Delirium a brief guide for nurses Alicia Massarotto
Delirium – a brief guide for nurses Alicia Massarotto Geriatric Advanced Trainee 2008

What this talk will cover • • Definition Risk factors Causes How to identify How to treat How to manage Some pictures of Cirque du Soleil
What is Delirium? • Rapid onset of impairment and fluctuation in CONCENTRATION • Altered CONSCIOUSNESS • Impaired COGNITION
How many people get it? • 10 -24% of older adults at time of admission to hospital • 56% of older adults have an episode of delirium during hospital admission
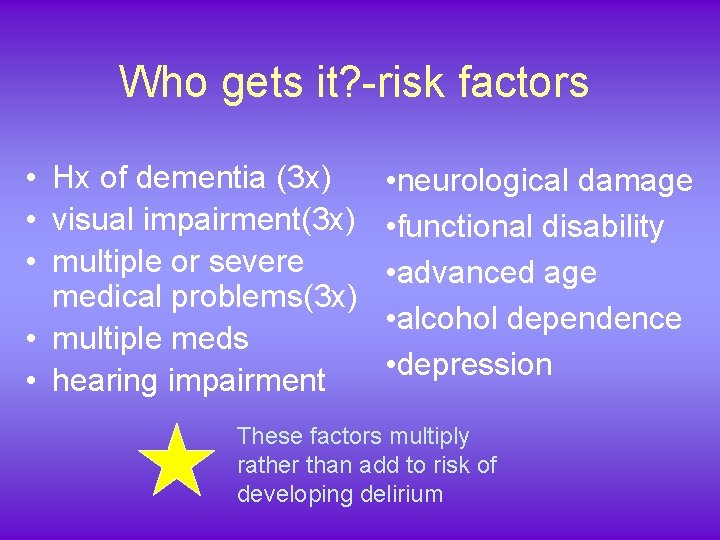
Who gets it? -risk factors • Hx of dementia (3 x) • visual impairment(3 x) • multiple or severe medical problems(3 x) • multiple meds • hearing impairment • neurological damage • functional disability • advanced age • alcohol dependence • depression These factors multiply rather than add to risk of developing delirium
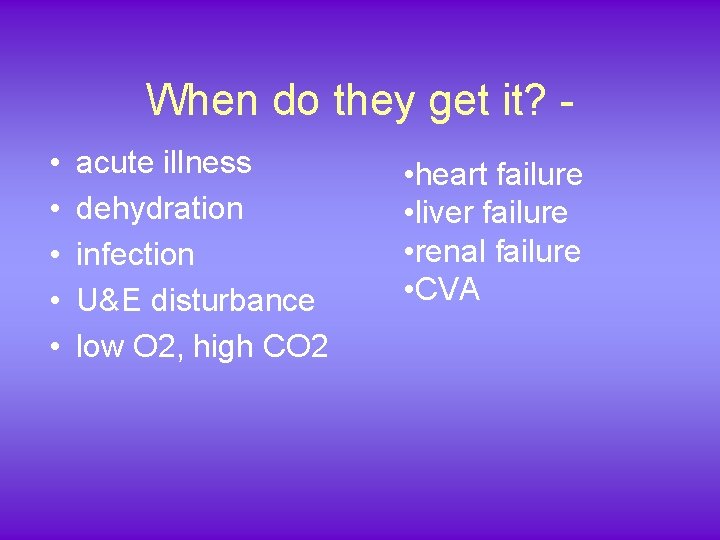
When do they get it? • • • acute illness dehydration infection U&E disturbance low O 2, high CO 2 • heart failure • liver failure • renal failure • CVA
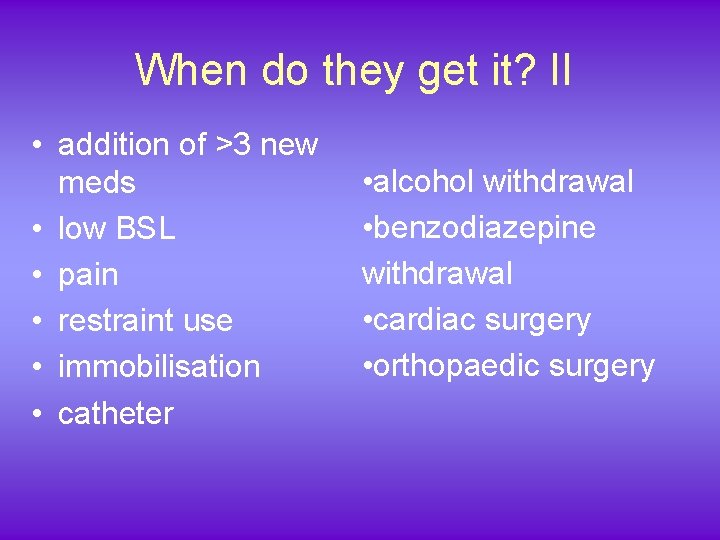
When do they get it? II • addition of >3 new meds • low BSL • pain • restraint use • immobilisation • catheter • alcohol withdrawal • benzodiazepine withdrawal • cardiac surgery • orthopaedic surgery
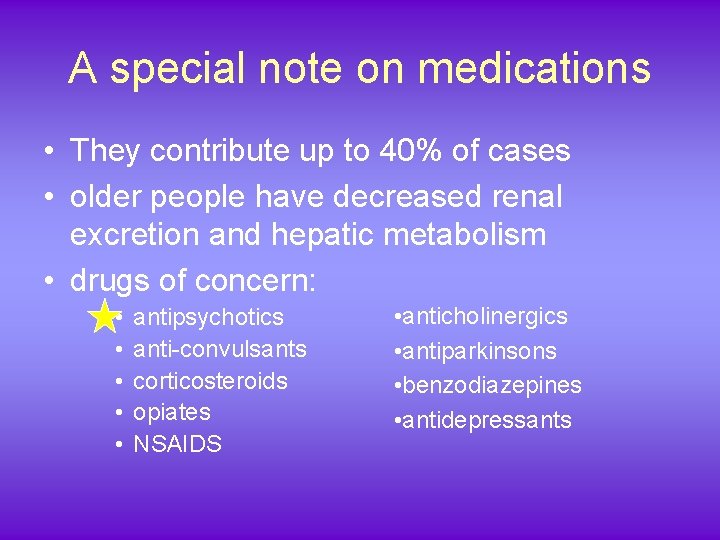
A special note on medications • They contribute up to 40% of cases • older people have decreased renal excretion and hepatic metabolism • drugs of concern: • • • antipsychotics anti-convulsants corticosteroids opiates NSAIDS • anticholinergics • antiparkinsons • benzodiazepines • antidepressants
Why do they get it? – Nobody really knows – Likely chemical imbalances caused by stress/inflammation/medications or combination thereof.

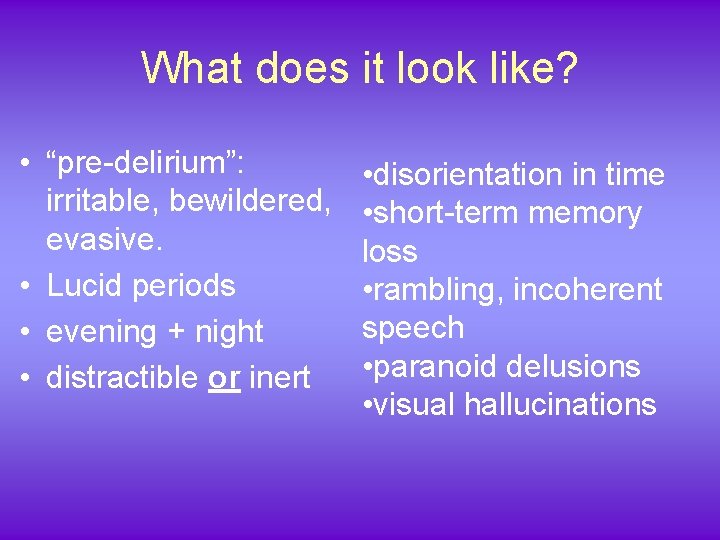
What does it look like? • “pre-delirium”: irritable, bewildered, evasive. • Lucid periods • evening + night • distractible or inert • disorientation in time • short-term memory loss • rambling, incoherent speech • paranoid delusions • visual hallucinations
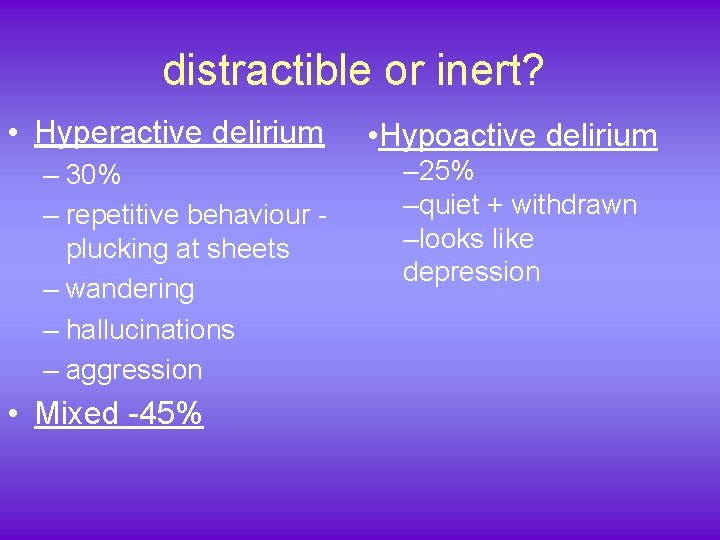
distractible or inert? • Hyperactive delirium – 30% – repetitive behaviour plucking at sheets – wandering – hallucinations – aggression • Mixed -45% • Hypoactive delirium – 25% –quiet + withdrawn –looks like depression
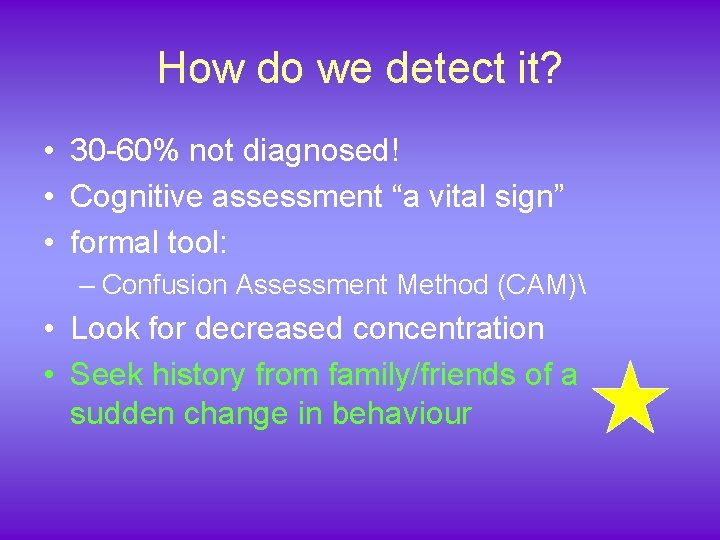
How do we detect it? • 30 -60% not diagnosed! • Cognitive assessment “a vital sign” • formal tool: – Confusion Assessment Method (CAM) • Look for decreased concentration • Seek history from family/friends of a sudden change in behaviour
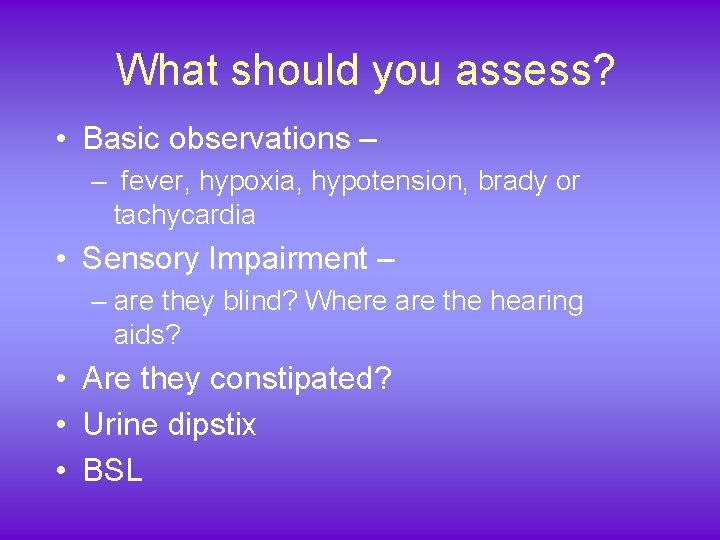
What should you assess? • Basic observations – – fever, hypoxia, hypotension, brady or tachycardia • Sensory Impairment – – are they blind? Where are the hearing aids? • Are they constipated? • Urine dipstix • BSL
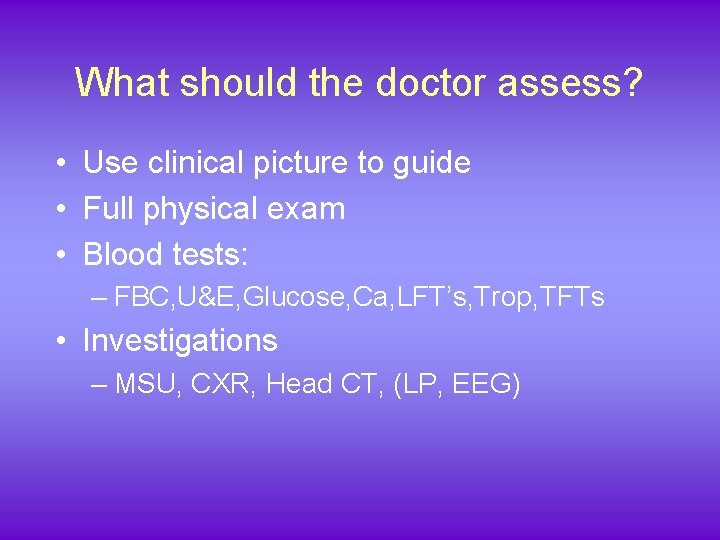
What should the doctor assess? • Use clinical picture to guide • Full physical exam • Blood tests: – FBC, U&E, Glucose, Ca, LFT’s, Trop, TFTs • Investigations – MSU, CXR, Head CT, (LP, EEG)


How do we treat it? • Treat risk factors and precipitants!!!!!
How do we treat while we wait for the definitive treatments to work?
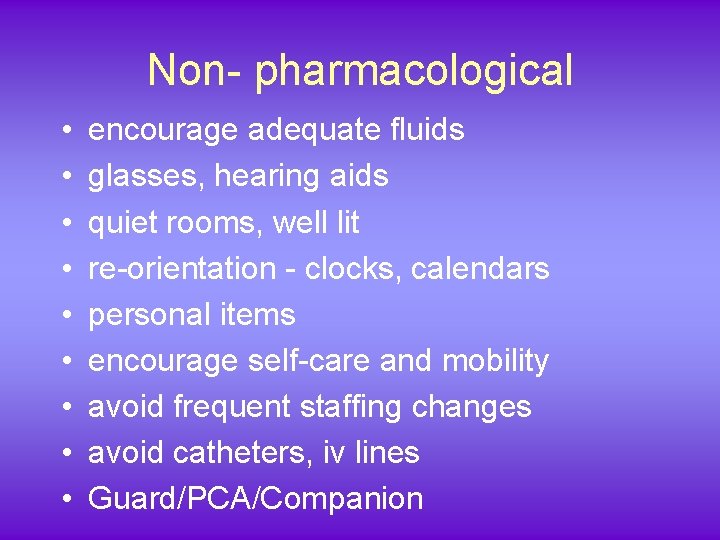
Non- pharmacological • • • encourage adequate fluids glasses, hearing aids quiet rooms, well lit re-orientation - clocks, calendars personal items encourage self-care and mobility avoid frequent staffing changes avoid catheters, iv lines Guard/PCA/Companion
Pharmacological • stop the baddies if possible • only use when patient is distressed, or is a danger to themselves or others • use small amounts • be acutely aware of side-effects - including INCREASE in agitation • dose regularly. Times should coincide with distressing behaviour
What agents to use? • Haloperidol • not much postural hypotension • lots of extrapyramidal/ or PARKINSONIAN side effects - rigidity, tardive dyskinesia • DON’T give to patients with hx Parkinson’s • Atypical anti-pyschotics • Olanzapine, Quetiapine, Risperidone • still some EP problems, also in diabetic patients • Benzodiazepines • mainly for ETOH withdrawal • often make delirium worse otherwise
How long does it last? • Can be for a long time!
Is it really that bad? • Doubles length of stay • 3 X relative risk of developing dementia • increases falls, incontinence and pressure areas • in hospital mortality of 25 -33% • increased risk of ongoing clinical depression
How do we prevent it? • • Identify high risk patients Do cognitive assessment as routine reduce bad drugs maintain adequate analgesia maintain U&E’s, Oxygenation, etc try not to move patients use the same nurse if possible familiar things - pictures from home, clothes, books
What you need to remember about delirium • Confusion with altered Concentration + Consciousness • Lots of Risk factors – dementia and blindness • Look for and treat underlying causes • Get history from family/friends • Avoid iv lines, catheters, changing rooms • Try familiar items, companions • Remember sedatives can make it worse!
Oh, and this Cirque du Soleil production was called “Delirium”.
- Slides: 27