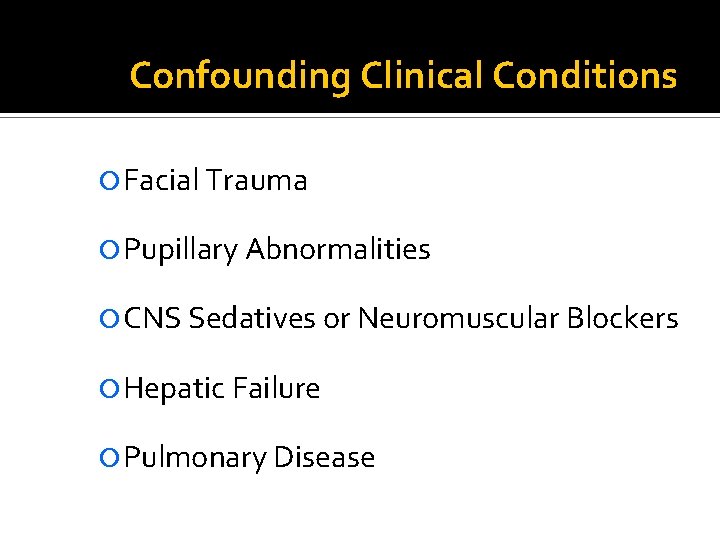
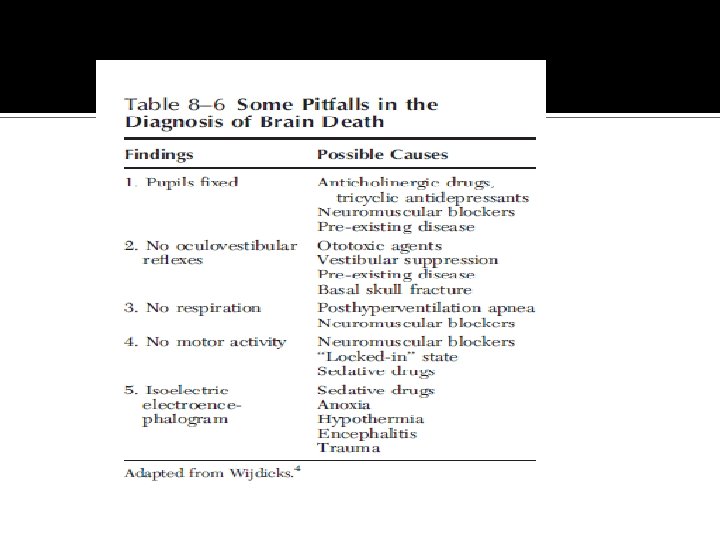
Confounding Clinical Conditions Facial Trauma Pupillary Abnormalities CNS Sedatives or Neuromuscular Blockers Hepatic Failure Pulmonary Disease
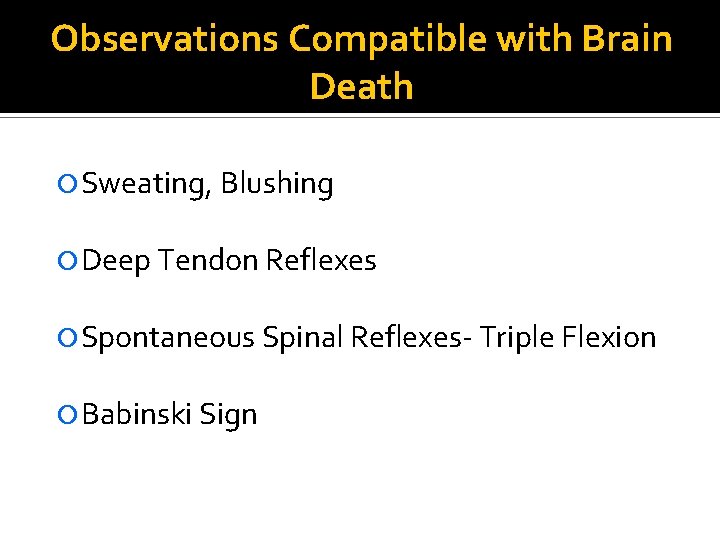
Observations Compatible with Brain Death Sweating, Blushing Deep Tendon Reflexes Spontaneous Spinal Reflexes- Triple Flexion Babinski Sign
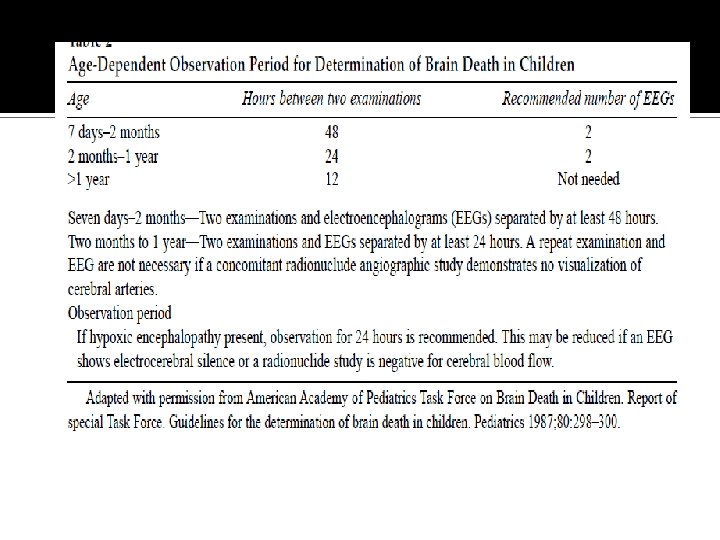
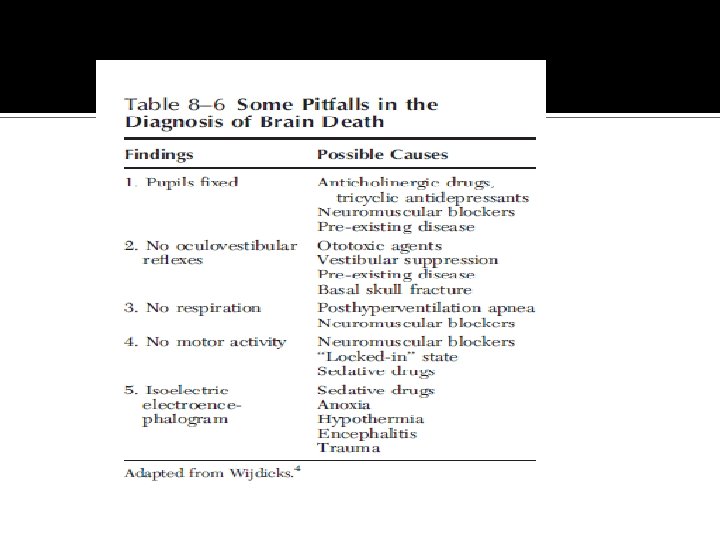
Confirmatory Testing Recommended when the proximate cause of coma is not known or when confounding clinical conditions limit the clinical examination
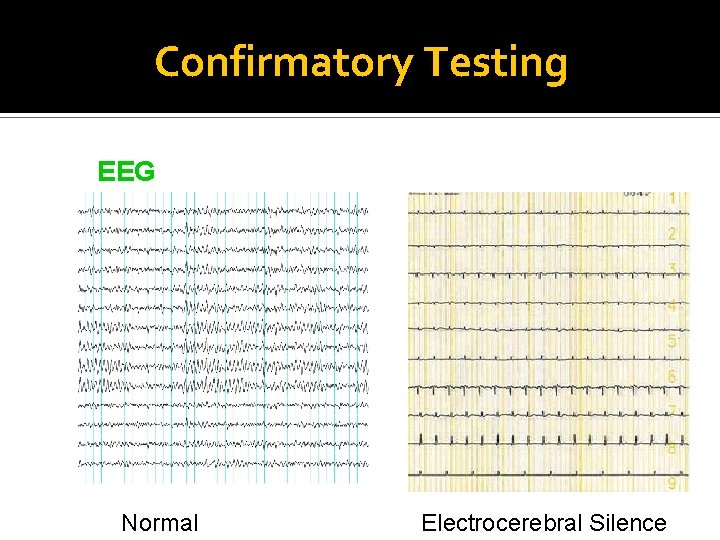
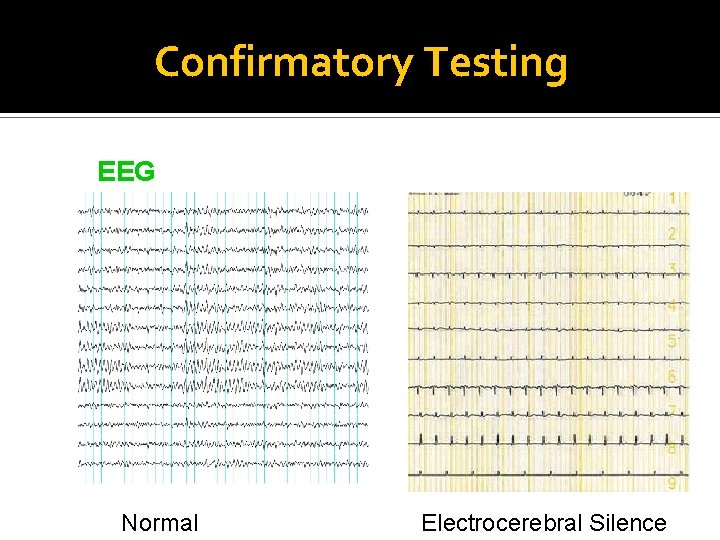
Confirmatory Testing EEG Normal Electrocerebral Silence
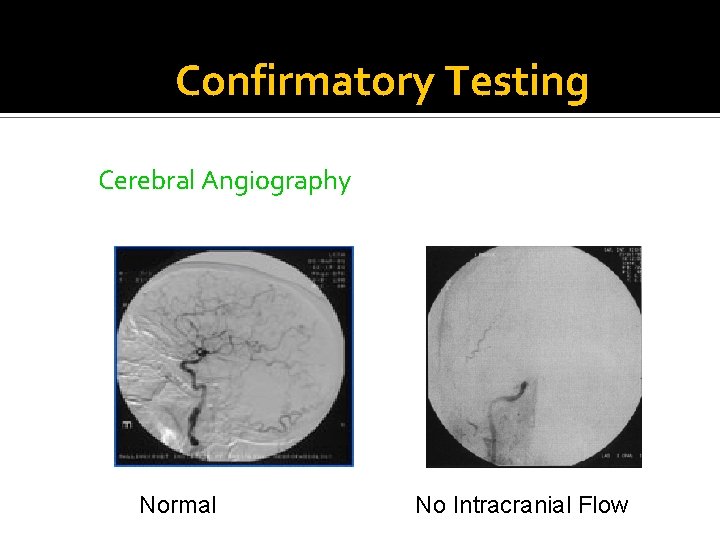
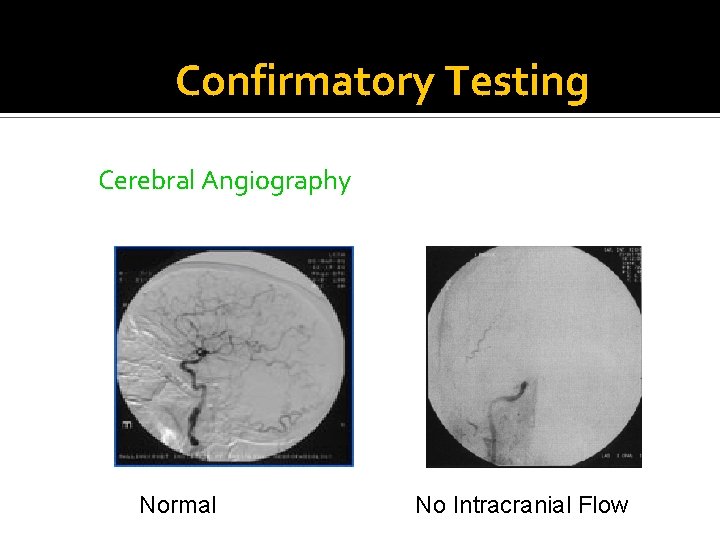
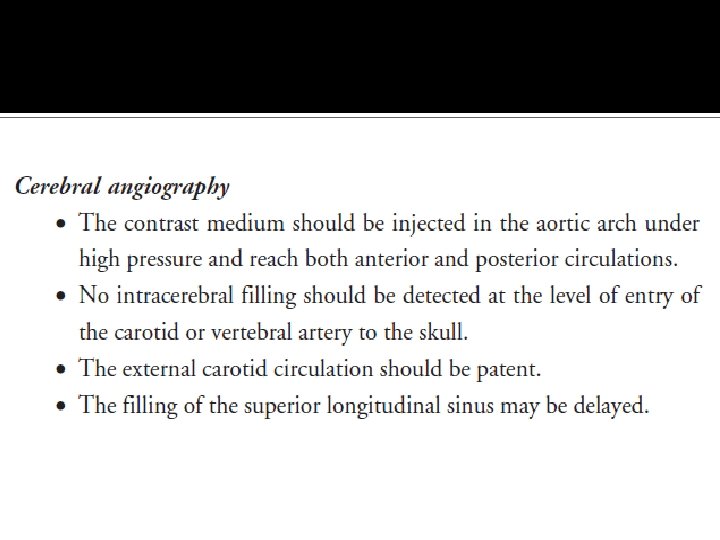
Confirmatory Testing Cerebral Angiography Normal No Intracranial Flow

Confirmatory Testing Technetium-99 Isotope Brain Scan

Confirmatory Testing MR- Angiography
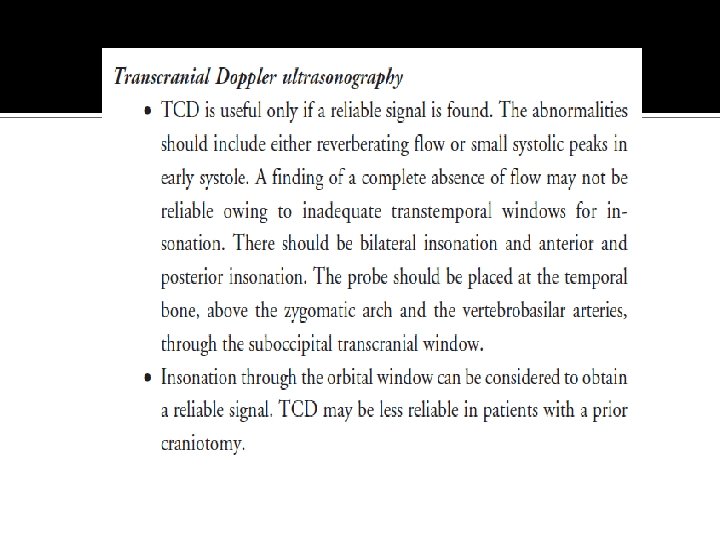
Confirmatory Testing Transcranial Ultrasonography
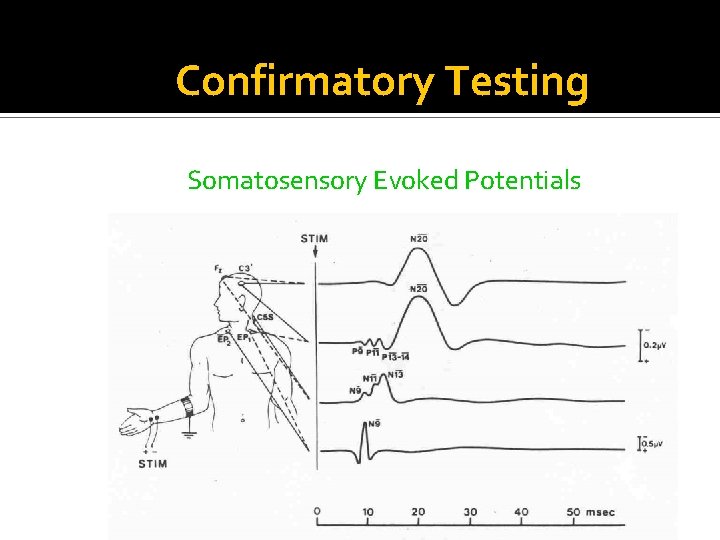
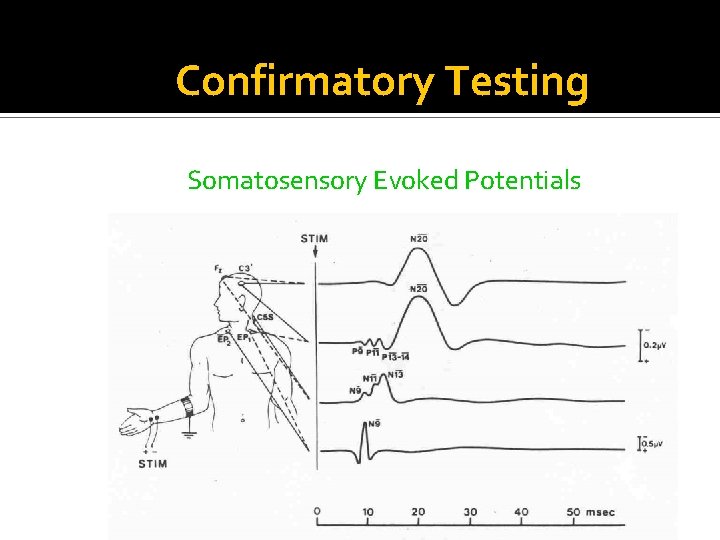
Confirmatory Testing Somatosensory Evoked Potentials

Somatosensory-evoked potentials. Bilateral absence of N 20 -P 22 response with median nerve stimulation.



THANK YOU

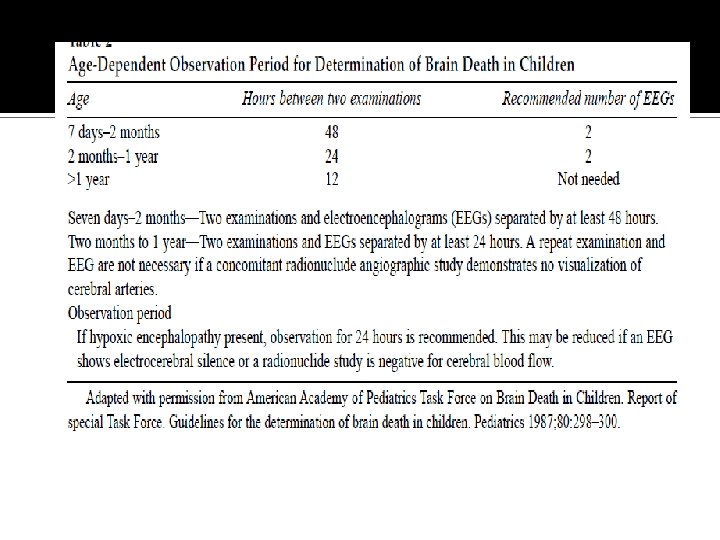
Question 1 Are there patients who fulfil the clinical criteria of brain death who recover brain function? There is insufficient evidence to determine the minimally acceptable observation period to ensure that neurologic functions have ceased irreversibly.
Question 2 What is an adequate observation period to ensure that cessation of neurologic function is permanent? There is insufficient evidence to determine the minimally acceptable observation period to ensure that neurologic functions have ceased irreversibly.
Question 3 Are complex motor movements that falsely suggest retained brain function sometimes observed in brain death? For some patients diagnosed as brain dead, complex, non– brain-mediated spontaneous movements can falsely suggest retained brain function. Additionally, ventilator autocycling may falsely suggest patient-initiated breathing.
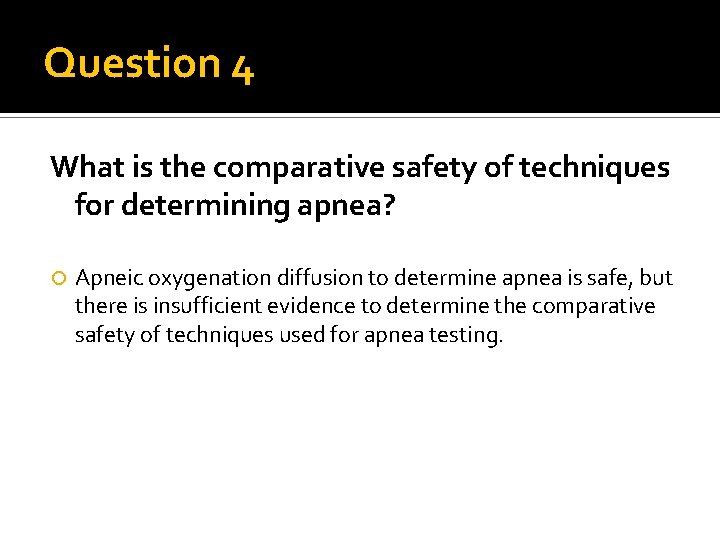
Question 4 What is the comparative safety of techniques for determining apnea? Apneic oxygenation diffusion to determine apnea is safe, but there is insufficient evidence to determine the comparative safety of techniques used for apnea testing.
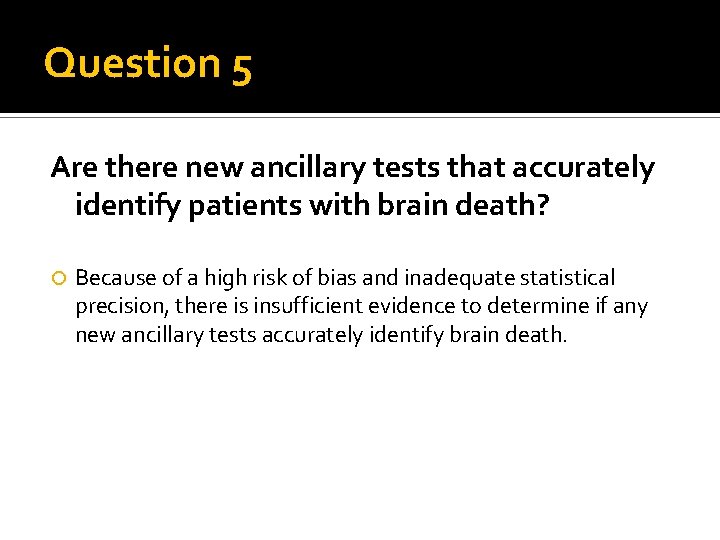
Question 5 Are there new ancillary tests that accurately identify patients with brain death? Because of a high risk of bias and inadequate statistical precision, there is insufficient evidence to determine if any new ancillary tests accurately identify brain death.
This update sought to use evidence-based methods to answer 5 QUESTIONS historically related to variations in brain death determination 4 to PROMOTE UNIFORMITY IN DIAGNOSIS.





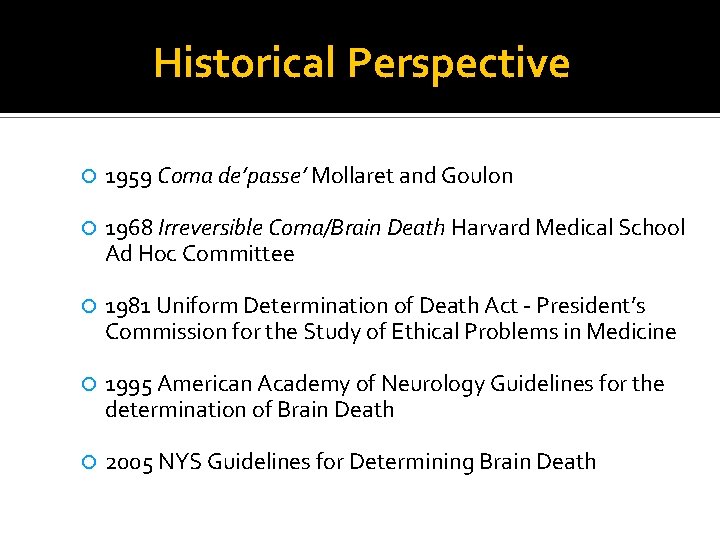
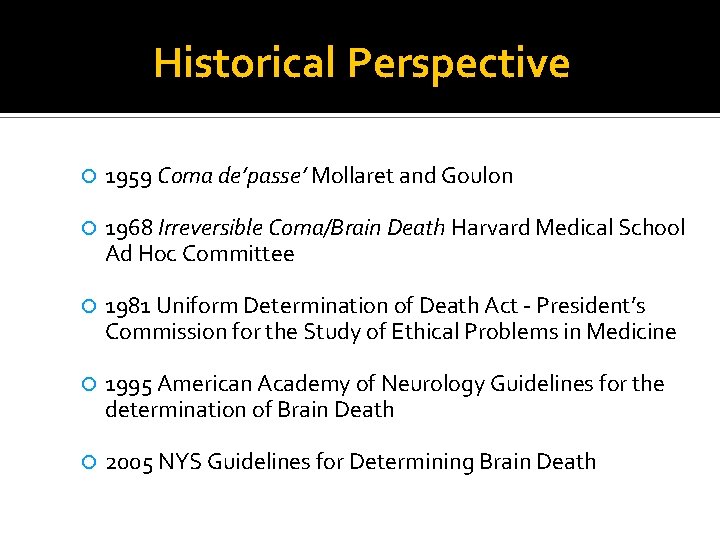
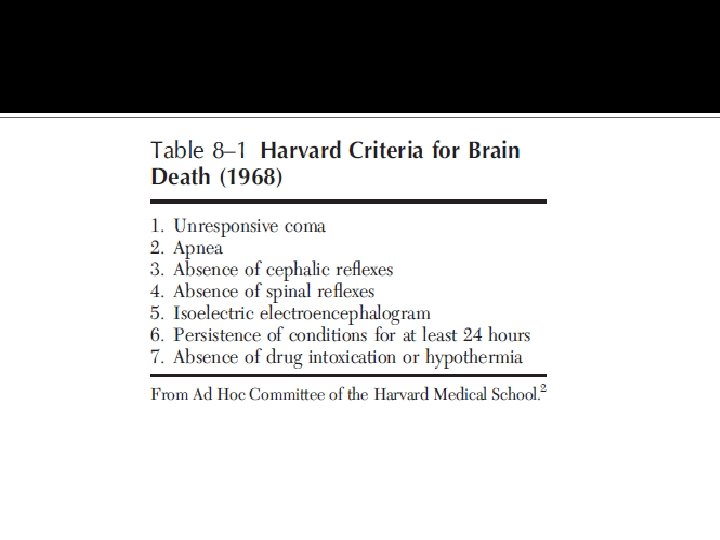
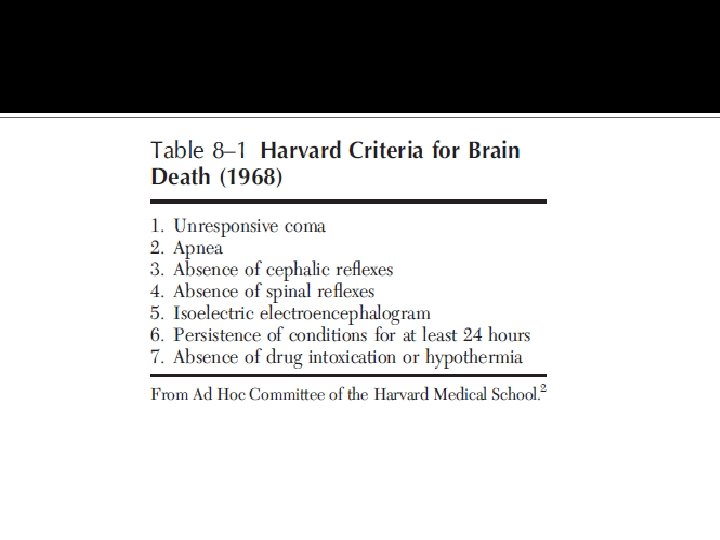
Historical Perspective 1959 Coma de’passe’ Mollaret and Goulon 1968 Irreversible Coma/Brain Death Harvard Medical School Ad Hoc Committee 1981 Uniform Determination of Death Act - President’s Commission for the Study of Ethical Problems in Medicine 1995 American Academy of Neurology Guidelines for the determination of Brain Death 2005 NYS Guidelines for Determining Brain Death
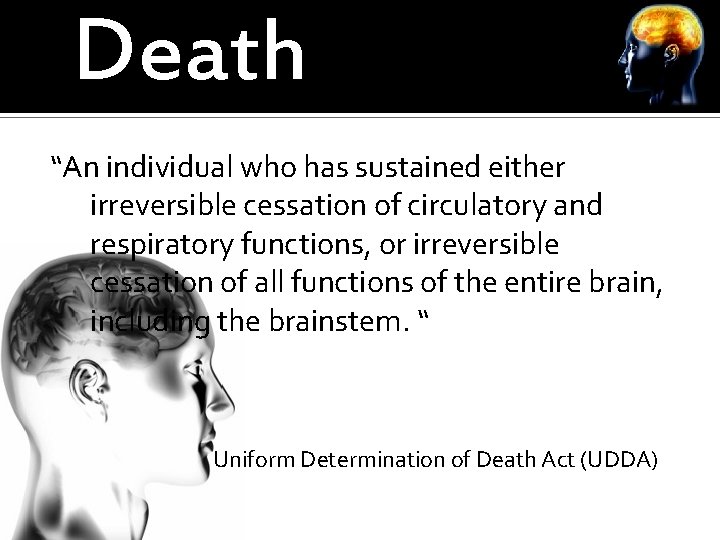
Death “An individual who has sustained either irreversible cessation of circulatory and respiratory functions, or irreversible cessation of all functions of the entire brain, including the brainstem. “ Uniform Determination of Death Act (UDDA)
A determination of death must be made with accepted medical standards The American Academy of Neurology (AAN) published a 1995 practice parameter to delineate the medical standards for the determination of brain death.
PRACTICAL (NON–EVIDENCEBASED) GUIDANCE FOR DETERMINATION OF BRAIN DEATH







 Department of neurology
Department of neurology Positive face negative face
Positive face negative face Kiran kaja
Kiran kaja Neoplasms
Neoplasms Kiran embedded
Kiran embedded Kiran ramchandani
Kiran ramchandani Define financial management
Define financial management Define decree nisi
Define decree nisi Kiran abraham
Kiran abraham Kiran fothergill
Kiran fothergill ओके गूगल
ओके गूगल Kiran mundy
Kiran mundy Shashi kiran shetty net worth
Shashi kiran shetty net worth The walton centre for neurology and neurosurgery
The walton centre for neurology and neurosurgery Neuro exam strength
Neuro exam strength Vanderbilt epilepsy monitoring unit
Vanderbilt epilepsy monitoring unit Alemutuzumab
Alemutuzumab Mary bridge pediatric neurology
Mary bridge pediatric neurology Difference between doppler and duplex
Difference between doppler and duplex Robert layzer md
Robert layzer md Obgyn shelf percentiles
Obgyn shelf percentiles Rrerl
Rrerl Nlff neurology
Nlff neurology Rachel ditrapani md
Rachel ditrapani md Dr raeburn forbes
Dr raeburn forbes Nin bajaj
Nin bajaj Joseph berger md neurology
Joseph berger md neurology Nlff neurology
Nlff neurology Nheent
Nheent Umass anesthesiology residency
Umass anesthesiology residency Midwest neurology
Midwest neurology Neurology
Neurology Oregon neurology associates
Oregon neurology associates Neurology near loomis
Neurology near loomis Tufts anesthesiology residency
Tufts anesthesiology residency Pvnt neurology
Pvnt neurology Uf neurology residency
Uf neurology residency Midwest neurology
Midwest neurology Monomyth amplification
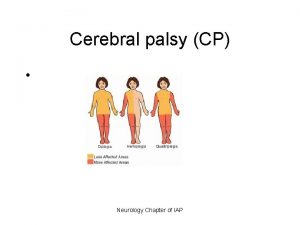
Monomyth amplification Cerebral palsy iap
Cerebral palsy iap Role of medical records
Role of medical records Medical education and drugs department
Medical education and drugs department Pasadena city college police department
Pasadena city college police department Ptal california medical board
Ptal california medical board Greater baltimore medical center medical records
Greater baltimore medical center medical records Hepburn osteometric board
Hepburn osteometric board Torrance memorial medical records
Torrance memorial medical records Cartersville medical center medical records
Cartersville medical center medical records Abu ali sina university peshawar
Abu ali sina university peshawar New york medical college interview
New york medical college interview Hawler medical university college of nursing
Hawler medical university college of nursing Google citations
Google citations Asd college college readiness program
Asd college college readiness program Early college high school at midland college
Early college high school at midland college Instrument processing optimization
Instrument processing optimization Planning strategies
Planning strategies Uta math
Uta math Swot analysis for procurement department
Swot analysis for procurement department What are four objectives of warehouse operation
What are four objectives of warehouse operation Wakulla recreation park
Wakulla recreation park Department st laghouat
Department st laghouat Undss
Undss Finance department functions
Finance department functions Bsc computer science ucl
Bsc computer science ucl Department of energy inspector general
Department of energy inspector general Tiffany taylor georgia department of education
Tiffany taylor georgia department of education What are the roles of marketing research
What are the roles of marketing research Operational plan template
Operational plan template Bloomington indiana police department
Bloomington indiana police department Aws rainfall in telangana
Aws rainfall in telangana Fire department succession planning
Fire department succession planning Rebecca corrigan olmsted township
Rebecca corrigan olmsted township Equipment
Equipment Nyc department of environmental protection
Nyc department of environmental protection State of texas emergency assistance registry
State of texas emergency assistance registry Nevada department of business and industry
Nevada department of business and industry National risk and resilience ambulance
National risk and resilience ambulance Pakistan meteorological department satellite images
Pakistan meteorological department satellite images City of san luis obispo building department
City of san luis obispo building department Amy williamson iowa
Amy williamson iowa Techniques for avoiding resource overload? *
Techniques for avoiding resource overload? * Department vs division
Department vs division Ucf io psychology
Ucf io psychology Koshwahini
Koshwahini Sierra madre planning department
Sierra madre planning department Pamlico county health department
Pamlico county health department Emergency department nursing orientation manual
Emergency department nursing orientation manual Oda
Oda Oklahoma department of career and technology education
Oklahoma department of career and technology education Division of academics department of mathematics
Division of academics department of mathematics New canaan police department
New canaan police department National core standards six priorities
National core standards six priorities Coe kfupm
Coe kfupm