Delirium Clinical scenario A 36 year old gentleman
- Slides: 21
Delirium
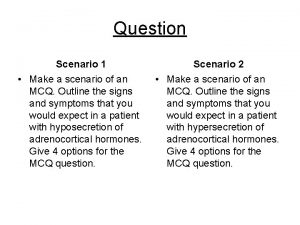
Clinical scenario • A 36 year old gentleman was admitted following a road traffic accident, underwent surgery for fracture of femur shaft. • On the second day after the accident, in hospital, post operatively is referred for being agitated, restless, seeing large insects crawling on the wall • On examination tremulous, diaphoretic with tachycardia • Not oriented to time, place or person; incoherent speech
What is this patient displaying? • Delirium • Psychosis • Dementia • Depression with psychotic features
What is this patient displaying? • Delirium • Psychosis • Dementia • Depression with psychotic features
Delirium – clinical features • Disturbance in attention or cognition • Acute onset • Change from baseline • Fluctuating severity
Delirium - clinical features • Encephalopathy, acute brain failure, acute confusional state, and postoperative or ICU psychosis • Organic psychosis • Variegated manifestations however has a relatively acute decline in cognition, fluctuating over hours to days • Deficit of attention • memory, executive function, visuospatial tasks, and language • sleep-wake cycle, perception, affect changes and autonomic findings
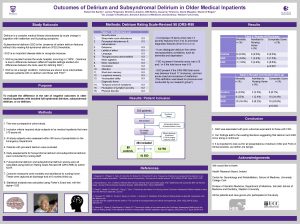
Epidemiology • Hospitalised patients – 10 to 50% • More in elder and with hip surgery • Underdiagnosed • Higher rates in ICU and difficult to diagnose • Outside acute settings rates are lower • Significant morbidity and mortality
Risk factors • Age • Underlying cognitive dysfunction • Other predisposing factors – sensory deprivation, poor overall health, including baseline immobility, malnutrition, and underlying medical or neurologic illness, in hospital risks • Precipitating factors – infections, systemic illnesses, anesthetic agents, uncontrolled pain
Risk factors • 85 year old gentleman, living with grandson • History of being forgetful for over 2 years, progressive although fluctuating, increased food intake • Forgetting meals and conversations • At times not identifying people • Hard of hearing and vision impaired for past 3 -4 years; Malunited Colles, immature cataract, pallor
Pathogenesis • Cholinergic deficiency • Dopamine • “Stress” can unmask a deficient state
Approach • History, examination and MSE • Bedside clinical • Scales – physicians, nurses • CAM • All acutely confused patients should be presumed to be delirious • Sundowning may be present
Diagnosis • Essentially clinical diagnosis, bedside • Spectrum of manifestations, can fluctuate • Hypoactive (depressants like benzodiazepines) to hyperactive (DT) • Potentially reversible in most cases, contingent upon identification of the underlying cause • Most cases remit after a variable time, generally days to weeks • Persistence and chronicity implying etiology being addressed inadequately • Long term sequelae unknown, may cause neuronal damage and cognitive decline
History • Information - ? self, informant version • Baseline cognition, course of illness, medication or drug use • Any baseline cognitive impairment must be sought • Temporal evolution • Anticholinergic, sedative, alcohol, OTC, herbal • Toxin exposure
Physical exam • Signs of infection • Status of hydration • Jaundice, cyanosis, needle tracks • May miss the picture in morning rounds • Altered consciousness • If preserved, then assess attention • Toxins, infections, electrolytes, metabolic and endocrine conditions, seizures, cerebrovascular, autoimmune
Investigations • If history and exam unable to identify etiology then staggering investigations
Initial Evaluation • History with special attention to medications (including over-thecounter and herbals) • General physical examination and neurologic examination Complete blood count • Electrolyte panel including calcium, magnesium, phosphorus • Liver function tests, including albumin • Renal function tests
Further Evaluation Guided by Initial Evaluation • Systemic infection screen - Urinalysis and culture, Chest radiograph, Blood cultures • Electrocardiogram • Arterial blood gas • Serum and/or urine toxicology screen (perform earlier in young persons) • Brain imaging with MRI with diffusion and gadolinium (preferred) or CT; EEG • Suspected CNS infection or other inflammatory disorder: lumbar puncture after brain imaging
Second-tier Further Evaluation • Vitamin levels: B 12, folate, thiamine • Endocrinologic laboratories: thyroid-stimulating hormone (TSH) and free T 4; cortisol, Serum ammonia; Sedimentation rate • Autoimmune serologies: antinuclear antibodies (ANA), complement levels; p-ANCA, consider paraneoplastic/autoimmune encephalitis serologies • Infectious serologies: rapid plasmin reagin (RPR); fungal and viral serologies if high suspicion; HIV antibody • Lumbar puncture (if not already performed) Brain MRI with and without gadolinium (if not already performed)
Treatment • Underlying cause to be addressed • Supportive care – reorient with visible clocks, calendars and outsidefacing windows • Avoid any sensory deprivation • Sleep wake cycle, especially in ICU • Nutrition, volume status, pain • Home bedding, clothing and nightstand objects • Safety – self and others, alarms, restraints in exceptional cases
Prevent • Identify high-risk patients • Manage sleep, pain • Manage any infection • Correct any sensory deficit • Reorient pre-emptively in ICU
Thank you
 R
R Nash delirium
Nash delirium Difference between delirium and dementia table
Difference between delirium and dementia table Gcs 456
Gcs 456 Acute confusion related to
Acute confusion related to Pinch me delirium
Pinch me delirium Delirium case presentation
Delirium case presentation Terminalt delirium
Terminalt delirium European delirium association
European delirium association Delirium definition
Delirium definition Difference between dementia and delirium
Difference between dementia and delirium Flocculation delirium
Flocculation delirium Cam icu escala
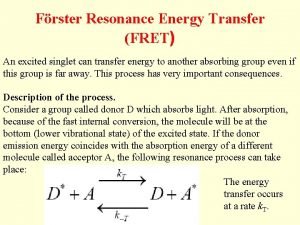
Cam icu escala Frster
Frster Sindrom delirium akut
Sindrom delirium akut Difference between delirium and dementia ppt
Difference between delirium and dementia ppt Delirium care pathways
Delirium care pathways Yr 6 leavers poem
Yr 6 leavers poem Lisa attempts to retrieve her bottle
Lisa attempts to retrieve her bottle Brigance scoring chart 3 year-old
Brigance scoring chart 3 year-old Average height of a 3 year old in centimeters
Average height of a 3 year old in centimeters 27-year old
27-year old