Death as Data Autopsy and the Death Certificate

- Slides: 29
Death as Data: Autopsy and the Death Certificate Two basic goals u value of the autopsy u proper use of the death certificate
Essential websites and URLS n Bruce. case@mcgill. ca National Association of Medical Examiners Death Certificate Tutorials: http: //www. thename. org/Cause. Death/main. htm A Canadian angle: 1998 article from the Canadian Medical Association Journal: http: //www. cma. ca/cmaj/vol-158/issue-10/1317. htm
Outline n Autopsy: history in three periods; n The fall of the autopsy: 1960 onward n Evidence of continuing relevance n Some attempts to explain the problem n Effects of falling rates n An example of the effect n Death certificate: what it is, how it should be approached
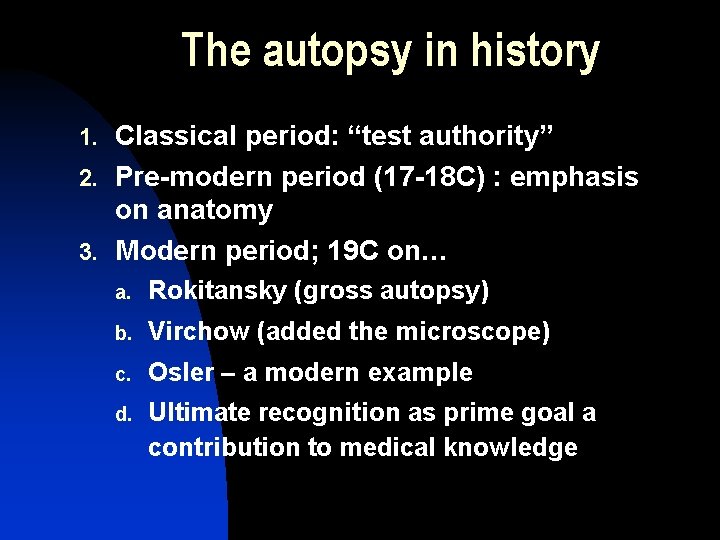
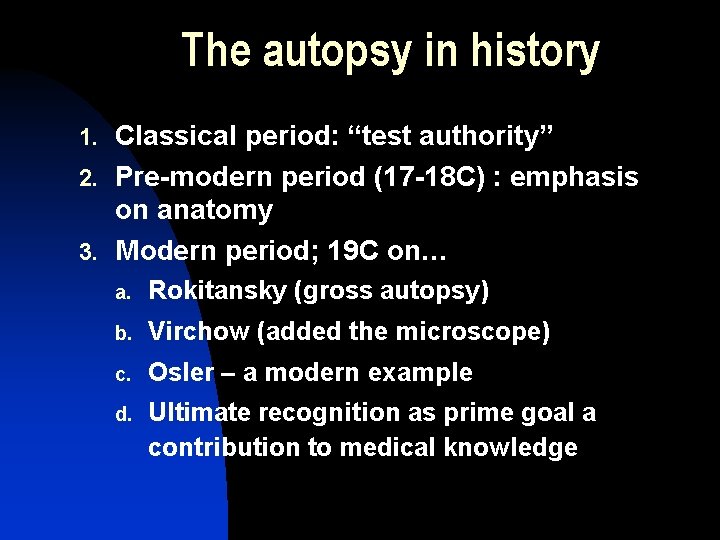
The autopsy in history 1. Classical period: “test authority” 2. Pre-modern period (17 -18 C) : emphasis on anatomy 3. Modern period; 19 C on… a. Rokitansky (gross autopsy) b. Virchow (added the microscope) c. Osler – a modern example d. Ultimate recognition as prime goal a contribution to medical knowledge
Falling Autopsy Rates 1. 2. 3. From 50% in the 1960’s to Much lower than 10% today, despite (for example) of three U. S. studies, an incorrect diagnosis of malignant tumors was shown in a. b. c. 36. 5% of cases (1923) 41% of cases (1972) 44% of cases (1998, Louisiana)
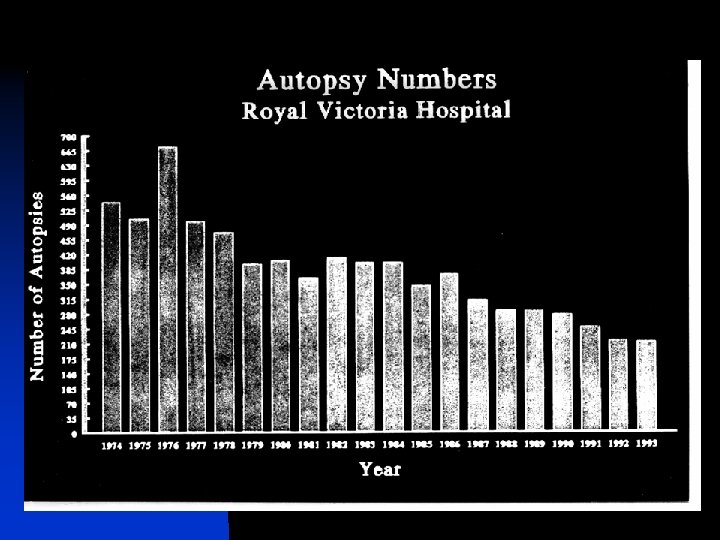
Falling Autopsy Rates: RVH 1998 DEATHS AUTOPSIE S RATE (%) ADULT INPATIENTS 721 92 12. 8% EMERGENC Y 43 3 7% INFANTS (OVER 500 g) 19 12 63% (figures from 1998)
JAMA 1998: Louisiana study 1. All autopsies 1986 -95 2. Outcome measure: discordance in clinical vs. autopsy for cancer 3. 1105 cases; mean age 48 years (very atypical) 4. 443 “neoplasms” at autopsy; 250 “malignant” 5. 111 wrong CLINICAL diagnoses of “malignancy” including 57 which caused death
So what is wrong? 1. Why do the rates keep falling in the face of continuing evidence of error? 1. Increasing reliance on imaging 2. Fear of lawsuits? May explain USA but not elsewhere
So what is wrong? 2. Changing patterns in pathology 1. Changing patterns in pathology and pathologists 2. A new but worrying factor: regard for autopsy practices as “violating civil rights” (lawsuit in UK over pediatric autopsies); reflects a constant fight over “values” over the years coupled with some abuses such as “Burking”…
So what is wrong? 3. Poor communication 5. Suggestions of poor communication between pathologists and clinicians: a. Wherever a special effort is made to “educate” rates increase, although this may be transitory. Rates can reach 100% in some centres!
So what is wrong? 4. 5. Suggestions of poor communication between pathologists and clinicians: b. Poor pay, lack of curiosity, lack of professional attitude to reporting can lead to “vicious circle” of late reporting; c. Clinical “mortality rounds” seem to result in higher rates when pathologists attend
Is anything right? 1. In academic centres cases with unknown cause still invoke requests for autopsy; 2. This means that almost every increasingly “rare autopsy” has become more “interesting” both for the pathologist, for teaching, and for publication, BUT. . . 3. This applies only to academic centres
Effects of falling rates 1. Similar to effects of bad death certificate reporting 2. National health statistics wrong; 3. Lack of Quality Control; 4. Problems for analytical epidemiology (garbage in, garbage out)
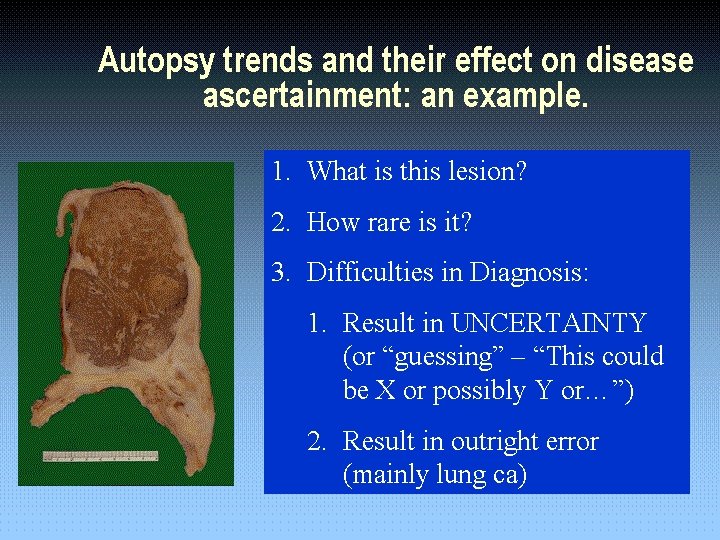
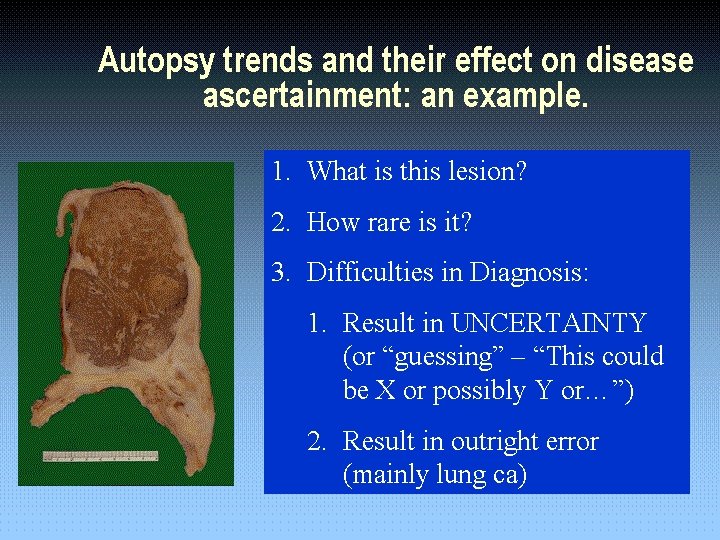
Autopsy trends and their effect on disease ascertainment: an example. 1. 1. What is this lesion? 2. 2. How rare is it? 3. 3. Difficulties in Diagnosis: 4. 1. Result in UNCERTAINTY (or “guessing” – “This could be X or possibly Y or…”) 1. 2. Result in outright error (mainly lung ca)
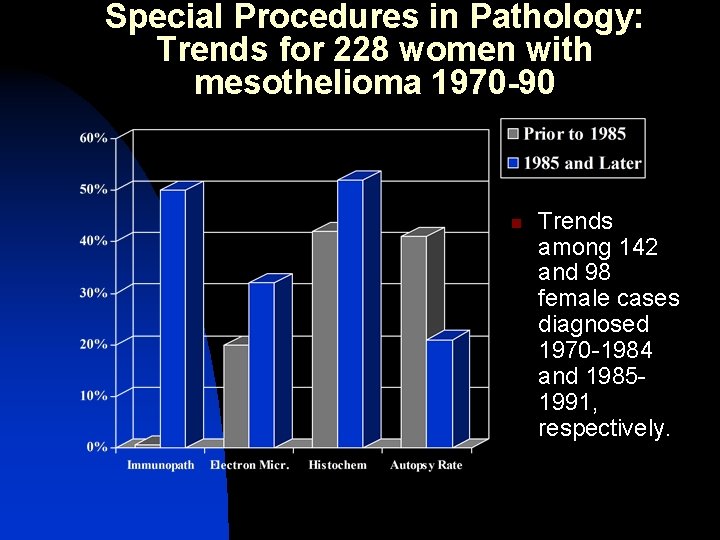
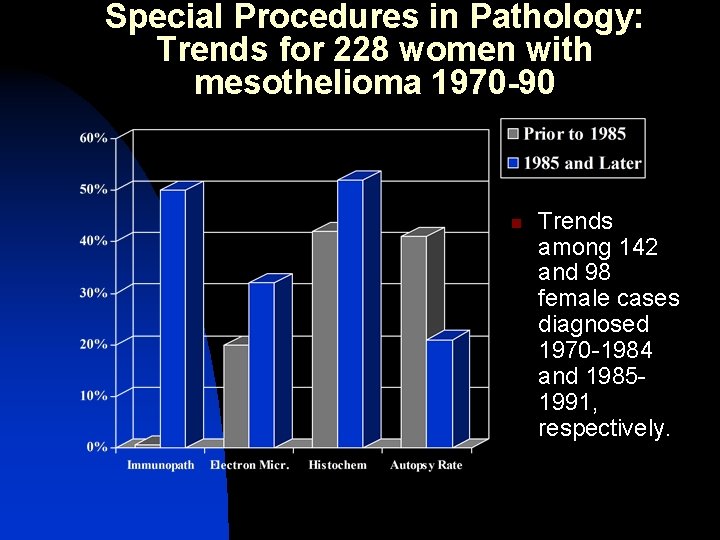
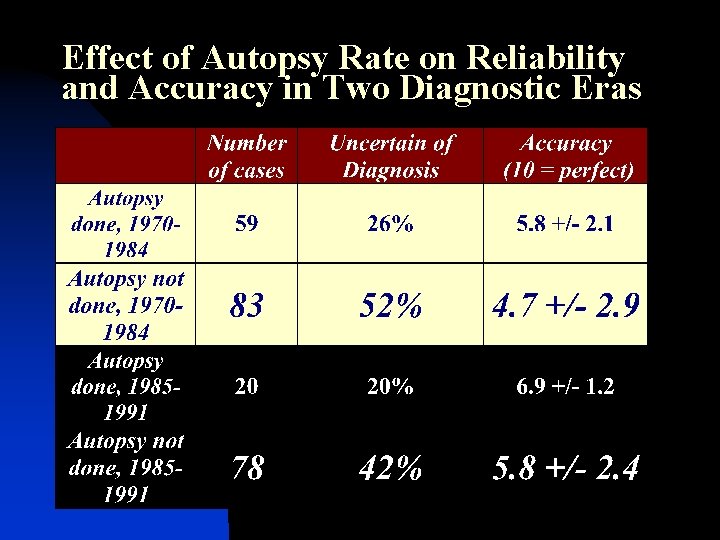
Special Procedures in Pathology: Trends for 228 women with mesothelioma 1970 -90 n Trends among 142 and 98 female cases diagnosed 1970 -1984 and 19851991, respectively.
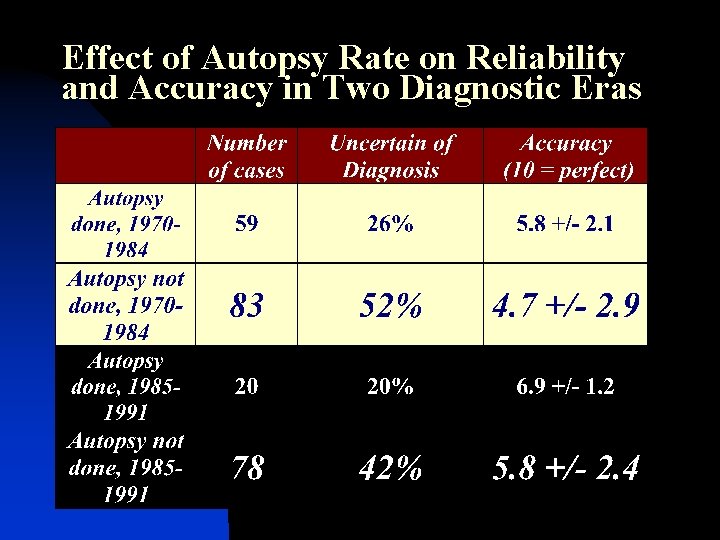
Effect of Autopsy Rate on Reliability and Accuracy in Two Diagnostic Eras
CMAJ ARTICLE 1. “Improving the accuracy of death certification” Eight case scenarios are presented Kathryn A. Myers, MD, Ed. M; Donald R. E. Farquhar, MD, SM CMAJ 1998; 158: 1317 -23
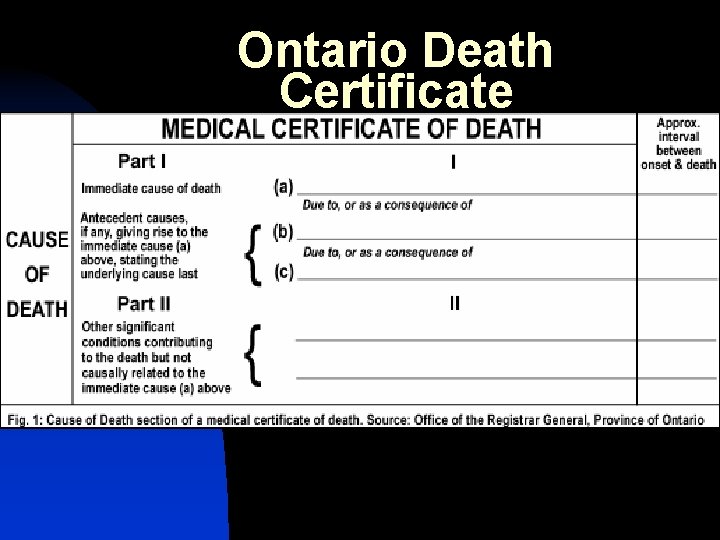
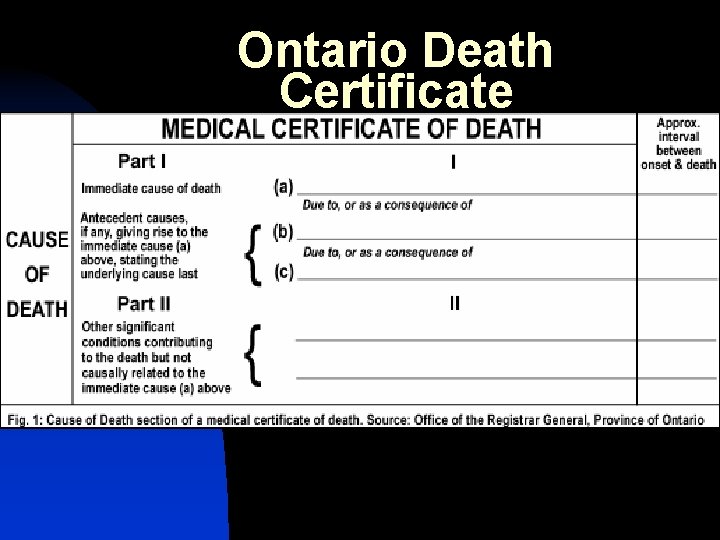
Ontario Death Certificate
2. WRITING CAUSE-OFDEATH STATEMENTS An On-Line Tutorial http: //www. thename. org/Cause. Dea th/main. htm

Why learn this now? n n n Often, a physician's first encounter with the death certificate occurs upon the physician's first patient death when he/she is handed the death certificate form and asked to complete it. This usually occurs during the first year of residency. Many, perhaps most, are not told “how” – and never learn!
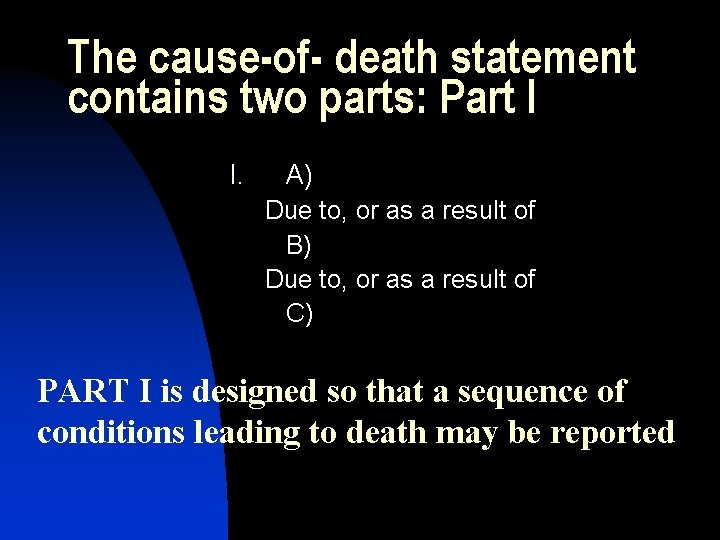
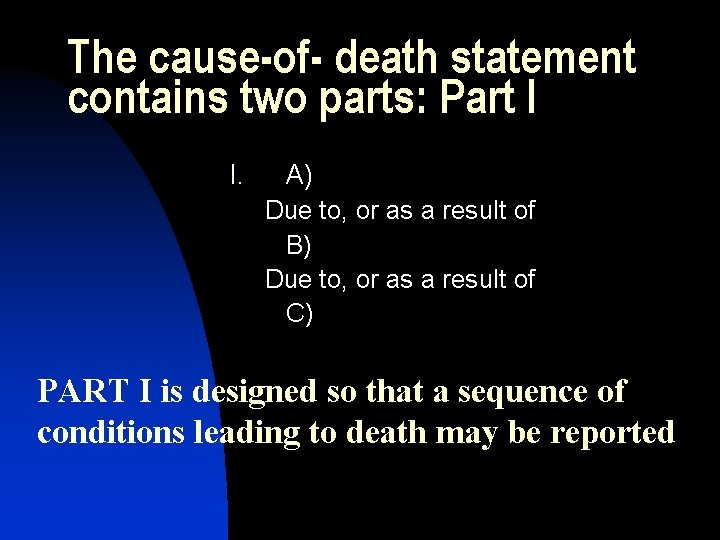
The cause-of- death statement contains two parts: Part I I. A) Due to, or as a result of B) Due to, or as a result of C) PART I is designed so that a sequence of conditions leading to death may be reported
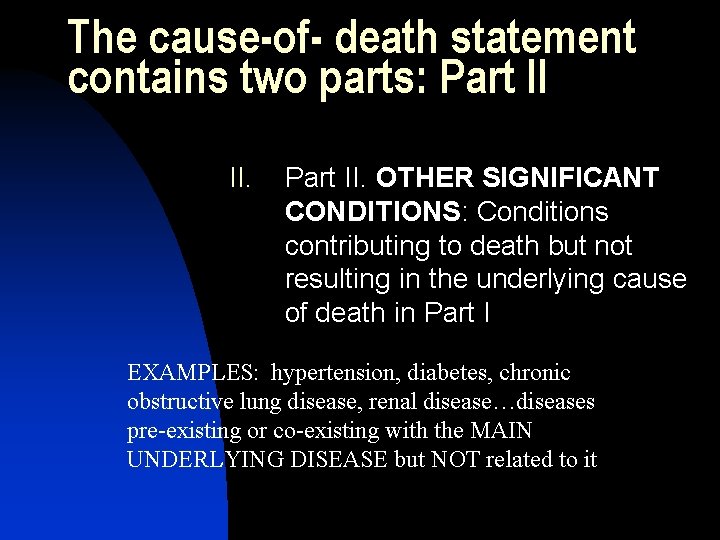
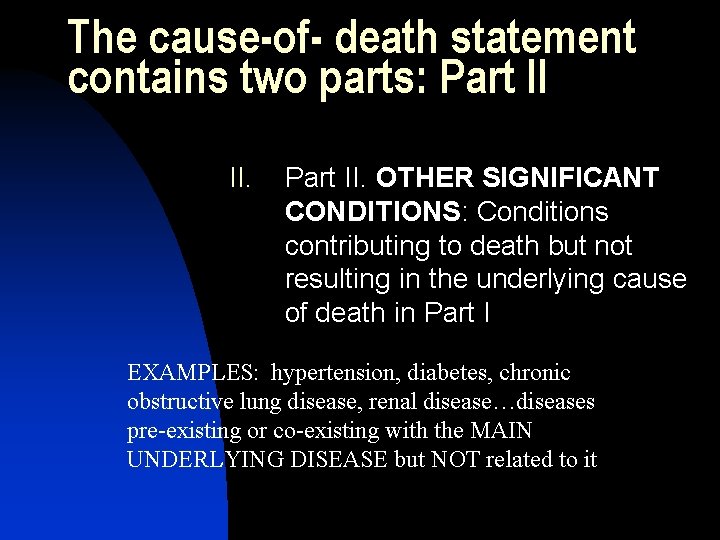
The cause-of- death statement contains two parts: Part II II. Part II. OTHER SIGNIFICANT CONDITIONS: Conditions contributing to death but not resulting in the underlying cause of death in Part I EXAMPLES: hypertension, diabetes, chronic obstructive lung disease, renal disease…diseases pre-existing or co-existing with the MAIN UNDERLYING DISEASE but NOT related to it
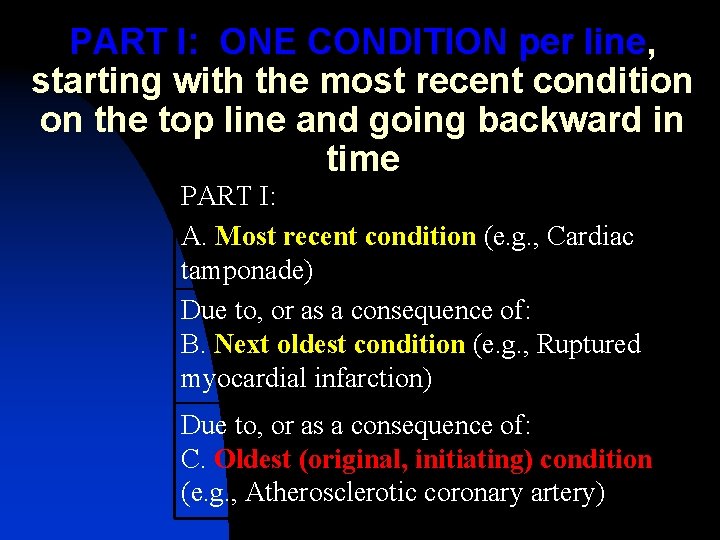
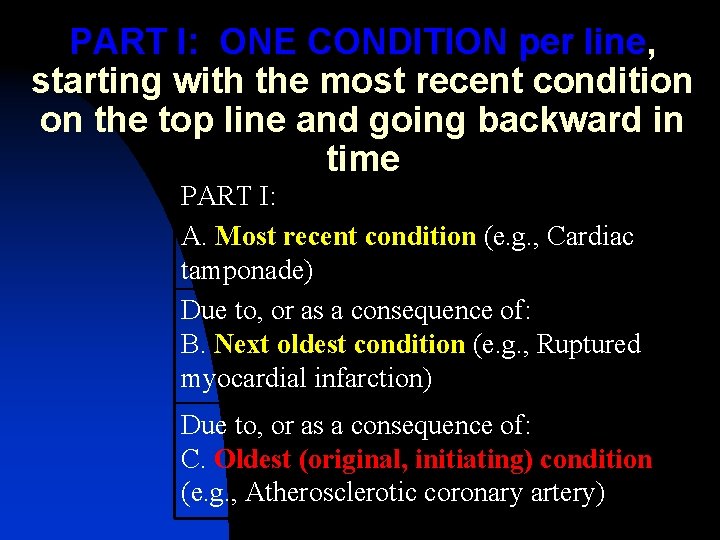
PART I: ONE CONDITION per line, starting with the most recent condition on the top line and going backward in time PART I: A. Most recent condition (e. g. , Cardiac tamponade) Due to, or as a consequence of: B. Next oldest condition (e. g. , Ruptured myocardial infarction) Due to, or as a consequence of: C. Oldest (original, initiating) condition (e. g. , Atherosclerotic coronary artery)
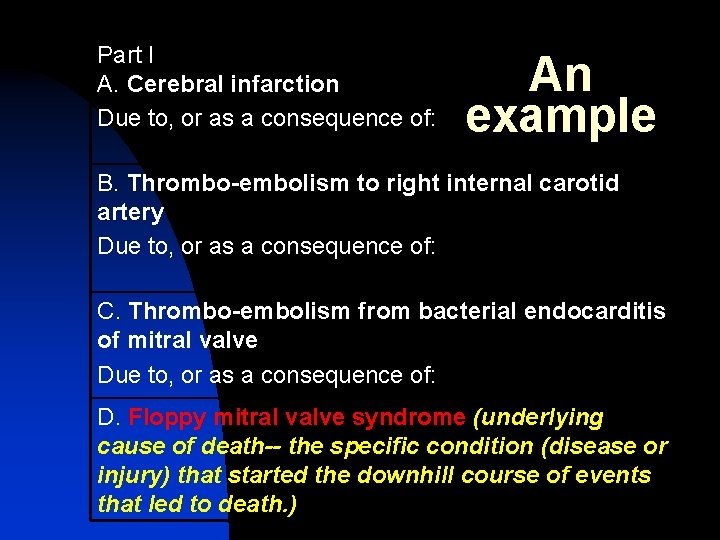
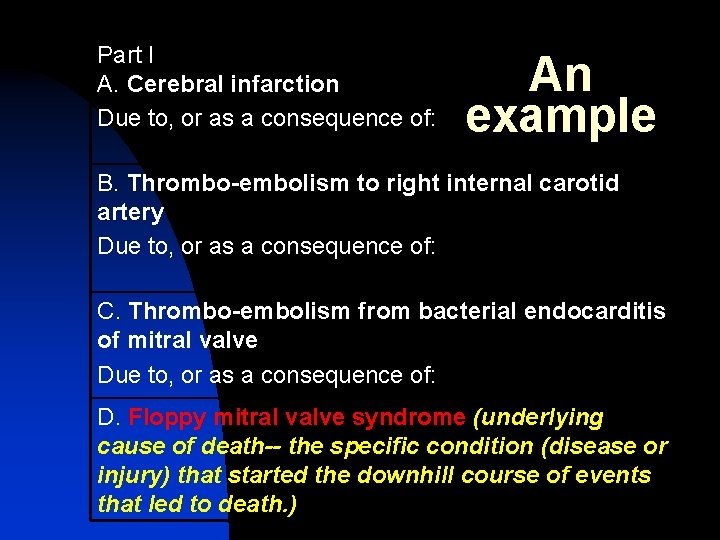
Part I A. Cerebral infarction Due to, or as a consequence of: An example B. Thrombo-embolism to right internal carotid artery Due to, or as a consequence of: C. Thrombo-embolism from bacterial endocarditis of mitral valve Due to, or as a consequence of: D. Floppy mitral valve syndrome (underlying cause of death-- the specific condition (disease or injury) that started the downhill course of events that led to death. )
Variants; problems n n Single Line Part I Format (missing data) e. g. no autopsy, patient dies at home, known to have prostate carcinoma uncertainty or presumption: use “probable” ALWAYS REPORT CANCER! Can “cheat” on part two to record risk factor (smoking, asbestos exposure)
Additional Information on the Death Certificate 1. 2. 3. 4. Usually a space to record TIME since onset of event Always indicate whether (a) an autopsy has been asked for and (b) whether the DC includes autopsy information In some places, can record occupation – “retired” is NOT an occupation!!! Mandatory reporting: violent death, certain infections; varies with state
Multiple cause-ofdeath coding 1. 2. 3. All data to date are based on a SINGLE cause of death but Modern national statistics programs record ALL information on the death certificate and can derive “multiple cause-of-death” data
http: //www. thename. org/Cau se. Death/main. htm (This is the web address for the tutorial on death certificates)