DELIRIUM ELDERLY ATRISK INSTRUMENT Nora Mc Pherson APRN





- Slides: 23
DELIRIUM ELDERLY AT-RISK INSTRUMENT Nora Mc. Pherson, APRN, CNS, Geriatrics Jill Tusing MS, RN, BC Service Line: Behavioral Health

SBAR: DELIRIUM IDENTIFYING HIGH RISK PATIENTS Situation: Delirium (acute confusion) a common, under recognized, postoperative complication in elective orthopaedic patients (10%-40%); manifests as acute impairment in cognition and attention. Background: Post-operative delirium is associated with poor outcomes, greater costs, longer lengths of stays, poor recovery, institutionalization, and mortality.
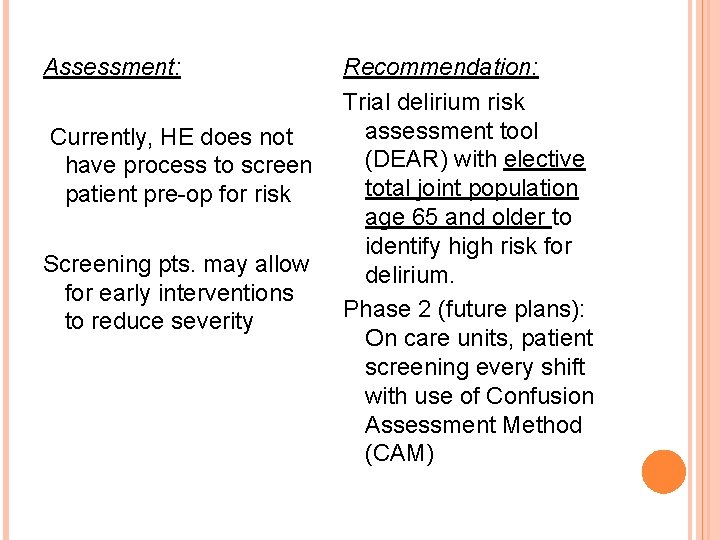
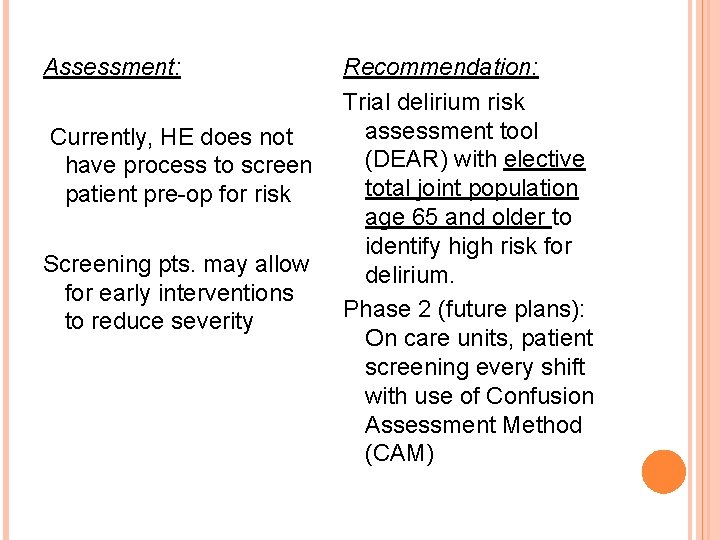
Assessment: Currently, HE does not have process to screen patient pre-op for risk Screening pts. may allow for early interventions to reduce severity Recommendation: Trial delirium risk assessment tool (DEAR) with elective total joint population age 65 and older to identify high risk for delirium. Phase 2 (future plans): On care units, patient screening every shift with use of Confusion Assessment Method (CAM)
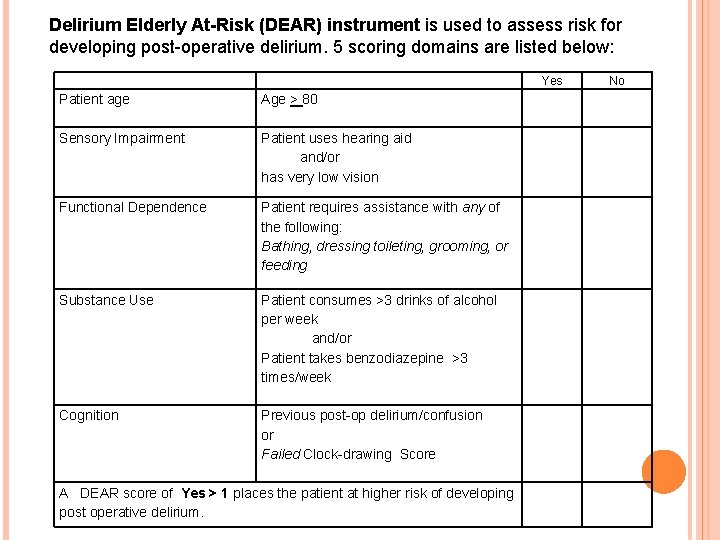
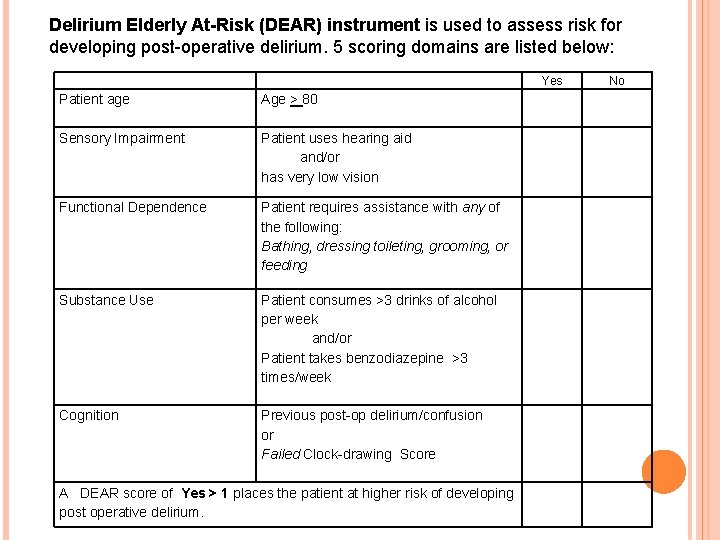
Delirium Elderly At-Risk (DEAR) instrument is used to assess risk for developing post-operative delirium. 5 scoring domains are listed below: Yes Patient age Age > 80 Sensory Impairment Patient uses hearing aid and/or has very low vision Functional Dependence Patient requires assistance with any of the following: Bathing, dressing toileting, grooming, or feeding Substance Use Patient consumes >3 drinks of alcohol per week and/or Patient takes benzodiazepine >3 times/week Cognition Previous post-op delirium/confusion or Failed Clock-drawing Score A DEAR score of Yes > 1 places the patient at higher risk of developing post operative delirium. No
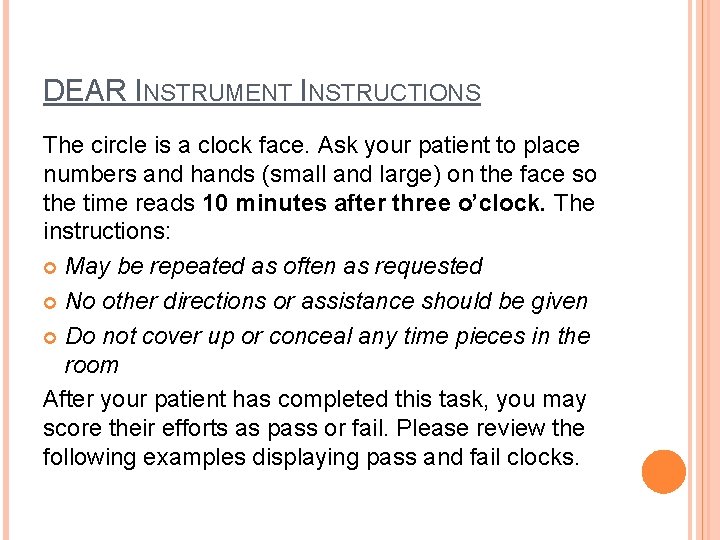
DEAR INSTRUMENT INSTRUCTIONS The circle is a clock face. Ask your patient to place numbers and hands (small and large) on the face so the time reads 10 minutes after three o’clock. The instructions: May be repeated as often as requested No other directions or assistance should be given Do not cover up or conceal any time pieces in the room After your patient has completed this task, you may score their efforts as pass or fail. Please review the following examples displaying pass and fail clocks.
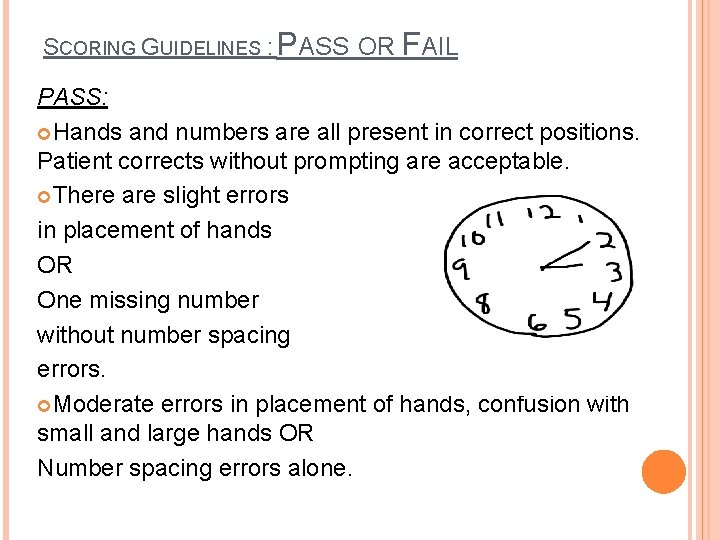
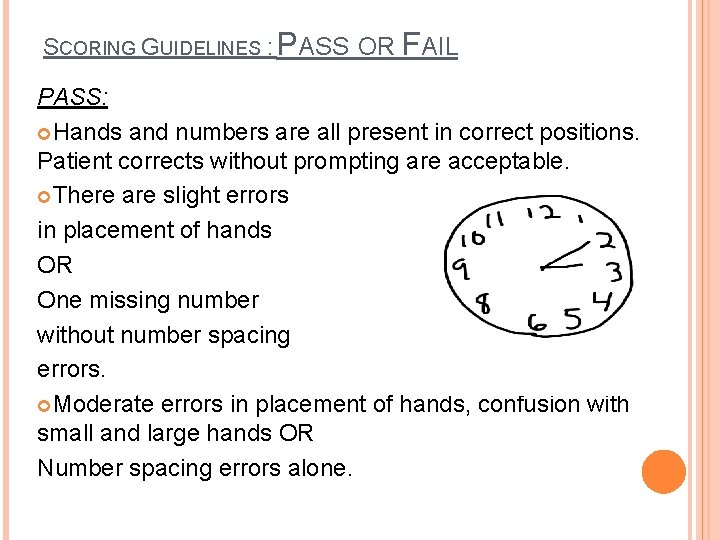
SCORING GUIDELINES : PASS OR FAIL PASS: Hands and numbers are all present in correct positions. Patient corrects without prompting are acceptable. There are slight errors in placement of hands OR One missing number without number spacing errors. Moderate errors in placement of hands, confusion with small and large hands OR Number spacing errors alone.

Scoring Passed Guidelines: Placement of hands is significantly off course OR Number spacing is inappropriate. Example: Even though there is bunching, distortion not grossly inappropriate. Typically seen in those who are cued to spatial mistakes once they get to the 6 (because they know it is supposed to be at the bottom), and make correction only to commit same error in subsequent numbers.
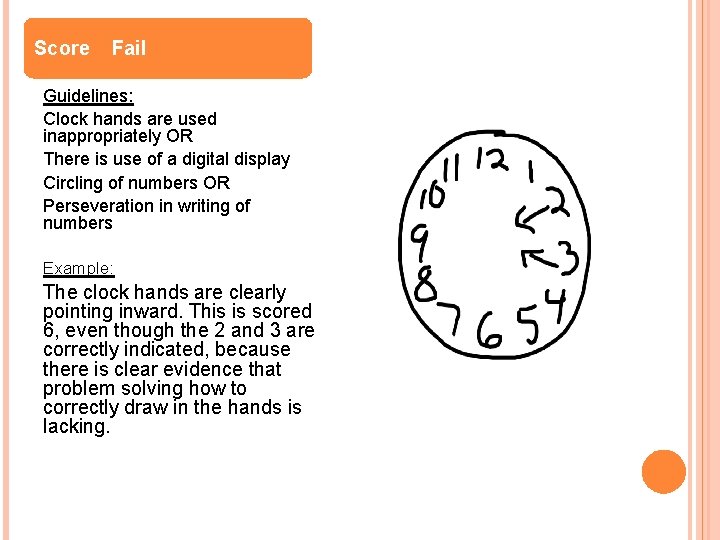
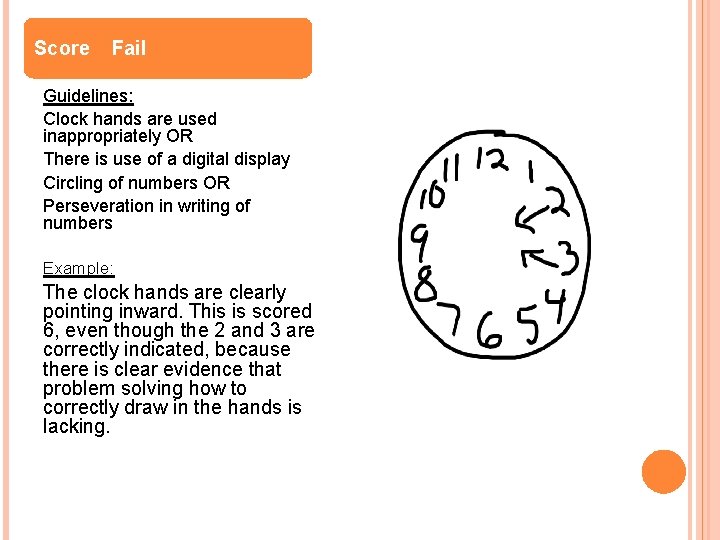
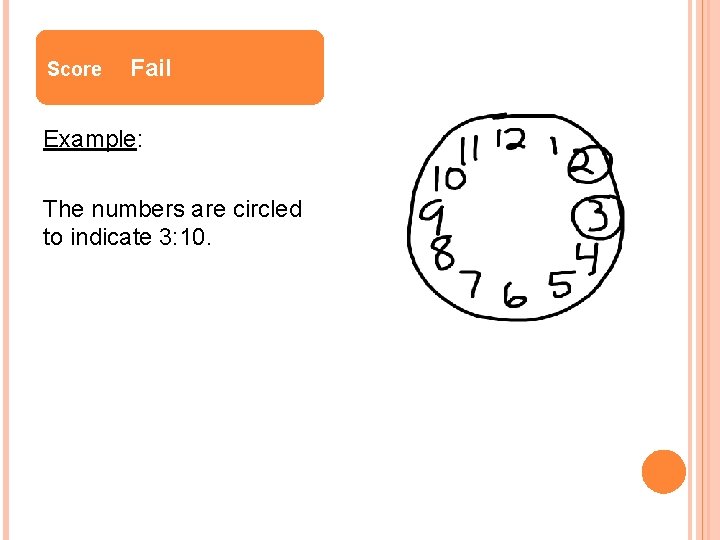
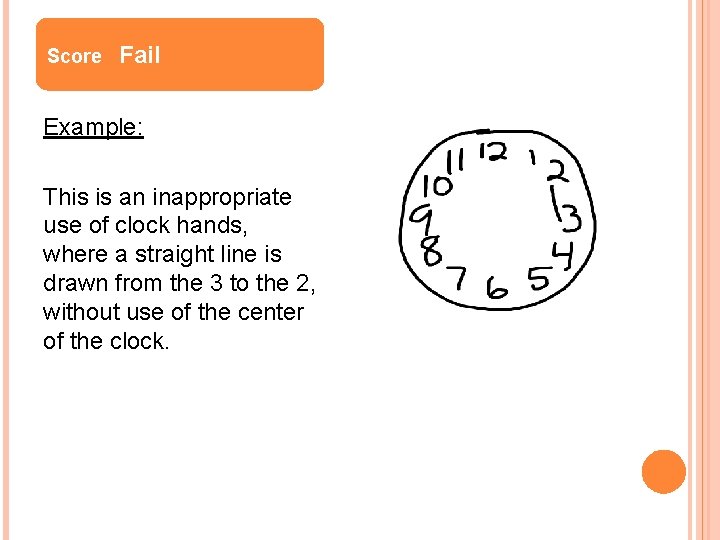
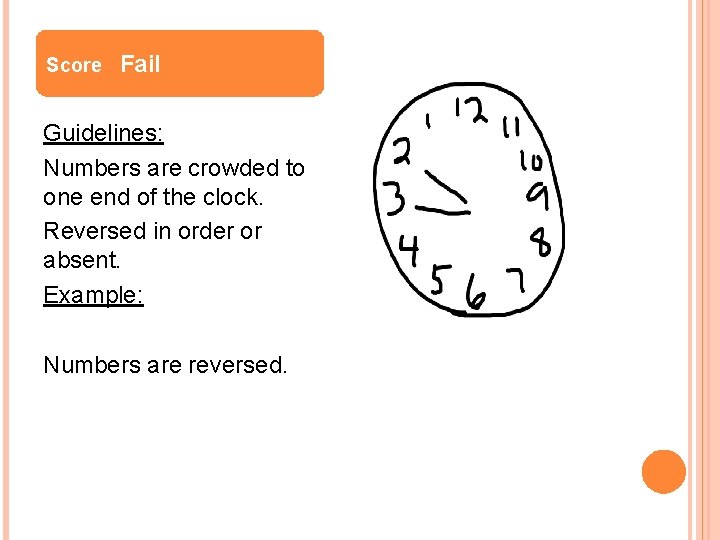
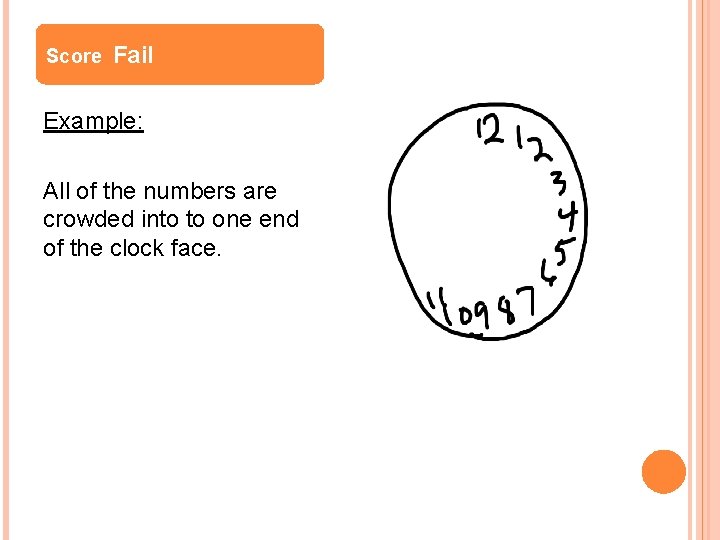
Score Fail Guidelines: Clock hands are used inappropriately OR There is use of a digital display Circling of numbers OR Perseveration in writing of numbers Example: The clock hands are clearly pointing inward. This is scored 6, even though the 2 and 3 are correctly indicated, because there is clear evidence that problem solving how to correctly draw in the hands is lacking.
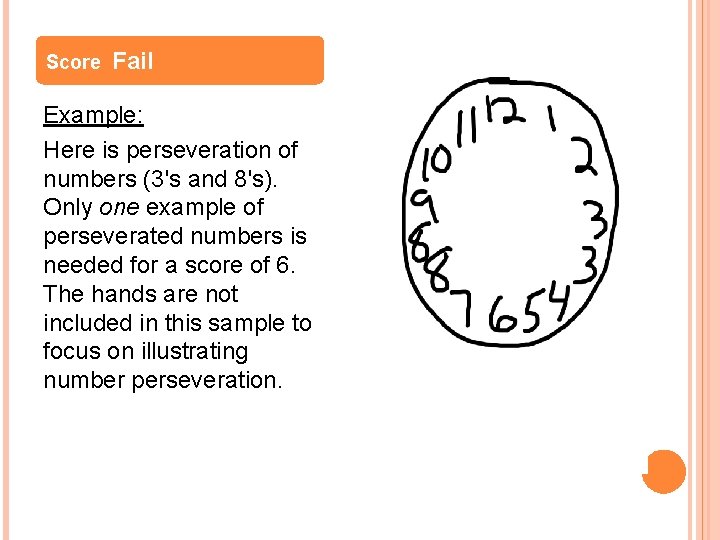
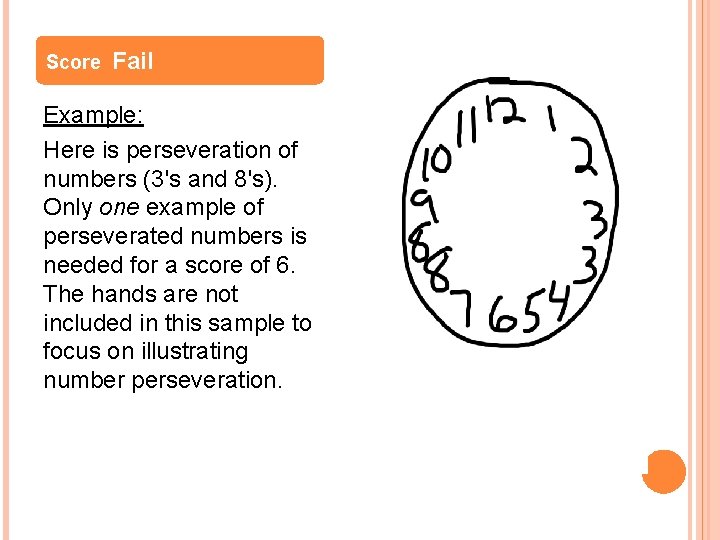
Score Fail Example: Here is perseveration of numbers (3's and 8's). Only one example of perseverated numbers is needed for a score of 6. The hands are not included in this sample to focus on illustrating number perseveration.
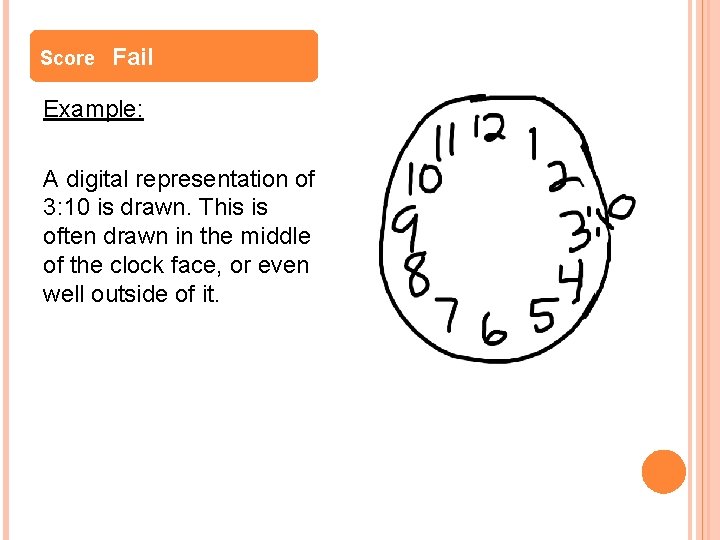
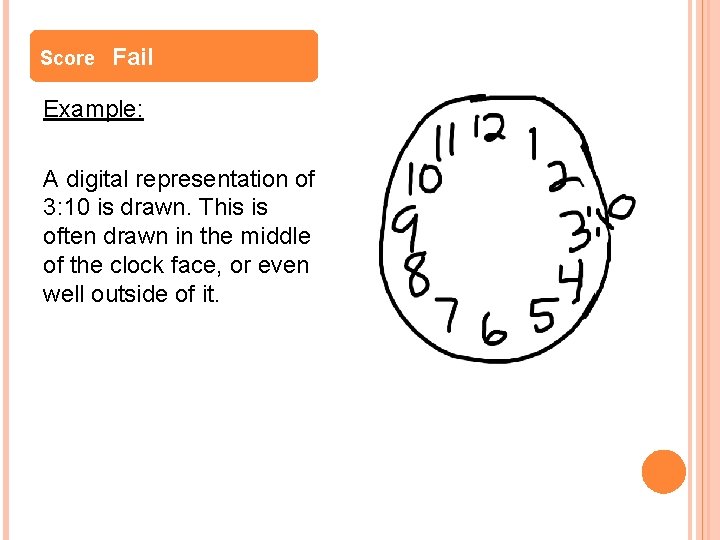
Score Fail Example: A digital representation of 3: 10 is drawn. This is often drawn in the middle of the clock face, or even well outside of it.
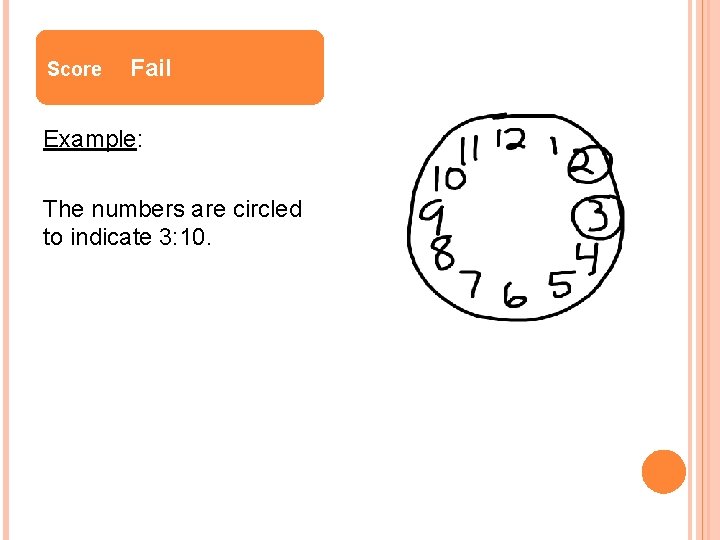
Score Fail Example: The numbers are circled to indicate 3: 10.
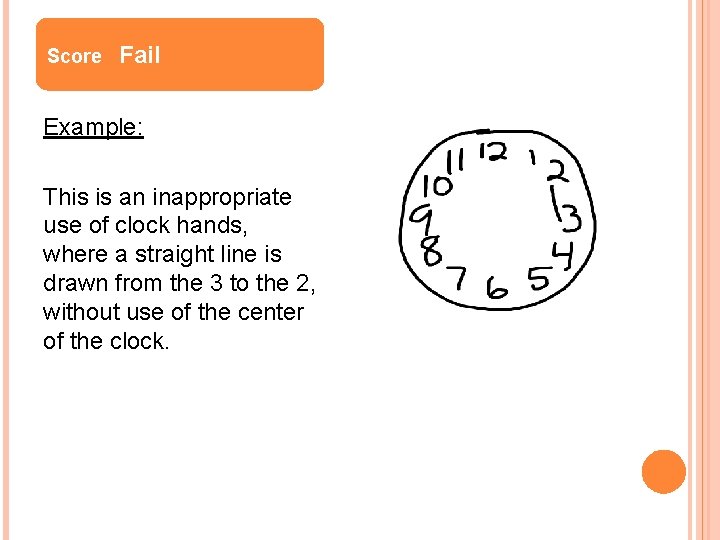
Score Fail Example: This is an inappropriate use of clock hands, where a straight line is drawn from the 3 to the 2, without use of the center of the clock.
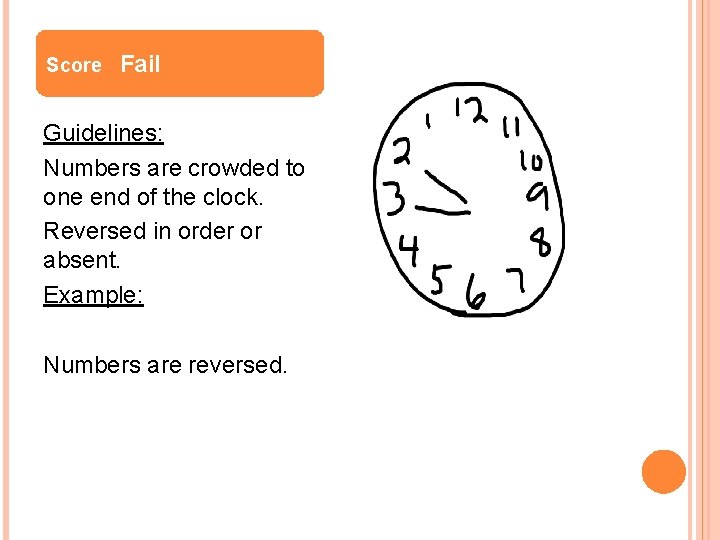
Score Fail Guidelines: Numbers are crowded to one end of the clock. Reversed in order or absent. Example: Numbers are reversed.
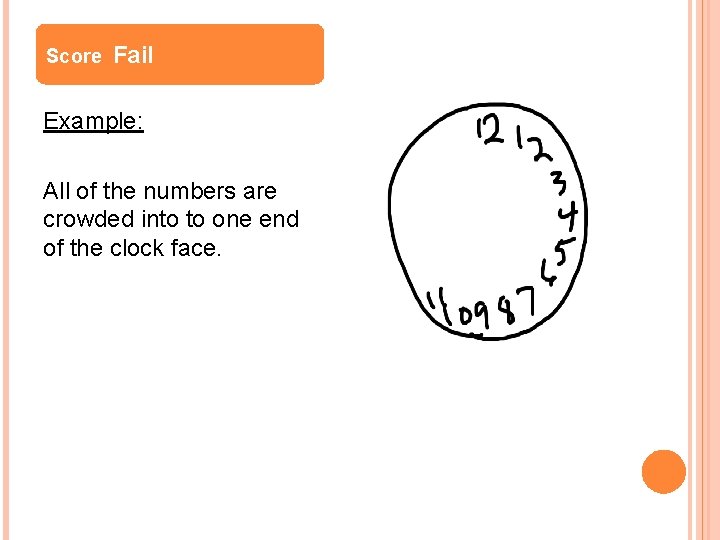
Score Fail Example: All of the numbers are crowded into to one end of the clock face.
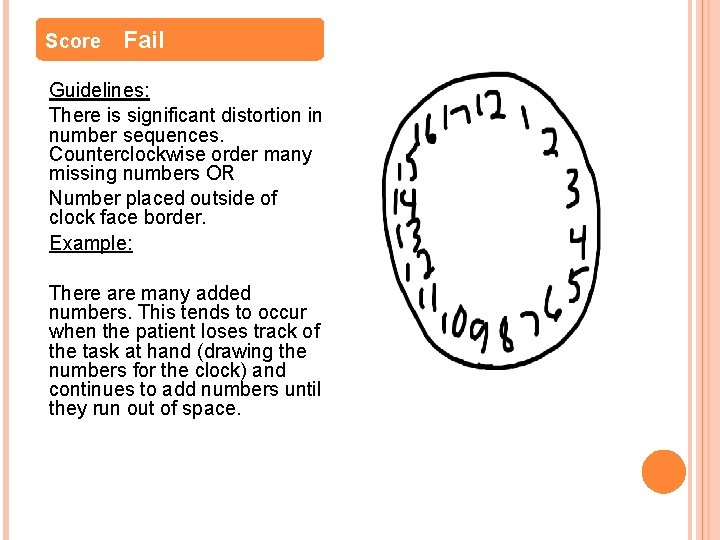
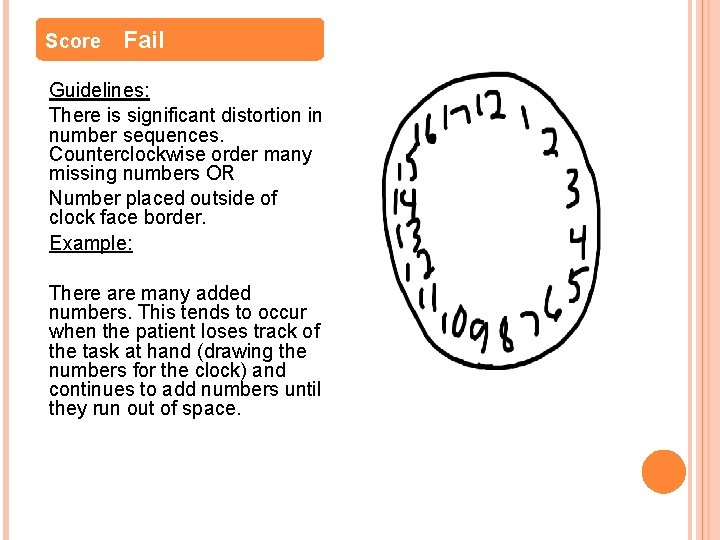
Score Fail Guidelines: There is significant distortion in number sequences. Counterclockwise order many missing numbers OR Number placed outside of clock face border. Example: There are many added numbers. This tends to occur when the patient loses track of the task at hand (drawing the numbers for the clock) and continues to add numbers until they run out of space.

Score Fail Example: Some numbers fall outside of the border
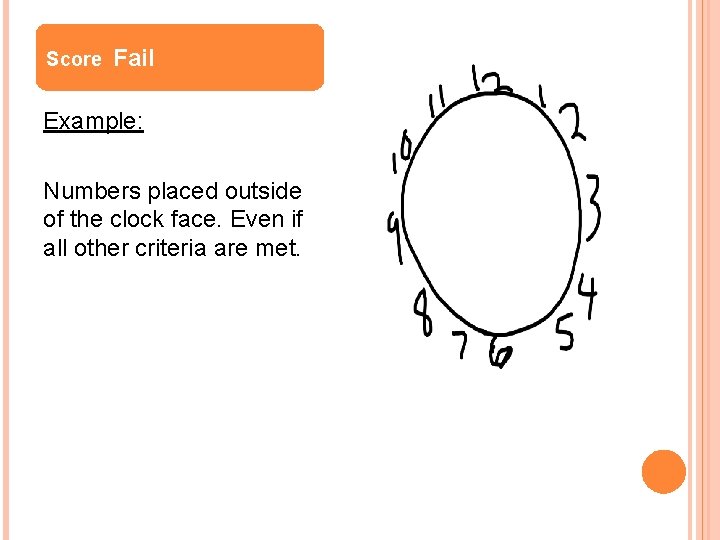
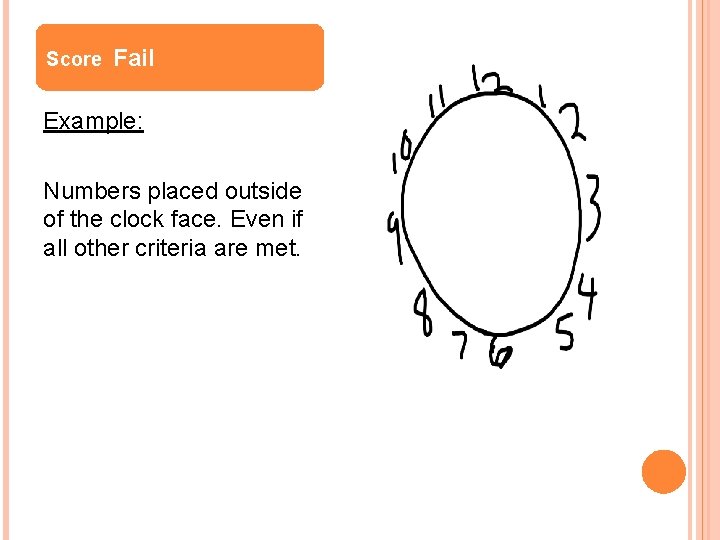
Score Fail Example: Numbers placed outside of the clock face. Even if all other criteria are met.
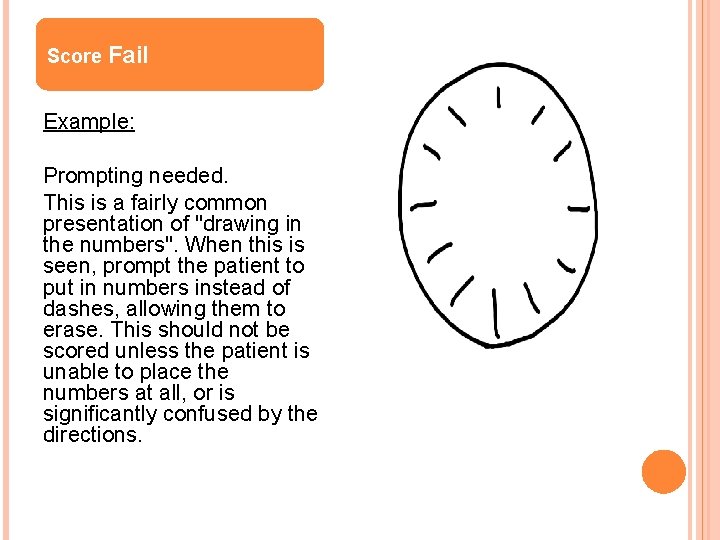
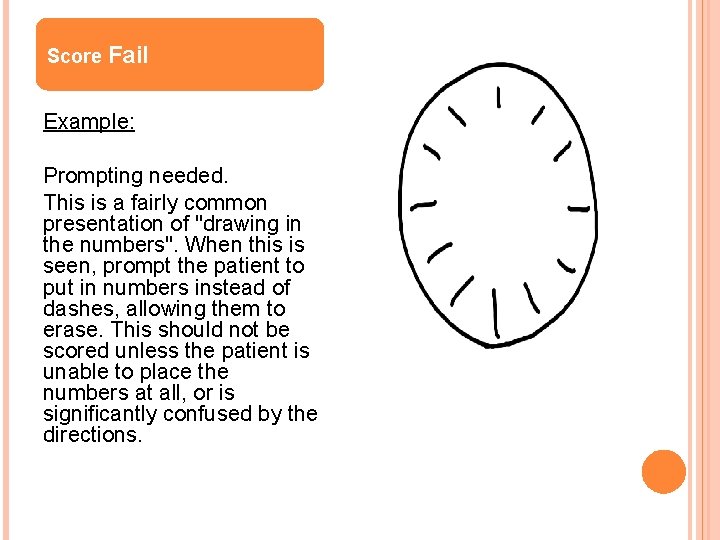
Score Fail Example: Prompting needed. This is a fairly common presentation of "drawing in the numbers". When this is seen, prompt the patient to put in numbers instead of dashes, allowing them to erase. This should not be scored unless the patient is unable to place the numbers at all, or is significantly confused by the directions.
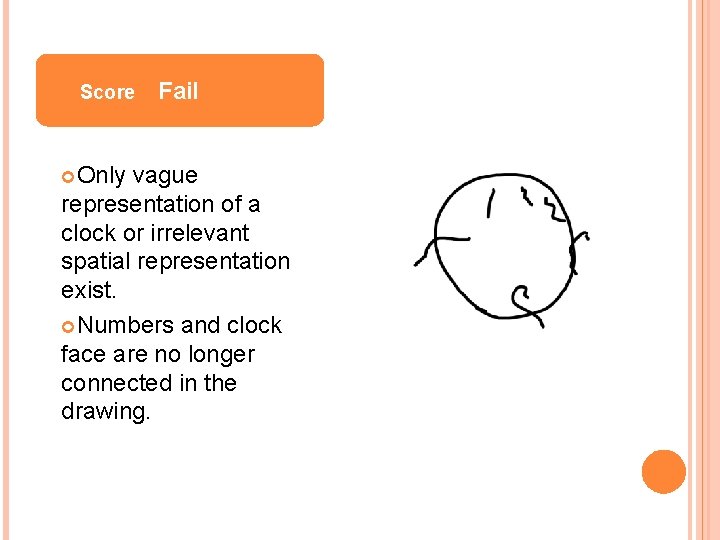
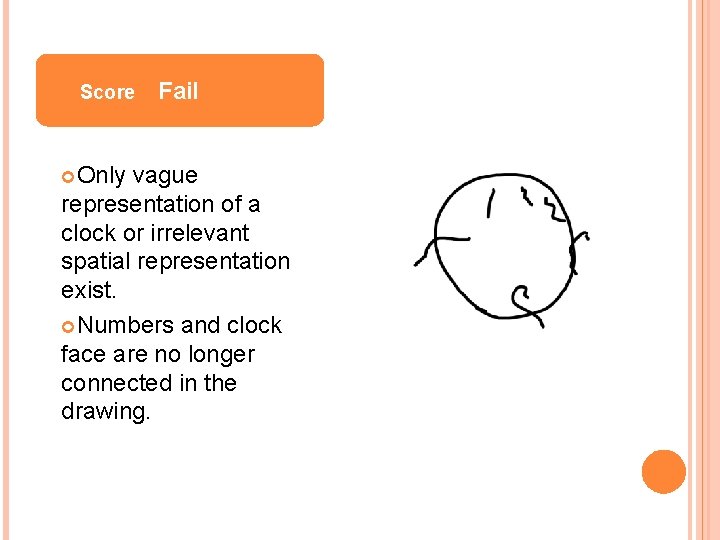
Score Only Fail vague representation of a clock or irrelevant spatial representation exist. Numbers and clock face are no longer connected in the drawing.
Score Fail Result cannot be interpreted OR No attempt is made to draw a clock

DEAR scores >1 indicate patient is at higher risk for developing delirium. : Yes No Patient age Age > 80 X Sensory Impairment Patient uses hearing aid and/or has very low vision X Functional Dependence Patient requires assistance with any of the following: Bathing, dressing toileting, grooming, or feeding X Substance Use Patient consumes >3 drinks of alcohol per week and/or Patient takes benzodiazepine >3 times/week X Cognition Previous post-op delirium/confusion or Failed Clock-drawing Score X A DEAR score of Yes > 1 places the patient at higher risk of developing post operative delirium. 2

Scoring DEAR Tool Add up all of the yes scores on the left side of the tool and place score on bottom. Scores of over 1 are considered high risk. If a patient is scored to be at high risk for delirium, communicate this risk with the medical team. Place High risk for delirium sticker on patient Care Plan (or write it yourself).
REFERENCES Feter, S. , Dunbar, M. , Mac. Leod, H. , Morrison, M. , Mac. Knight, C. , et al. (2005) Predicting postoperative delirium in elective orthopaedic patients: the Delirium Elderly At-Risk (DEAR) instrument. Age and Ageing, 34(2), 169 -184. Health. East A 3 team: Joe Clubb, Director Behavior Health, Dr. David Frenz; Dr. Alvin Holm, Jill Tusing RN Education, Nora Mc. Pherson, APRN, CNS.
 Office of intelligence and analysis
Office of intelligence and analysis Scott mc pherson
Scott mc pherson Sc aprn license
Sc aprn license Wisconsin aprn modernization act
Wisconsin aprn modernization act Georgia composite medical board aprn
Georgia composite medical board aprn Lace consensus model
Lace consensus model Ky aprn license
Ky aprn license 201 kar 20:057
201 kar 20:057 What is an aprn
What is an aprn Driver diagram palliative care
Driver diagram palliative care Energy transfer theory
Energy transfer theory Difference between dementia and delirium
Difference between dementia and delirium Difference between delirium and dementia ppt
Difference between delirium and dementia ppt Delirium care pathways
Delirium care pathways Escala cam icu
Escala cam icu Delirium refractario
Delirium refractario Dr rose dinda martini
Dr rose dinda martini Gcs normal
Gcs normal Acute confusion related to
Acute confusion related to Delirium case presentation
Delirium case presentation Nash delirium
Nash delirium Types of amnesia
Types of amnesia Delirium definition
Delirium definition Lucie big delirium
Lucie big delirium