Deep tissue pressure injury Intact or nonintact skin














- Slides: 28

Deep tissue pressure injury Intact or non-intact skin with localized area of persistent non-blanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood filled blister. Pain and temperature change often precede skin color changes. Discoloration may appear differently in darkly pigmented skin. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss.

Deep Tissue Injury

Unstagable: obscured full-thickness skin and tissue loss Full thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar If slough or eschar is removed, usually a stage 3 or 4 pressure injury is revealed.

Unstageable Unable to visualize wound bed. May have initially presented as a deep tissue injury
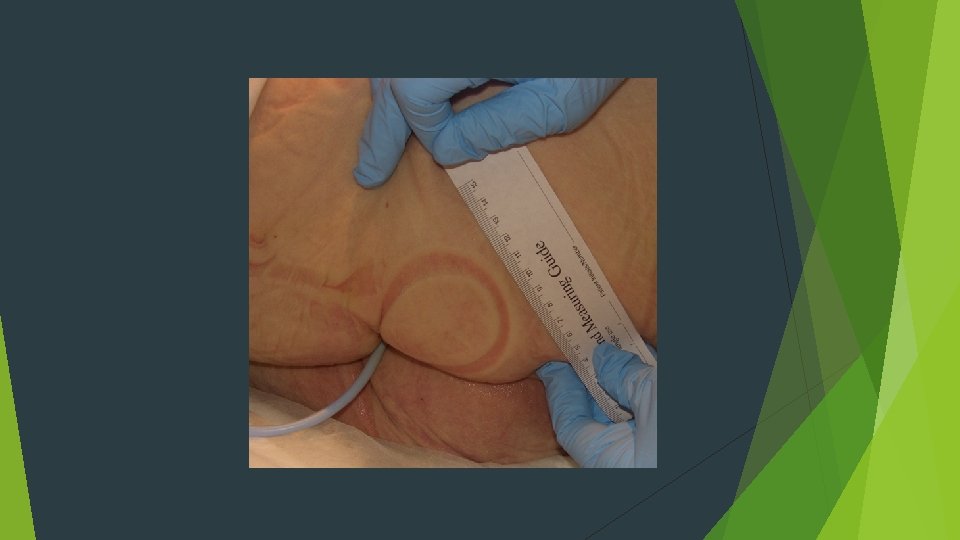
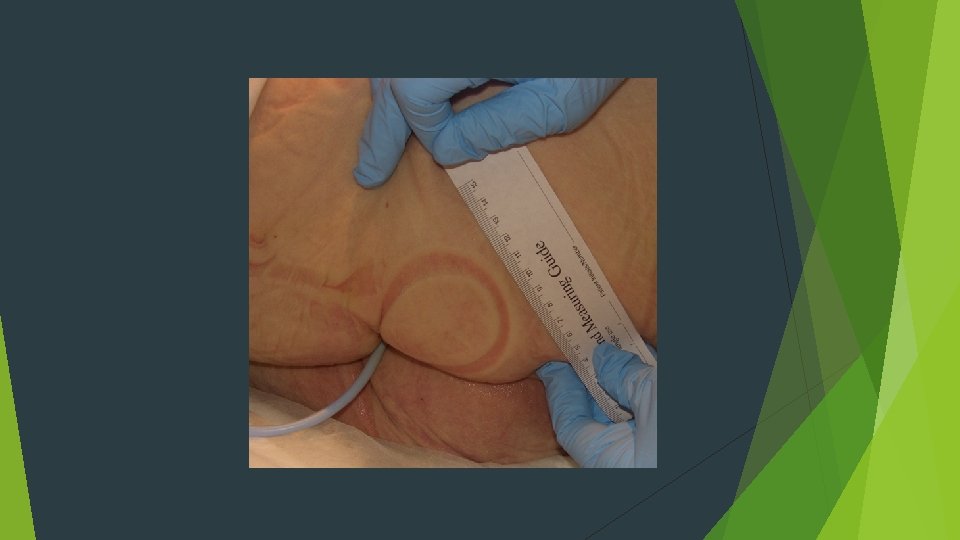
Additional definitions Medical device related pressure injury This describes an etiology of an injury. They generally conform to the pattern or shape of the device. They should be staged using the staging system Mucosal membrane pressure injury Found on the mucous membrane w/history of a device in use at the location of the injury. These injuries cannot be staged due to the anatomical location


Prevention and Treatment
Prevention techniques Re-distribute pressure Float heels and/or support surfaces does not mean you don’t have to turn the patient Turn Use q 2 h thick foam or boot style protectors Clam shell can injure Achilles area or put strain on the knee. You must still assess the skin daily
Support Surface Standards Initiative (S 3 I) NPUAP and experts in the field have spent over 5 years working on this project, which has now developed into a continuing sub committee under the NPUAP Research Committee with the charge to implement appropriate standards. coordinating the development of a uniform terminology, test methods and reporting standards for support surfaces. guidelines will provide an objective means for evaluating and comparing support surface characteristics. Support surface “A specialized device for pressure redistribution designed for management of tissue loads, microclimate and/or otherapeutic functions” [per NPUAP support surface standards initiative (S 3 I)]
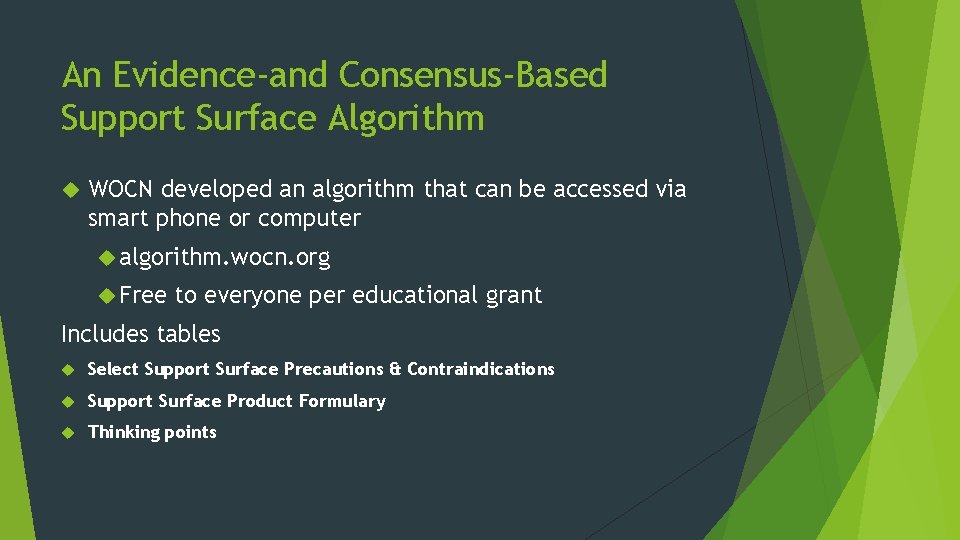
An Evidence-and Consensus-Based Support Surface Algorithm WOCN developed an algorithm that can be accessed via smart phone or computer algorithm. wocn. org Free to everyone per educational grant Includes tables Select Support Surface Precautions & Contraindications Support Surface Product Formulary Thinking points
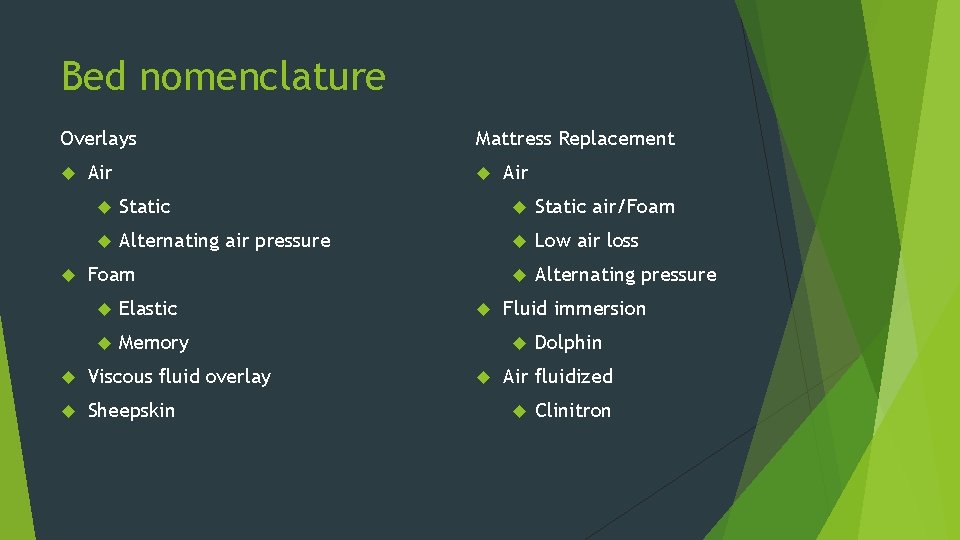
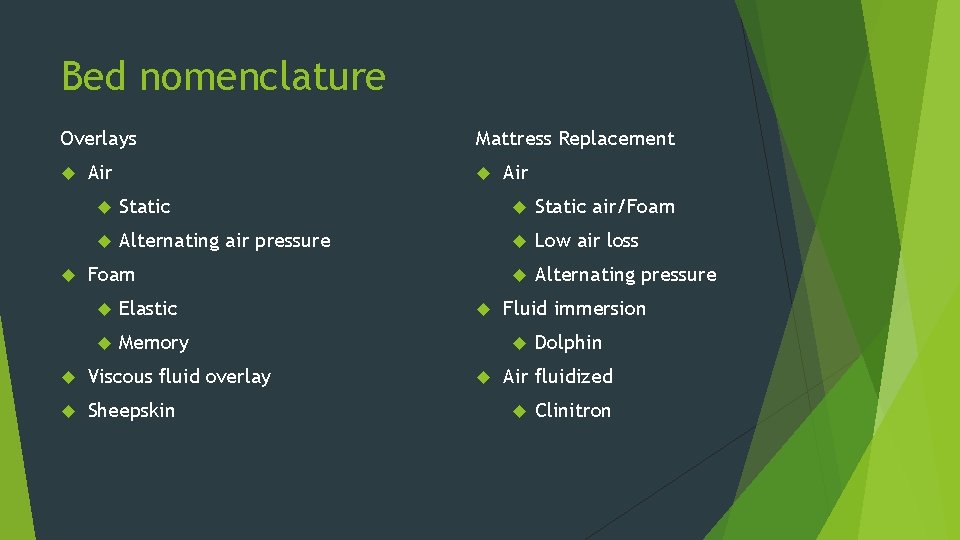
Bed nomenclature Overlays Air Mattress Replacement Air Static air/Foam Alternating air pressure Low air loss Alternating pressure Foam Elastic Memory Viscous fluid overlay Sheepskin Fluid immersion Dolphin Air fluidized Clinitron

Goals to Promote Healing Maintain moist wound environment Prevent infection Debride autolytic Prevent further trauma Fill dead space Don’t pack too tightly KISS and LIB
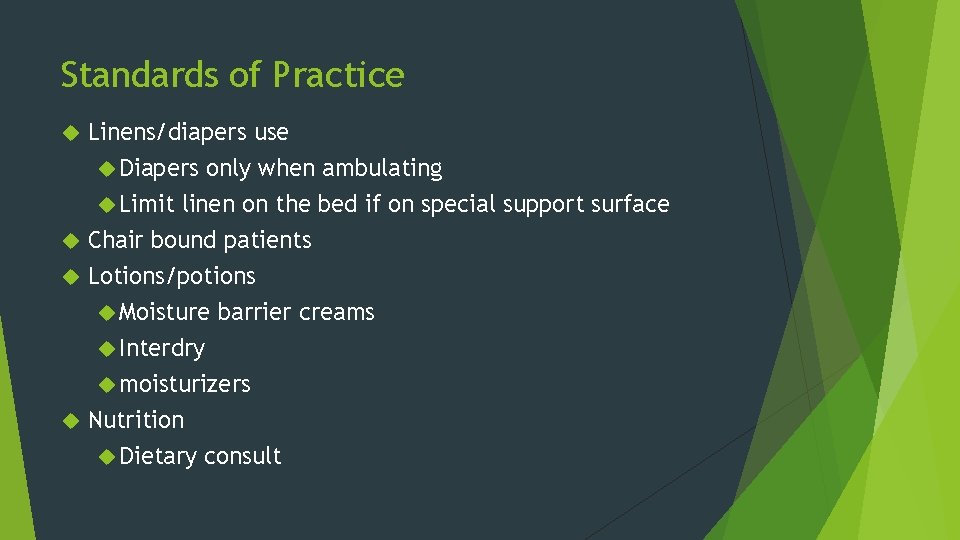
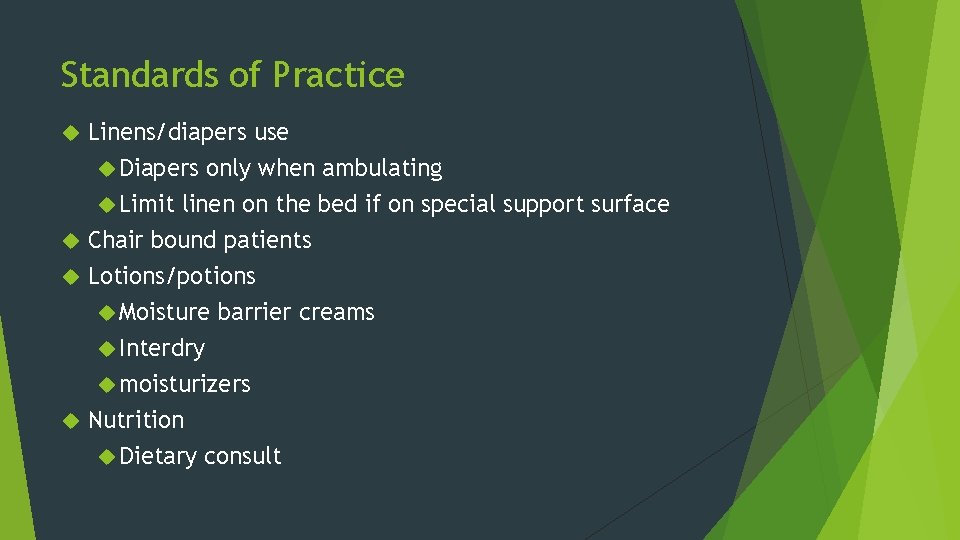
Standards of Practice Linens/diapers use Diapers only when ambulating Limit linen on the bed if on special support surface Chair bound patients Lotions/potions Moisture barrier creams Interdry moisturizers Nutrition Dietary consult
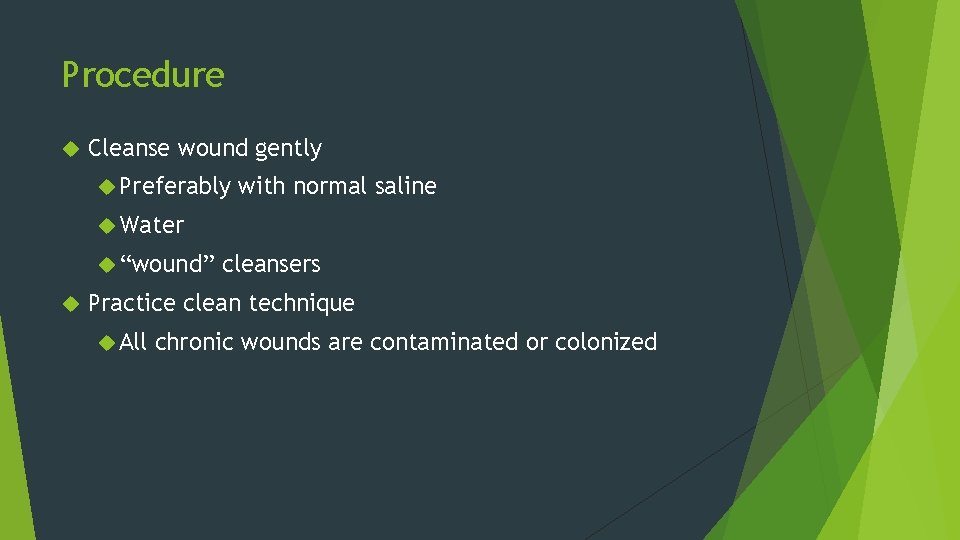
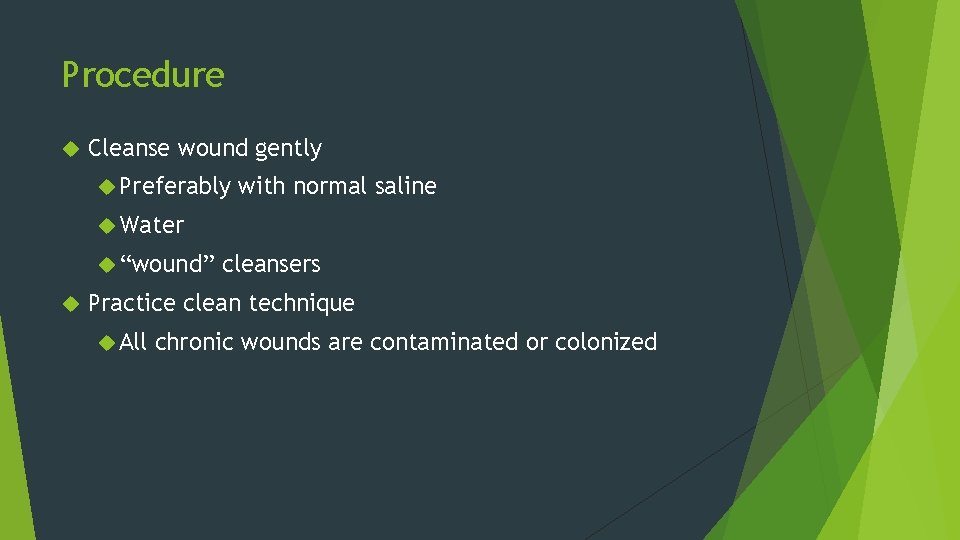
Procedure Cleanse wound gently Preferably with normal saline Water “wound” cleansers Practice clean technique All chronic wounds are contaminated or colonized
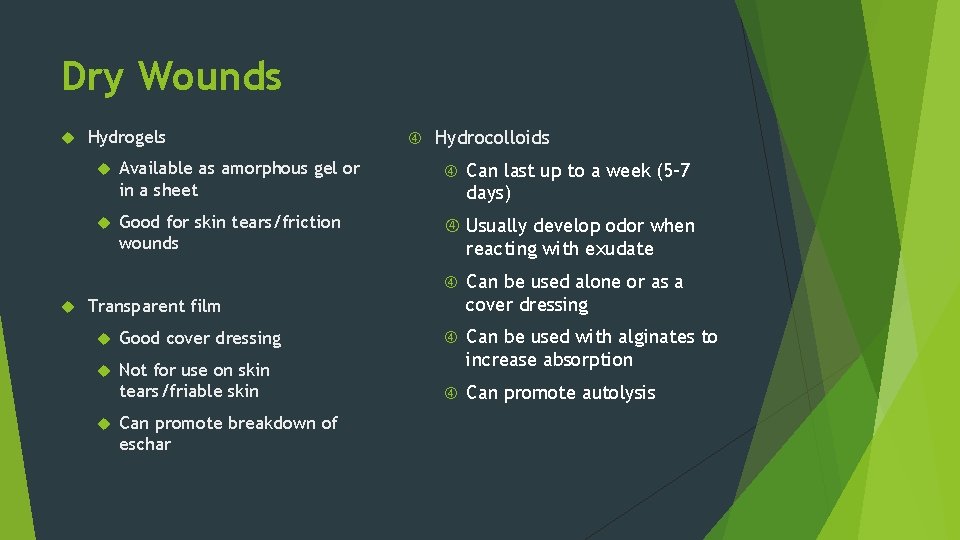
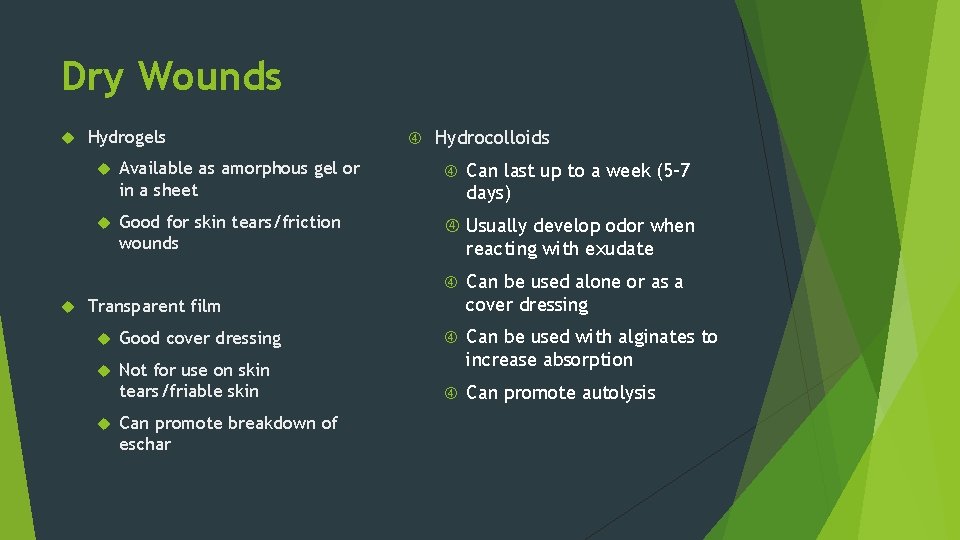
Dry Wounds Hydrogels Hydrocolloids Available as amorphous gel or in a sheet Good for skin tears/friction wounds Usually develop odor when Can last up to a week (5 -7 days) reacting with exudate Can be used alone or as a cover dressing Transparent film Good cover dressing Not for use on skin tears/friable skin Can be used with alginates to increase absorption Can promote autolysis Can promote breakdown of eschar
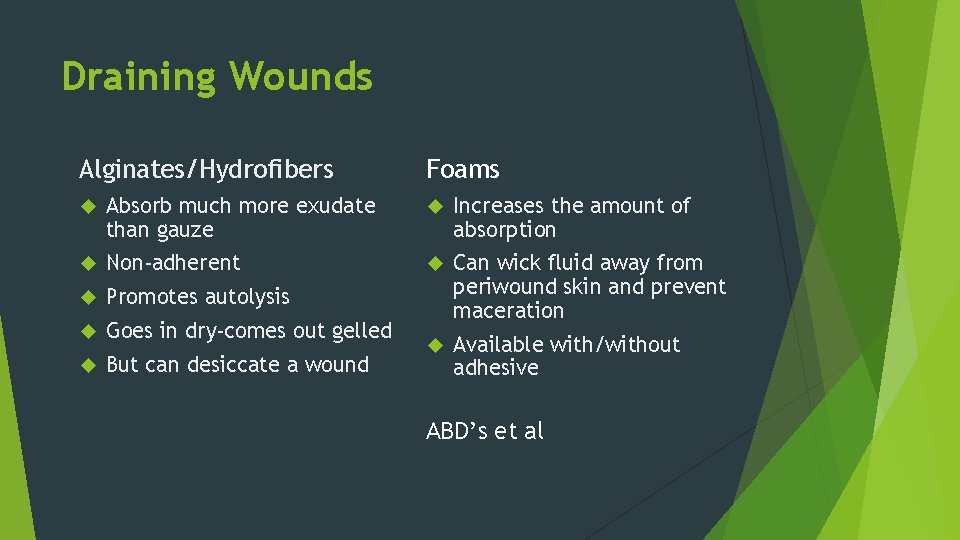
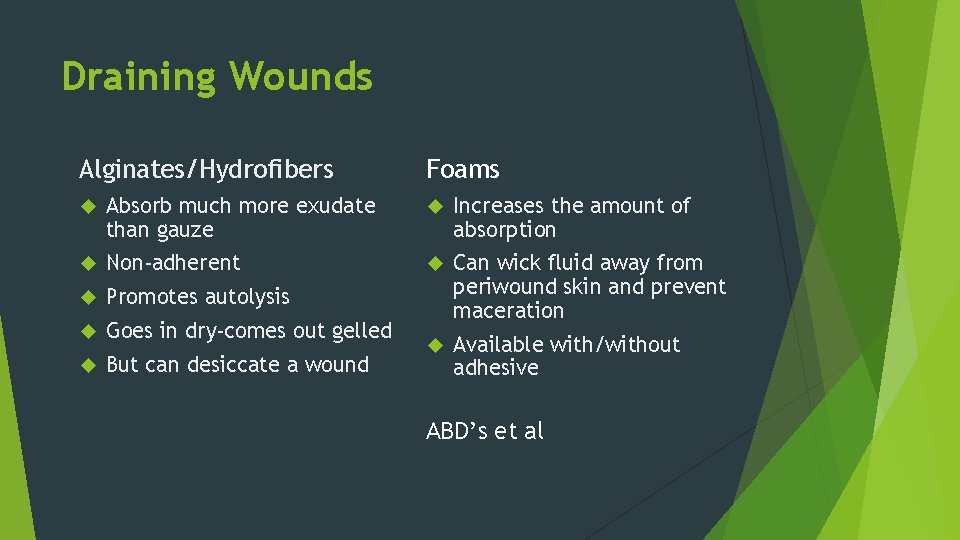
Draining Wounds Alginates/Hydrofibers Foams Absorb much more exudate than gauze Increases the amount of absorption Non-adherent Promotes autolysis Goes in dry-comes out gelled Can wick fluid away from periwound skin and prevent maceration But can desiccate a wound Available with/without adhesive ABD’s et al

Other options Impregnated Gauze Can be impregnated with various substances Contact layers Reduce pain with dressing changes Protect friable periwound skin Protect graft sites Some contact layers are designed to be reused
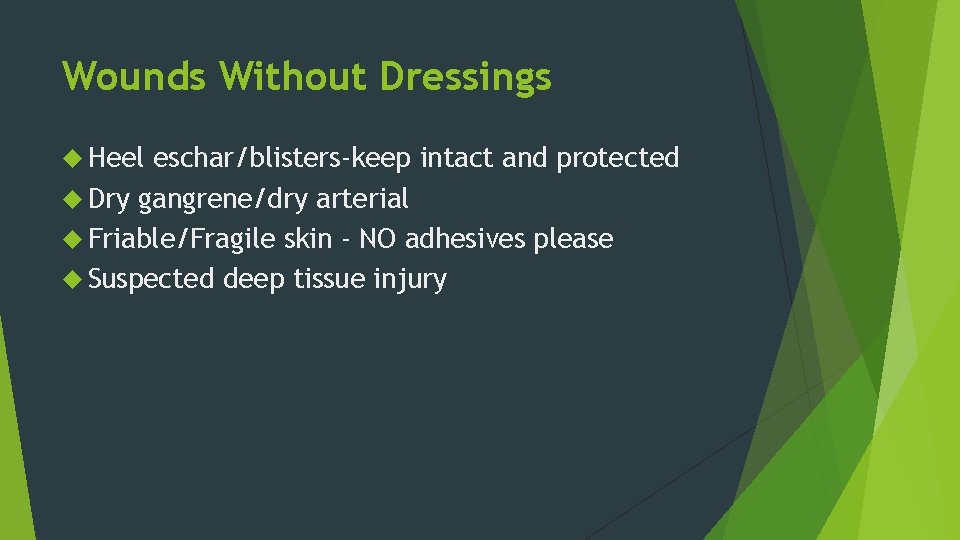
Wounds Without Dressings Heel eschar/blisters-keep intact and protected Dry gangrene/dry arterial Friable/Fragile skin - NO adhesives please Suspected deep tissue injury

Dry heel eschar

Arterial wounds or dry gangrene

Chemical damage-not pressure

Calciphylaxis (calcific uremic arteriolopathy)
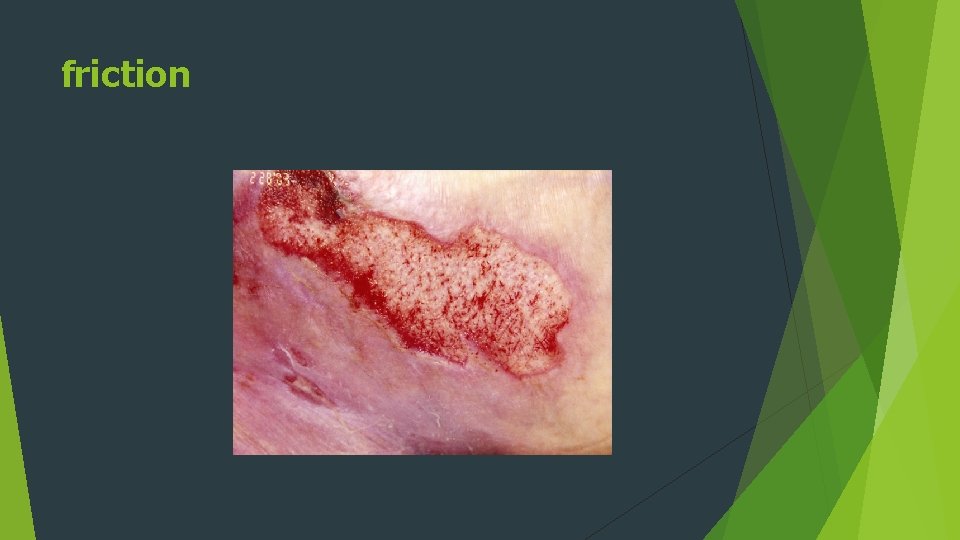
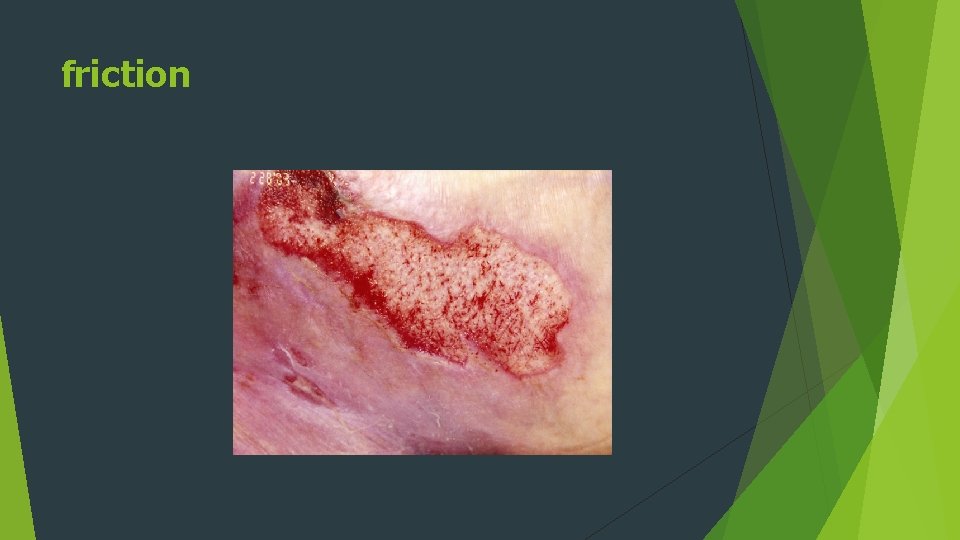
friction


Resources www. npuap. org www. wocn. org www. medlineuniversity. com