DENTAL CARIES CONTENTS INTRODUCTION EPIDEMIOLOGY DEFINITION CLASSIFICATION THEORIES















- Slides: 92
DENTAL CARIES

CONTENTS INTRODUCTION EPIDEMIOLOGY DEFINITION CLASSIFICATION THEORIES OF CARIES CURRENT CONCEPTS IN CARIES ETIOLOGY § HISTOPATHOLOGY § § § § CONCLUSION

INTRODUCTION

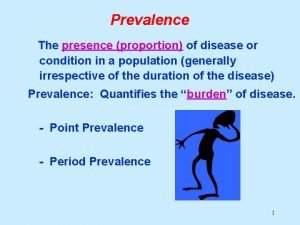
EPIDEMIOLOGY § Pre-historic man have decreased caries prevalence § Decreased caries prevalence in African and Asian communities § 1. 2. 3. 4. Factors affecting caries prevalence: Race Age Sex Familial
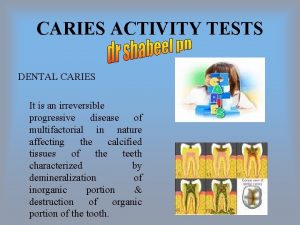
DEFINITION 1. “Dental caries is a microbial disease of the calcified tissues of the teeth, characterized by demineralization of the inorganic portion and destruction of the organic substance of the tooth” [Shaffer] 2. “Localized post eruptive pathologic process of external origin involving softening of the hard tissue and proceeding to the formation of a cavity” [WHO]
3. “An infectious microbiological disease of the teeth that results in localized dissolution and destruction of calcified tissues” [Sturdevant]
CLASSIFICATION I. STURDEVANT Based on - Location - Extent - Rate of progression
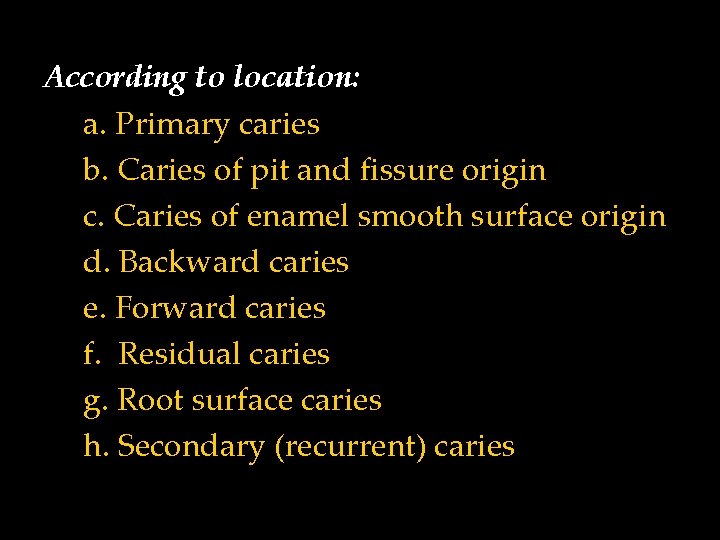
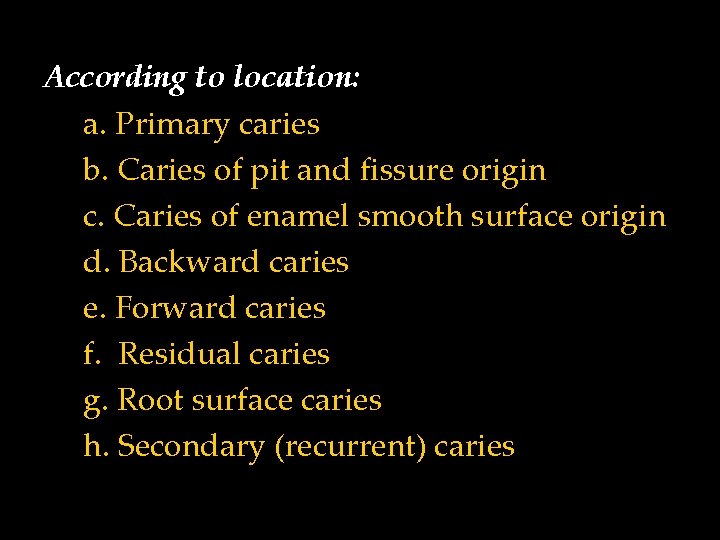
According to location: a. Primary caries b. Caries of pit and fissure origin c. Caries of enamel smooth surface origin d. Backward caries e. Forward caries f. Residual caries g. Root surface caries h. Secondary (recurrent) caries
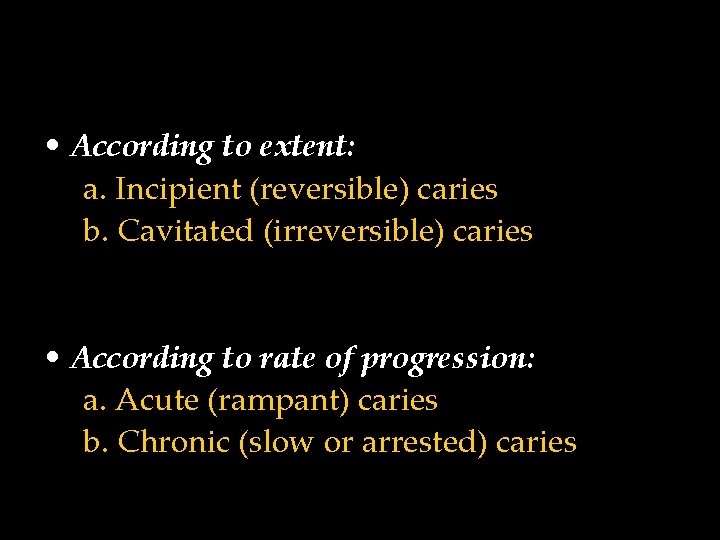
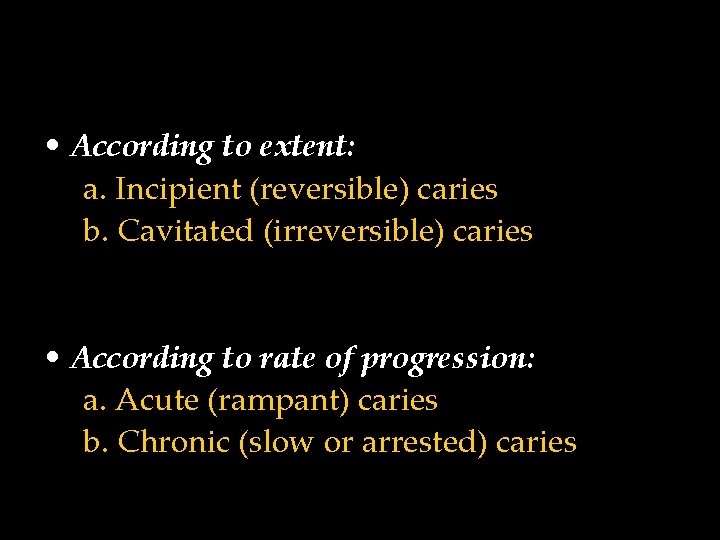
• According to extent: a. Incipient (reversible) caries b. Cavitated (irreversible) caries • According to rate of progression: a. Acute (rampant) caries b. Chronic (slow or arrested) caries
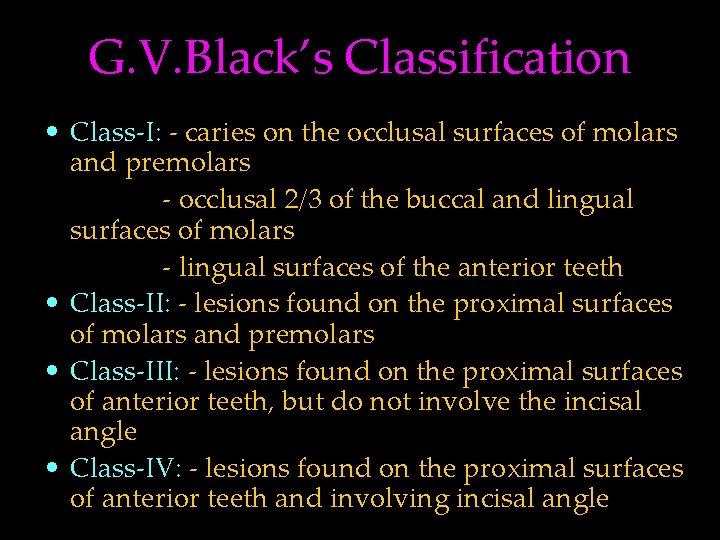
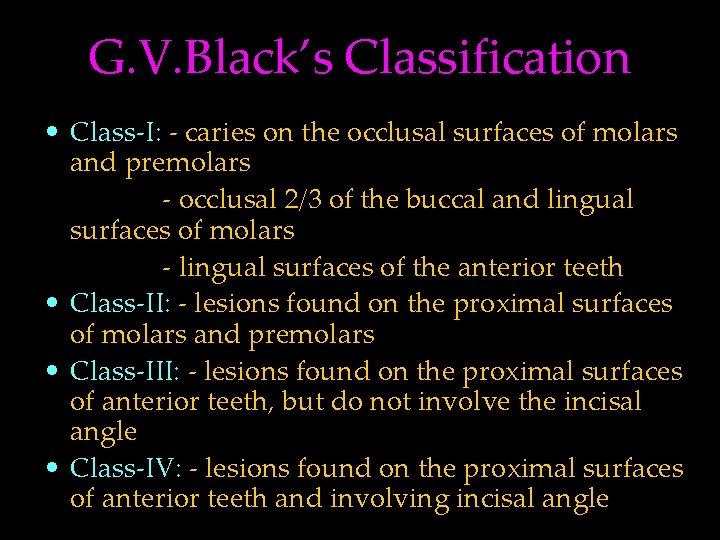
G. V. Black’s Classification • Class-I: - caries on the occlusal surfaces of molars and premolars - occlusal 2/3 of the buccal and lingual surfaces of molars - lingual surfaces of the anterior teeth • Class-II: - lesions found on the proximal surfaces of molars and premolars • Class-III: - lesions found on the proximal surfaces of anterior teeth, but do not involve the incisal angle • Class-IV: - lesions found on the proximal surfaces of anterior teeth and involving incisal angle
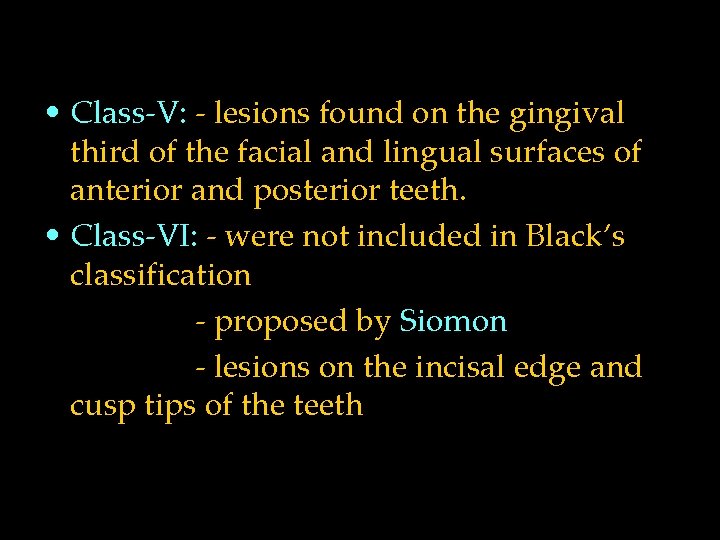
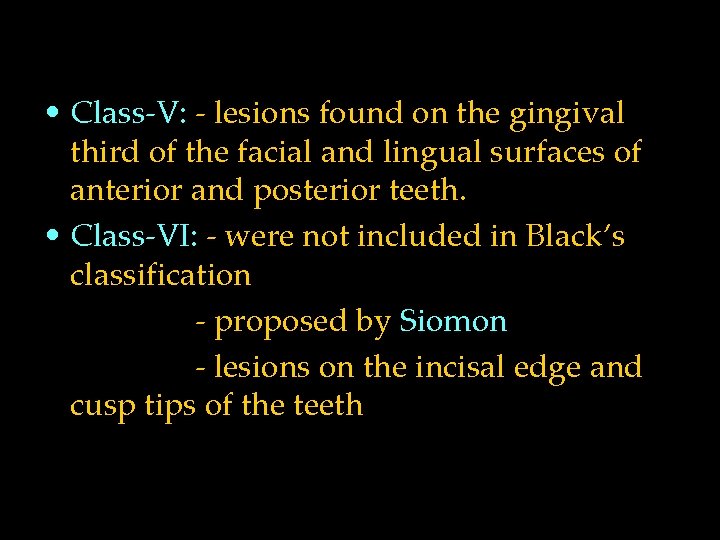
• Class-V: - lesions found on the gingival third of the facial and lingual surfaces of anterior and posterior teeth. • Class-VI: - were not included in Black’s classification - proposed by Siomon - lesions on the incisal edge and cusp tips of the teeth
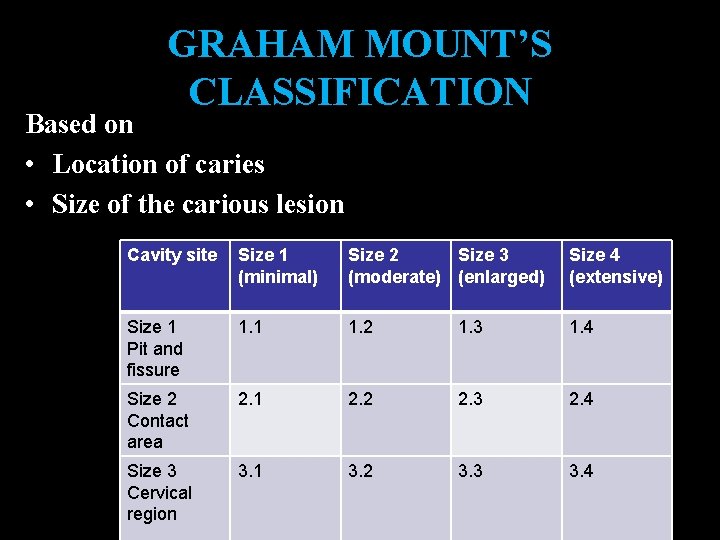
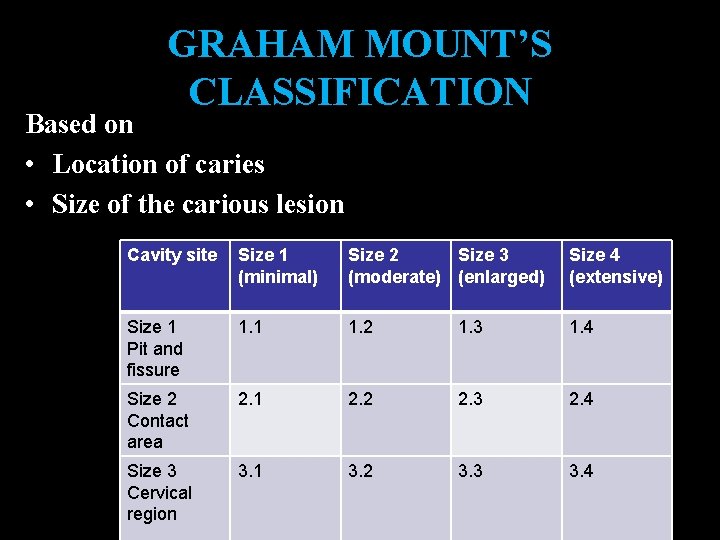
GRAHAM MOUNT’S CLASSIFICATION Based on • Location of caries • Size of the carious lesion Cavity site Size 1 (minimal) Size 2 Size 3 (moderate) (enlarged) Size 4 (extensive) Size 1 Pit and fissure 1. 1 1. 2 1. 3 1. 4 Size 2 Contact area 2. 1 2. 2 2. 3 2. 4 Size 3 Cervical region 3. 1 3. 2 3. 3 3. 4
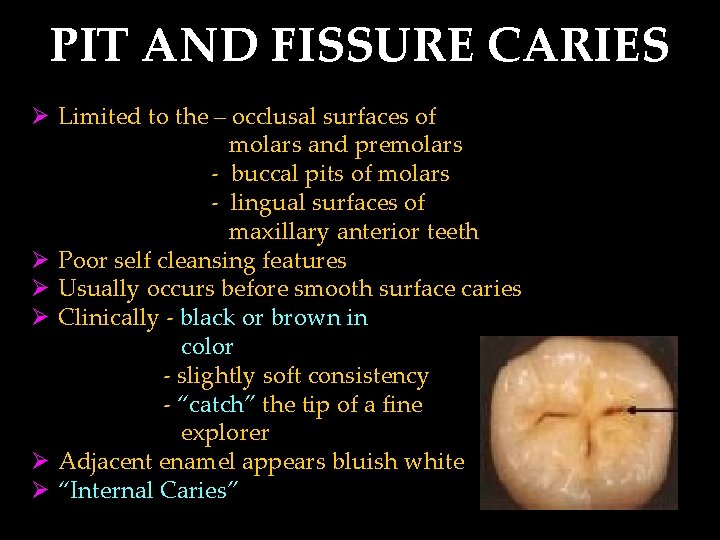
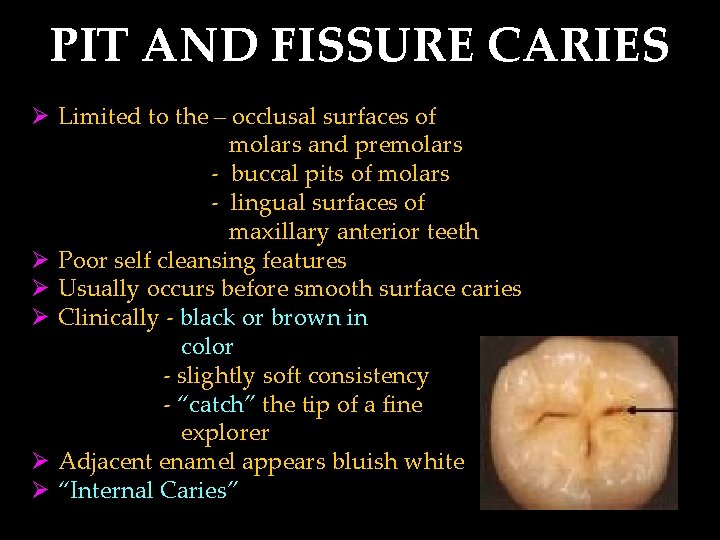
PIT AND FISSURE CARIES Ø Limited to the – occlusal surfaces of molars and premolars - buccal pits of molars - lingual surfaces of maxillary anterior teeth Ø Poor self cleansing features Ø Usually occurs before smooth surface caries Ø Clinically - black or brown in color - slightly soft consistency - “catch” the tip of a fine explorer Ø Adjacent enamel appears bluish white Ø “Internal Caries”
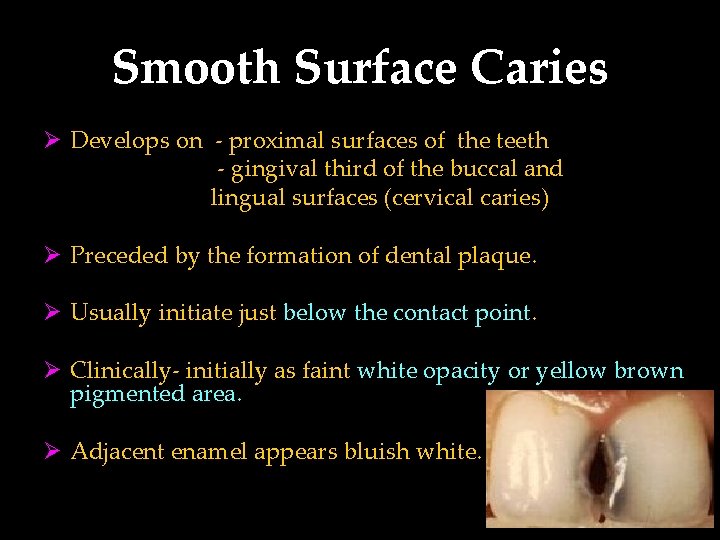
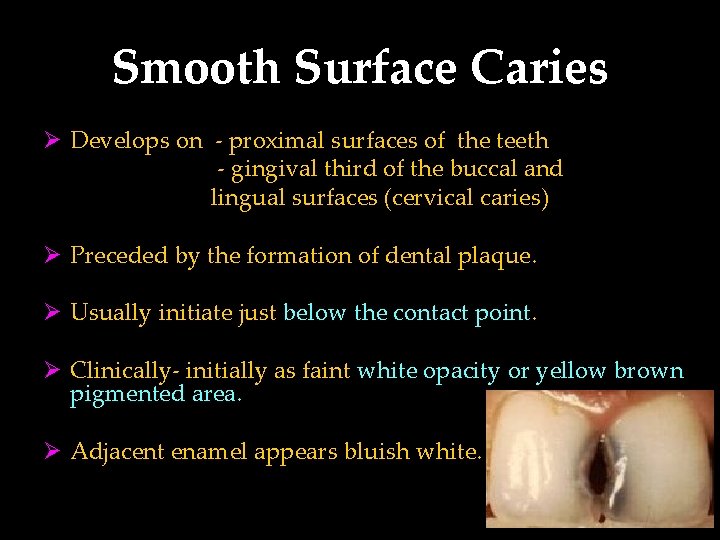
Smooth Surface Caries Ø Develops on - proximal surfaces of the teeth - gingival third of the buccal and lingual surfaces (cervical caries) Ø Preceded by the formation of dental plaque. Ø Usually initiate just below the contact point. Ø Clinically- initially as faint white opacity or yellow brown pigmented area. Ø Adjacent enamel appears bluish white.
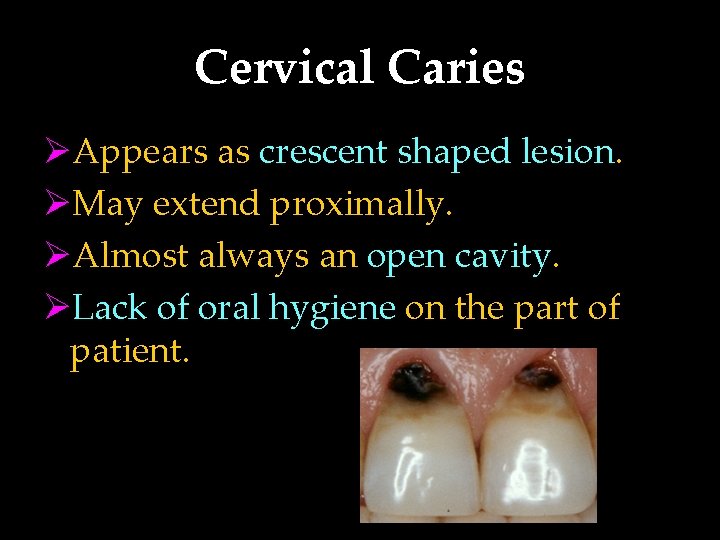
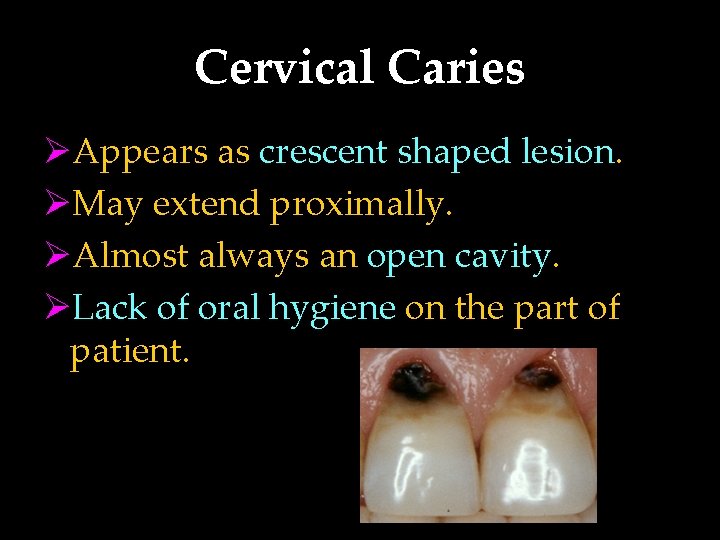
Cervical Caries ØAppears as crescent shaped lesion. ØMay extend proximally. ØAlmost always an open cavity. ØLack of oral hygiene on the part of patient.
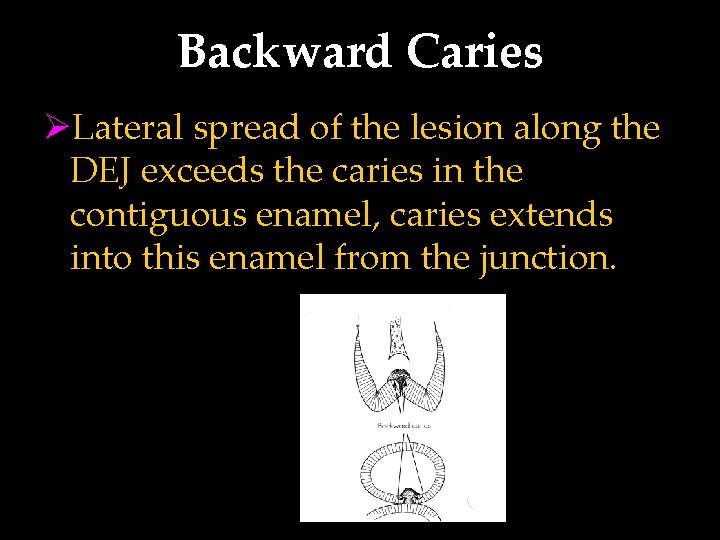
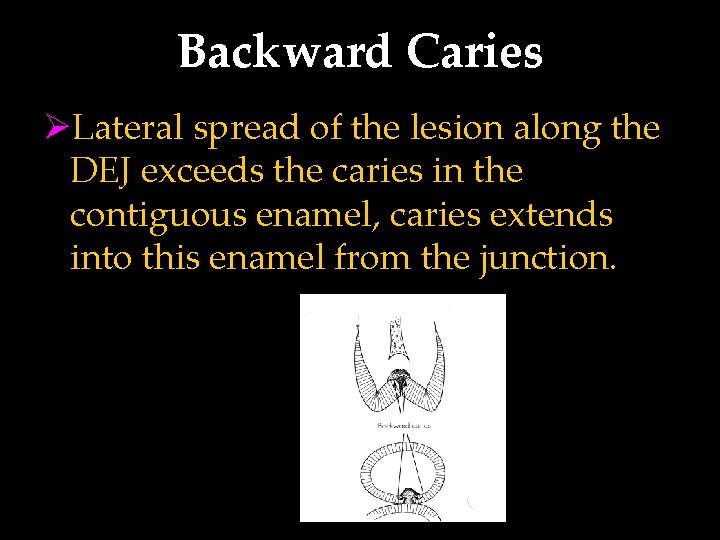
Backward Caries ØLateral spread of the lesion along the DEJ exceeds the caries in the contiguous enamel, caries extends into this enamel from the junction.
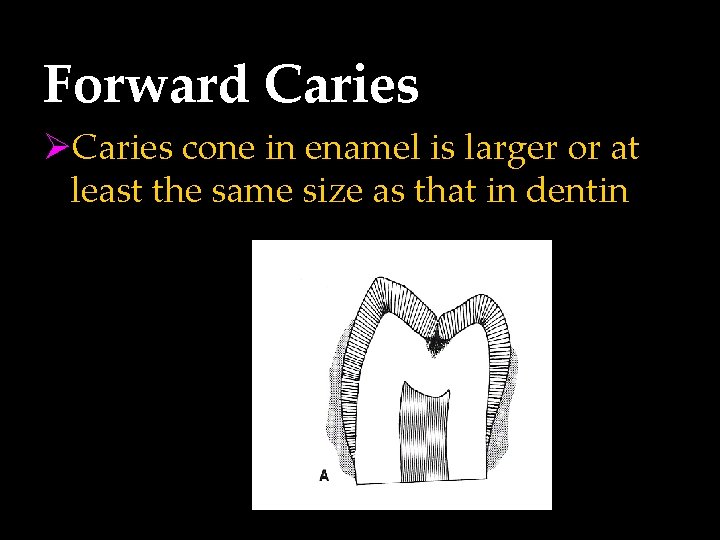
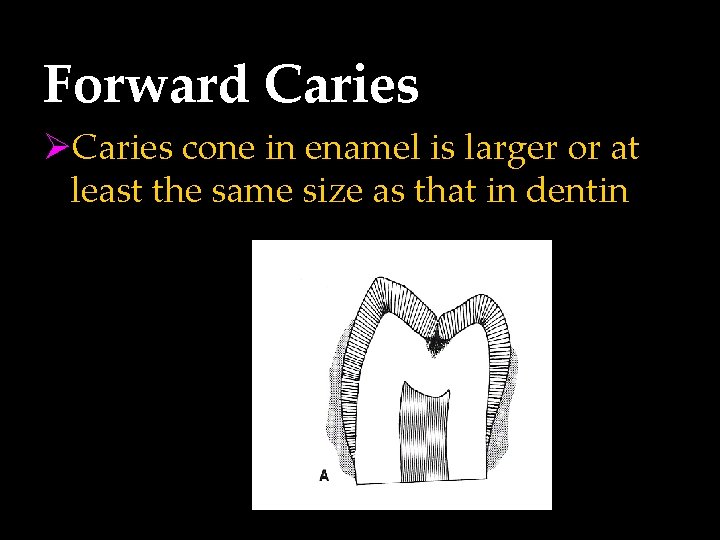
Forward Caries ØCaries cone in enamel is larger or at least the same size as that in dentin
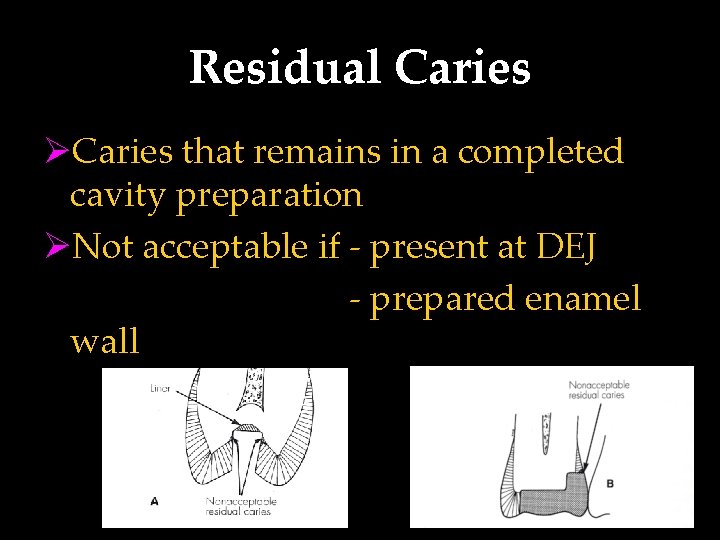
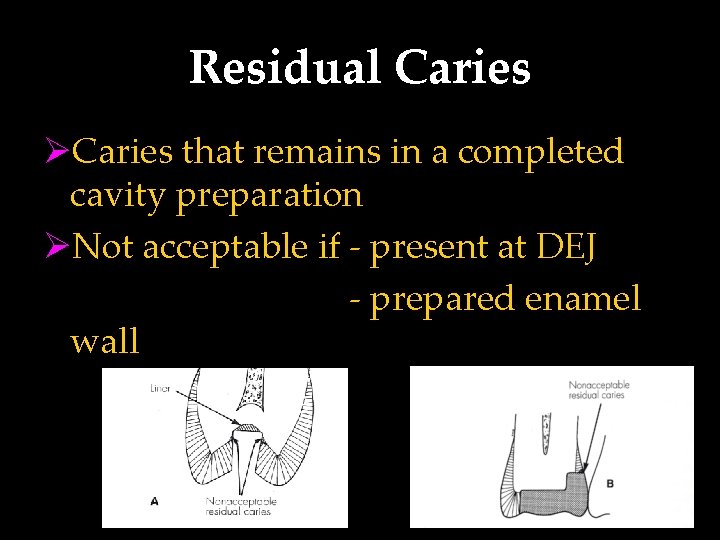
Residual Caries ØCaries that remains in a completed cavity preparation ØNot acceptable if - present at DEJ - prepared enamel wall

Root Surface Caries Ø In old age patients Ø Initiates at the surface of a mineralized dentin and cementum which have greater organic content Ø Usually have rapid clinical course
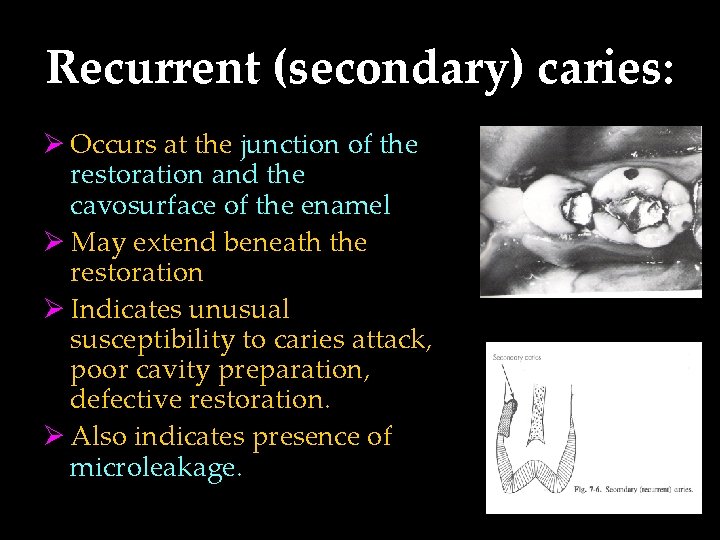
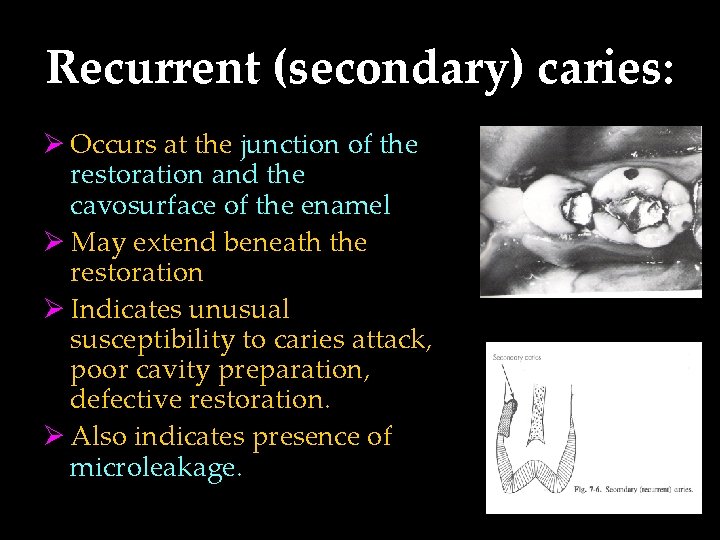
Recurrent (secondary) caries: Ø Occurs at the junction of the restoration and the cavosurface of the enamel Ø May extend beneath the restoration Ø Indicates unusual susceptibility to caries attack, poor cavity preparation, defective restoration. Ø Also indicates presence of microleakage.
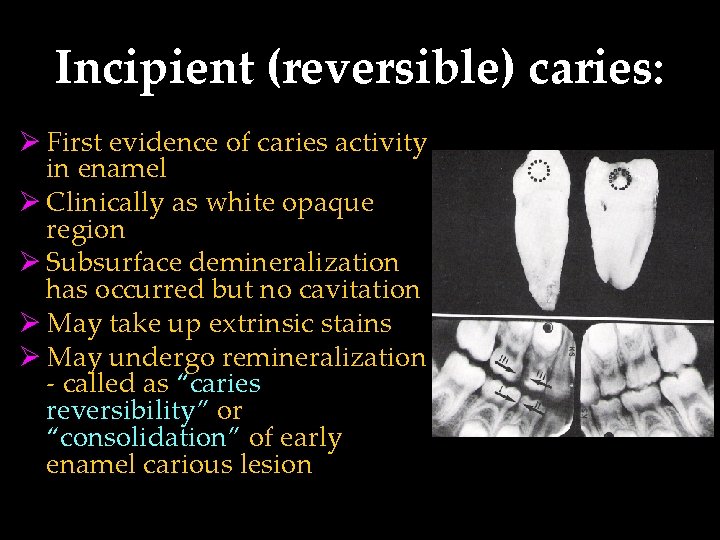
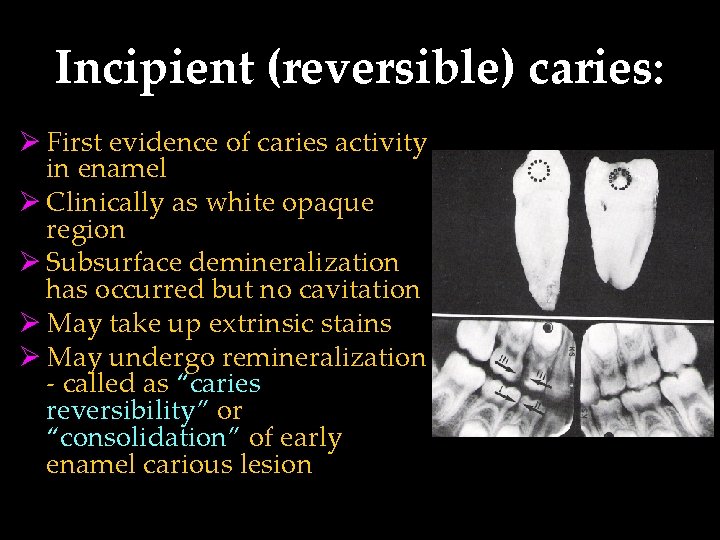
Incipient (reversible) caries: Ø First evidence of caries activity in enamel Ø Clinically as white opaque region Ø Subsurface demineralization has occurred but no cavitation Ø May take up extrinsic stains Ø May undergo remineralization - called as “caries reversibility” or “consolidation” of early enamel carious lesion
Cavitated (irreversible) caries: Ø Lesion that has advanced into dentin with broken surface Ø Remineralization is not possible Ø Treatment include cavity preparation and restoring with suitable material.
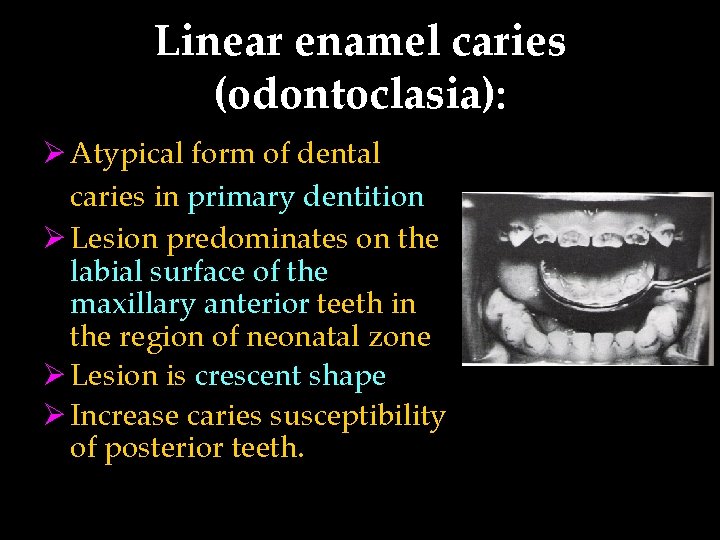
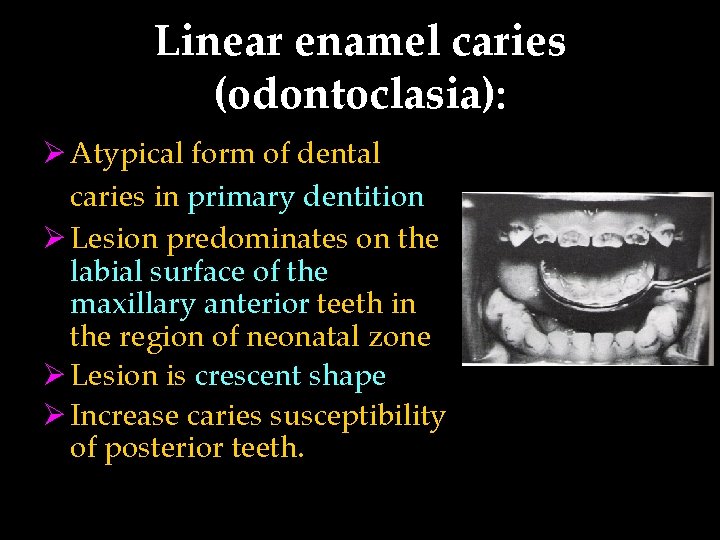
Linear enamel caries (odontoclasia): Ø Atypical form of dental caries in primary dentition Ø Lesion predominates on the labial surface of the maxillary anterior teeth in the region of neonatal zone Ø Lesion is crescent shape Ø Increase caries susceptibility of posterior teeth.
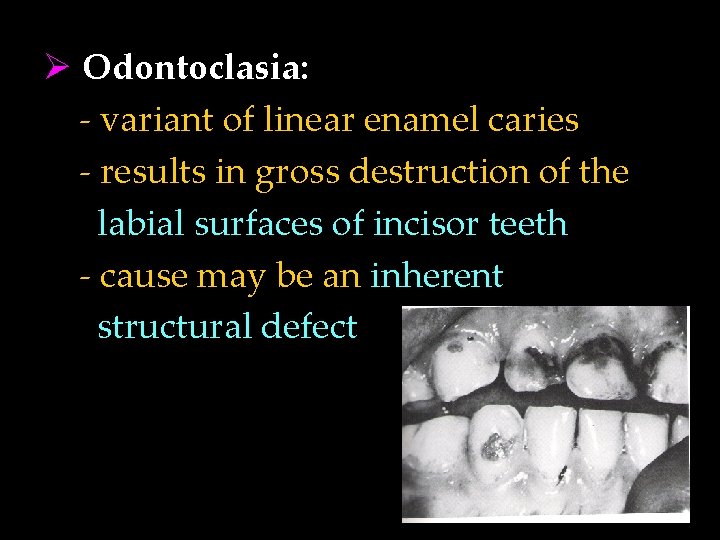
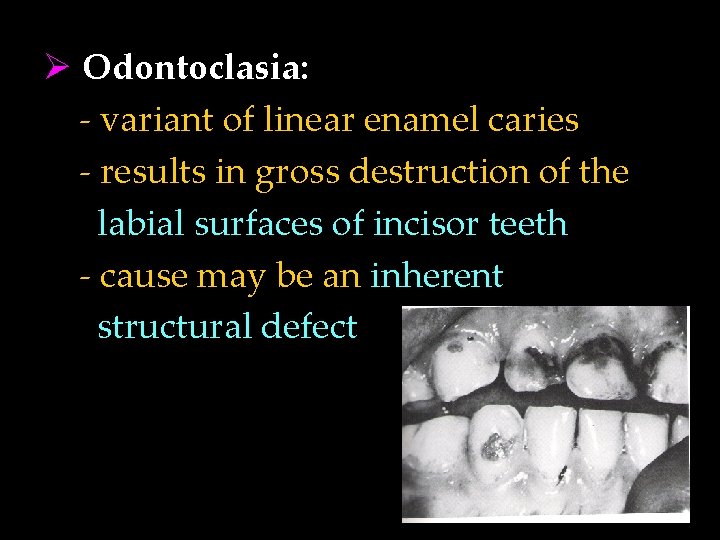
Ø Odontoclasia: - variant of linear enamel caries - results in gross destruction of the labial surfaces of incisor teeth - cause may be an inherent structural defect

Acute dental caries: Ø Rapid clinical course resulting in early pulp involvement Ø Frequently in children and young adults Ø Entry of lesion remains small while rapid spread along the DEJ Ø Clinically appears light yellow in colour Ø Pain is often present

Chronic dental caries ØSlowly progressive lesion that involves pulp much later ØCommon in adults ØLarge entrance of the lesion ØDentin is stained deep brown ØModerate lateral spread of caries at DEJ ØPain is not a common clinical finding.
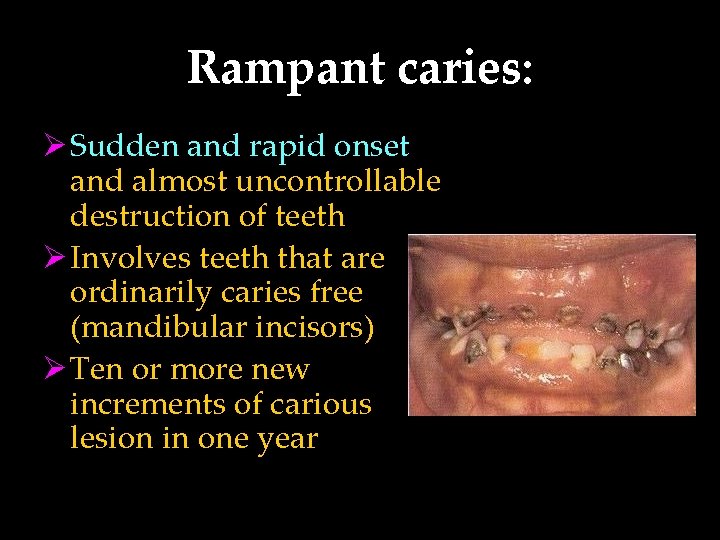
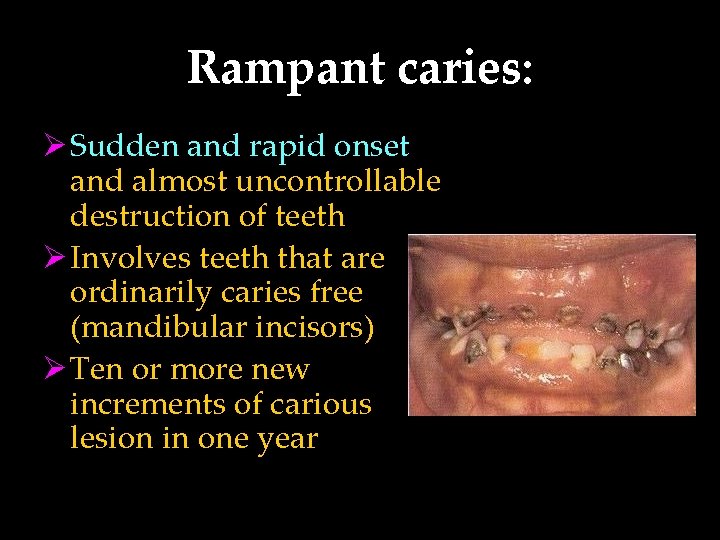
Rampant caries: Ø Sudden and rapid onset and almost uncontrollable destruction of teeth Ø Involves teeth that are ordinarily caries free (mandibular incisors) Ø Ten or more new increments of carious lesion in one year
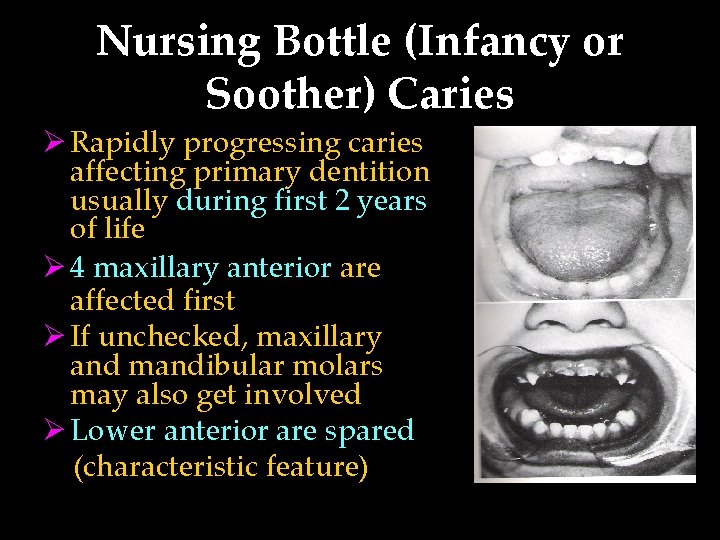
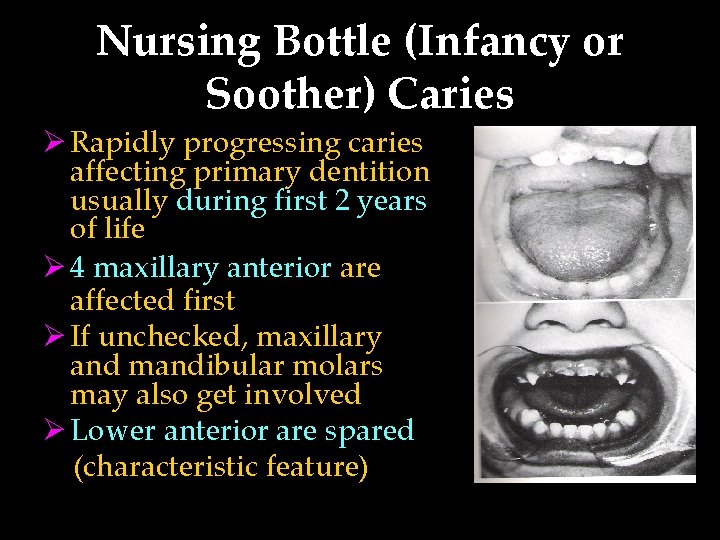
Nursing Bottle (Infancy or Soother) Caries Ø Rapidly progressing caries affecting primary dentition usually during first 2 years of life Ø 4 maxillary anterior are affected first Ø If unchecked, maxillary and mandibular molars may also get involved Ø Lower anterior are spared (characteristic feature)
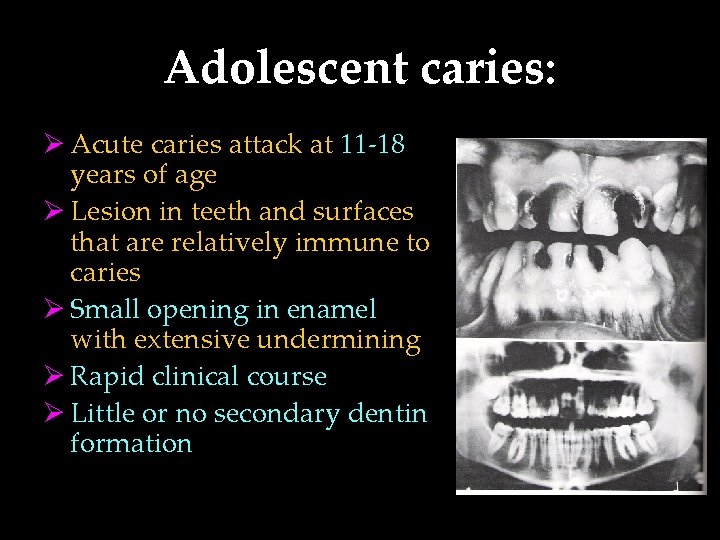
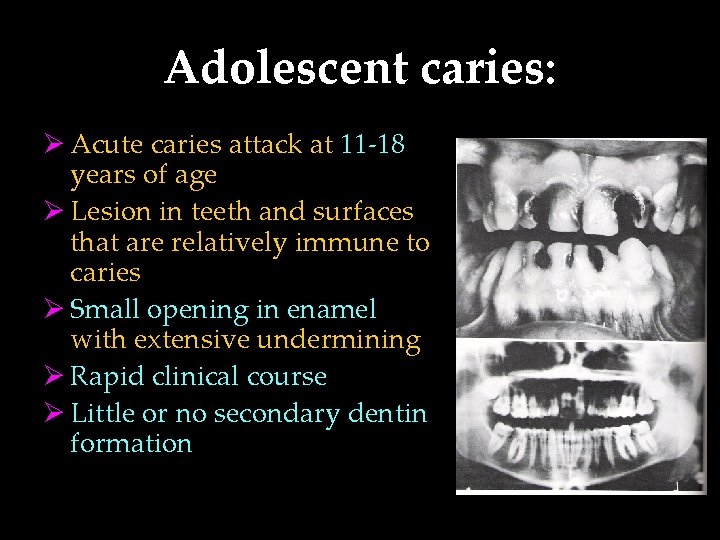
Adolescent caries: Ø Acute caries attack at 11 -18 years of age Ø Lesion in teeth and surfaces that are relatively immune to caries Ø Small opening in enamel with extensive undermining Ø Rapid clinical course Ø Little or no secondary dentin formation
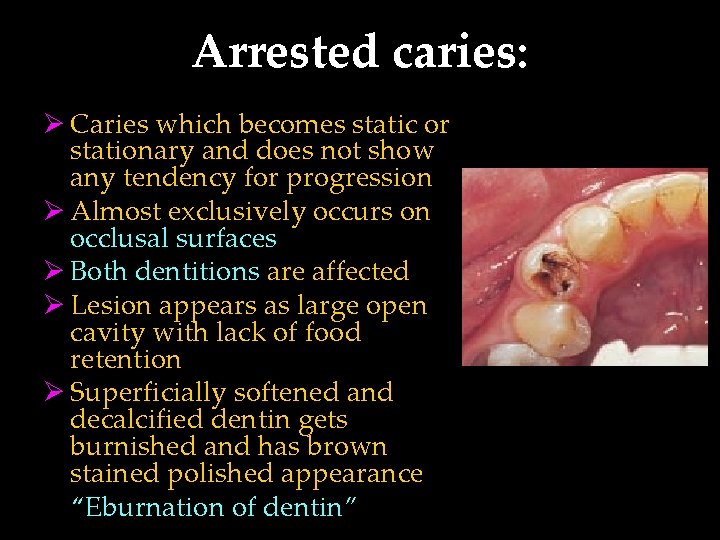
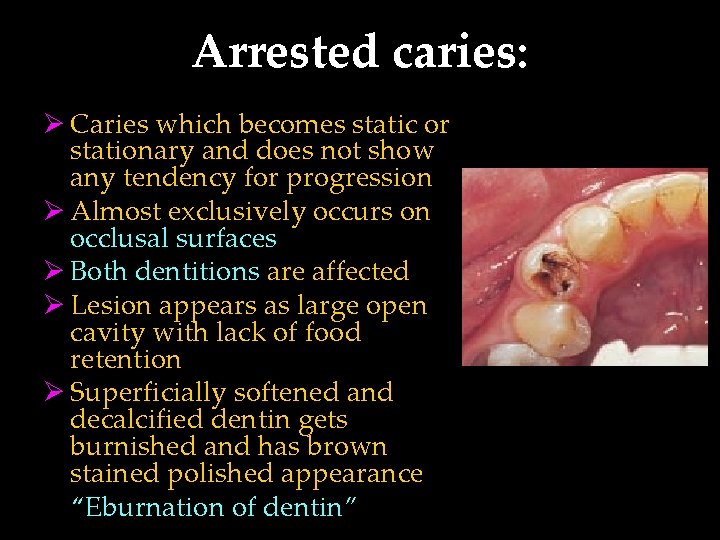
Arrested caries: Ø Caries which becomes static or stationary and does not show any tendency for progression Ø Almost exclusively occurs on occlusal surfaces Ø Both dentitions are affected Ø Lesion appears as large open cavity with lack of food retention Ø Superficially softened and decalcified dentin gets burnished and has brown stained polished appearance “Eburnation of dentin”
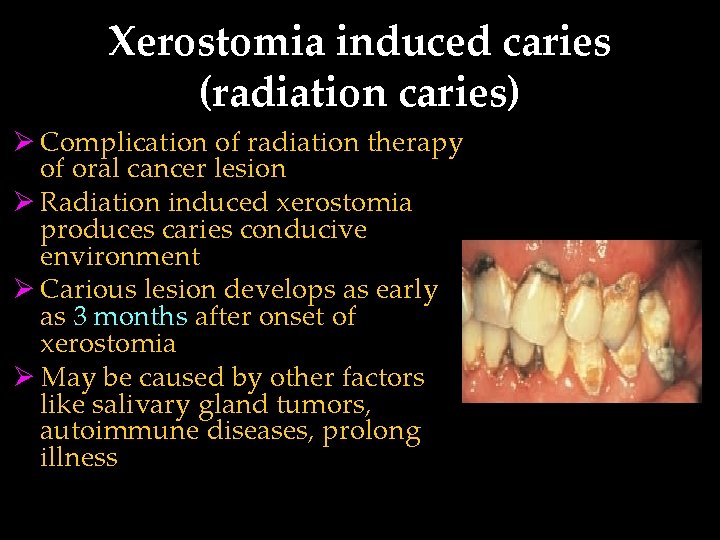
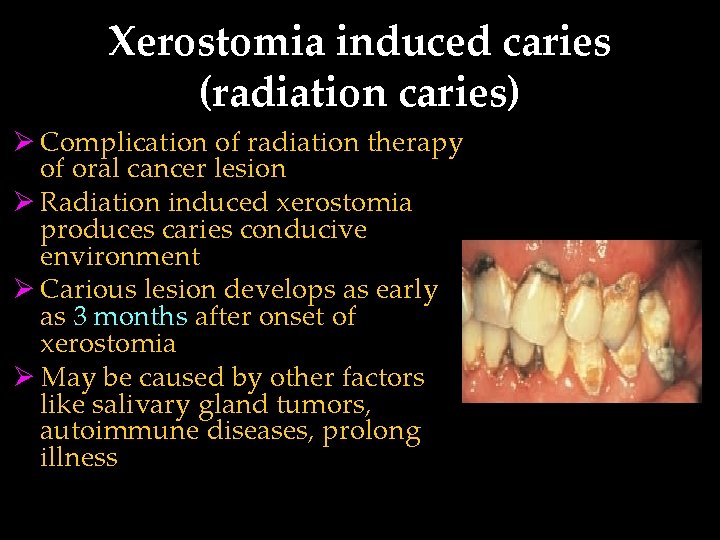
Xerostomia induced caries (radiation caries) Ø Complication of radiation therapy of oral cancer lesion Ø Radiation induced xerostomia produces caries conducive environment Ø Carious lesion develops as early as 3 months after onset of xerostomia Ø May be caused by other factors like salivary gland tumors, autoimmune diseases, prolong illness

Senile Caries ØCaries activity that spurts up during the old age. ØThey are located exclusively on the root surfaces of the teeth. ØAlso seen in association with partial denture clasps. ØCauses: gingival recession, decreased salivary secretion, poor oral hygiene.

Occult Caries / Hidden Caries • Not clinically diagnosed, but detected only on radiograph. • Seen in persons with low caries index suggestive of increased fluoride exposure. • Also called as fluoride bombs or fluoride syndrome

1. Simple caries: one surface is involved 2. Compound caries: two surfaces are involved 3. Complex caries: three or more surfaces are involved
ETIOLOGICAL THEORIES Early theories Endogenous theories Exogenous theories
EARLY THEORIES 1. The Legend of the Worm: • According to an ancient Sumerian text, tooth ache was caused by a worm that drank the blood of the teeth and fed on the roots of the jaws • Antony Van Leeuwenhock (1700) the father of modern microscopy wrote a letter to the Royal Society of London describing little worms taken out of a corrupt tooth and said that they caused the pain in tooth ache.
ENDOGENOUS THEORY • Humoral Theory “dental caries is produced by internal action of acid and corroding humors”. • Four elemental fluids of the body-blood, phlegm, black bile and yellow bile • Vital Theory “tooth decay originated, like bone gangrene, from within the tooth itself”
EXOGENOUS THEORY • Chemical (Acid) theory: “ teeth are destroyed by acids formed in the oral cavity ” • Parasitic (Septic) theory: “ microorganisms are associated with carious process ”
Acidogenic Theory § Proposed by W. B. Miller 1890, most accepted. § “Acids formed due to the fermentation of dietary carbohydrates by oral bacteria leads to progressive decalcification of tooth structure with subsequent disintegration of organic matrix. ”
§ He isolated micro-organisms from his experiments & stated that many were involved in the carious process. § 3 important factors which can influence process of tooth destruction in process of dental caries: Dietary carbohydrates, micro-organisms and acid
Proteolytic Theory § Proposed by Glottlieb in 1941. § “formation of dental caries is essentially proteolytic process. Bacteria present produce hydrolytic enzymes and cause proteolysis leading to the dissolution of organic substance. ” § Microorganisms invade the organic substance first.
§ He did admit that, acid formation accompanied the proteolysis. § Yellow pigmentation of dental caries is because of pigment production by proteolytic organism. § Caries is initiated at slightly alkaline p. H.
Proteolytic-chelation Theory § Proposed by Schwatz in 1955. § Stated that two processes are involved in caries – proteolysis & chelation.

§ Chelation is a process involving complexing of ions into a complexing substance by covalent bond which results in a highly stable, poorly dissociated and weekly ionized compound called chelate. § Bacterial attack on enamel is initiated by keratolytic microorganisms. § Eg: citrates, lactates § Chelates are always –ve.
Sucrose Chelation Theory • If there is a very high concentration of sucrose in mouth of a caries active individual, there can be formation of complexes like calcium saccharates, calcium complexing intermediaries, etc by action of phosphorylating enzymes • These complexes cause release of Ca, P ions from enamel and result in DC
Autoimmune Theory § Few odontoblast cells at specific sites within pulp of specific teeth are damaged by autoimmune mechanism § Due to this the defense capacity & integrity of of enamel and dentin in those specific areas are compromised and act as potential sites for caries development in future
Sulfatase Theory § Proposed by Pincus in 1951. § Bacterial sulfatases hydrolyses the mucoitin sulfate of enamel and chondroitin sulfate of dentin producing sulfuric acid that in turn causes decalcification. § Limitation: Sulfated polysacharide in enamel is very small and not readily accessible as a substrate for enzymatic degradation. So, this is highly unlikely hypothisis for the degragation of tooth enamel.
Levine’s theory § Proposed by Levine in 1977. § Established chemical relationship between enamel, plaque and factors which favors the movement of minerals between them. § Also called as “SEW – SAW” mechanism.
§ Said enamel demineralization and remineralization is a continuous process. § Movement of ions between enamel and plaque occurs in both direction which depend upon - plaque ph - calcium and phosphate ions at the interface - fluoride ion concentration
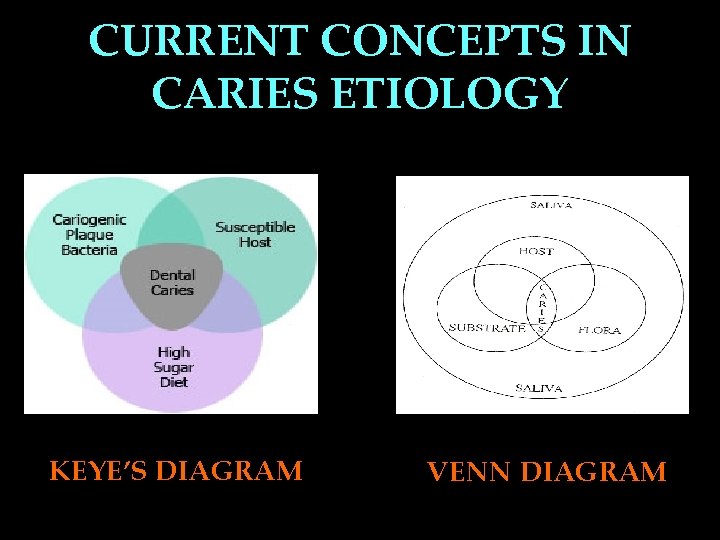
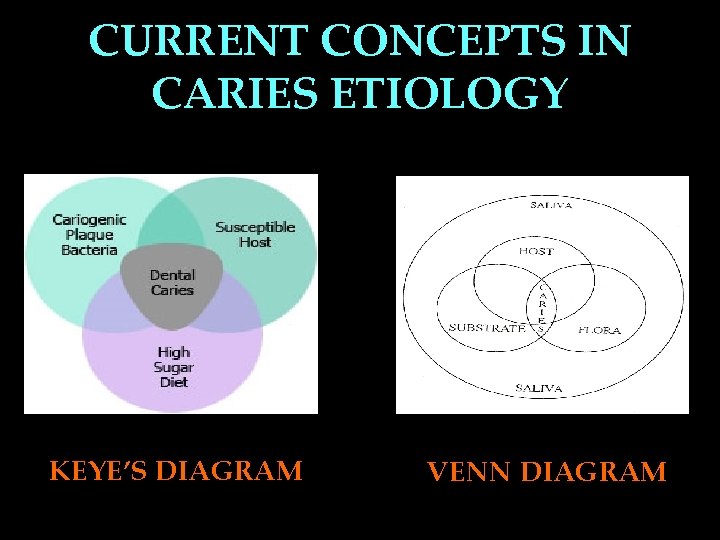
CURRENT CONCEPTS IN CARIES ETIOLOGY KEYE’S DIAGRAM VENN DIAGRAM
TEETH 1. • • • Morphology: Accentuated pits and fissures Enamel hypoplasia Mottled enamel 2. • • Position: Malpositioned teeth Rotated teeth
• Deep pits and fissures in any tooth make them susceptible to caries because of food impaction and bacterial stagnation. That is why most of the occlusal surfaces are prone to dental caries. • Mandibular first molars—most susceptible teeth followed by maxillary first molars then mandibular and maxillary second molars.

• Irregularities in the arch form, crowding and overlapping of the teeth also favour the development of caries. • Partially impacted third molars are more prone to caries and so are buccally or lingually placed teeth.

3. Composition: • Surface vs subsurface enamel
• Surface enamel is more caries resistant than the subsurface enamel. • The surface enamel has more minerals and more organic matter and relatively less water. • In addition certain elements such as fluoride, chloride, zinc lead etc accumulate more on the surface enamel than subsurface enamel.

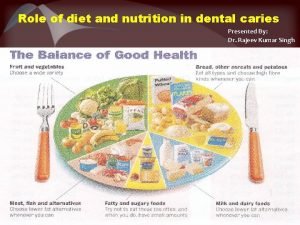
DIET • • 1. 2. 3. 4. 5. 6. Carbohydrate is a cariogenic diet Cariogenicity is based on Physical nature Chemical nature Mode of intake Clearance rate Frequency of intake Other dietary factors
PLAQUE AND MICROORGANISMS PLAQUE: • The concept about dental plaque was first proposed by Williams in 1897 • Consist of - salivary component- mucin - desquamated epithelial cells - microorganisms - calcium and phosphate
To produce caries, micro organisms should have following properties: 1. Should be acedogenic. 2. Should be aceduric. 3. Should posses attachment mechanism. 4. Should have the capacity to store sucrose. 5. Should be able to synthesize extracellular glucans.
1. Pioneer / primary bacteria – initiate caries • S. mutans (smooth surface caries) • Lactobacillus acidophilus (pit & fissure caries) • Actinomyces (root surface caries) 2. Invaders / secondary bacteria • Staphylococcus, Veillonellae
Streptococci mutans: • Chief etiological agent in dental caries disease 1. it can produce low p. H (acidogenic) 2. it can survive in low p. H (acidouric) 3. utilize sucrose at a faster rate than other bacteria 4. can metabolize sucrose to synthesize glucan and fructan ( attachment mechanism ) 5. it can store intracellular glycogen amylopectin type polysaccharides that act as a reservoir of substrate and prolongs its metabolic activity
Other Bacteria • Lactobacillus acidophilus – Found in carious dentin & saliva of persons with high caries activity – Release lactic acid • Actinomyces – Found esp. in root caries – Acidogenic – Attachment to tooth by glycoprotein called Lectin
Acids produced are a) Lactic acid b) Acetic acid c) Butyric acid d) Propionic acid e) Traces of formic acid • Lactic acid is the strongest acid
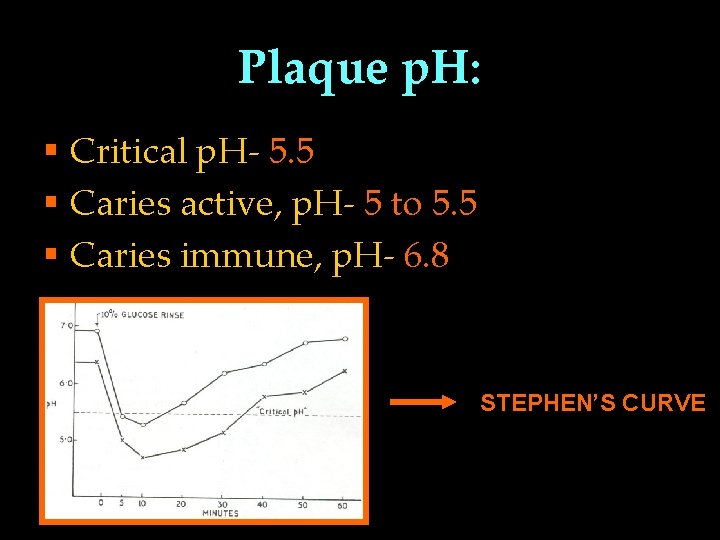
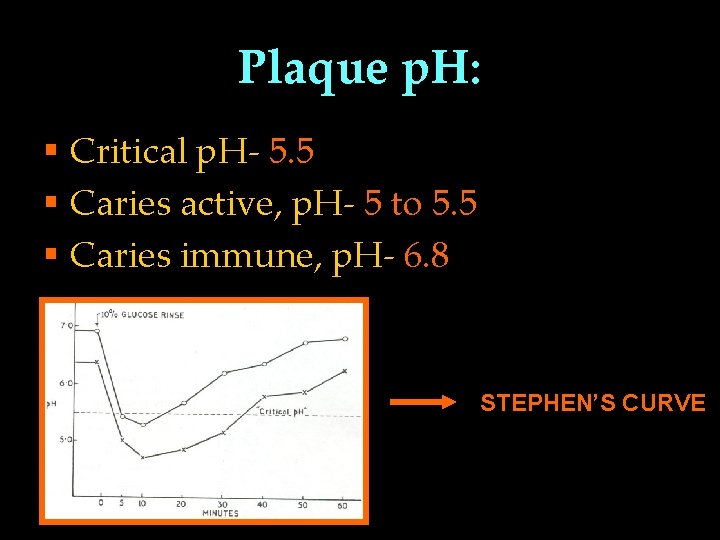
Plaque p. H: § Critical p. H- 5. 5 § Caries active, p. H- 5 to 5. 5 § Caries immune, p. H- 6. 8 STEPHEN’S CURVE
• The p. H at which any particular saliva ceases to be saturated with calcium and phosphorus is referred to as the critical p. H. Under normal conditions the critical p. H is 5. 5. • Below this value, the inorganic material of the tooth may dissolve.
• The normal p. H of resting saliva is 6 -7. • A buffer is a solution that tends to maintain a constant p. H. A fall in buffer capacity of saliva leads to increase in caries incidence.
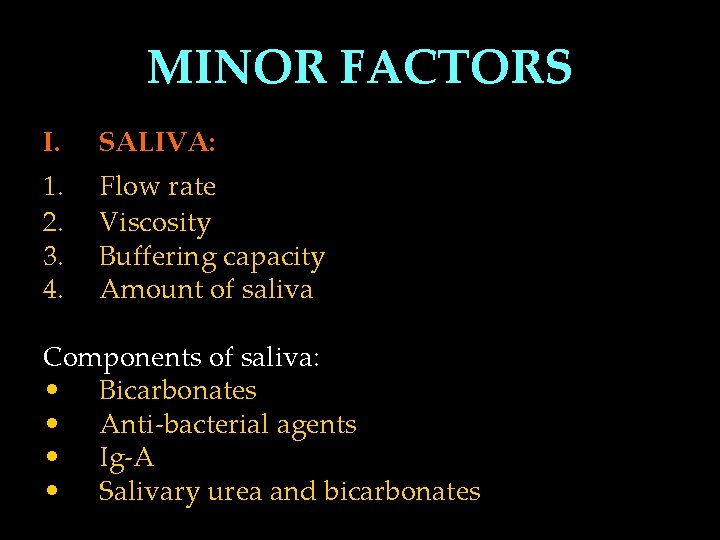
MINOR FACTORS I. SALIVA: 1. 2. 3. 4. Flow rate Viscosity Buffering capacity Amount of saliva Components of saliva: • Bicarbonates • Anti-bacterial agents • Ig-A • Salivary urea and bicarbonates
• The composition of saliva varies considerably. The conc of inorganic calcium and phosphorous shows considerable variation within resting and stimulated saliva. • Caries prone individuals have low calcium and phosphorous levels.
• Patients suffering from decreased flow of saliva or lack of salivary secretion usually have increased rate of dental caries. • Increased caries susceptibility is seen in patients following radiation therapy of mouth regardless of whether the teeth are present inside or outside the field of radiation, because of the decreased flow of saliva. Caries

• Certain drugs influence salivary flow and in turn result in rampant caries. • Drugs which may lead to xerostomia, either partial or total , include antidepressants, antihistamines etc. prolonged use of these drugs may cause dry mouth and extensive caries.
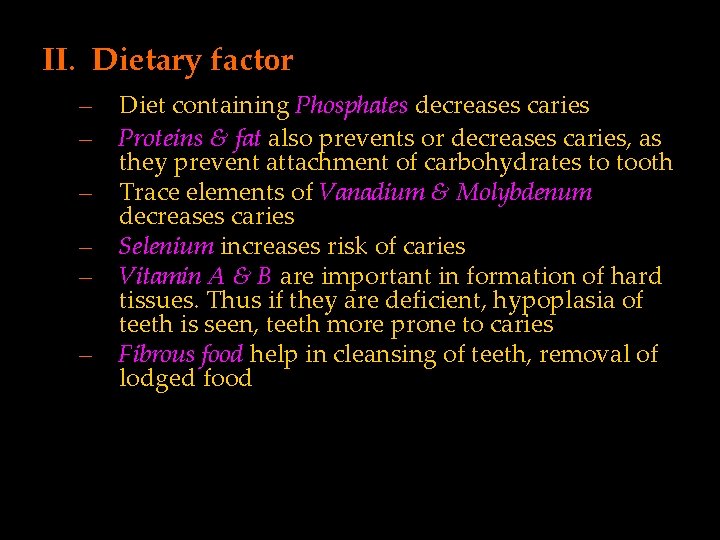
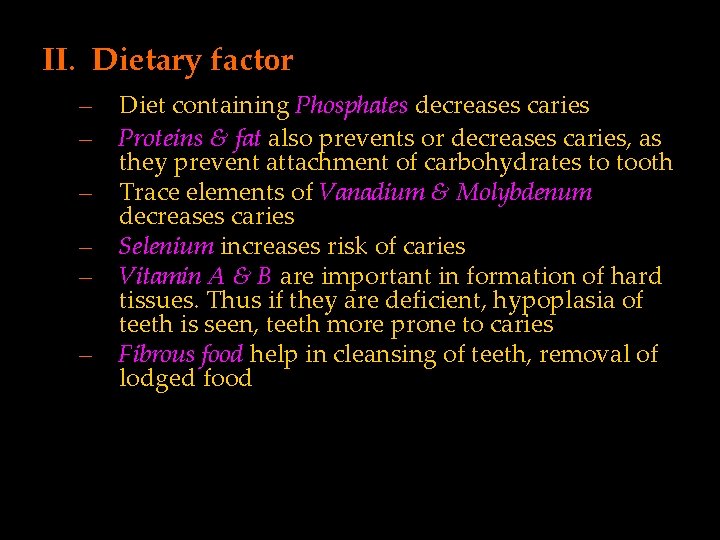
II. Dietary factor – – – Diet containing Phosphates decreases caries Proteins & fat also prevents or decreases caries, as they prevent attachment of carbohydrates to tooth Trace elements of Vanadium & Molybdenum decreases caries Selenium increases risk of caries Vitamin A & B are important in formation of hard tissues. Thus if they are deficient, hypoplasia of teeth is seen, teeth more prone to caries Fibrous food help in cleansing of teeth, removal of lodged food
• The physical nature of diet affects caries indirectly. The diet of the primitive man consisted of raw food including sand soil coatings which led to attrition and also cleansing the debris, thereby reducing the caries. • Modern diet includes refined foods, soft drinks and eatables, which lead to collection of debris predisposing to more caries.
• Furthermore, the mastication of food reduces the number of micro organisms. • Mechanical rubbing and cleaning definetly has role in caries reduction.

• III. Hereditary factors:
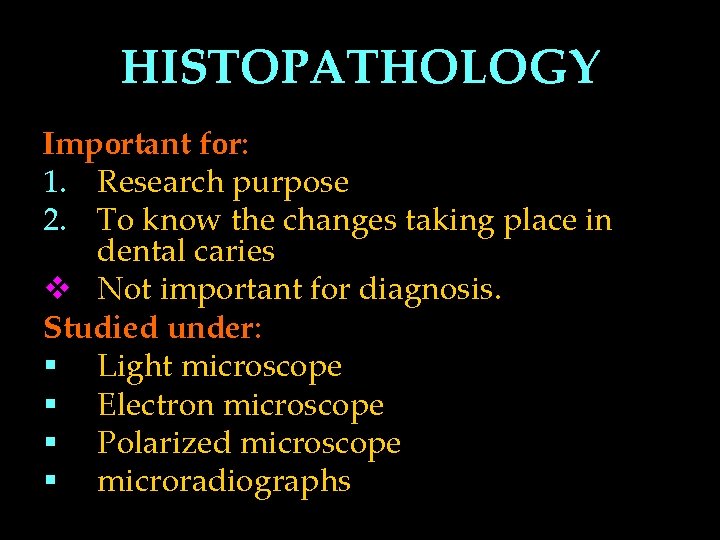
HISTOPATHOLOGY Important for: 1. Research purpose 2. To know the changes taking place in dental caries v Not important for diagnosis. Studied under: § Light microscope § Electron microscope § Polarized microscope § microradiographs
H/F of early enamel caries – Loss of inter-rod substance – prominent enamel-rods – Appearance of transverse striations of enamel rods due to segmental demineralization – Accentuation of incremental striae of Retzius
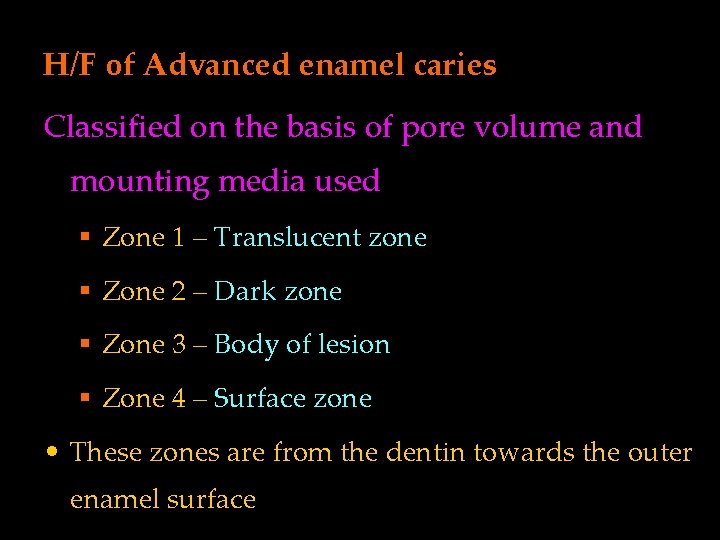
H/F of Advanced enamel caries Classified on the basis of pore volume and mounting media used § Zone 1 – Translucent zone § Zone 2 – Dark zone § Zone 3 – Body of lesion § Zone 4 – Surface zone • These zones are from the dentin towards the outer enamel surface
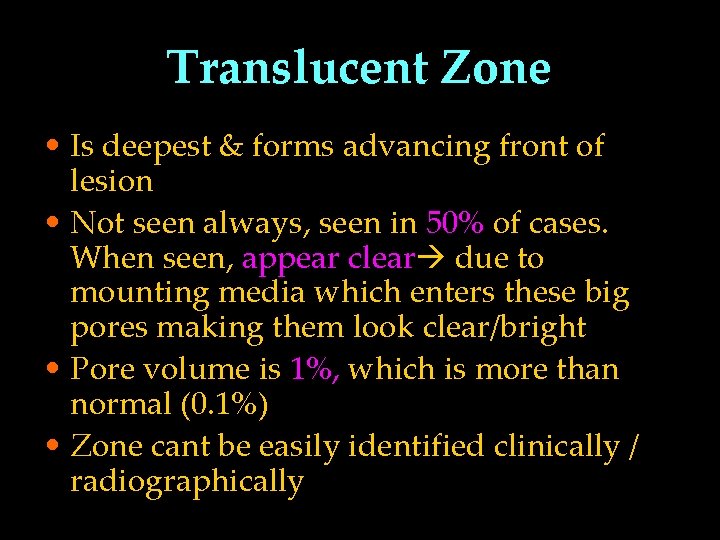
Translucent Zone • Is deepest & forms advancing front of lesion • Not seen always, seen in 50% of cases. When seen, appear clear due to mounting media which enters these big pores making them look clear/bright • Pore volume is 1%, which is more than normal (0. 1%) • Zone cant be easily identified clinically / radiographically
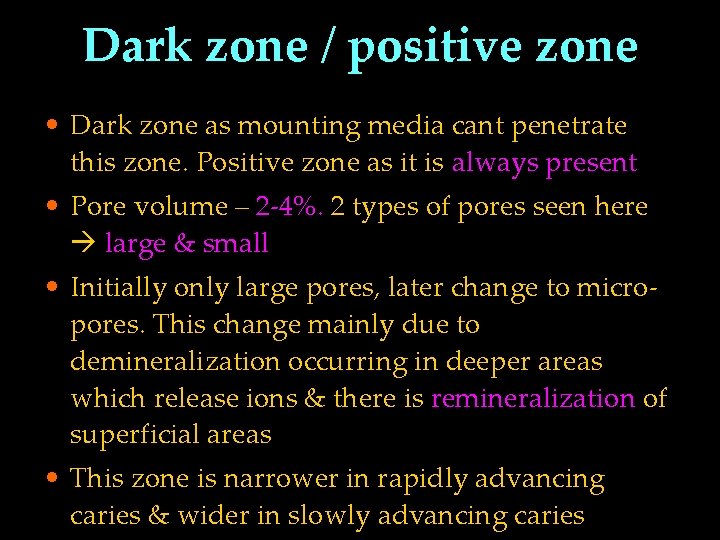
Dark zone / positive zone • Dark zone as mounting media cant penetrate this zone. Positive zone as it is always present • Pore volume – 2 -4%. 2 types of pores seen here large & small • Initially only large pores, later change to micropores. This change mainly due to demineralization occurring in deeper areas which release ions & there is remineralization of superficial areas • This zone is narrower in rapidly advancing caries & wider in slowly advancing caries
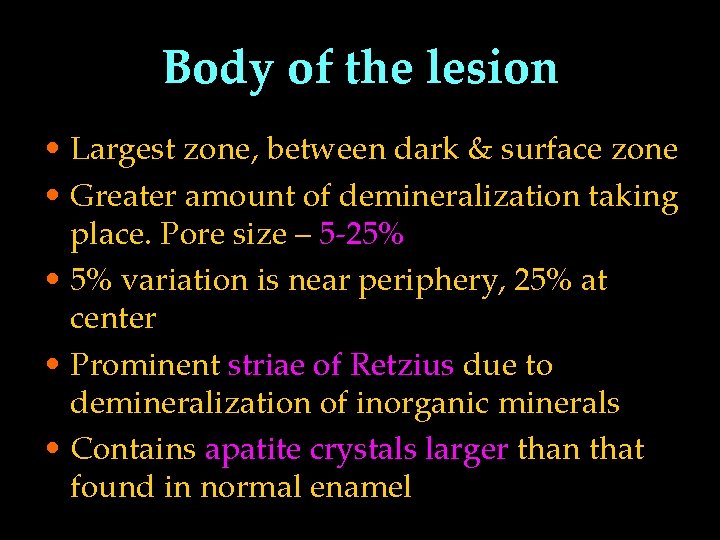
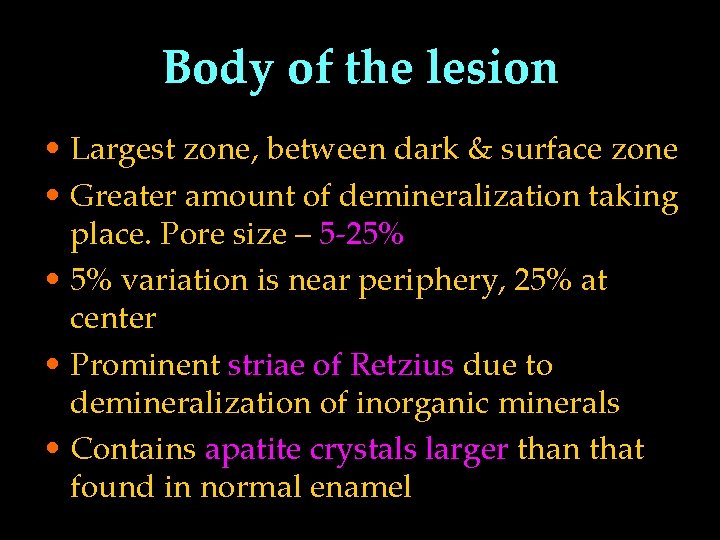
Body of the lesion • Largest zone, between dark & surface zone • Greater amount of demineralization taking place. Pore size – 5 -25% • 5% variation is near periphery, 25% at center • Prominent striae of Retzius due to demineralization of inorganic minerals • Contains apatite crystals larger than that found in normal enamel
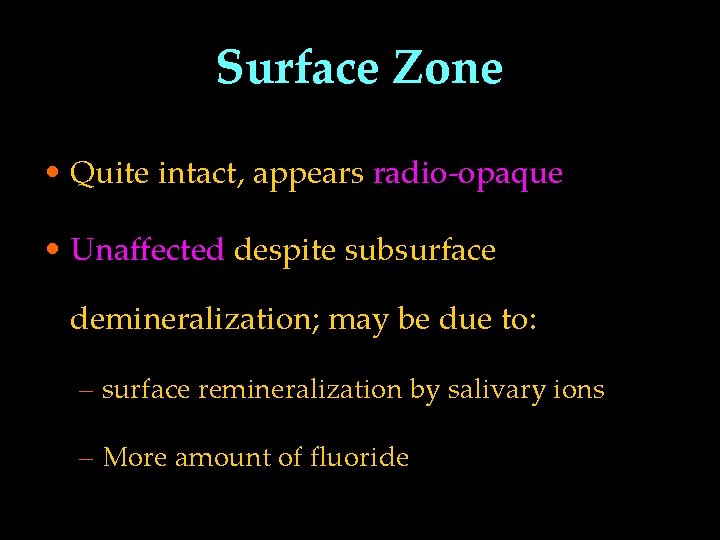
Surface Zone • Quite intact, appears radio-opaque • Unaffected despite subsurface demineralization; may be due to: – surface remineralization by salivary ions – More amount of fluoride
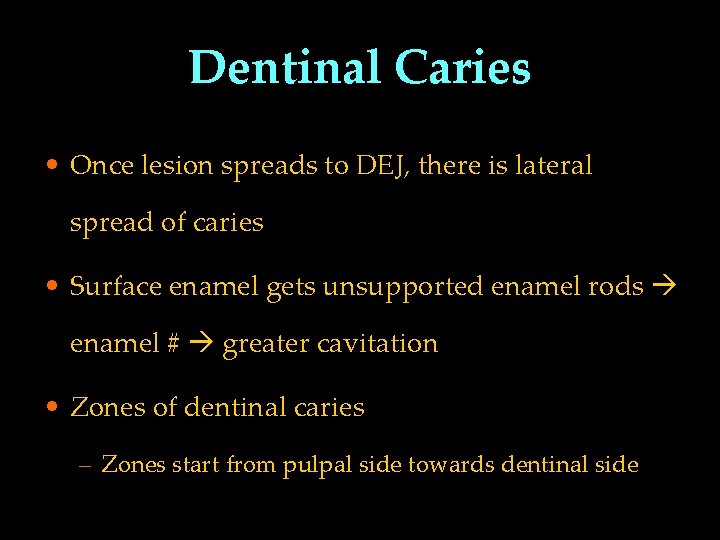
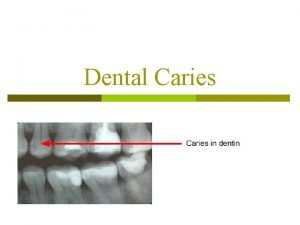
Dentinal Caries • Once lesion spreads to DEJ, there is lateral spread of caries • Surface enamel gets unsupported enamel rods enamel # greater cavitation • Zones of dentinal caries – Zones start from pulpal side towards dentinal side
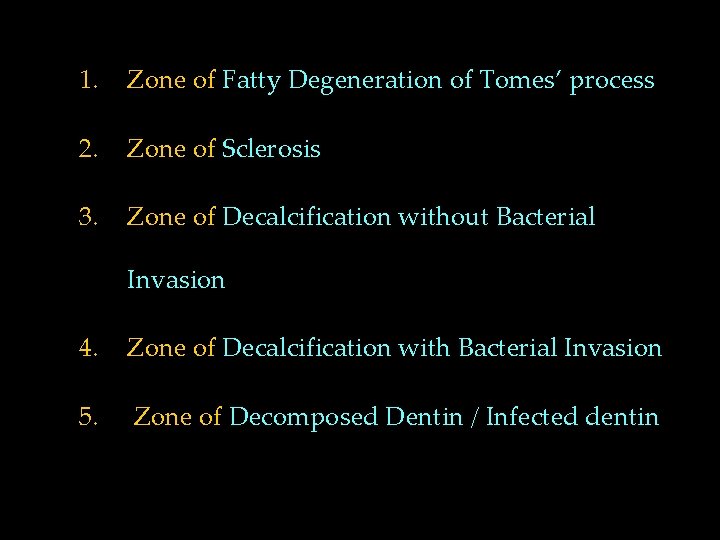
1. Zone of Fatty Degeneration of Tomes’ process 2. Zone of Sclerosis 3. Zone of Decalcification without Bacterial Invasion 4. Zone of Decalcification with Bacterial Invasion 5. Zone of Decomposed Dentin / Infected dentin
Fatty Degeneration of Tomes’ Process • Innermost layer of dentinal caries towards pulp • Due to deposition of fatty tissue in odontoblastic processes • Seen usually in rapidly progressing caries • No crystals or bacteria in lumen of tubules • Intertubular dentin normal
Zone of Sclerosis/Sub. Transparent Dentin § As the microorganisms cause destruction to dentin, initially there is an attempt to stop the advancement of caries by depositing the minerals. § There is a deposition of mineral in intertubular dentin. § Zone is called “transparent zone” § Odontoblasts are also start depositing dentin. § At the periphery of sclerotic dentin, dead tracts are present.
Zone of Decalcification without Bacterial Invasion / Transparent Dentin • Decalcification is by bacterial acid diffusion • Very narrow zone, softer than normal dentin • Further loss of minerals from inter tubular dentin • Large crystals within lumen of dentinal tubules
Zone of Decalcification with Bacterial Invasion / Turbid Dentin • Initially only few tubules are involved & microorgs also less • These are acidogenic, pioneer bacteria (initiators), present long before lesion is clinically detected • Bacteria multiply within tubules & are seen in advancing front of lesion
• Walls of tubules are thin & when microorgs penetrate, they cause irregularities/distensions of walls ROSARY BEAD appearance • Later, bacteria have proteolytic activity, areas of proteolysis appear as spaces containing necrotic material & bacteria • These areas “Liquefaction Foci of Miller”. • These areas vary in number & are parallel to dentinal tubules
Zone of Decomposed Dentin / Infected Dentin • Outermost zone, large scale destruction of dentin • Foci of Miller join together • Areas of dentin decomposition, occur perpendicular to dentinal tubules “Transverse Clefts”
• Mechanism of formation of Clefts - not known – May follow course of incremental lines or – May result from coalescence of liquefaction of adjacent tubules – Also may rise by extensive proteolytic activity along interconnecting lateral branches of odontoblastic processes • Bacteria shift from dentinal tubules to the peri & inter tubular dentin
Secondary / Reactionary dentin • Protective mechanism to protect pulp • Develops as a result of localized, non-specific irritation to odontoblasts • Hyper mineralized, less number of dentinal tubules having irregular & torturous course
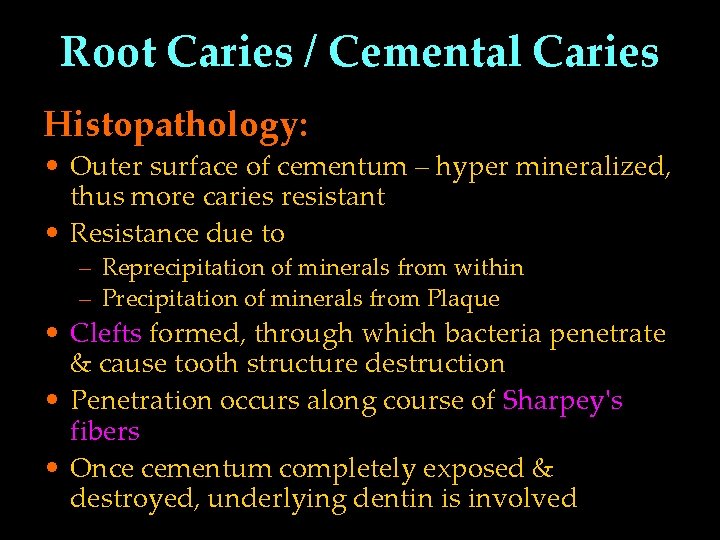
Root Caries / Cemental Caries Histopathology: • Outer surface of cementum – hyper mineralized, thus more caries resistant • Resistance due to – Reprecipitation of minerals from within – Precipitation of minerals from Plaque • Clefts formed, through which bacteria penetrate & cause tooth structure destruction • Penetration occurs along course of Sharpey's fibers • Once cementum completely exposed & destroyed, underlying dentin is involved
CONCLUSION
 Odontoclasia definition
Odontoclasia definition Mount and hume classification
Mount and hume classification Beaded dentinal tubules
Beaded dentinal tubules Dentobuff strip system
Dentobuff strip system Rampant caries definition
Rampant caries definition Gv black classification
Gv black classification Gj mount classification
Gj mount classification Hopewood house study ppt
Hopewood house study ppt Dental caries
Dental caries Zones of dentinal caries
Zones of dentinal caries G.v. black cavity preparation
G.v. black cavity preparation Define nutritional epidemiology
Define nutritional epidemiology Meaning of epidermiology
Meaning of epidermiology Prevalence definition epidemiology
Prevalence definition epidemiology Epidemiology definition
Epidemiology definition Contents introduction
Contents introduction Ukuran asosiasi dalam epidemiologi
Ukuran asosiasi dalam epidemiologi Logistic regression epidemiology
Logistic regression epidemiology Point and period prevalence
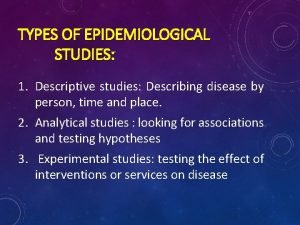
Point and period prevalence Descriptive vs analytic epidemiology examples
Descriptive vs analytic epidemiology examples Attack rate calculation
Attack rate calculation Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Person place and time model in epidemiology
Person place and time model in epidemiology Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Bibliography of epidemiology
Bibliography of epidemiology Recall bias example
Recall bias example Attack rate calculation
Attack rate calculation Gate frame epidemiology
Gate frame epidemiology Wheel theory of disease causation
Wheel theory of disease causation Defination of prevalence
Defination of prevalence Defination of epidemiology
Defination of epidemiology Epidemiology concept
Epidemiology concept What is descriptive study in epidemiology
What is descriptive study in epidemiology Spurious association in epidemiology
Spurious association in epidemiology Field epidemiology ppt
Field epidemiology ppt Level of prevention
Level of prevention Cbic recertification
Cbic recertification Gordon nichols
Gordon nichols Epidemiology kept simple
Epidemiology kept simple Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology Distribution in epidemiology
Distribution in epidemiology Effect modification vs confounding
Effect modification vs confounding Distribution in epidemiology
Distribution in epidemiology Ramboman analysis
Ramboman analysis How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Nutritional epidemiology
Nutritional epidemiology Epidemiology of malaria
Epidemiology of malaria Attack rate epidemiology
Attack rate epidemiology How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Seven uses of epidemiology
Seven uses of epidemiology Epidemiology triad
Epidemiology triad Celiac beri beri
Celiac beri beri Orlies
Orlies Introduction to nursing theories
Introduction to nursing theories An introduction to theories of learning
An introduction to theories of learning Mobility classification
Mobility classification Auxiliary dental materials examples
Auxiliary dental materials examples Burs classification
Burs classification Utility wax dental uses
Utility wax dental uses Composite chemistry definition
Composite chemistry definition Gingival margin trimmer dental instrument
Gingival margin trimmer dental instrument Permanent medicated filling
Permanent medicated filling Shape dental burs names and uses
Shape dental burs names and uses Efda in public health dentistry
Efda in public health dentistry Dicor
Dicor Topic
Topic Caries risk assessment form
Caries risk assessment form Universal tooth numbering system deciduous
Universal tooth numbering system deciduous Cervical burnout dental
Cervical burnout dental Caries ad pulpam penetrans
Caries ad pulpam penetrans Zone of caries
Zone of caries Mount and hume classification
Mount and hume classification Copyright
Copyright Que es caries
Que es caries Caries stabilization
Caries stabilization Detal caries
Detal caries Rci index dental
Rci index dental Modified bass
Modified bass Teoria del glucogeno de la caries
Teoria del glucogeno de la caries Teoria proteolisis quelacion
Teoria proteolisis quelacion Texas first steps
Texas first steps Dientes en pala
Dientes en pala Hidden caries
Hidden caries Caries
Caries Zinc amalgam is an alloy of
Zinc amalgam is an alloy of Medical model of caries management
Medical model of caries management Introduction to dental materials ppt
Introduction to dental materials ppt Introduction to dental materials
Introduction to dental materials Robert woofendale
Robert woofendale Types of utilitarianism
Types of utilitarianism Theoretical approaches to gender development
Theoretical approaches to gender development Psychodynamic theories definition
Psychodynamic theories definition