Delirium in ICU Carmen Lopez Soto SCF ICM






- Slides: 20
Delirium in ICU Carmen Lopez Soto, SCF ICM Teaching Sessions

üDefinition üEpidemiology & Risk Factors üAssesment üManagement
Why is #icudelirium a trending topic? Associated with 1. Increased mortality 2. Prolonged ICU and hospital LOS 3. Post-ICU cognitivie impairment
Definition Acute Cerebral dysfunction Fluctuating baseline mental status Key Features Also… 1. 2. 3. 4. Disturbed/Altered level of consciousness Change in condition Development perceptual disturbance Disorganised thinking Sleep disturbances Abnormal psychomotor activity Emotional disturbances
Definition Psychomotor slowing Apathy Decreased responsiveness Psychomotor agitation Hallucinations Emotional lability
Epidemiology - Up to 80% - Mechanical ventilated - 4 -16 billion USD - Usually underdiagnosed
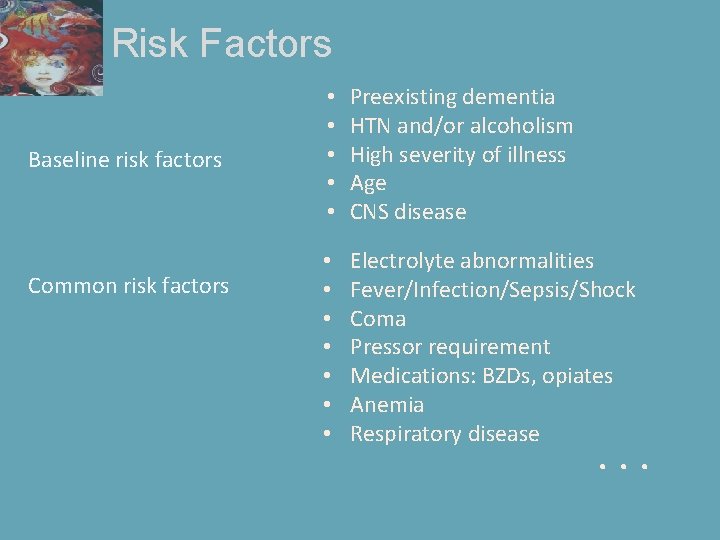
Risk Factors Baseline risk factors Common risk factors • • • Preexisting dementia HTN and/or alcoholism High severity of illness Age CNS disease • • Electrolyte abnormalities Fever/Infection/Sepsis/Shock Coma Pressor requirement Medications: BZDs, opiates Anemia Respiratory disease . . .
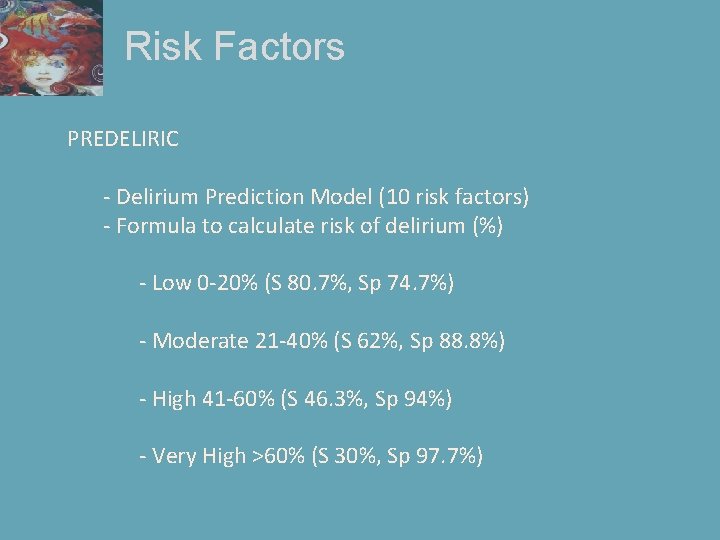
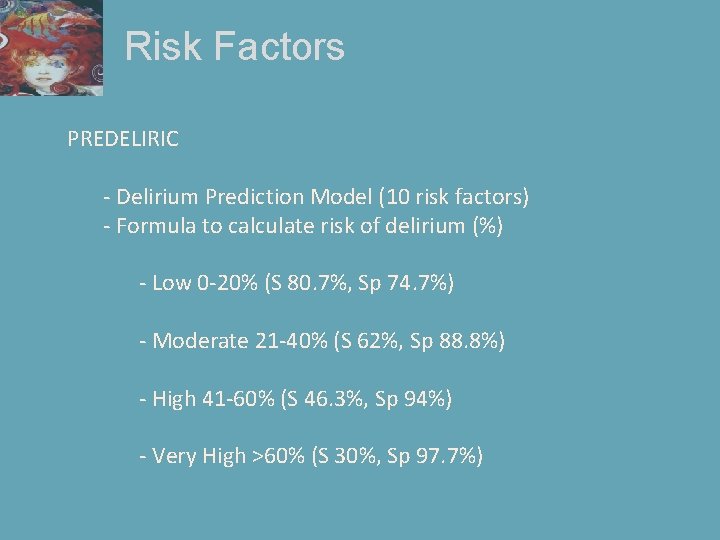
Risk Factors PREDELIRIC - Delirium Prediction Model (10 risk factors) - Formula to calculate risk of delirium (%) - Low 0 -20% (S 80. 7%, Sp 74. 7%) - Moderate 21 -40% (S 62%, Sp 88. 8%) - High 41 -60% (S 46. 3%, Sp 94%) - Very High >60% (S 30%, Sp 97. 7%)
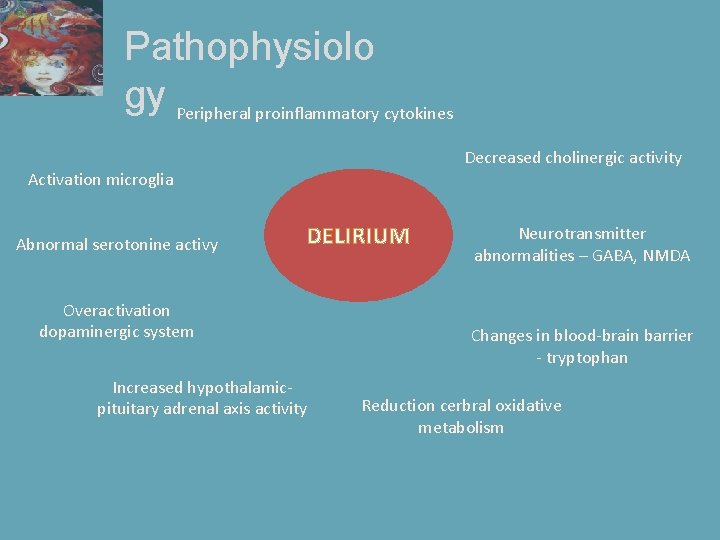
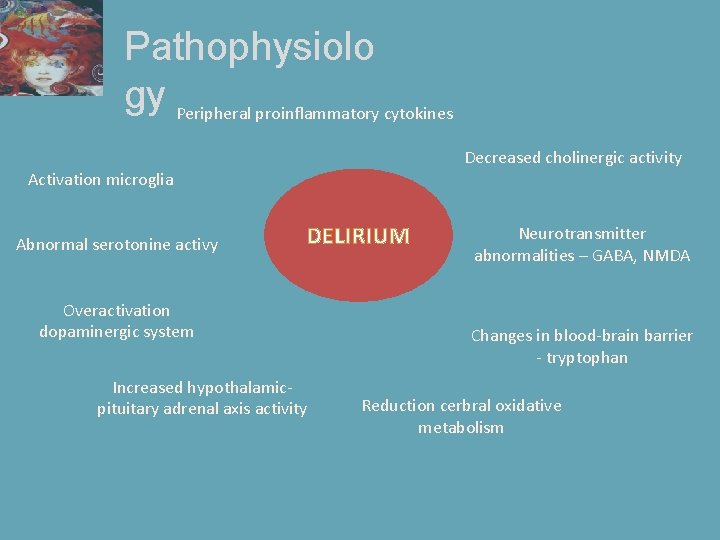
Pathophysiolo gy Peripheral proinflammatory cytokines Decreased cholinergic activity Activation microglia Abnormal serotonine activy DELIRIUM Overactivation dopaminergic system Increased hypothalamicpituitary adrenal axis activity Neurotransmitter abnormalities – GABA, NMDA Changes in blood-brain barrier - tryptophan Reduction cerbral oxidative metabolism
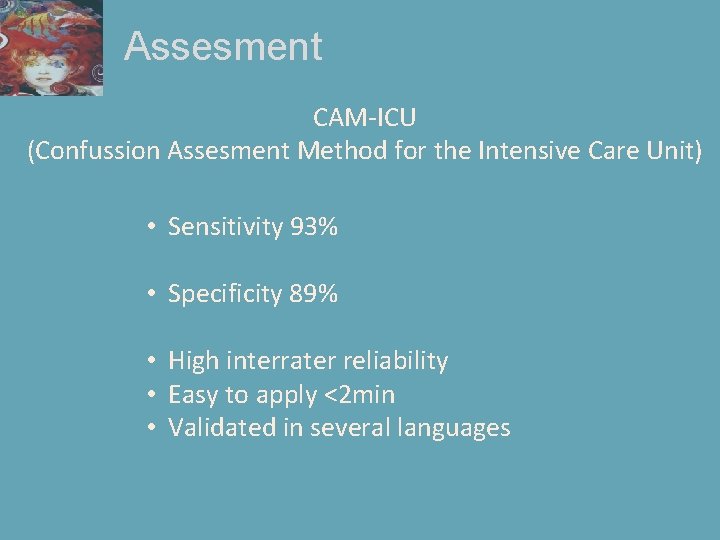
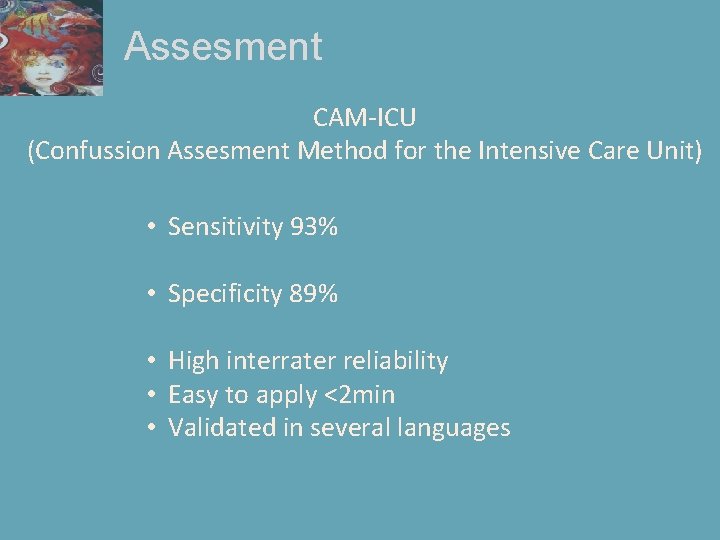
Assesment CAM-ICU (Confussion Assesment Method for the Intensive Care Unit) • Sensitivity 93% • Specificity 89% • High interrater reliability • Easy to apply <2 min • Validated in several languages
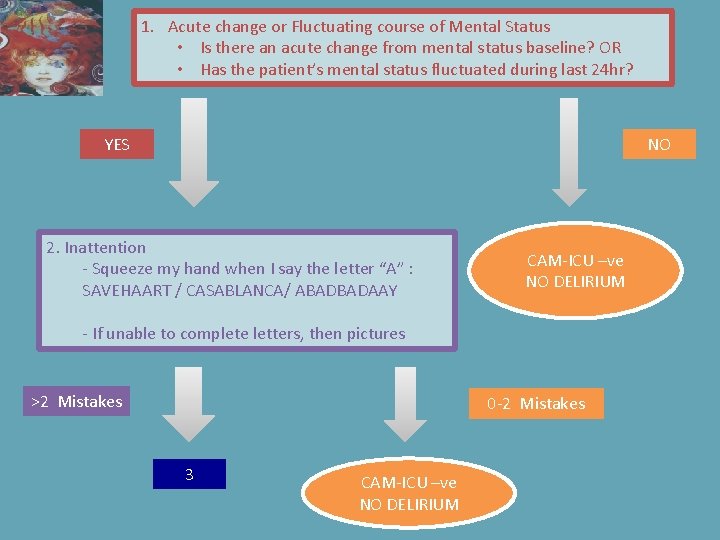
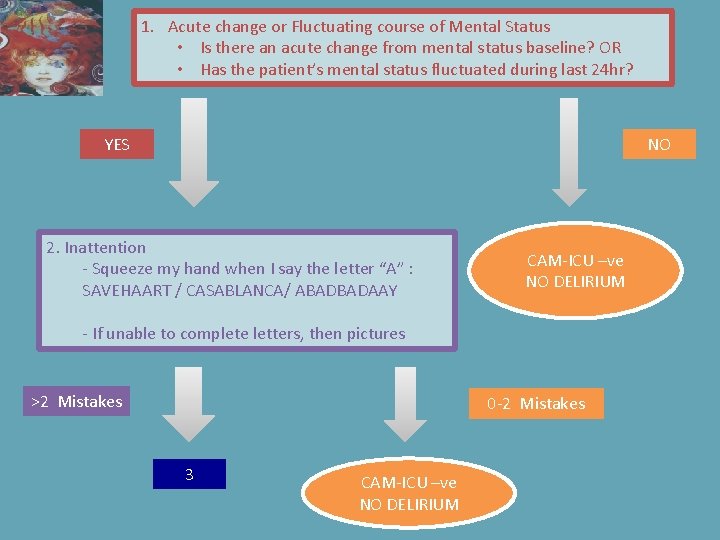
1. Acute change or Fluctuating course of Mental Status • Is there an acute change from mental status baseline? OR • Has the patient’s mental status fluctuated during last 24 hr? YES NO 2. Inattention - Squeeze my hand when I say the letter “A” : SAVEHAART / CASABLANCA/ ABADBADAAY CAM-ICU –ve NO DELIRIUM - If unable to complete letters, then pictures >2 Mistakes 0 -2 Mistakes 3 CAM-ICU –ve NO DELIRIUM
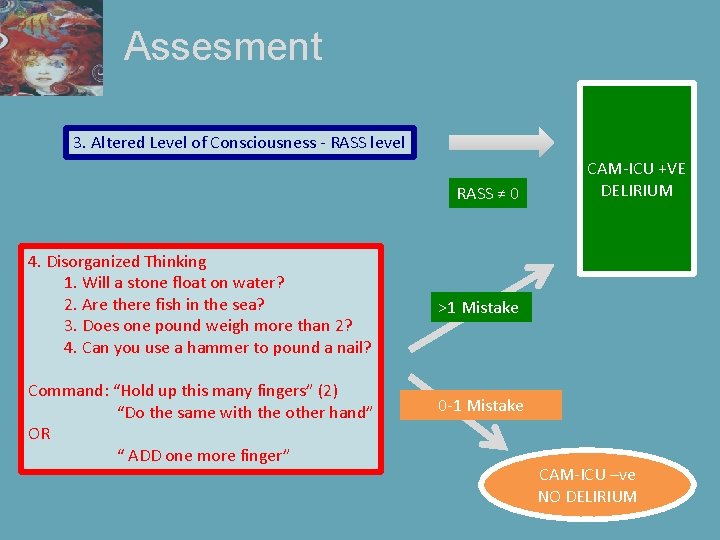
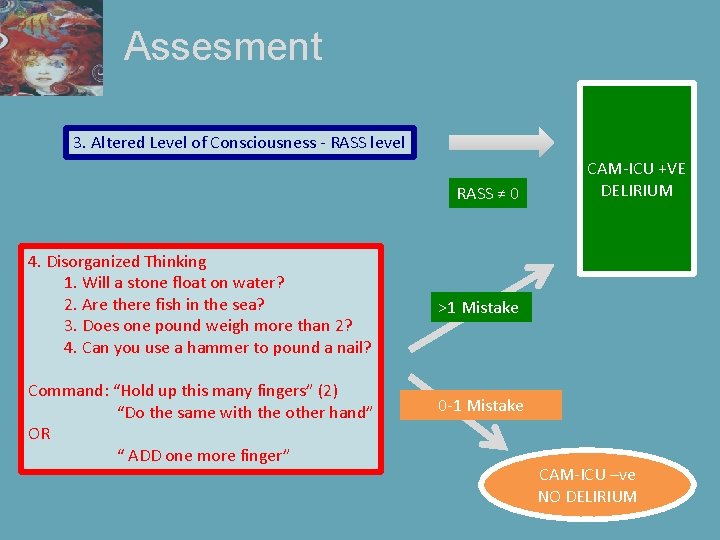
Assesment 3. Altered Level of Consciousness - RASS level RASS ≠ 0 4. Disorganized Thinking 1. Will a stone float on water? 2. Are there fish in the sea? 3. Does one pound weigh more than 2? 4. Can you use a hammer to pound a nail? Command: “Hold up this many fingers” (2) “Do the same with the other hand” OR “ ADD one more finger” CAM-ICU +VE DELIRIUM >1 Mistake 0 -1 Mistake CAM-ICU –ve NO DELIRIUM
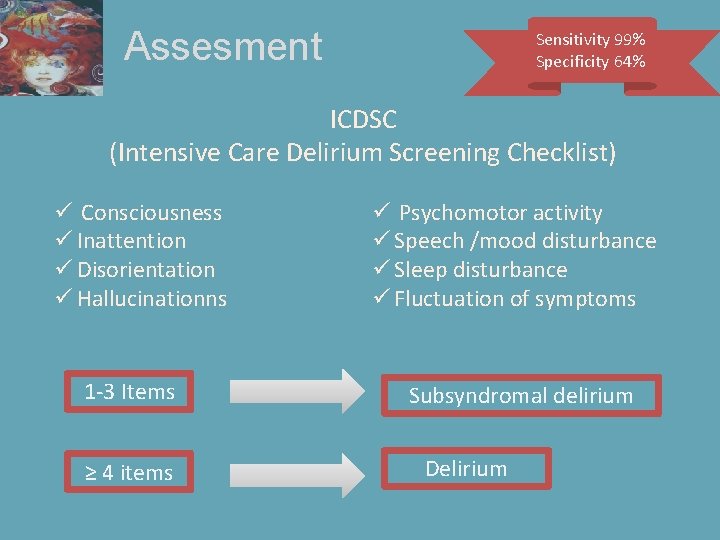
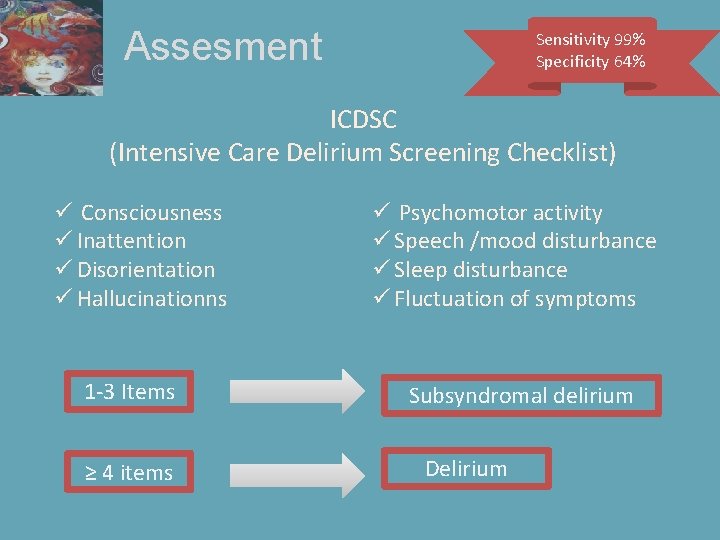
Assesment Sensitivity 99% Specificity 64% ICDSC (Intensive Care Delirium Screening Checklist) ü Consciousness ü Inattention ü Disorientation ü Hallucinationns 1 -3 Items ≥ 4 items ü Psychomotor activity ü Speech /mood disturbance ü Sleep disturbance ü Fluctuation of symptoms Subsyndromal delirium Delirium

Manageme nt Non-Pharmacological (Preventive) • • • Effective communication Reorientation Reassurance Non pharmacological sleep protocol Early mobilization Timely removal of catheters and physical restraints
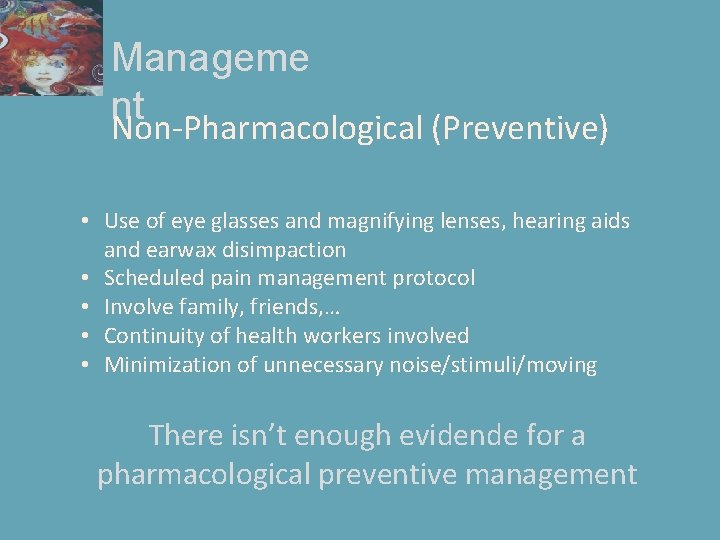
Manageme nt Non-Pharmacological (Preventive) • Use of eye glasses and magnifying lenses, hearing aids and earwax disimpaction • Scheduled pain management protocol • Involve family, friends, … • Continuity of health workers involved • Minimization of unnecessary noise/stimuli/moving There isn’t enough evidende for a pharmacological preventive management

Manageme nt Pharmacological • Forget about BZD!!. . . Unless Alcohol withdrawal • Cholinesterase inhibitos (rivastigmine) § Not recommended ? Harmful

Manageme nt Pharmacological Haloperidol - There isn’t evidence in reduction of duration Atypical antipsychotics (olanzapine, quetiapine) - May reduce duration of delirium Should not be used in patients with prolonged QT… Monitor ECG!!

Manageme nt Pharmacological α 2 -adrenergic agonists Clonidine - Decreases pain + sedation requirements - Facilitates weaning from ventilation - Bioavailability 100% orally Dexmethomedimine - Analgesia + “cooperative sedation” - Reduced duration of delirium in ventilated patients
References • Long Term Cognitive Disfunction after Critical Illness, Pandharipande PP, et al. N Engl J Med. Oct 2013 3; 369(14): 1306 -16. • NICE Guideline: Delirium. NICE quality standards (QS 63) • Icudelirium. org • Clinical Practice Guidelines on for the management of Pain, Agitation and Delirium in Adult Patients in the Critical Care Unit. Barr J. , et al. Crit Care Med. 2013 Jan; 41(1): 263 -306. • Ely E, Inouye SK, Bernard GR, et al. Delirium in Mechanically Ventilated Patients: Validity and Reliability of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). JAMA. 2001; 286(21): 2703 -2710 • Bergeron N, Dubois M-J, Dumong M, et al. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001; 27(5): 859 -64 • M van Boogaard et al. Development and validation of PRE-DELIRIC delirium prediciton model for intensive care patients: observational multicentre study. BM. 2012; 344: e 420

Thank you!!
 Doña carmen sanchez de lopez
Doña carmen sanchez de lopez Scf instructure
Scf instructure Societe generale investor relations
Societe generale investor relations Scf ttm
Scf ttm Amnesia
Amnesia Delirium definition
Delirium definition Difference between dementia and delirium
Difference between dementia and delirium Flocculation delirium
Flocculation delirium Cam icu escala
Cam icu escala Driver diagram palliative care
Driver diagram palliative care Excited delirium перевод
Excited delirium перевод Sindrom delirium akut
Sindrom delirium akut Francisco fernandez md
Francisco fernandez md Delirium care pathways
Delirium care pathways Escala de cam
Escala de cam Nash delirium
Nash delirium Kesadaran gcs
Kesadaran gcs Acute confusion related to
Acute confusion related to Pinch me delirium
Pinch me delirium Delirium case presentation
Delirium case presentation Terminalt delirium
Terminalt delirium