Deep Tendon Reflexes DTRs muscle stretch reflexes MSRs

- Slides: 27
Deep Tendon Reflexes - DTRs (muscle stretch reflexes - MSRs)
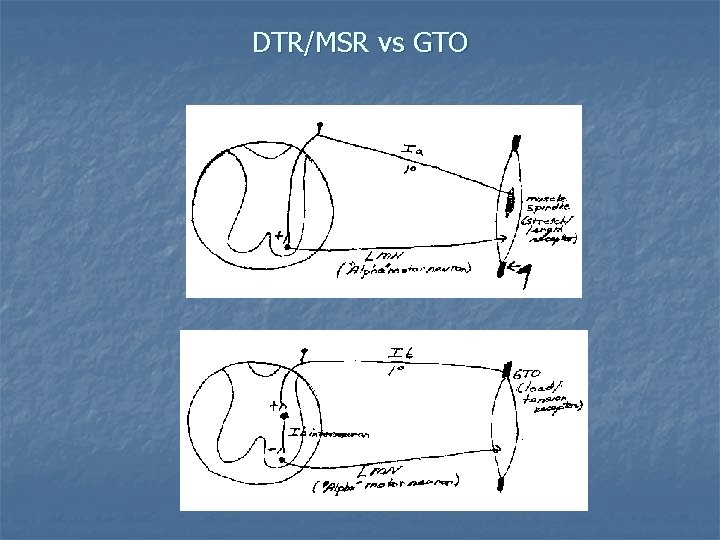
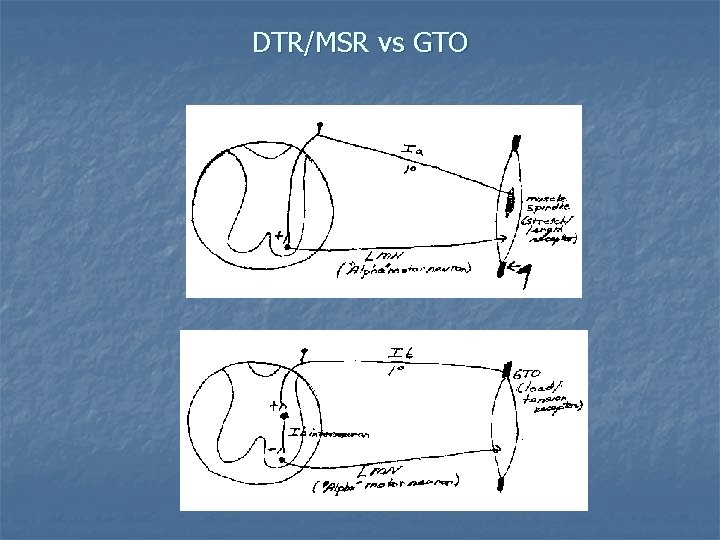
DTR/MSR vs GTO
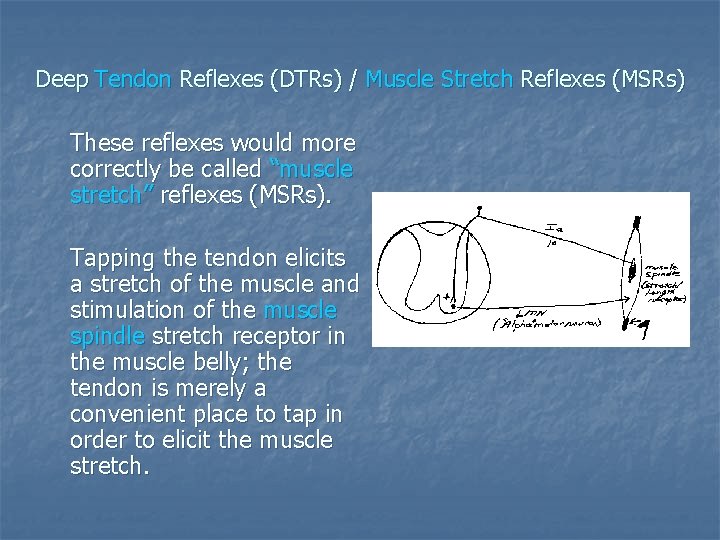
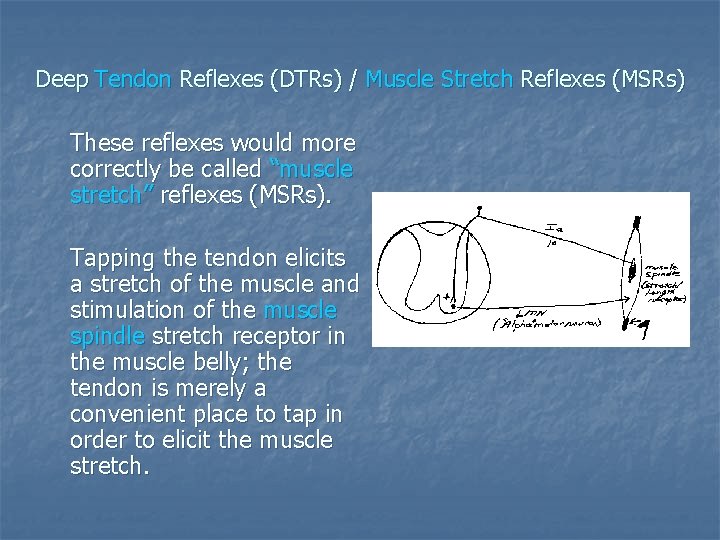
Deep Tendon Reflexes (DTRs) / Muscle Stretch Reflexes (MSRs) These reflexes would more correctly be called “muscle stretch” reflexes (MSRs). Tapping the tendon elicits a stretch of the muscle and stimulation of the muscle spindle stretch receptor in the muscle belly; the tendon is merely a convenient place to tap in order to elicit the muscle stretch.
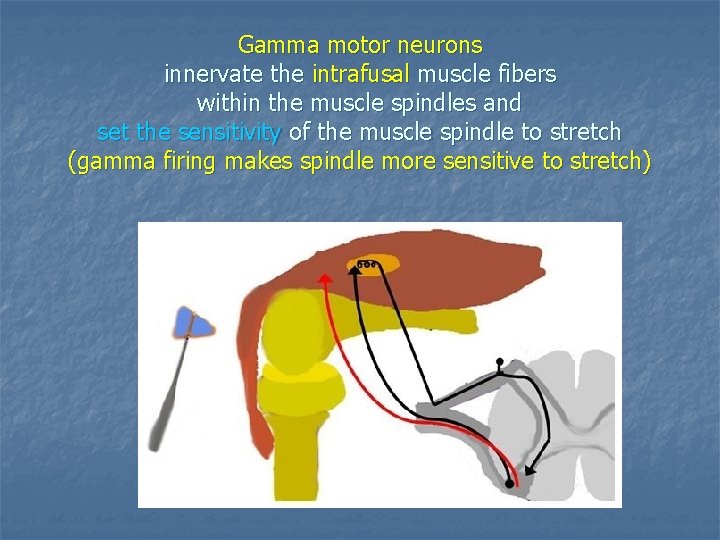
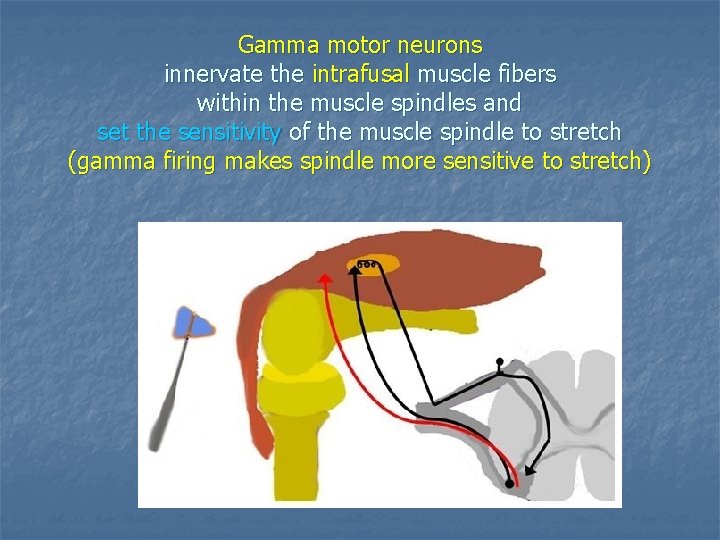
Gamma motor neurons innervate the intrafusal muscle fibers within the muscle spindles and set the sensitivity of the muscle spindle to stretch (gamma firing makes spindle more sensitive to stretch)
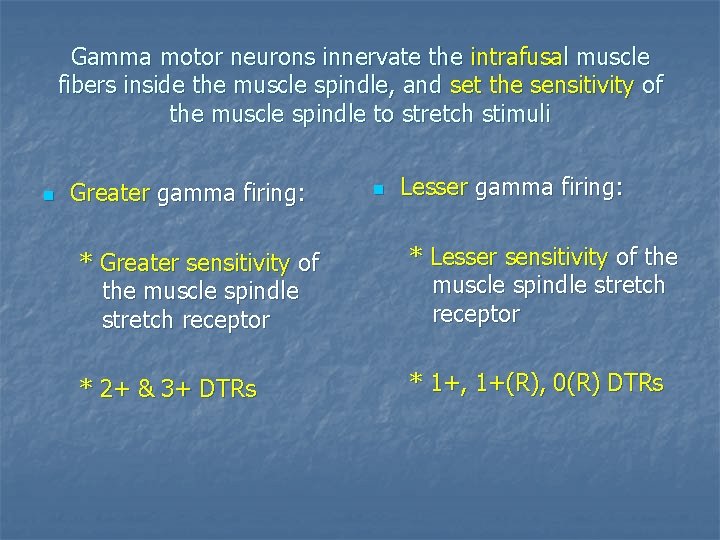
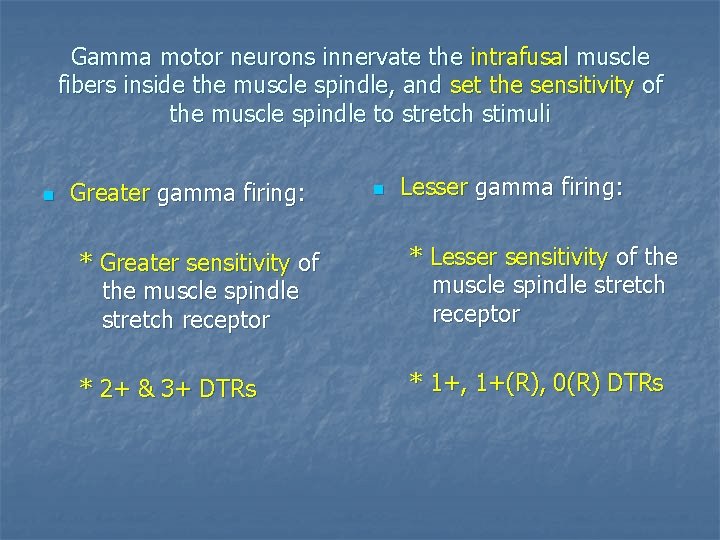
Gamma motor neurons innervate the intrafusal muscle fibers inside the muscle spindle, and set the sensitivity of the muscle spindle to stretch stimuli n Greater gamma firing: n Lesser gamma firing: * Greater sensitivity of the muscle spindle stretch receptor * Lesser sensitivity of the muscle spindle stretch receptor * 2+ & 3+ DTRs * 1+, 1+(R), 0(R) DTRs
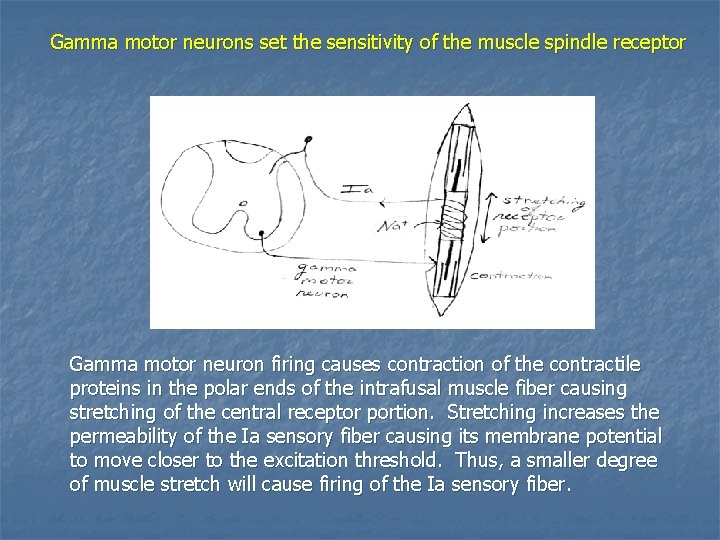
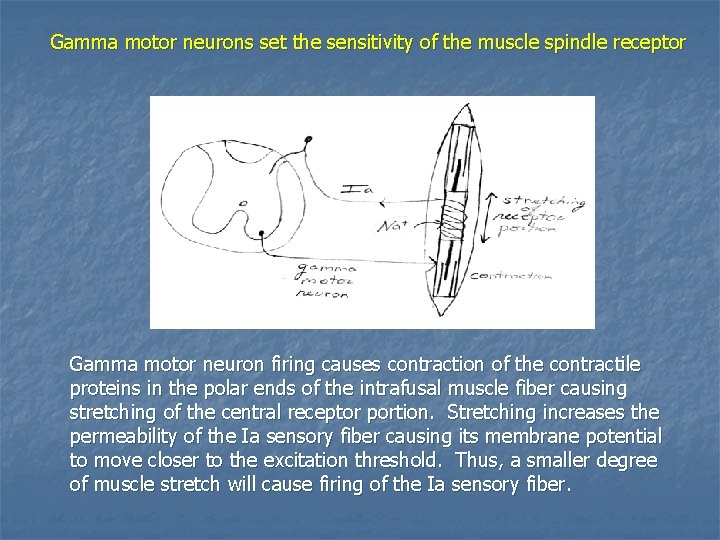
Gamma motor neurons set the sensitivity of the muscle spindle receptor Gamma motor neuron firing causes contraction of the contractile proteins in the polar ends of the intrafusal muscle fiber causing stretching of the central receptor portion. Stretching increases the permeability of the Ia sensory fiber causing its membrane potential to move closer to the excitation threshold. Thus, a smaller degree of muscle stretch will cause firing of the Ia sensory fiber.
Principles of DTR testing Proper testing of muscle stretch reflexes is dependent upon the following: a. b. c. d. e. relaxation of the patient optimal muscle tension correct placement of the stimulus adequate stretch stimulus proper reinforcement methods if a reflex is not elicited by usual methods
Principles of DTR testing a. relaxation of the patient The patient must have muscles relaxed with the extremity hanging loosely, or resting comfortably. Any muscle tension to maintain the posture may artificially increase or decrease the reflex. Distracting the patient by engaging in conversation may be more effective than encouraging the patient to relax. If necessary, choose an alternate testing position.
Principles of DTR testing b. optimal muscle tension Because the briskness of the response depends largely upon the state of tone of the muscle, the muscle should be in a slight state of tension. A reflex may not be elicited form a muscle that is stretched too much, or too little. The proper degree of tension is usually obtained when the muscle is placed midway between its greatest and shortest lengths. Be sure the testing positions are symmetrical as you compare reflex activity side-to-side. If a reflex can not be elicited, by varying the length of the muscle.
Principles of DTR testing c. correct placement of the stimulus The examiner must know the correct location of the tendon in order to properly elicit each reflex. If a reflex is not elicited, ask the patient to contract the muscle against your resistance, and palpate to determine the correct location of the tendon. Most reflexes are elicited by tapping the tendon directly, however, the biceps and the medial hamstring reflexes are elicited by tapping the examiners thumb which is contacting and tensioning the tendon.
Principles of DTR testing d. adequate stretch stimulus The stimulus should be quick, but initially light. If the reflex is not elicited a stronger stimulus is applied. The reflex hammer should be held loosely between the thumb and fingers so that it swings freely, striking the tendon briskly, and rebounds.
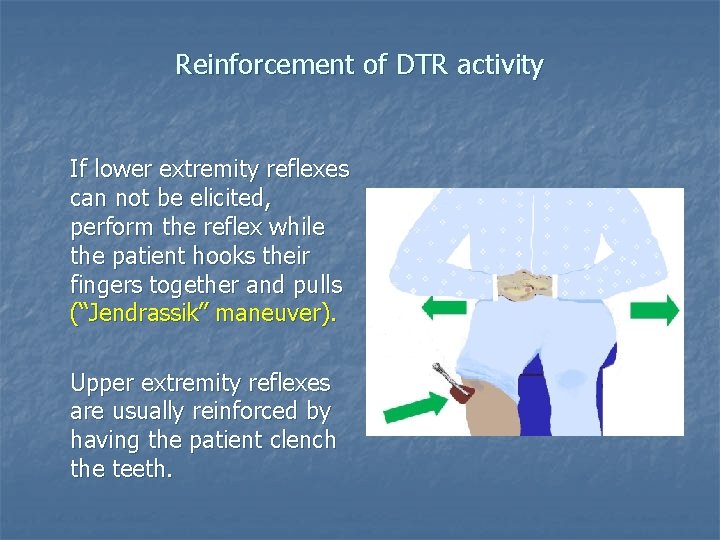
Principles of DTR testing e. reinforcement If a muscle stretch reflex is not elicited after the above steps are taken, and effort to reinforce the reflex should be made. The most common method of reinforcement is to have the patient isometrically contract muscles not involved in the examination. The increased reflex activity is probably due to facilitation of alpha and/or gamma motor neuron activity.
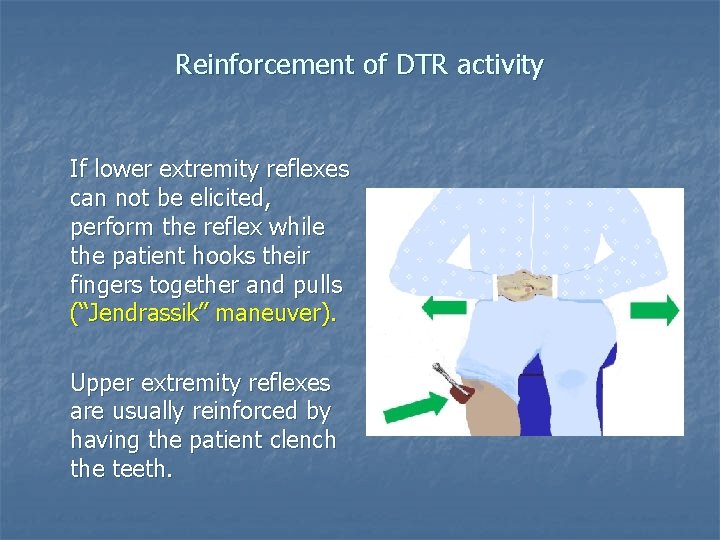
Reinforcement of DTR activity If lower extremity reflexes can not be elicited, perform the reflex while the patient hooks their fingers together and pulls (“Jendrassik” maneuver). Upper extremity reflexes are usually reinforced by having the patient clench the teeth.
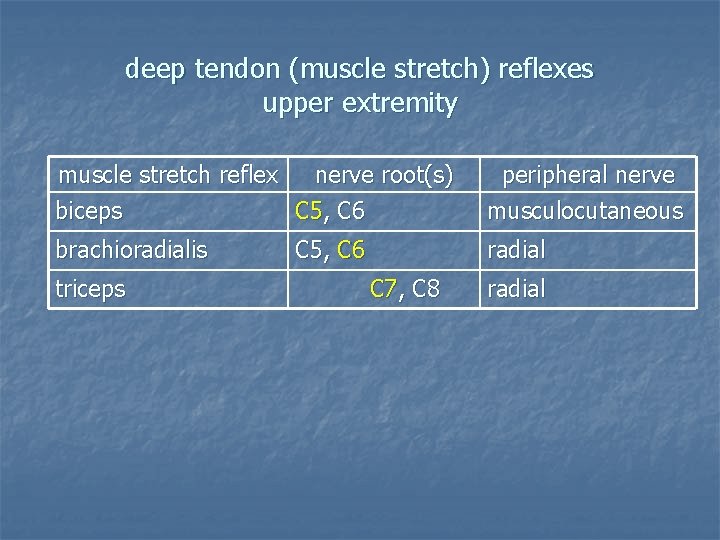
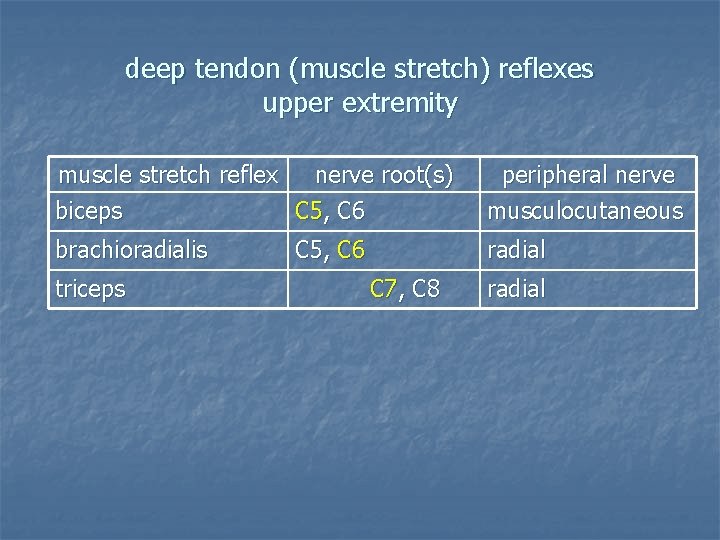
deep tendon (muscle stretch) reflexes upper extremity muscle stretch reflex nerve root(s) biceps C 5, C 6 peripheral nerve musculocutaneous brachioradialis radial triceps C 5, C 6 C 7, C 8 radial
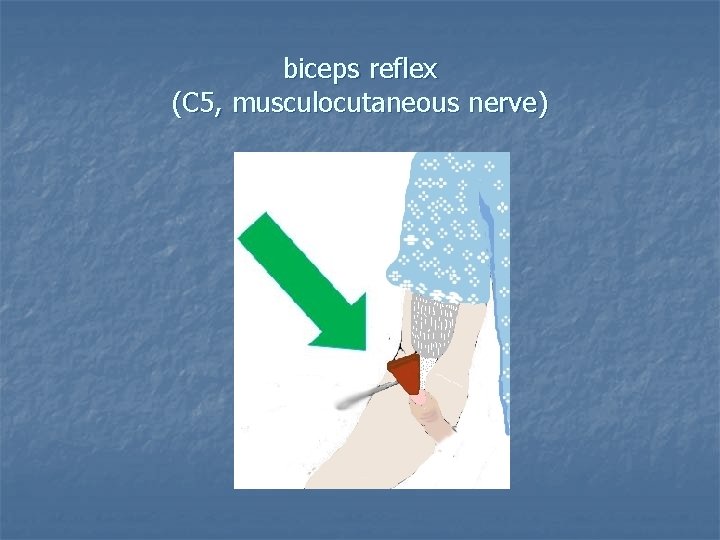
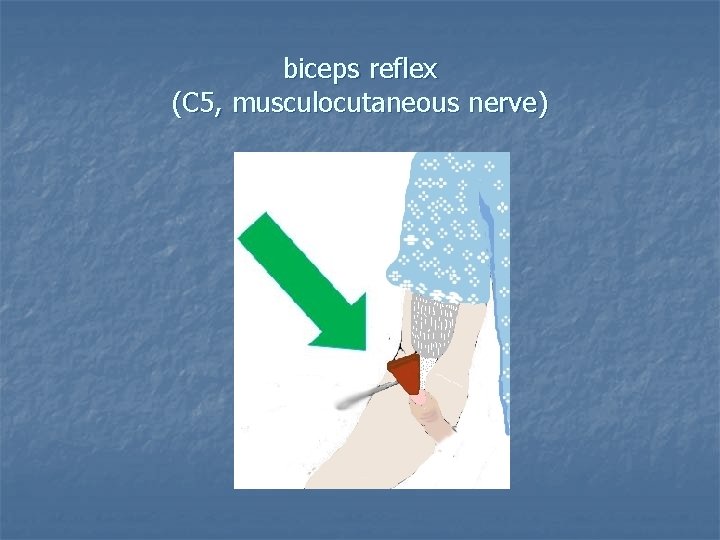
biceps reflex (C 5, musculocutaneous nerve)
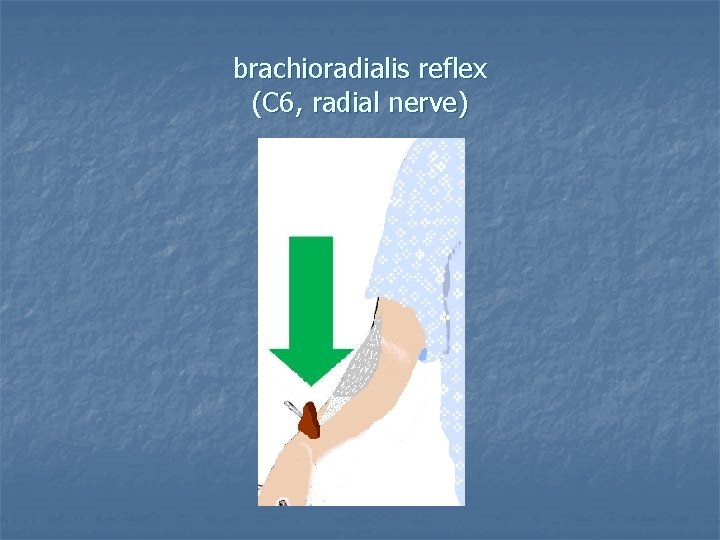
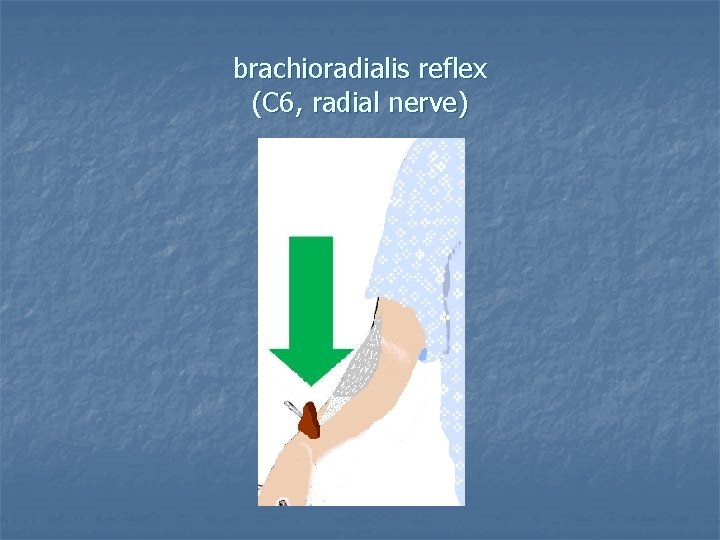
brachioradialis reflex (C 6, radial nerve)
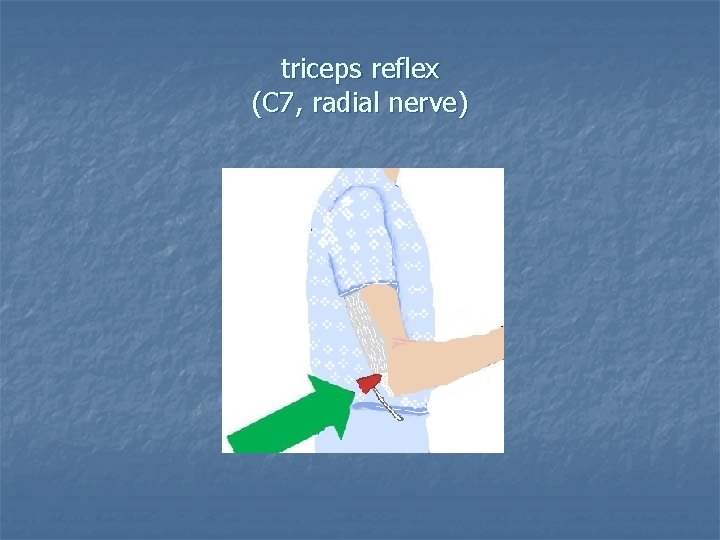
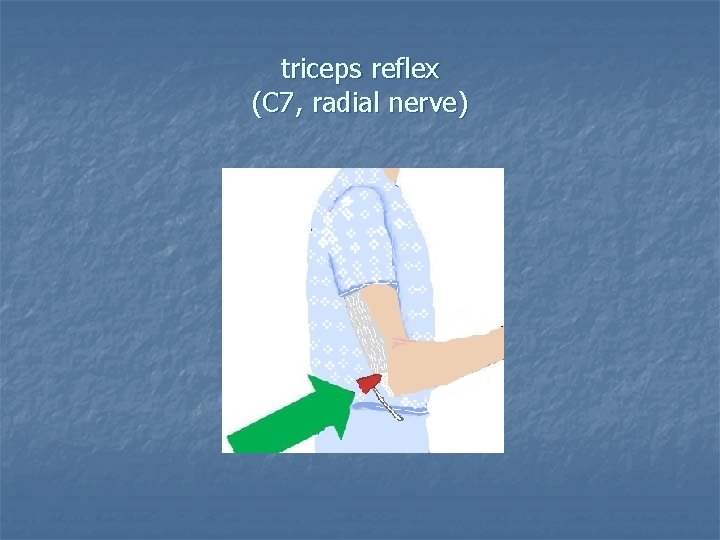
triceps reflex (C 7, radial nerve)
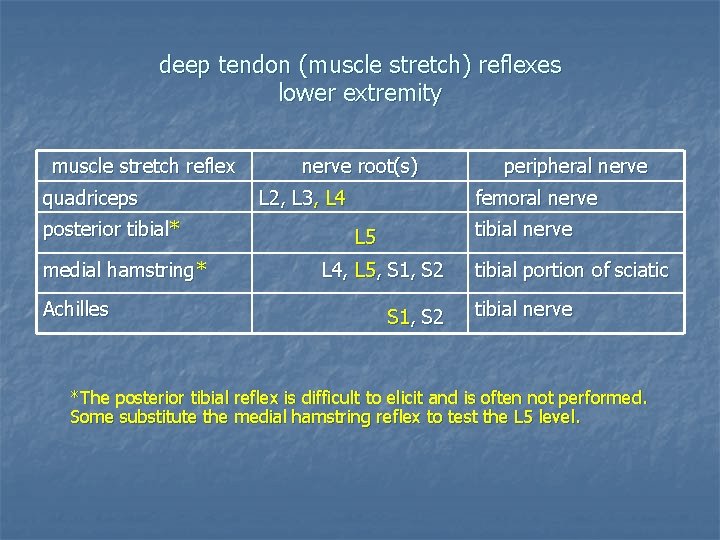
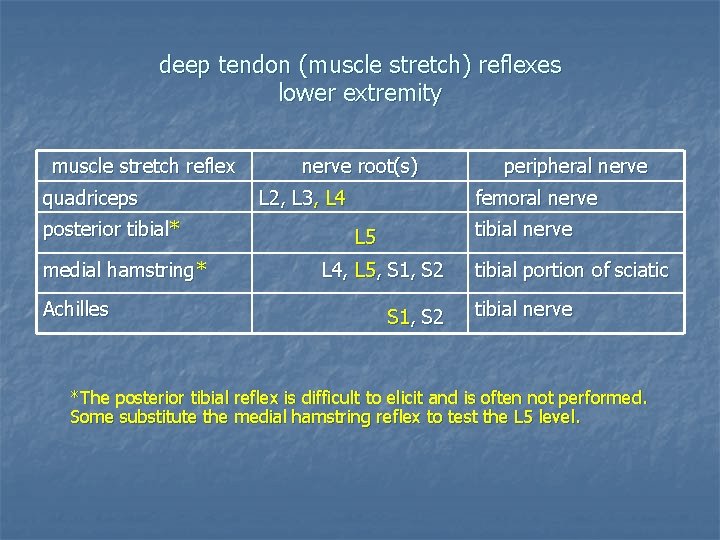
deep tendon (muscle stretch) reflexes lower extremity muscle stretch reflex quadriceps posterior tibial* medial hamstring* Achilles nerve root(s) L 2, L 3, L 4 peripheral nerve femoral nerve tibial nerve L 5 L 4, L 5, S 1, S 2 tibial portion of sciatic tibial nerve *The posterior tibial reflex is difficult to elicit and is often not performed. Some substitute the medial hamstring reflex to test the L 5 level.
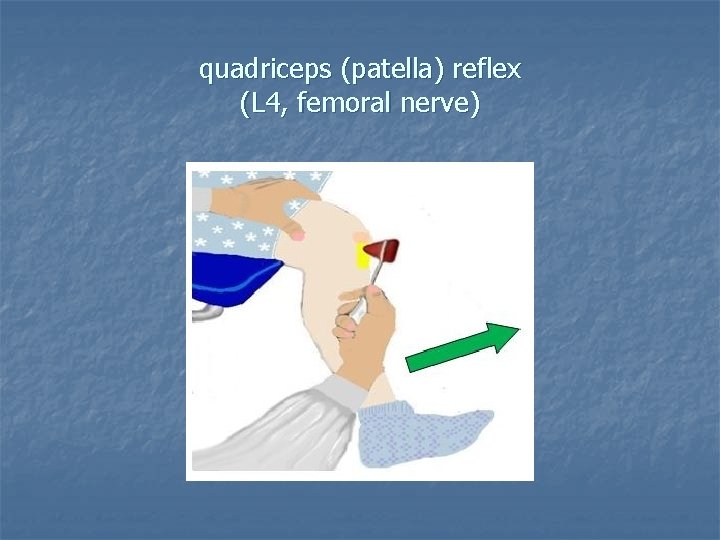
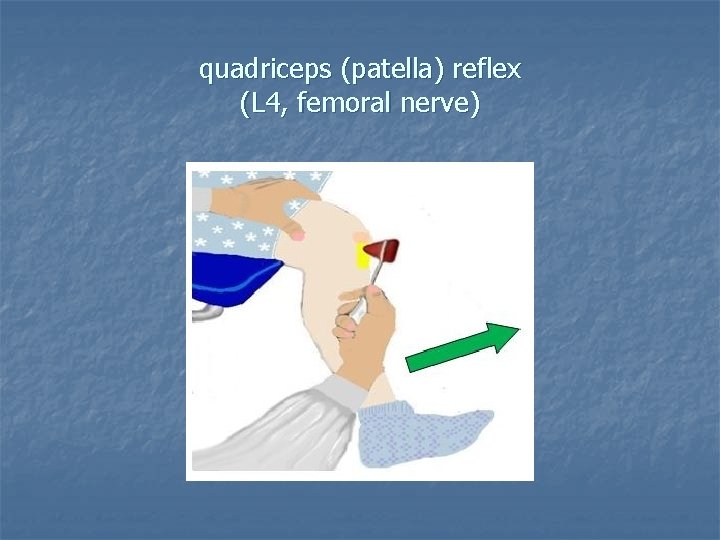
quadriceps (patella) reflex (L 4, femoral nerve)
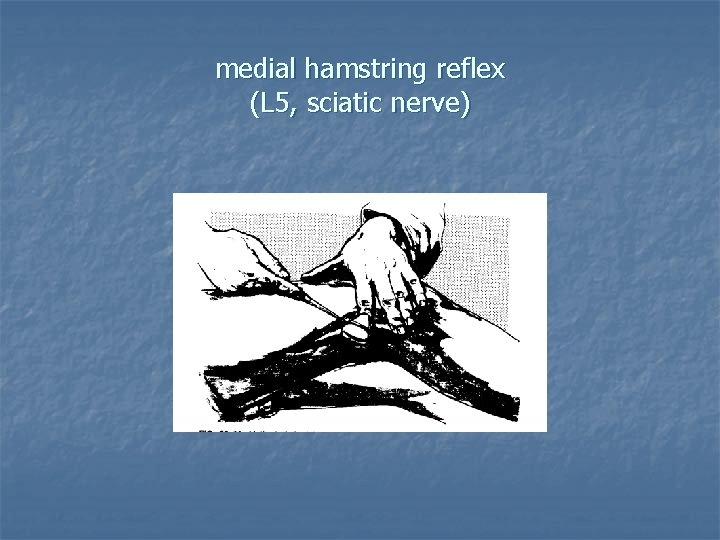
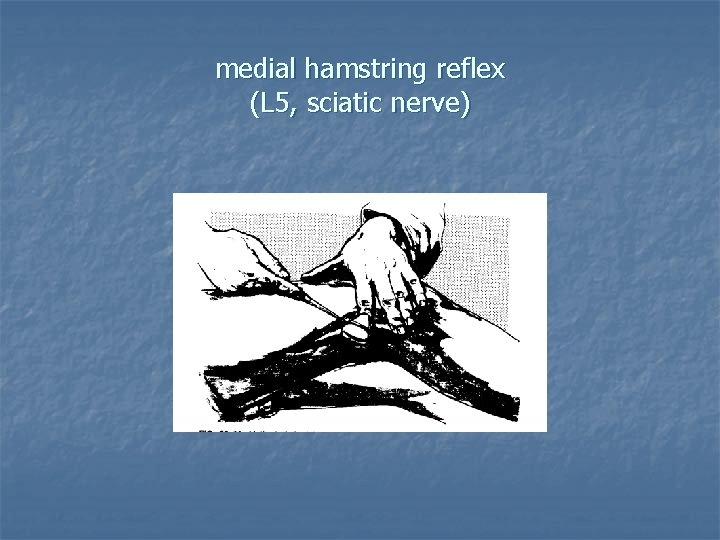
medial hamstring reflex (L 5, sciatic nerve)

Achilles reflex (S 1, tibial nerve)
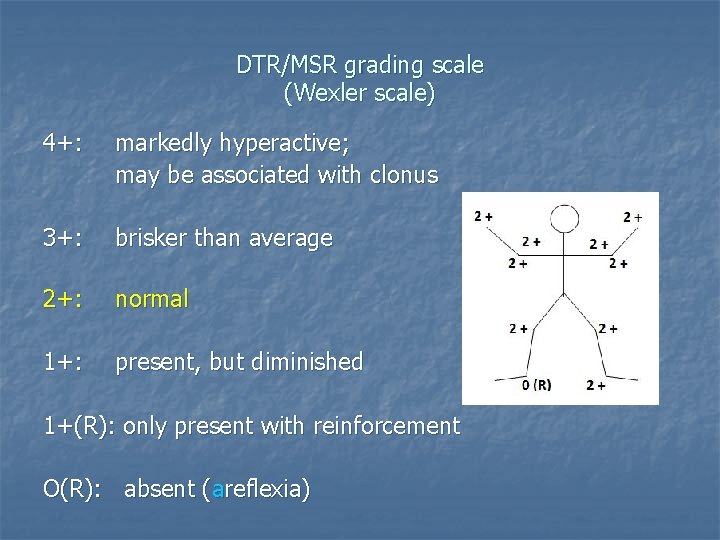
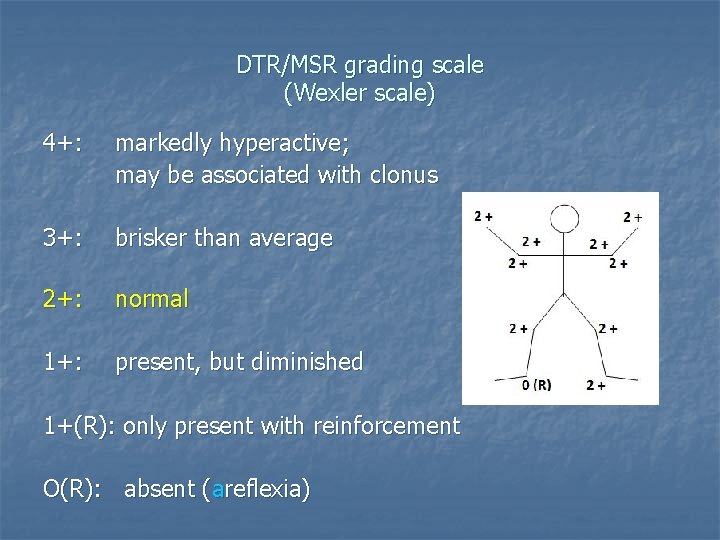
DTR/MSR grading scale (Wexler scale) 4+: markedly hyperactive; may be associated with clonus 3+: brisker than average 2+: normal 1+: present, but diminished 1+(R): only present with reinforcement O(R): absent (areflexia)
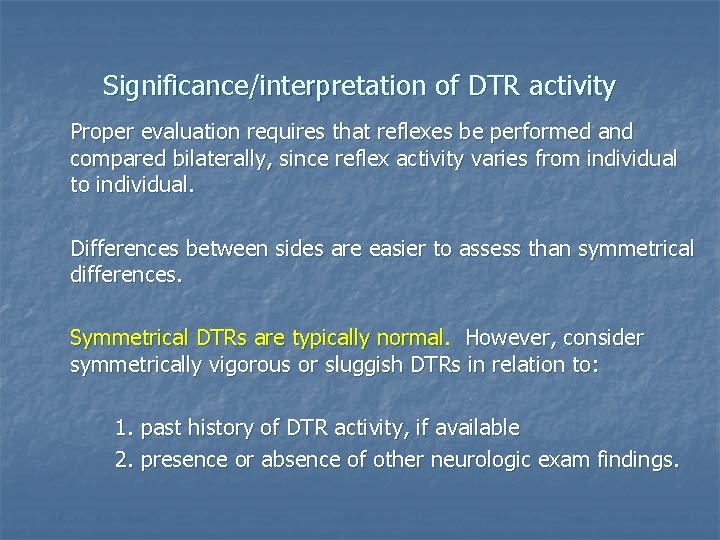
Significance/interpretation of DTR activity Proper evaluation requires that reflexes be performed and compared bilaterally, since reflex activity varies from individual to individual. Differences between sides are easier to assess than symmetrical differences. Symmetrical DTRs are typically normal. However, consider symmetrically vigorous or sluggish DTRs in relation to: 1. past history of DTR activity, if available 2. presence or absence of other neurologic exam findings.
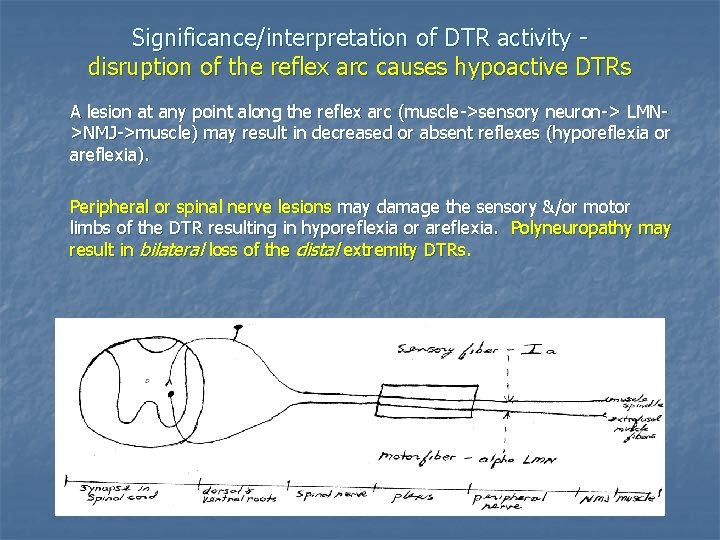
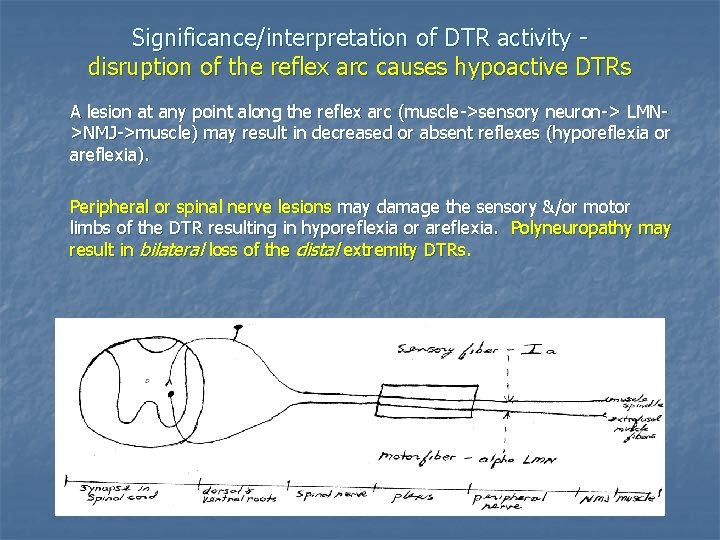
Significance/interpretation of DTR activity disruption of the reflex arc causes hypoactive DTRs A lesion at any point along the reflex arc (muscle->sensory neuron-> LMN>NMJ->muscle) may result in decreased or absent reflexes (hyporeflexia or areflexia). Peripheral or spinal nerve lesions may damage the sensory &/or motor limbs of the DTR resulting in hyporeflexia or areflexia. Polyneuropathy may result in bilateral loss of the distal extremity DTRs.
Less common lesions of the DTR arc hyporeflexia 1. anterior horn cell disorder (LMN cell body): a. polio b. ALS 2. spinal cord sensory-motor synaptic region: syringomyelia 3. NMJ disorders 4. myopathy (proximal reflexes may be affected initially)
Other causes of hyporeflexia/areflexia 1. Cerebellar disease 2. Hypothyroidism (slowing of the reflex’s relaxation, esp. Achilles; may be difficult to assess) 3. “Spinal shock” phase of UMN lesion (areflexia & flaccid paralysis) Reflexes may not return until a major portion of motor strength has recovered. Sometimes there is persistent areflexia even after complete recovery of both motor and sensory functions.
Significance/interpretation of hyperactive DTRs 1. UMN lesions 2. hyperthyroidism