DDimer Clinical significance and application n Ddimer is



- Slides: 15
D--Dimer Clinical significance and application
n D-dimer is a specific degradation product produced by fibrin monomer crosslinked by activating factor XIII and then hydrolyzed by plasmin. It is a specific marker of fibrinolysis process. D-dimer is derived from cross-linked fibrin clot dissolved by plasmin.
n n n Normal range qualitatively negative; Quantification is less than 200μg/L.
Clinical significance n n D dimer mainly reflects the fibrinolytic function. Increased or positive is seen in secondary fibrinolytic hyperfunction, such as hypercoagulable state, diffuse intravascular coagulation, kidney disease, organ transplant rejection, thrombolytic therapy, etc. As long as there is activated thrombosis and fibrinolytic activity in the blood vessels of the body, D-dimer will increase. Myocardial infarction, cerebral infarction, pulmonary embolism, venous thrombosis, surgery, tumors, diffuse intravascular coagulation, infection and tissue necrosis can all lead to increased D-dimer. Especially for the elderly and hospitalized patients, due to bacteremia and other diseases, it is easy to cause coagulation abnormalities and lead to increased D-dimer.
The clinical significance and clinical application of D-dimer determination n n Determination of the main factors of the fibrinolytic system is of great significance for the diagnosis and treatment of fibrinolytic system diseases (such as DIC, various thrombosis) and fibrinolytic systemrelated diseases (such as tumors, pregnancy syndrome), as well as thrombolytic therapy monitoring. n The increased level of fibrin degradation product D indicates that there are frequent fibrin degradation processes in the body. Therefore, fiber D-dimer is a key indicator of deep vein thrombosis (DVT), pulmonary embolism (PE), and diffuse intravascular coagulation (DIC). 。
Fibrinolytic system and the formation mechanism of D dimer Fibrinolytic system in the body: Under the action of plasmin activating enzyme, it dissolves fibrin and fibrinogen, deposits some fibrin in blood vessels and removes the microfibrin that has settled in blood vessels. Normal people maintain a dynamic balance between plasmin and inhibitory enzymes, so that blood circulation can proceed normally. In a pathological state, when the body undergoes coagulation, thrombin acts on fibrin and transforms it into cross-linked fibrin. At the same time, the fibrinolytic system is activated and degrades to form various FDP fragments. The r chain can connect two fragments containing D fragments to form a D-dimer. The increase of D-dimer indicates that fibrinolytic activity is enhanced, indicating that there is frequent fibrin degradation process in the body.
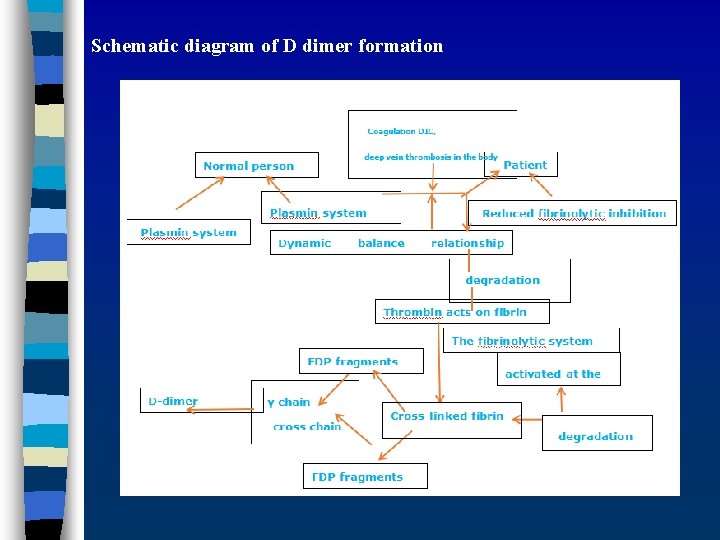
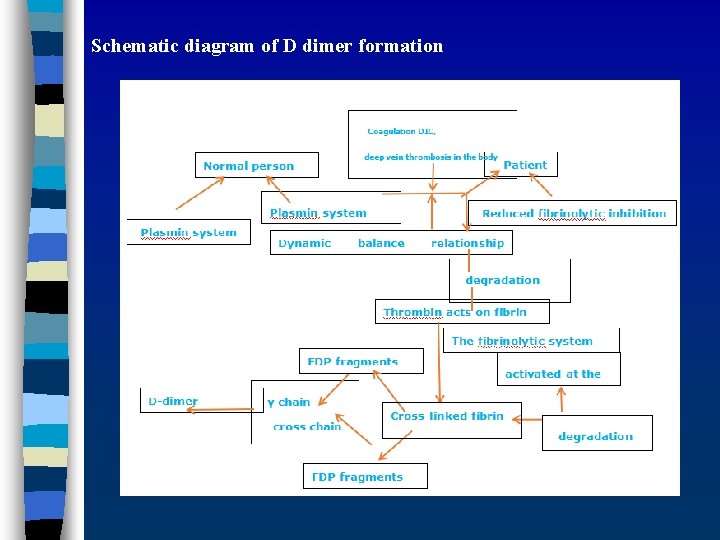
Schematic diagram of D dimer formation
3 P test Qualitative test of FDP fragment X and soluble fiber monomer FM compound. After the addition of protamine sulfate, the X fragments dissociated from the monomer, and the FM polymerized into fibrin filaments immediately, which was a jelly-like substance, which was positive for the 3 P test. Disadvantages of this test: The sensitivity is poor, the positive rate of DIC is 30 -69%; it can only be qualitative but not quantitative, and the test time is long; there are many interfering factors: poor blood sampling and hemolysis can affect the results. The test is now replaced by D-dimer.
D-dimer determination Latex agglutination method: simple and fast, but low sensitivity, qualitative or semi-quantitative. ELISA: Sensitivity, high energy quantification, cumbersome operation, long time, unable to meet emergency requirements. Immunofiltration method: high sensitivity, quantitative, fast and simple. The test range (0. 1 -20 mg/L) is of diagnostic value for secondary hyperfibrinolysis. Reference value <0. 3 mg/L; close to or > 0. 3 mg/l disease state should be considered.

Clinical application of D-dimer detection 1. Early diagnosis of DIC The level of D-dimer in DIC patients has increased significantly. It is more helpful for subclinical DIC diagnosis. 2. Screening for Deep Vein Thrombosis (DVT) Negative plasma D-dimer can rule out the possibility of DVT. The radiography confirmed that D-dimer was 100% positive in DVT patients. It can be used for medication guidance and efficacy observation for thrombolytic therapy and heparin anticoagulation. D-dimer can reflect the change of thrombus size. If the content increases again, it indicates that the thrombus will reoccur; it continues to be high during the treatment period, and the size of the thrombus does not change, indicating that the treatment is invalid. Old thrombosis does not increase. 3. Pulmonary embolism patients The level of D-dimer rises to varying degrees. After treatment with tissue plasmin and activator (t-PA), Ddimer rises rapidly, which can understand the patient's fibrinolytic state and guide heparin treatment. 4. Coronary heart disease Patients with unstable angina pectoris are higher than acute angina pectoris. D-dimer is increased during thrombolytic therapy in AMI patients, which is of great significance for thrombolytic therapy. 31% of preeclampsia, D-dimer increased, with clinical symptoms and precocious fetus, D-dimer can assist in diagnosis and guide treatment. Patients with hepatitis B (e. Ag+) have increased D-dimer and are related to the severity of the disease. In addition, cerebral thrombosis, chronic nephritis, etc. have different degrees of increase.
The relationship between D-dimer and malignant tumor n A large amount of literature shows that tumors can cause an increase in the concentration of Ddimer in patients, and can be used as a criterion for staging and prognosis. Masatoshi Oya et al. found in a study that the D-dimer of patients with colorectal cancer was significantly higher than that of patients with benign diseases, and the preoperative D-dimer was positively correlated with the pathological results and stage of the tumor. Patients with high preoperative D-dimer levels have significantly shorter postoperative survival than those with low D-dimer levels (16)。 n Kong Rong (17) and others performed D-dimer determination on 128 patients with malignant tumors. The results showed that: the acute leukemia group, malignant lymphoma group, and solid tumor group were significantly higher than the control group. There are significant differences (P<0. 05), the remission period is significantly lower than the initial stage (P<0. 05); the level of D-dimer varies in the malignant lymphoma group with different stages, and the solid tumor metastasis group is significantly higher than the non-metastatic group. The ratio difference is significant (P<0. 01). Osamu Taguchi et al. (18) divided all patients with lung cancer into two groups according to the median value of 150 mg/ul of D-dimer for all patients. The survival rate of the high D-dimer group was lower than that of the low D-dimer group, and This predictor excludes the influence of tumor stage, tissue type, and tumor size on survival (19). It is speculated that the hypercoagulable state in tumor patients is related to the tissue factor-dependent exogenous pathway and non-tissue factorrelated tumor procoagulation. The exogenous pathway is thought to be activated by the host's monocytes or vascular endothelial cells (19, 20). Non-tissue factor-related tumor procoagulant effect is considered to be a direct activator of factor X Urokinase plasminogen acticator activates fibrinolysis is another feature of tumors (21). The u-PA secreted by tumor stromal cells is bound by u-PA receptors on the surface of tumor cells, which not only activates plasminogen, but also causes fibrosis. Protein degradation; and activation of proteolytic enzymes, causing matrix decomposition at the tumor host interface, causing tumor metastasis and invasion (22 n n n
D—The relationship between dimer and detection in liver disease n n In liver disease, the content of plasma D-dimer is significantly increased, and it is positively correlated with the severity of liver disease (30) Wilder et al. measured 59 cases of acute and chronic liver disease with plasma D-dimer, 48 of which were different Increase in degree (31) Kruskal et al. measured D dimer in patients with various liver diseases and found that the level of D dimer in patients was in the order of severe hepatitis group> cirrhosis group> chronic hepatitis group, severe group> acute liver group> chronic hepatitis group. It is related to the damage to the anticoagulant system. Antiplasmin and AT-III are synthesized by the liver. When liver disease, their synthesis is reduced, causing hyperfibrinolysis. Fibrin and fibrinogen are degraded under the activation of plasmin, and its degradation product D -Dimers etc. are significantly increased, so the concentration of D-dimer can be used as a sign to judge the degree of liver damage.

The significance of D-dimer in other diseases n Many diseases cause the activation of the coagulation system and/or fibrinolytic system in the body, thereby causing the increase of D-dimer level, and this activation is closely related to the disease stage, severity and treatment of the disease, so in these diseases Detecting the level of D-dimer can be used as a marker for disease staging, prognosis and treatment.
Summary n D-dimer-positive DVT patients are sensitive to anticoagulation and thrombolysis, and have good short-term curative effects, but DVT is prone to relapse. DVT patients with negative D-dimer are generally sensitive to anticoagulation and thrombolysis, but the recurrence rate is low after DVT is cured. Therefore, from this perspective, if conditions are available, check this indicator after DVT is diagnosed. Guide treatment and judge prognosis.
