DEMENTIA Notice and Agreement Class materials hereafter including
- Slides: 50
DEMENTIA
Notice and Agreement • • Class materials (hereafter including Power. Points, Handouts and Lecture Recordings) are distributed for the exclusive use of students in the Jerry M. Wallace School of Osteopathic Medicine. Student access to and use of materials are conditioned on agreement with the terms and conditions set out below. Any student who does not agree to them is prohibited from accessing or making any use of such materials. Any student accessing materials (1) acknowledges the faculty members’ intellectual property rights and that distribution of the materials violates the CUSOM Copyright Policy; (2) recognizes the privacy rights of fellow students who speak in class; (3) accepts that distributing, posting, or uploading materials to students or any other third party not authorized to receive them or to those outside CUSOM is an Honor Code violation; and (4) agrees that the materials are to be accessed and used only as directed by the faculty member(s) teaching the course. Students are not permitted to take photographs or screenshots of any screens or projected materials during lectures, exams or quizzes. Audio recording are also not permitted outside of what is provided through the recorded Tegrity sessions.
OBJECTIVES At the end of this presentation, learners will be able to: • Describe the definition of dementia. • Describe the epidemiology of dementia. • Recognize risk factors for dementia. • Recognize cognitive and behavioral symptoms of the various dementias.
OBJECTIVES (cont. ) • Understand the rationale of screening for dementia. • Describe specific Cognitive Assessment Screening Tools and their appropriate use. • Describe the pharmacological and nonpharmacological treatment of dementia.
Definition of Dementia • The progressive loss of cognitive and intellectual functions, without impairment of perception or consciousness, that is severe enough to interfere with the performance of everyday activities
Definition of AD • DSM-IV-TR definition for AD is based on the clinical criteria of multiple cognitive deficits, including memory impairment, assoc. with a decline in ability to carry out daily activities. The deficits must represent a decline from a previous level of functioning and occur in the absence of disturbed or clouded consciousness.
Epidemiology of 7 Dementia/AD • Approximately 6%-8% of persons older than 65 have AD. • Prevalence doubles every 5 years, so that nearly 30% of the population older than 85 has AD. • Approximately 5. 4 million Americans have AD currently. • That number will increase to 13. 5 million by 2050.
8 Epidemiology (con’t) • Dementia is the most important contributor to disability in the elderly. • Dementia contributed 10. 2% of years of disability in people aged at least 65 years. • Estimated worldwide cost of dementia is $604 billion (2010 US $$). • The US estimated cost of AD is $183 billion.
9 Epidemiology (con’t) • Dementia creates significant emotional and financial burden on caregivers as 70%-90% of Americans with dementia live at home. • Cost of informal care is valued at $202 billion/year. • 230, 00 people with Dementia live in nursing homes, comprising approx. 15% of the NH population.
10 Epidemiology (con’t) • Dementia is progressive in nature, leading to severe functional and cognitive decline. • Dementia results in increased comorbid disease and is a major determinant of institutionalization and mortality in the elderly. • Dementia has a significant impact on caregivers, and healthcare systems and their resources.
IMPACT • Dementing illnesses have significant impact on their victims, families, caregivers & society. • Most elderly with dementia become progressively functionally dependent for their IADLs & ADLs.
Functional Dependence = ↓Quality of life ↑Costs ↑Mortality ↑Caregiver stress ↑Risk of elder abuse/neglect
Risk Factors 13 for AD • Advancing age • Family history • Genetic mutations: apolipoprotein E-4 gene, Down’s syndrome • Atherosclerotic vascular changes • Head trauma • Female sex • Lower educational level
Common Causes of Dementia • Mild Cognitive Impairment (MCI) • Alzheimer’s Disease (AD) • Frontotemporal Dementia (FTD) • Vascular Dementia • Lewy Body Dementia (LBD) • Mixed Dementia *Often the dementia will have more than one degenerative cause.
Mild Cognitive Impairment (MCI) • Characterized by memory complaint and objective memory impairment with other cognitive domains and IADLs intact. • May represent a “pre-dementia state” • Conversion rates to AD may range 12% to 15% a year and up to 80% in 6 years
MCI (cont. ) • MCI criteria have expanded to include ‘nonamnestic’ MCI (e. g. language, executive function) that may place one at risk for developing another form of dementia (e. g. vascular or fronto-temporal dementia) • Persons with non-amnestic multi-domain MCI are more likely to develop non-AD dementia
Screening tests for MCI • Thorough neuropsychological evaluation that measures delayed recall, executive function, and language skills. • Montreal Cognitive Assessment (Mo. CA) has shown some promise to distinguish normal controls from MCI and MCI from early AD
TREATMENT • Pharmacological: treatment with cholinesterase inhibitors may slow progression. • Non-pharmacological: Exercise, diet, BP control, social involvement/stimulation
Alzheimer’s Disease (AD) • Most common of the dementing illnesses accounting for 50 – 75% of cases • An irreversible degenerative brain disorder that progresses gradually (onset → death ≈10 years). • Hallmark of AD at autopsy is the presence of amyloid plaques and neurofibrillary tangles • The result of both is progressive neuronal death
Cardinal Symptoms of AD: • • Amnesia (memory impairment) Aphasia (language disturbances) Agnosia (impaired ability to recognize/identify objects) Apraxia (difficulty performing motor activities) Disturbance in executive function Impairment in social and occupational function Slow progressive cognitive decline
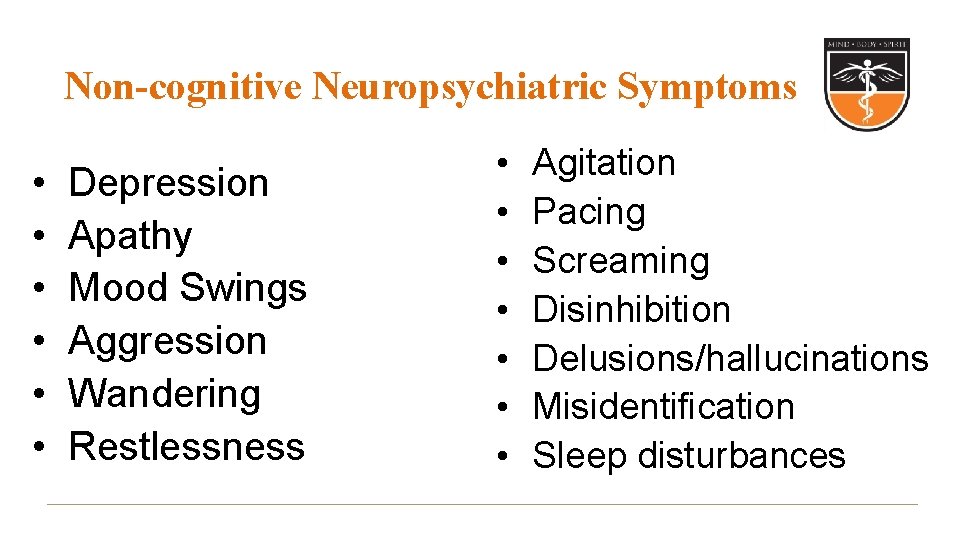
Non-cognitive Neuropsychiatric Symptoms • • • Depression Apathy Mood Swings Aggression Wandering Restlessness • • Agitation Pacing Screaming Disinhibition Delusions/hallucinations Misidentification Sleep disturbances
TREATMENT • Pharmacological: treatment with cholinesterase inhibitors and/or memantine to slow disease progression; symptomatic treatment • Non-pharmacological: stable environment, offer a consistent routine, diet, exercise, reminiscent therapy
Vascular Dementia (VD) • Formerly Multi-infarct Dementia (MID) • Results when a person has sustained cortical or subcortical strokes, which may be too small to cause permanent or residual neurological deficits or evidence of stroke on CT • Accounts for 1/3 of all dementias • Risk factors include: HTN, strokes, TIAs, CAD, HL, smoking, male gender, age >60 years
CV Etiology: • Factors predicting CV etiology for dementia: – aphasia – major dominate stroke – history of CV disease – low education level • Best clue: dementia whose onset coincides with a stroke; step-wise progression • Often co-occurs with AD (mixed dementia)
Symptoms associated with VD • Executive function is commonly impaired and in a greater degree than is seen in AD • Impairment of naming and verbal fluency • Impaired psychomotor speed and measures of attention • Depression
TREATMENT • • • Control HTN Treat CV risk factors Stop smoking Diet/exercise Cholinesterase inhibitors may help
Frontotemporal Dementia (FTD) • Pathology involved in the frontal and anterior temporal areas • Common cause of dementia in those under 65 years old; may account for 20% of dementia cases in those 45 -65 years old • Characterized by early onset and poor executive and language function and relatively spared memory function
Clinical Manifestations • 2 broad patterns of clinical manifestations: – Early behavioral changes: disinhibition, apathy, hyperorality, inappropriate social interaction – changes in expressive language or in naming and comprehension • Spared memory and visuospatial skills
TREATMENT • Pharmacological: the efficacy of cholinesterase inhibitors is perceived to be poorest in FTD. • Non-pharmacological: behavioral management
Dementia with Lewy Bodies (DLB) • Extensive neuritic plaques, similar to AD brains, but fewer neurofibrillary tangles • The Lewy Body, an additional lesion, is found throughout the cortex and substantia nigra
Cognitive Features of DLB: • Fluctuating cognition • • • episodes of confusion excessive sleepiness/daytime drowsiness/lethargy inattention incoherent/disorganized speech varying ability to perform tasks
Cognitive features of DLB: • Recurrent, detailed visual hallucinations • Spontaneous motor features of Parkinsonism (bradykinesia, rigidity, gait disturbance) • Sensitivity to neuroleptics/phenothiazine-based antipsychotics • Poor response to L-dopa replacement for Parkinsonian features
Evaluation of Dementia • Purpose: • Determine deficits (cortical vs. subcortical) • Determine severity of cognitive/functional impairments • Determine presence of motor impairments • Identify any psychiatric or behavioral features
Benefits of early diagnosis: 1. Consequences of functional decline can be better managed (finances, driving, falls) 2. Promote understanding and treat changes in behaviors and personality of the patient 3. Afford time for long-range planning of the inevitable outcomes of dementia 4. Improved response to treatment in earlier stages may delay progression.
Behavior/Mood • • Depression Isolation Irritability Aggression Disinhibition Delusions Hallucinations
Imaging Studies: (MRI/CT) • Identify other conditions to explain/contribute to dementia • 5% of patients revealed clinically unexpected lesions • Quantitative MRI, in the future, may be useful in documenting the rate and degree of cerebral atrophy in MCI and AD
Cognitive Assessment: • • MMSE Mo. CA Mini-Cog GDS
Mini-Mental State Exam (MMSE) • Developed by Folstein (1975) • Most commonly used cognitive function test and dementia screening tool • Takes approximately 10 minutes to administer • Age and education affect performance on the MMSE
MMSE (cont. ) • Not sensitive for detecting MCI or early dementia • Does not discriminate severity of illness in more advanced cases • Useful of following the course of illness and response to therapy
Geriatric Depression Scale (GDS) • 30 item questionnaire to determine mood • Utilizes yes/no answers • Scores of > 10 suggest the presence of a depressive episode
MINI-COG 42 – Composed of 3 item recall and a clock drawing test (CDT) – Can be used to detect dementia quickly and easily in various settings – Assesses registration, executive function, and recall
MINI-COG 43(con’t) • Target Population: – Appropriate for use in all health care settings. – Appropriate for use with older adults at various heterogeneous language, culture, and literacy levels
MINI-COG 44 (con’t) • Strengths and Limitations: – – Takes about 3 minutes to administer Not influenced by culture, language, or education Requires simple, short training to perform accurately Perceived by patients as less stressful than longer mental status tests – Remains accurate across heterogenic groups
Montreal Cognitive Assessment (Mo. CA) • Designed as a rapid screening for mild cognitive impairment. • Assesses: attention, concentration, executive function, memory, language, visuoconstructional skills, conceptual thinking, calculations, and orientation. • Takes 10 minutes to administer. • Total possible score is 30, with a score of 26 or above considered normal.
Recommendations for protecting your patients against dementia: • • • Control hypertension Control hypercholesterolemia ASA 81 mg QD Regular physical exercise Regular cognitive exercises Regular social interaction/involvement
Cholinergic Agents: • Acetylcholinesterase inhibitors (Ach. E-I) o Mainstay of treatment o Slows disease progress o If discontinued, disease progression returns o ONLY drugs shown to slow AD progression
Cholinergic Agents (cont. ) • Currently there are 3 drugs available: » Donepezil (Aricept) » Rivastigmine (Exelon) » Galantamine (Reminyl)
Memantine (Namenda) • First and only NMDA-receptor antagonist. • Used to treat moderate to severe Alzheimer’s disease. • Effective first line treatment as monotherapy or in combination with Ach-I. • Side effects may include dizziness, headache and constipation.
THANK YOU!!