Definity Health Future of Disease Management Under CDHC



- Slides: 51

Definity Health Future of Disease Management Under CDHC Consumer Driven. A Better Way. Tomás D. Valdivia, MD, MS Chief Medical Officer Definity Health
Overview • CDHC introduced new dynamics between the consumer and plan, doctor and DM. • IOM and many others are driving toward a patient-centered health care system with ubiquitous information about the system. • “DM” has a unique challenge to respond to the new health care environment to create and support health care consumers.
Agenda • • Define Consumer-Drive Health Care Describe the effect on constituents Other important activities Implications for Disease Management
Consumer-Driven Healthcare
The Problems
Consumer Driven Healthcare As a benefit strategy: reduces waste and improves healthcare outcomes (including member satisfaction) by giving members the financial responsibility, information, and tools to become empowered consumers of discretionary and routine healthcare services
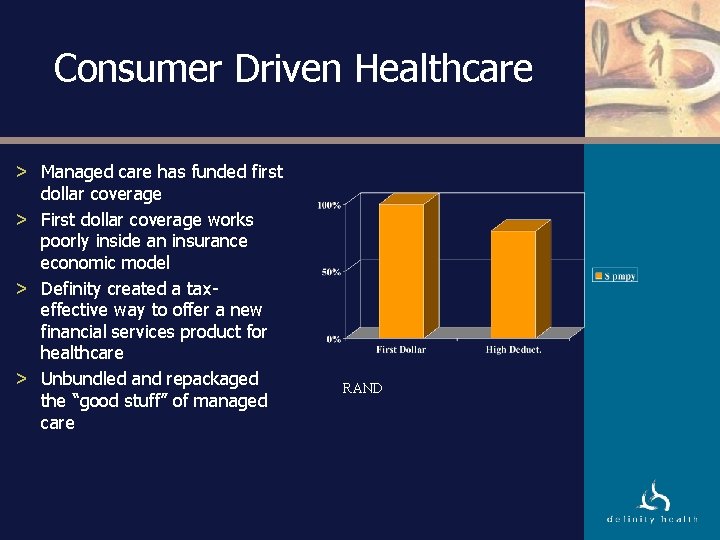
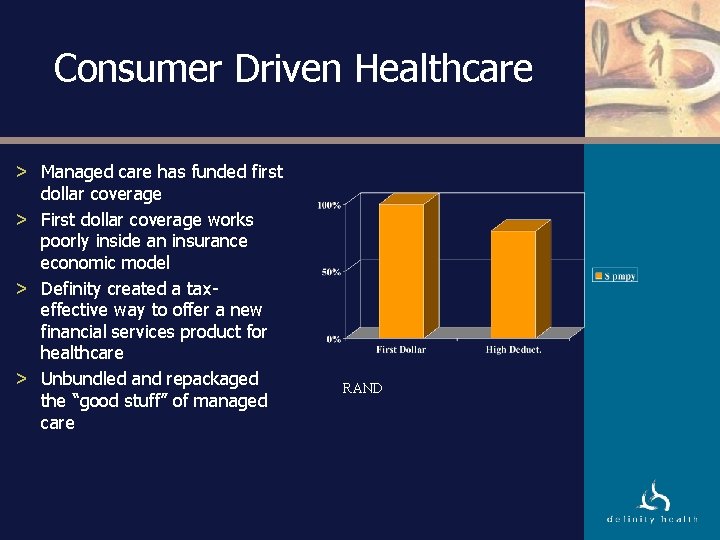
Consumer Driven Healthcare > Managed care has funded first dollar coverage > First dollar coverage works poorly inside an insurance economic model > Definity created a taxeffective way to offer a new financial services product for healthcare > Unbundled and repackaged the “good stuff” of managed care RAND
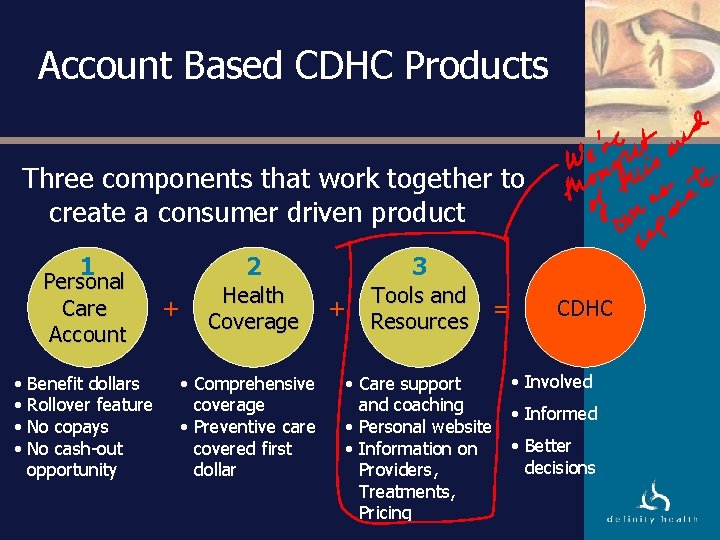
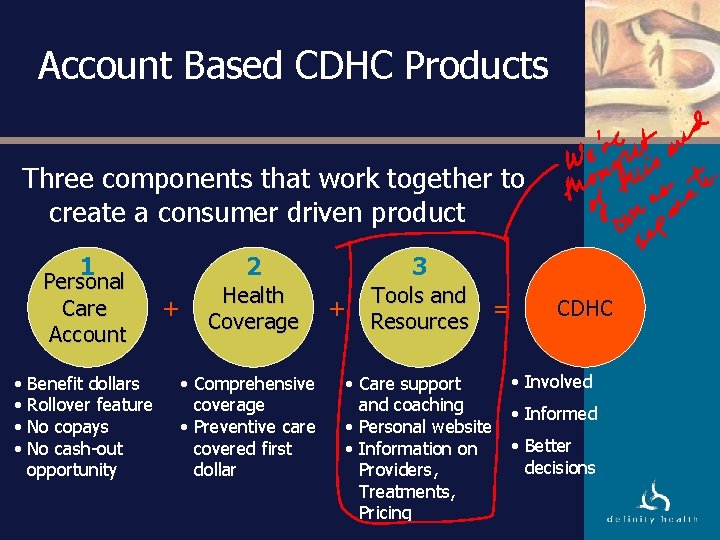
Account Based CDHC Products Three components that work together to create a consumer driven product 1 Personal Care Account • Benefit dollars • Rollover feature • No copays • No cash-out opportunity + 2 3 Health Coverage Tools and Resources • Comprehensive coverage • Preventive care covered first dollar + • Care support and coaching • Personal website • Information on Providers, Treatments, Pricing = CDHC • Involved • Informed • Better decisions
CDHC An Example Meet Phil and Nancy, a growing family with one child, Lisa. Phil and Nancy’s family plan: • Employer-funded PCA allocation: $2, 000 • Health Coverage annual deductible: $3, 000
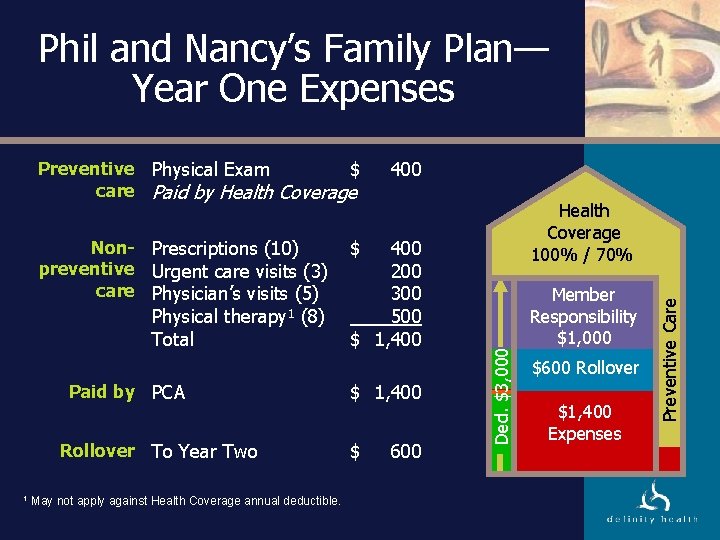
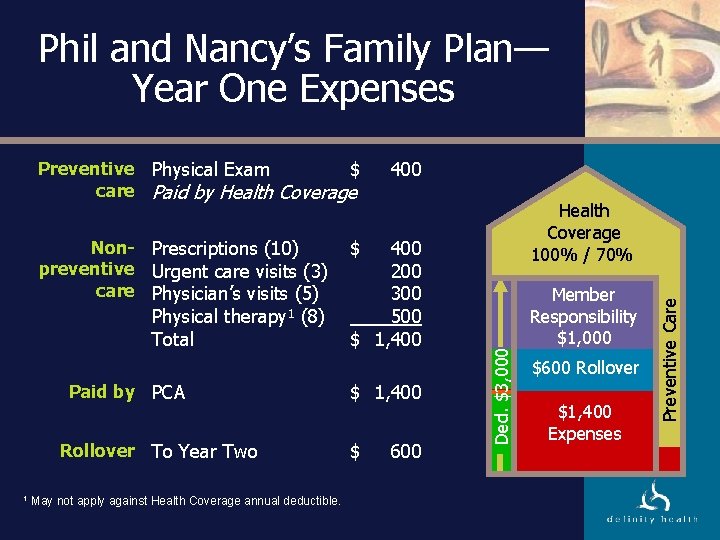
Phil and Nancy’s Family Plan— Year One Expenses Physical therapy 1 (8) Total Paid by PCA Rollover To Year Two 1 May not apply against Health Coverage annual deductible. 400 200 300 500 $ 1, 400 Health Coverage 100% / 70% $ $ 1, 400 $ 600 Ded. $3, 000 Non- Prescriptions (10) preventive Urgent care visits (3) care Physician’s visits (5) 400 Member Responsibility $1, 000 $600 PCA Rollover $2, 000 $1, 400 Expenses Preventive Care Preventive Physical Exam $ care Paid by Health Coverage
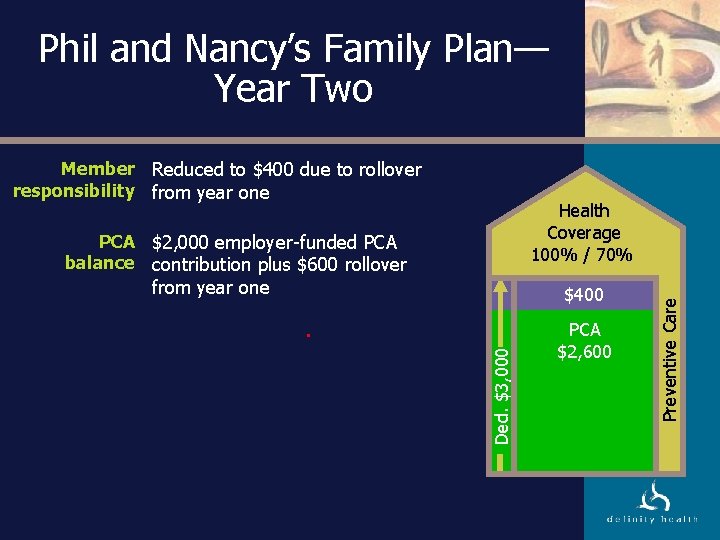
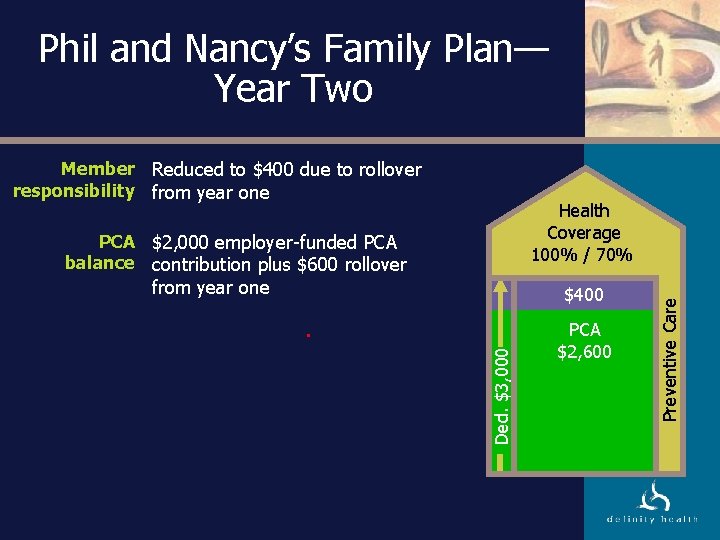
Phil and Nancy’s Family Plan— Year Two Member Reduced to $400 due to rollover responsibility from year one PCA $2, 000 employer-funded PCA balance contribution plus $600 rollover from year one Ded. $3, 000 $400 $600 PCA Rollover $2, 600 PCA $2, 000 Preventive Care Health Coverage 100% / 70%
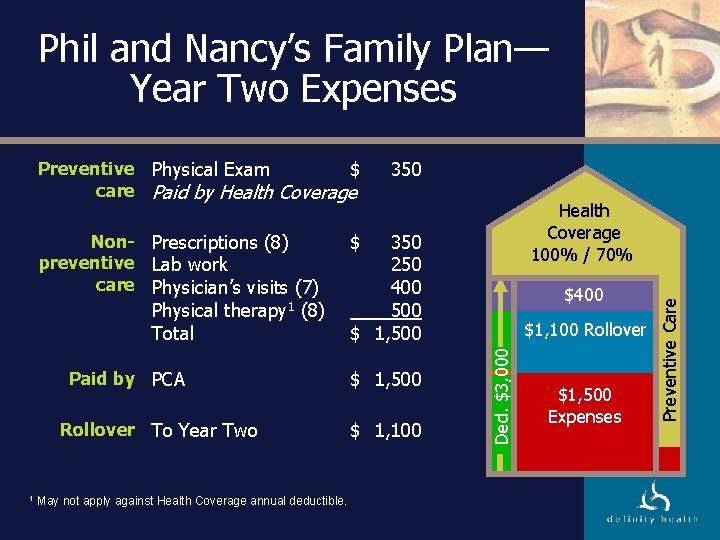
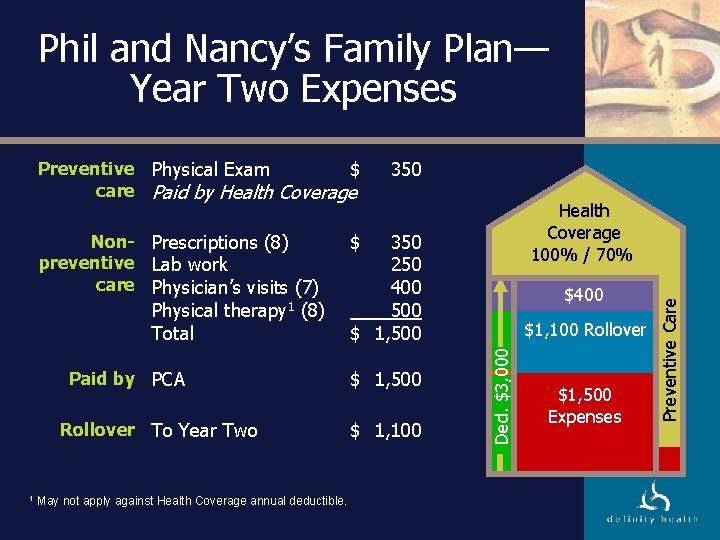
Phil and Nancy’s Family Plan— Year Two Expenses Physical Total therapy 1 (8) Paid by PCA Rollover To Year Two 1 May not apply against Health Coverage annual deductible. Health Coverage 100% / 70% $ 350 250 400 500 $ 1, 100 $400 Ded. $3, 000 Non- Prescriptions (8) preventive Lab work care Physician’s visits (7) 350 $1, 100 PCA Rollover $2, 600 $1, 500 Expenses Preventive Care Preventive Physical Exam $ care Paid by Health Coverage
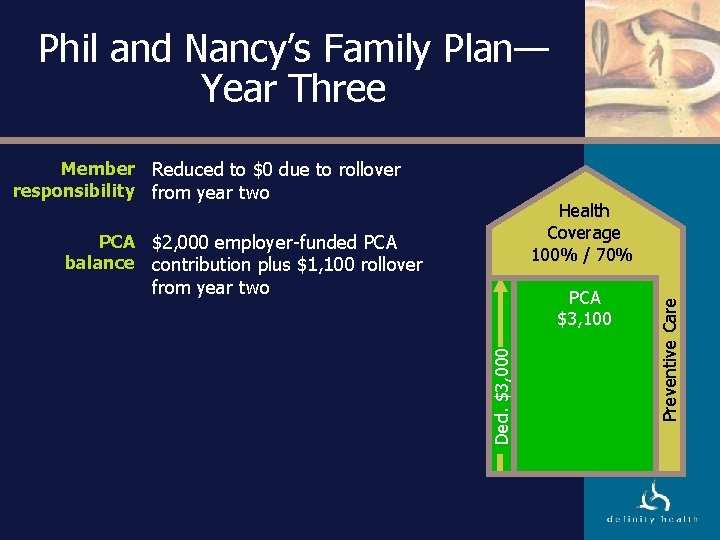
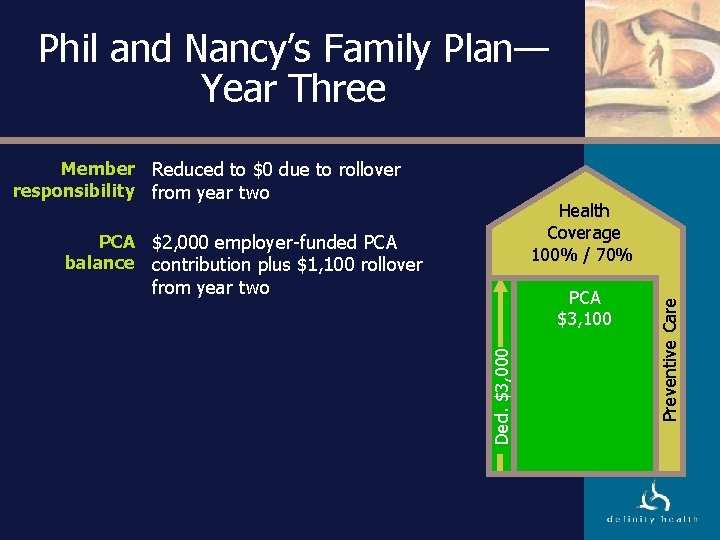
Phil and Nancy’s Family Plan— Year Three Member Reduced to $0 due to rollover responsibility from year two PCA $2, 000 employer-funded PCA balance contribution plus $1, 100 rollover from year two Ded. $3, 000 $1, 100 Rollover PCA $3, 100 PCA $2, 000 Preventive Care Health Coverage 100% / 70%
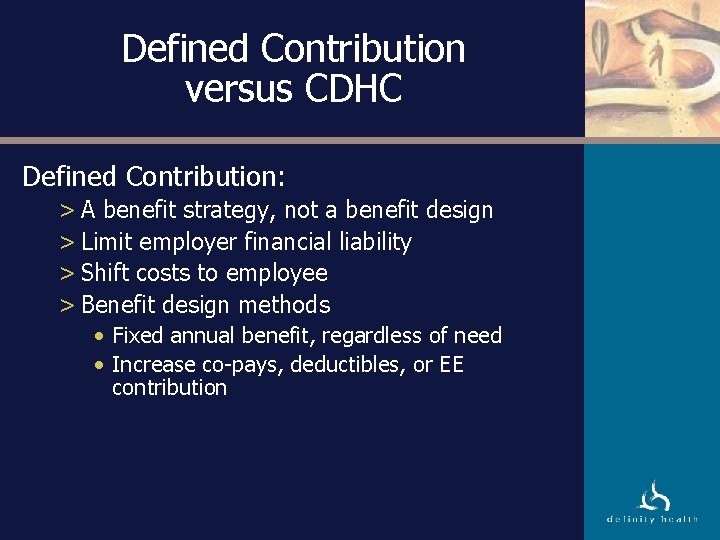
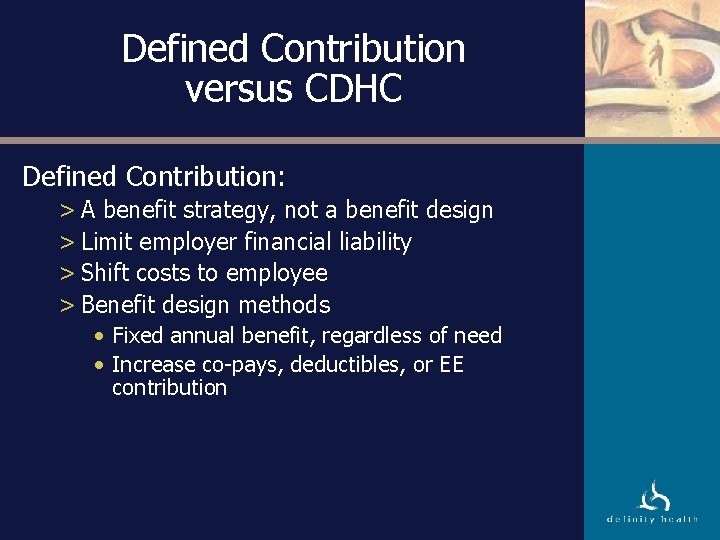
Defined Contribution versus CDHC Defined Contribution: > A benefit strategy, not a benefit design > Limit employer financial liability > Shift costs to employee > Benefit design methods • Fixed annual benefit, regardless of need • Increase co-pays, deductibles, or EE contribution
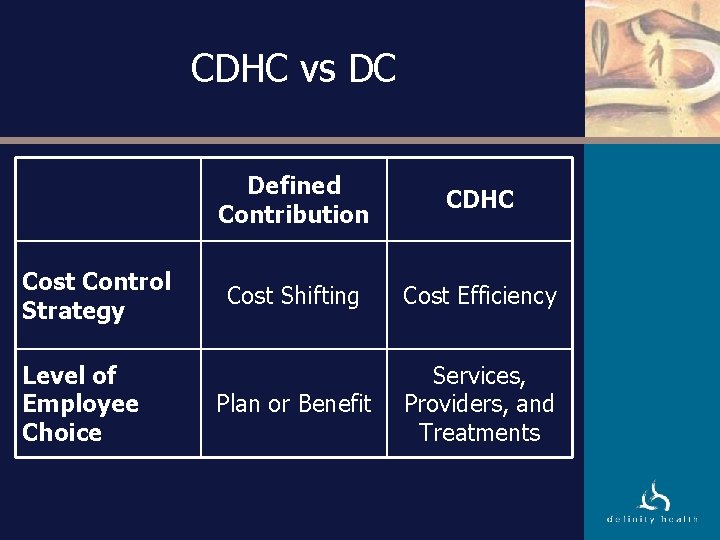
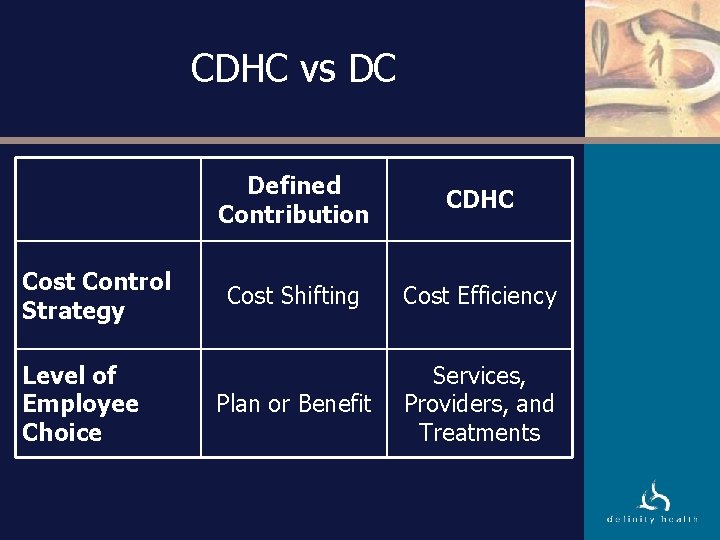
CDHC vs DC Cost Control Strategy Level of Employee Choice Defined Contribution CDHC Cost Shifting Cost Efficiency Plan or Benefit Services, Providers, and Treatments
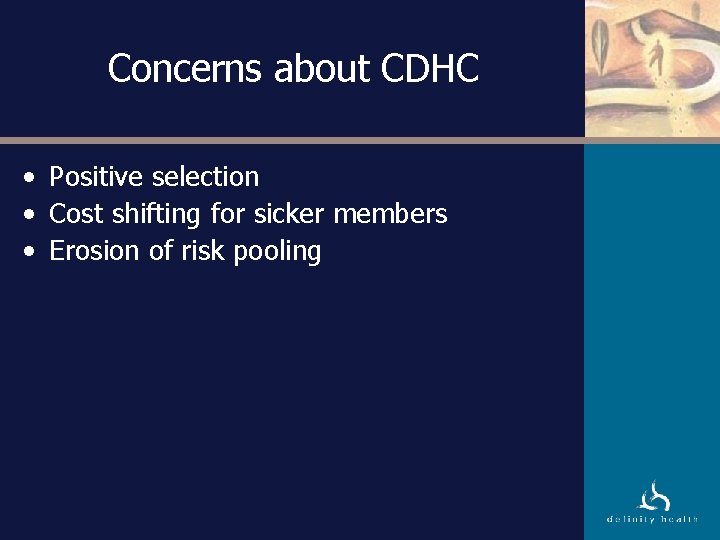
Concerns about CDHC • Positive selection • Cost shifting for sicker members • Erosion of risk pooling
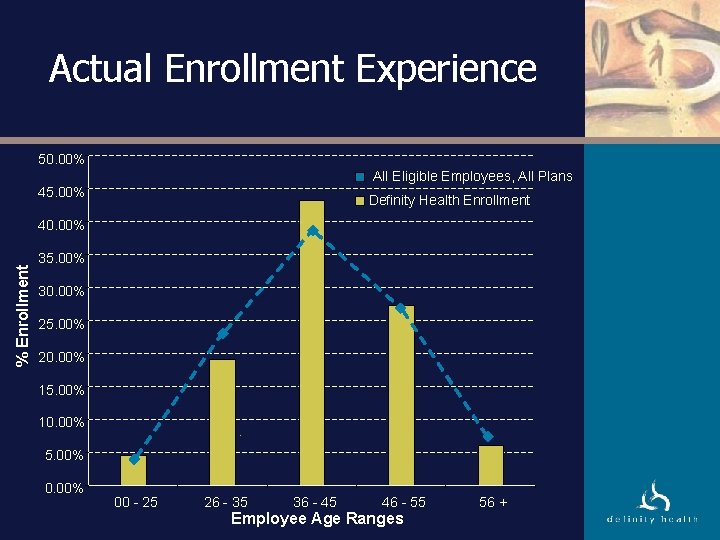
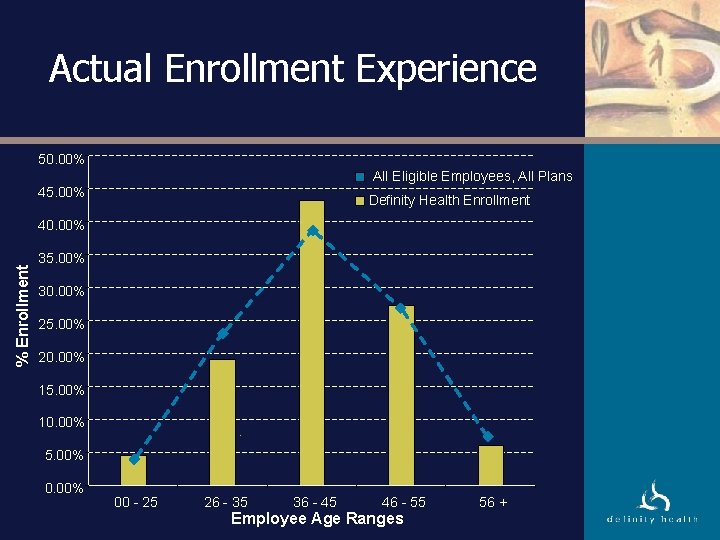
Actual Enrollment Experience 50. 00% All Eligible Employees, All Plans 45. 00% Definity Health Enrollment % Enrollment 40. 00% 35. 00% 30. 00% 25. 00% 20. 00% 15. 00% 10. 00% 5. 00% 00 - 25 26 - 35 36 - 45 46 - 55 Employee Age Ranges 56 +
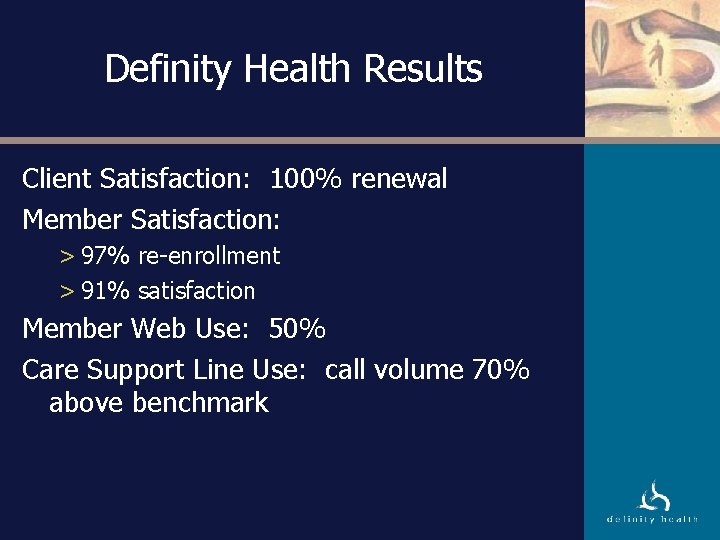
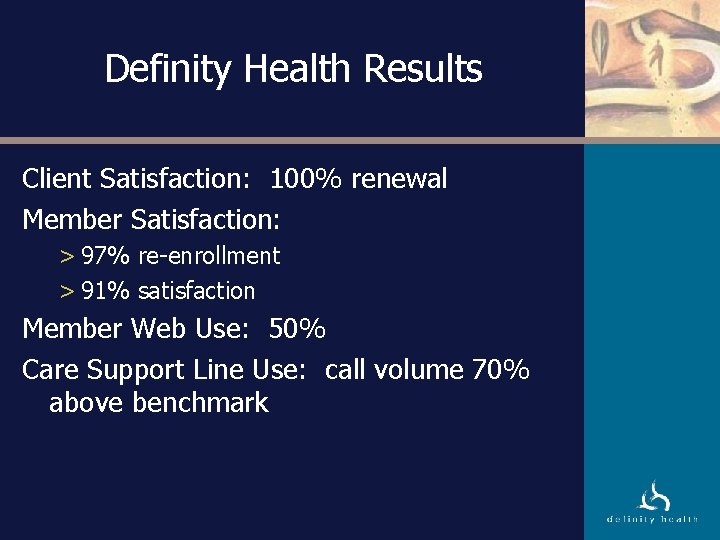
Definity Health Results Client Satisfaction: 100% renewal Member Satisfaction: > 97% re-enrollment > 91% satisfaction Member Web Use: 50% Care Support Line Use: call volume 70% above benchmark

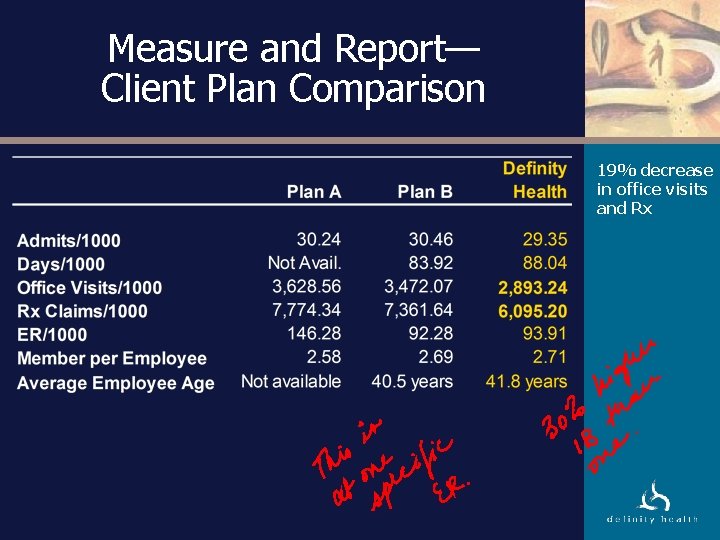
Utilization Results Cost control: better than market trend Utilization: > Inpatient: comparable to M&R well managed > Outpatient: 20% reduction in office visits > Pharmacy: better than Medco tightly managed benchmark > Preventive services: at or above national benchmarks
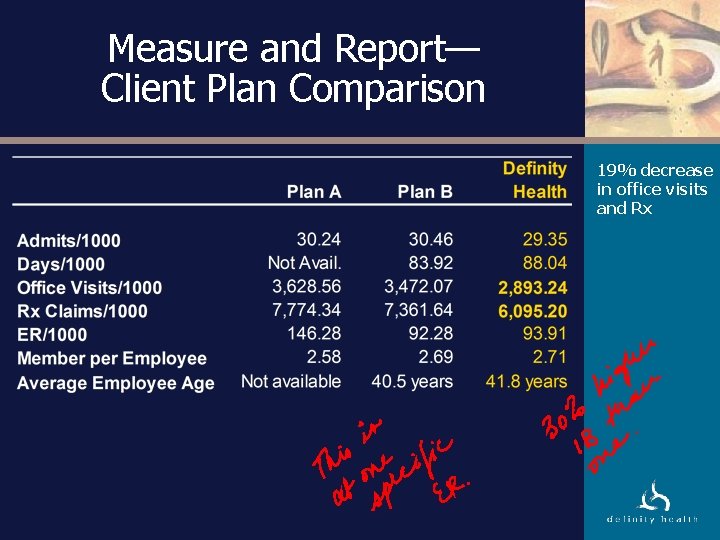
Measure and Report— Client Plan Comparison 19% decrease in office visits and Rx
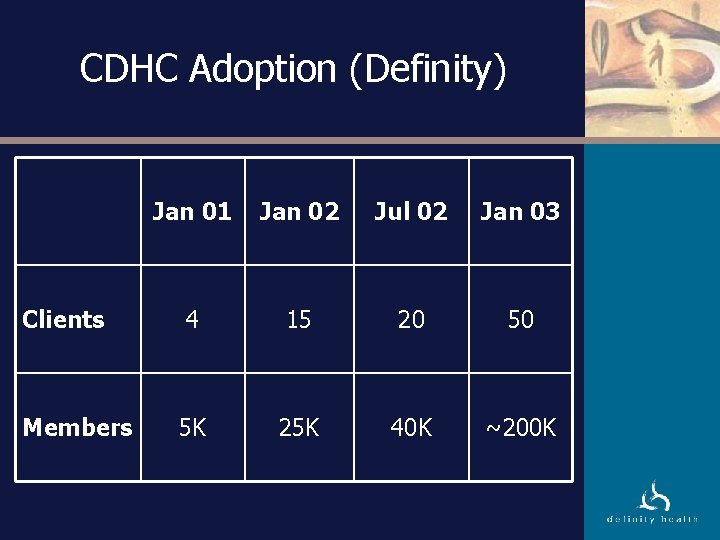
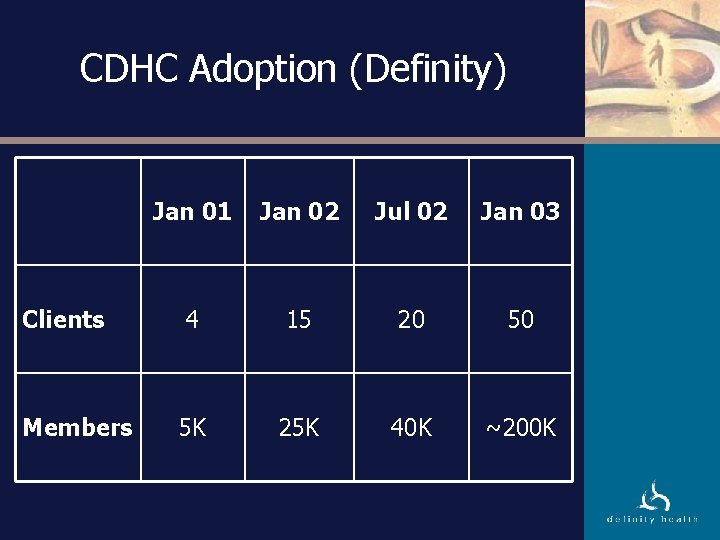
CDHC Adoption (Definity) Jan 01 Jan 02 Jul 02 Jan 03 Clients 4 15 20 50 Members 5 K 25 K 40 K ~200 K
Effect of CDHC on Constituents

New Behaviors Employee Passive Participant Active Consumer Employer Primary Purchaser Financial Contributor Health Plan Barrier Enabler Provider Restricted Care Manager
Old DM
Definition: A Health Care Consumer A health care consumer is > An individual… > …choosing the services… > …they use… > …and bearing the consequences (financial and others) of those choices. • More technologically savvy • Well-educated • Wealthier than their parents
Our Members: Engaged Concerned (and informed) about costs Involved as an active decision maker Longer term view of healthcare spending > No longer year to year > More interested in preventive health
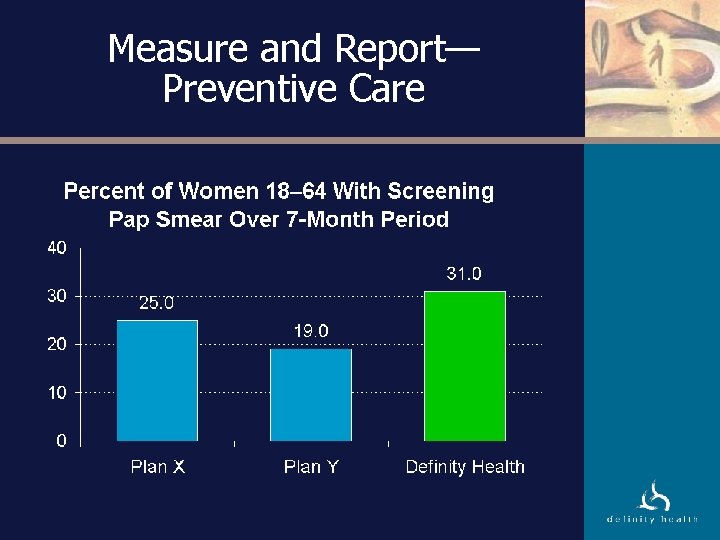
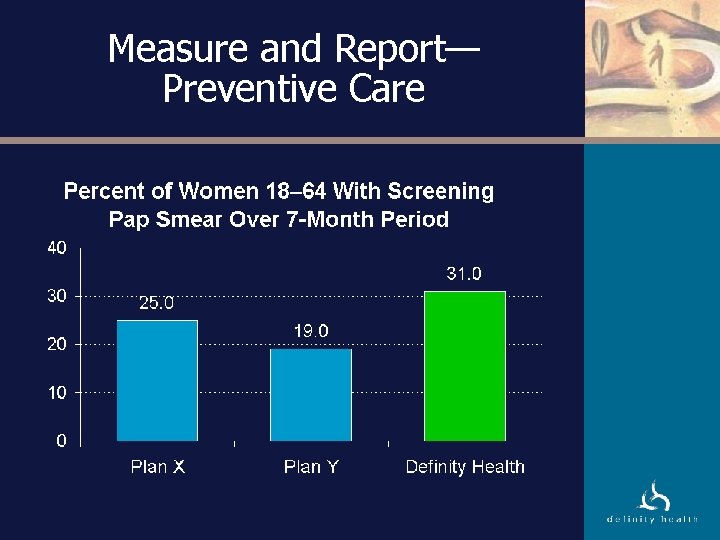
Measure and Report— Preventive Care
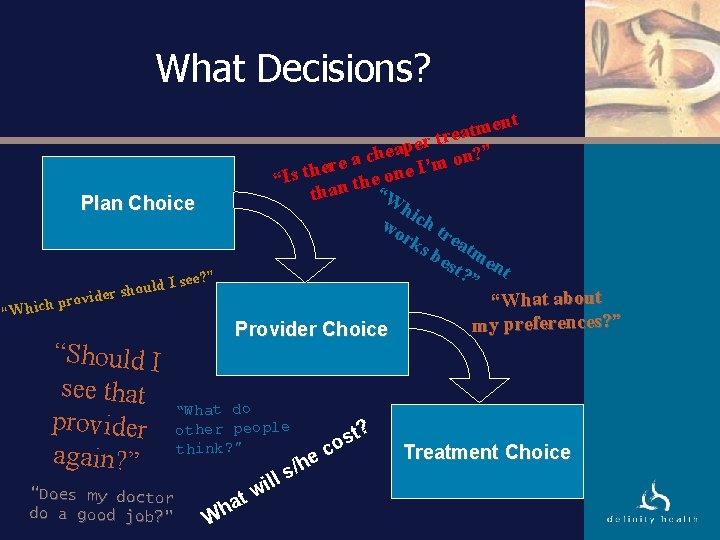
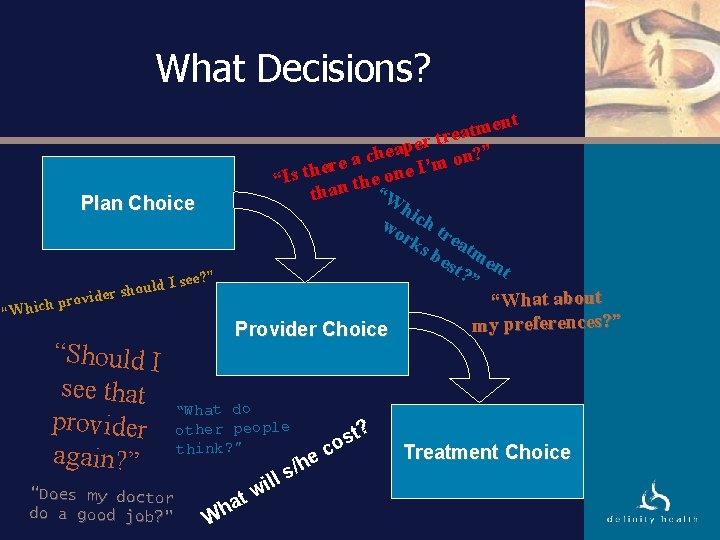
What Decisions? Plan Choice ee? ” “Which uld I s o h s r e vid pro “Should I see that provider again? ” ent m t a tre r e p a ? ” che n o a e m r e I’ “Is th n the one “W tha hic wo h tr rk s b eatm est en ? ” t “What about my preferences? ” Provider Choice “What do other people think? ” “Does my doctor do a good job? ” a h W ill w t e s/h st? o c Treatment Choice
Effect on Physicians: Intrigued Three possible paths: > Continued “commoditization”: price competition only, now at the individual provider level > Differentiation and market segmentation on the basis of quality and value and member preferences > Isolated care monopolies: no change?
Other Important Activities
Focus on Information Availability • Institute of Medicine -To Err is Human (1999) • Leapfrog Group (2000) • Institute of Medicine - Envisioning the National Health Care Quality Report (2001) • Midwest Business Group on Health - Cost of Poor Quality (2002)
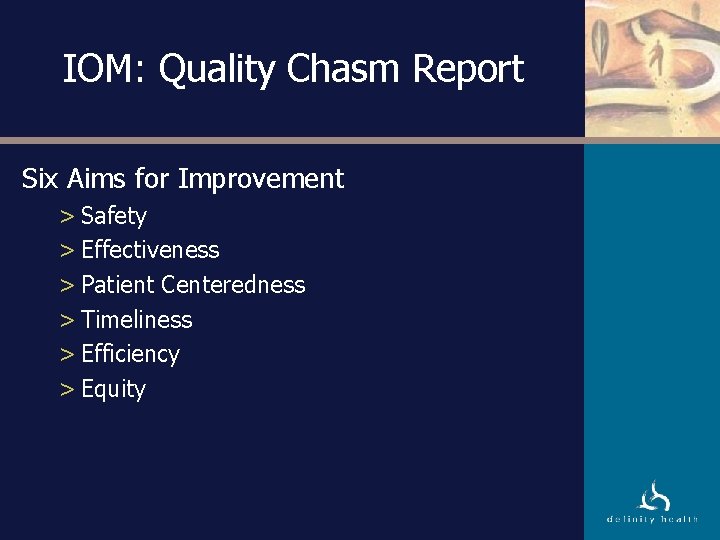
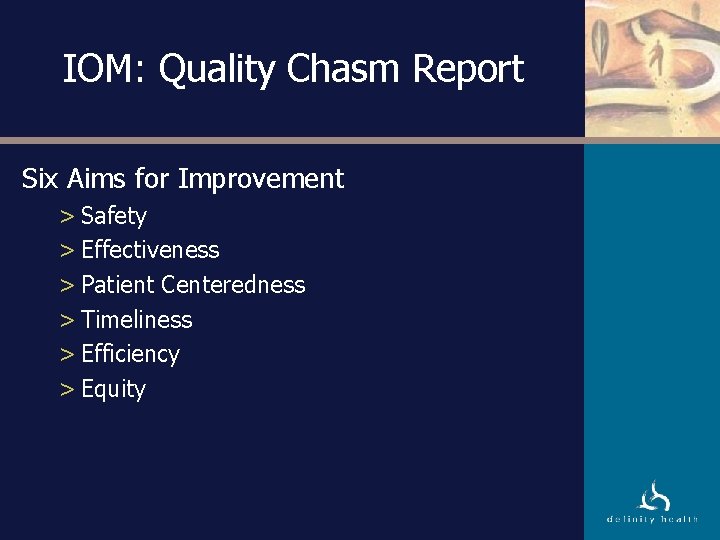
IOM: Quality Chasm Report Six Aims for Improvement > Safety > Effectiveness > Patient Centeredness > Timeliness > Efficiency > Equity
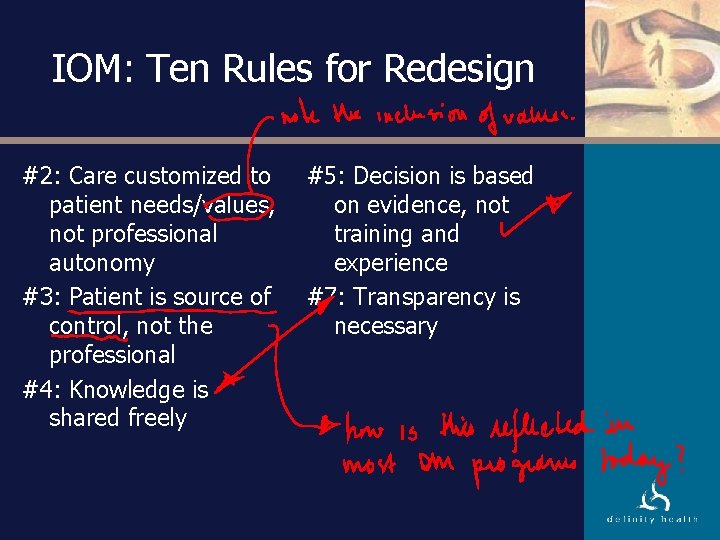
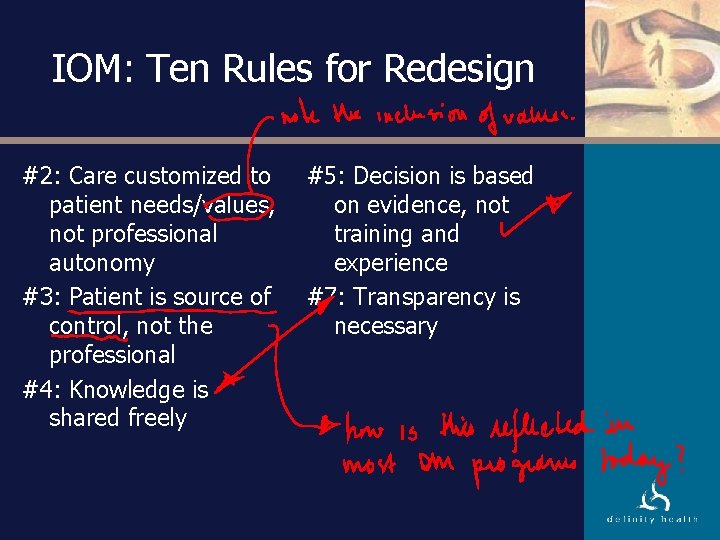
IOM: Ten Rules for Redesign #2: Care customized to patient needs/values, not professional autonomy #3: Patient is source of control, not the professional #4: Knowledge is shared freely #5: Decision is based on evidence, not training and experience #7: Transparency is necessary
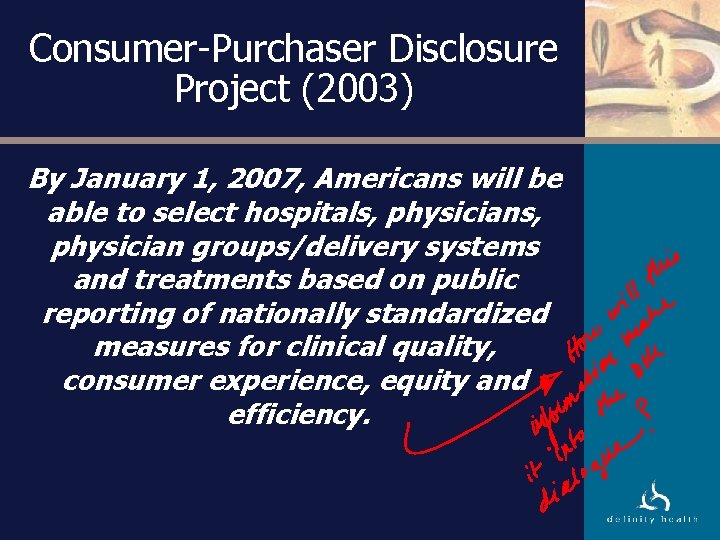
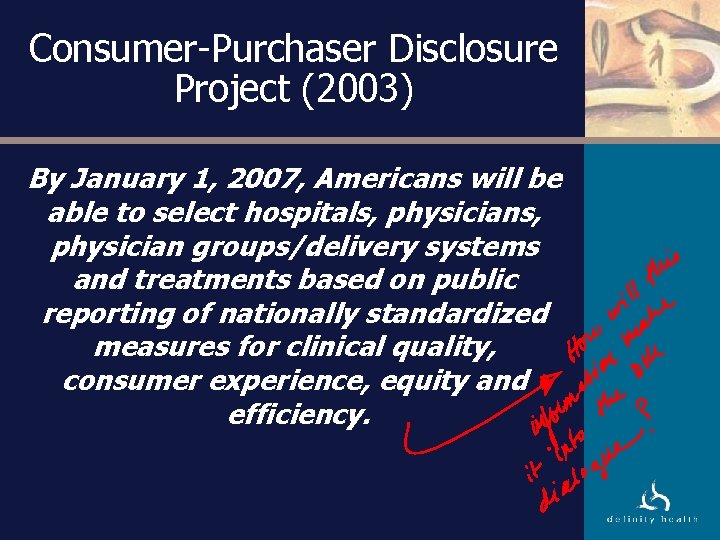
Consumer-Purchaser Disclosure Project (2003) By January 1, 2007, Americans will be able to select hospitals, physician groups/delivery systems and treatments based on public reporting of nationally standardized measures for clinical quality, consumer experience, equity and efficiency.
Implications for DM
New Directions in DM
New Directions in DM Plan Level > Consumer incentives “baked” into the plan • Implicit • Explicit > Plan services integration > Changing perspective: “Right care at the right time, right place, …”
New Directions in DM Program Features > Consider the practice context at identification step > New information: comprehensible transparency of cost and quality > Support extended to non-standard practices for • value decisions in health care • new transparency of information • non-traditional matters (significant medical decisions) > Create consumers
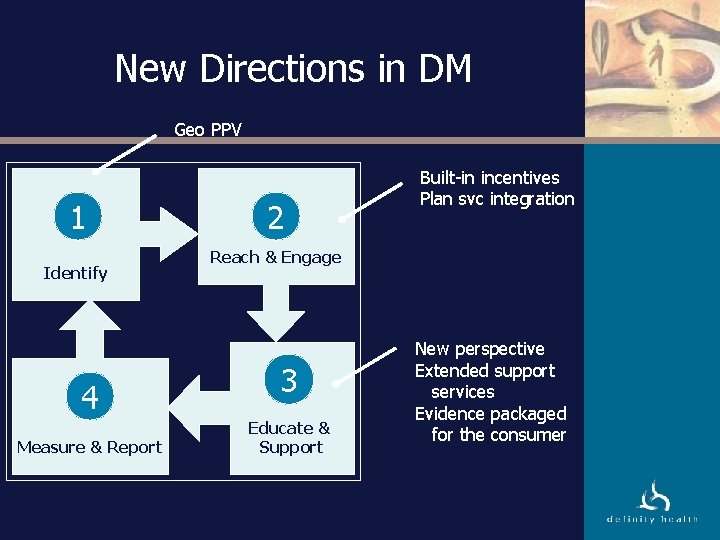
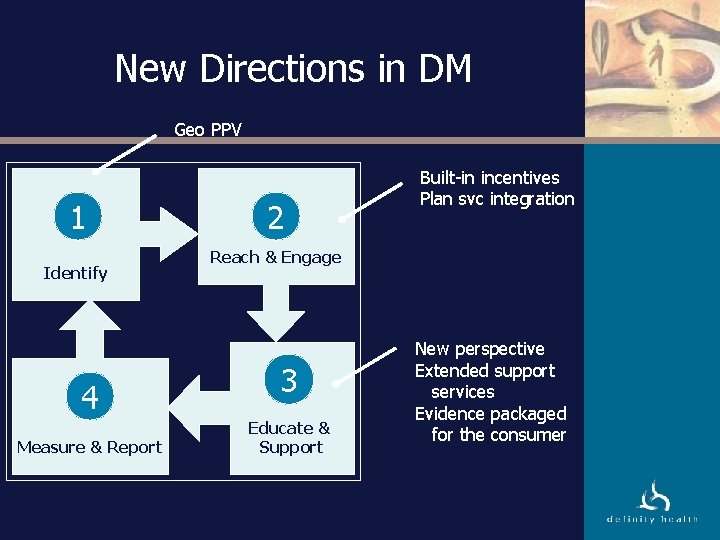
New Directions in DM Geo PPV 1 Identify 4 Measure & Report 2 Built-in incentives Plan svc integration Reach & Engage 3 Educate & Support New perspective Extended support services Evidence packaged for the consumer
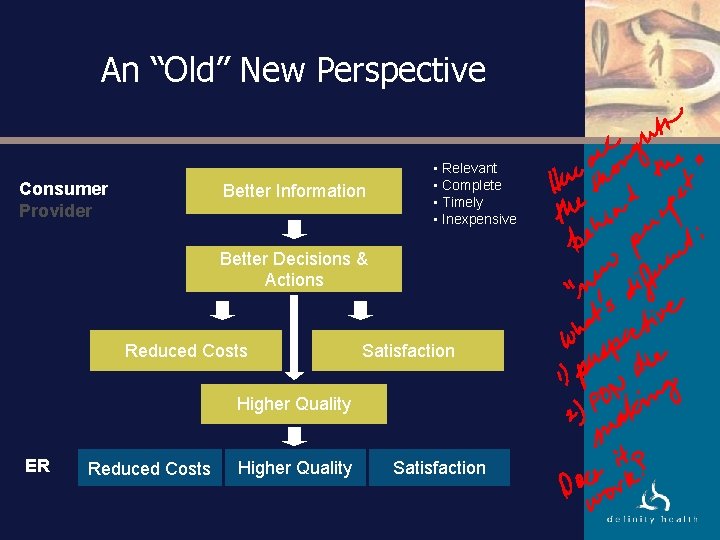
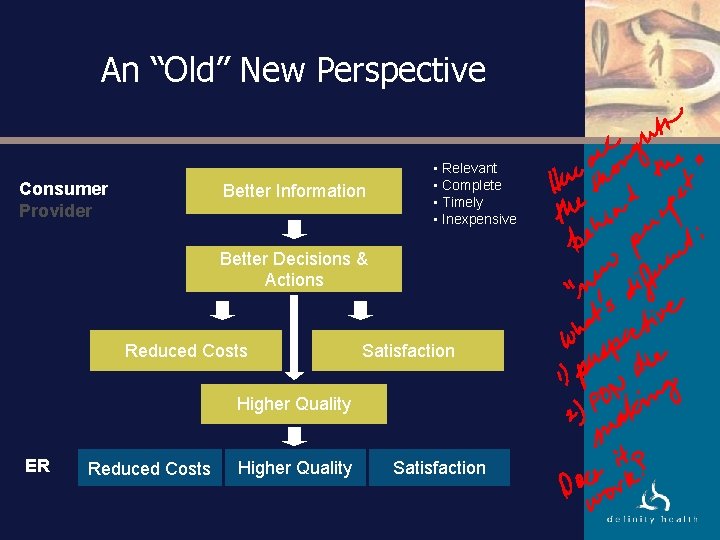
An “Old” New Perspective Consumer Provider Better Information • Relevant • Complete • Timely • Inexpensive Better Decisions & Actions Reduced Costs Satisfaction Higher Quality ER Reduced Costs Higher Quality Satisfaction
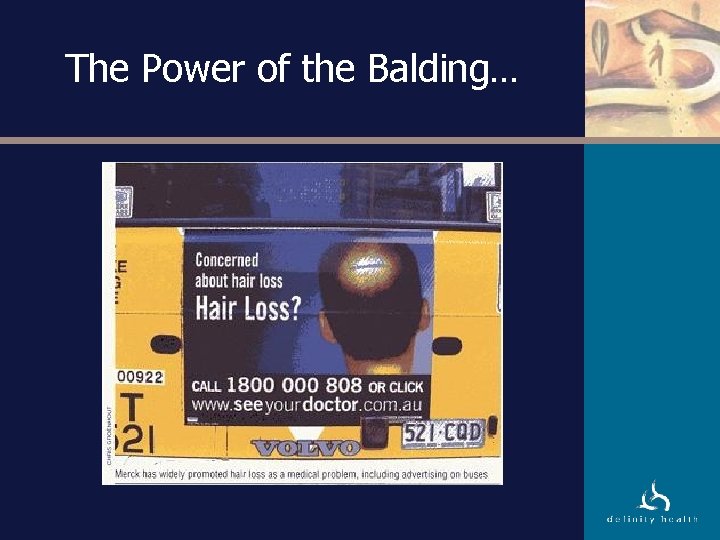
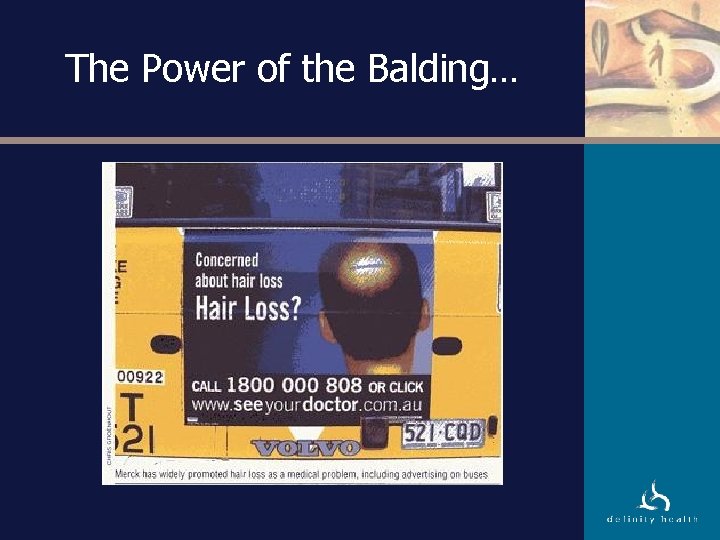
The Power of the Balding…
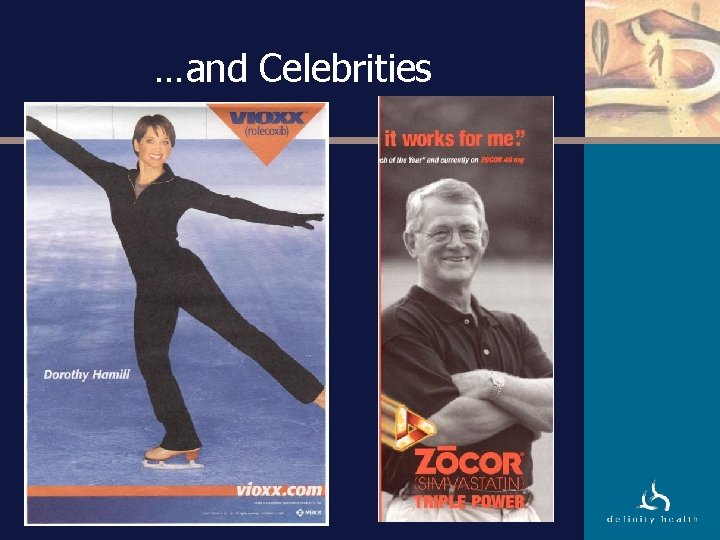
…and Celebrities
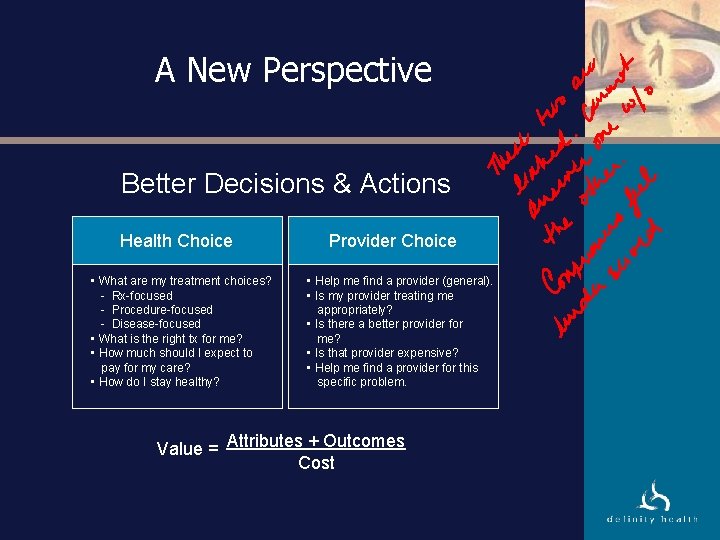
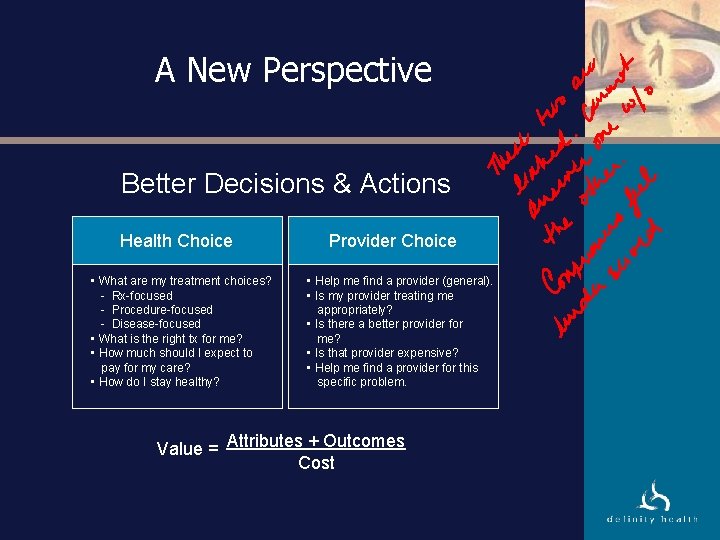
A New Perspective Better Decisions & Actions Health Choice • What are my treatment choices? - Rx-focused - Procedure-focused - Disease-focused • What is the right tx for me? • How much should I expect to pay for my care? • How do I stay healthy? Provider Choice • Help me find a provider (general). • Is my provider treating me appropriately? • Is there a better provider for me? • Is that provider expensive? • Help me find a provider for this specific problem. Value = Attributes + Outcomes Cost
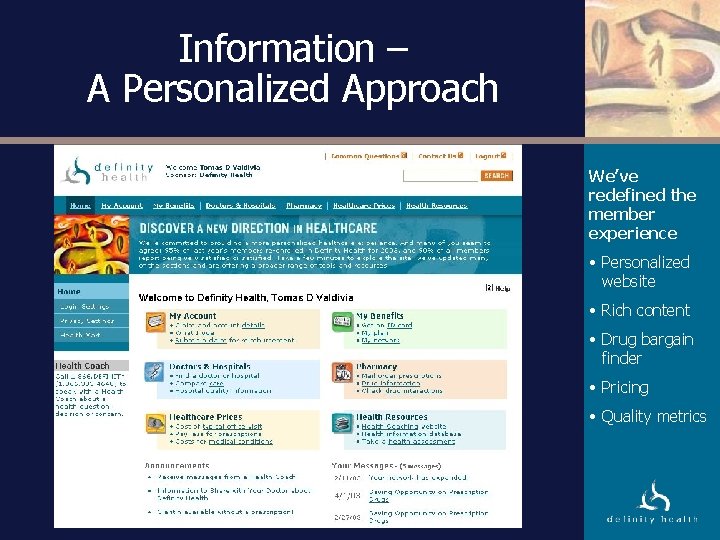
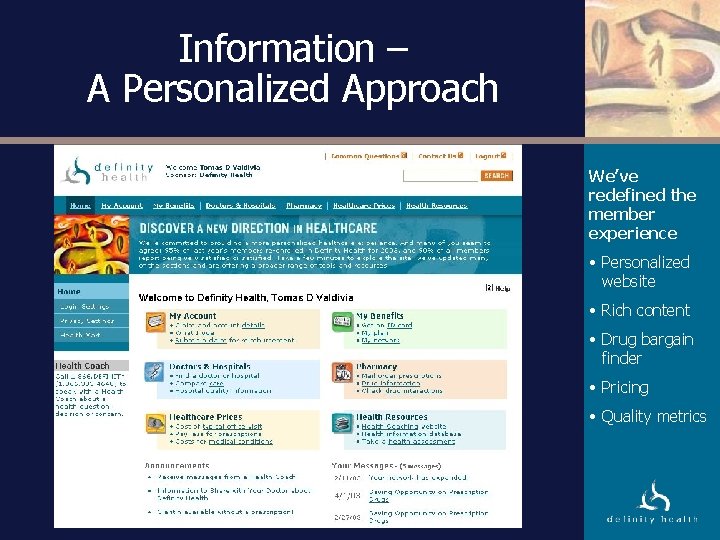
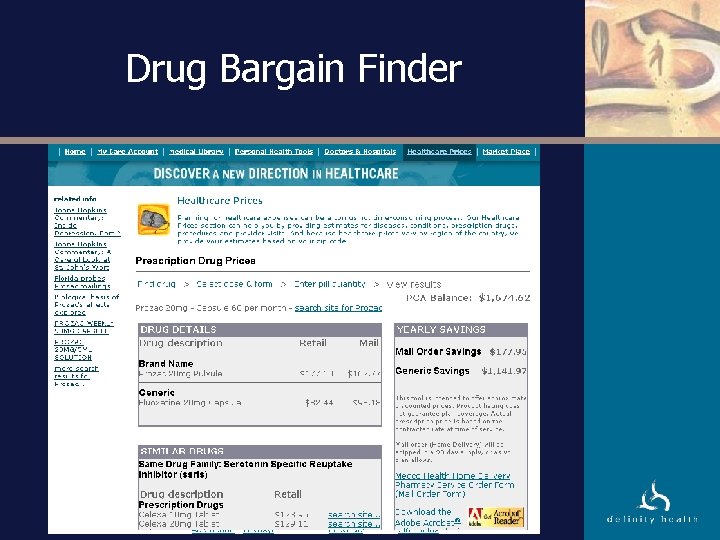
Information – A Personalized Approach We’ve redefined the member experience • Personalized website • Rich content • Drug bargain finder • Pricing • Quality metrics
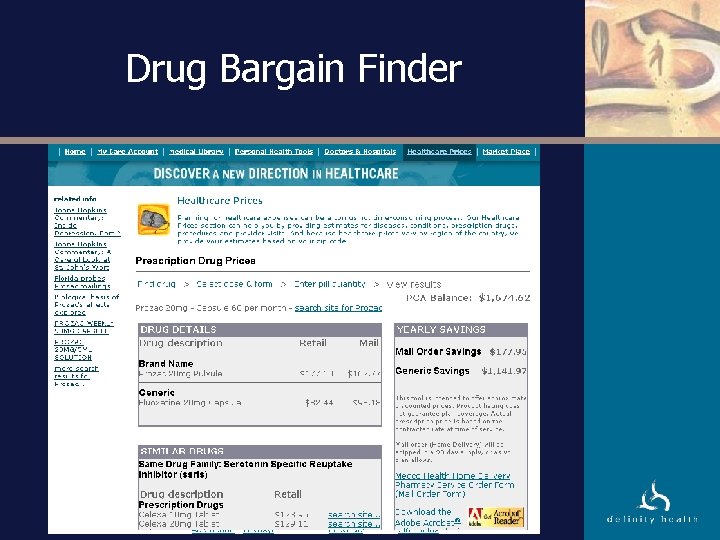
Drug Bargain Finder
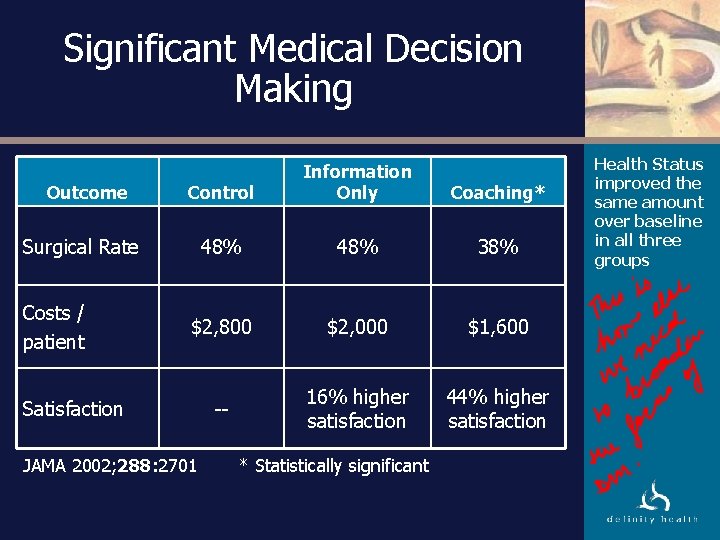
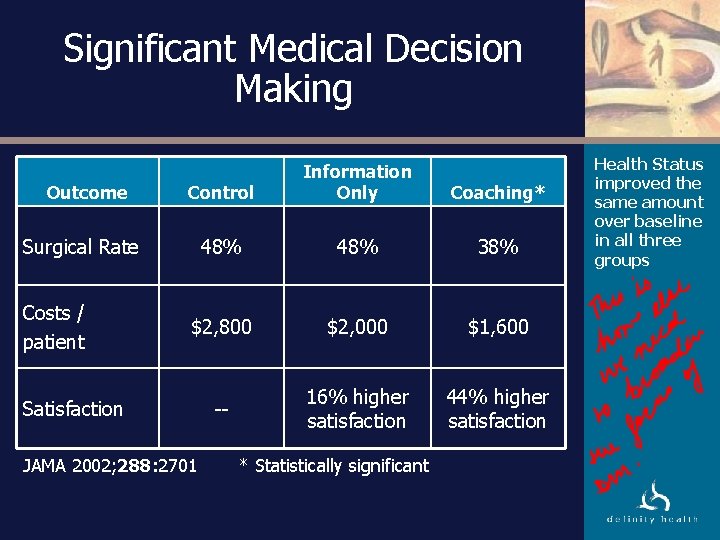
Significant Medical Decision Making Outcome Control Information Only Coaching* 48% 38% $2, 800 $2, 000 $1, 600 -- 16% higher satisfaction 44% higher satisfaction Surgical Rate Costs / patient Satisfaction JAMA 2002; 288: 2701 * Statistically significant Health Status improved the same amount over baseline in all three groups
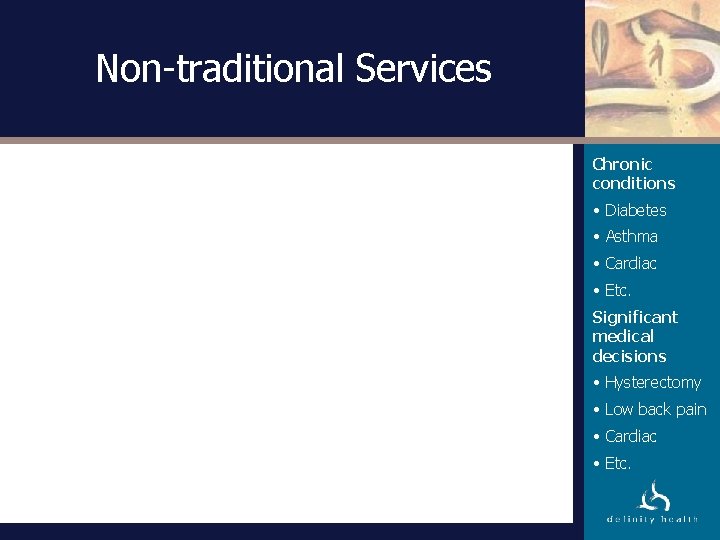
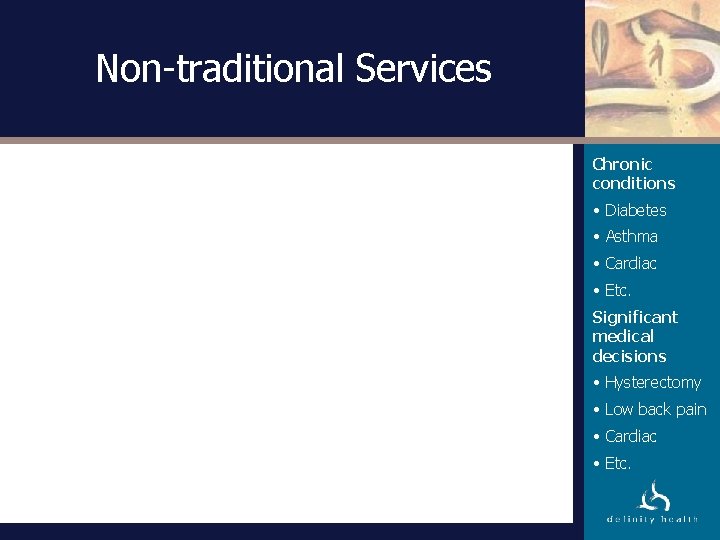
Non-traditional Services Chronic conditions • Diabetes • Asthma • Cardiac • Etc. Significant medical decisions • Hysterectomy • Low back pain • Cardiac • Etc.
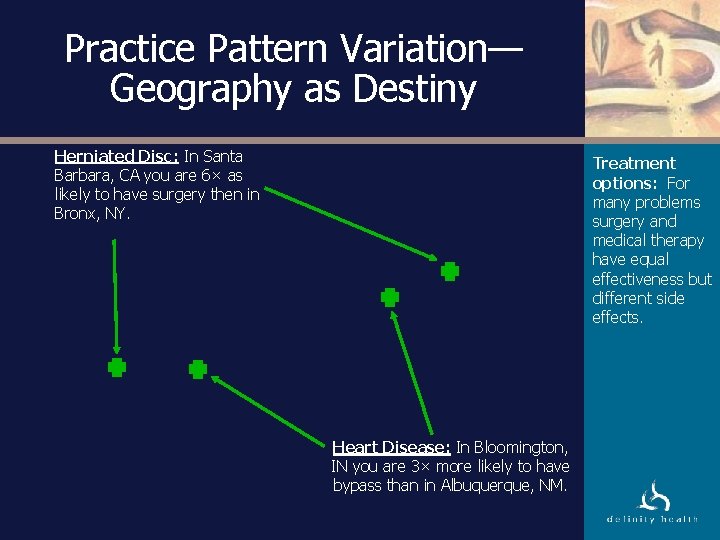
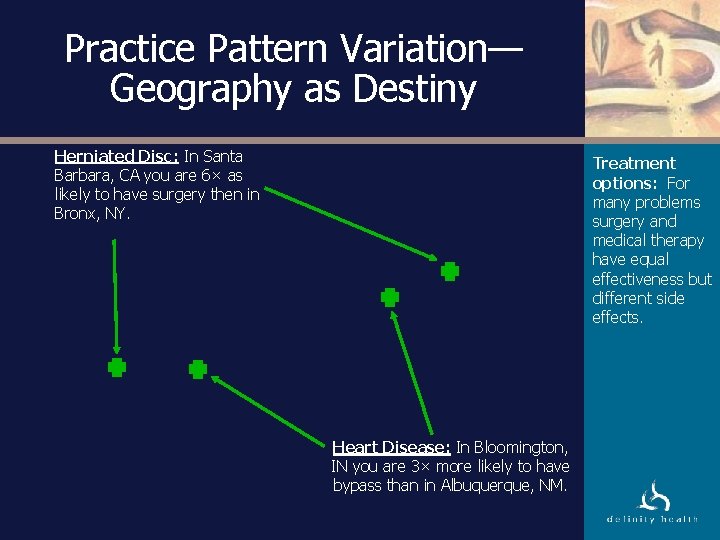
Practice Pattern Variation— Geography as Destiny Herniated Disc: In Santa Barbara, CA you are 6× as likely to have surgery then in Bronx, NY. Treatment options: For many problems surgery and medical therapy have equal effectiveness but different side effects. Heart Disease: In Bloomington, IN you are 3× more likely to have bypass than in Albuquerque, NM.
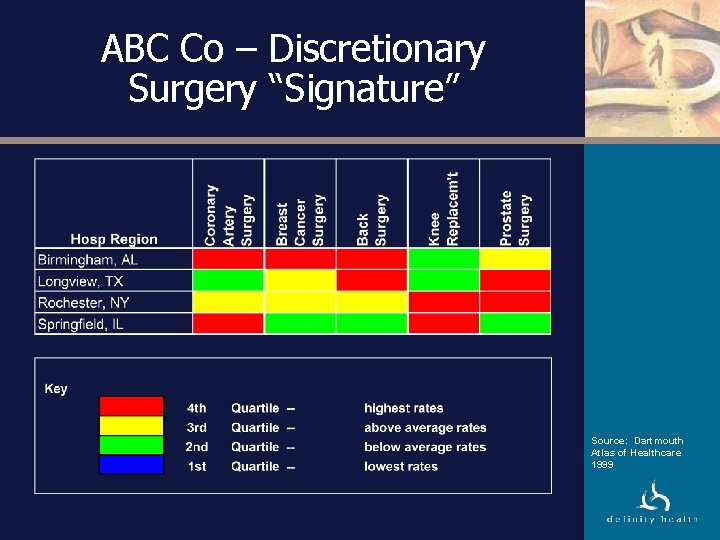
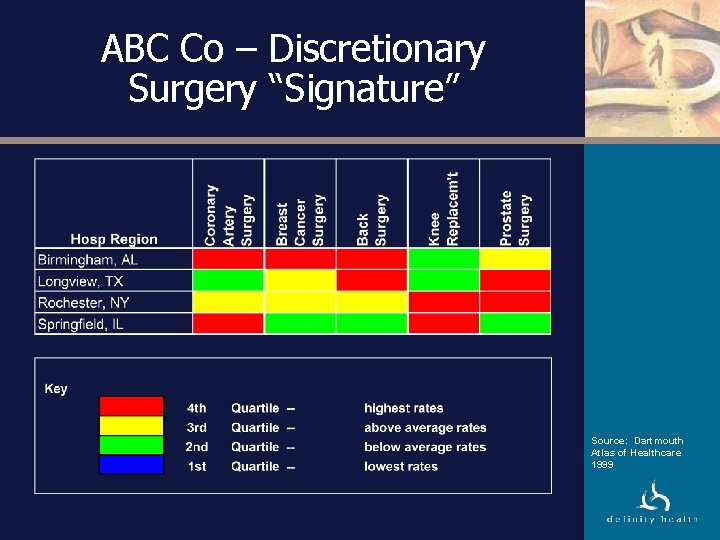
ABC Co – Discretionary Surgery “Signature” Source: Dartmouth Atlas of Healthcare 1999
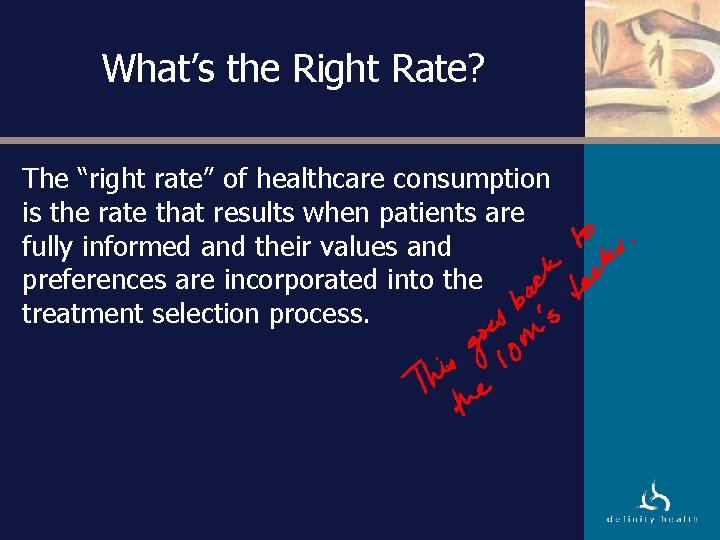
What’s the Right Rate? The “right rate” of healthcare consumption is the rate that results when patients are fully informed and their values and preferences are incorporated into the treatment selection process.
Summary • CDHC introduced new dynamics between the consumer and plan, doctor and DM. • IOM and many others are driving toward a patient-centered health care system with ubiquitous information about the system. • “DM” has a unique challenge to respond to the new health care environment.