Definition of Chronic Kidney Disease 1 3 GFR







- Slides: 58

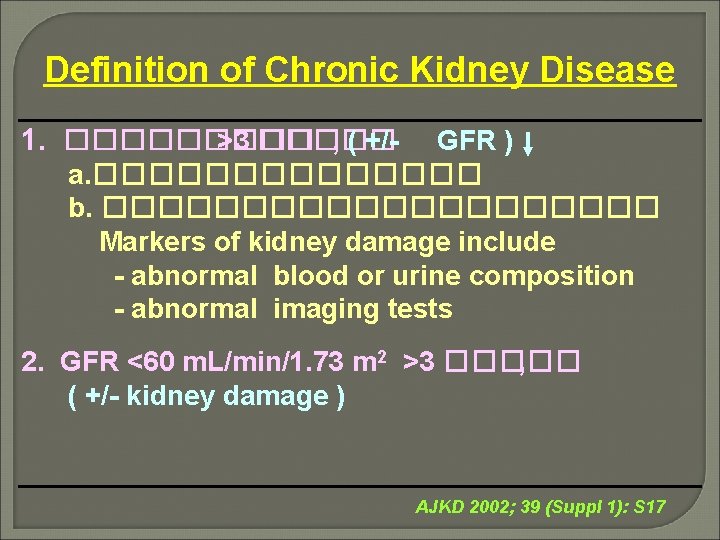
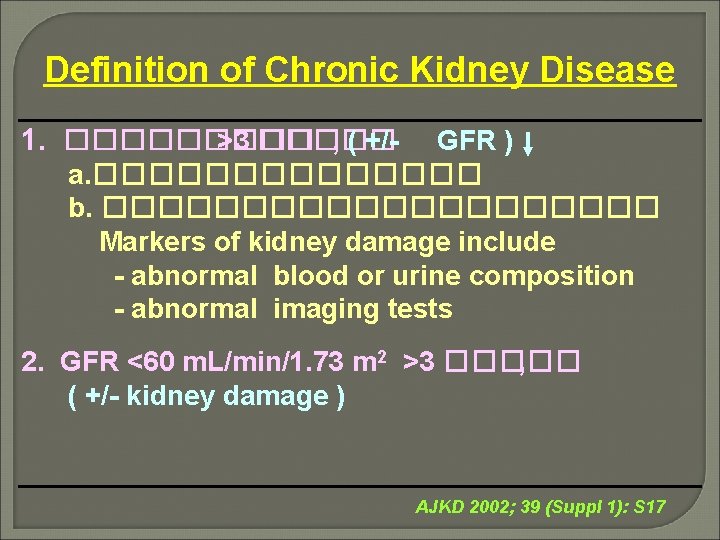
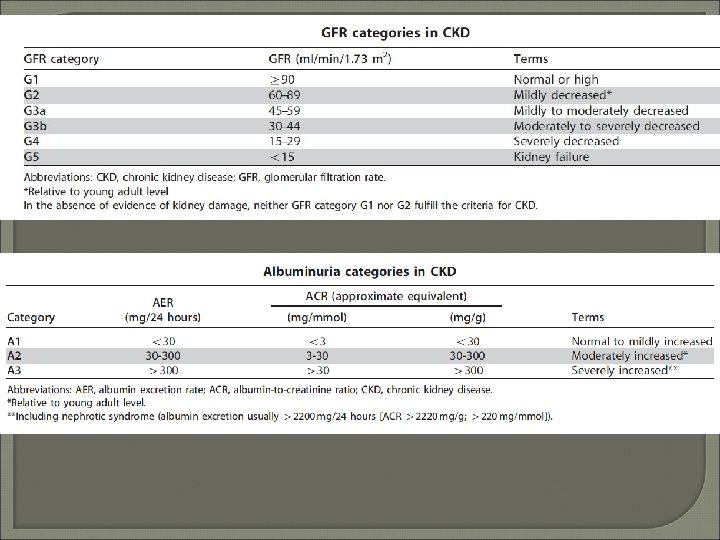
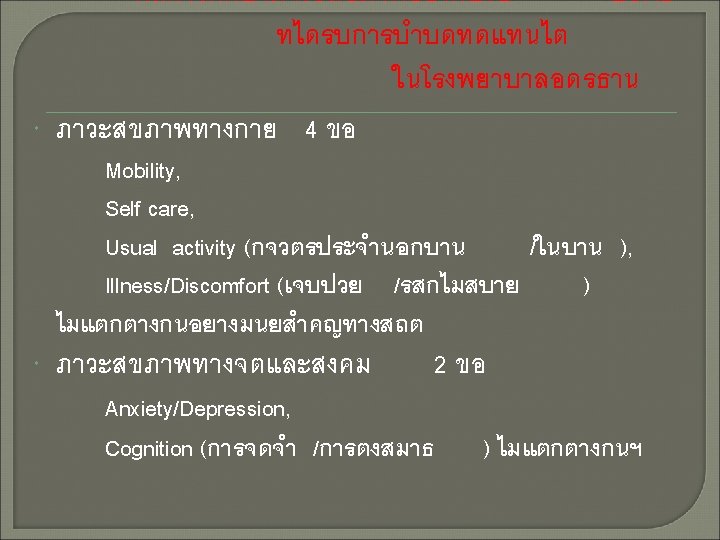
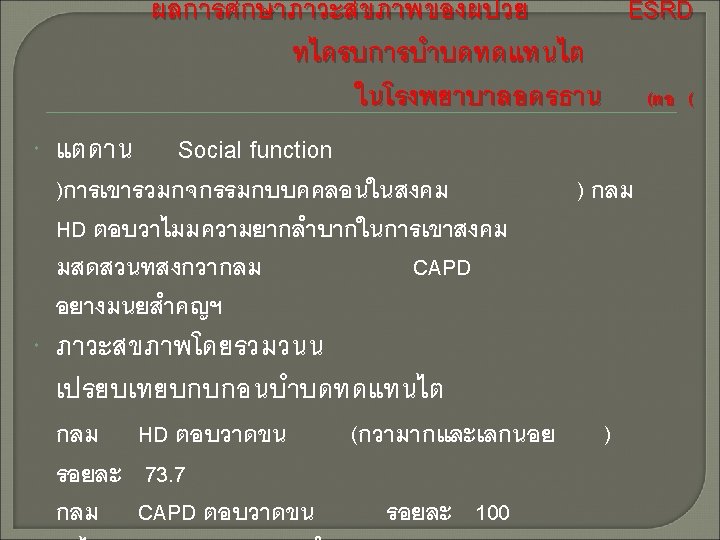
Definition of Chronic Kidney Disease 1. ����� >3 ����� , ( +/- GFR ) a. ������� b. ���������� Markers of kidney damage include - abnormal blood or urine composition - abnormal imaging tests 2. GFR <60 m. L/min/1. 73 m 2 >3 ����� , ( +/- kidney damage ) AJKD 2002; 39 (Suppl 1): S 17
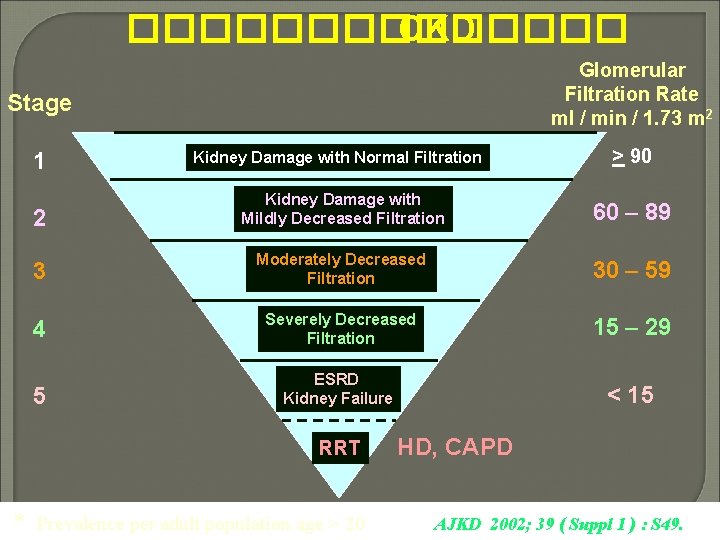
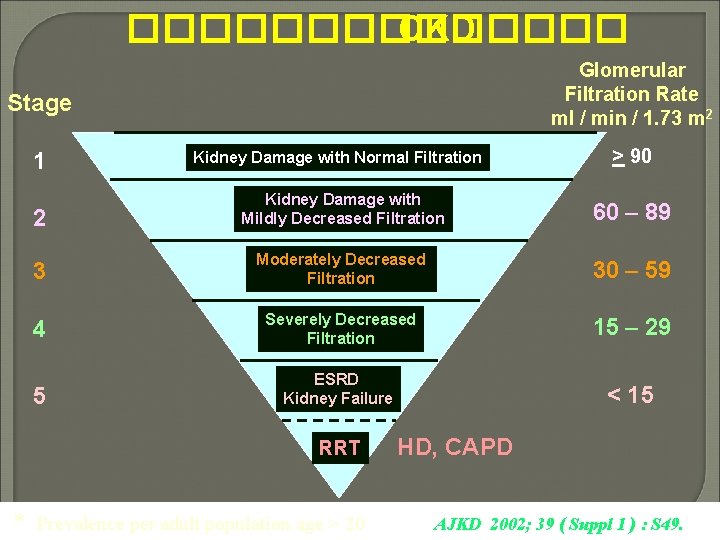
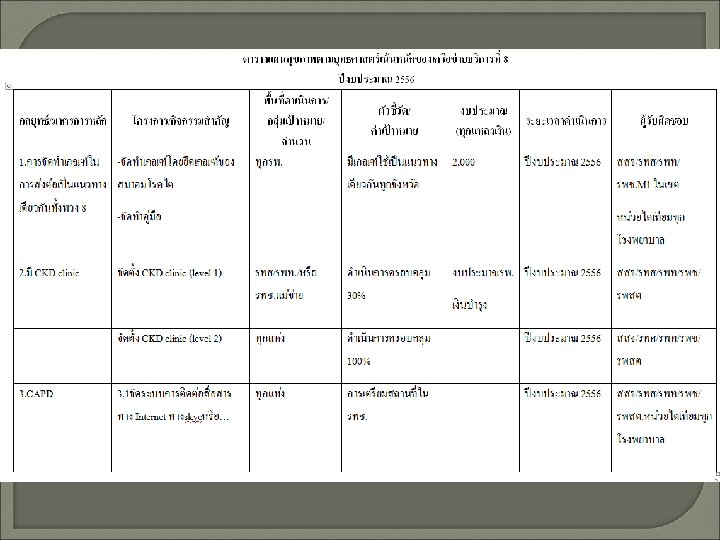
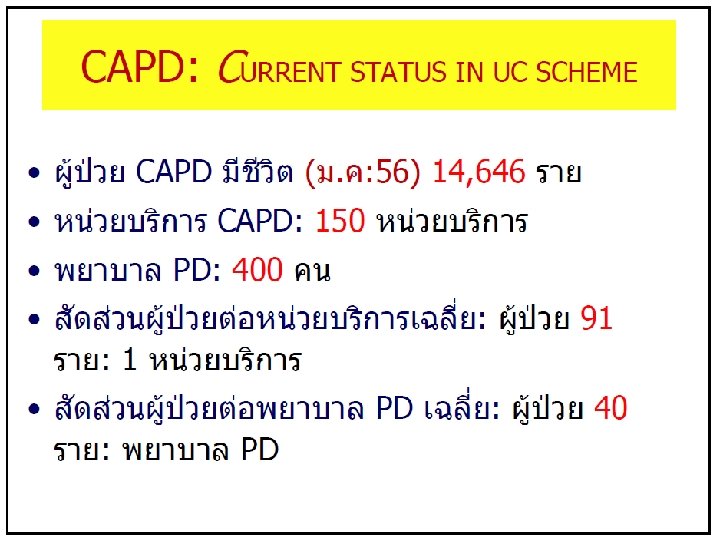
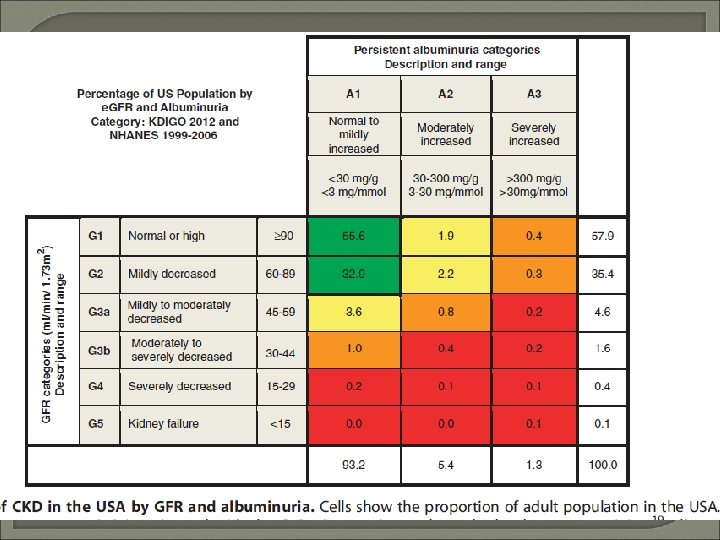
������� CKD Glomerular Filtration Rate ml / min / 1. 73 m 2 Stage 1 Kidney Damage with Normal Filtration > 90 2 Kidney Damage with Mildly Decreased Filtration 60 – 89 3 Moderately Decreased Filtration 30 – 59 4 Severely Decreased Filtration 15 – 29 5 ESRD Kidney Failure < 15 RRT * Prevalence per adult population age > 20 HD, CAPD AJKD 2002; 39 ( Suppl 1 ) : S 49.
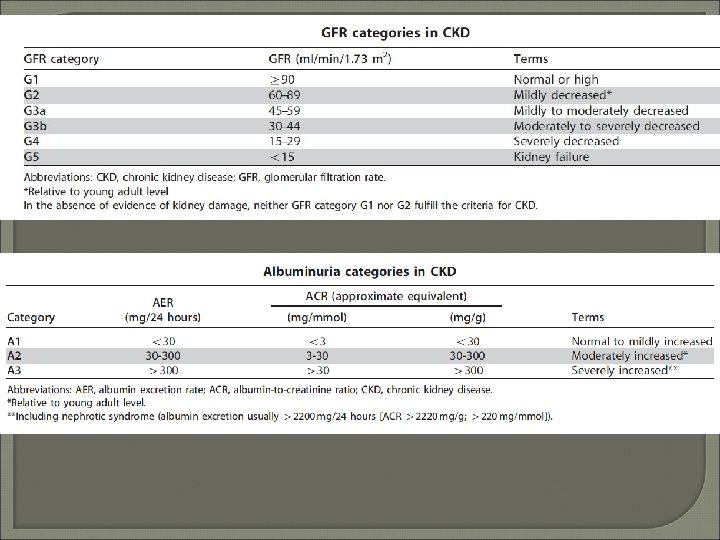
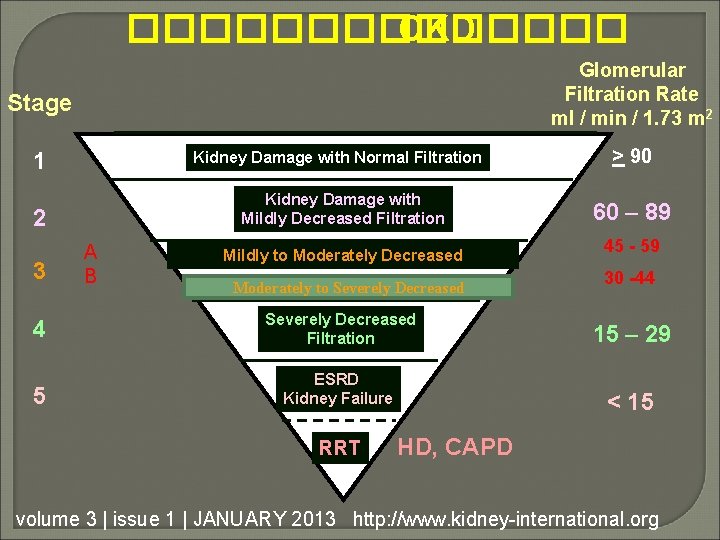
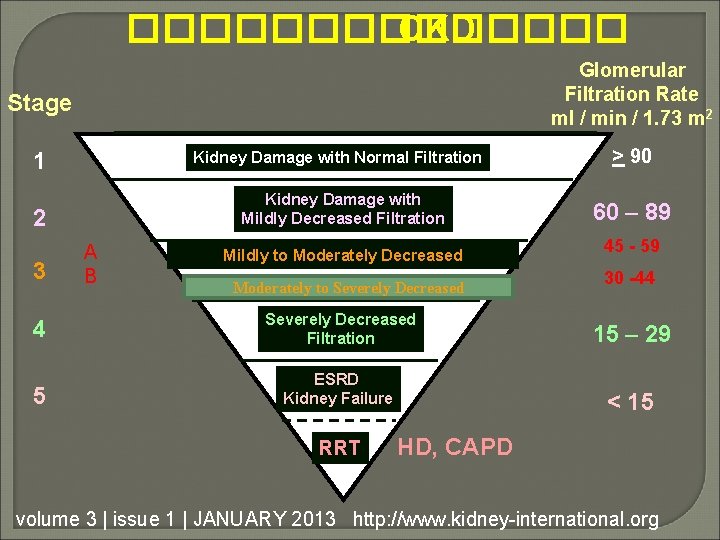
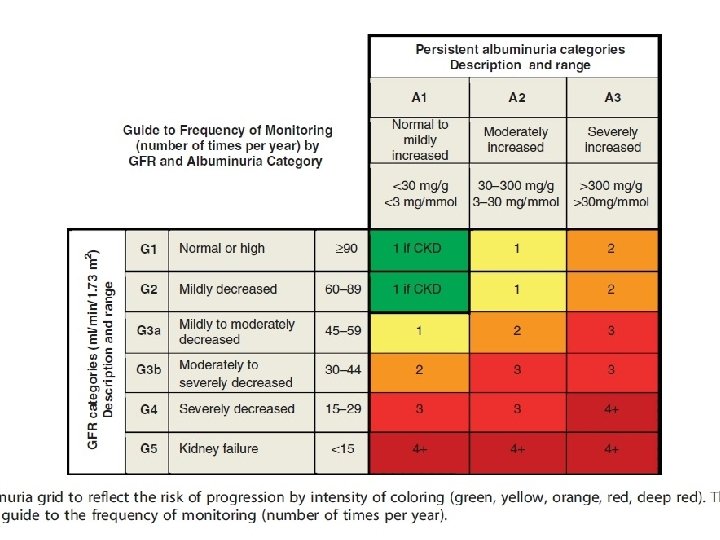
������� CKD Glomerular Filtration Rate ml / min / 1. 73 m 2 Stage 1 Kidney Damage with Normal Filtration Kidney Damage with Mildly Decreased Filtration 2 3 A B Mildly to Moderately Decreased Moderately to Severely Decreased > 90 60 – 89 45 - 59 30 -44 4 Severely Decreased Filtration 15 – 29 5 ESRD Kidney Failure < 15 RRT HD, CAPD volume 3 | issue 1 | JANUARY 2013 http: //www. kidney-international. org
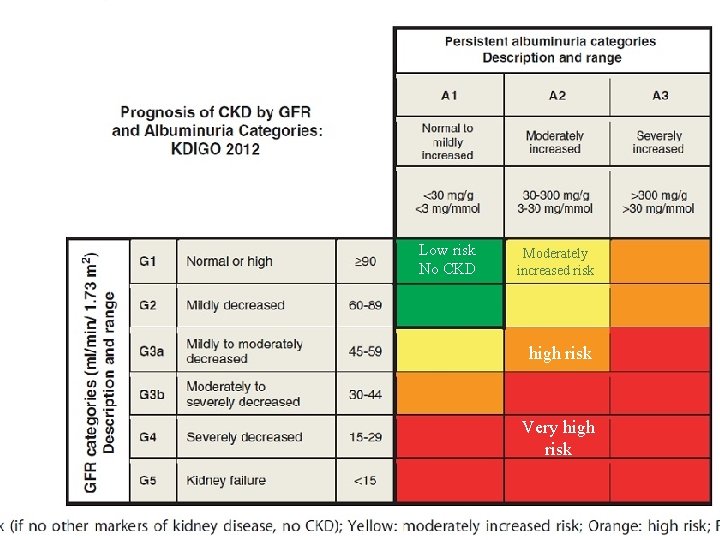
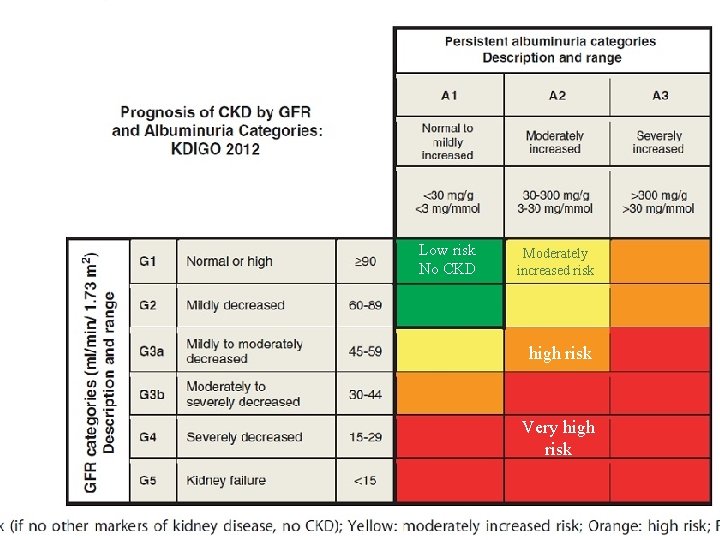
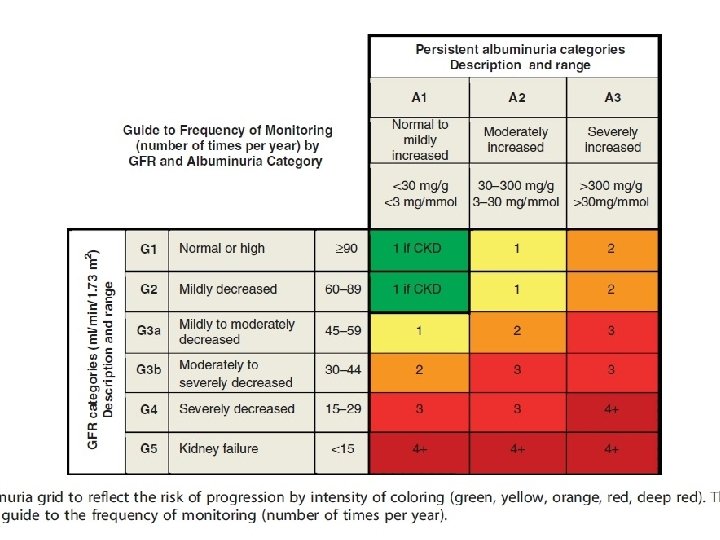
Low risk No CKD Moderately increased risk high risk Very high risk
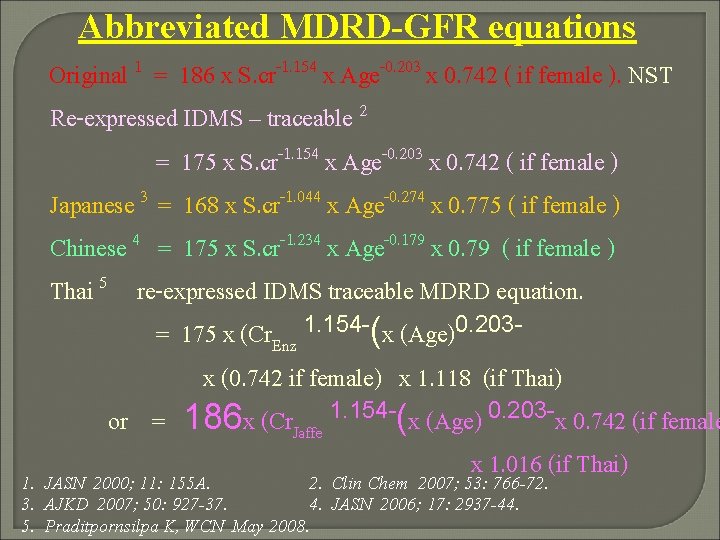
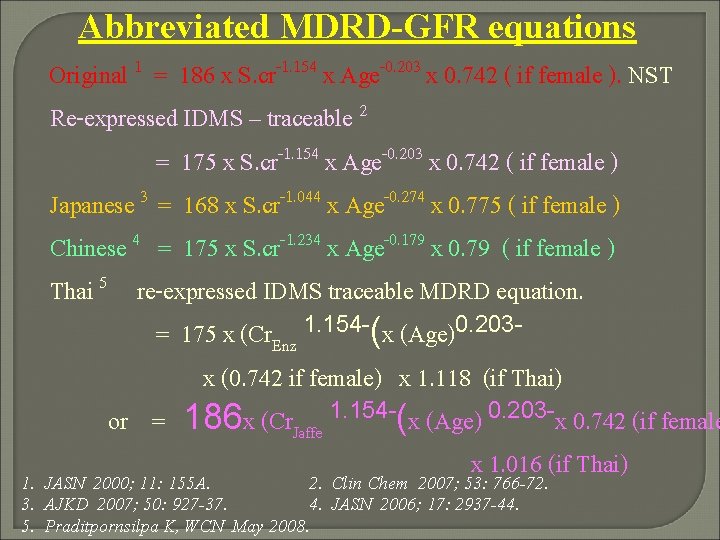
Abbreviated MDRD-GFR equations Original 1 = 186 x S. cr-1. 154 x Age-0. 203 x 0. 742 ( if female ). NST Re-expressed IDMS – traceable 2 = 175 x S. cr-1. 154 x Age-0. 203 x 0. 742 ( if female ) Japanese 3 = 168 x S. cr-1. 044 x Age-0. 274 x 0. 775 ( if female ) Chinese 4 = 175 x S. cr-1. 234 x Age-0. 179 x 0. 79 ( if female ) Thai 5 re-expressed IDMS traceable MDRD equation. = 175 x (Cr. Enz 1. 154 -(x (Age)0. 203 x (0. 742 if female) x 1. 118 (if Thai) or = 186 x (Cr. Jaffe 1. 154 -(x (Age) 0. 203 -x 0. 742 (if female x 1. 016 (if Thai) 1. JASN 2000; 11: 155 A. 2. Clin Chem 2007; 53: 766 -72. 3. AJKD 2007; 50: 927 -37. 4. JASN 2006; 17: 2937 -44. 5. Praditpornsilpa K, WCN May 2008.
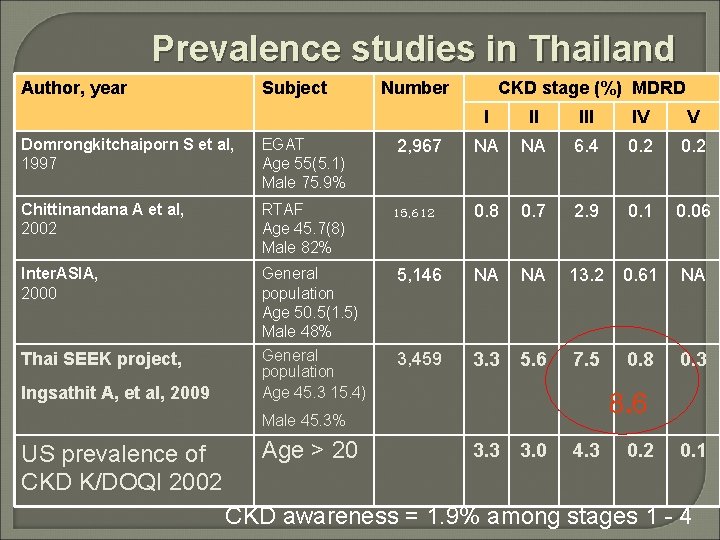
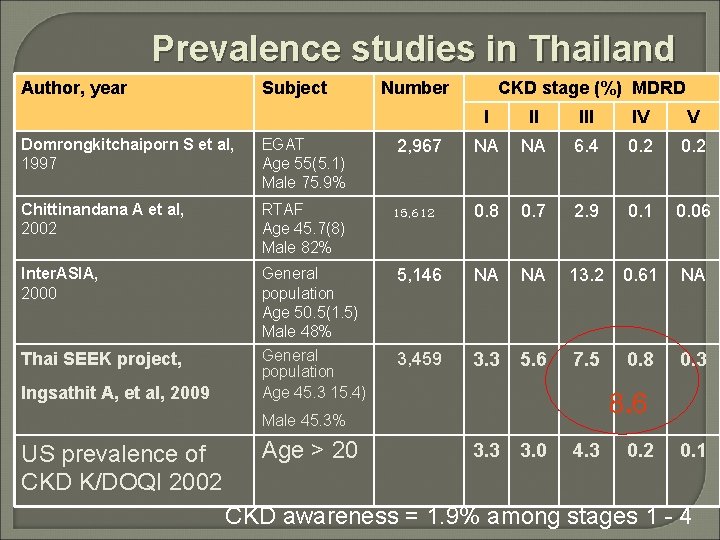
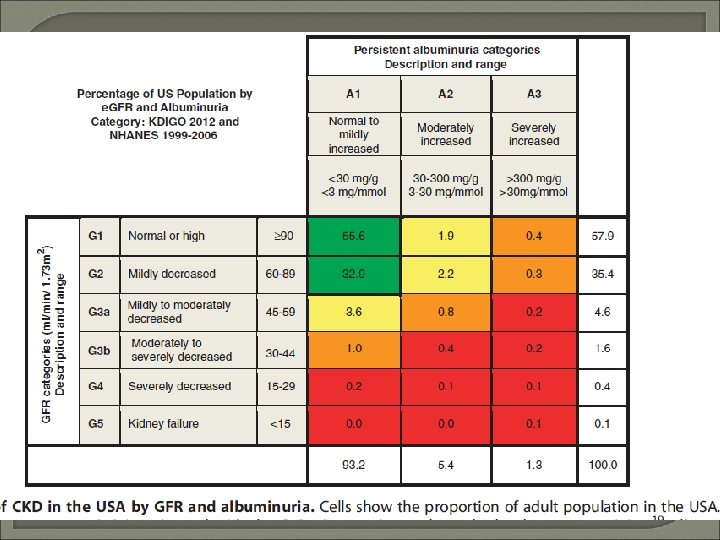
Prevalence studies in Thailand Author, year Subject Number CKD stage (%) MDRD I II IV V 2, 967 NA NA 6. 4 0. 2 15, 612 0. 8 0. 7 2. 9 0. 1 0. 06 Domrongkitchaiporn S et al, 1997 EGAT Age 55(5. 1) Male 75. 9% Chittinandana A et al, 2002 RTAF Age 45. 7(8) Male 82% Inter. ASIA, 2000 General population Age 50. 5(1. 5) Male 48% 5, 146 NA NA 13. 2 0. 61 NA Thai SEEK project, General population Age 45. 3 15. 4) 3, 459 3. 3 5. 6 7. 5 0. 8 0. 3 Ingsathit A, et al, 2009 8. 6 Male 45. 3% US prevalence of CKD K/DOQI 2002 Age > 20 3. 3 3. 0 4. 3 0. 2 0. 1 CKD awareness = 1. 9% among stages 1 - 4
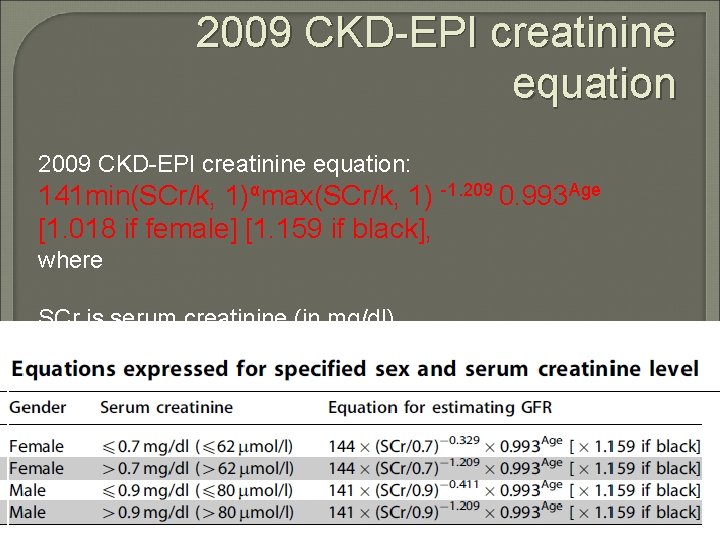
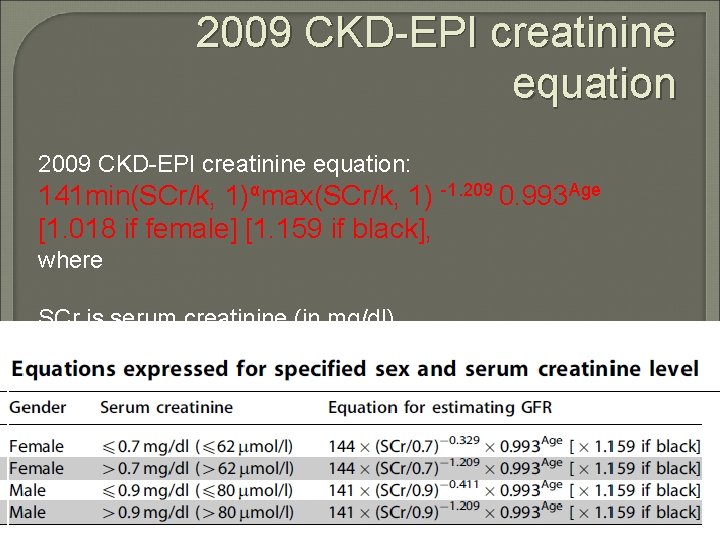
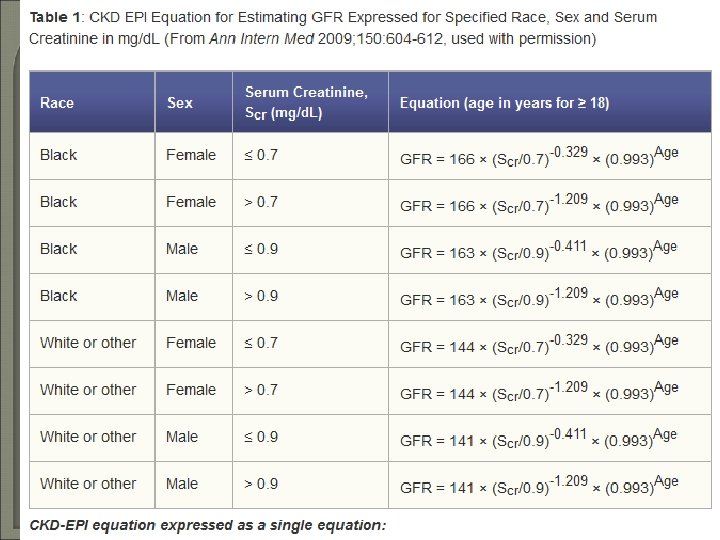
2009 CKD-EPI creatinine equation: 141 min(SCr/k, 1)αmax(SCr/k, 1) -1. 209 0. 993 Age [1. 018 if female] [1. 159 if black], where SCr is serum creatinine (in mg/dl), k is 0. 7 for females and 0. 9 for males, α is 0. 329 for females and 0. 411 for males, min is the minimum of SCr/k or 1, and max is the maximum of SCr/k or 1.
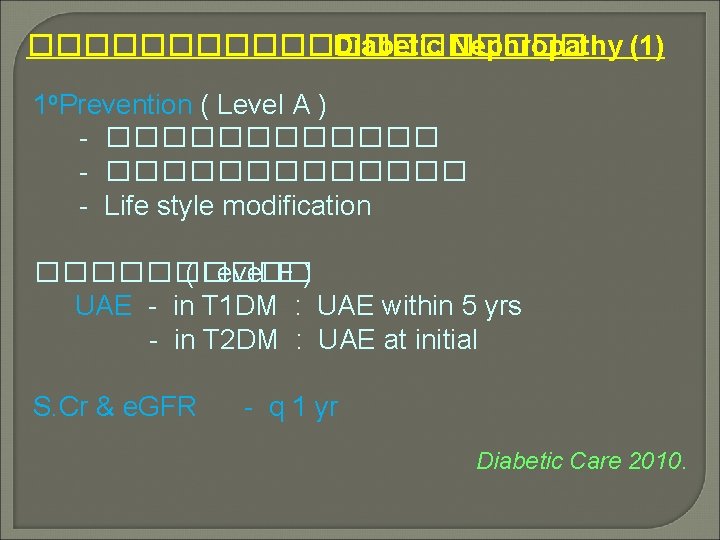
���������� Diabetic Nephropathy (1) 1 o. Prevention ( Level A ) - ������������� - Life style modification ����� ( Level E ) UAE - in T 1 DM : UAE within 5 yrs - in T 2 DM : UAE at initial S. Cr & e. GFR - q 1 yr Diabetic Care 2010.
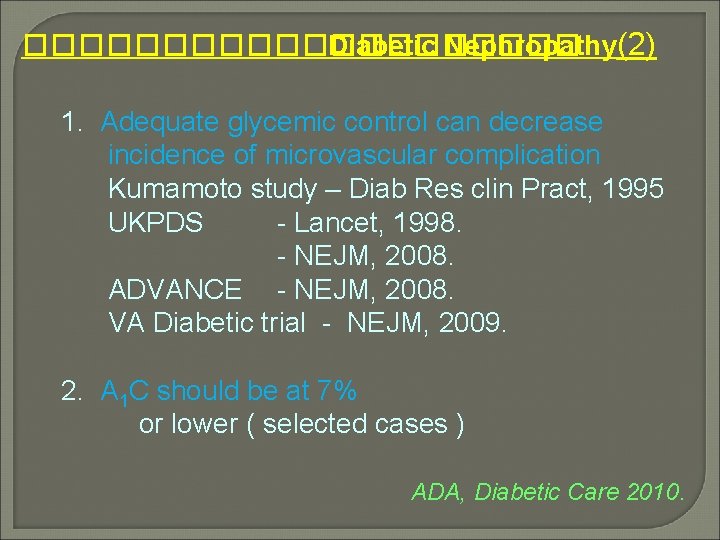
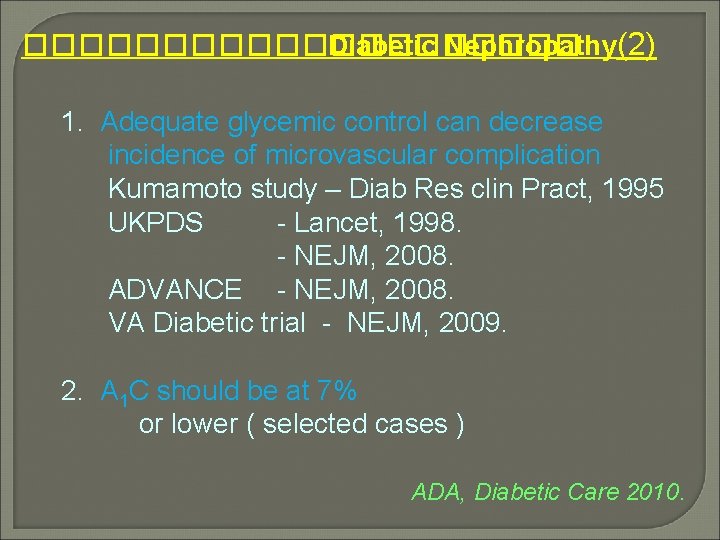
���������� Diabetic Nephropathy(2) 1. Adequate glycemic control can decrease incidence of microvascular complication Kumamoto study – Diab Res clin Pract, 1995 UKPDS - Lancet, 1998. - NEJM, 2008. ADVANCE - NEJM, 2008. VA Diabetic trial - NEJM, 2009. 2. A 1 C should be at 7% or lower ( selected cases ) ADA, Diabetic Care 2010.
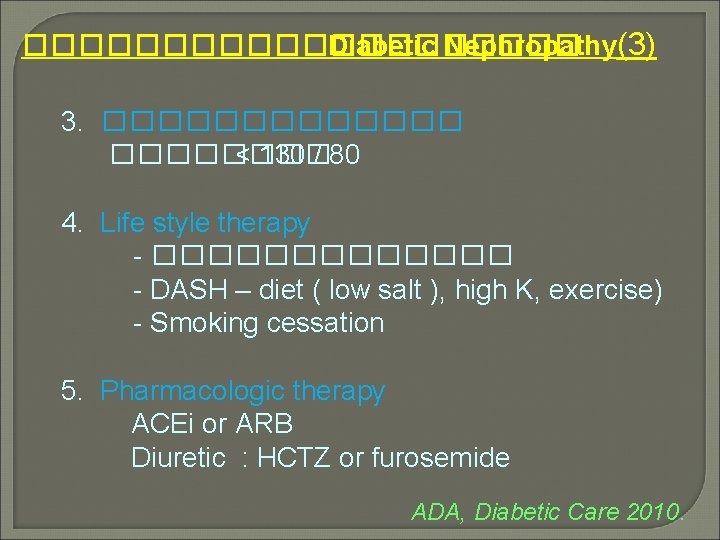
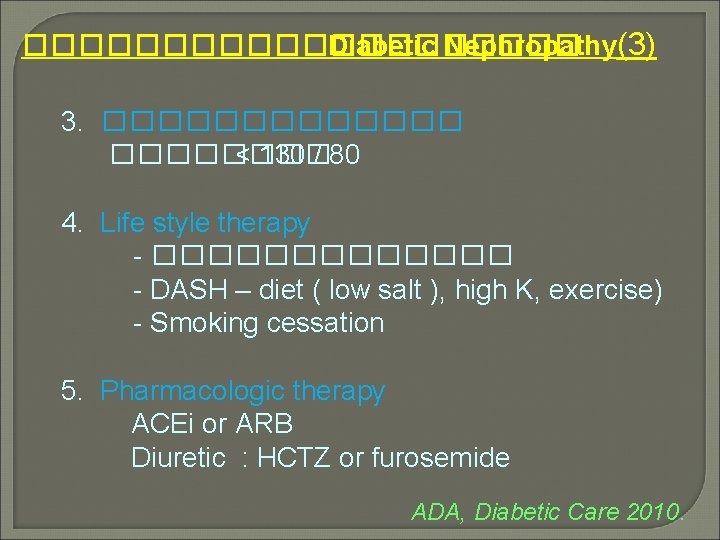
���������� Diabetic Nephropathy(3) 3. ������� < 130 / 80 4. Life style therapy - ������� - DASH – diet ( low salt ), high K, exercise) - Smoking cessation 5. Pharmacologic therapy ACEi or ARB Diuretic : HCTZ or furosemide ADA, Diabetic Care 2010.
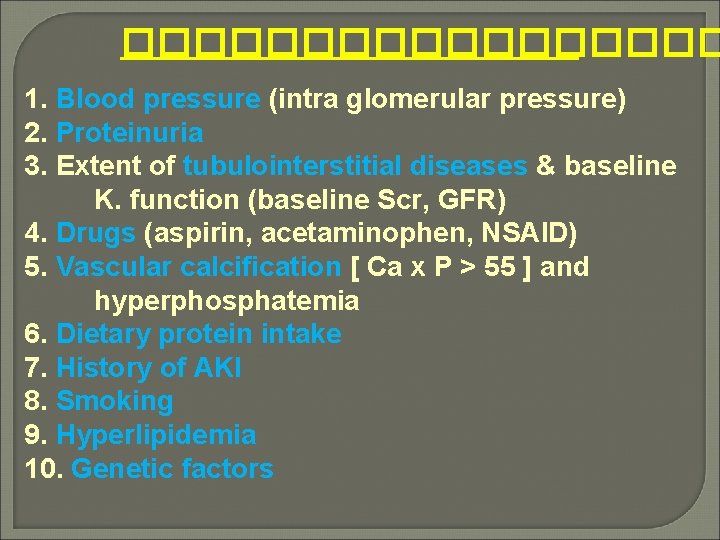
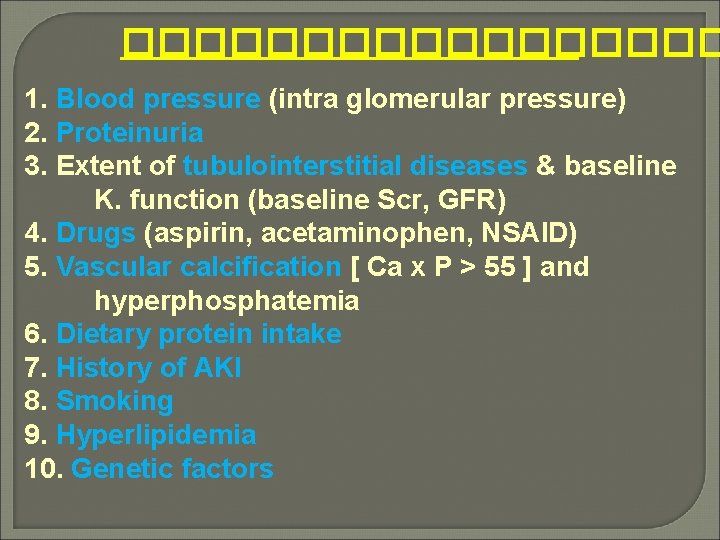
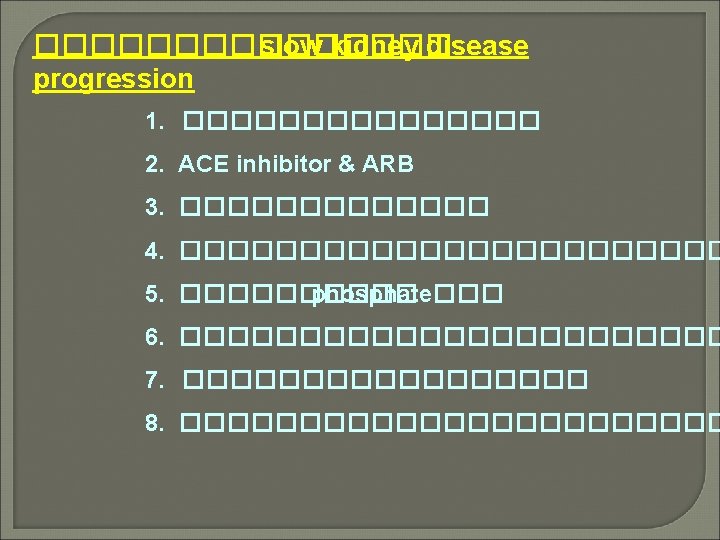
��������� 1. Blood pressure (intra glomerular pressure) 2. Proteinuria 3. Extent of tubulointerstitial diseases & baseline K. function (baseline Scr, GFR) 4. Drugs (aspirin, acetaminophen, NSAID) 5. Vascular calcification [ Ca x P > 55 ] and hyperphosphatemia 6. Dietary protein intake 7. History of AKI 8. Smoking 9. Hyperlipidemia 10. Genetic factors
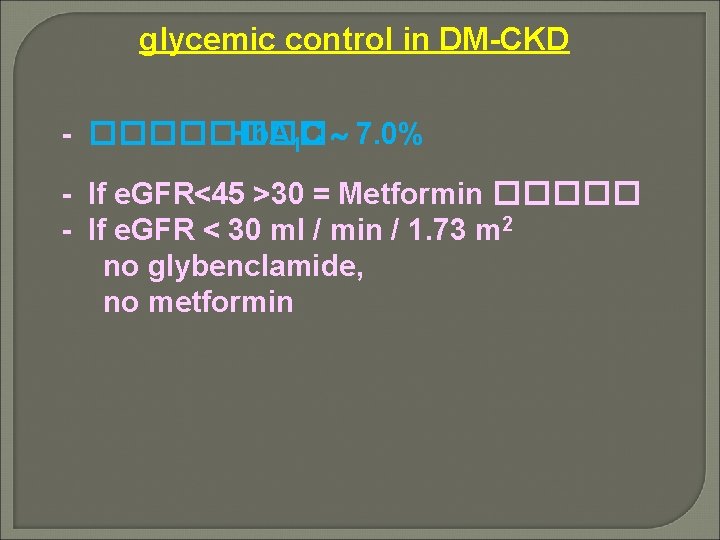
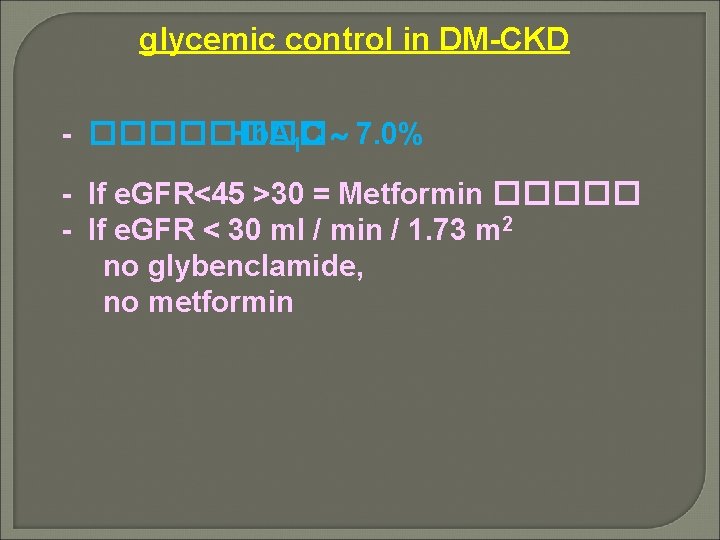
glycemic control in DM-CKD - ���� Hb. A 1 C 7. 0% - If e. GFR<45 >30 = Metformin ����� - If e. GFR < 30 ml / min / 1. 73 m 2 no glybenclamide, no metformin
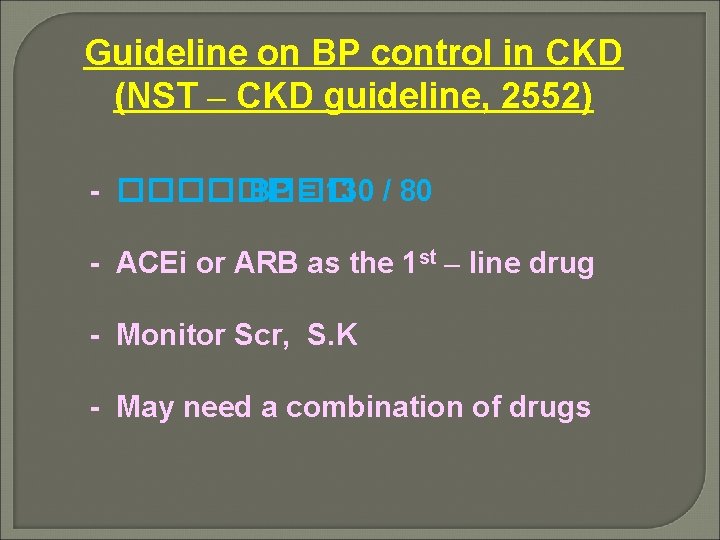
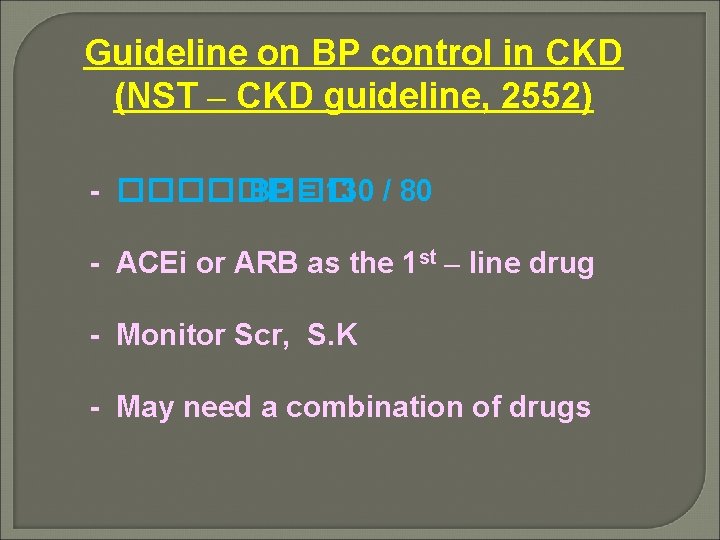
Guideline on BP control in CKD (NST – CKD guideline, 2552) - ���� BP = 130 / 80 - ACEi or ARB as the 1 st – line drug - Monitor Scr, S. K - May need a combination of drugs
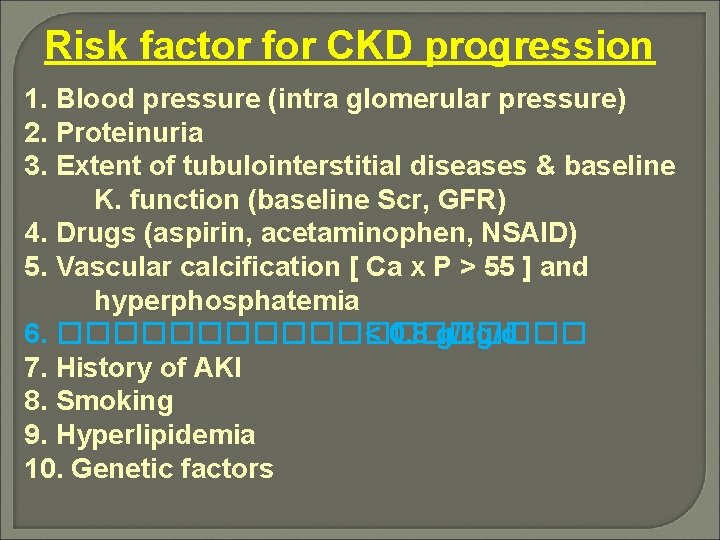
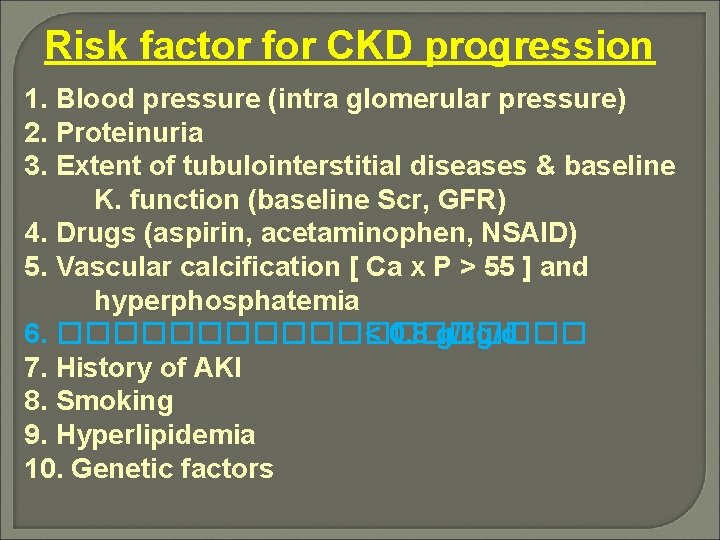
Risk factor for CKD progression 1. Blood pressure (intra glomerular pressure) 2. Proteinuria 3. Extent of tubulointerstitial diseases & baseline K. function (baseline Scr, GFR) 4. Drugs (aspirin, acetaminophen, NSAID) 5. Vascular calcification [ Ca x P > 55 ] and hyperphosphatemia 6. ���������� < 0. 8 g/kg/d 7. History of AKI 8. Smoking 9. Hyperlipidemia 10. Genetic factors
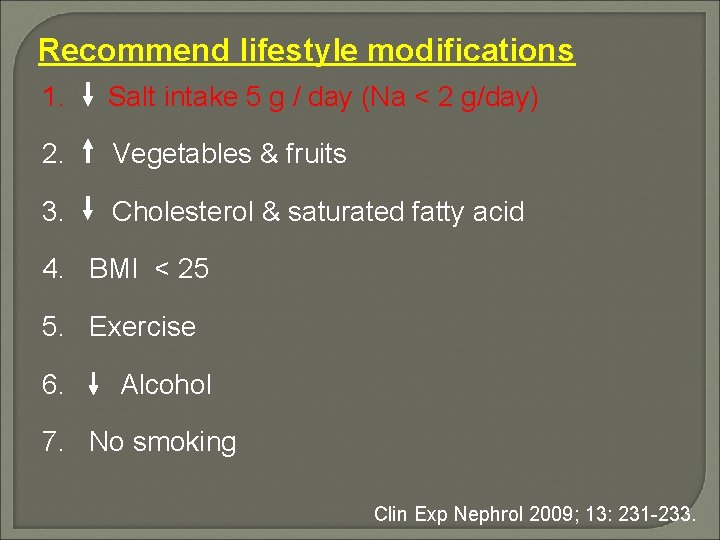
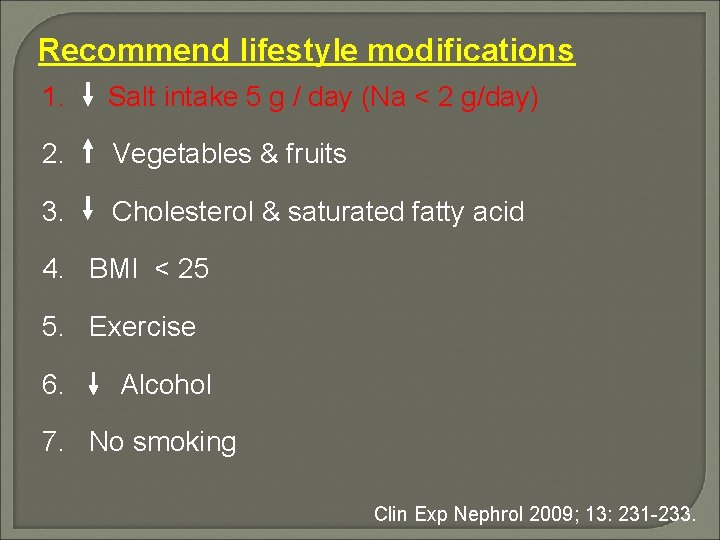
Recommend lifestyle modifications 1. Salt intake 5 g / day (Na < 2 g/day) 2. Vegetables & fruits 3. Cholesterol & saturated fatty acid 4. BMI < 25 5. Exercise 6. Alcohol 7. No smoking Clin Exp Nephrol 2009; 13: 231 -233.
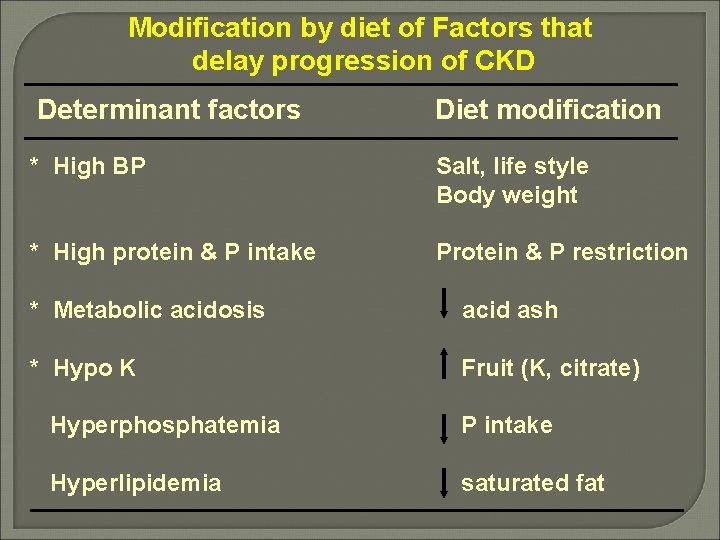
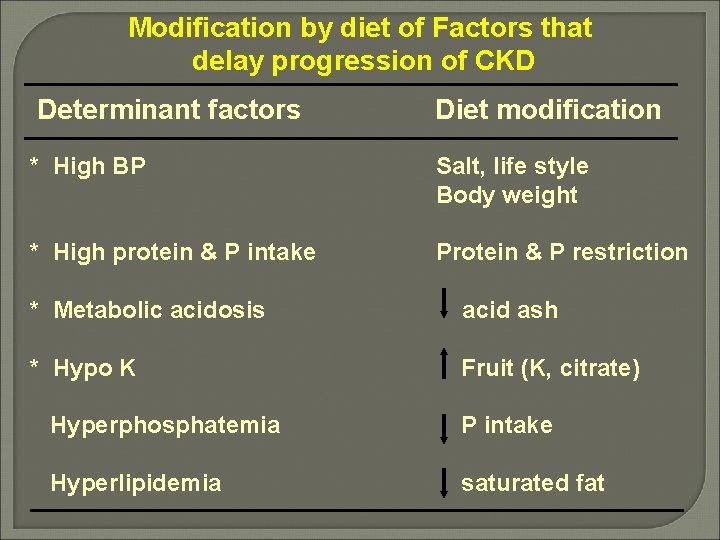
Modification by diet of Factors that delay progression of CKD Determinant factors Diet modification * High BP Salt, life style Body weight * High protein & P intake Protein & P restriction * Metabolic acidosis acid ash * Hypo K Fruit (K, citrate) Hyperphosphatemia P intake Hyperlipidemia saturated fat
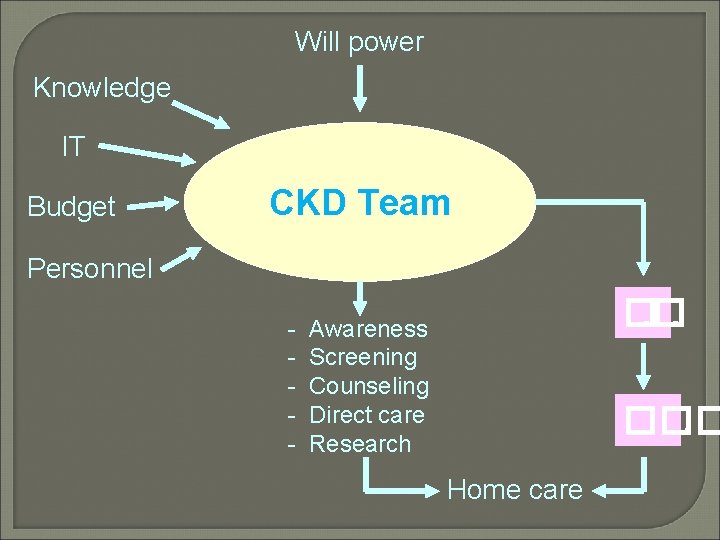
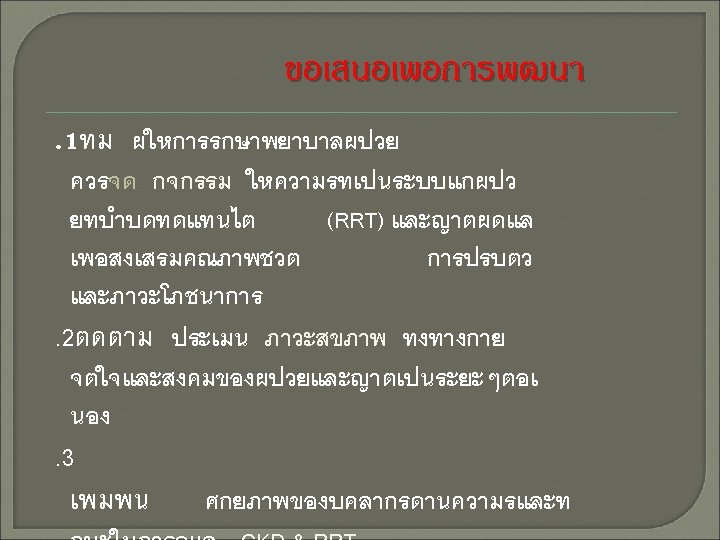
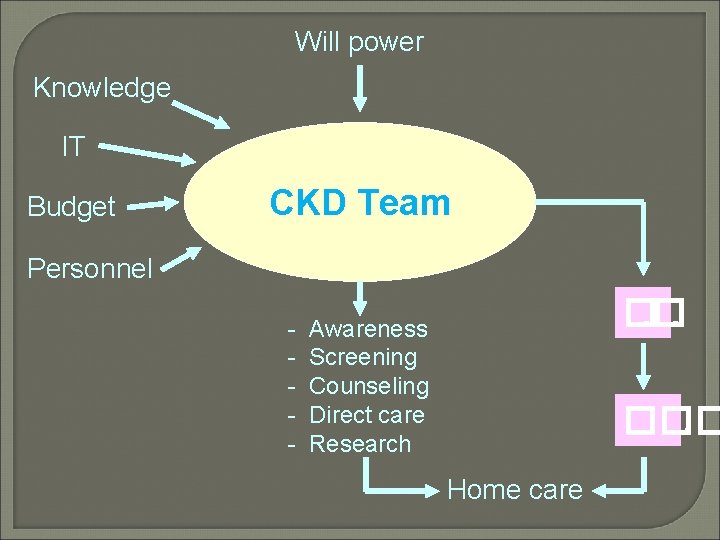
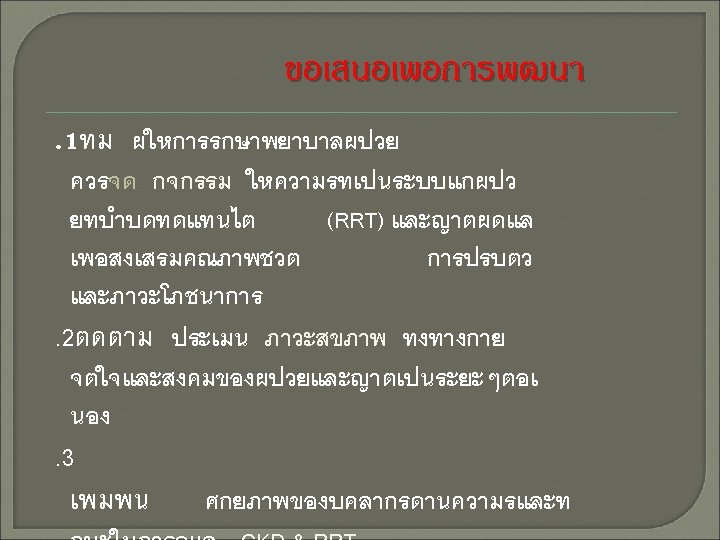
Will power Knowledge IT Budget CKD Team Personnel - �. �. Awareness Screening Counseling Direct care Research ���. Home care
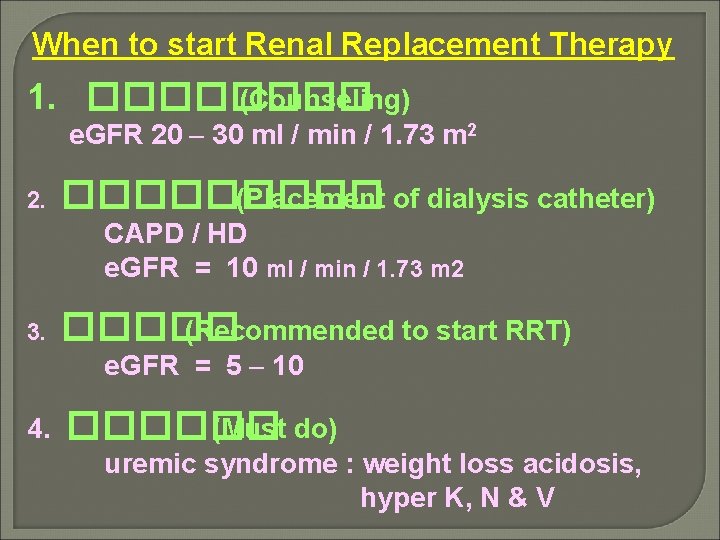
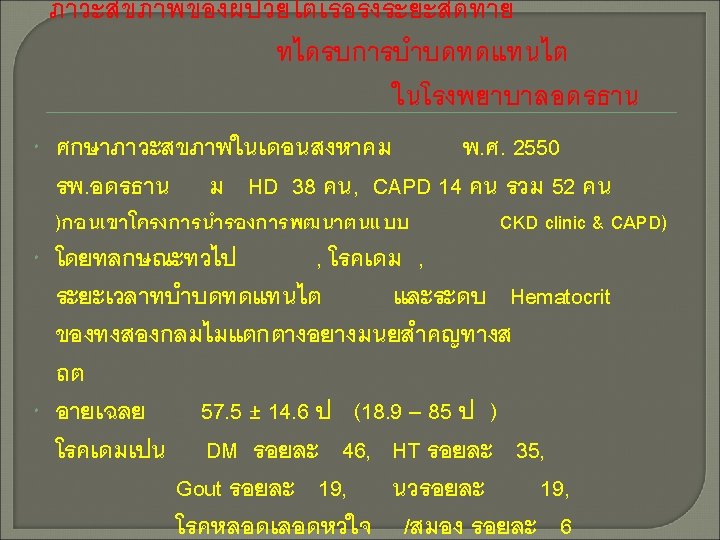
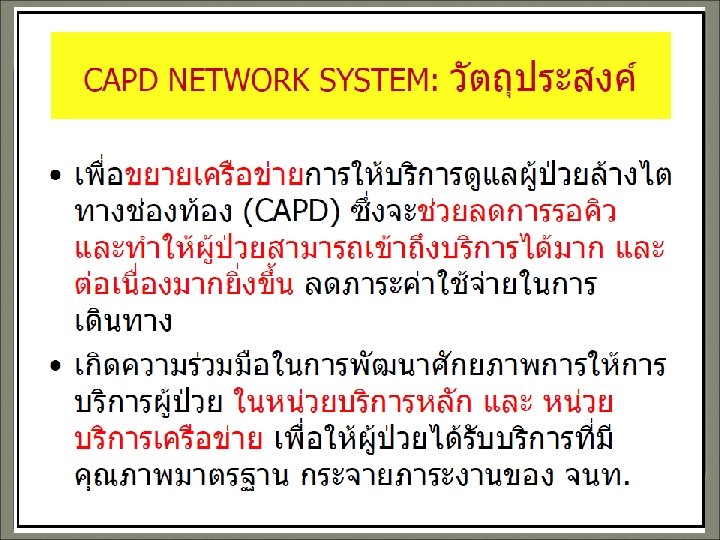
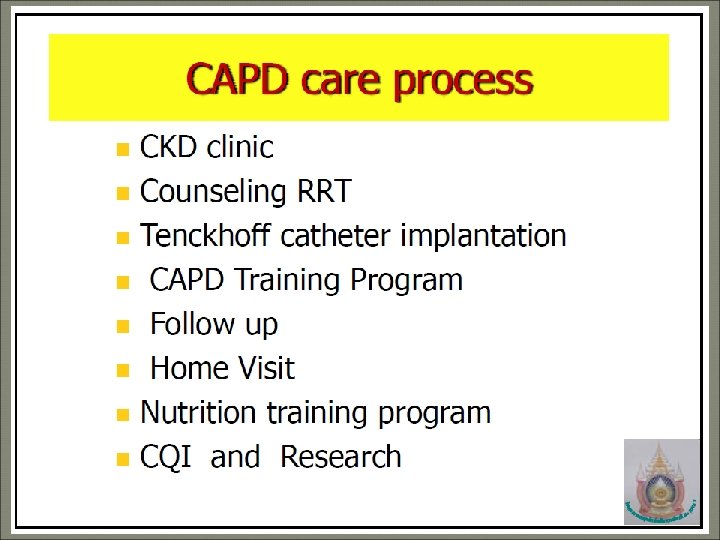
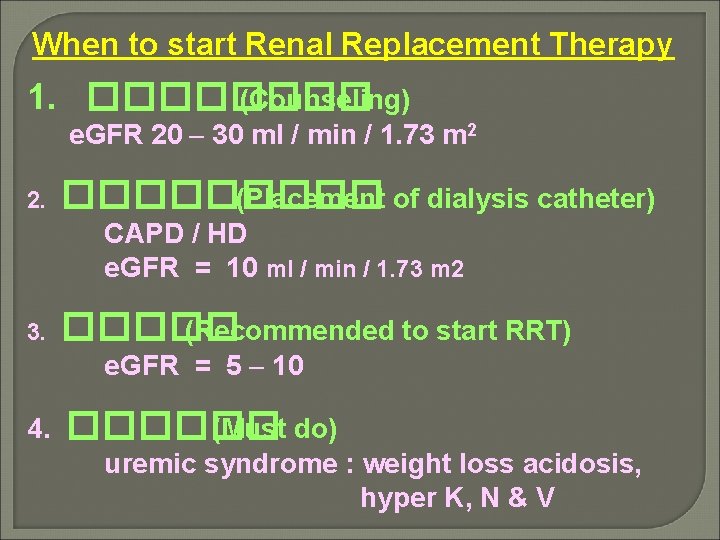
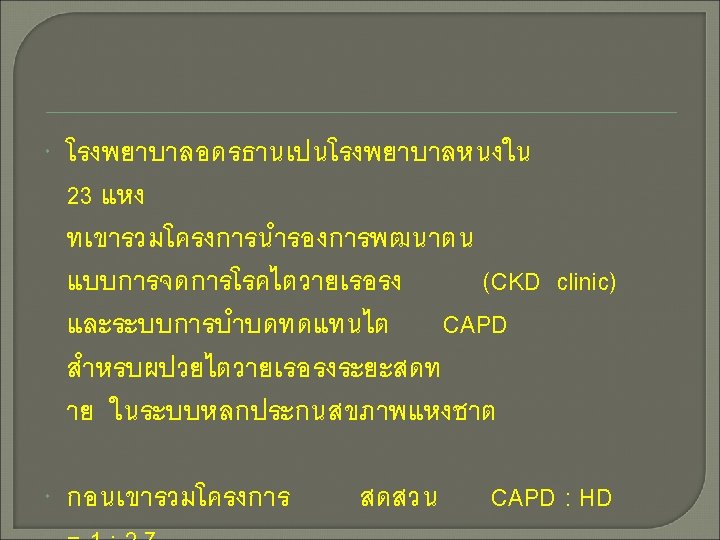
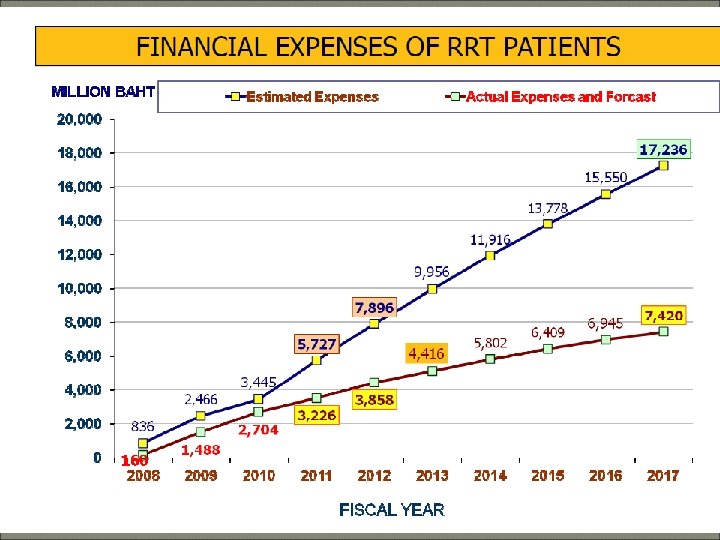
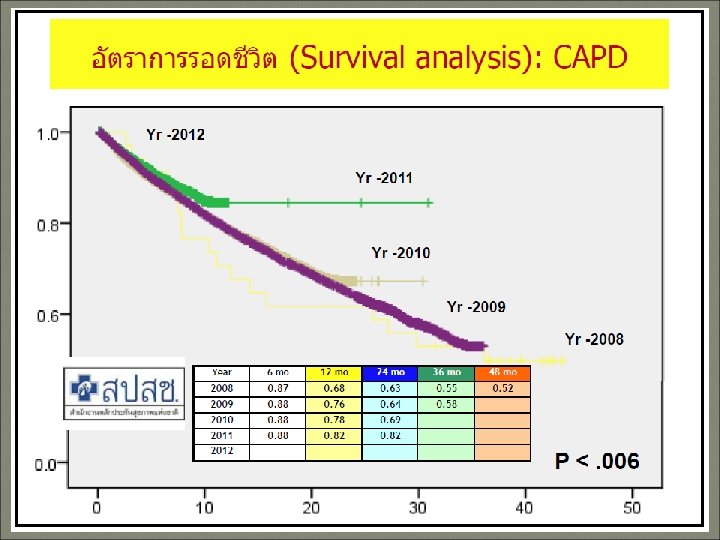
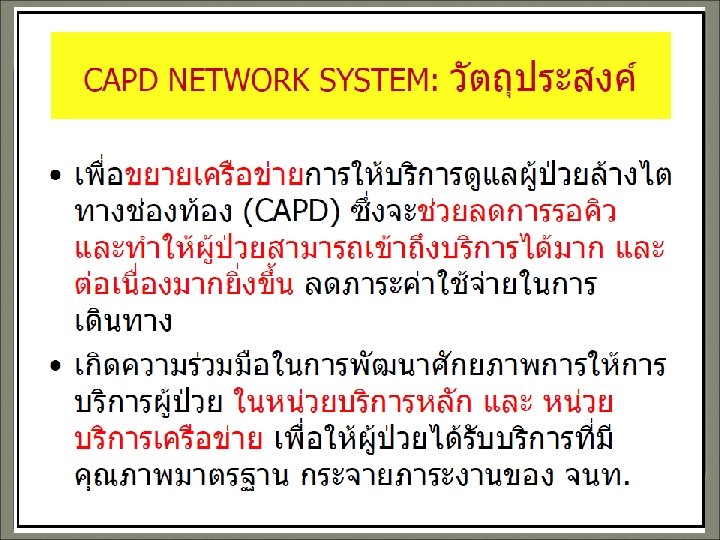
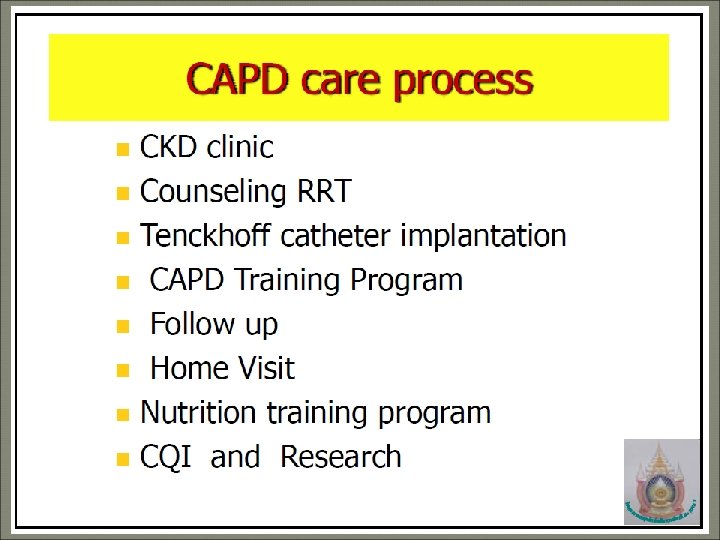
When to start Renal Replacement Therapy 1. ���� (Counseling) e. GFR 20 – 30 ml / min / 1. 73 m 2 2. ����� (Placement of dialysis catheter) CAPD / HD e. GFR = 10 ml / min / 1. 73 m 2 3. ����� (Recommended to start RRT) e. GFR = 5 – 10 4. ������ (Must do) uremic syndrome : weight loss acidosis, hyper K, N & V