Definition and Incidence Epilepsy is recurring spontaneous seizures


- Slides: 40
Definition and Incidence Epilepsy is recurring spontaneous seizures due to sudden excessive and disordered electrical discharge from the neurones of the Cerebral cortex. It is estimated that 7% of epileptic women become pregnant and epilepsy affects about 0. 5 -1% of pregnant women. Epilepsy can be partial or generalized.
Classification Of Epilepsy A- Partial Seizures (Focal Seizures): This is the commonest type and is subcategorized as 1 -Simple Partial Seizures (Jacksonian epilepsy): The affected woman does not lose consciousness but may experience confusion, tingling, or odd mental and emotional events. Such events may include déjà vu phenomenon, mild hallucinations, or extreme responses to smell and taste. After the seizure, the patient usually has temporary weakness in certain muscles.
2 - Complex Partial Seizures (>50% in adults): They can result in loss of judgment, involuntary uncontrolled behavior & loss of consciousness. Prior to the actual seizure, some people may experience a warning aura, which can be an odd odor, a feeling of warmth, or a visual or auditory hallucination. They then may lose consciousness briefly and appear to others as motionless with a vacant stare. After a few seconds, some may begin to perform repetitive movements, such as chewing or smacking of lips. Episodes usually last no more than two minutes. Ocassionally a simple or complex partial seizures evolve into secondarily generalized seizures. The progress may be so rapid that the partial stage is not even noticed.
BGeneralized Seizures They occur in more diffuse areas of the brain and they have more serious effect on the patient. They are further subcategorized as follows: 1 -Tonic-Clonic (Grand Mal) Seizures: a-The tonic phase: muscles suddenly contract, causing the patient to fall and lie rigidly for about 10 to 30 seconds. Some people experience aura; most, lose consciousness without warning. If the throat or larynx is affected, stridor occurs when the patient inhales. b-The clonic phase: Seizure is said to enter this phase when the muscles begin to alternate between relaxation and rigidity. After this phase, the patient may lose bowel or urinary control. The seizure usually lasts a total of two to three minutes, after which the patient remains unconscious for a while and then awakens to confusion and extreme fatigue.
2 - Absence (Petit Mal) Seizures: Petit mal or absence seizures are brief (three to 30 seconds) losses of consciousness and may consist of only a short cessation of physical movement and loss of attention. Such seizures may pass unnoticed by others. About 25% of patients with petit mal develop grand mal seizures
COther Seizures: 1 - Atonic (Akinetic) Seizures. A person who has an atonic (or akinetic) seizure loses muscle tone. Sometimes it may affect only one part of the body so that, for instance, the jaw slackens and the head drops. At other times, the whole body may lose muscle tone, and the person can suddenly fall. 2 - Simply Tonic or Clonic Seizures can also be simply tonic or clonic. In tonic seizures, the muscles contract and consciousness is altered for about 10 seconds, but the seizures do not progress to the clonic phase. Clonic seizures, which are very rare, occur primarily in young children, who experience spasms of the muscles but not their tonic rigidity. 3 - Myoclonic seizures are a series of brief jerky contractions of specific muscle groups, such as the face or trunk.
4 -Gestational epilepsy: Some patients experience their first seizures during pregnancy. This can be a result of true gestational epilepsy, a rare syndrome of seizures occurring only during pregnancy. Patients with this syndrome have a variable presentation with single or multiple seizures in one or more of their pregnancies. It can also be a manifestation of epilepsy that may extend beyond the pregnancy. The workup of these patients should involve a neurologic examination, consultation with a neurologist, CBC count, chemistry panel (particularly for electrolytes), head MRI versus CT scan, and EEG. The differential diagnosis should include eclampsia and any possible etiology considered in the nonpregnant patient, including stroke, electrolyte abnormalities, tumor, trauma, drugs/withdrawal, and epilepsy
Effects Of Pregnancy On Epilepsy Unpredictable 1 -Seizure frequency may increase: due to: Enhanced metabolism & increased drug clearance associated with pregnancy can result in decreased serum drug concentration. Increased volume of distribution of the AED. Increased serum binding proteins. Decreased or non-compliance with medication. Sleep deprivation, hormonal changes of pregnancy and associated psychological and emotional stress of pregnancy all lower the threshold for seizures. Nausea and vomiting.
2 -Seizure frequency may decrease: Due to improved compliance with drug regimen in some patients. 3 -Seizure frequency unchanged. may remain
Effect Of Epilepsy On Pregnancy v 1 st trimester losses, PROM, ante-partum hemorrhage, operative vaginal delivery and CS are inconclusive. Increased incidence of IUGR, cognitive dysfunction, microcephaly and perinatal mortality (1. 2 - 3 times normal) v Increased congenital malformations. v
Effect Of Epilepsy On Lactation u Breast feeding should be stopped if obvious sedation develops in an infant and is likely to relate to the presence of AED in breast milk.
Effects Of Epilepsy On Fetus And Neonate 1 -There is increased risk for infants of epileptic mothers to have epilepsy. The risk of neonatal susceptibility depends on: u u Nature of the mother’s seizure disorder. Genetic factors. Seizures arises during pregnancy. Metabolic & toxic consequences of seizures and AEDs. 2 -Increase perinatal morbidity.

Management I-Preconceptional Care: A-Re-assessment: may show that the patient does not have epilepsy or may reveal a treatable cause before pregnancy (e. g. blood vessel abnormality in the brain). B-Counseling: explain to the patient that: u There is a chance of 90% of having normal child. u Increased chance of having epileptic child (2 -5%). u Increased pregnancy complications. u Increased unfortunate outcome if seizures arises during pregnancy. u Increased risk of congenital malformations.
C-Measurement of the free unbound anti-epileptic drug level in maternal serum. D- Preconceptional folate supplementation: 5 mg daily. E- No trial to stop AED unless the patient is seizure free at least for 2 years. The AED dose should be tapered till stopped completely at least 6 months prior to any planned pregnancy to provide some reassurance that seizures are not going to recur.
II-Antenatal Care A-Investigations: u Metabolic: serum glucose, urea, electrolytes, Ca & Mg u EEK u MRI/CT scan of the head. B-Drugs: Monotherapy at the lowest effective dose should be employed. If large daily doses are needed, use frequent smaller doses or extended-release formula to avoid high peak levels. Monitoring of serum AEDs level is mandatory. Usually, women don't suspect they are pregnant until their fourth to sixth week of pregnancy. By that time, if there any harmful effects from their AEDs, most of these effects would have already occurred.
C-Selenium supplementation: in a dose of 200 µ/day may be important to minimize the free radical mediated damage. D-Folic acid supplements. E-Morning sickness: If hyperemesis gravidarum, consider giving alternative route if vomiting is severe or prolonged. F-Antenatal diagnosis: of congenital malformations (screening should be done by detailed ultrasound and measurement of æ fetoprotein at 18 weeks).
G-Vitamin K: Oral 20 mg daily is prescribed from 36 weeks until delivery to mothers taking hepatic enzyme-inducing drugs (phenytoin, phenobarbitone, primidone, carbamazepine and topiramate - Not necessary with sodium valproate). are using whether it is a hepatic enzyme inducing or not. Most of the newer AEDs are not enzyme inducers).
III-Labor and Delivery “The risk of developing a seizure during labor is 9 times that during the rest of pregnancy”. Management of women with epilepsy upon labor and delivery: u u u Check levels of AEDs. Inform all health care providers that the patient has epilepsy. Consider seizure prophylaxis with intravenous benzodiazepines or phenytoin.
u u u Manage seizures acutely with intravenous benzodiazepines (1 -2 mg of diazepam), then load phenytoin (1 g loaded over 1 h). Labor management should be based on routine standards of care. Start administration of vitamin K for the infant, and send the cord blood for clotting studies.
Management of a pregnant patient in status epilepticus: u Establish the ABCs, and check vital signs. u Assess the fetal heart rate. u Rule out eclampsia. u Administer a bolus of lorazepam (0. 1 mg/kg, ie, 5 -10 mg) at no faster than 2 mg/min.
u u Load phenytoin (20 mg/kg, ie, 1 -2 g) at no faster than 50 mg/min, with cardiac monitoring. If this is not successful, load phenobarbital (20 mg/kg, ie, 1 -2 g) at no faster than 100 mg/min. Check laboratory findings, including electrolytes, AED levels, glucose, and toxicology screen. If fetal testing results are nonreassuring, move to emergent delivery.
u u The majority of women who have epilepsy have a safe vaginal delivery without seizure occurrence; provided, the AED is taken before and throughout labor. Generalized tonic clonic seizures needs aggressive interference because of the high risk for the mother and fetus, especially if they progress to status epilepticus. Oxygen should be administered to the patient and she should be placed on her left side to increase uterine blood flow and decrease the risk for maternal aspiration.
u u u Emergency C. S. should be performed when repeated GTCSs cannot be controlled during labor or when the mother is unable to cooperate. Any lady having a seizure during labour must be observed closely for the next 72 hours. Obstetric analgesia may be used to allow for rest before delivery. Pethidine should never be used because it is metabolised to norpethidine, which is epileptogenic. Diamorphine is an option. Few cases of postpartum seizures were reported following epidural analgesia.
u u During labor, oral absorption of AEDs may be inappropriate and any vomiting might complicate the situation. PB, PHT, and VPA can be given IV at the same maintenance dosage. Convulsive seizures and repeated seizures during labor should be treated promptly with parenteral lorazepam or diazepam. Benzodiazepines, in large doses, can cause neonatal cardiac and respiratory depression; therefore, close monitoring for these neonates is mandatory.
IV-Postnatal Care A-Infant: - Inspected for malformation. -Vitamin k 0. 1 mg/kg IM at birth reduces risks of hemorrhagic disease. B-Bathing: never should be performed alone, as a brief lapse in attention can result in a fatal drowning. Wet sponge not water bath. Changing diapers and clothes are performed best on the floor rather than on an elevated changing table. C-Breast Feeding: encouraged in suitable position. If excessive infant sedation is encountered, as may be seen with phenobarbital or primidone, the infant should be weaned slowly with monitoring for signs and symptoms of withdrawal and infant drug levels.
D- The following safety issues must be taken into account: u u If the mother is likely to drop objects she is holding but remain upright, then she should use a harness when carrying the baby. If she is likely to fall, then a stroller kept at home is a must.
E- Sleep: If the mother is breastfeeding, sleep deprivation may be unavoidable. The mother should make up any missed sleep during the infant's daytime naps, whenever possible. F-Anticonvulsant: Any increase in drugs during pregnancy will need to be decreased slowly to pre-pregnancy doses over 3 -4 weeks to avoid toxicity. G-Contraceptions: Barriers and IUDs are recommended. Many AEDs induce the hepatic cytochrome P-450 system, which is the primary metabolic pathway of the sex steroid hormones. This leads to rapid clearance of steroid hormones and allow ovulation in women taking OCPs or other hormonal forms of birth control
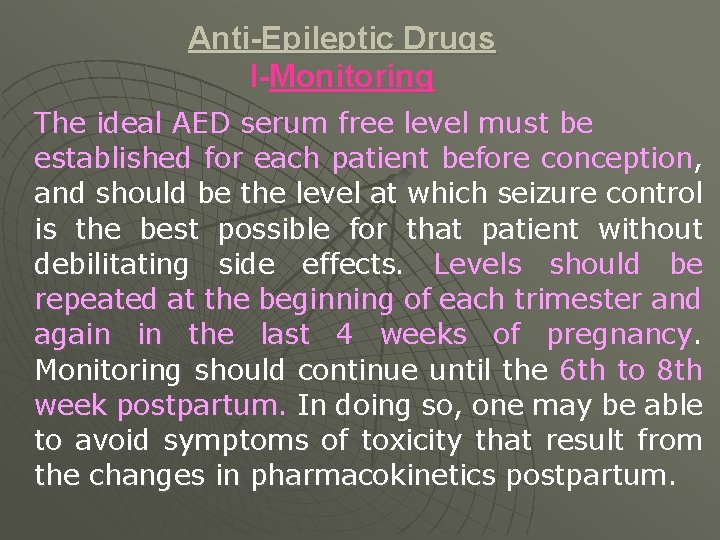
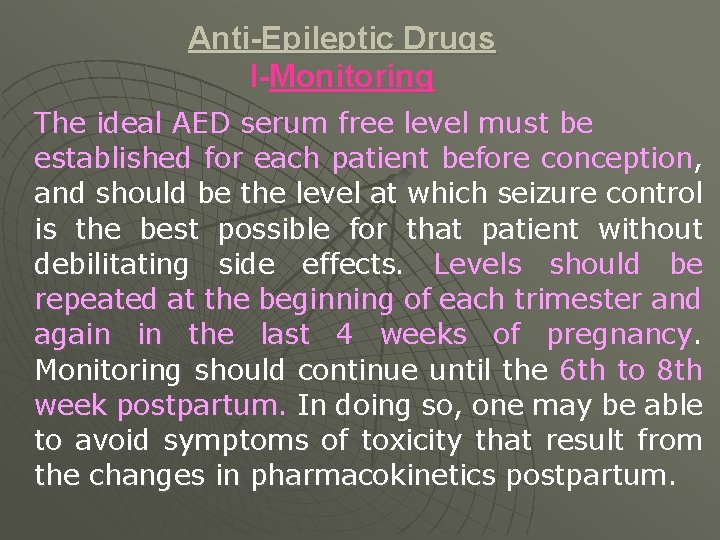
Anti-Epileptic Drugs I-Monitoring The ideal AED serum free level must be established for each patient before conception, and should be the level at which seizure control is the best possible for that patient without debilitating side effects. Levels should be repeated at the beginning of each trimester and again in the last 4 weeks of pregnancy. Monitoring should continue until the 6 th to 8 th week postpartum. In doing so, one may be able to avoid symptoms of toxicity that result from the changes in pharmacokinetics postpartum.
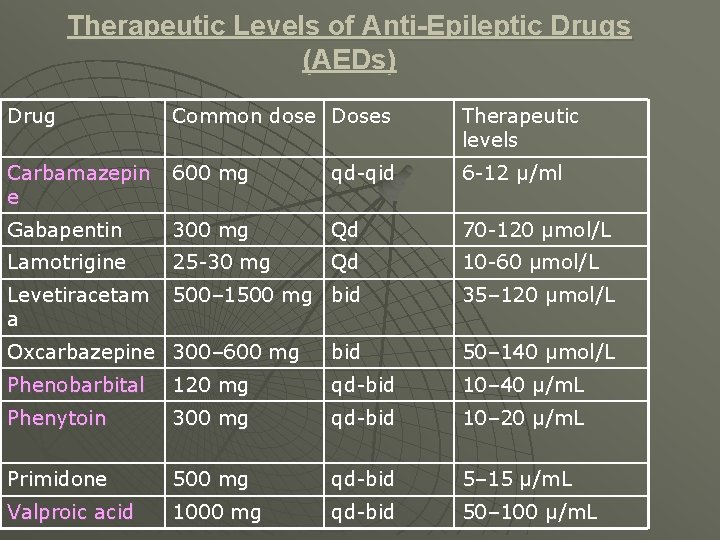
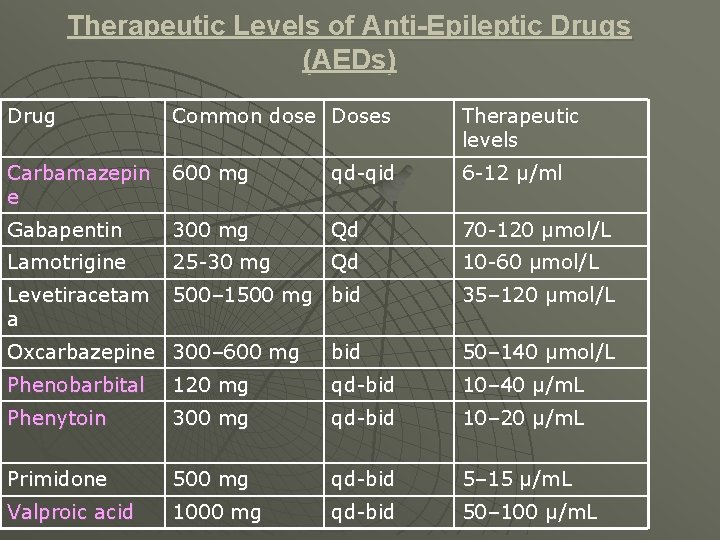
Therapeutic Levels of Anti-Epileptic Drugs (AEDs) Drug Common dose Doses Therapeutic levels Carbamazepin e 600 mg qd-qid 6 -12 μ/ml Gabapentin 300 mg Qd 70 -120 μmol/L Lamotrigine 25 -30 mg Qd 10 -60 μmol/L Levetiracetam a 500– 1500 mg bid 35– 120 μmol/L Oxcarbazepine 300– 600 mg bid 50– 140 μmol/L Phenobarbital 120 mg qd-bid 10– 40 μ/m. L Phenytoin 300 mg qd-bid 10– 20 μ/m. L Primidone 500 mg qd-bid 5– 15 μ/m. L Valproic acid 1000 mg qd-bid 50– 100 μ/m. L
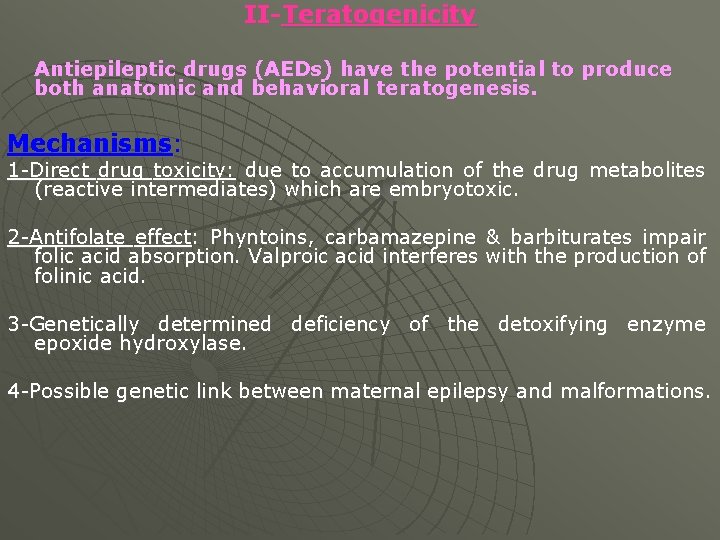
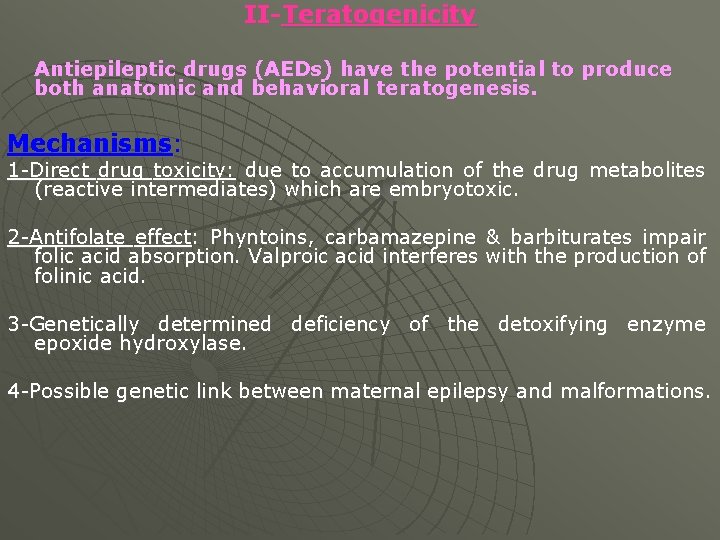
II-Teratogenicity Antiepileptic drugs (AEDs) have the potential to produce both anatomic and behavioral teratogenesis. Mechanisms: 1 -Direct drug toxicity: due to accumulation of the drug metabolites (reactive intermediates) which are embryotoxic. 2 -Antifolate effect: Phyntoins, carbamazepine & barbiturates impair folic acid absorption. Valproic acid interferes with the production of folinic acid. 3 -Genetically determined deficiency of the detoxifying enzyme epoxide hydroxylase. 4 -Possible genetic link between maternal epilepsy and malformations.
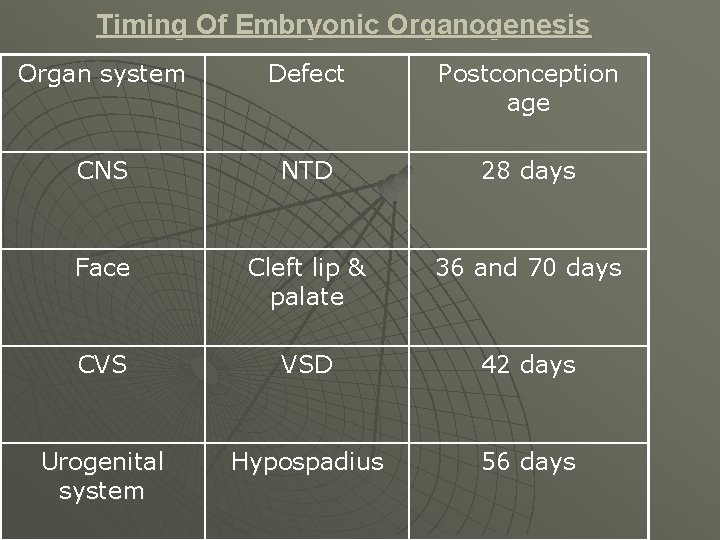
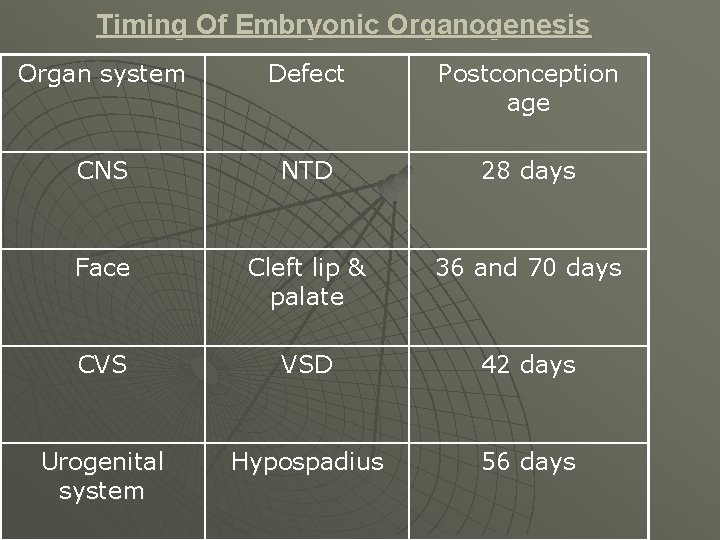
Timing Of Embryonic Organogenesis Organ system Defect Postconception age CNS NTD 28 days Face Cleft lip & palate 36 and 70 days CVS VSD 42 days Urogenital system Hypospadius 56 days
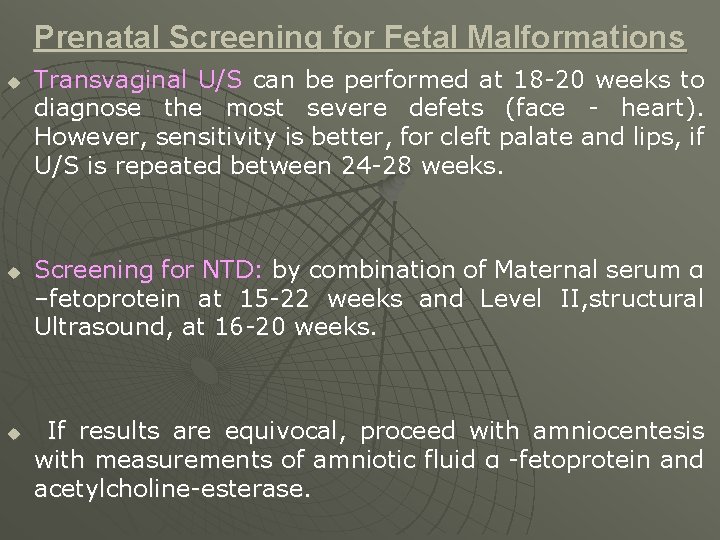
Prenatal Screening for Fetal Malformations u u u Transvaginal U/S can be performed at 18 -20 weeks to diagnose the most severe defets (face - heart). However, sensitivity is better, for cleft palate and lips, if U/S is repeated between 24 -28 weeks. Screening for NTD: by combination of Maternal serum α –fetoprotein at 15 -22 weeks and Level II, structural Ultrasound, at 16 -20 weeks. If results are equivocal, proceed with amniocentesis with measurements of amniotic fluid α -fetoprotein and acetylcholine-esterase.
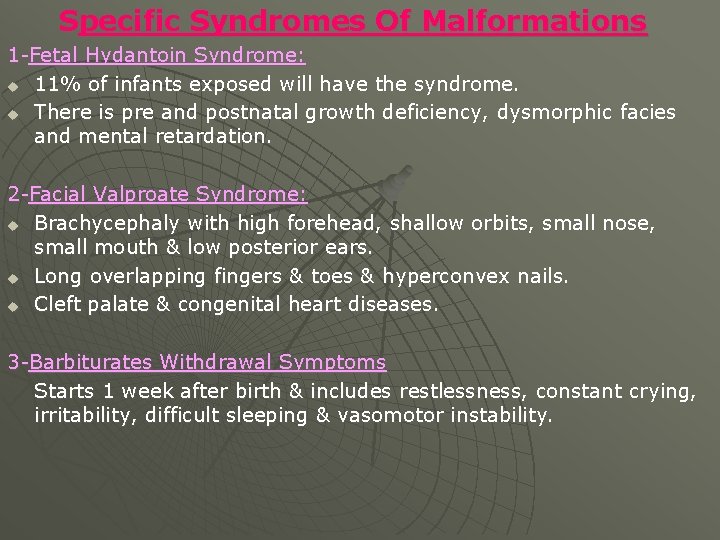
Specific Syndromes Of Malformations 1 -Fetal Hydantoin Syndrome: u 11% of infants exposed will have the syndrome. u There is pre and postnatal growth deficiency, dysmorphic facies and mental retardation. 2 -Facial Valproate Syndrome: u Brachycephaly with high forehead, shallow orbits, small nose, small mouth & low posterior ears. u Long overlapping fingers & toes & hyperconvex nails. u Cleft palate & congenital heart diseases. 3 -Barbiturates Withdrawal Symptoms Starts 1 week after birth & includes restlessness, constant crying, irritability, difficult sleeping & vasomotor instability.
Behavioral Teratogenesis In utero AED exposure can produce long-term behavioral changes: u u u babies exposed in utero to phenobarbital had a 7 -point decline in verbal IQ. the mean verbal IQ score following in utero exposure to valproate was 82 compared with 96 for carbamazepine and 95 for healthy controls. school-aged children exposed to in utero AEDs, 30% of children exposed to valproate monotherapy had additional educational needs compared with 3. 2% of children exposed to carbamazepine monotherapy and 6. 5% for other ani-epileptics.
III-Mono Versus Polytherapy u u u It is better to prescribe the lowest possible dose of a single drug to prevent and control fits. higher incidence of malformations polytherapy compared to montherapy. with If large daily doses are needed, then frequent smaller doses or extended-release formula may be helpful to avoid high peak levels. Dose should be divided into 3 -4 doses/day. This is because high peak plasma levels of the drug is more teratogenic.
VI-Clinical Or Subclinical Coagulopathy u Factors II, VII, IX & X are decreased. u Factors V, VIII & fibrinogen are normal. u PT & PTT should be determined at delivery. u If values are low or clinical coagulopathy develops in the neonatal period, TTT is by the infusion of FFP or concentrates of deficient factors in addition to the routine administration of vitamin K 1.
IV-Failure of AEDs An AED's failure to reduce seizures can be attributed to factors such as: 1 -Wrong dosing. 2 -Improper timing. 3 -Rapid administration of the drug. 4 -Ignoring conditions that precipitated the seizure. 5 -Instability of the drugs. Many drugs disintegrate easily with moisture. AEDs should be stored in a dry place and kept away from heat. 6 -Toxicity. 40% of patients experience toxic effects from older AEDs which often causes them to withdraw. Among the most distressing are sleepiness, problems in coordination and weight gain.
