Deep Nasal Suctioning Nick Betz RN BSN CPEN
Deep Nasal Suctioning Nick Betz RN, BSN CPEN
Deep Nasal Suctioning � It is a Nursing Intervention � Determined by Assessment…NOT timed
Suction Purposes � Remove secretions obstructing the trachea and nasopharyngeal airway � Obtain secretions for diagnostic purposes � Prevent infection from occurring due to accumulated secretions
Assessment Findings to determine the need for suctioning � Dyspnea � Poor skin color � Decreased Sa. O 2 levels � Visible or audible secretions � Restlessness � Retractions
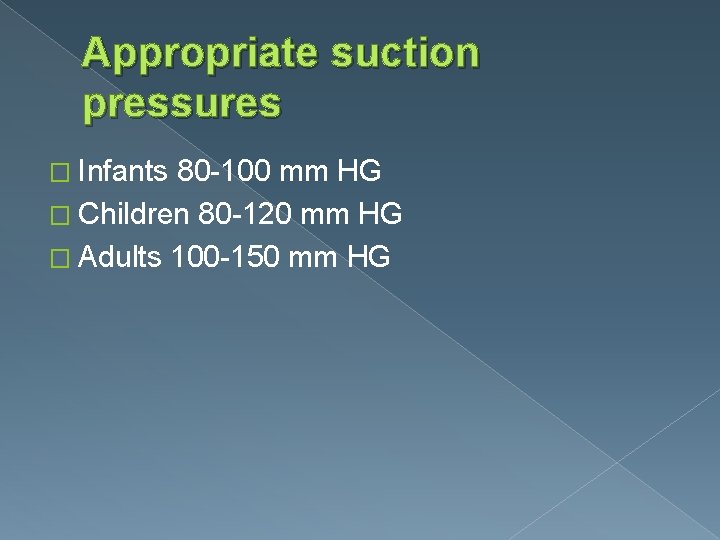
Appropriate suction pressures � Infants 80 -100 mm HG � Children 80 -120 mm HG � Adults 100 -150 mm HG
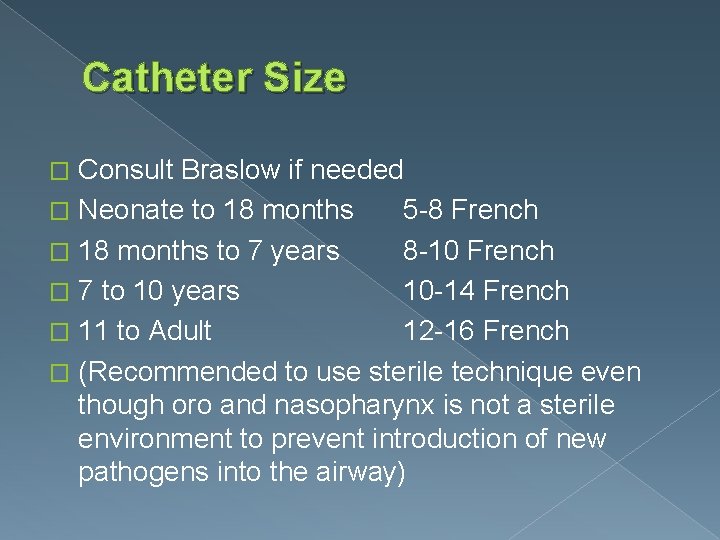
Catheter Size Consult Braslow if needed � Neonate to 18 months 5 -8 French � 18 months to 7 years 8 -10 French � 7 to 10 years 10 -14 French � 11 to Adult 12 -16 French � (Recommended to use sterile technique even though oro and nasopharynx is not a sterile environment to prevent introduction of new pathogens into the airway) �
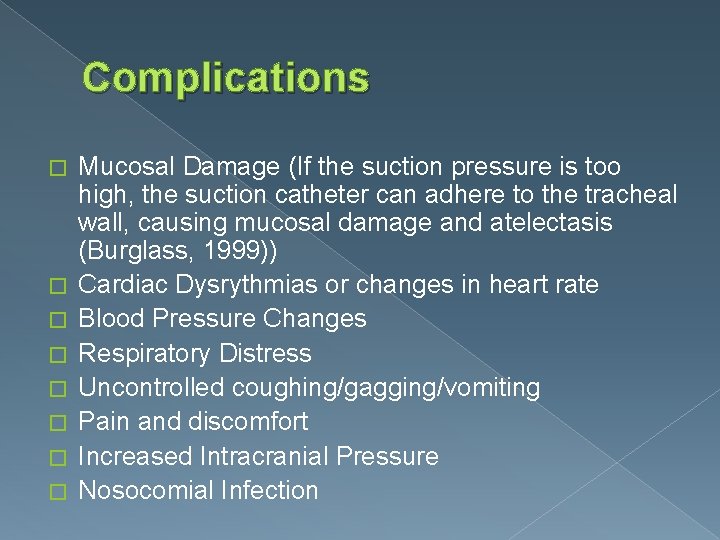
Complications � � � � Mucosal Damage (If the suction pressure is too high, the suction catheter can adhere to the tracheal wall, causing mucosal damage and atelectasis (Burglass, 1999)) Cardiac Dysrythmias or changes in heart rate Blood Pressure Changes Respiratory Distress Uncontrolled coughing/gagging/vomiting Pain and discomfort Increased Intracranial Pressure Nosocomial Infection
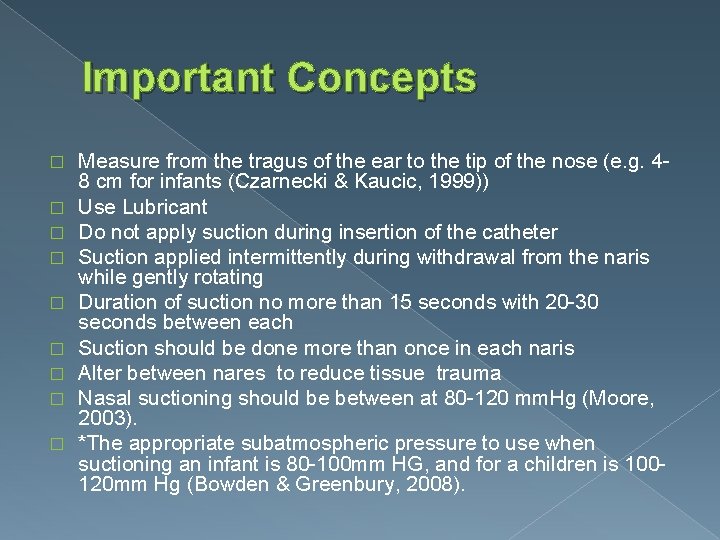
Important Concepts � � � � � Measure from the tragus of the ear to the tip of the nose (e. g. 48 cm for infants (Czarnecki & Kaucic, 1999)) Use Lubricant Do not apply suction during insertion of the catheter Suction applied intermittently during withdrawal from the naris while gently rotating Duration of suction no more than 15 seconds with 20 -30 seconds between each Suction should be done more than once in each naris Alter between nares to reduce tissue trauma Nasal suctioning should be between at 80 -120 mm. Hg (Moore, 2003). *The appropriate subatmospheric pressure to use when suctioning an infant is 80 -100 mm HG, and for a children is 100120 mm Hg (Bowden & Greenbury, 2008).
Document Post-suctioning assessment should include the type, tenacity, consistency and amount of secretions � Normal secretions are white and mucoid. � If the secretions are loose, copious in amount, pink, frothy or blood stained, this may indicate fluid overload (pulmonary edema). � Yellow or green secretions may indicate infection � Rusty-colored sputum may mean that the patient has pneumonia �
References � � � � � Bowden, V. , & Greenberg, C. (2008). Nasotracheal suctioning. In Pediatric Nursing Procedures (2 nd ed. , pp. 476 -481). Philadelphia: Lippincott Williams & Wilkins. Burglass E (1999) Tracheostomy care: tracheal suctioning and humidification. British Journal of Nursing. 8, 8, 500 -504 Czarnecki, M. , & Kaucic, C. (1999). Practice applications of research. Infant nasal-pharyngeal suctioning: is it beneficial? . Pediatric Nursing, 25(2), 193. Moore, T. (2003). Continuing professional development. Suctioning techniques for the removal of respiratory secretions. Nursing Standard, 18(9), 47 -55. Luce J et al (1999) Intensive Respiratory Care, Second edition Philadelphia PA, WB Saunders
- Slides: 10