Dental Pulp Disorders V ampachov Dental pulp tissue
- Slides: 50
Dental Pulp Disorders V. Žampachová
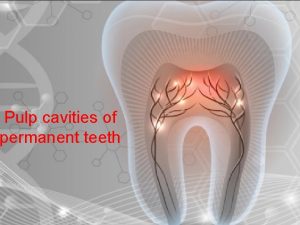
Dental pulp tissue confined to a space limited by hard tissues n no collateral circulation n biopsies or direct application of medication impossible, would lead to entire pulp necrosis n limited clinical signs – n pain, but problematic localization n level of sensitivity n
Pulpitis common inflammatory reaction n pathologic external stimuli → cytokine release → vasodilatation + edema → increased pulpal pressure in the limited space → compression of venous return → possible arterial strangulation → possible necrosis + spread n normal intrapulpal pressure 5 -20 mm Hg, n pulpitis → 60 mm Hg n
Pulpitis - causes n n n dental caries irritation thermal/chemical incl. iatrogenic trauma n n cracked tooth crown fracture traumatic pulp exposure (cavity preparation) secondary progression of periapical/periodontal inflammation from adjacent teeth
Pulpitis - etiology n n mechanical damage (trauma, dental procedure, attrition, abrasion, barotrauma) thermal injury (in dental procedures, uninsolated metallic materials) chemical irritation (in erosion, acidic dental materials), possible reactionary dentin formation. bacteria (directly in caries, haematogenous; indirectly – toxins)
Barotrauma (aerodontalgia) n n n Flying at high altitude in unpressurized aircraft, or rapid decompression in divers. Attributed to formation of nitrogen bubbles or fat emboli in pulp tissue or vessels (decompression sy). Not a direct cause, but rather an exacerbating cause in presence of caries.
Pulpitis Dynamic process with continuous spectrum of changes, depending on cause and host defenses n - Acute or chronic. - Partial or total. - Open or closed. - Exudative or suppurative. - Reversible or irreversible. n n Poor correlation between microscopic changes and clinical symptoms.
Pulpitis Modifying factors: n Nature, severity and duration of insult. n Quality of dental tissues (abrasion, attrition, . . . ) n Efficiency of host defenses. n Efficiency of pulpo-dentinal complex defenses. reactionary dentine (pulp capping, regular tubules) n reparative dentine (irregular structure) n
Pulpitis Patient history n Clinical examination n Tests n percussion n heat n cold n electric n
Pulpitis (clinical) n Acute pulpitis: Severe throbbing, lancinating pain on thermal stimulation or lying down, keeps patient awake. Generally for 10 -15 minutes (reversible pulpitis). With progression, may become spontaneous + continuous (irreversible pulpitis). n Chronic pulpitis Bouts of dull aching, an hour or more. Pain on thermal stimulation or spontaneously. May be asymptomatic.
Acute pulpitis n n n progression of focal reversible pulpitis possible exacerbation of preexisting chronic pulpitis usually pain constant, severe, localized heat/cold sensitive stage n n n early – electric hyperreactivity late – reduced/missing response commonly +/- normal percussion test
Chronic pulpitis n n low grade, long term injury intermittent, mild symptoms n n no symptoms possible reduced response to stimulation
Pulpitis Most important decision clinically is whether pulpitis is reversible or irreversible → different management. n Decision based on many factors including: n Severity of symptoms. n Duration of symptoms. n Size of carious lesion. n Pulp tests. n Direct observation during operative procedure. n Age of the patient. n
Pulpitis - signs n reversible – possible regeneration; sudden short pain in local thermal and/or chemical stimuli (cold, sweet, sour); no percussion sensitivity, no change in radiograph n irreversible – no regeneration, common bacterial invasion n n early – longer, more intensive pain, may be continuous; still may be localised late – severe continuous pain, radiation to jaw, face, neck, … (trigeminal irritation)
Reversible pulpitis n Clinical examination: n intermittent pain n vitality test: positive, „short” response n Focal change, acute n Treatment: copy n removing of the offending agent n making a filling (or pulp capping)
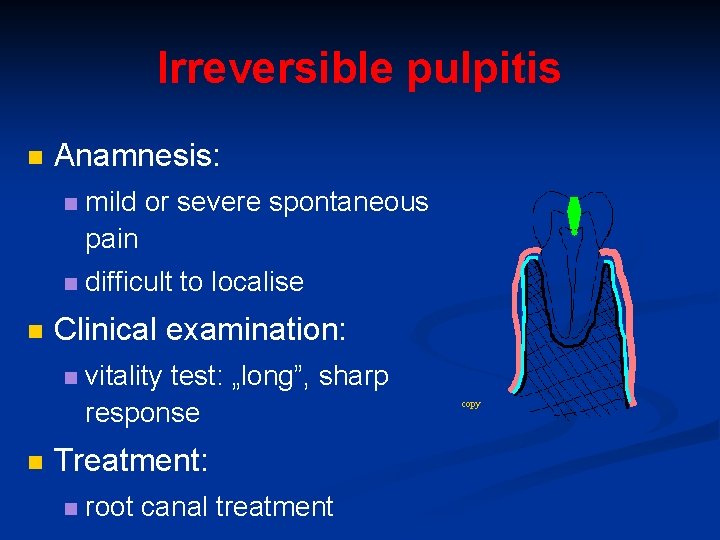
Irreversible pulpitis n n Anamnesis: n mild or severe spontaneous pain n difficult to localise Clinical examination: n n vitality test: „long”, sharp response Treatment: n root canal treatment copy
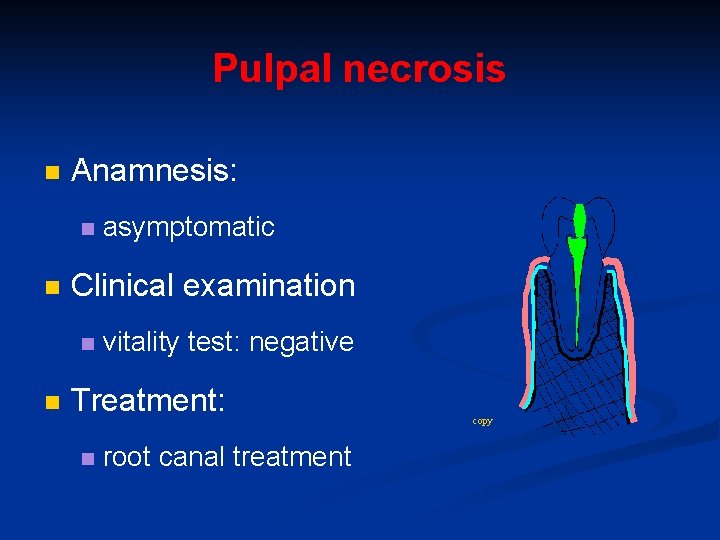
Pulpal necrosis n Anamnesis: n n Clinical examination n n asymptomatic vitality test: negative Treatment: n root canal treatment copy
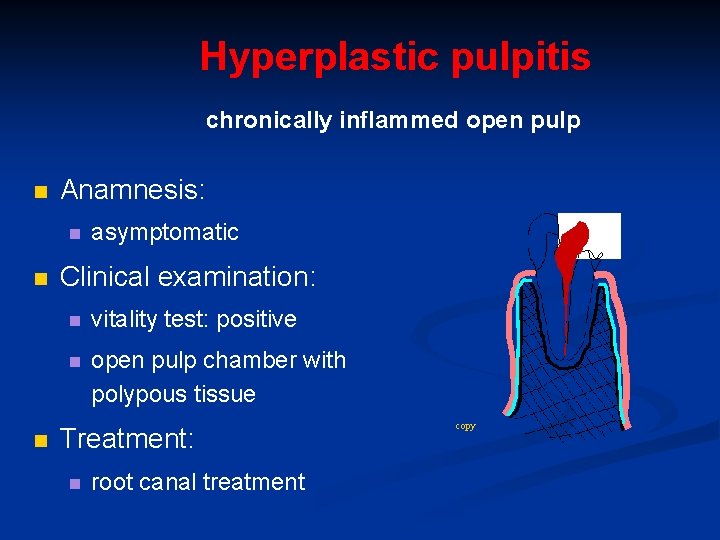
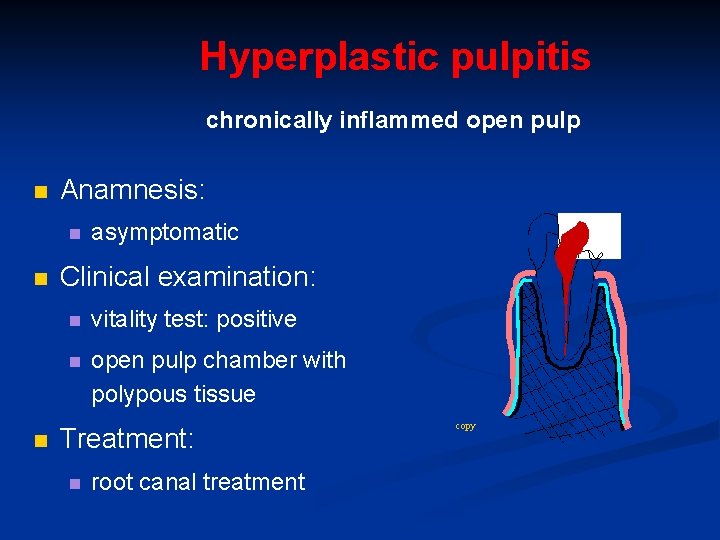
Hyperplastic pulpitis chronically inflammed open pulp n Anamnesis: n n n asymptomatic Clinical examination: n vitality test: positive n open pulp chamber with polypous tissue Treatment: n root canal treatment copy
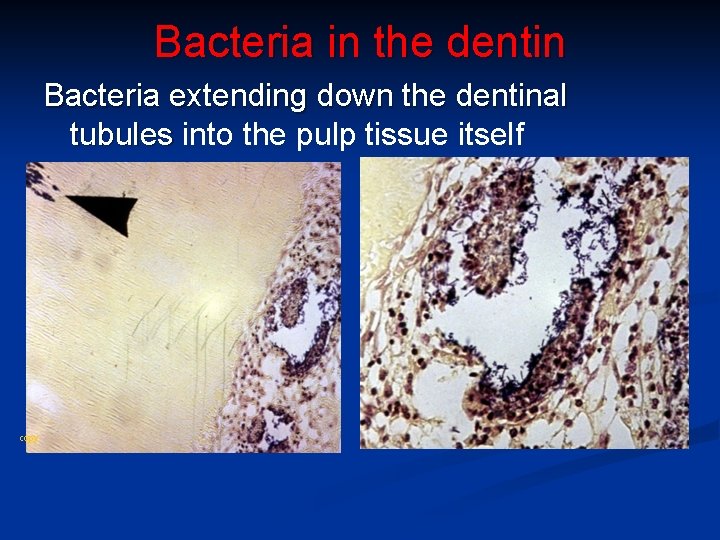
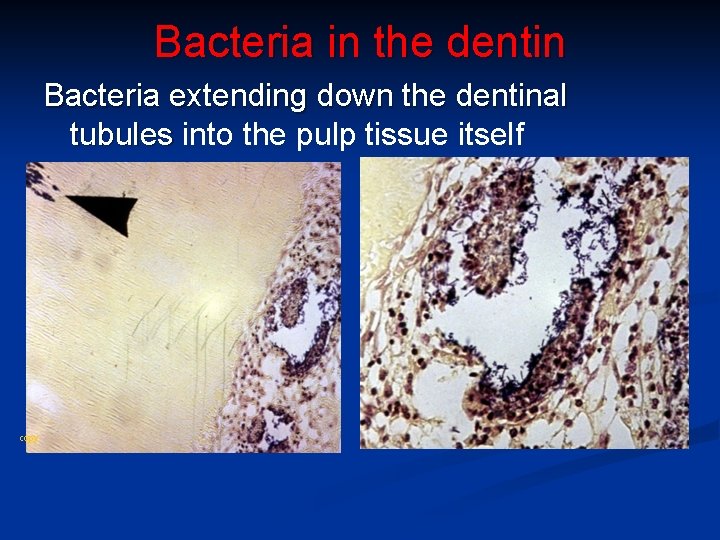
Bacteria in the dentin Bacteria extending down the dentinal tubules into the pulp tissue itself copy
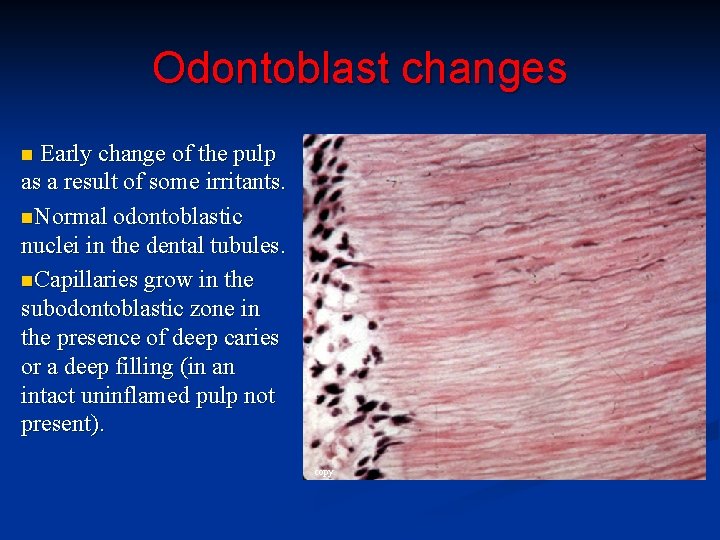
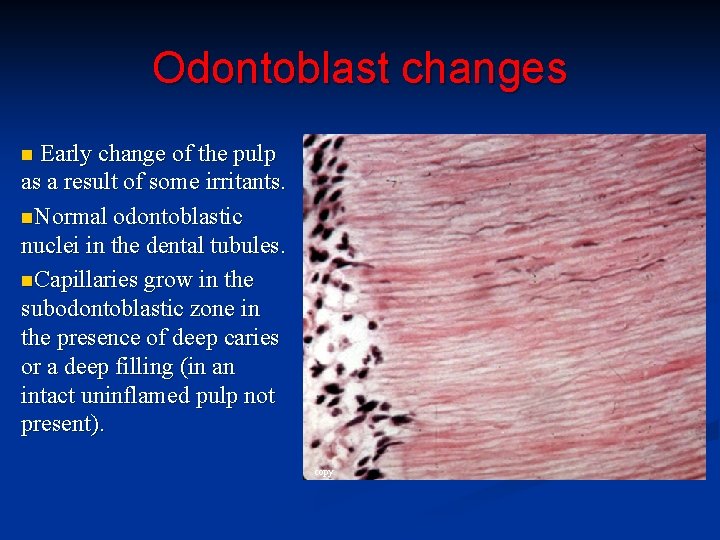
Odontoblast changes Early change of the pulp as a result of some irritants. n. Normal odontoblastic nuclei in the dental tubules. n. Capillaries grow in the subodontoblastic zone in the presence of deep caries or a deep filling (in an intact uninflamed pulp not present). n copy
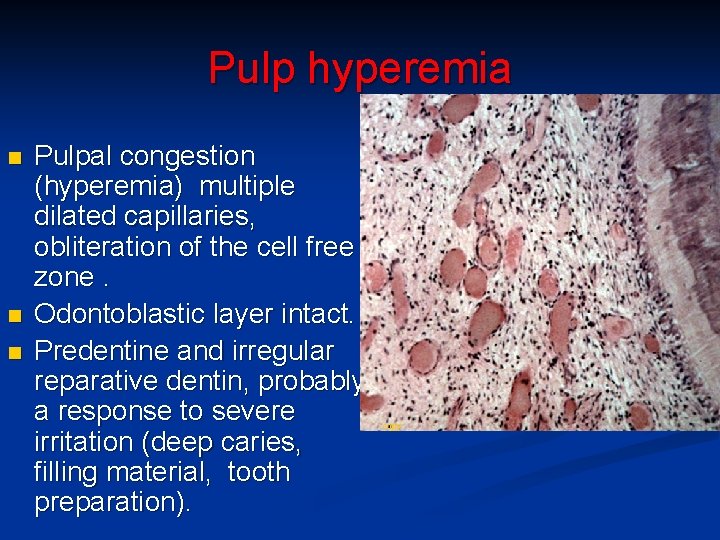
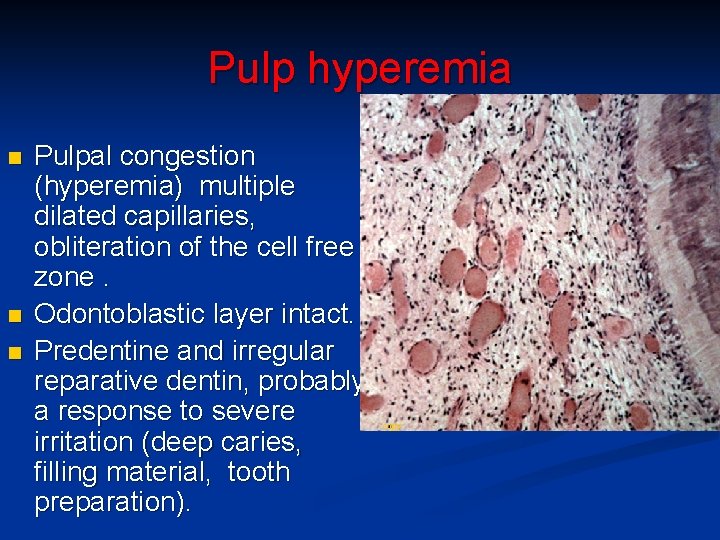
Pulp hyperemia n n n Pulpal congestion (hyperemia) multiple dilated capillaries, obliteration of the cell free zone. Odontoblastic layer intact. Predentine and irregular reparative dentin, probably a response to severe irritation (deep caries, filling material, tooth preparation). copy
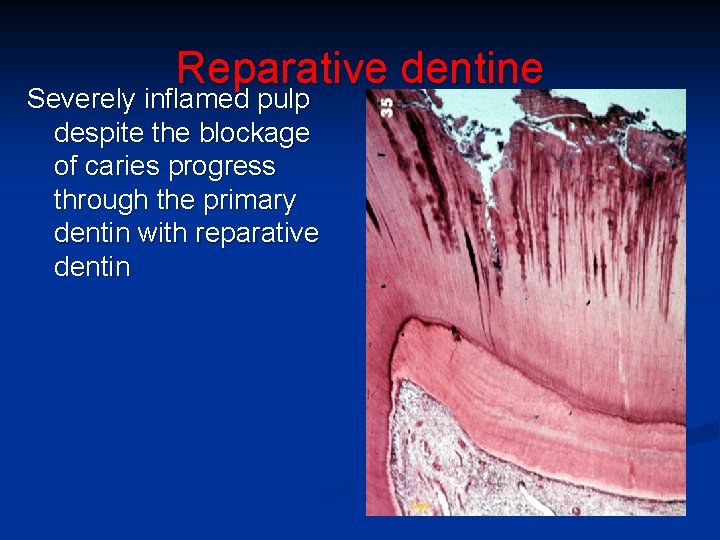
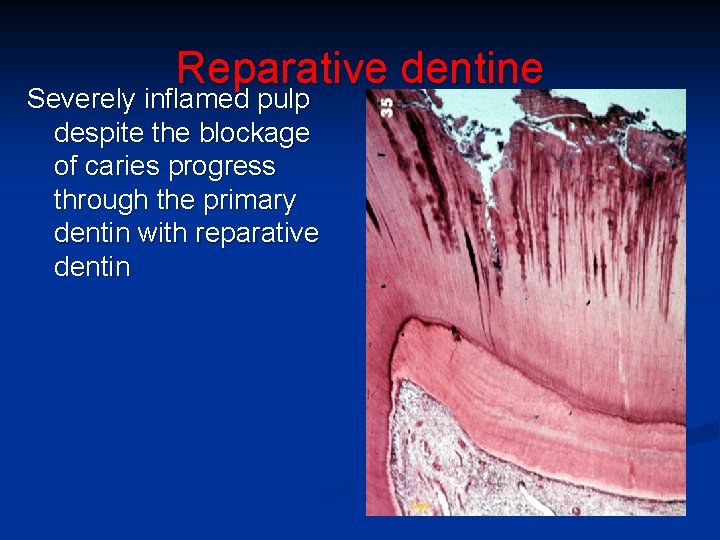
Reparative dentine Severely inflamed pulp despite the blockage of caries progress through the primary dentin with reparative dentin copy
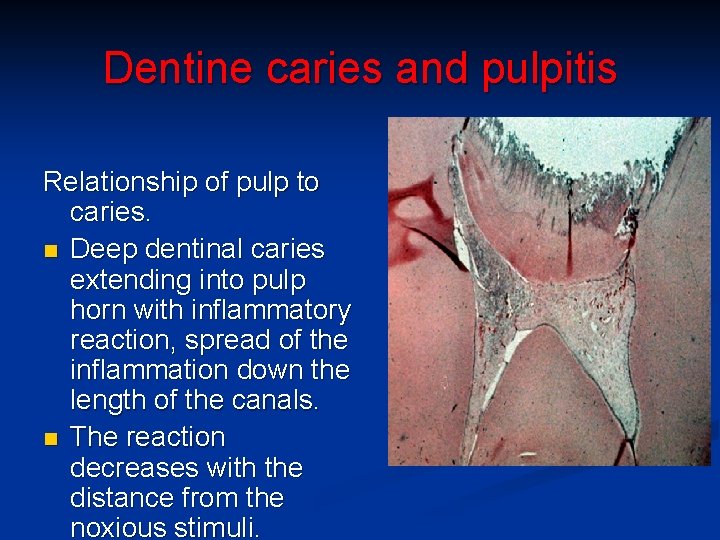
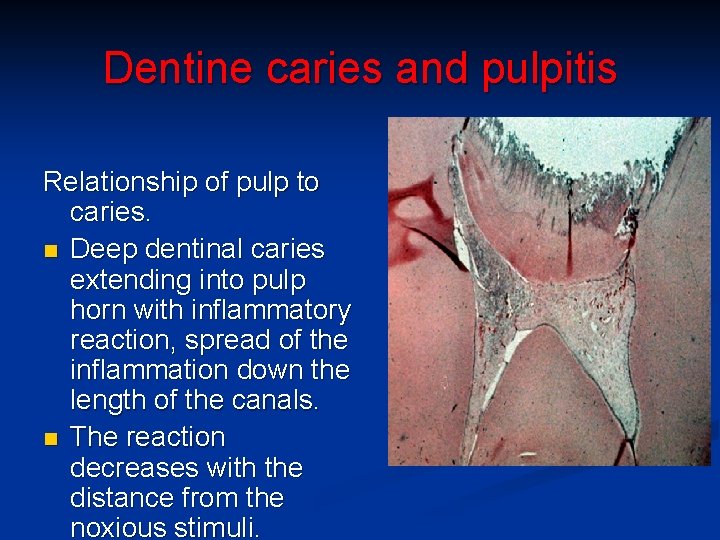
Dentine caries and pulpitis Relationship of pulp to caries. n Deep dentinal caries extending into pulp horn with inflammatory reaction, spread of the inflammation down the length of the canals. n The reaction decreases with the distance from the noxious stimuli.
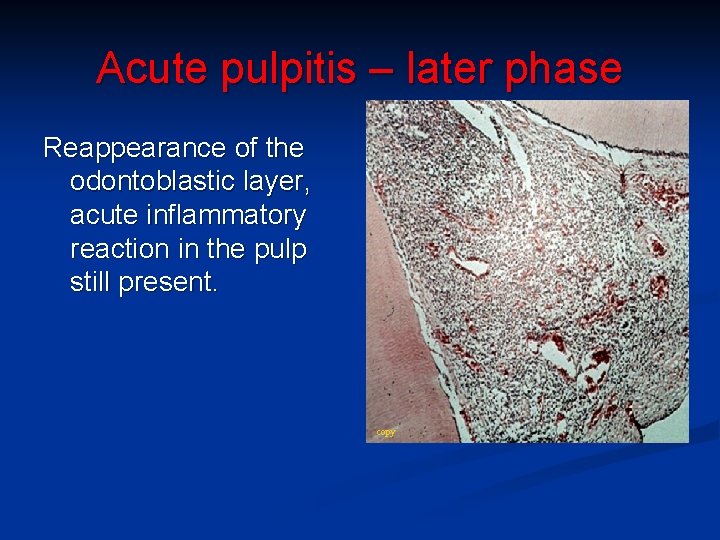
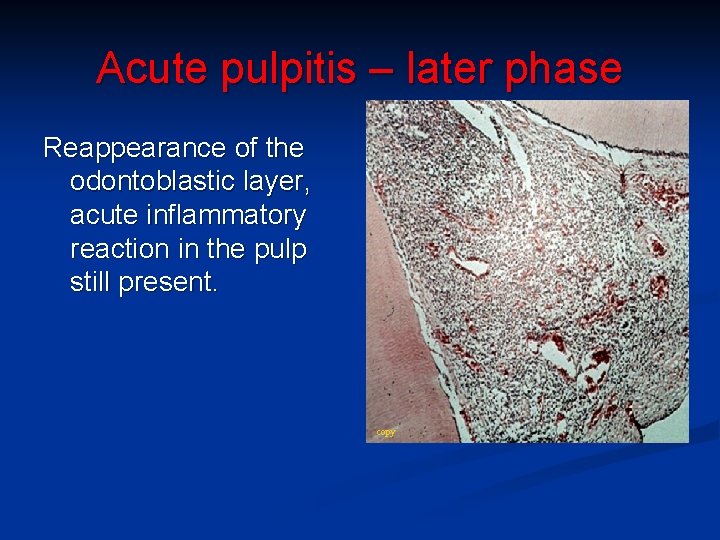
Acute pulpitis – later phase Reappearance of the odontoblastic layer, acute inflammatory reaction in the pulp still present. copy
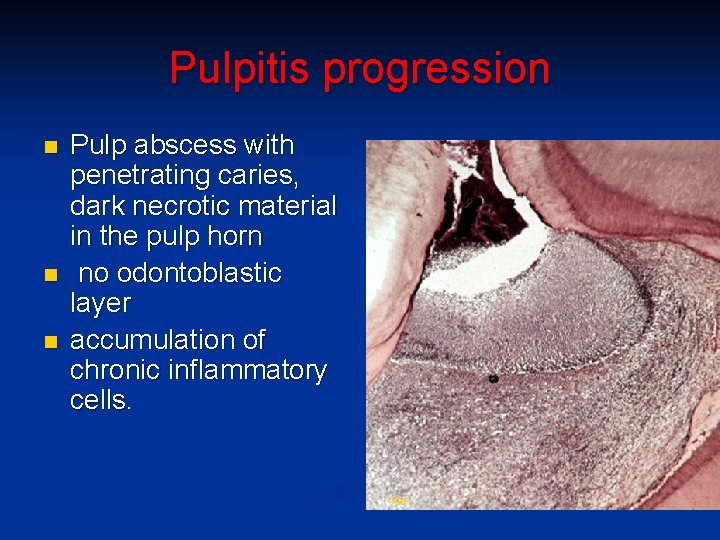
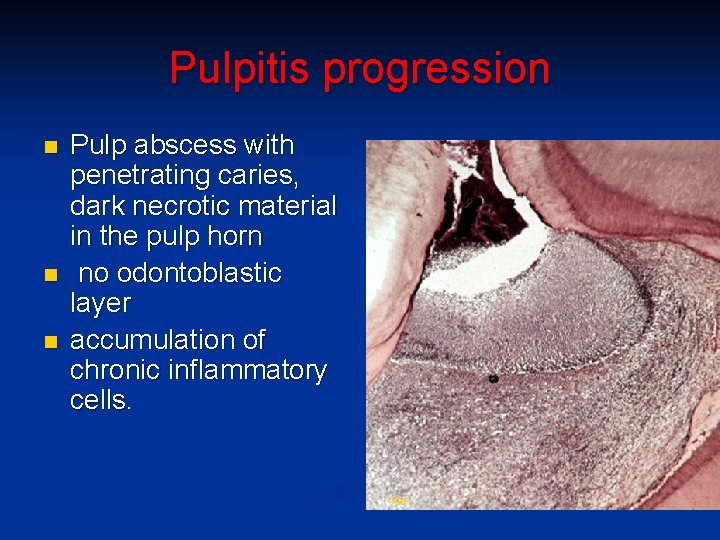
Pulpitis progression n Pulp abscess with penetrating caries, dark necrotic material in the pulp horn no odontoblastic layer accumulation of chronic inflammatory cells. copy
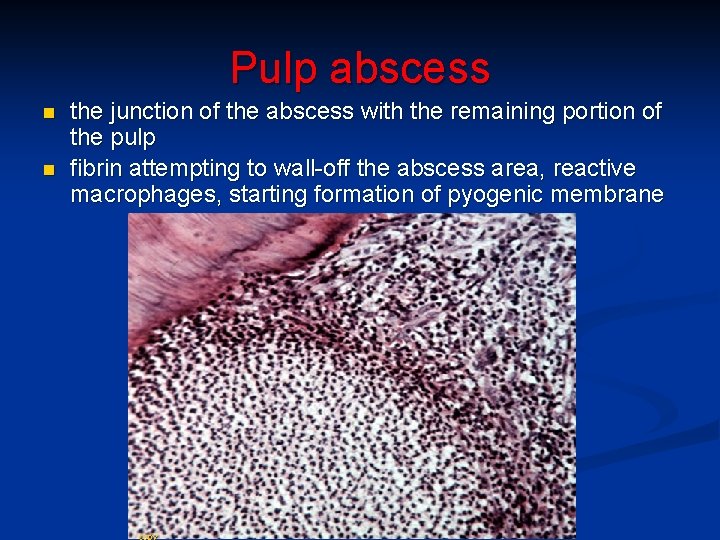
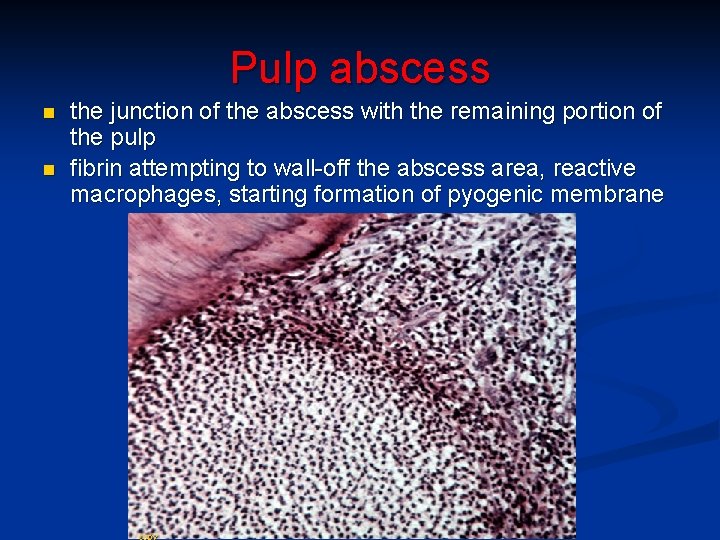
Pulp abscess n n the junction of the abscess with the remaining portion of the pulp fibrin attempting to wall-off the abscess area, reactive macrophages, starting formation of pyogenic membrane
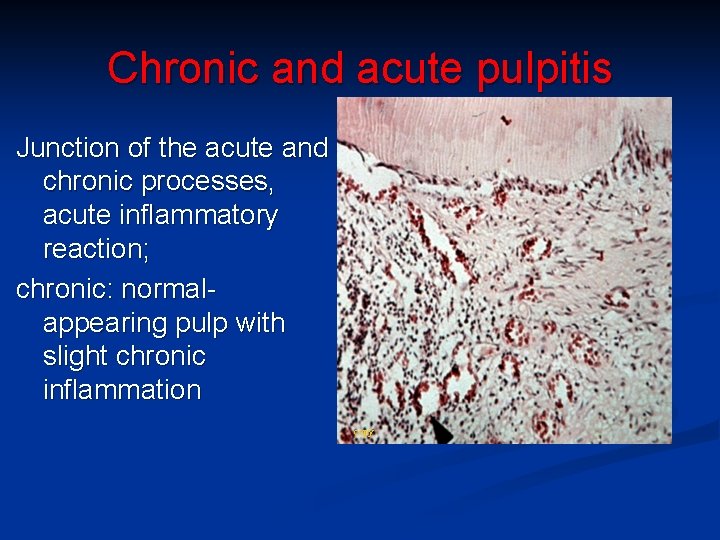
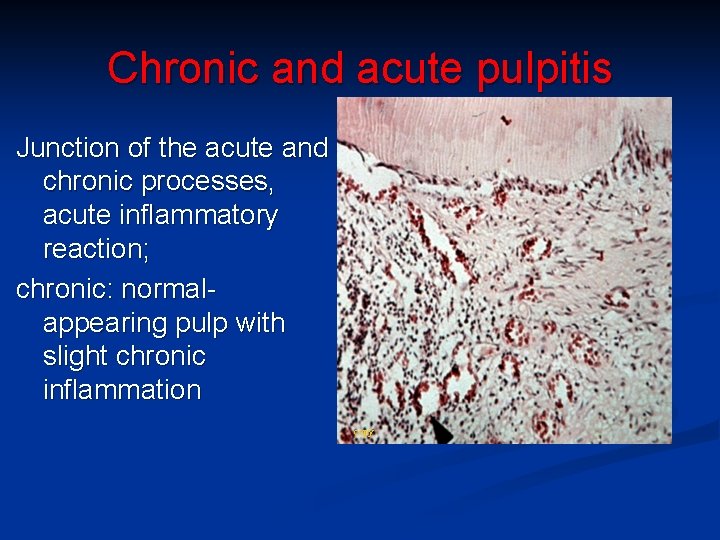
Chronic and acute pulpitis Junction of the acute and chronic processes, acute inflammatory reaction; chronic: normalappearing pulp with slight chronic inflammation copy
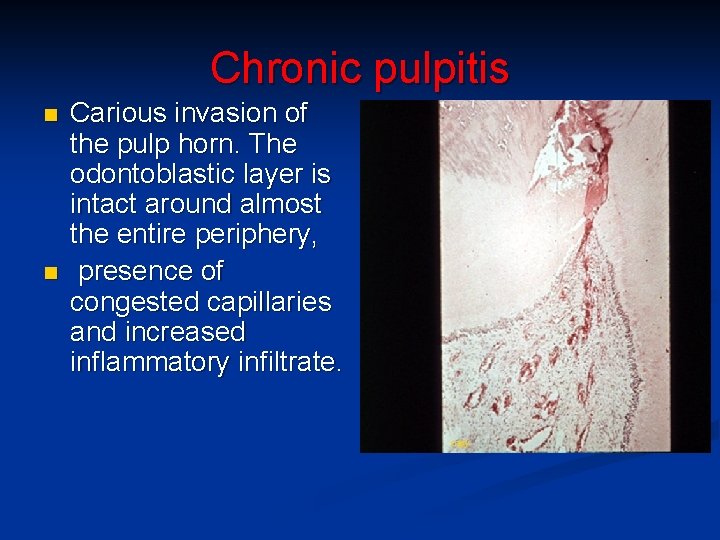
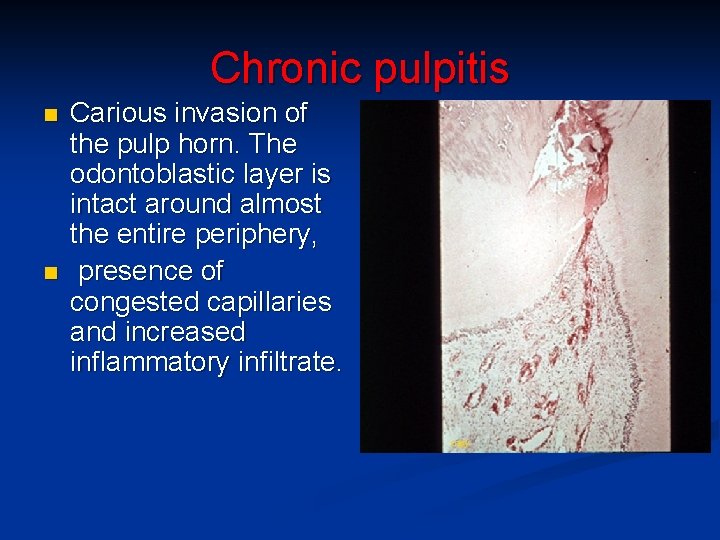
Chronic pulpitis n n Carious invasion of the pulp horn. The odontoblastic layer is intact around almost the entire periphery, presence of congested capillaries and increased inflammatory infiltrate. copy
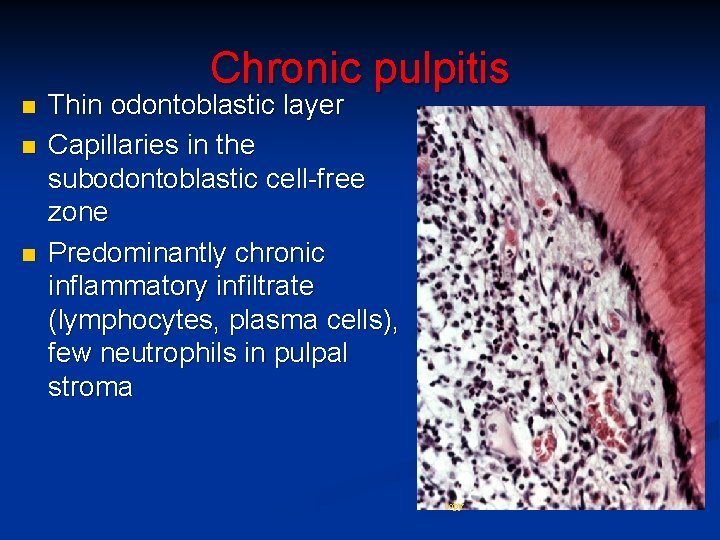
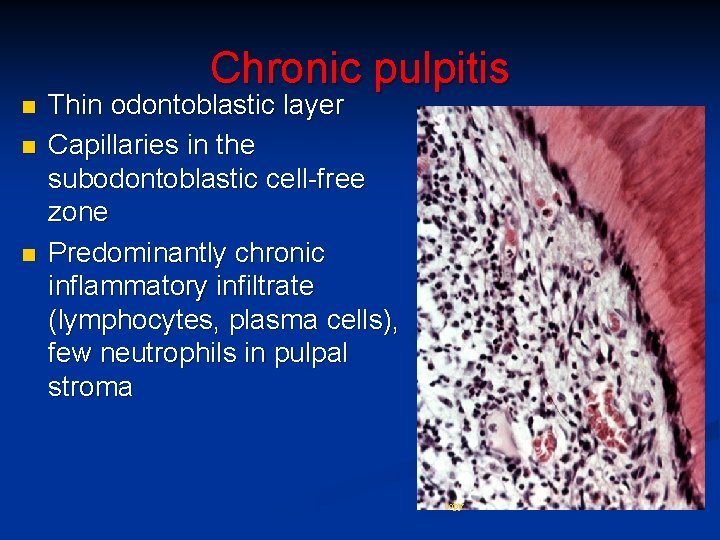
Chronic pulpitis n n n Thin odontoblastic layer Capillaries in the subodontoblastic cell-free zone Predominantly chronic inflammatory infiltrate (lymphocytes, plasma cells), few neutrophils in pulpal stroma copy
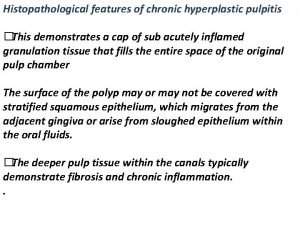
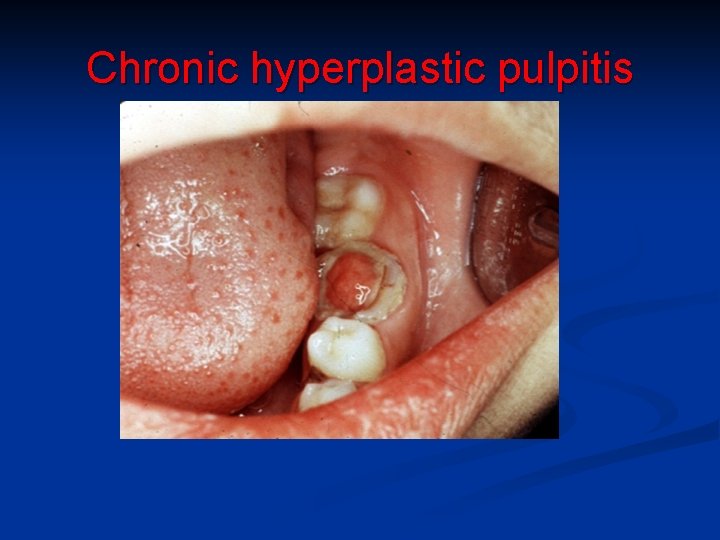
Chronic hyperplastic pulpitis n n n in children, young adults large open pulp chambers (molars), dentinal defect, wide apices and good blood supply large carious cavities proliferation + protrusion of granulation tissue possible epithelialization by spontaneous grafting of desquamated oral epithelial cells from saliva. commonly asymptomatic, if ulcerated may bleed
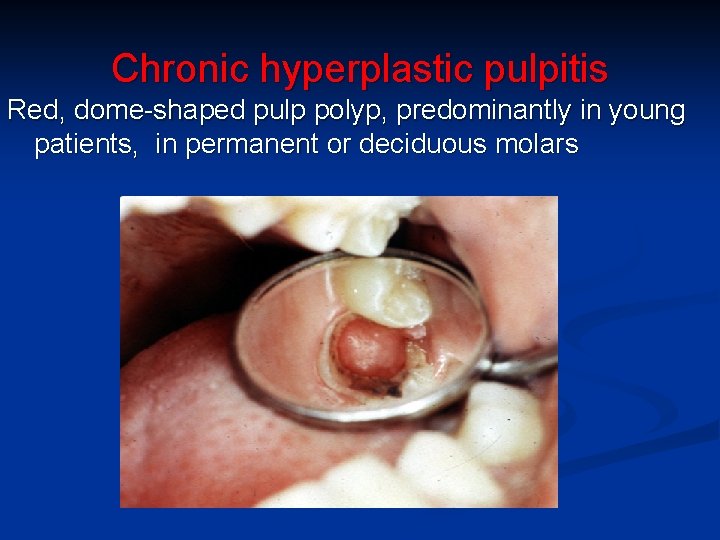
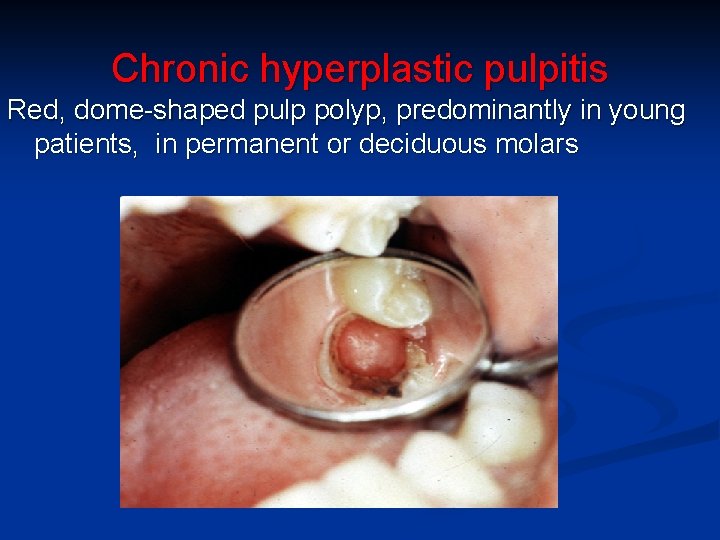
Chronic hyperplastic pulpitis Red, dome-shaped pulp polyp, predominantly in young patients, in permanent or deciduous molars
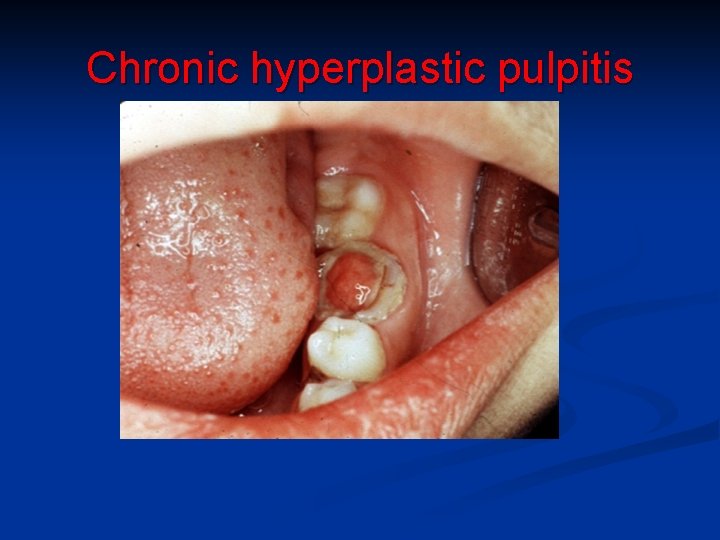
Chronic hyperplastic pulpitis
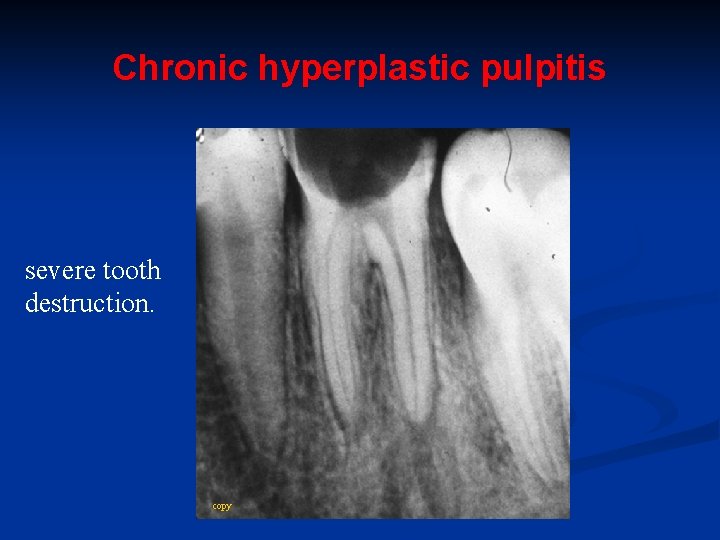
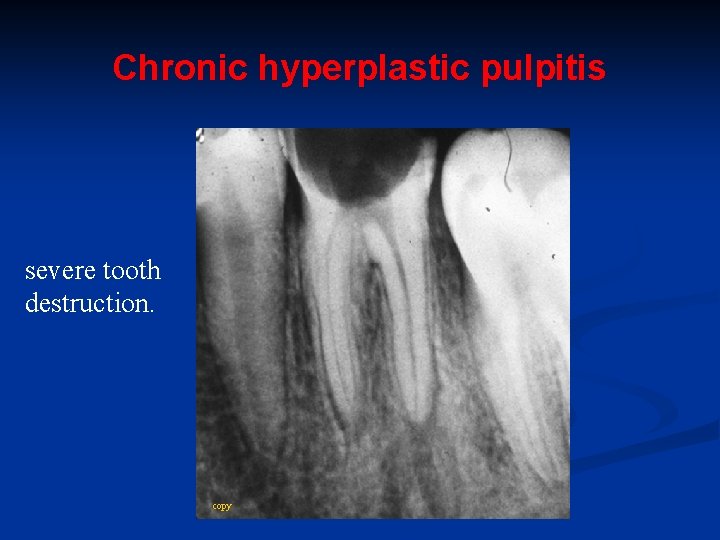
Chronic hyperplastic pulpitis severe tooth destruction. copy
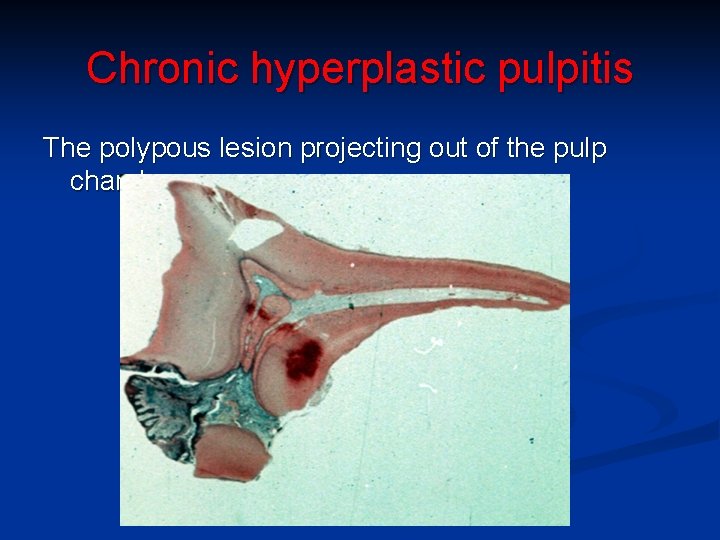
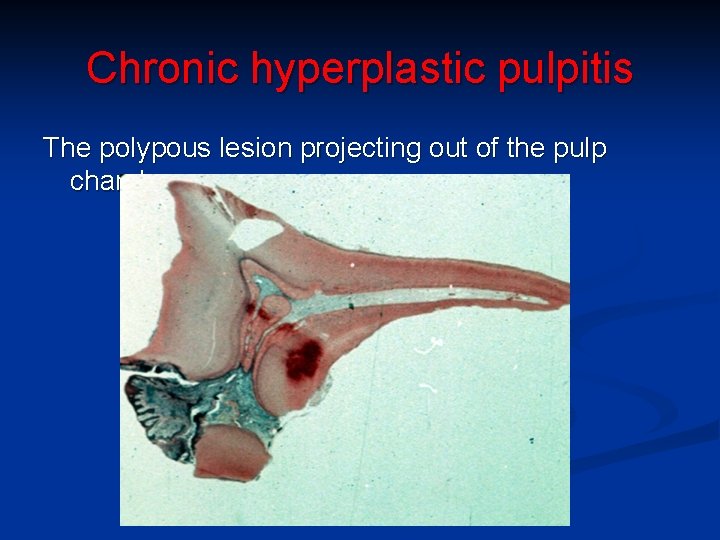
Chronic hyperplastic pulpitis The polypous lesion projecting out of the pulp chamber.
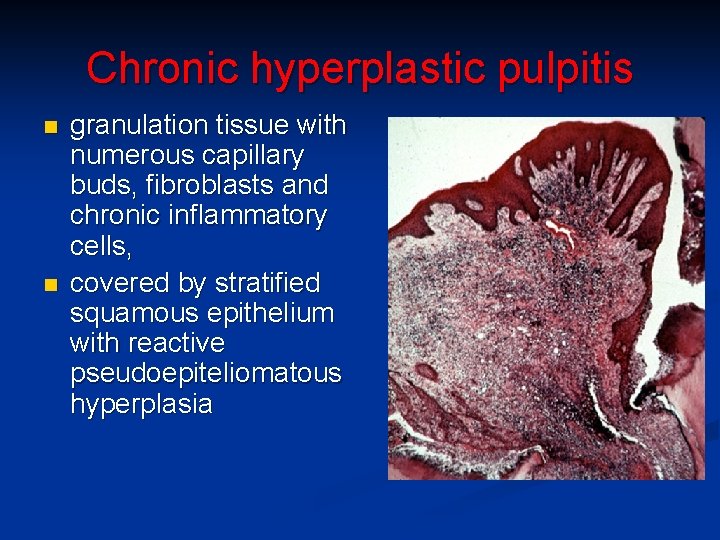
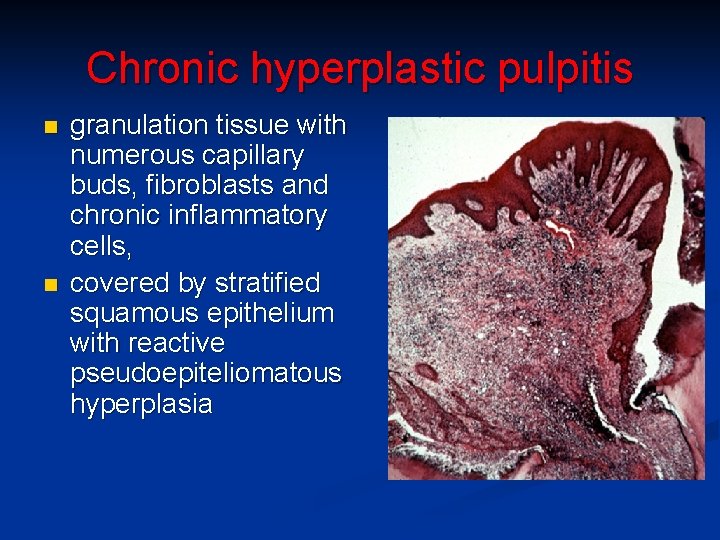
Chronic hyperplastic pulpitis n n granulation tissue with numerous capillary buds, fibroblasts and chronic inflammatory cells, covered by stratified squamous epithelium with reactive pseudoepiteliomatous hyperplasia
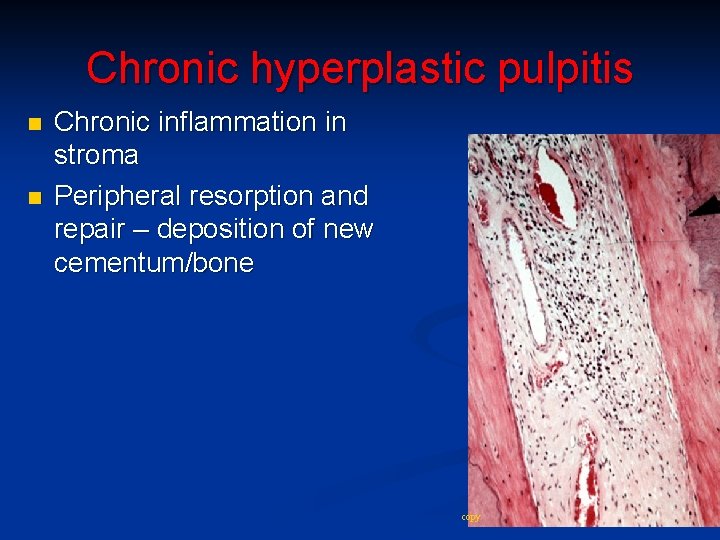
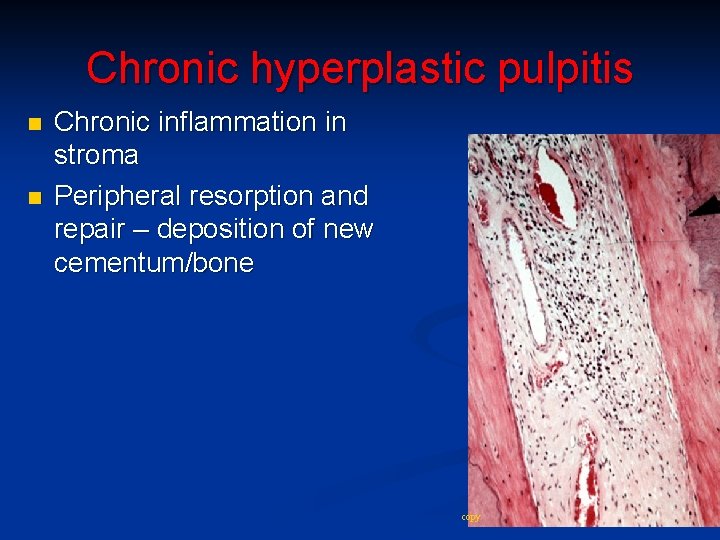
Chronic hyperplastic pulpitis n n Chronic inflammation in stroma Peripheral resorption and repair – deposition of new cementum/bone copy
Effects of cavity preparation and restorative materials n n Cavity preparation: speed, heat, pressure and coolant may all cause pulp irritation. Aspiration or displacement of odontoblasts into dentinal tubules, with reduction of numbers (dead tracts). Possible further complications of pulpitis caused by caries or other causes. Thickness and nature (quality, opened tubules) of remaining dentin may affect pulp response to dental material.
Pulp healing n n n Injured odontoblasts replaced by new cells from pulp. Pulpitis may resolve after removal of irritant. It may resolve due to reactionary dentine formation even without removal of caries. Pulp capping after traumatic pulp exposure or pulpotomy: calcium hydroxide agents – high p. H, kill bacteria, stimulate formation of a calcified barrier (dentin). Variable barrier quality, possible leakage of toxins
Pulp calcification n n n ~20% on X-ray (size>200 μm) Pulp stones (denticles): calcified bodies, organic matrix true – developmental, with tubules + odontoblasts, possible covering of predentin false - concentric calcifications growth with age (number, size), in trauma or caries usually asymptomatic
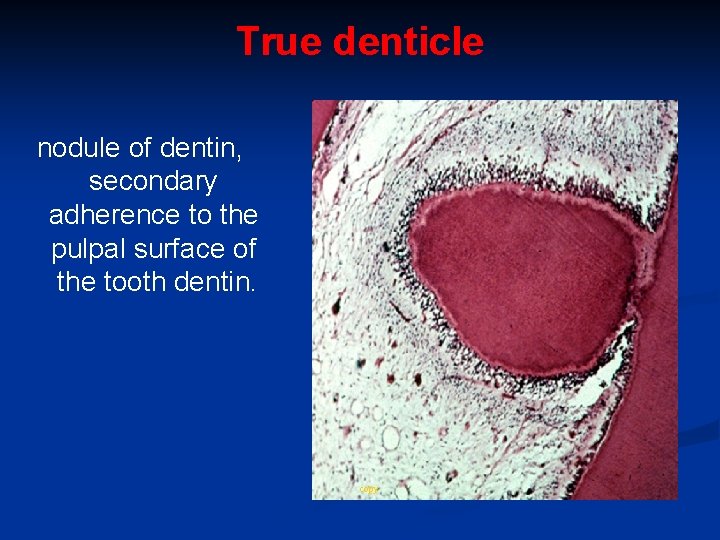
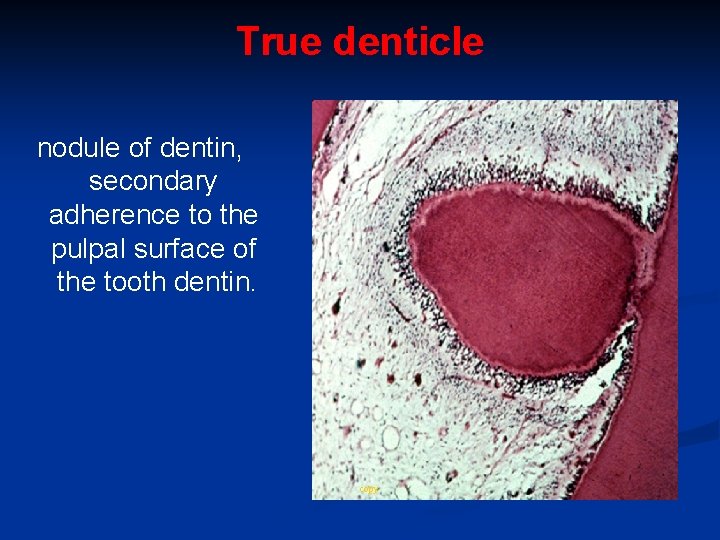
True denticle nodule of dentin, secondary adherence to the pulpal surface of the tooth dentin. copy
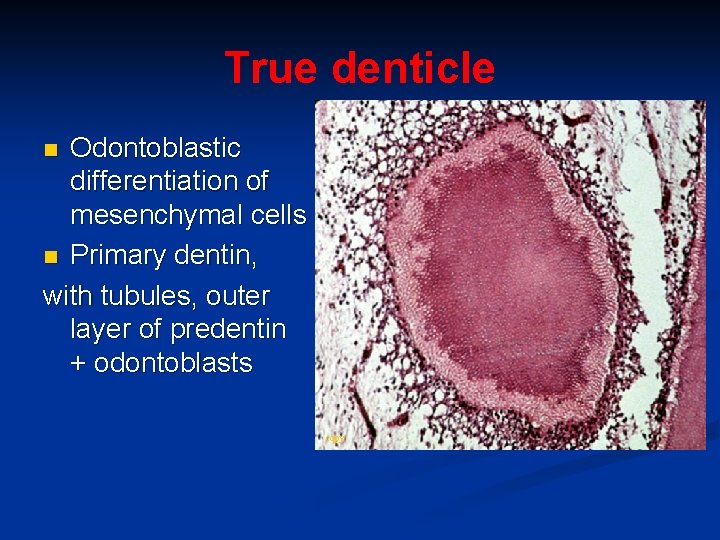
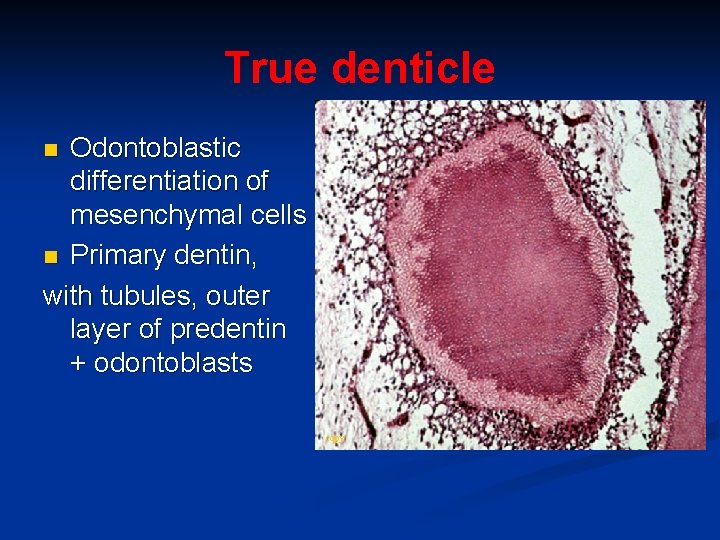
True denticle Odontoblastic differentiation of mesenchymal cells n Primary dentin, with tubules, outer layer of predentin + odontoblasts n copy
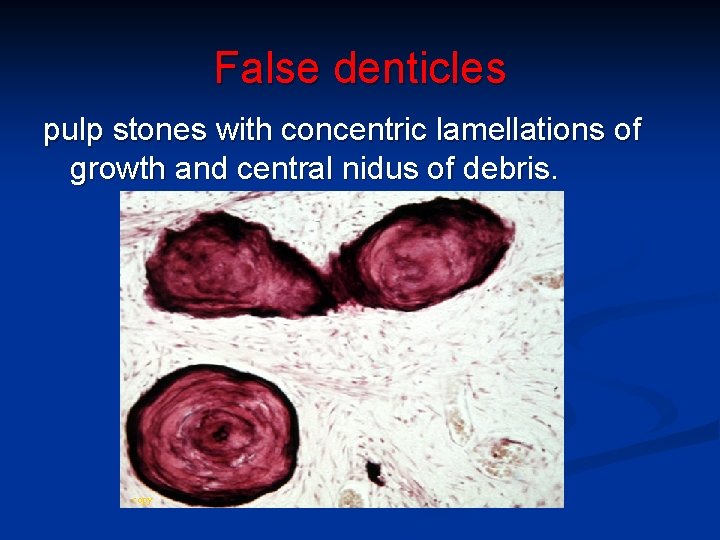
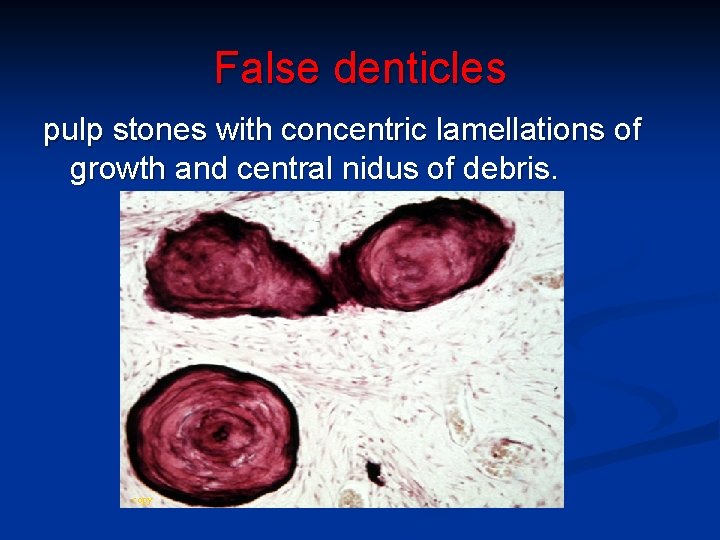
False denticles pulp stones with concentric lamellations of growth and central nidus of debris. copy
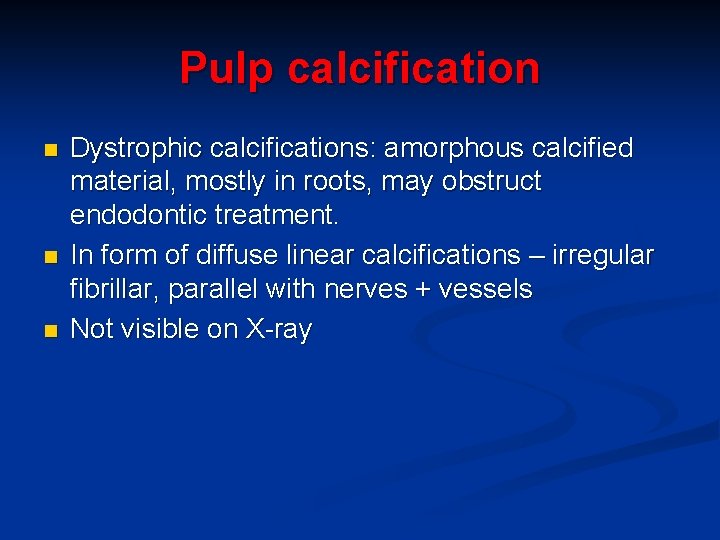
Pulp calcification n Dystrophic calcifications: amorphous calcified material, mostly in roots, may obstruct endodontic treatment. In form of diffuse linear calcifications – irregular fibrillar, parallel with nerves + vessels Not visible on X-ray
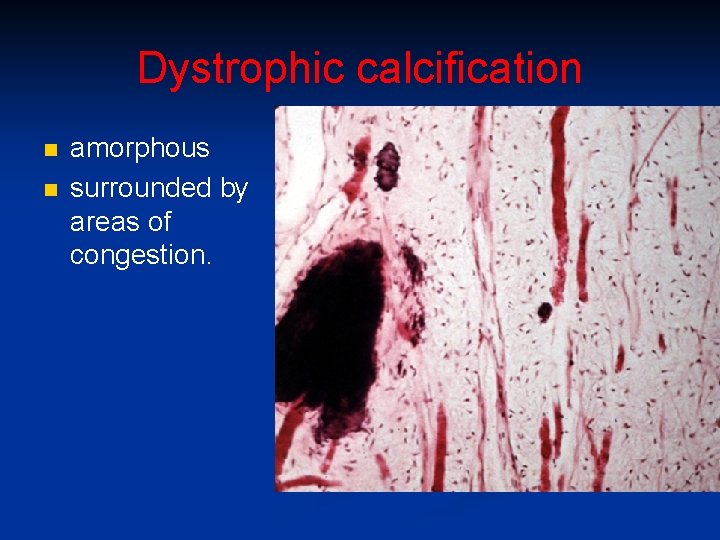
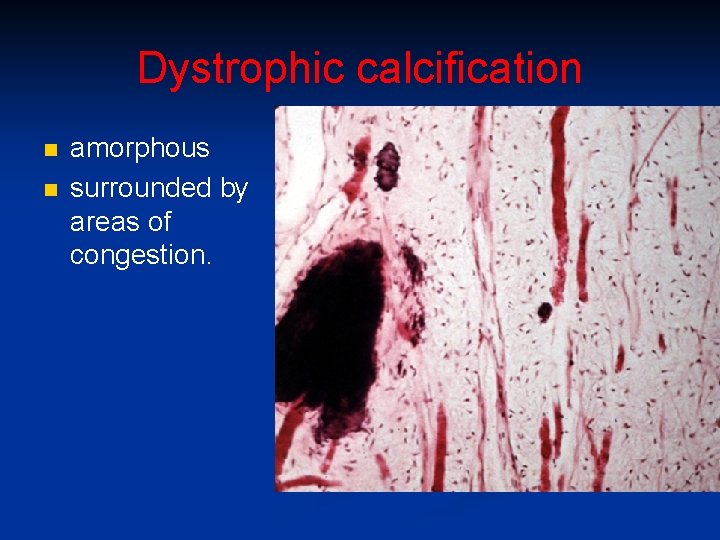
Dystrophic calcification n n amorphous surrounded by areas of congestion.
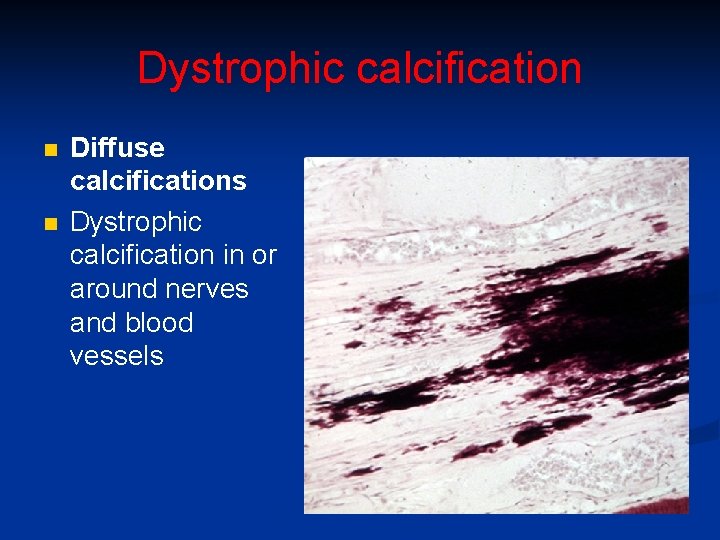
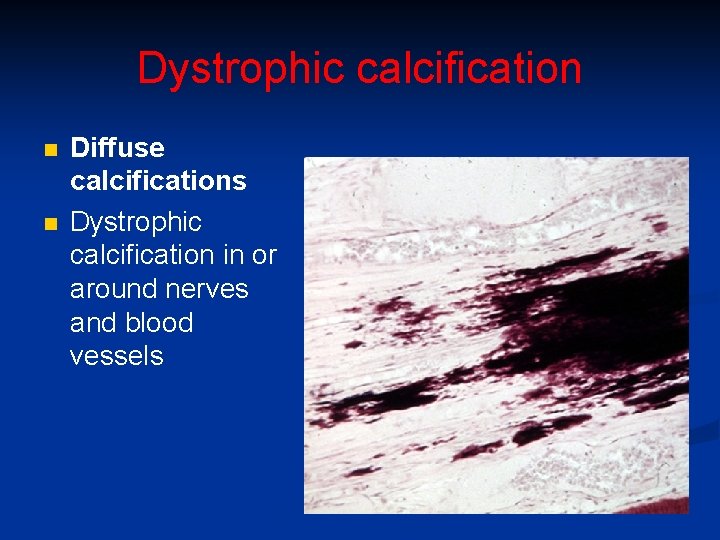
Dystrophic calcification n n Diffuse calcifications Dystrophic calcification in or around nerves and blood vessels
Pulp obliteration n n by irregular dentin after traumatic vessel injury not sufficient to cause necrosis. possible in dentinogenesis imperfecta and dentinal dysplasia.
Pulp necrosis n n n May follow pulpitis or trauma to apical blood vessels. Coagulative necrosis after ischemia. Liquefactive necrosis after pulpitis Gangrenous (with foul odor) due to infection by putrefactive caries bacteria. Pulp necrosis in sickle cell anemia (blockage of microcirculation).
Age changes in the pulp n n n Gradual decrease in volume due to secondary dentin formation. Decreased vascularity and cellularity. Increased collagen fiber content. Impaired response to injury and healing potential. Increase of pulp stones and diffuse calcification.
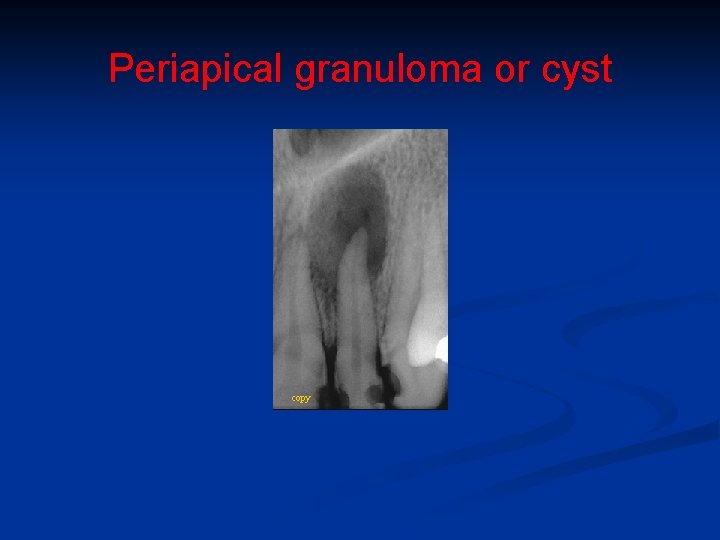
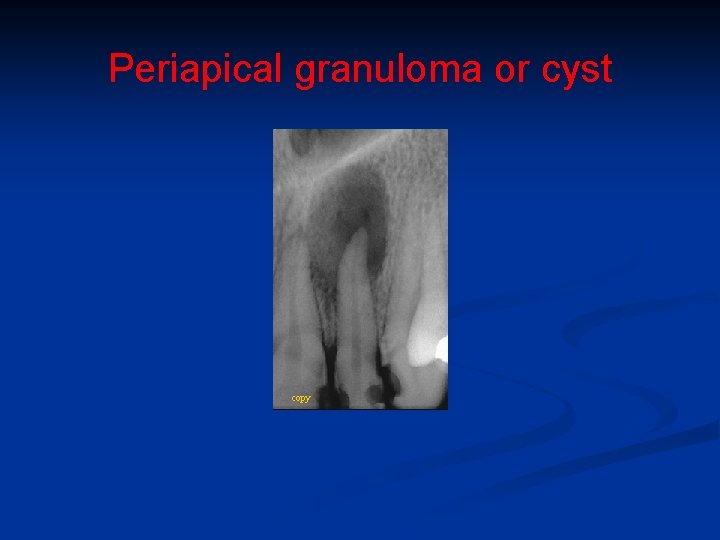
Periapical granuloma or cyst copy
Selected sources n n Odell EW: Cawson‘s Essentials of Oral Pathology and Oral Medicine, 9 th ed. , Elsevier 2017 Regezi JA, Sciubba JJ, Jordan RKC: Oral pathology: Clinical Pathologic Correlations, 7 th ed. , Elsevier 2017
 True denticle
True denticle How is aerolar tissue different than aerenchyma tissue?
How is aerolar tissue different than aerenchyma tissue? Pulp fiction
Pulp fiction Rcp pulp
Rcp pulp Ketchup joke pulp fiction
Ketchup joke pulp fiction Celesa pulp
Celesa pulp Palmar subaponeurotic space
Palmar subaponeurotic space Pulp oximeter
Pulp oximeter Pulp protection liners and bases
Pulp protection liners and bases Indirect pulp capping
Indirect pulp capping Odontoblastic zone of pulp
Odontoblastic zone of pulp Pulp diagnosis
Pulp diagnosis Mandibular canine access opening
Mandibular canine access opening Space of parona boundaries
Space of parona boundaries Chronic hyperplastic pulpitis
Chronic hyperplastic pulpitis Periapical granuloma vs abscess
Periapical granuloma vs abscess Wood pulp
Wood pulp Difference between liner and varnish
Difference between liner and varnish Type of pulp
Type of pulp White pulp
White pulp Dora mali
Dora mali Timon waugh
Timon waugh Pulp dentin
Pulp dentin Pulp fiction three act structure
Pulp fiction three act structure Fish pulp
Fish pulp Pitkyaranta pulp
Pitkyaranta pulp Enamel pulp
Enamel pulp Behavioral disorders
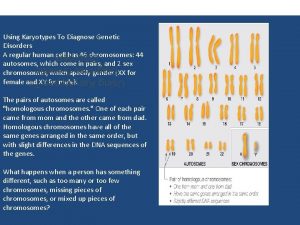
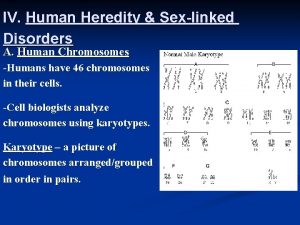
Behavioral disorders Using karyotypes to diagnose genetic disorders
Using karyotypes to diagnose genetic disorders Avoidant personality traits
Avoidant personality traits Cluster c personality disorder
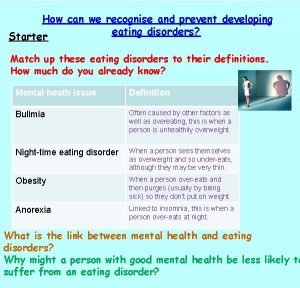
Cluster c personality disorder How to spot eating disorders
How to spot eating disorders Psychiatric disorders
Psychiatric disorders An extreme harmful eating behavior
An extreme harmful eating behavior Chapter 11 childhood and neurodevelopmental disorders
Chapter 11 childhood and neurodevelopmental disorders Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Sleep disorders
Sleep disorders Bipolar and other related disorders
Bipolar and other related disorders Chronic insomnia
Chronic insomnia Neurobehavioral disorders list
Neurobehavioral disorders list Unit 14 physiological disorders
Unit 14 physiological disorders Hilda bruch
Hilda bruch Unit 14 health and social care level 3
Unit 14 health and social care level 3 Non neoplastic epithelial disorders
Non neoplastic epithelial disorders What is a sex linked disorder
What is a sex linked disorder Chapter 11 genetic disorders concept mapping
Chapter 11 genetic disorders concept mapping Physiological disorders of onion
Physiological disorders of onion Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Personality disorder vs mental illness
Personality disorder vs mental illness Disorders of the nervous system
Disorders of the nervous system Neurotic stress-related and somatoform disorders
Neurotic stress-related and somatoform disorders