DENTAL PLAQUE CONTENTS Introduction n Definition n Macroscopic

- Slides: 107

DENTAL PLAQUE
CONTENTS Introduction n Definition n Macroscopic appearance n Methods to detect plaque. n Composition n Classification n Formation of plaque n Plaque hypothesis n Growth dynamics of plaque n
Translocation n Quorum sensing n Koch’s postulates n Socranksy’s postulates n Key characteristics of specific periodontopathogens n Factors affecting plaque formation n Indices to measure plaque n Plaque control measures n Conclusion n
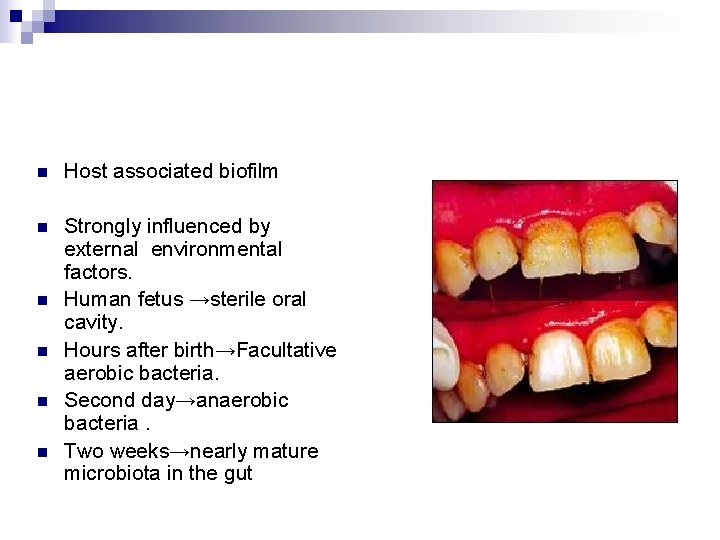
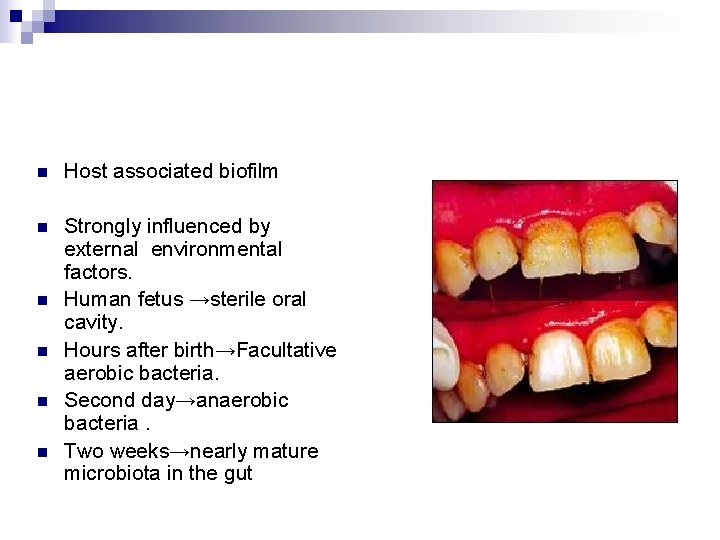
n Host associated biofilm n Strongly influenced by external environmental factors. Human fetus →sterile oral cavity. Hours after birth→Facultative aerobic bacteria. Second day→anaerobic bacteria. Two weeks→nearly mature microbiota in the gut n n
DEFINITION n “ Nonmineralised n “ A soft deposit that form the biofilm adhering to the tooth surfaces in the oral cavity including removable and fixed restorations. Bowen W- 1976 microbial accumulation that adheres tenaciously to tooth surfaces, restorations and prosthetic appliances showing structural organisations and with predominance of filamentous forms. It is composed of an organic matrix derived from salivary glycoproteins and extracellular microbial products and cannot be removed by rinsing or water spray”. Nolte – 1982
n Pellicle – Glycoprotein derived from components of saliva and GCF as well as bacterial and host tissue cell products and debris. n Materia Alba - Soft accumulations of bacteria and tissue cells that lack the organised structure of dental plaque and are easily displaced water spray. n Calculus – Hard deposit that forms by mineralisation of dental plaque and is generally covered by a layer of unmineralised plaque
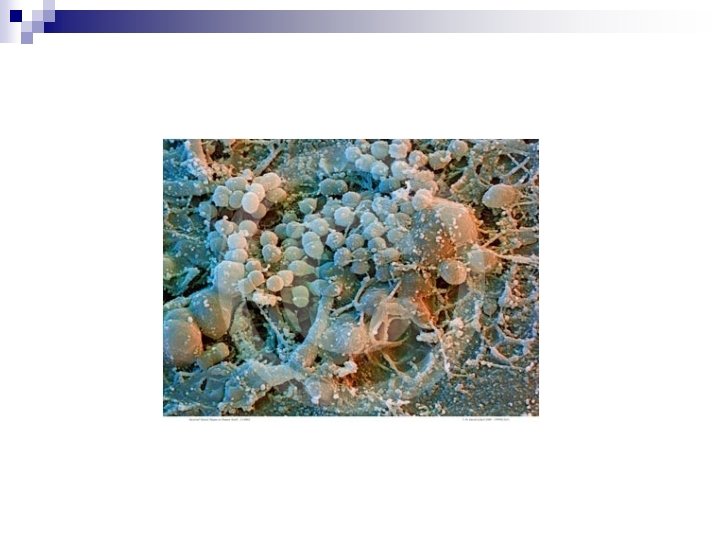
MACROSCOPIC APPEARANCE n Readily visible on the tooth surface after 1 -2 days. n Whitish, Grayish/ yellowish colour , has a globular appearance n Removed by movement of tissues and food materials. n Accumulates in the gingival third and in pits, cracks, fissures, overhanging restorations and around malaligned ooth.
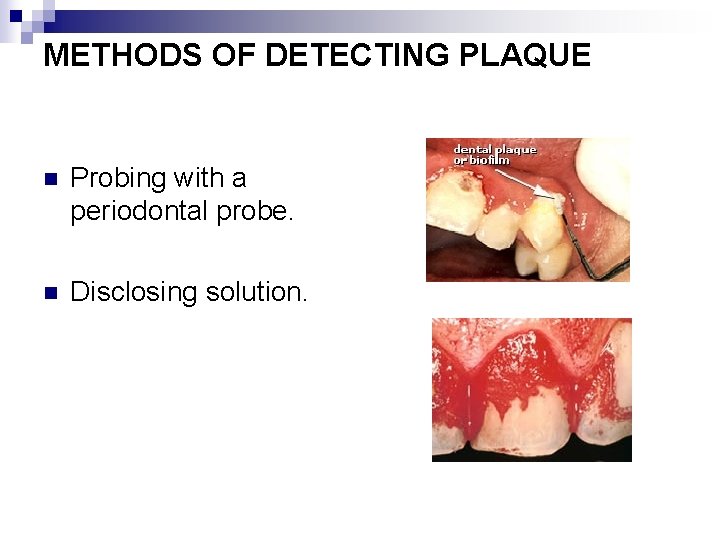
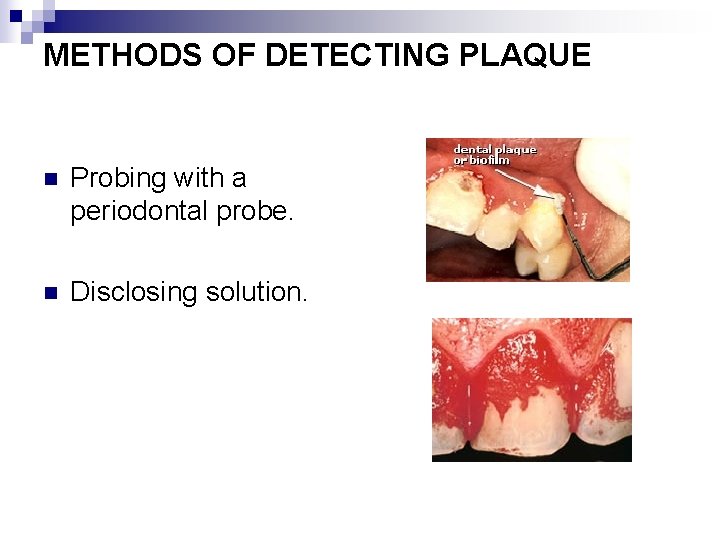
METHODS OF DETECTING PLAQUE n Probing with a periodontal probe. n Disclosing solution.
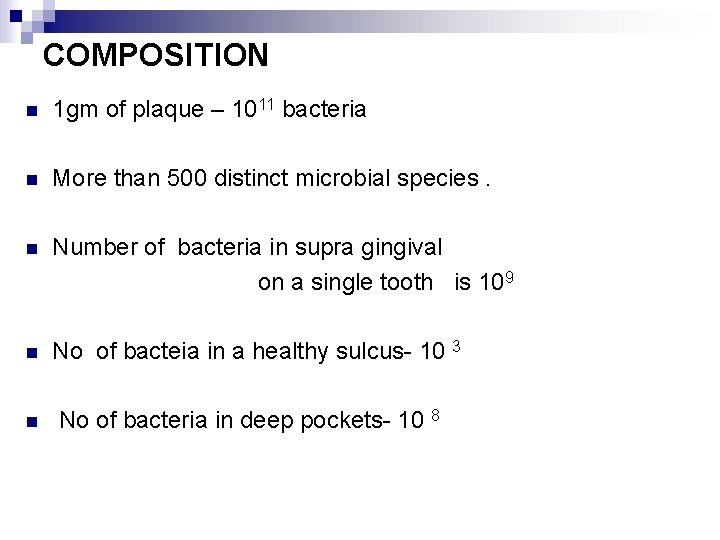
COMPOSITION n 1 gm of plaque – 1011 bacteria n More than 500 distinct microbial species. n Number of bacteria in supra gingival on a single tooth is 10 9 n No of bacteia in a healthy sulcus- 10 3 n No of bacteria in deep pockets- 10 8
n Two varieties. Transient group: Brought in to the oral cavity by air, food, water, foreign objects. Resident group: Varies from individual to individual, and appears rather constant for each individual. Nonbacterial microorganisms : Mycoplasma, Yeasts, Protozoa, Viruses.
INTERMICROBIAL MATRIX n n Accounts for 20 -30 % of plaque mass. Consists of organic and inorganic matrix derived from saliva , GCF, and bacterial products. Host cells in intercellular matrix n n n Epithelial cells Macrophages Leukocytes
Organic Constituents of Intercellular Matrix Polysaccharides Proteins Glycoproteins Lipid material POLYSACCHARIDES 1. FRUCTAN Synthesised from dietary sucrose Provides storage of energy 2. GLUCANS Synthesised from sucrose
Two Types, Dextrans: Predominant form, mainly serves as energy storage. Mutans: cannot be degraded easily. Polysaccharides act as a skeleton in the matrix , allows attachment of pellicle as well as microorganisms,
PROTEINS Albumin originates from the GCF. Other proteins are: Salivary enzymes Bacterial enzymes Immunoglobulin LIPIDS derived from membranes of disrupted bacterial and host cells and possibly cell debris. Food products
GLYCOPROTEINS Derived from saliva important components of pellicle. become inorporated in to the developing plaque biofilm. Inorganic Constituents Predominantly ; Calcium, Phosphorus. Trace elements: Sodium , Potassium , Flouride.
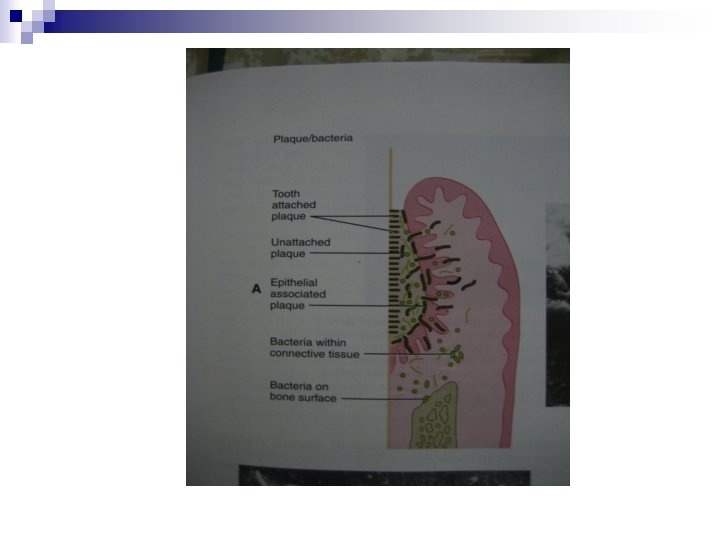
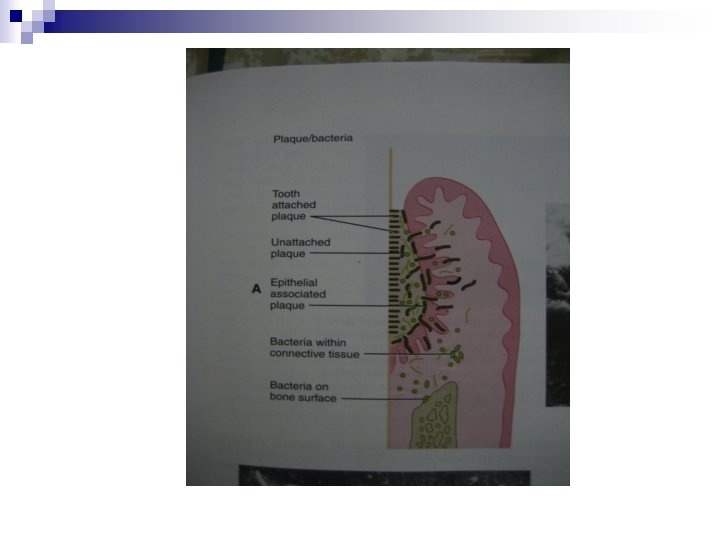
CLASSIFICATION SUPRAGINGIVAL Coronal Marginal SUBGINGIVAL Tooth Attahed Plaque Unattahed Plaque Epithelium Asscoiated Plaque
n Marginal plaque→ gingivitis n Supragingival and tooth associated subgingival plaque→calculus formation n Tissue associated subgingival plaque→periodontal tissue destruction n Subgingival toothattached plaque→calculus formation and root caries
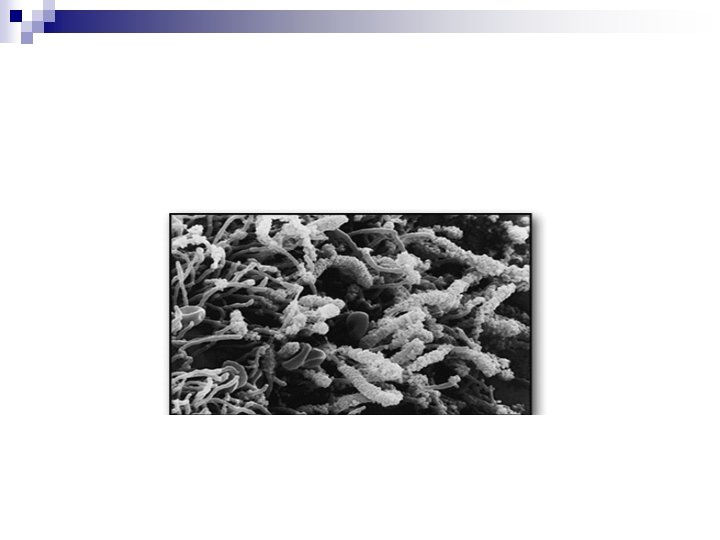
SUPRAGINGIVAL PLAQUE n Demonstrates stratified organisation of bacterial morphotypes. n Gram –positive cocci and short rods predominate at the tooth surface area, n Gram –ve rods filaments as well as spirochaetes pedominate the outer surface of mature plaque mass.
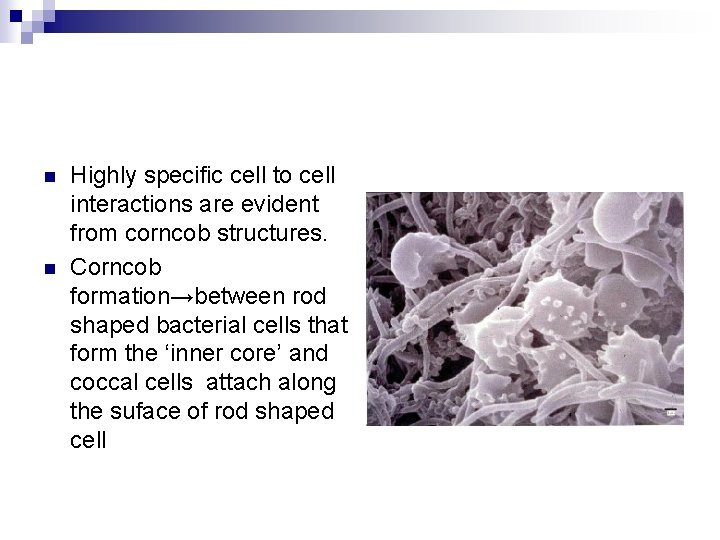
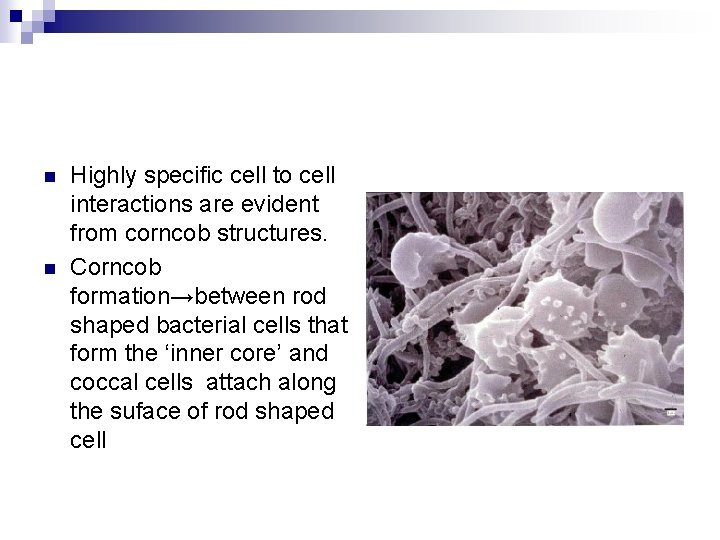
n n Highly specific cell to cell interactions are evident from corncob structures. Corncob formation→between rod shaped bacterial cells that form the ‘inner core’ and coccal cells attach along the suface of rod shaped cell
SUBGINGIVAL PLAQUE TISSUE / EPITHELIUM ASSOCIATED PLAQUE -Loosely arranged Lack definite intermicrobial matrix - Comprises of Gram-negative rods and cocci, large number of filaments, flagellated rods, spirochaetes. -Local availability of blood products and low redox potential - Gingival crevicular fluid → nutrients
n Predominaence of S oralis, s intermedius, P streptococcus micros, P gingivalis P intermedia, Tannerella forsythus and fusobacterium nucleatum
TOOTH ASSOCIATED ( Attached Plaque) ¨ Cervical part : densely arranged consists of gam +ve rods and cocci including Streptococcus mitis , Streptococcus sanguis, Actinobacillus Viscosus, A. naeslundi and Eubacterium species. ¨ Deeper ¨ Apical parts filamentous forms are fewer border of plaque mass is separated from junctional epithelium by a layer of host leukocytes. increased concentration of gram negative rods, no filamentous forms, spirochaetes
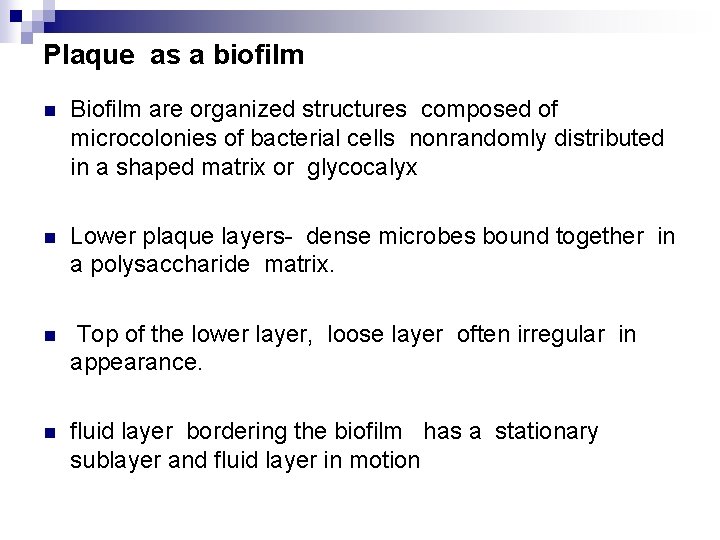
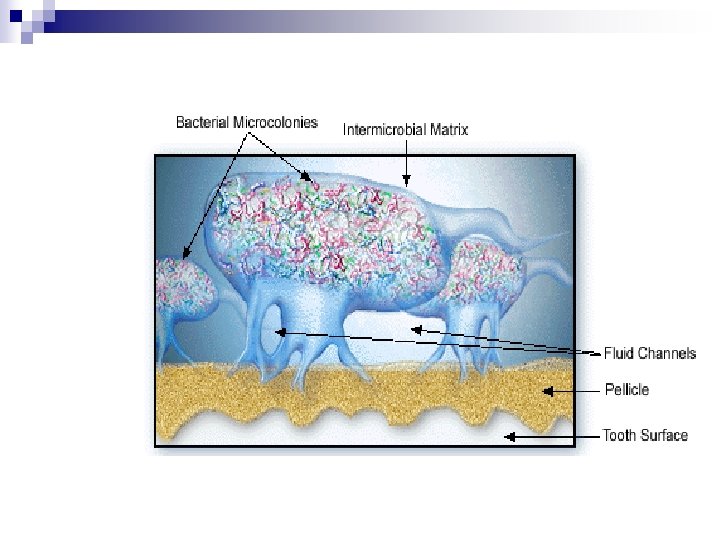
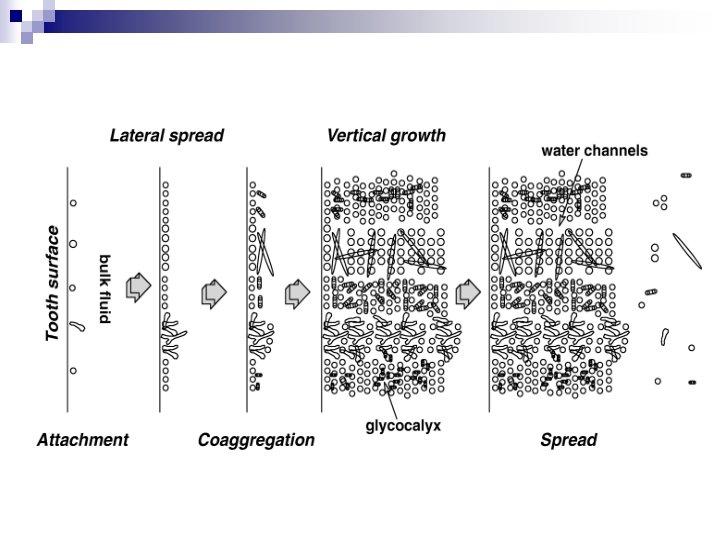
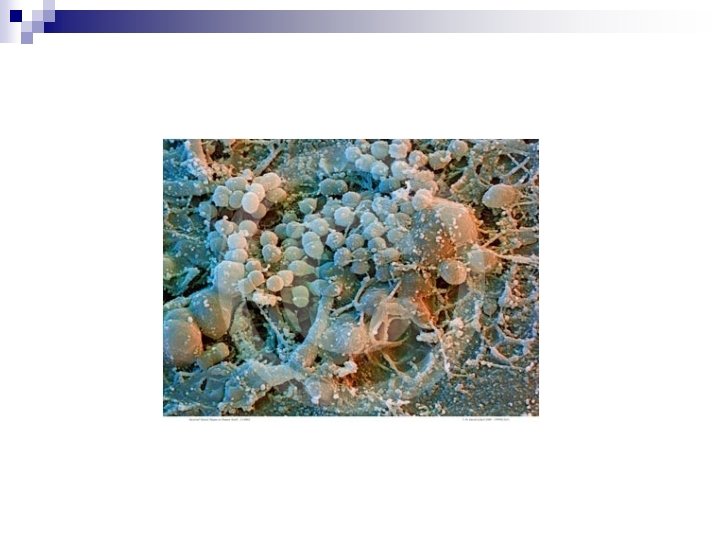
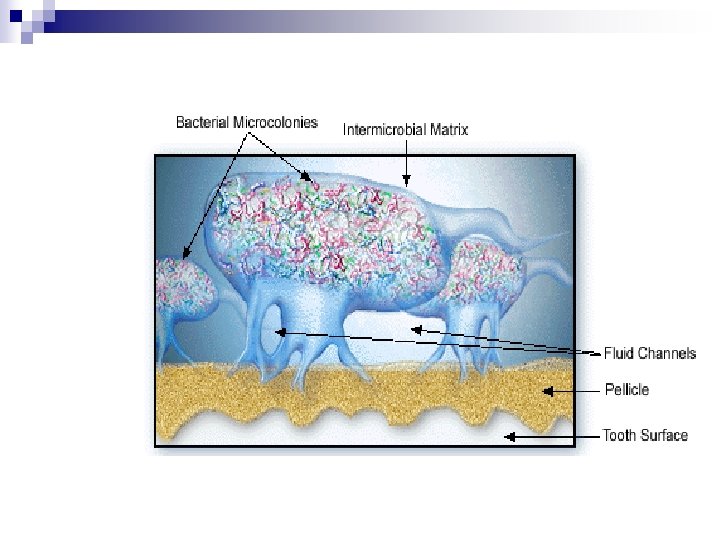
Plaque as a biofilm n Biofilm are organized structures composed of microcolonies of bacterial cells nonrandomly distributed in a shaped matrix or glycocalyx n Lower plaque layers- dense microbes bound together in a polysaccharide matrix. n Top of the lower layer, loose layer often irregular in appearance. n fluid layer bordering the biofilm has a stationary sublayer and fluid layer in motion
n Nutrients penetrate by molecular diffusion n Dental plaque →heterogenous structure fluid filled channels running across the plaque. n Nutrients contact with sessile microcolonies by diffusion from water channels to the microcolony.
n Bacteria exist and proliferate n Substances produced by bacteria are retained and essentially concentrated
MECHANISMS OF PLAQUE FORMATION n “Experimental gingivitis model”( Loe etal 1965) n This protocol involves the examination of subjects who abstain from any oral hygiene measures for a period of three weeks. n These studies have provided much information on the structural and microbiological characteristics of dental plaque
n n Pellicle formation – A lighly stained material on a tooth surface when patients use disclosing solution. Brownish due to the presence of tannins. Stains for proteins and sugars. n Derived from salivary components selectively adsorbed on to the tooth surface n Components- albumin, lysozyme, amylase, immunoglobulin A, proline rich poteins and mucins, sugars like rhamnose, muramic acid, diaminopimelic acid n First step in plaque formation. Granular, homogenous material of variable thickness n
Initial Adhesion and Attachment of Bacteria Phase I: Transport to the surface n Random contacts through brownian motion. n Sedimentation of microorganisms n Through liquid flow n Active bacterial movement ( chemotactic activity).
Phase 2 ; Initial adhesion n n n reversible adhesion of bacterium Through long and short range forces The interaction energy, total gibbs energy (G tot= GA+GE)( separation distance bw negatively charged particle and negatively charged surface Sec minimum- reversible binding Positive maximum ( energy barrier to adhesion Primary minimum( irreversible adhesion is established, short range forces – hydrogen bonding , iron pair formation steric interaction.
n Phase 3 : attachment Firm anchorage→ specific interactions ( covalent, hydrogen bonding ) Direct contact or bridging through specific extracellular proteinecious components of organisms and complementory receptors ( proteins and glycoproteins or polysaccharides on the surface )
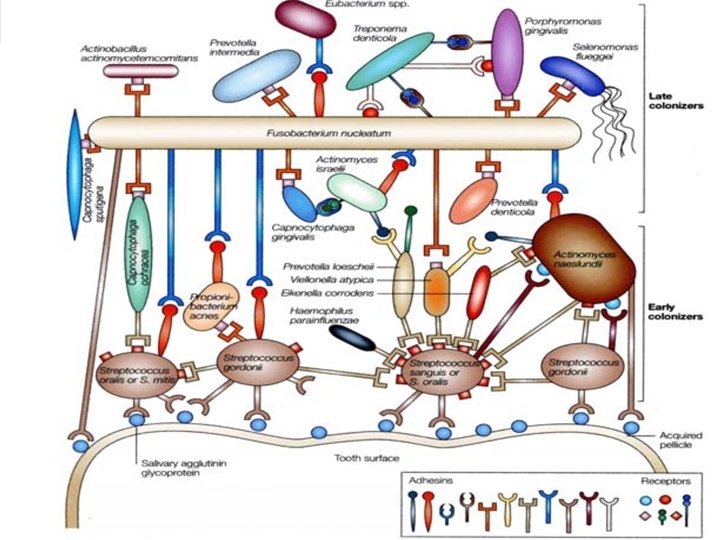
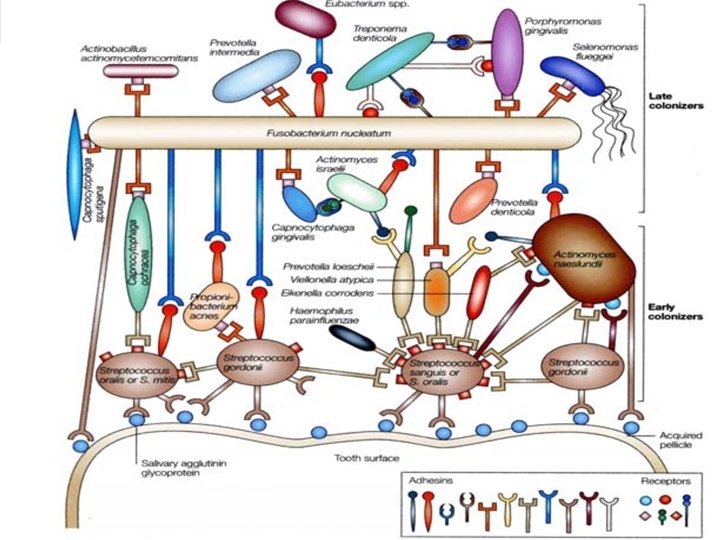
n n n S. sanguis ( principle early coloniser )bind to proline rich proteins and other receptors in the pellicle such as alpha amylase and sialic acid. A. viscosus posses fimbriae →adhesins →proline rich proteins. A viscosus recognises cryptic segments of proline rich proteins. Phase 4: Colonisation of surface and biofilm formation.
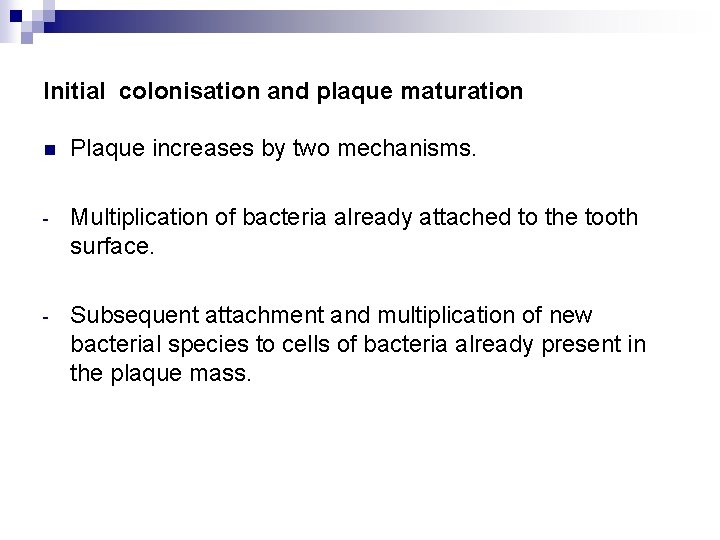
Initial colonisation and plaque maturation n Plaque increases by two mechanisms. - Multiplication of bacteria already attached to the tooth surface. - Subsequent attachment and multiplication of new bacterial species to cells of bacteria already present in the plaque mass.
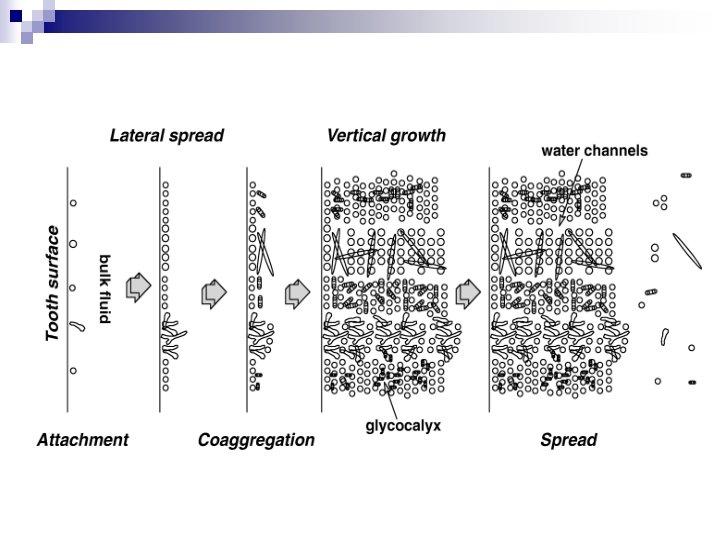
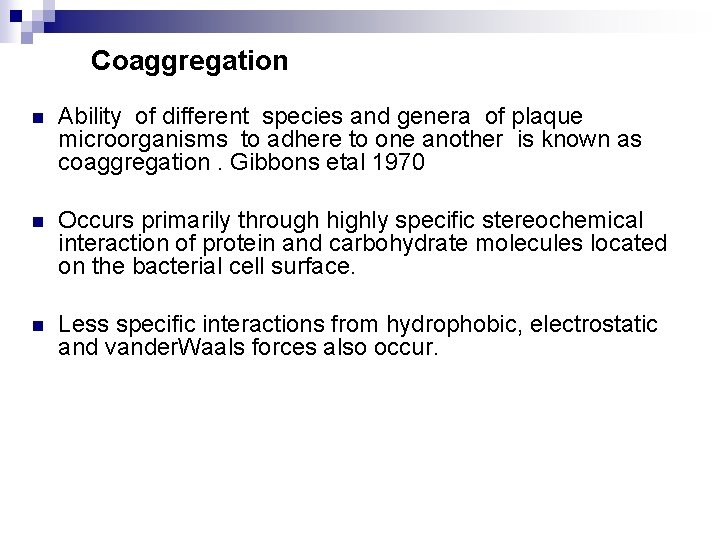
Coaggregation n Ability of different species and genera of plaque microorganisms to adhere to one another is known as coaggregation. Gibbons etal 1970 n Occurs primarily through highly specific stereochemical interaction of protein and carbohydrate molecules located on the bacterial cell surface. n Less specific interactions from hydrophobic, electrostatic and vander. Waals forces also occur.
n 18 genera have some form of coaggregration n Fusobacteria coaggregate with all the human bacteria n Vellionelle , capnocytophagae and prevotelle bind to streptococci and actinomyecetes. n Mediated by lectin like adhesins which can be inhibited by lactose and galactose.
n Eg: F nucleatum with S Sanguis P loeschii with A viscosus C Ochracea with A viscosus n Early stages, coaggregation occurs among different grampositive species and between gram positive and gram negative species. n Later stages , b between different gram negative species. Eg: E. nucleatum, P. gingivalis and T. denticola
Secondary colonisers n Gram negative species- Fusobacterium nucleatum, Prevotella intermedia , Porphyromonas gingivalis, Prevotella loeschii and capnocytophaga species. n Adehere to the gram positive species already present in the plaque. n 1 -3 days of accummulation. n A complex array of bacterial rods, filaments and cocci appear.
Tertiary colonisers After one week of plaque accumulation other gram negative species may also appear P gingivalis, C rectus. , E corrodens A A Comitans and the oral spirochaetes( Treponema species)
n Socransky etal → 13000 plaque samples Used cluster analysis and community coordination techniques to demonstrate the presence of specific microbial groups. DNA hybridisation methodology defined “ complexes” of periodontal microorganisms
n n Yellow complexes-streptococcus species. Green Complex: E corrodens, A. actinomycetemcomitans serotype a, and Capnocytophaga species. n Orange Complex : Fusobacterium , prevotela and Campylobacter species. n Red Complex: P gingivalis, Tanerella forsythus and T denticola. They are aasociated with bleeding on probing. Purple complex consisting of Veillonella parvula and Actinomyces odontolyticus. n
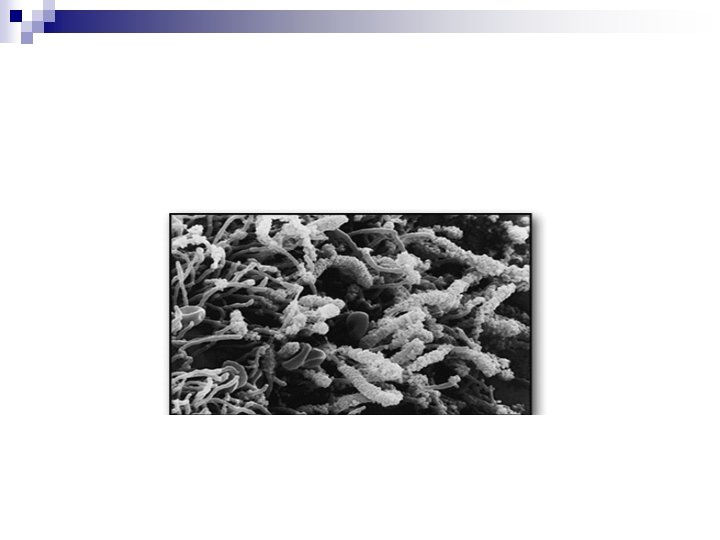
Formation of subgingival plaque n Undisturbed growth of supragingival plaque →soft tissue alterations n Gingival margin→Inflammatory changes Deepened sulcus →anaerobic environment Anaerobic bacteria→motile rods and spirochaetes Rods and filaments arranged in palisading manner with long axis perpendicular to the tooth surface. Occurs 3 -12 weeks of plaque formation.
n Unique bacterial aggregates resembling testtube bristles can be found attached to the adhering plaque and extend deep in to space between bacterial layer and the adjacent soft tissue wall. n Bristles of these “Test tube brush ” formation are gram positive filamentous bacteria , some of which may be flagellated. n Lack of well defined microbial colonies may be due high degree of mobility among the resident microbial flora.
PLAQUE HYPOTHESIS n The nonspecific and specific Plaque Hypothesis were delineated in 1976 by Walter Loesche n Nonspecific plaque hypothesis: Periodontal disease results from the “ Elaboration of noxious products by the entire plaque flora. According to this hypothesis, when only small amounts of plaque are present, the noxious products are neutralised by the host. Similarly large amounts of plaque would produce large amounts of noxious products, which would essentially overwhelm the host defenses. According to this concept the control of periodontal disease depends on control of amount of plaque accumulation. n
Specific plaque hypothesis n States that only certain plaque is pathogenic and its pathogenicity depends on the presence of or increase in specific microorganisms. n This concept predicts that of plaque harbouring specific bacterial pathogens results in the periodontal disease because these organisms produce substances that mediate the destruction of host tissues.
Growth dynamics of plaque n n n First 2 -8 hours→pioneering streptococci , cover 3 -30% OF ENAMEL SURFACE Next 20 hrs→short period of rapid growth. One day , it can be called biofilm. As bacterial densities approach 2 -6 million bacteria /mm 2, a marked increase in growth rate can be observed up to 32 million bacteria/mm 2 Thickness slowly increases with time to 20 - 30 µm after 3 days. After 4 days 30% of the tooth crown is covered by plaque.
Variation within dentition Early plaque formation occurs faster in n The lower jaw compared to upper jaw. n In molar areas n On buccal tooth surfaces compared to oral site n Interdental regions Impact on gingival iflammation n More rapid in tooth margins facing the inflamed gingiival margins than adjacent halthy gingiva. Hence it is suggested that crevicular fluid enhances plaque accumulation.
Physiological properties of dental plaque n Early colonisers use oxygen and reduce the redox potential which then favours anaerobic species. n gram +ve species use sugars as energy source and saliva as carbon source. n Mature plaque bacteria use aminoacids and small peptides as energy source n Lactate and formate→by products of streptococci and actinomyecetes , used by other microbes.
n Growth of P gingivalis is enhanced by succinate from Capnocytophaga and protoheme by Campylobacter rectus. n Ammonia from host cells after degradation processesis used by bacteria as nitrogen source. n Hemin from breakdown of hemoglobin is important in the metabolism of P gingivalis. n Steroid hormones→proportions of P intermedia in subgingival plaque.
TRANSLOCATION Intraoral transmission of bacteria from one niche to another. n Cross infection. n Can jeopardise the outcome of periodontal surgery. n
Quorum Sensing In a biofilm, the bacteria have the capacity to communicate with each other. n Involves regulation of expression of specific genes through the accumulation of signaling compounds that mediate intercellular communication. n
Criteria for identification -Koch’s postulates. n n Must be routinely isolated from diseased individuals. Must be grown in pure culture in laboratory. Must produce a similar disease when inoculated into susceptible laboratory animals. Must be recovered from lesions in a diseased laboratory animal.
Sigmund socransky- criteria for identification of periodontal pathogens. n Must be associated with disease, as evident by increases in the number of organisms at diseased sites. n Must be eliminated or decreased in sites that demonstrate clinical resolution of disease with treatment
n Must demonstrate a host response , in the form of an alteration in the host cellular or humoral immune response. n Must be capable of causing disease in experimental animal models. n Must demonstrate virulence factors responsible for enabling the microorganisms to cause destruction of periodontal tissues.
Key characteristics of Specific Periodontopathogens Actinobacillus actinomyecetemcomitans n n n Small , straight or curved rod with rounded end Nonmotile and gram negative Forms ; five serotypes( a to e ) , based on differences in polysaccharide composition. Grows in white translucent , smooth, nonhemolytic colony on blood agar. Possess lipopolysaccharide, leukotoxin, collagenase and protease.
Tannerella forsythia n n n Nonmotile, spindle shaped, highly pleomorphic rod, Gram negative obligate anaerobe Grows slowly only in anaerobic conditions and needs several growth factors from other species. Produce several proteolytic enzymes that are able to destroy immunoglobulns and factors of the complement system. Induces apoptotic cell death.
Porphyromonas gingivalis n n Nonmotile , pleomorphic rod, gram negative obligate anaerobe Different forms are present based on their genotype. Grows in anerobic medium with dark pimentation ( brown, dark green or black ) on blood agar. Has strong proteolytic activity.
n Aggressive periodontal pathogen- fimbriae mediate adhesion and capsule defend against phagocytosis. n Produces proteases , collagenases , hemolysins n Prevents the migration pf PMNLs across the epithelial barrier and affects the production or degradation of cytokines. n Potential to invade soft tissues.
Prevotella intermedia, Prevotella nigrescens n n Short rounded gram negative rods, Grow anaerobically with dark pigmentation. Campylobacter rectus n n n Rare motile organism Gram negative, short rod, curved or helical Motility→polar flagellum Grows anaerobically with dark pigmentationwhen sulphide is added. Gts transformed in to greyish Fe. S Produces leukotoxin Less virulent and less proteolytic
Fusobacterium nucleatum n Gram negative, cigar shaped bacilli with pointed ends. n Several subspecies are present n Grows anaerobically in blood agar. n Induce apoptotic cell death in polynuclear and mononuclear cells. n Can trigger the release of cytokines. , elastate and oxygen radicals from leukocytes n Coaggregates with most of the oral microorganisms. Bridging organism between primary and secondary colonisers. n
Peptostreptococcus micros n Rare cocci in periodontitis n Gram positive and grows obligate anaerobically. Eubacterium species. n Gram positive , obligate anaerobic , small pleomorphic rod n Several forms are classified including E nodatum, E timidum, E brachy. n Grow anaerobically but with difficulty in standard blood agar.
Spirochaetes n Diverse group of spiral and motile organisms n Helical rods 5 -15µm long , diameter 0. 5µm n Have 3 to 8 irregular spirals n Cell wall is gram negative , but they stain poorly. n Forms: T denticola, T. Vincenti , t socranski, T pallidum n Able to travel through viscous enviroment like GCF and penetrate epithelium and connective tissue n Some have the capacity to degrade collagen and even dentin n T denticola produces proteolytic enzymes that can destroy immunoglobulins( Ig. A, Ig. M, Ig. G) or complement factors
Full mouth disinfection n Full mouth scaling and root planing within 24 hours to reduce the number of subgingival pathogenic organisms. n Subgingival irrigation of all pockets with a 1% chlorhexidine gel to kill remaining bacteria.
n Tongue brushing with an antiseptic to suppress the bacteria in the niche. n Mouthrinsing with an antiseptic to reduce the bacteria in the saliva.
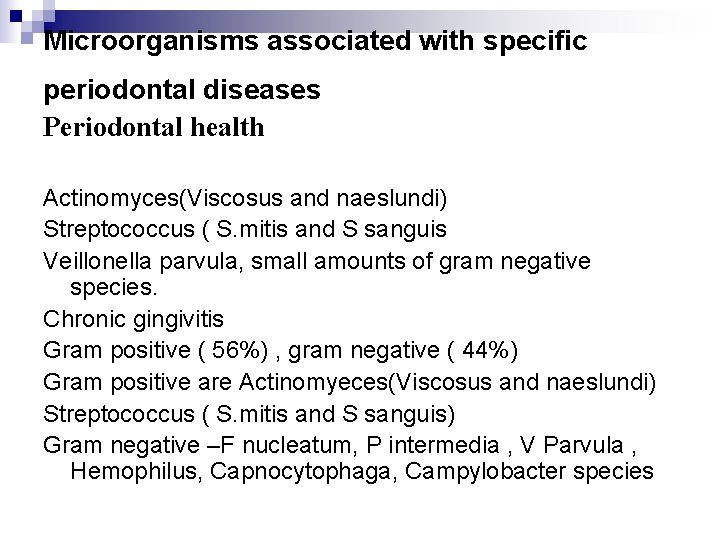
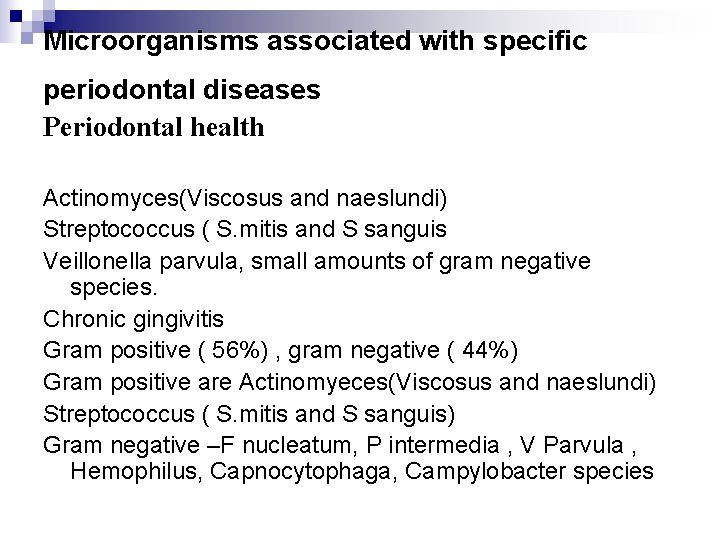
Microorganisms associated with specific periodontal diseases Periodontal health Actinomyces(Viscosus and naeslundi) Streptococcus ( S. mitis and S sanguis Veillonella parvula, small amounts of gram negative species. Chronic gingivitis Gram positive ( 56%) , gram negative ( 44%) Gram positive are Actinomyeces(Viscosus and naeslundi) Streptococcus ( S. mitis and S sanguis) Gram negative –F nucleatum, P intermedia , V Parvula , Hemophilus, Capnocytophaga, Campylobacter species
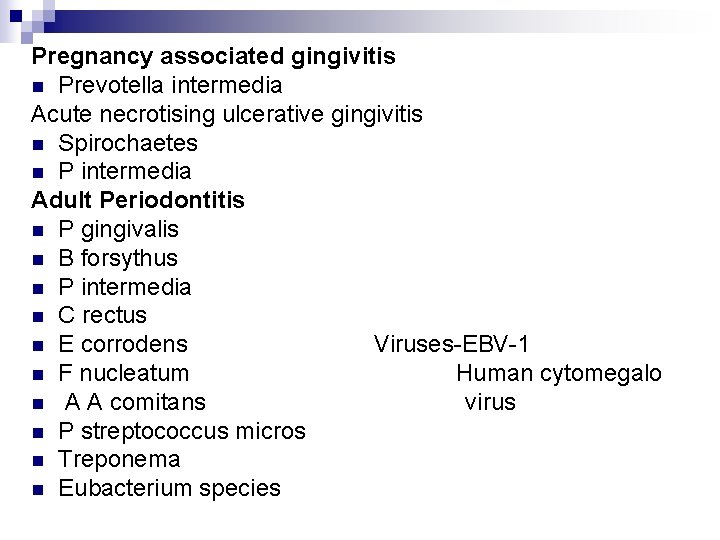
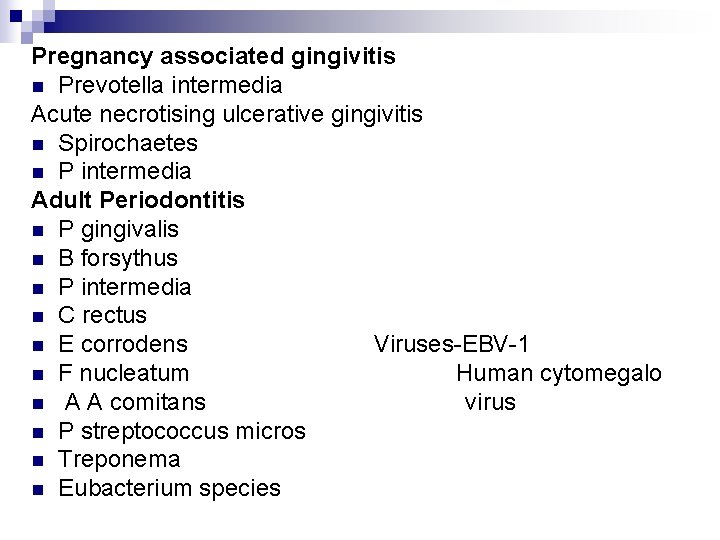
Pregnancy associated gingivitis n Prevotella intermedia Acute necrotising ulcerative gingivitis n Spirochaetes n P intermedia Adult Periodontitis n P gingivalis n B forsythus n P intermedia n C rectus n E corrodens Viruses-EBV-1 n F nucleatum Human cytomegalo n A A comitans virus n P streptococcus micros n Treponema n Eubacterium species
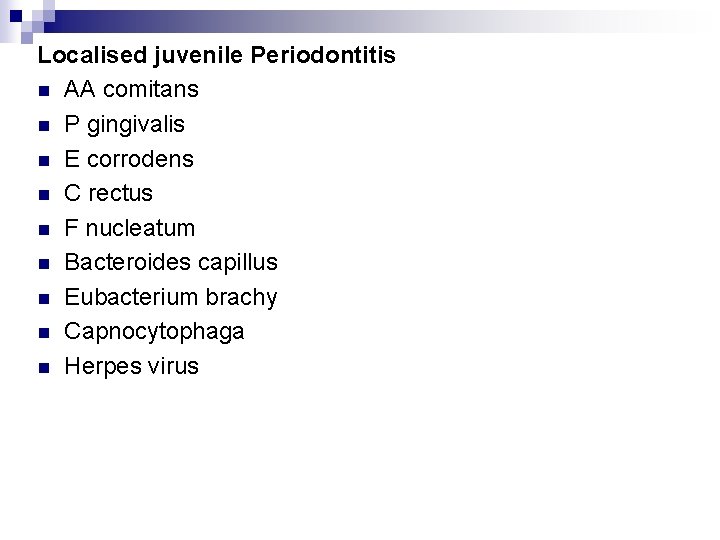
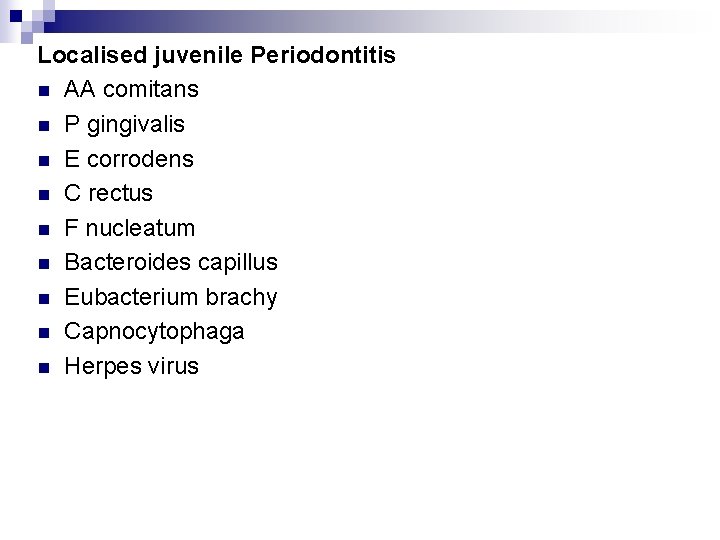
Localised juvenile Periodontitis n AA comitans n P gingivalis n E corrodens n C rectus n F nucleatum n Bacteroides capillus n Eubacterium brachy n Capnocytophaga n Herpes virus
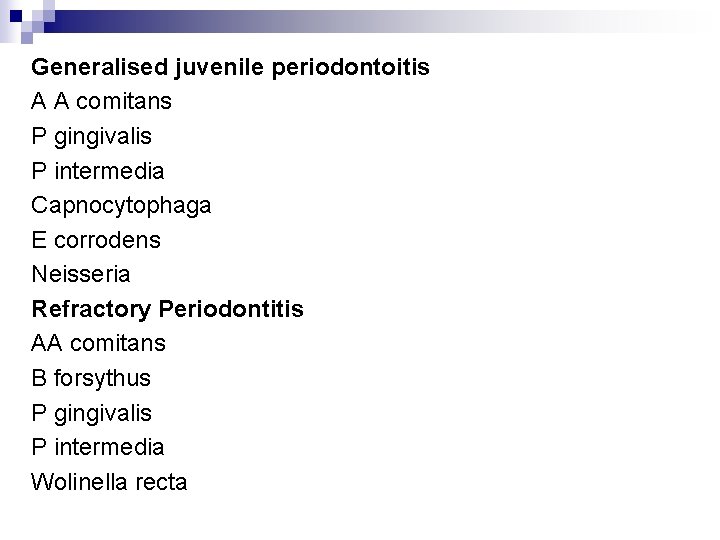
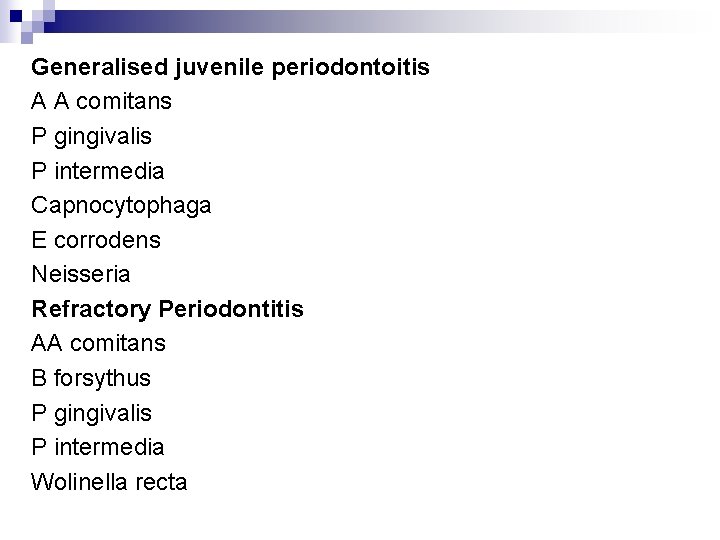
Generalised juvenile periodontoitis A A comitans P gingivalis P intermedia Capnocytophaga E corrodens Neisseria Refractory Periodontitis AA comitans B forsythus P gingivalis P intermedia Wolinella recta
Abcesses of the periodontiun F nucleatum P intermdia Pstreptococcus micros B forsythus P gingivalis
Factors affecting plaque formation n Saliva n Diet n Oral Hygiene Habits n Other local factors.
n Saliva p. H- Increase in salivary flow increases the p. H In low p. H there may be an increse in the cariogenic bacteria. 1.
DIET n Consistency and texture: fibrous foods may be beneficial tp periodontal health than soft, sticky foods. n Chewing fibrous food exerts a natural cleaning action , paticularly with respect tyo the removal of the plaque from gingival half of the tooth. n Changes in nitrient concentrations. Stoodly demonstrated that there was a ten fold increase in carbon and nitrogen concentration.
Oral Hygiene Status n In the absence of oral hygiene measures , plaque continues to accumulate until a balance is reached between the forces of plaque removal and those of plaque formation.
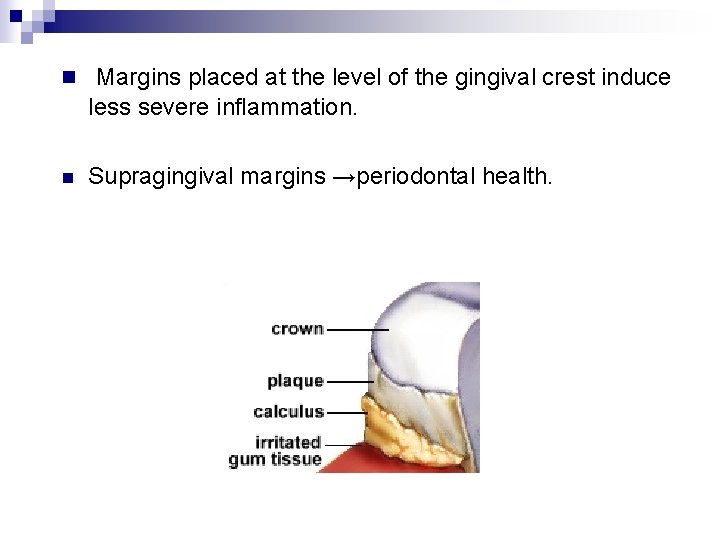
Other local factors n Margins of restorations: Overhanging margins of restorations changes the ecological balance of the gingival sulcus to an area that favours the growth of disease associated organisms at the expense of health associated organisms. n Also inhibit the patients access to remove accumulated plaque. n Subgingival margins are associated with large amounts of plaque accumulation , gingival inflammation and the rate of gingival fluid flow.
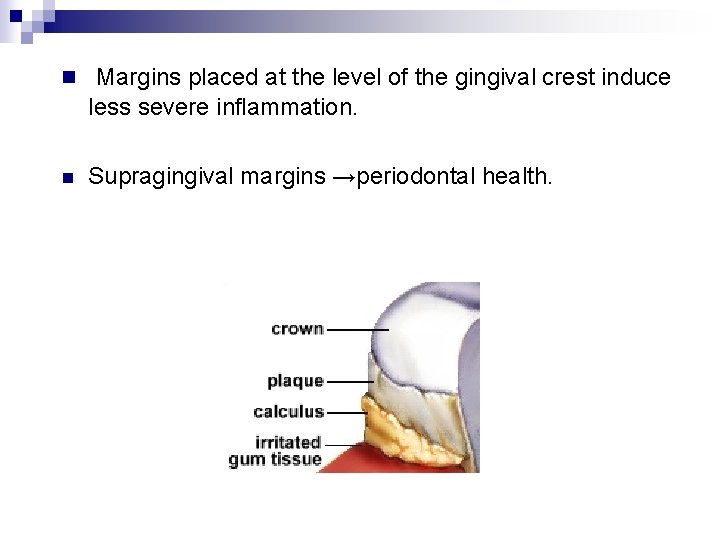
n Margins placed at the level of the gingival crest induce less severe inflammation. n Supragingival margins →periodontal health.
Sources of marginal roughness. n Grooves and scratches in the surface of polished restorations n Separation of restoration margin and polished restorations , n Cervical finish line , exposing the rough surface of the prepared tooth. n dissolution and disintegration of the luting material between the preparation and the restoration , leaving a space. n Inadequate margins fit of therestoration
Contours Over contoured crowns and restorations→more plaque accumulation. Design of Removable Partial Denture Quantitative and qualitative changes in plaque Emergence of spirochaetal microrgnisms. Malocclusion Plaque control becomes more difficult.
Orthodontic Therapy n Retain plaque and food debris n modify the gingival ecosystem n Increases P melaninigenica , P intermedia, Actinimyces odontolyticus n Decrease in the proportion of facultative microorganisms. In the gingival sulcus
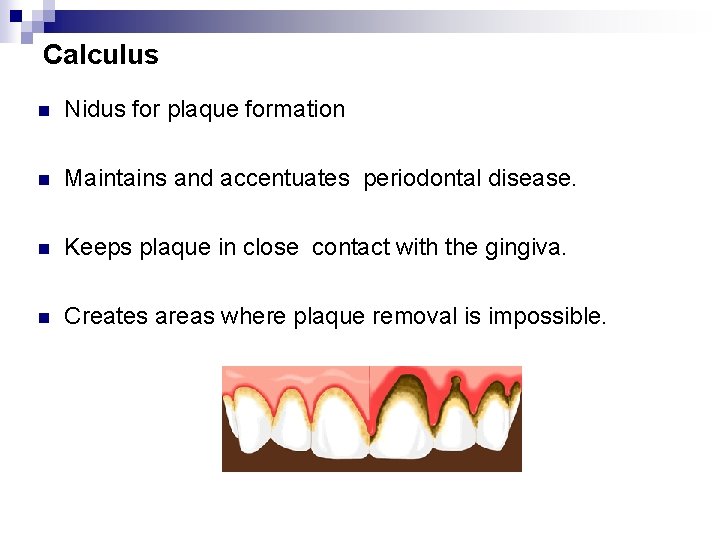
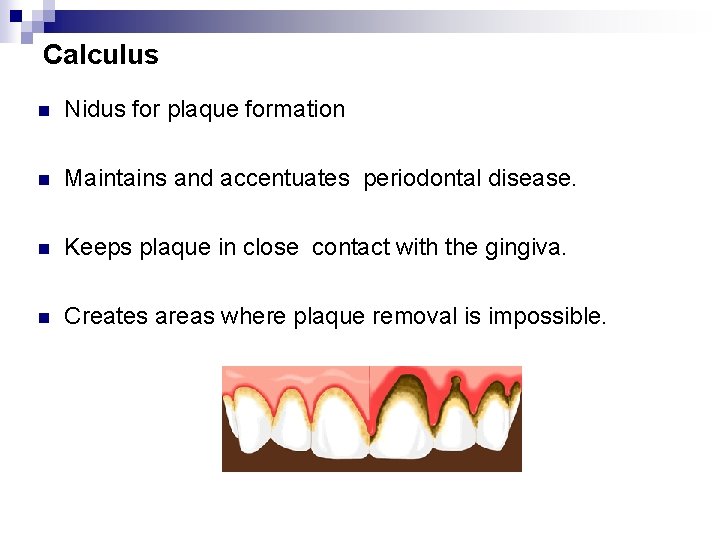
Calculus n Nidus for plaque formation n Maintains and accentuates periodontal disease. n Keeps plaque in close contact with the gingiva. n Creates areas where plaque removal is impossible.
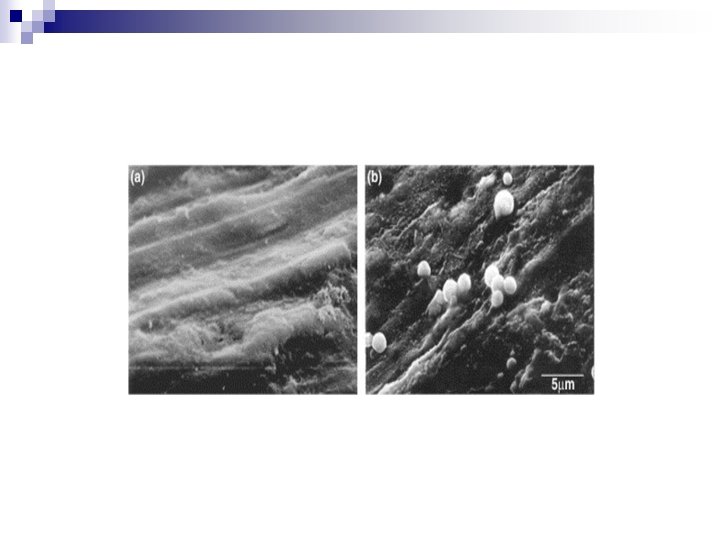
Methods to Study Dental Plaque Direct Observation Simple clinical index systems with or without disclosing solutions. Morphological analysis Light and electron microscopy Several investigators have studied sections from extracted teeth. Others have examined plaque accumulation on enamel fragments and other materials inserted in to prosthetic appliances Mandel and colleagues used plastic strips to study plaque Lisgarten etal performed exttensive studies on plaque grown on plastic crowns.
n Histochemical methods and immunoflourescence techniques have been used localise specific microorganisms and specific substances. Radioautography to study salivary glycoproteins and dietary contribution to plaque matrix. Metabolic study in situ Microelectrodes inserted in to plaque and radioelectrometry built in to prosthetic appliances have been used to study p. H changes associated with the metabolism of bacteria in plaque.
Biochemical Analysis High molecular weight polymers of glucose and other sugars , altered salivary glycoprotein, proteases and various chemotactic and inflammation inducing substances have been detected and patially characterised. n
Microbiologic techniques Techniques for sampling, isolating, enumerating, identifying and studying metabolism have been used.
n determine number, viability and identity of microorganisms n Changes in the microflora with age , maturation, and pathogenecity of plaque. n Utilisation of metabolites such as sucrose and elaboration of extracellular materials , including glucans and various toxic substances n Aggregation and adherence of microorganisms to one another and to tooth surfaces. identification of odontopathic and periodontopathic microorganisms n
Indices used to measure plaque Plaque component of periodontal diseases Index Sigurd P Ramford -1959 Teeth scored -16, 21, 24, 36, 41 and 44 Method: Bismarck brown solutionis used Scoring criteria 0 - No plaque present 1 -plaque present in some bot not all interproximal , buccal and lingual surfaces. of the tooth. 2 - Plaque present on all inter[proximal, buccal and lingual surfaces , but covering less than one half of these surfaces 3 -Plaque extending all over interproximal , buccal and lingual surfaces and covering more than one half of these surfaces n
Schick and Ash modification of plaque criteria 1961 Only gingival half, facial and lingual surface Scoring criteria: 0 - Abence of dental plaque 1 - Denatl plaque in the interproximal areas or at the gingival half of the facial and lingual surfaces of the tooth. 2 - Covering more than 1/3 rd but less than 2/3 rd of the gingival half of the facial or lingual surface of the tooth. 3 - Covering 2/3 rd or more of the gingival half of the facial/lingual surface of the tooth.
3. Oral hygiene index john C Greene and Jack R vermillion 4. Simplified Oral hygiene index ( OHI-S) John C. Greene & Jack R Vermillion- 1964 5. Quigley Hein plaque index Quigley G. and Hein j- 1982 gingival third of the tooth , on labial , buccal and lingual surfaces , using disclosing agents. Numerical scoring o- 5 was used.
Turresky- Gilmore - Glickman modification of Quigley – Hein plaque index Plaque was assessed on labial , buccal and lingual surfaces of all the teeth after using disclosing agent. Scoring Criteria: 0 - no plaque 1 -separate fleck of plaque , cervical region 2 -A thin continuous band of plaque ( up to 1 mm) at the cervical margin 3 - A band of plaque wider than 1 mm less than 1/3 rd of the crown 4 - Plaque covering at least 1/3 rd but less than 2/3 rd of the crown 5 - Plaque covering 2/3 rd or more of the crown
Plaque Index: silness and Loe H in 1964 n Assesses only the thickness of plaque in at the gingival area of the tooth. Surfaces – Distofacial, mesiofacial and lingual. Scoring criteria n 0 - gingival area is literally free of plaque. The surface is tested by running a pointed probe across the tooth surface at the entrance of the gingival crevice. After tooth has been perfectly dried. If no soft matter adheres to the point of the probe , thearea is considered clean
1 - No plaque can be observed in situ by naked eye. A film of plaque adhering to the free gingival margin and adjacent area of the tooth which can be recognised only by running the explorer /pointed probe across the tooth surface or by using a disclosing agent. 3 - A thin to moderate accumulation of soft deposits within the gingival pocket or on the tooth and gingival margin , which can be seen with naked eye. 4 - Abundance of soft matter within the gingival pocket and or on the tooth surface and gingival margin. The interdental area is stuffed with soft debris.
Plaque control measures Mechanical plaque control Tooth brushes Chew sticks Dental floss Interproximal cleansing aids( brushes and wooden devices)
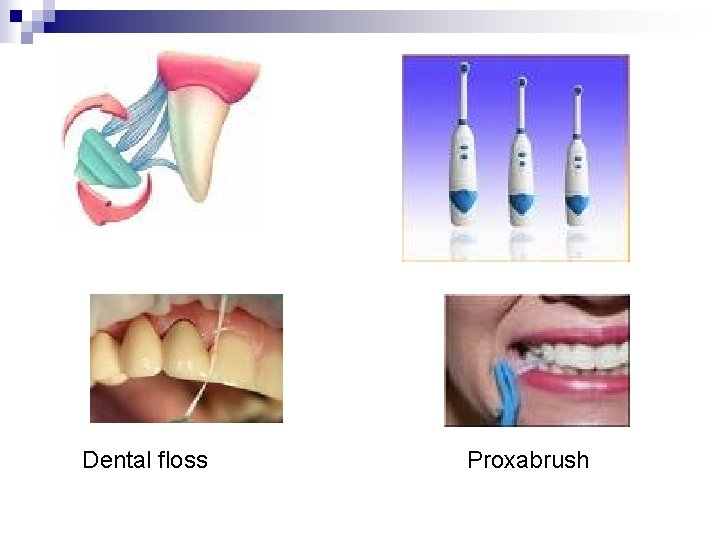
Dental floss Proxabrush
Antiplaque agents n Depending on efficacy and substantivity , they are classified as. n First generation agents- reduce plaque score by 20 - 50 percent, efficacy is limited because of poor substantivity. eg- antibiotics, , quarterinary ammonium compunds, sanguinarine. Should be used 4 to 6 times daily. n Second generation agents- retained longer in the tissues, slow release property provides overall reduction in plaque score by 70 to 90 percent ( should be used twice daily)eg- chlorhexidiene, triclosan with either copolymer or zinc citrate.
n Third generation agents: Should be effective against specific periodontopathic organisms. The most promising agent is delmopinol which is a surface active agent. Weak antimicrobial agent , can exert its effect by binding to salivary proteins and thereby alters the cohesive and adhesive properties of the film formed.
FLOURIDES: n Stannous flourides is an effective antiplaque agent. n Available in the form of gel n Develoment of black stain on some teeth.
BIBISGUANIDES: n Chlorhexidiene gluconate→most widely used 0. 12% or 0. 2% n Reduces plaque by 50 -55% and gingivitis by 45%. n Should be used twice daily. n Brown staining of teeth, taste alteration, oral desquamation n Rupture of bacterial cell walls and precipitation of the cytoplasmic content.
ESSENTIAL OILS n Listerine→Neutral in electric charge. n Combination of phenol related essential oils , thymol and eucalyptol , mixed with menthol and methyl salicylate. n Plaque reduction of 20 -34 % was noticed. n Initial burning sensation n Cell wall destruction, inhibition of bacterial enzymes May extract lipopolysaccharides from endotoxins.
QUARTERNARY AMMONIUM COMPOUNDS n Cetylpyridinium chloride (0. 05%) n Cationic and rapidly binds to oral tissues n Rapidly released , hence not as effective as chlorhexidiene. n Rupture of cell wall and alteration of cytoplasmic contents. n Side effects are similar to that of chlorhexidiene.
SANGUNARINE n Used as both mouth rinse and tooth paste. n Alkaloid extract from blood root plant (Sangunaria Canadensis) n Contain the extract at 0. 03% and 0. 2 % Zinc chloride n Plaque reduction of 17 -42 %, reduction in gingivitis is 1742% n Burning sensation
TRICLOSAN n Available as mouthrinses and dentrifices. n Bisphenol and nonionic germicide with low toxicity and broad spectrum antibacterial activity. n Widely used in soaps, antiperspirants and cosmetic toiletries. n Various formulations enhance their ability to bind to plaque and teeth. n Zinc citrate →antiplaque affect Copolymer of methoxyethylene and maleic acid→increase retention time. Pyrophosphates →enhance anticalculus properties.
Conclusion Bacterial plaque is regarded as one of the main aetiological factors in the initiation and promotion of periodontal disease ie gingivitis and periodontitis. The knowledge of the fact has been derived from epidemological studies as well as clinical experiments. Several clinical studies of experimental gingivitis, established the direct cause and effect relationship between plaque and gingival inflammation. Thus it is of paramount importance to understand the complex structure of plaque and its inter relation and influence on the development of oral diseases.
References n n n Clinical Periodontology carranza – 9 th and 10 th edt Periodontology 2000, Vol 5, Vol 8, Periodontal diseases- Schluger Clinical Periodontology- Jan Lindhe- 4 th edition. Preventive and Community dentistry- Soben Peter