Decipherin g the neuro logy of rare inborn
Decipherin g the neuro logy of rare inborn errors of metabolism with a focu s on organi c acidemias and fatty a cid oxidation d isorders Andrea Gro pman, M. D. , Professor, G FAAP, FACM eorge Wash G ington Univ ersity of the Health Scien Attending, C ces hildren’s Na tional Medic al Center
Goals 0 Discuss the major neurological features of FAOs and OAs 0 Seizures 0 Muscle disease 0 Developmental delay/MR
Fatty Oxidation Disorders (FODs) 0 Genetic disorders in which the body is unable to oxidize (breakdown) fatty acids to make energy 0 Enzyme deficiency 0 Inherited disorder
Fatty acid oxidation disorders 0 0 0 0 0 Medium-chain acyl-Co. A dehydrogenase (MCAD) deficiency Very-long-chain acyl-Co. A dehydrogenase (VLCAD) deficiency Short-chain acyl-Co. A dehydrogenase (SCAD) deficiency Multiple acyl-Co. A dehydrogenase (MAD) deficiency (= Glutaric aciduria type II, GA II) Long-chain hydroxyacyl-Co. A dehydrogenase (LCHAD) deficiency Trifunctional protein deficiency Carnitine palmitoyl-transferase I (CPT I) deficiency Carnitine palmitoyl-transferase II (CPT II) deficiency Carnitine acylcarnitine translocase deficiency Primary (systemic) carnitine deficiency
How does it cause symptoms 0 Energy from fat keeps us going when our bodies run low of their main source of energy, sugar (glucose) 0 Our bodies rely on fat when we don’t eat for a period of time such as an overnight fast 0 When an enzyme is missing or not working well, the body cannot use fat for energy and must rely solely on glucose
How does it cause symptoms 0 Glucose is a good source of energy but there is a limited amount available 0 Once the glucose is gone, the body tries to use fat without success 0 This leads to low blood sugar, called hypoglycemia, and to the build up of harmful substances in the blood
Fatty acid oxidation defects 0 Risk: cause recurrent disturbances of brain function 0 The neurological symptoms attributed to 0 Hypoglycemia 0 Hypoketonemia 0 Effects of potentially toxic organic acids 0 Symptoms occur during fasting
Fatty acid oxidation defects 0 Symptoms 0 0 Drowsiness Stupor and coma occur during acute metabolic crises Seizures Long term neurological effects 0 Muscle tone 0 Cognition/thinking
Organic acidurias: 0 Result From: 0 Deficiencies of mitochondrial enzymes that metabolize Co. A activated carboxylic acids 0 derived from amino acid breakdown. 0 Neurological Symptoms 0 Encephalopathy 0 Changes in level of consciousness 0 Seizures 0 Episodic metabolic acidosis 0 caused by build up of toxic metabolites 0 Disturbance of mitochondrial energy production
Organic acidurias 0 Treatment 0 Dietary restriction of the amino acids that cannot be broken down 0 Prevention protein catabolism 0 Supplementation with carnitine and or glycine to form less toxic intermediate conjugates 0 Supplementation with biotin/vitamin to act as a cofactor for mitochondrial carboxylase enzymes
Neurological complications 0 Fatty acid oxidation disorders 0 Hypotonia 0 Seizures 0 due to hypoglycemia 0 Developmental delay or mental retardation 0 Muscle disease 0 VLCAD 0 VLCHAD 0 Organic acidemias 0 Tone abnormalites 0 Hypotonia 0 Hypertonia 0 Seizures 0 Developmental delay or mental retardation 0 Movement disorders
Short and Long term Neurological consequences of FAOs and OAs 0 Hypotonia 0 0 Low muscle tone Results in delayed gross, fine and speech milestones Usually trunk muscles Improves with therapy
Short and Long term Neurological consequences of FAOs and OAs 0 Hypertonia 0 0 0 0 High resting muscle tone Muscles are contracted and stiff Prevents movements Using limb muscles Stretching therapies Medications Surgeries 0 Tendon releases and transfers
Short and Long term Neurological consequences of FAOs and OAs 0 Movement disorders 0 0 Fixed postures Interfere with purposeful movement Writhing or rapid movements May be induced by purposeful movement
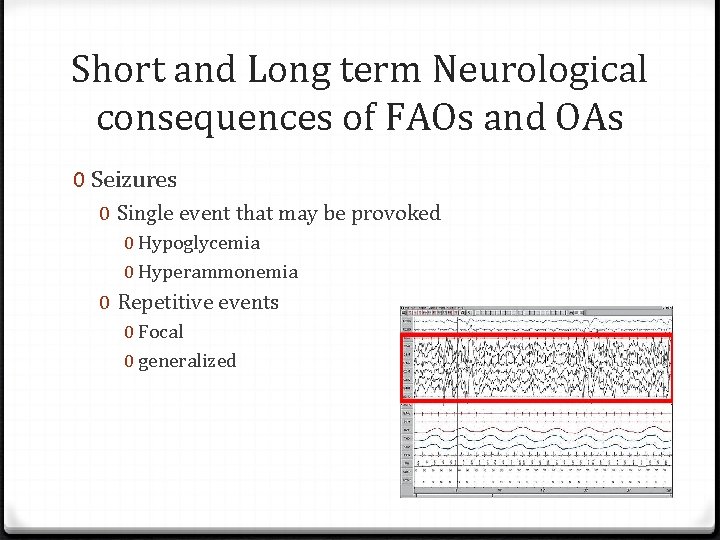
Short and Long term Neurological consequences of FAOs and OAs 0 Seizures 0 Single event that may be provoked 0 Hypoglycemia 0 Hyperammonemia 0 Repetitive events 0 Focal 0 generalized
Short and Long term Neurological consequences of FAOs and OAs 0 Developmental delay/mental retardation 0 Variable degrees 0 Disorder affects brain 0 Hypoglycemia 0 Seizures 0 Repeated injury
Short and Long term Neurological consequences of FAOs 0 Muscle weakness 0 At rest 0 After exercise
Hypotonia 0 Medical term used to describe decreased muscle tone 0 the amount of resistance to movement in a muscle 0 It is not the same as muscle weakness, although the two conditions can co-exist 0 Not a specific medical disorder 0 It can be a condition on its own or it can be associated with another problem where there is progressive loss of muscle tone
Hypotonia 0 Hypotonia can be caused by a variety of conditions 0 Central nervous system (brain and muscle) 0 Muscle disorders 0 Genetic disorders 0 It is usually first noticed during infancy 0 Floppy infant 0 Poor head control 0 Weak suck and swallow
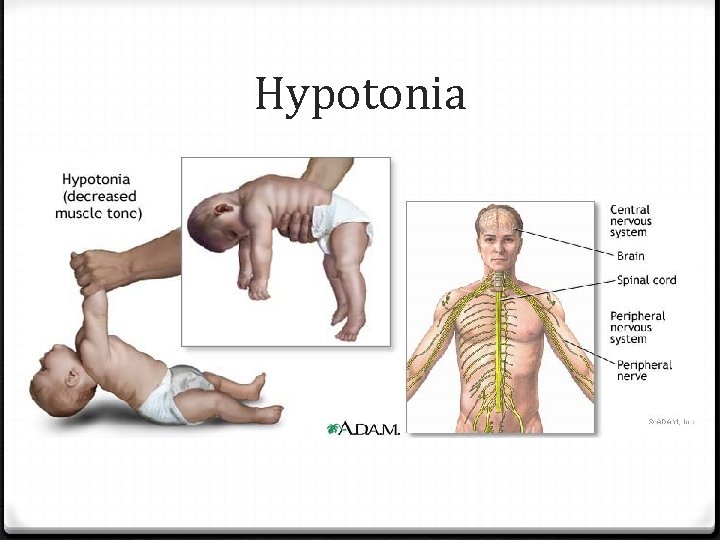
Hypotonia
Clinical aspects of hypotonia 0 Can involve only the trunk or trunk and extremities 0 Delayed Motor skills (requires strength and movement against gravity) 0 Hypermobile or hyperflexible joints 0 Drooling and speech difficulties
Clinical manifestations of hypotonia 0 Poor tendon reflexes 0 Decreased strength 0 Decreased activity tolerance 0 Rounded shoulder posture and curved back when sitting
Infantile hypotonia 0 Floppy, rag doll 0 Difficulty with feeding 0 Mouth muscles cannot maintain a proper suck-swallow pattern or a good breastfeeding latch 0 Hypotonic infants are late in 0 0 0 0 Lifting their heads while lying on their stomachs Rolling over Lifting themselves into a sitting position Sitting without falling over Balancing Crawling Walking independently
Hypotonia and motor delays 0 Delayed developmental milestones 0 degree of delay can vary widely 0 Motor skills are particularly susceptible to the lowtone disability
Hypotonia and motor delays 0 They can be divided into two areas 0 gross motor skills 0 fine motor skills 0 Fine motor skills delays 0 grasping a toy 0 transferring a small object from hand to hand 0 pointing out objects 0 following movement with the eyes 0 self feeding
Speech delays and hypotonia 0 Speak later than their peers 0 appear to understand a large vocabulary 0 can obey simple commands 0 Difficulties with muscles in the mouth and jaw 0 inhibit proper pronunciation 0 discourage experimentation with word combination and sentence-forming 0 Feeding difficulties 0 Chewing 0 Textures 0 Mouth play
Hypotonia versus weakness 0 The low muscle tone associated with hypotonia is often confused with low muscle strength 0 Muscle tone is the ability of the muscle to respond to a stretch 0 The child with low tone has muscles that are 0 slow to initiate a muscle contraction 0 contract very slowly in response to a stimulus 0 cannot maintain a contraction 0 Muscles remain loose and very stretchy
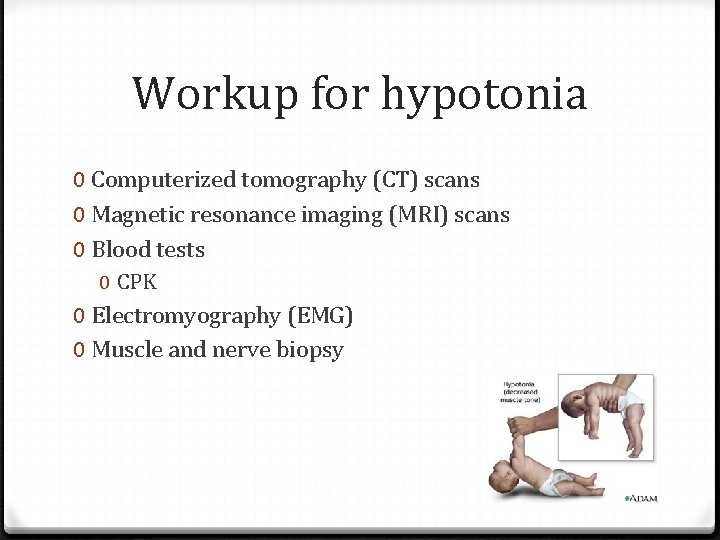
Workup for hypotonia 0 Computerized tomography (CT) scans 0 Magnetic resonance imaging (MRI) scans 0 Blood tests 0 CPK 0 Electromyography (EMG) 0 Muscle and nerve biopsy
Hypotonia 0 Often evaluated by physical and occupational therapists through a series of exercises designed to assess developmental progress, or observation of physical interactions 0 Hypotonic child has difficulty deciphering his spatial location 0 develop recognizable coping mechanisms 0 locking the knees while attempting to walk 0 tendency to observe the physical activity of those around them for a long time before attempting to imitate
Different names for hypotonia 0 Low Muscle Tone 0 Benign Congenital Hypotonia 0 Congenital Muscle Weakness 0 Amyotonia Congenita 0 Floppy Baby Syndrome 0 Infantile Hypotonia
Management and treatment 0 No known treatment or cure for most (or perhaps all) causes of hypotonia 0 The outcome depends on the underlying disease 0 In some cases, muscle tone improves over time 0 Patient may learn or devise coping mechanisms that enable him to overcome the most disabling aspects of the disorder
Management of hypotonia 0 If the underlying cause is known, treatment is tailored to the specific disease, followed by symptomatic and supportive therapy for the hypotonia 0 In very severe cases, treatment may be primarily supportive
Management of hypotonia 0 Physical therapy can improve fine motor control and overall body strength 0 Occupational therapy to assist with fine motor skill development and hand control, and speech-language therapy can help breathing, speech, and swallowing difficulties 0 Therapy for infants and young children may also include sensory stimulation programs 0 Ankle/foot orthoses are sometimes used for weak ankle muscles 0 Toddlers and children with speech difficulties may benefit greatly by using sign language or picture exchange
Hypotonia 0 Diagnostic tests 0 CT or MRI scan of the brain 0 EMG to evaluate nerve and muscle function 0 EEG to measure electrical activity in the brain may also be necessary
Treatment 0 Once a diagnosis has been made 0 underlying condition is treated first 0 followed by symptomatic and supportive therapy for the hypotonia
Hypertonia 0 Abnormal increase in the tightness of muscle tone 0 Reduced ability of a muscle to stretch 0 increased stiffness 0 Accompanied by spasticity
Causes of hypertonia 0 Damage to upper motor neurons 0 Causes hypertonia 0 Spasticity (overactive reflexes) 0 Rigidity (constant muscle contractions)
Hypertonia 0 Other names for hypertonia 0 0 0 Cerebral palsy Hemiparesis Quadriparesis Hemiplegia Diplegia
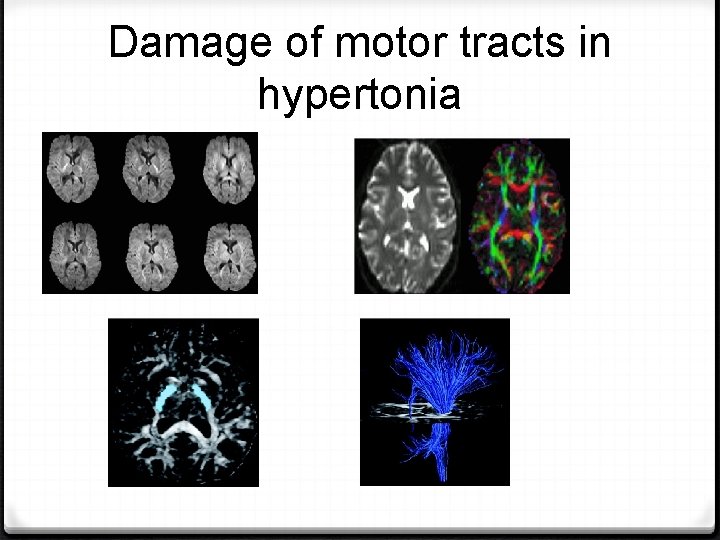
Damage of motor tracts in hypertonia
Hypertonia • Diagnostic tests – CT or MRI scan of the brain – EEG to measure electrical activity in the brain may also be necessary
Diagnosis of hypertonia
Management of hypertonia • Physical therapy can encourage stretching and prevent contractures • Occupational therapy to assist with fine motor skill development and hand control, and speech-language therapy can help breathing, speech, and swallowing difficulties • Ankle/foot orthoses are used to prevent contractures at the heel cords • Toddlers and children with speech difficulties may benefit greatly by using sign language or picture exchange
Spells, seizures, and epilepsy 0 The medical syndrome of recurrent, unprovoked seizures is termed epilepsy 0 A single seizure is not yet epilepsy 0 A “spell” may be a seizure or may be something else 0 Movement disorder 0 GERD 0 Sleep disorder
Things that go bump in the night: Spells, seizures, and epilepsies 0 A seizure 0 Temporary abnormal electrophysiologic phenomenon of the brain 0 Results in abnormal synchronization of electrical neuronal activity 0 Can manifest as 0 Alteration in mental state/awareness 0 Tonic or clonic movements 0 Convulsions 0 Various other psychic symptoms (such as déjà vu or jamais vu
Seizures 0 Cause involuntary changes in 0 0 0 body movement Function Sensation Awareness behavior 0 Can last from 0 few seconds 0 status epilepticus, a continuous seizure that will not stop without intervention 0 Seizure is often associated with a sudden and involuntary contraction of a group of muscles
Seizures 0 A seizure can also be as subtle as 0 0 0 Marching numbness of a part of the body A brief loss of memory Sparkling or flashes Sensing an unpleasant odor A strange sensation in the stomach Sensation of fear
Seizures 0 Seizures are typically classified as 0 0 Motor Sensory Autonomic Emotional/cognitive
Seizures 0 Symptoms depend on where in the brain the disturbance in electrical activity occurs 0 In children, seizures often happen in sleep or the transition from sleep to wake 0 A person having a tonic-clonic seizure may cry out, lose consciousness and fall to the ground, and convulse, often violently
Seizures 0 Complex partial seizure 0 Person may appear confused or dazed 0 not be able to respond to questions or direction 0 Sometimes, the only clue that a person is having an absence seizure 0 Rapid blinking 0 Mouthing movements 0 Few seconds of staring into space
Hypoglycemia and seizures 0 Hypoglycemia 0 Lower than normal level of glucose (sugar) in the blood 0 Why is this important? 0 Brain metabolism depends primarily on glucose for fuel in most circumstances 0 A limited amount of glucose can be made from glycogen stored in astrocytes, but it is used up within minutes 0 Brain is dependent on a continual supply of glucose diffusing from the blood into central nervous system and into the neurons themselves
Hypoglycemia 0 Caused by a continuing demand for glucose by brain and other organs 0 Results from the primary biochemical defect of fattyacid oxidation since fats cannot be broken down efficiently 0 Treatment 0 Avoidance of catabolism (more break down) 0 Requires the use of fatty acids except in FAOs 0 L-Carnitine supplementation 0 Some patients may benefit from medium-chain triglyceride supplementation as a source of fat
Hypoglycemia and seizures 0 If the amount of glucose supplied by the blood falls, the brain is one of the first organs affected 0 In most people, reduction of mental abilities occur when the glucose falls below 65 mg/dl (3. 6 m. M)
Hypoglycemia and seizures 0 Impairment of action and judgement usually becomes obvious below 40 mg/dl (2. 2 m. M) 0 Seizures may occur as the glucose falls further 0 As blood glucose levels fall below 10 mg/dl (0. 55 m. M), most neurons become electrically silent and nonfunctional, resulting in coma
Hypoglycemia and seizures 0 Brief or mild hypoglycemia produces no lasting effects on the brain 0 Can temporarily alter brain responses to additional hypoglycemia 0 Prolonged, severe hypoglycemia can produce lasting damage of a wide range 0 Impairment of cognitive function, motor control, or even consciousness
Hypoglycemia and seizures 0 The likelihood of permanent brain damage from any given instance of severe hypoglycemia is difficult to estimate 0 Depends on a many factors 0 0 0 Age Underlying disorder Recent blood and brain glucose concurrent Problems such as hypoxia Availability of alternative fuels
Hypoglycemia, symptoms 0 Abnormal thinking, impaired judgement 0 anxiety, moodiness, depression, crying 0 irritability, combativeness 0 Personality change, emotional lability 0 Fatigue, weakness, apathy, lethargy, daydreaming, sleep 0 Confusion, amnesia, dizziness, delirium 0 Staring, "glassy" look, blurred vision, double vision
Hypoglycemia, symptoms 0 Automatic behavior, also known as automatism 0 Difficulty speaking, slurred speech 0 Ataxia, incoordination, sometimes mistaken for "drunkenness" 0 Focal or general motor deficit, paralysis, hemiparesis 0 Paresthesia, headache 0 Stupor, coma, abnormal breathing 0 Generalized or focal seizures
Management of hypoglycemic seizures 0 Failure to administer glucose would be harmful to the patient 0 Recurrent seizures 0 Anti-epilepsy drugs 0 Give single drug at lowest concentration if possible 0 Careful with certain conditions 0 Drug treatment geared towards whether focal, generalized, etc. 0 Trileptal, Keppra, Zonergran, Lamictal, Depakote, Klonopin, Dilantin, Tegretol
Movement disorders-Organic acidemias 0 Dystonia 0 Abnormal fixed posture of an extremity (arms or legs, neck) 0 sustained muscle contraction 0 resulting in abnormal posture 0 Chorea 0 Fast, dance like movements of the distal extremities (fingers and toes) 0 Athetosis 0 Slow, writhing movements of the extremities
Movement disorders-Organic acidemias 0 Patient may have combination of movement disorders at baseline or with special circumstances 0 Stress 0 Illness 0 Attempt at purposeful movement
FAOs and Muscle disease 0 SCAD 0 VLCAD 0 LCHAD 0 Symptoms 0 0 0 Weakness Pain/cramps Exercise intolerance Red urine Muscle breakdown rhabdomyolysis
Rhabdomyolysis 0 Elevations of CPK
FAOs with muscle disease 0 SCAD 0 Hypotonia 0 metabolic acidosis 0 NBS: 0 elevated C 4 0 UOA have elevated ethylmalonic acid 0 Common mild variants of ? Significance
FAOs with muscle disease 0 LCHAD 0 0 0 Cardiomyopathy hypotonia, rhabdomyolysis moms have HELLP syndrome NBS 0 Acylcarnitine profile with elevated C 14 -OH, C 16 -OH , C 18 OH and C 18: 1 -OH
FAOs with muscle disease 0 VLCAD 0 0 0 Cardiomyopathy hepatomegaly, SIDS Rhabdomyolysis Acylcarnitine profile: 0 Elevations of C 14: 1 and C 14: 1/ C 12: 1
General management guidelinesmedical 0 Fatty acid oxidation 0 Provide brain fuel 0 Glucose 0 Calories 0 Sick day management 0 Organic acidurias 0 Provide brain fuel 0 Calories 0 Glucose and nonprotein/fat 0 Sick day management
General management guidelinesmedical 0 Malignant hyperthermia 0 Risk with anesthesia for surgery 0 G tube 0 Orthopedic surgery to correct hypertonia 0 Dental work 0 Etc.
Management of metabolic disorders 0 Mechanical assistance with basic life functions 0 breathing and feeding 0 physical therapy to prevent muscle atrophy and maintain joint mobility 0 Treatments to improve neurological status 0 medication for a seizure disorder 0 medicines or supplements to stabilize a metabolic disorder 0 surgery to help relieve the pressure from hydrocephalus (increased fluid in the brain).
General management guidelinestherapies 0 Physical therapy 0 Large muscles, gross motor skills 0 Occupational therapy 0 Fine motor skills 0 Speech therapy 0 Speech articulation, communication 0 Feeding therapy 0 May be done by either speech or occupational therapist
Metabolic crisis 0 extreme sleepiness 0 behavior changes 0 irritable mood 0 poor appetite 0 Other symptoms then follow: 0 fever 0 nausea 0 diarrhea 0 vomiting 0 hypoglycemia
Consequences of metabolic crises 0 0 0 0 If a metabolic crisis is not treated, a child with CTD can develop: • breathing problems • swelling of the brain • seizures • coma, sometimes leading to death Babies who are not treated may have other effects: • enlarged heart • enlarged liver • muscle weakness • anemia Repeated episodes of metabolic crisis can cause brain damage. This can result in learning problems or mental retardation. Symptoms of a metabolic crisis often happen after having nothing to eat for more than a few hours. Symptoms are also more likely when a child with CTD gets sick or has an infection.
Thank you f or your attenti on Questions? ? ?
- Slides: 72