Demystifying Telephone Triage Dr Lucy Fisher NDUC Northern
- Slides: 35
Demystifying Telephone Triage Dr Lucy Fisher NDUC Northern Doctors Urgent Care L Fisher 2015
Demystifying Telephone Triage Why am I here tonight? L Fisher 2015
Demystifying Telephone Triage Why are you here tonight? L Fisher 2015
You already know it all L Fisher 2015
Aims To promote safe, efficient telephone consultations, with high patient satisfaction L Fisher 2015
Objectives 1. 2. 3. 4. 5. At the end of the talk we should have: Clarified what telephone triage and telephone consultations are. Compared and contrasted face to face, and telephone assessments. Reviewed the basic structure of a telephone triage. Considered what elements make for safe telephone triage and consultations. Gained experience in tricky triage situations. L Fisher 2015
Telephone Triage versus Telephone Consultation What’s the difference? L Fisher 2015
Telephone Triage versus Telephone Consultation Triage is the sorting of patients according to the urgency of their need for care. A Consultation is a meeting with a professional or expert for purposes of gaining information. L Fisher 2015
Similarities telephone cf. face to face 1. 2. 3. 4. 5. 6. 7. Preparation Introduction Information gathering Management/disposition plan Ending the consultation/Safety netting Time management Record keeping L Fisher 2015
A Telephone Triage Call What went well? What didn’t go well? L Fisher 2015
Telephone Triage: Basic Structure L Fisher 2015
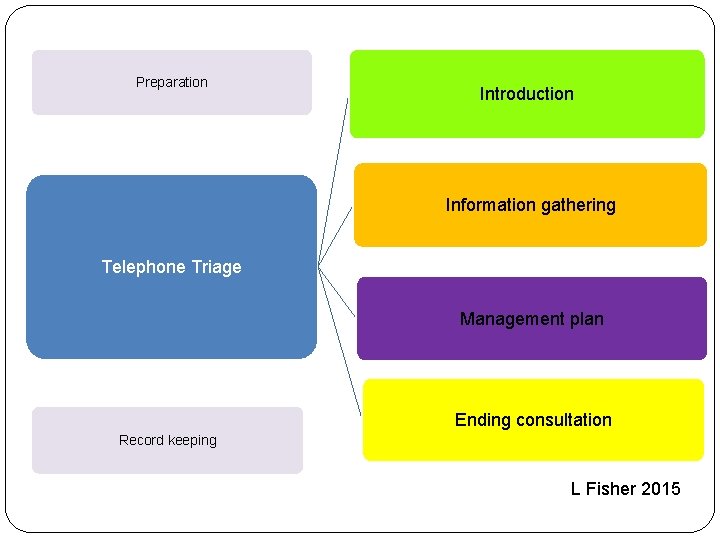
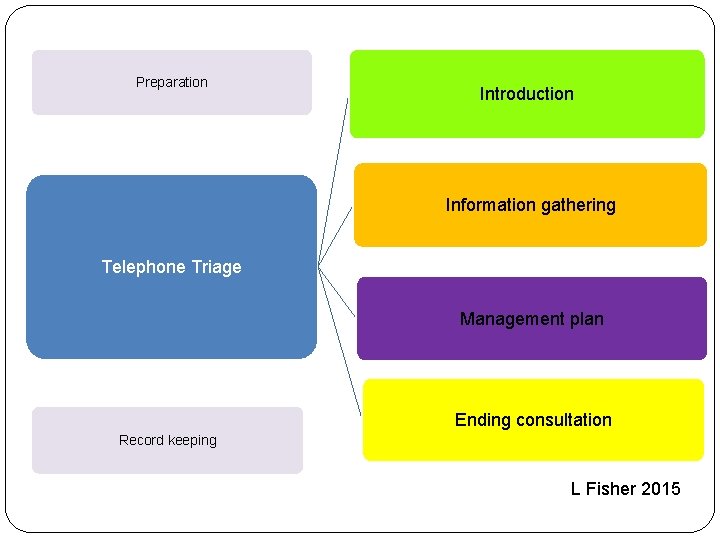
Preparation Introduction Information gathering Telephone Triage Management plan Ending consultation Record keeping L Fisher 2015
Telephone Triage: Basic Structure Preparation L Fisher 2015
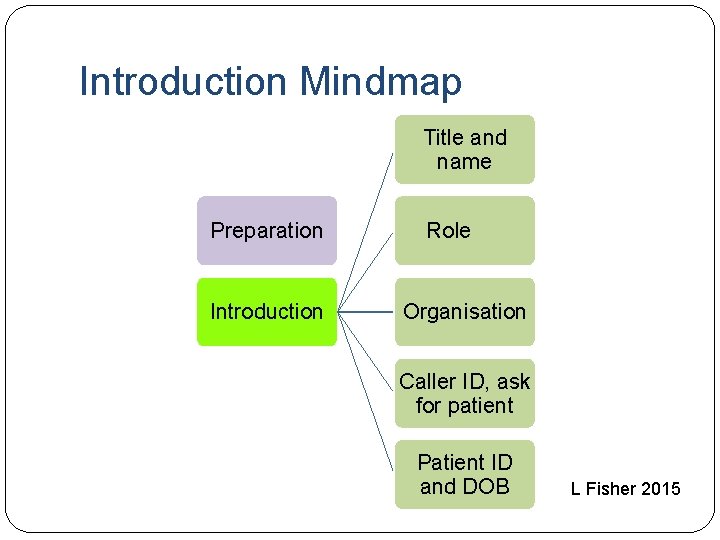
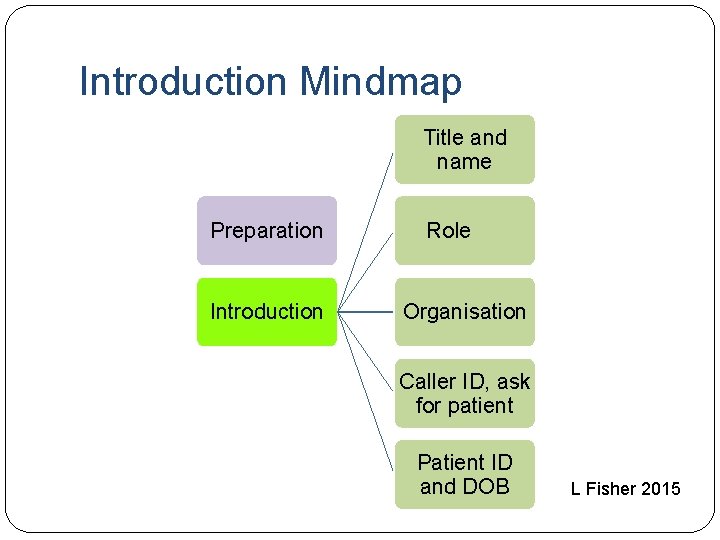
Introduction Mindmap Title and name Preparation Introduction Role Organisation Caller ID, ask for patient Patient ID and DOB L Fisher 2015
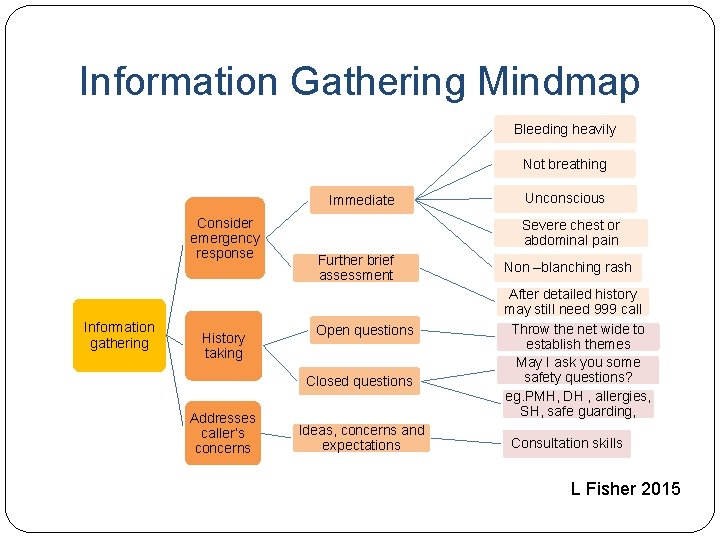
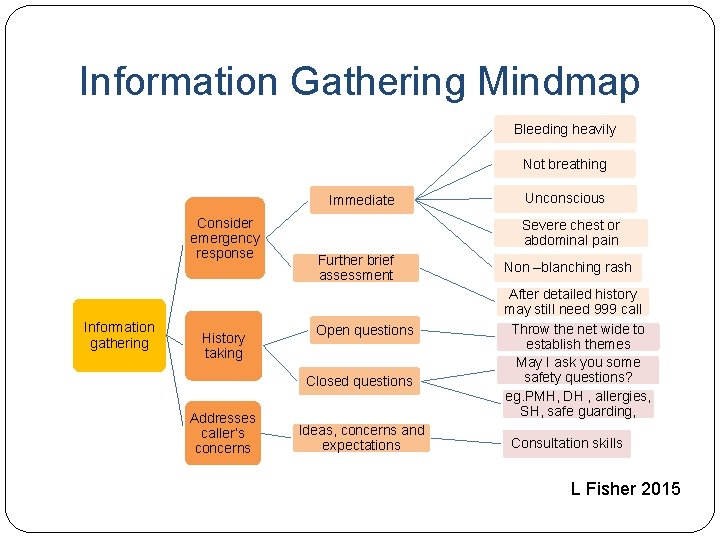
Information Gathering Mindmap Bleeding heavily Not breathing Immediate Consider emergency response Information gathering History taking Severe chest or abdominal pain Further brief assessment Open questions Closed questions Addresses caller’s concerns Unconscious Ideas, concerns and expectations Non –blanching rash After detailed history may still need 999 call Throw the net wide to establish themes May I ask you some safety questions? eg. PMH, DH , allergies, SH, safe guarding, Consultation skills L Fisher 2015
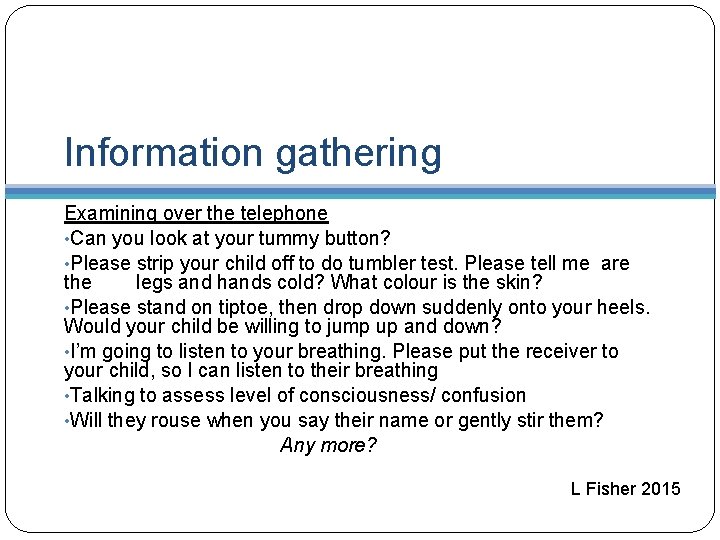
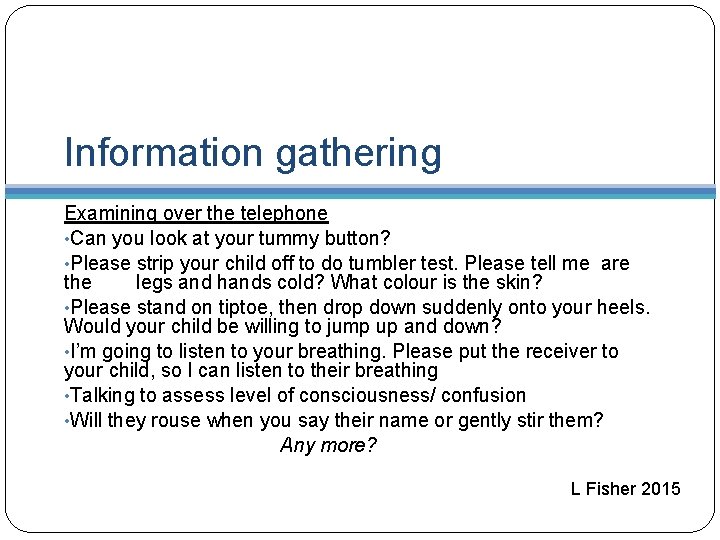
Information gathering Examining over the telephone • Can you look at your tummy button? • Please strip your child off to do tumbler test. Please tell me are the legs and hands cold? What colour is the skin? • Please stand on tiptoe, then drop down suddenly onto your heels. Would your child be willing to jump up and down? • I’m going to listen to your breathing. Please put the receiver to your child, so I can listen to their breathing • Talking to assess level of consciousness/ confusion • Will they rouse when you say their name or gently stir them? Any more? L Fisher 2015
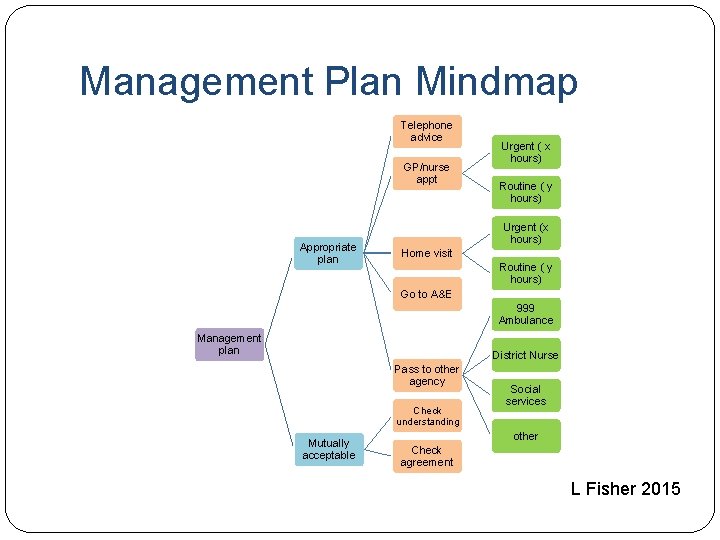
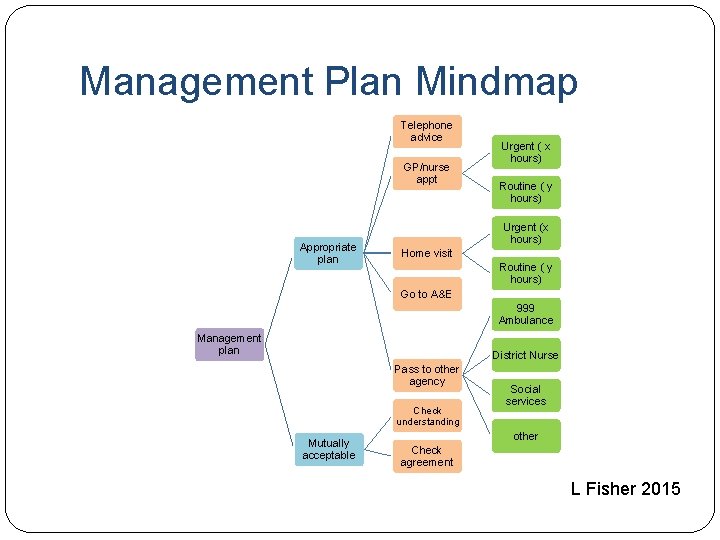
Management Plan Mindmap Telephone advice GP/nurse appt Appropriate plan Urgent ( x hours) Routine ( y hours) Urgent (x hours) Home visit Routine ( y hours) Go to A&E 999 Ambulance Management plan District Nurse Pass to other agency Check understanding Mutually acceptable Social services other Check agreement L Fisher 2015
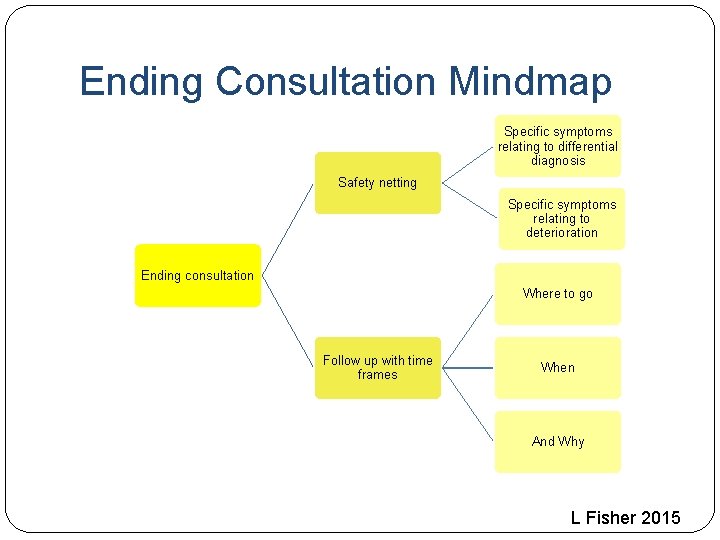
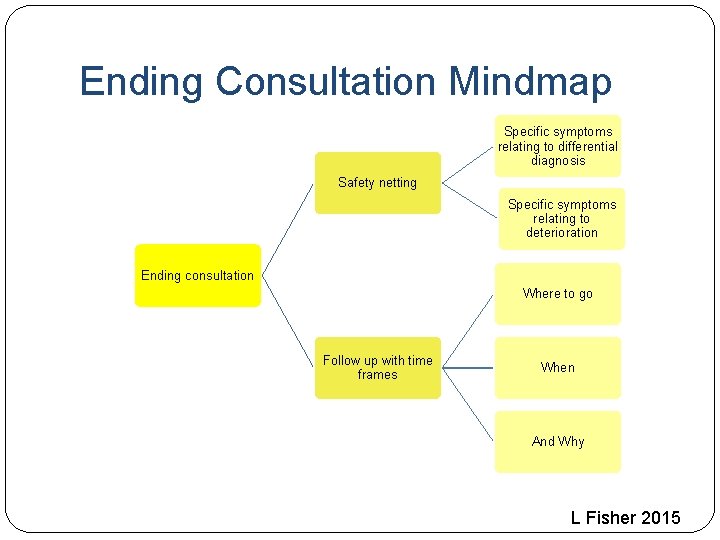
Ending Consultation Mindmap Specific symptoms relating to differential diagnosis Safety netting Specific symptoms relating to deterioration Ending consultation Where to go Follow up with time frames When And Why L Fisher 2015
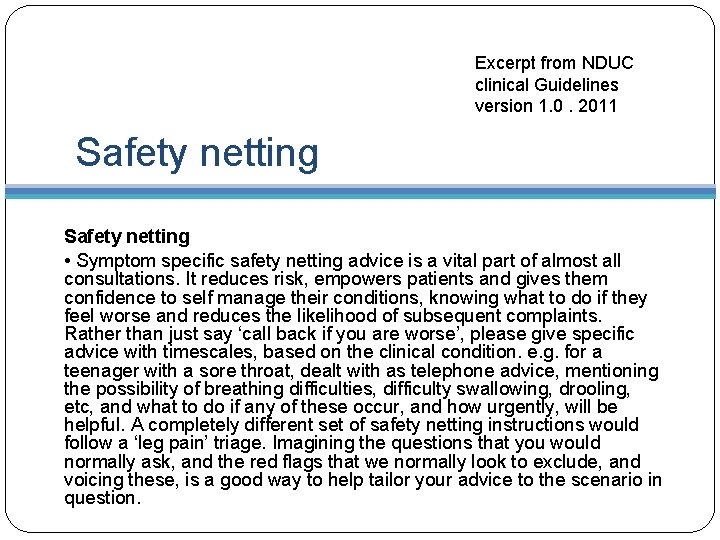
Excerpt from NDUC clinical Guidelines version 1. 0. 2011 Safety netting • Symptom specific safety netting advice is a vital part of almost all consultations. It reduces risk, empowers patients and gives them confidence to self manage their conditions, knowing what to do if they feel worse and reduces the likelihood of subsequent complaints. Rather than just say ‘call back if you are worse’, please give specific advice with timescales, based on the clinical condition. e. g. for a teenager with a sore throat, dealt with as telephone advice, mentioning the possibility of breathing difficulties, difficulty swallowing, drooling, etc, and what to do if any of these occur, and how urgently, will be helpful. A completely different set of safety netting instructions would follow a ‘leg pain’ triage. Imagining the questions that you would normally ask, and the red flags that we normally look to exclude, and voicing these, is a good way to help tailor your advice to the scenario in question.
Role Play Rehearsing some trickier situations. Applying knowledge from guidelines L Fisher 2015
Case 1 � 18 Month old with fever and diarrhoea L Fisher 2015
Case 1 �Which guidelines are useful in assessment and management? �Importance of eliciting ICE on patient satisfaction �Empowering self care L Fisher 2015
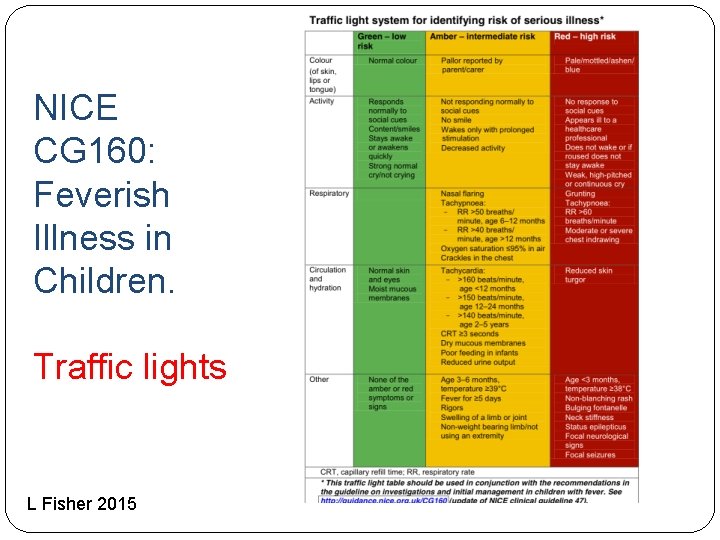
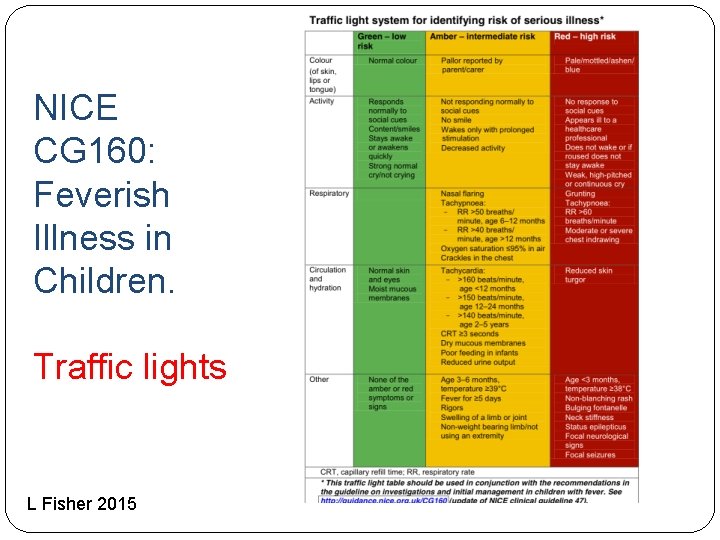
NICE CG 160: Feverish Illness in Children. Traffic lights L Fisher 2015
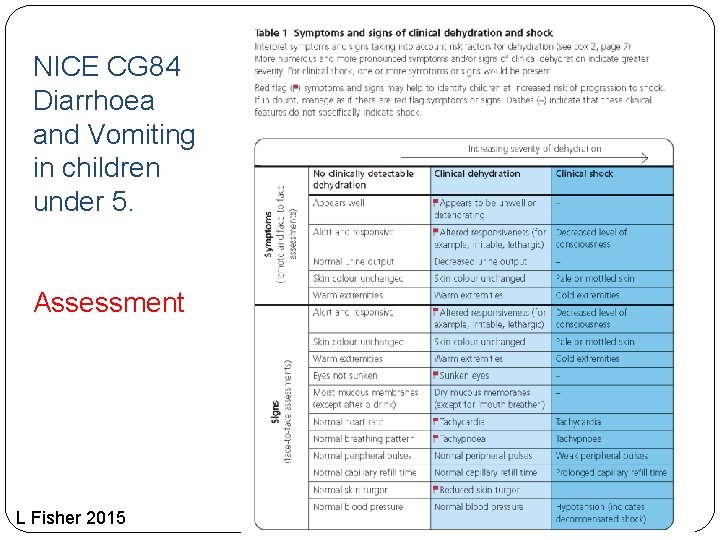
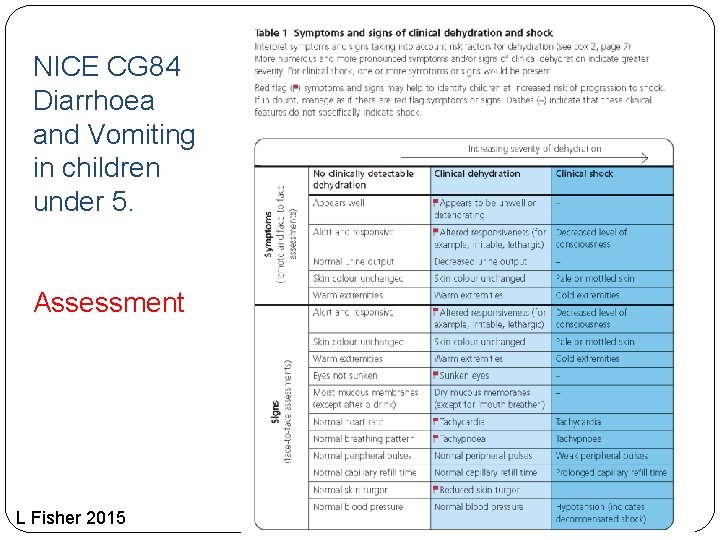
NICE CG 84 Diarrhoea and Vomiting in children under 5. Assessment L Fisher 2015
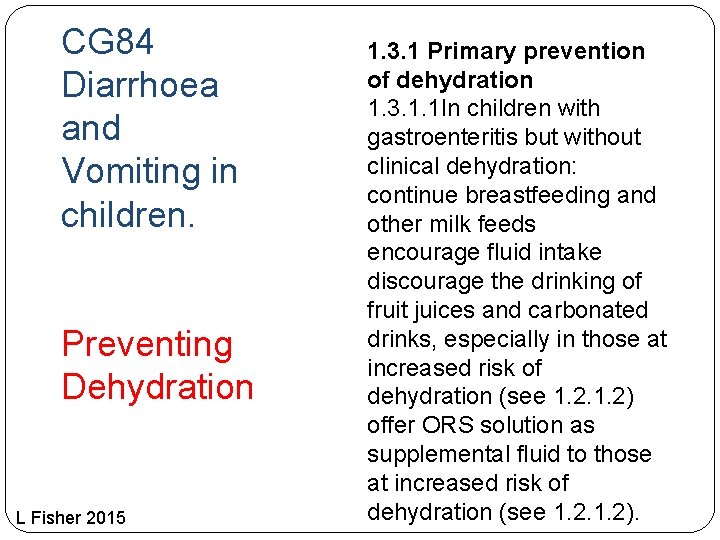
CG 84 Diarrhoea and Vomiting in children. Preventing Dehydration L Fisher 2015 1. 3. 1 Primary prevention of dehydration 1. 3. 1. 1 In children with gastroenteritis but without clinical dehydration: continue breastfeeding and other milk feeds encourage fluid intake discourage the drinking of fruit juices and carbonated drinks, especially in those at increased risk of dehydration (see 1. 2) offer ORS solution as supplemental fluid to those at increased risk of dehydration (see 1. 2).
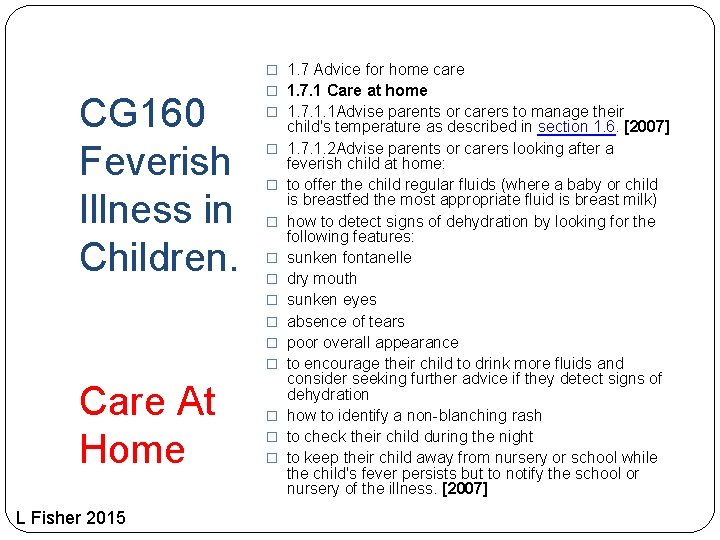
� 1. 7 Advice for home care CG 160 Feverish Illness in Children. � 1. 7. 1 Care at home � 1. 7. 1. 1 Advise parents or carers to manage their � � � � � Care At Home L Fisher 2015 � � � child's temperature as described in section 1. 6. [2007] 1. 7. 1. 2 Advise parents or carers looking after a feverish child at home: to offer the child regular fluids (where a baby or child is breastfed the most appropriate fluid is breast milk) how to detect signs of dehydration by looking for the following features: sunken fontanelle dry mouth sunken eyes absence of tears poor overall appearance to encourage their child to drink more fluids and consider seeking further advice if they detect signs of dehydration how to identify a non-blanching rash to check their child during the night to keep their child away from nursery or school while the child's fever persists but to notify the school or nursery of the illness. [2007]
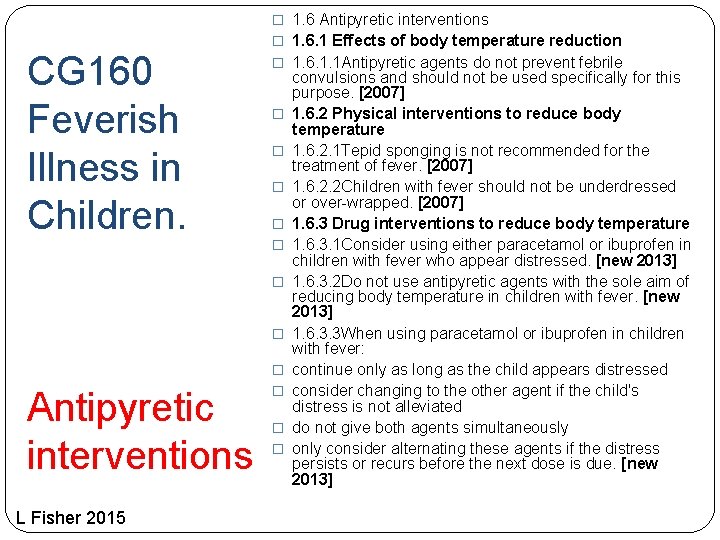
� 1. 6 Antipyretic interventions CG 160 Feverish Illness in Children. � 1. 6. 1 Effects of body temperature reduction � 1. 6. 1. 1 Antipyretic agents do not prevent febrile � � � � Antipyretic interventions L Fisher 2015 � � � convulsions and should not be used specifically for this purpose. [2007] 1. 6. 2 Physical interventions to reduce body temperature 1. 6. 2. 1 Tepid sponging is not recommended for the treatment of fever. [2007] 1. 6. 2. 2 Children with fever should not be underdressed or over-wrapped. [2007] 1. 6. 3 Drug interventions to reduce body temperature 1. 6. 3. 1 Consider using either paracetamol or ibuprofen in children with fever who appear distressed. [new 2013] 1. 6. 3. 2 Do not use antipyretic agents with the sole aim of reducing body temperature in children with fever. [new 2013] 1. 6. 3. 3 When using paracetamol or ibuprofen in children with fever: continue only as long as the child appears distressed consider changing to the other agent if the child's distress is not alleviated do not give both agents simultaneously only consider alternating these agents if the distress persists or recurs before the next dose is due. [new 2013]
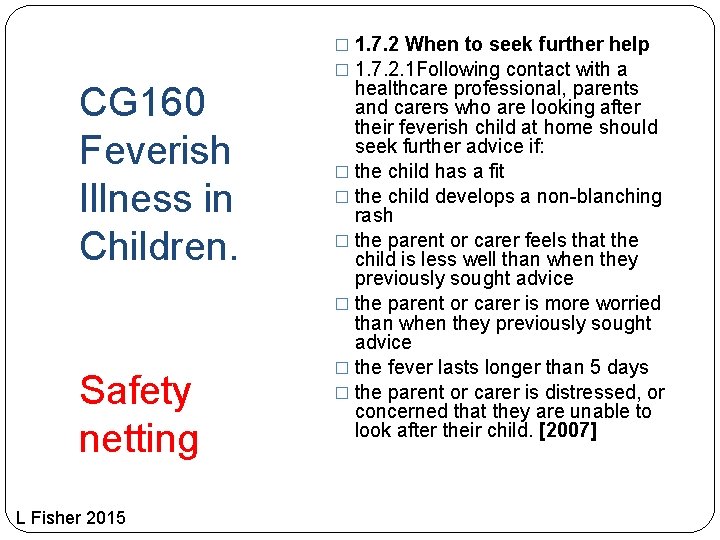
CG 160 Feverish Illness in Children. Safety netting L Fisher 2015 � 1. 7. 2 When to seek further help � 1. 7. 2. 1 Following contact with a healthcare professional, parents and carers who are looking after their feverish child at home should seek further advice if: � the child has a fit � the child develops a non-blanching rash � the parent or carer feels that the child is less well than when they previously sought advice � the parent or carer is more worried than when they previously sought advice � the fever lasts longer than 5 days � the parent or carer is distressed, or concerned that they are unable to look after their child. [2007]
Case 2 � 42 year old man with sore throat L Fisher 2015
Case 2 �Do you go back for the notes? �Did you ask to speak to the patient? (explanation) �Differential diagnoses and discriminating questions L Fisher 2015
GP Notebook �Epiglottitis • The symptoms of epiglottitis usually develop quickly and rapidly worsen. Symptoms include: • a high temperature (fever) of 38 C (100 F), or above, • a severe sore throat, • difficulty and pain when swallowing - most children will refuse to eat due to the pain, • difficulty breathing, • breathing that sounds abnormal and high pitched, • the skin takes on a bluish tinge (cyanosis), • voice sounds muffled, and • drooling saliva. L Fisher 2015
NHS choices symptom checker Symptoms of epiglottitis The symptoms of epiglottitis usually develop quickly and get rapidly worse, although they can develop over a few days in older children and adults. � Symptoms include: � a severe sore throat � difficulty and pain when swallowing � difficulty breathing, which may improve when leaning forwards � breathing that sounds abnormal and high pitched (stridor) � a high temperature (fever) of 38ºC (100. 4ºF) or above � irritability and restlessness � muffled or hoarse voice � drooling L Fisher 2015
Did we achieve our Objectives? 1. 2. 3. 4. 5. At the end of the talk we should have: Clarified what telephone triage and telephone consultations are. Compared and contrasted face to face, and telephone assessments. Reviewed the basic structure of a telephone triage. Considered what elements make for safe telephone triage and consultations. Gained experience in tricky triage situations. L Fisher 2015
Any Questions? L Fisher 2015
Thank you Please return all case scenarios and completed evaluation forms to me L Fisher 2015