Data Quality From Clinical Assessment Protocols and Outcome

- Slides: 42
Data Quality: From Clinical Assessment Protocols and Outcome Scales to Care Planning • Please put your speaker phone on mute (*6) • Do not put your phone on hold ! • Your screen should show a Participants panel and a Chat panel • If not, go into the panel menu by clicking the green tab • Then click on the Participants icon to open the Participant box and the Chat icon to open the Chat box • To ask a question during the Web. Ex, write it out in the Chat box and select “send to all participants
Agenda • The benefits of using the inter. RAI CHA CAPs and Outcome Scales to enhance the care planning process – Review of selected resources in the inter. RAI CAPs manual and care planning binder – Share some tips on how to create a care plan – Discuss short care planning scenarios • Share examples of how HSPs have incorporated the CAPs and Outcome Scales into their daily work flow
Objectives • Understand the impact of using the CAPs and Outcome Scales when creating individualized care/service plans • How to incorporate CAPs and Outcome Scales into the care planning process to enhance client outcomes • Introduce strategies other HSPs have used to enhance their care planning process
Back to the Basics
What is the inter. RAI CHA? inter. RAI Community Health Assessment (CHA) helps identify adults needing supports to prevent or stabilize early functional or health decline • • An electronic standardized comprehensive assessment Modular format Not all inclusive – “minimum” data set Data elements designed to be used for: – Care planning – Quality improvement using quality indicators – Outcome measures based on clinical scales 5
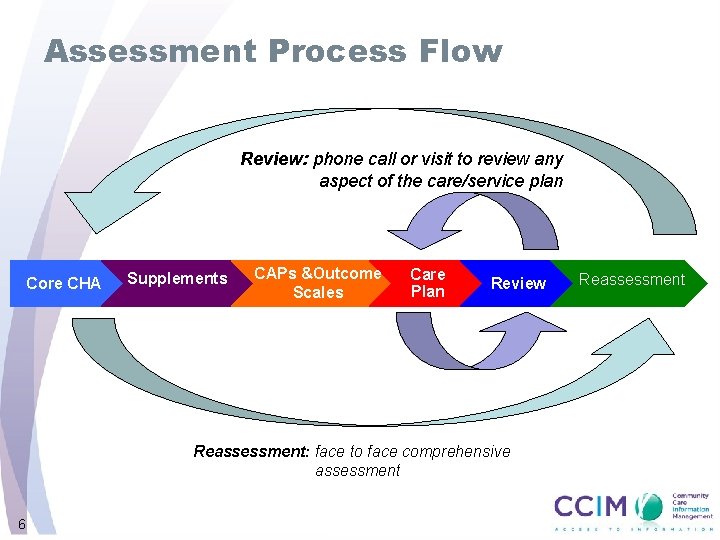
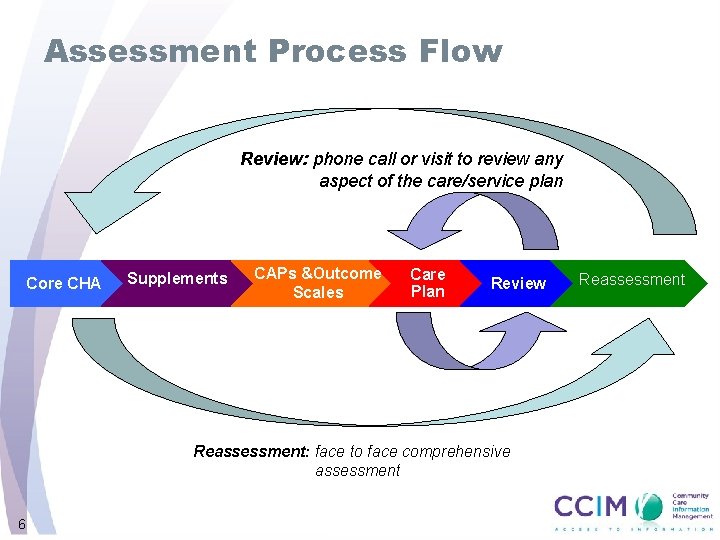
Assessment Process Flow Review: phone call or visit to review any aspect of the care/service plan Core CHA Supplements CAPs &Outcome Scales Care Plan Review Reassessment: face to face comprehensive assessment 6 Reassessment
inter. RAI CHA Outputs Outcome Scales/Measures & Clinical Assessment Protocols
Outcome Scales / Measures • Used to evaluate the clinical status of a client or group of clients and track their changes over time • Software generated • Derived from data collected by the completion of the inter. RAI CHA assessments • Evidence based for decision making
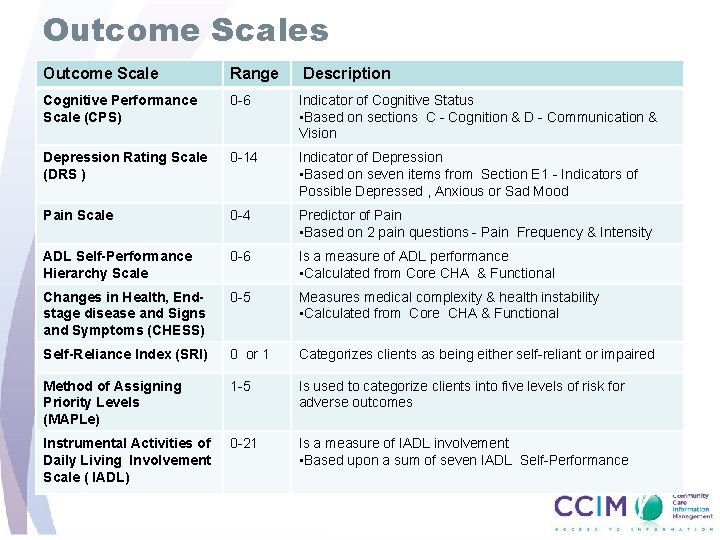
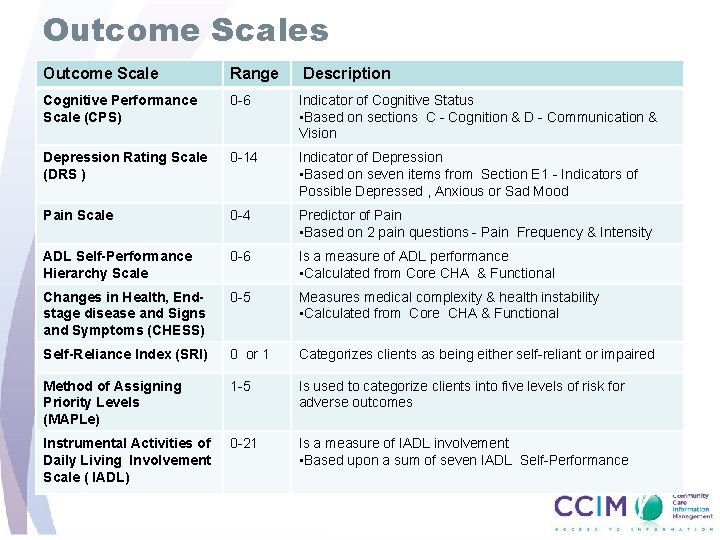
Outcome Scales Outcome Scale Range Description Cognitive Performance Scale (CPS) 0 -6 Indicator of Cognitive Status • Based on sections C - Cognition & D - Communication & Vision Depression Rating Scale (DRS ) 0 -14 Indicator of Depression • Based on seven items from Section E 1 - Indicators of Possible Depressed , Anxious or Sad Mood Pain Scale 0 -4 Predictor of Pain • Based on 2 pain questions - Pain Frequency & Intensity ADL Self-Performance Hierarchy Scale 0 -6 Is a measure of ADL performance • Calculated from Core CHA & Functional Changes in Health, Endstage disease and Signs and Symptoms (CHESS) 0 -5 Measures medical complexity & health instability • Calculated from Core CHA & Functional Self-Reliance Index (SRI) 0 or 1 Categorizes clients as being either self-reliant or impaired Method of Assigning Priority Levels (MAPLe) 1 -5 Is used to categorize clients into five levels of risk for adverse outcomes Instrumental Activities of Daily Living Involvement Scale ( IADL) 0 -21 Is a measure of IADL involvement • Based upon a sum of seven IADL Self-Performance
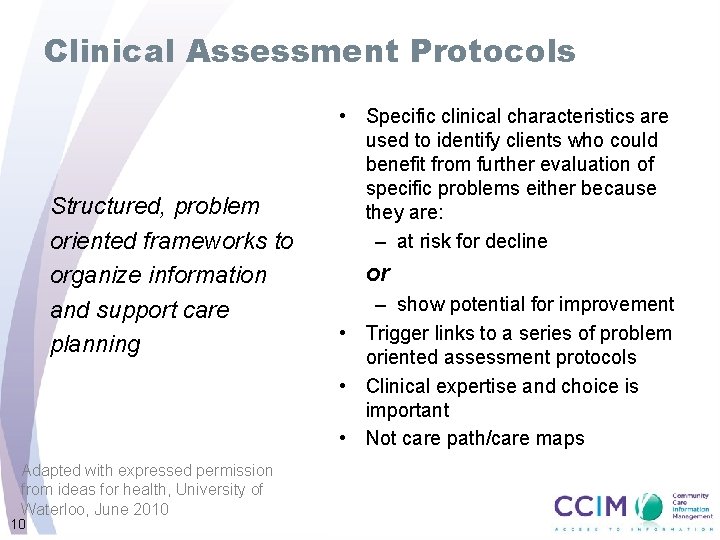
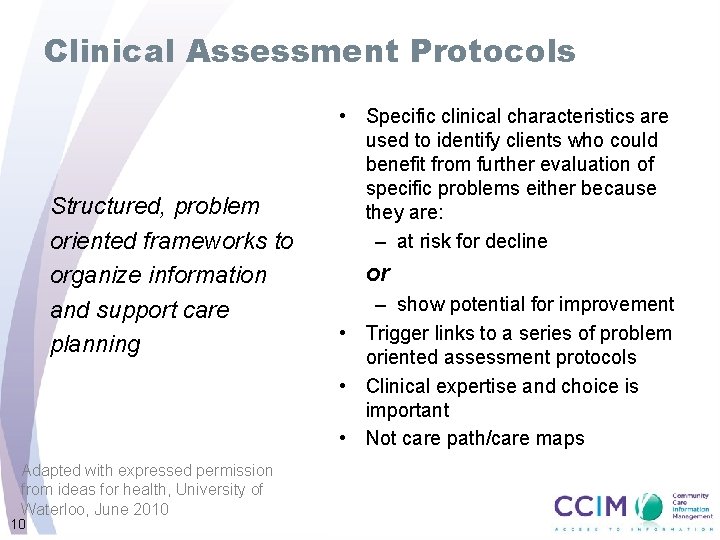
Clinical Assessment Protocols Structured, problem oriented frameworks to organize information and support care planning Adapted with expressed permission from ideas for health, University of Waterloo, June 2010 10 • Specific clinical characteristics are used to identify clients who could benefit from further evaluation of specific problems either because they are: – at risk for decline or – show potential for improvement • Trigger links to a series of problem oriented assessment protocols • Clinical expertise and choice is important • Not care path/care maps
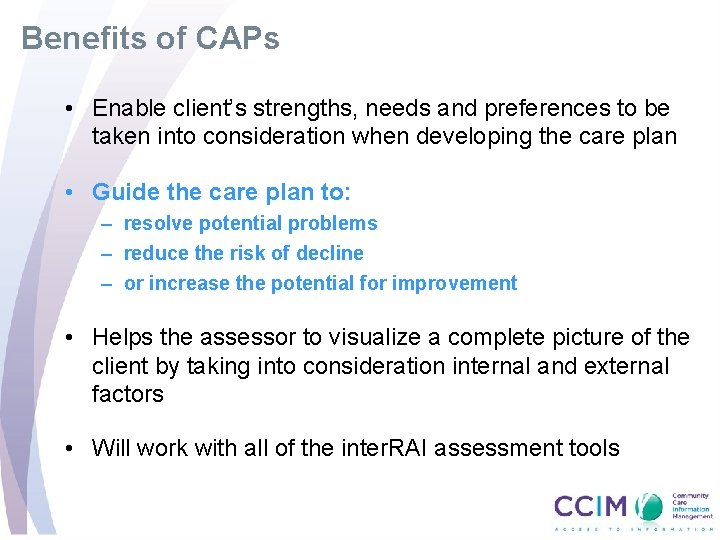
Benefits of CAPs • Enable client’s strengths, needs and preferences to be taken into consideration when developing the care plan • Guide the care plan to: – resolve potential problems – reduce the risk of decline – or increase the potential for improvement • Helps the assessor to visualize a complete picture of the client by taking into consideration internal and external factors • Will work with all of the inter. RAI assessment tools
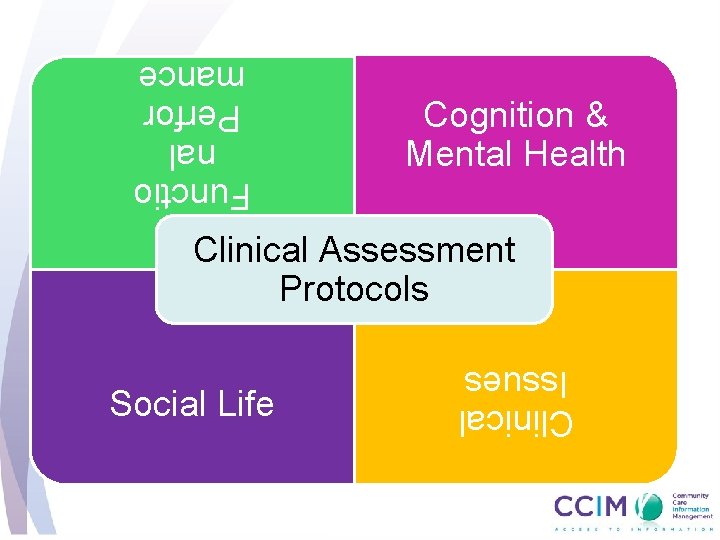
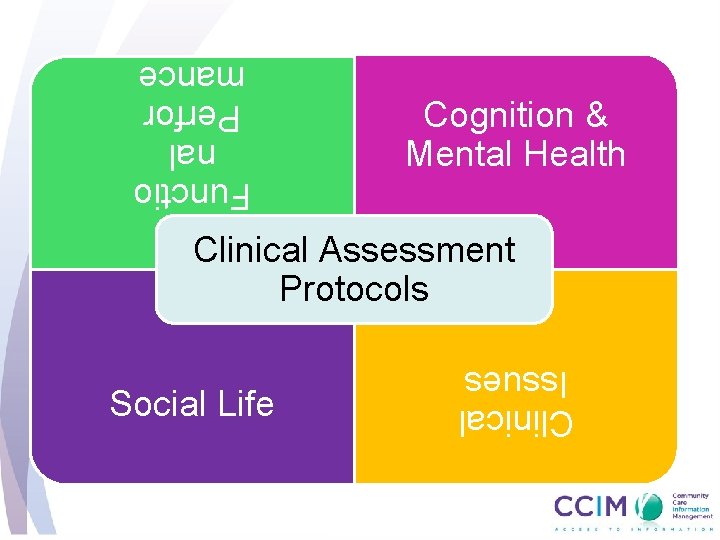
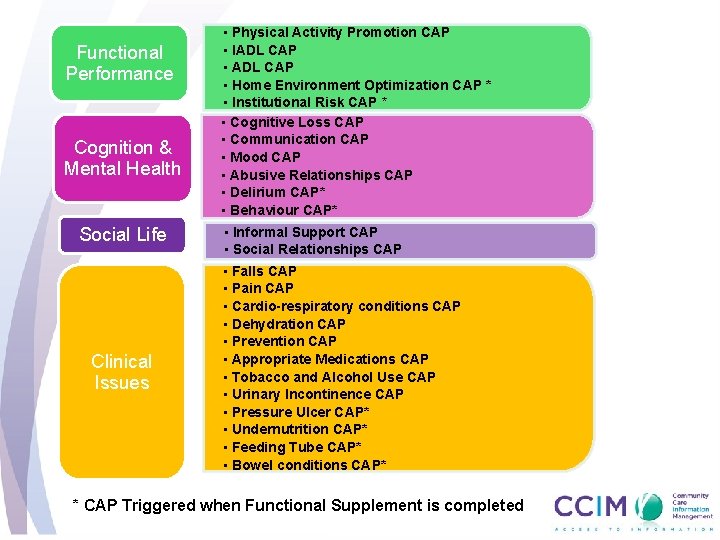
Cognition & Mental Health Functio nal Perfor mance Clinical Assessment Protocols Clinical Issues Social Life
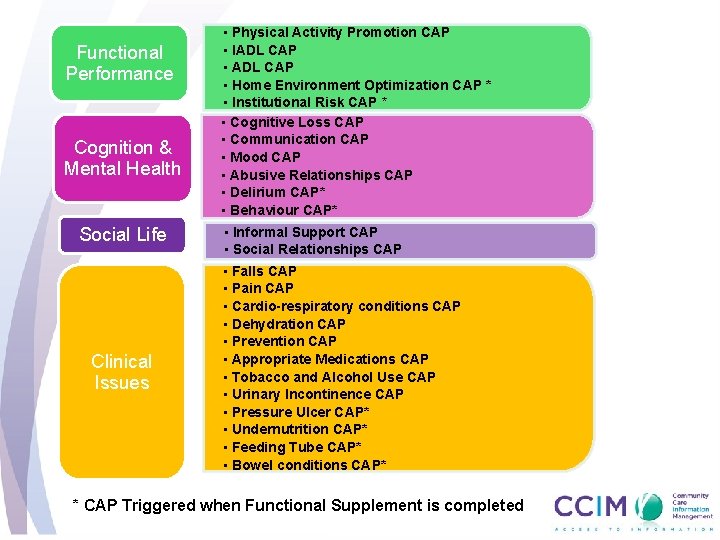
Functional Performance Cognition & Mental Health Social Life Clinical Issues • Physical Activity Promotion CAP • IADL CAP • Home Environment Optimization CAP * • Institutional Risk CAP * • Cognitive Loss CAP • Communication CAP • Mood CAP • Abusive Relationships CAP • Delirium CAP* • Behaviour CAP* • Informal Support CAP • Social Relationships CAP • Falls CAP • Pain CAP • Cardio-respiratory conditions CAP • Dehydration CAP • Prevention CAP • Appropriate Medications CAP • Tobacco and Alcohol Use CAP • Urinary Incontinence CAP • Pressure Ulcer CAP* • Undernutrition CAP* • Feeding Tube CAP* • Bowel conditions CAP* * CAP Triggered when Functional Supplement is completed
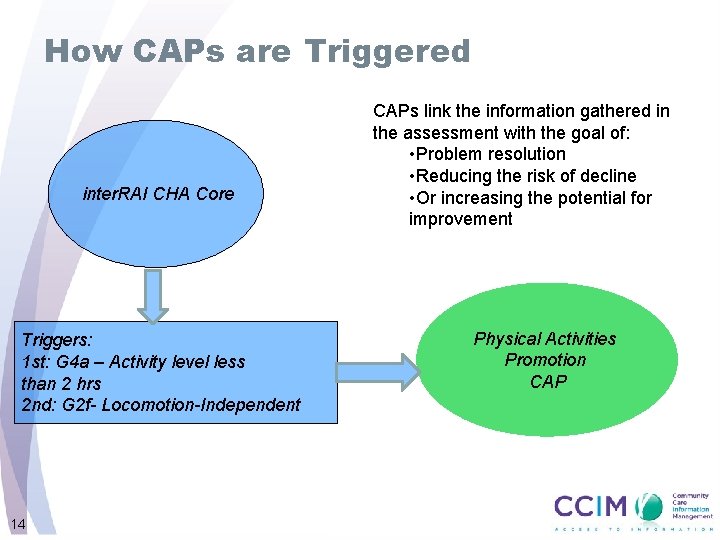
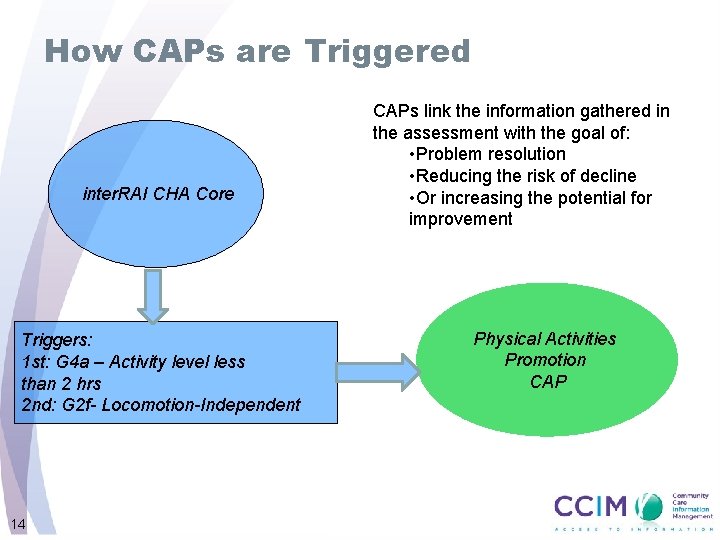
How CAPs are Triggered inter. RAI CHA Core Triggers: 1 st: G 4 a – Activity level less than 2 hrs 2 nd: G 2 f- Locomotion-Independent 14 CAPs link the information gathered in the assessment with the goal of: • Problem resolution • Reducing the risk of decline • Or increasing the potential for improvement Physical Activities Promotion CAP
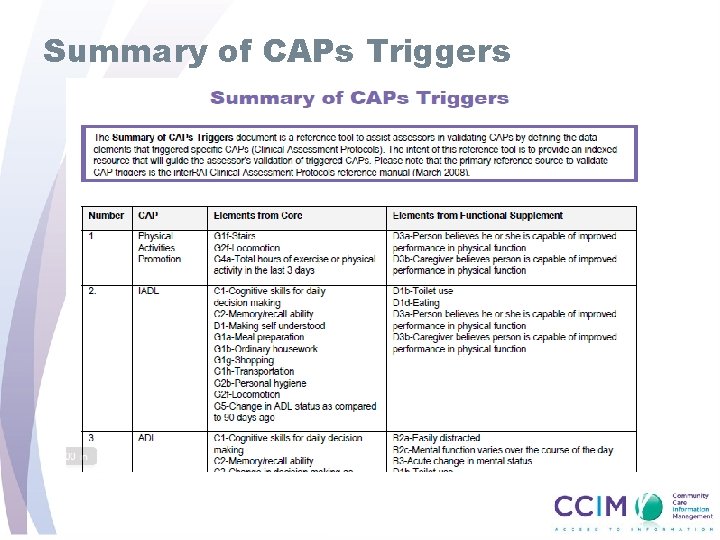
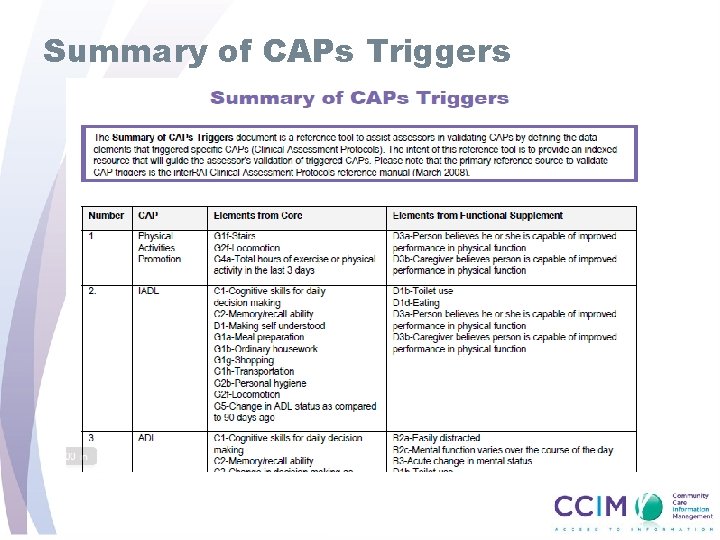
Summary of CAPs Triggers
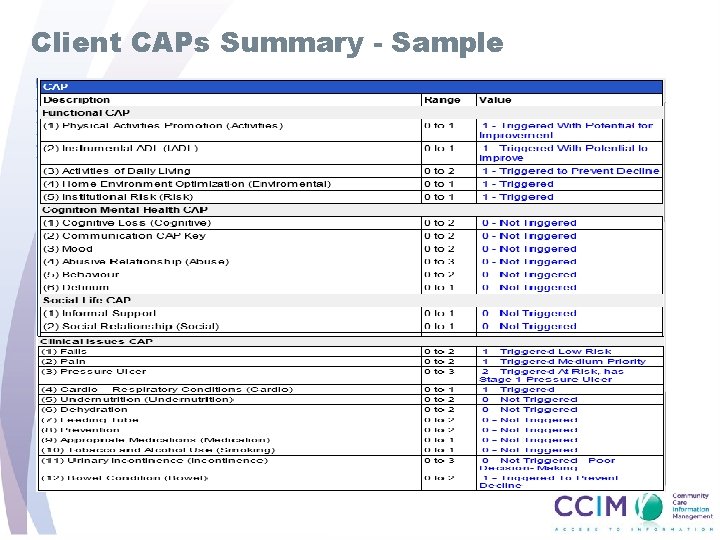
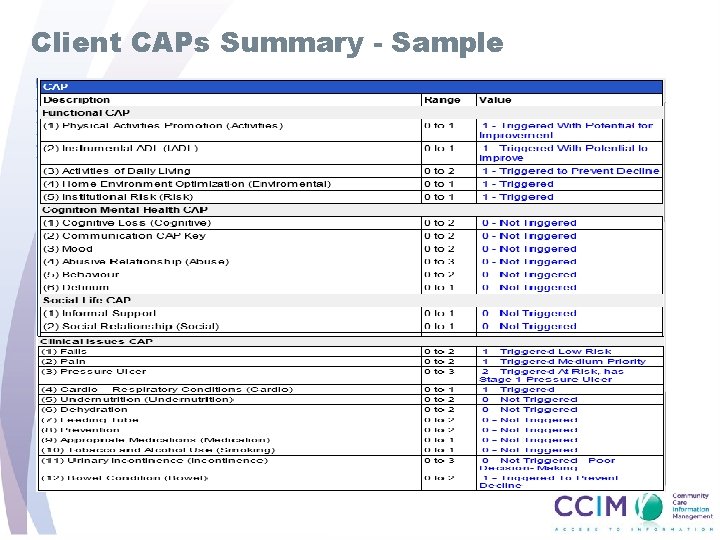
Client CAPs Summary - Sample
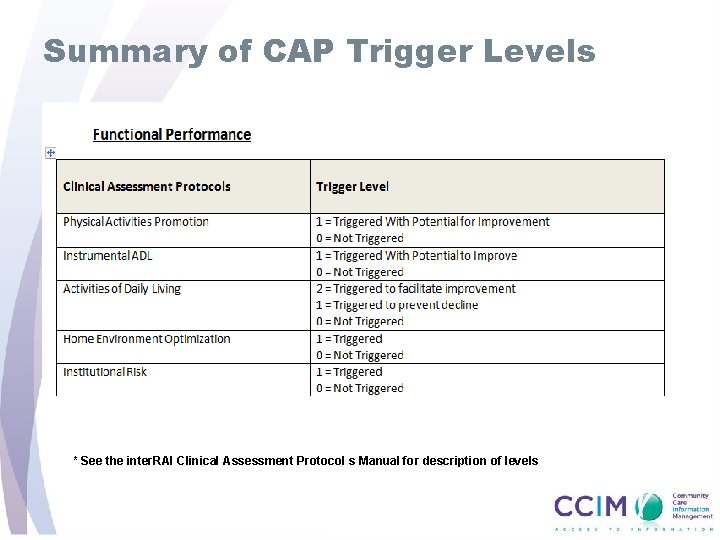
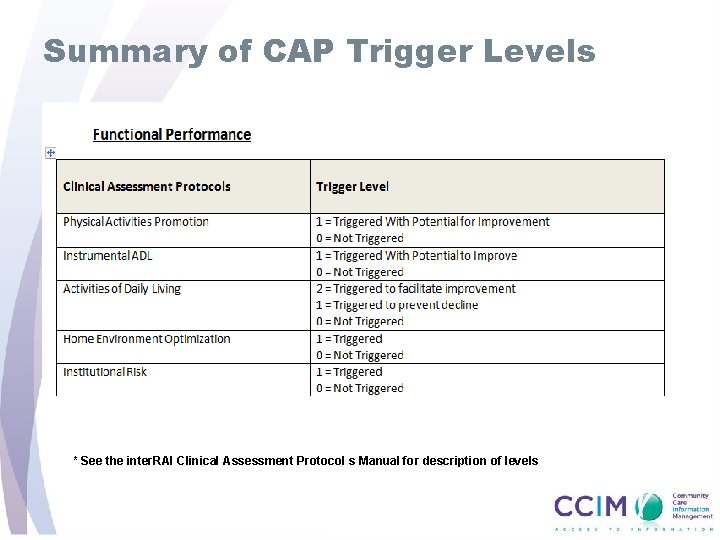
Summary of CAP Trigger Levels * See the inter. RAI Clinical Assessment Protocol s Manual for description of levels
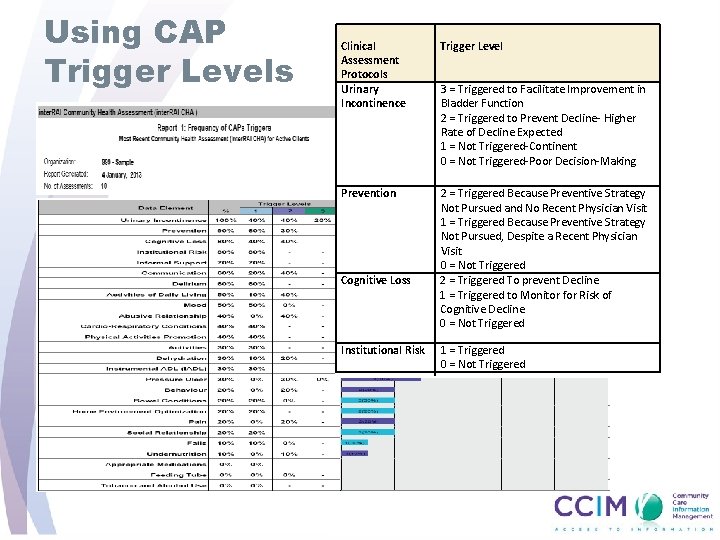
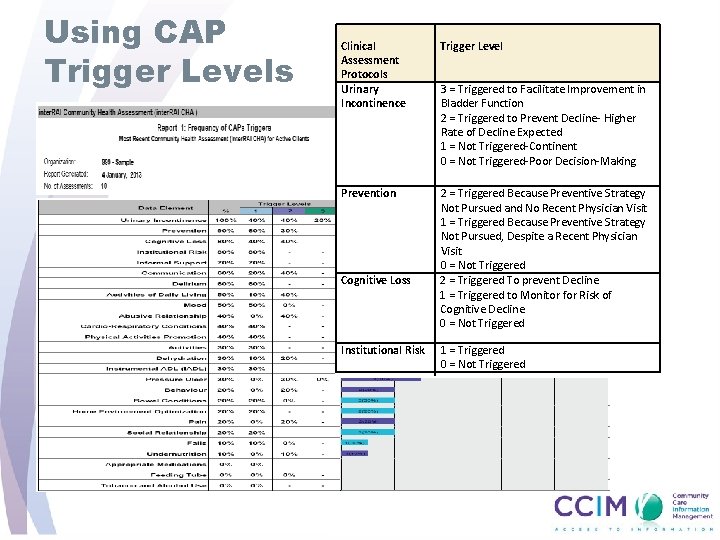
Using CAP Trigger Levels Clinical Assessment Protocols Urinary Incontinence Trigger Level Prevention 2 = Triggered Because Preventive Strategy Not Pursued and No Recent Physician Visit 1 = Triggered Because Preventive Strategy Not Pursued, Despite a Recent Physician Visit 0 = Not Triggered 2 = Triggered To prevent Decline 1 = Triggered to Monitor for Risk of Cognitive Decline 0 = Not Triggered Cognitive Loss Institutional Risk 3 = Triggered to Facilitate Improvement in Bladder Function 2 = Triggered to Prevent Decline- Higher Rate of Decline Expected 1 = Not Triggered-Continent 0 = Not Triggered-Poor Decision-Making 1 = Triggered 0 = Not Triggered
How CAPs are Organized In the inter. RAI Clinical Assessment Protocol Manual
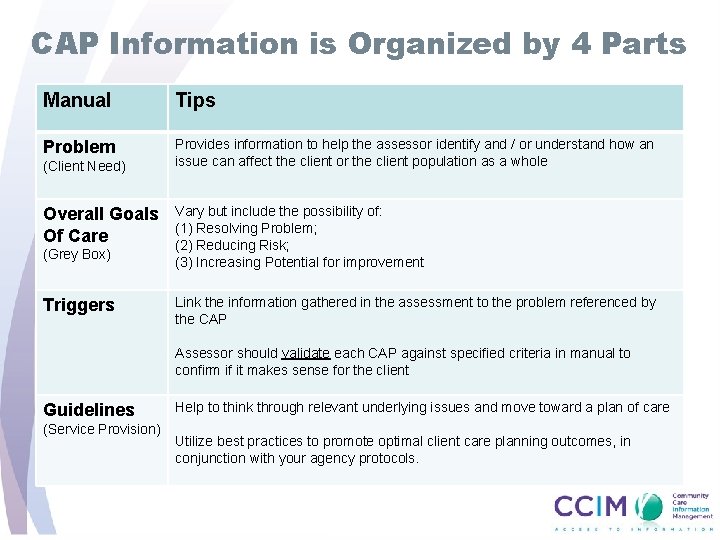
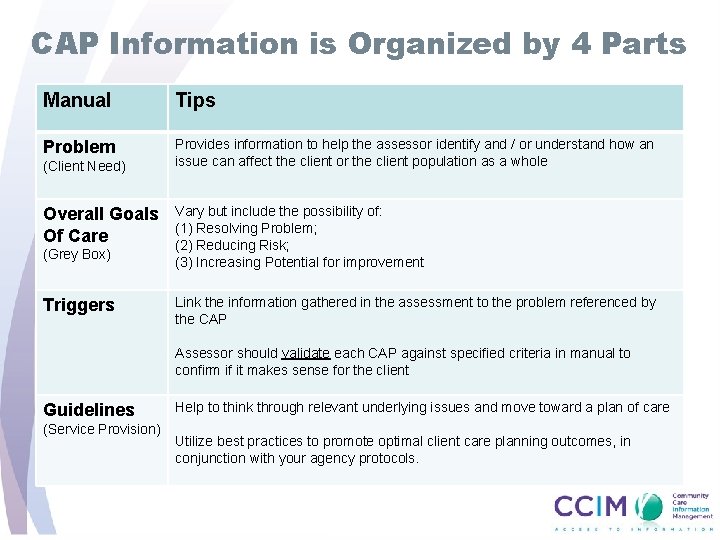
CAP Information is Organized by 4 Parts Manual Tips Problem Provides information to help the assessor identify and / or understand how an issue can affect the client or the client population as a whole (Client Need) Overall Goals Of Care (Grey Box) Triggers Vary but include the possibility of: (1) Resolving Problem; (2) Reducing Risk; (3) Increasing Potential for improvement Link the information gathered in the assessment to the problem referenced by the CAP Assessor should validate each CAP against specified criteria in manual to confirm if it makes sense for the client Guidelines (Service Provision) Help to think through relevant underlying issues and move toward a plan of care Utilize best practices to promote optimal client care planning outcomes, in conjunction with your agency protocols.
From CAPs to Care Planning • All triggered CAPs must be addressed in a care/service plan • Validate triggered CAPs with client to ensure that they are relevant and important • Prioritize triggered CAPs with client for the development of the care plan Adapted with expressed permission from ideas for health, University of Waterloo 21
Sharing their Journey • HSPs share how they have incorporated CAPs and Outcome Scales into the care planning process • Tips for success • Resources used or developed
Enhancing the Care/Service Planning Process Overview
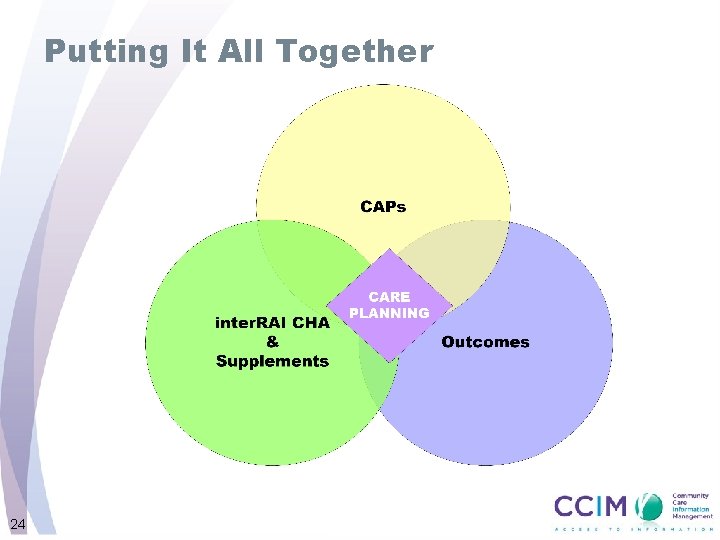
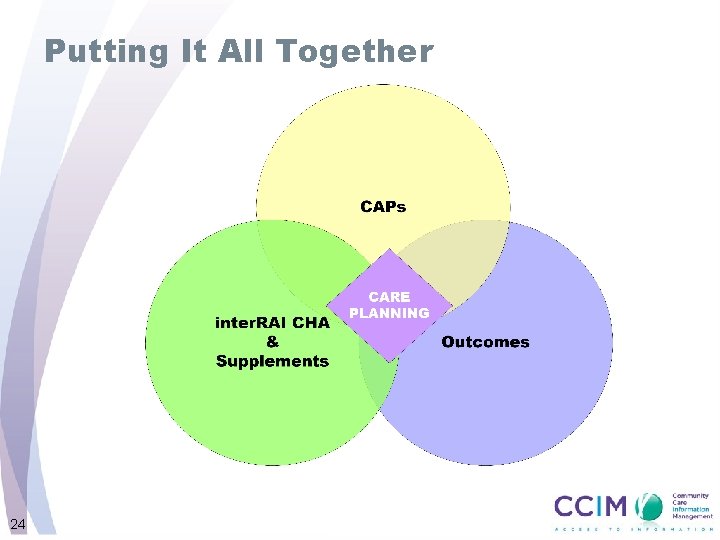
Putting It All Together 24
What is a Care/Service Plan • Roadmap to provide direction and guidance to all those involved in the clients care • Essential communication tool • A collaborative plan of service created with input from client and assessor
Characteristics of a Care/Service Plan Client Centered Current Accurate Clear Relevant Collaborative
Components of a Care/Service Plan • Care/service plans are generally organized by four categories: 1. 2. 3. 4. Problem statement/client needs Client goals Service provision/interventions Review date
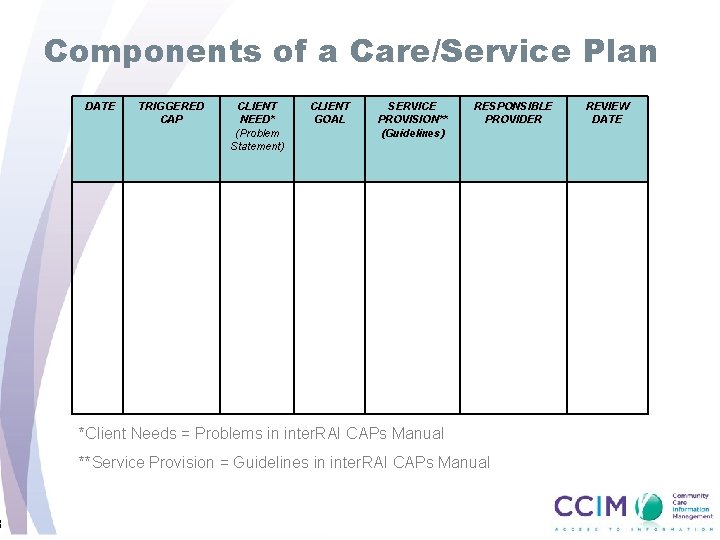
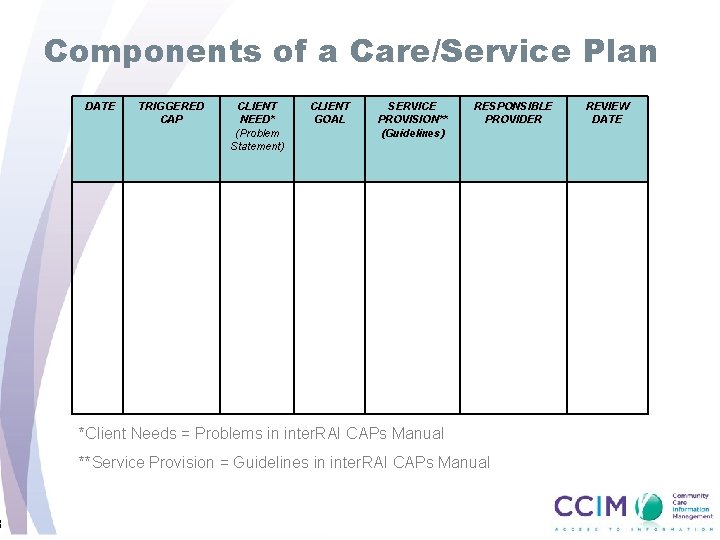
8 Components of a Care/Service Plan DATE TRIGGERED CAP CLIENT NEED* (Problem Statement) CLIENT GOAL SERVICE PROVISION** (Guidelines) RESPONSIBLE PROVIDER *Client Needs = Problems in inter. RAI CAPs Manual **Service Provision = Guidelines in inter. RAI CAPs Manual REVIEW DATE

Care/Service Planning
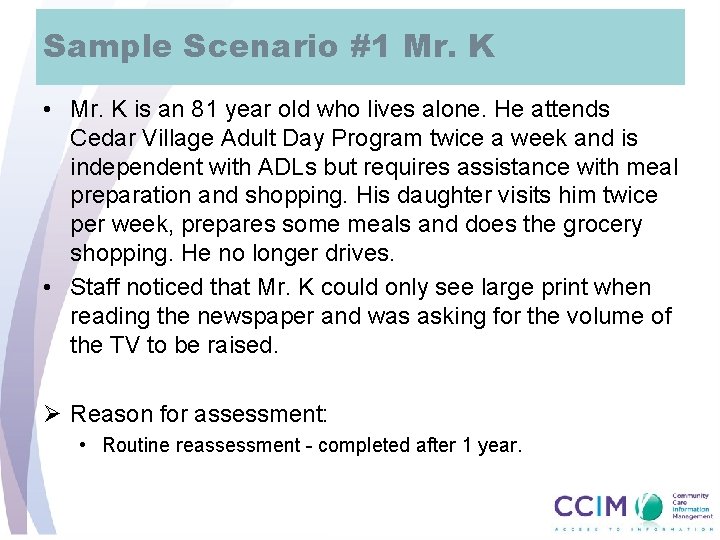
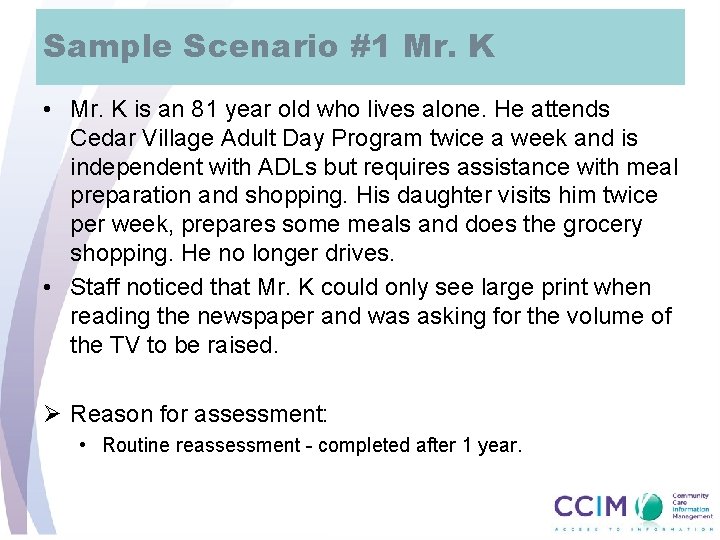
Sample Scenario #1 Mr. K • Mr. K is an 81 year old who lives alone. He attends Cedar Village Adult Day Program twice a week and is independent with ADLs but requires assistance with meal preparation and shopping. His daughter visits him twice per week, prepares some meals and does the grocery shopping. He no longer drives. • Staff noticed that Mr. K could only see large print when reading the newspaper and was asking for the volume of the TV to be raised. Ø Reason for assessment: • Routine reassessment - completed after 1 year.
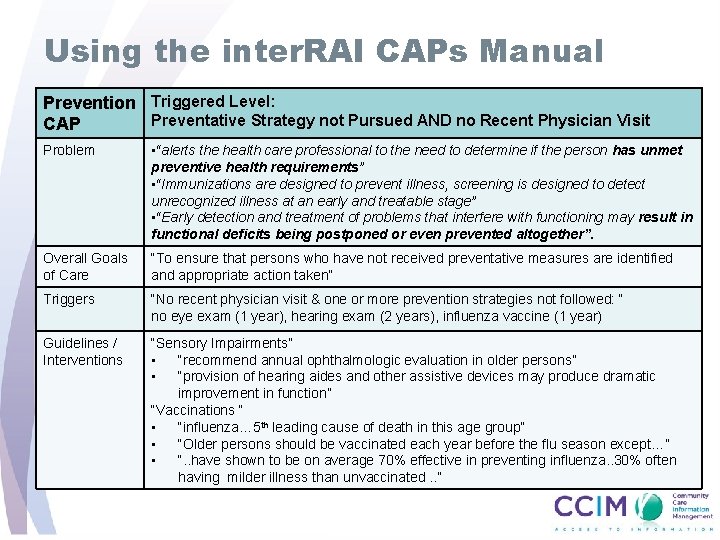
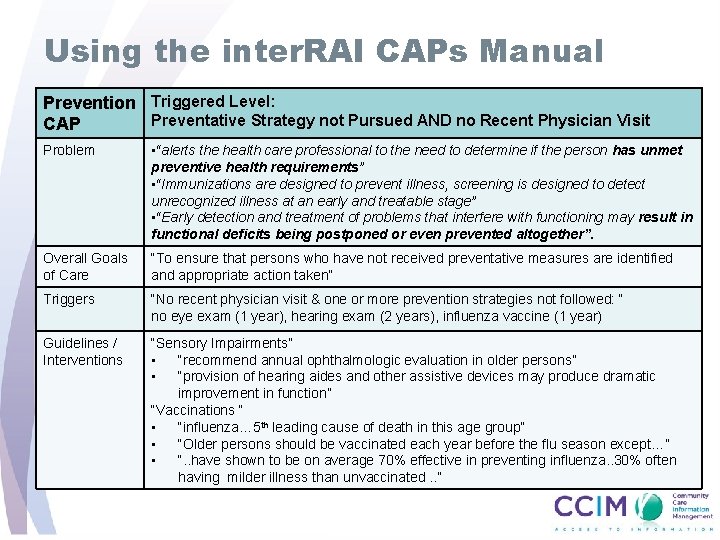
Using the inter. RAI CAPs Manual Prevention Triggered Level: Preventative Strategy not Pursued AND no Recent Physician Visit CAP Problem • “alerts the health care professional to the need to determine if the person has unmet preventive health requirements” • “Immunizations are designed to prevent illness, screening is designed to detect unrecognized illness at an early and treatable stage” • “Early detection and treatment of problems that interfere with functioning may result in functional deficits being postponed or even prevented altogether”. Overall Goals of Care “To ensure that persons who have not received preventative measures are identified and appropriate action taken” Triggers “No recent physician visit & one or more prevention strategies not followed: “ no eye exam (1 year), hearing exam (2 years), influenza vaccine (1 year) Guidelines / Interventions “Sensory Impairments” • “recommend annual ophthalmologic evaluation in older persons” • “provision of hearing aides and other assistive devices may produce dramatic improvement in function” “Vaccinations “ • “influenza… 5 th leading cause of death in this age group” • “Older persons should be vaccinated each year before the flu season except…” • “. . have shown to be on average 70% effective in preventing influenza. . 30% often having milder illness than unvaccinated. . ”
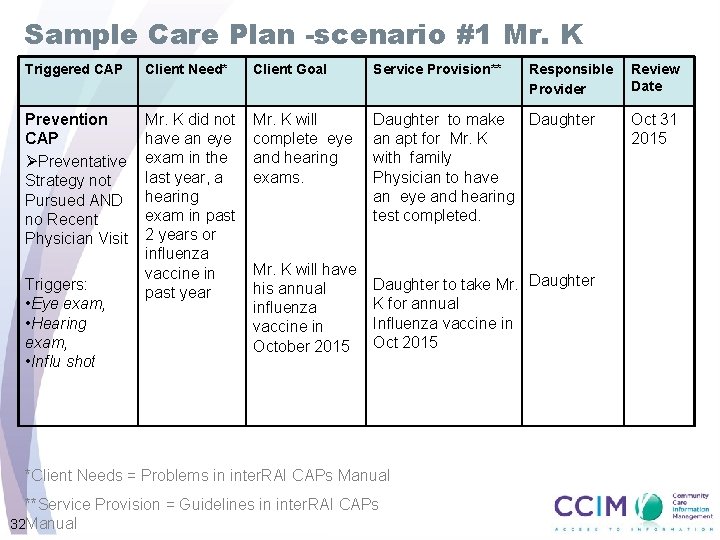
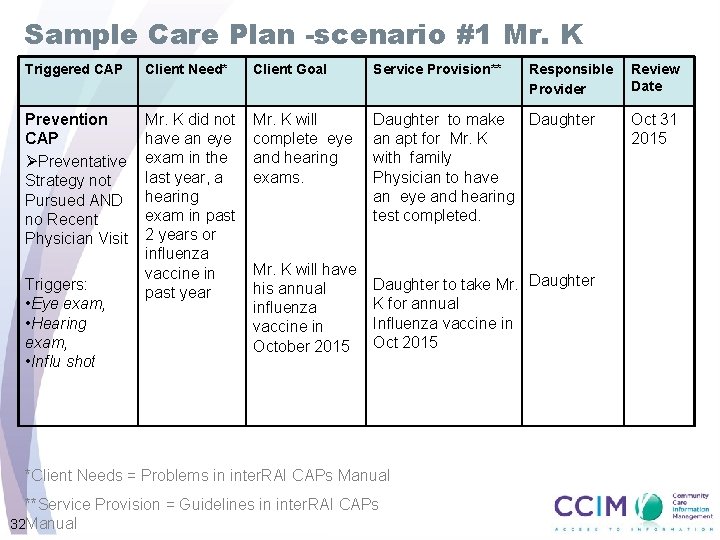
Sample Care Plan -scenario #1 Mr. K Triggered CAP Client Need* Client Goal Service Provision** Prevention CAP ØPreventative Strategy not Pursued AND no Recent Physician Visit Mr. K did not have an eye exam in the last year, a hearing exam in past 2 years or influenza vaccine in past year Mr. K will complete eye and hearing exams. Daughter to make Daughter an apt for Mr. K with family Physician to have an eye and hearing test completed. Triggers: • Eye exam, • Hearing exam, • Influ shot Mr. K will have his annual influenza vaccine in October 2015 Responsible Provider Daughter to take Mr. Daughter K for annual Influenza vaccine in Oct 2015 *Client Needs = Problems in inter. RAI CAPs Manual **Service Provision = Guidelines in inter. RAI CAPs 32 Manual Review Date Oct 31 2015
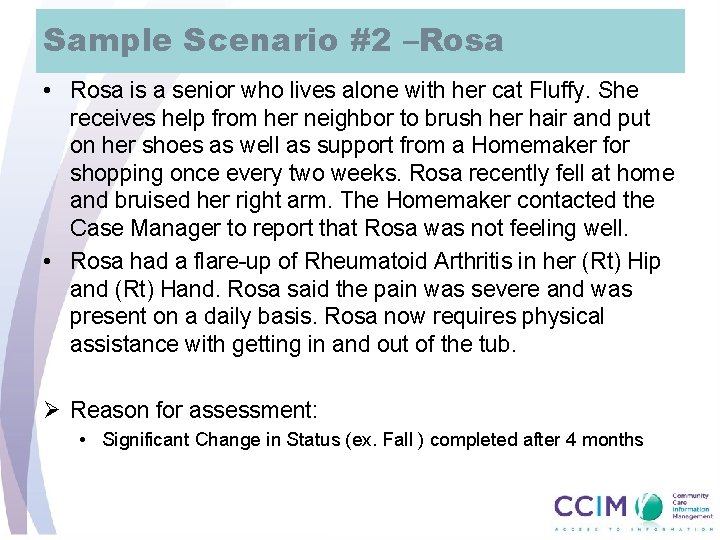
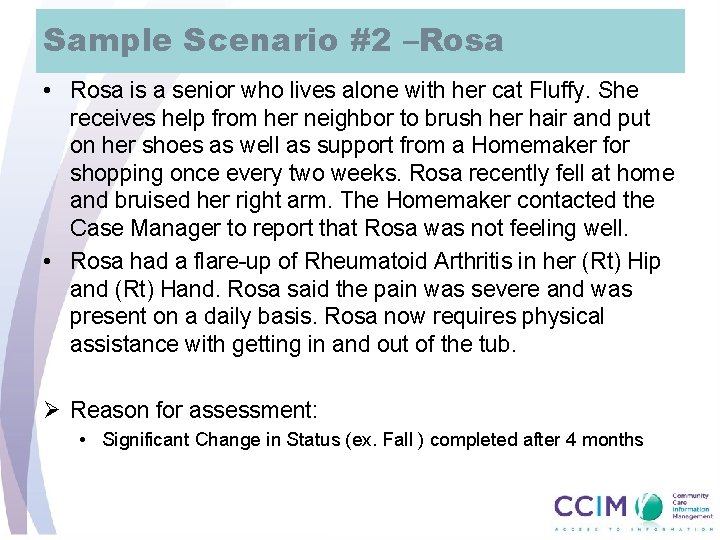
Sample Scenario #2 –Rosa • Rosa is a senior who lives alone with her cat Fluffy. She receives help from her neighbor to brush her hair and put on her shoes as well as support from a Homemaker for shopping once every two weeks. Rosa recently fell at home and bruised her right arm. The Homemaker contacted the Case Manager to report that Rosa was not feeling well. • Rosa had a flare-up of Rheumatoid Arthritis in her (Rt) Hip and (Rt) Hand. Rosa said the pain was severe and was present on a daily basis. Rosa now requires physical assistance with getting in and out of the tub. Ø Reason for assessment: • Significant Change in Status (ex. Fall ) completed after 4 months
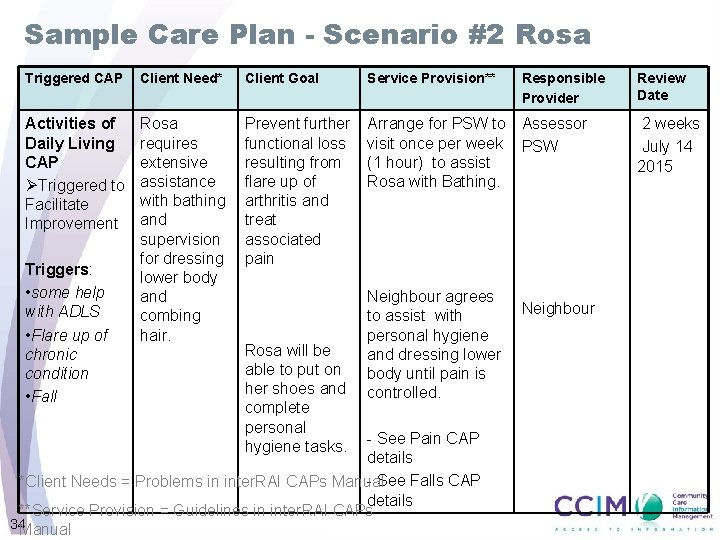
Sample Care Plan - Scenario #2 Rosa Triggered CAP Client Need* Client Goal Service Provision** Activities of Daily Living CAP ØTriggered to Facilitate Improvement Rosa requires extensive assistance with bathing and supervision for dressing lower body and combing hair. Prevent further functional loss resulting from flare up of arthritis and treat associated pain Arrange for PSW to Assessor visit once per week PSW (1 hour) to assist Rosa with Bathing. Triggers: • some help with ADLS • Flare up of chronic condition • Fall Rosa will be able to put on her shoes and complete personal hygiene tasks. Neighbour agrees to assist with personal hygiene and dressing lower body until pain is controlled. - See Pain CAP details - See Falls CAP *Client Needs = Problems in inter. RAI CAPs Manual details **Service Provision = Guidelines in inter. RAI CAPs 34 Manual Responsible Provider Neighbour Review Date 2 weeks July 14 2015
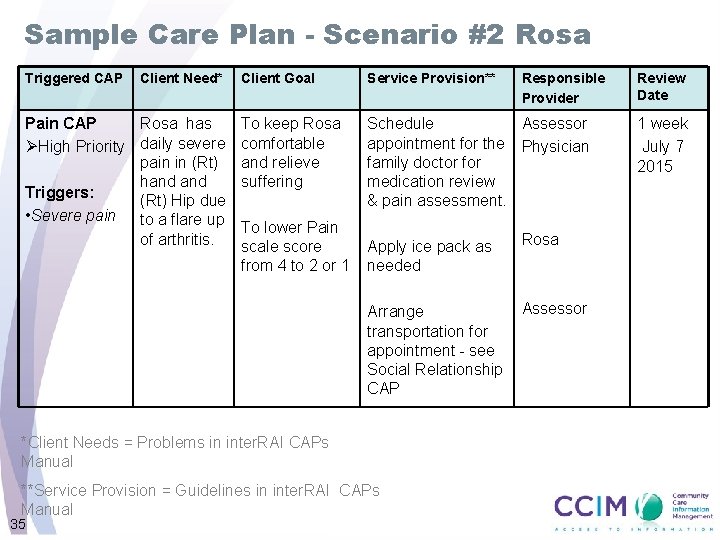
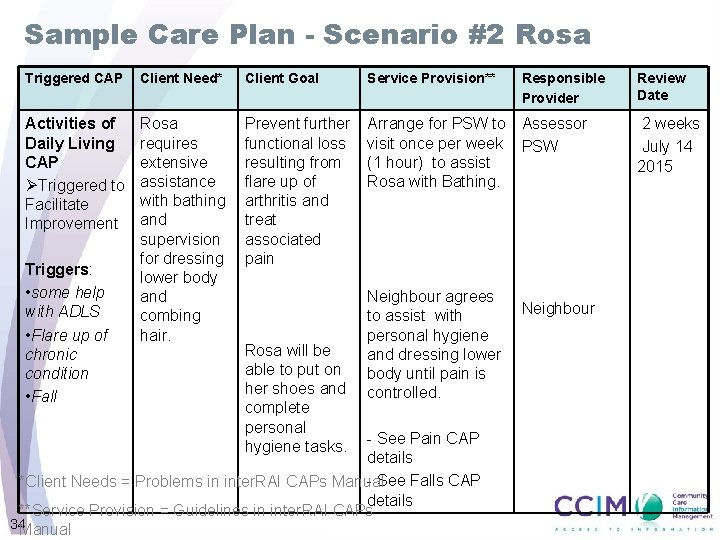
Sample Care Plan - Scenario #2 Rosa Triggered CAP Client Need* Pain CAP Rosa has ØHigh Priority daily severe pain in (Rt) hand Triggers: (Rt) Hip due • Severe pain to a flare up of arthritis. Client Goal Service Provision** To keep Rosa comfortable and relieve suffering Schedule Assessor appointment for the Physician family doctor for medication review & pain assessment. To lower Pain scale score from 4 to 2 or 1 Apply ice pack as needed Rosa Arrange transportation for appointment - see Social Relationship CAP Assessor *Client Needs = Problems in inter. RAI CAPs Manual **Service Provision = Guidelines in inter. RAI CAPs Manual 35 Responsible Provider Review Date 1 week July 7 2015
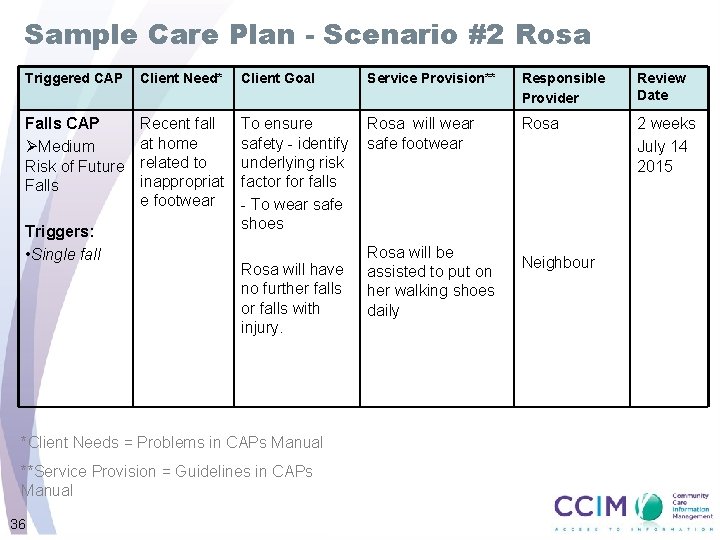
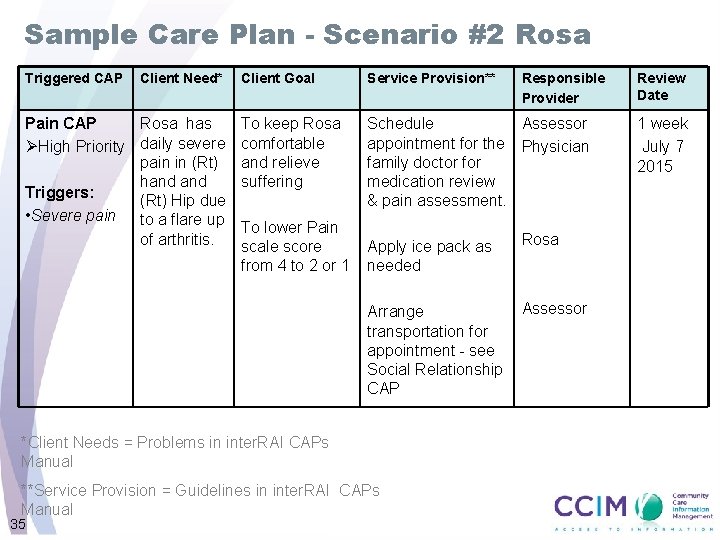
Sample Care Plan - Scenario #2 Rosa Triggered CAP Client Need* Client Goal Service Provision** Responsible Provider Review Date Falls CAP ØMedium Risk of Future Falls Recent fall at home related to inappropriat e footwear To ensure safety - identify underlying risk factor falls - To wear safe shoes Rosa will wear safe footwear Rosa 2 weeks July 14 2015 Triggers: • Single fall Rosa will have no further falls or falls with injury. *Client Needs = Problems in CAPs Manual **Service Provision = Guidelines in CAPs Manual 36 Rosa will be assisted to put on her walking shoes daily Neighbour
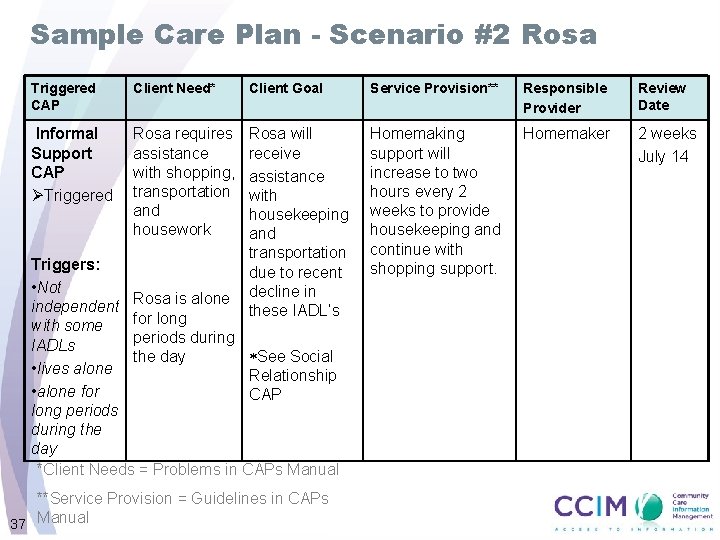
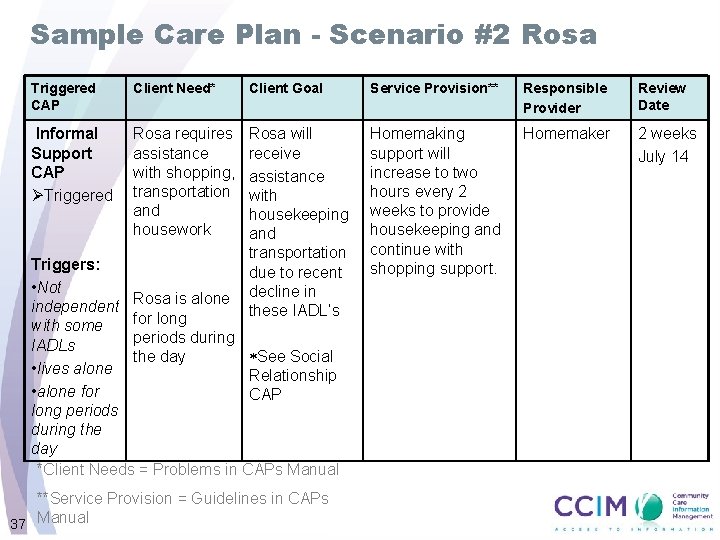
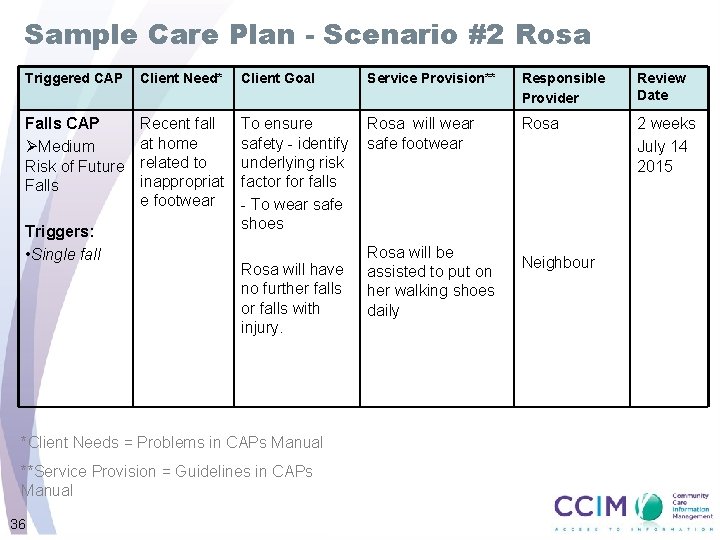
Sample Care Plan - Scenario #2 Rosa Triggered CAP Client Need* Client Goal Service Provision** Responsible Provider Review Date Informal Support CAP ØTriggered Rosa requires assistance with shopping, transportation and housework Rosa will receive assistance with housekeeping and transportation due to recent decline in these IADL’s Homemaking support will increase to two hours every 2 weeks to provide housekeeping and continue with shopping support. Homemaker 2 weeks July 14 Triggers: • Not independent Rosa is alone for long with some periods during IADLs See Social the day • lives alone Relationship • alone for CAP long periods during the day *Client Needs = Problems in CAPs Manual **Service Provision = Guidelines in CAPs 37 Manual
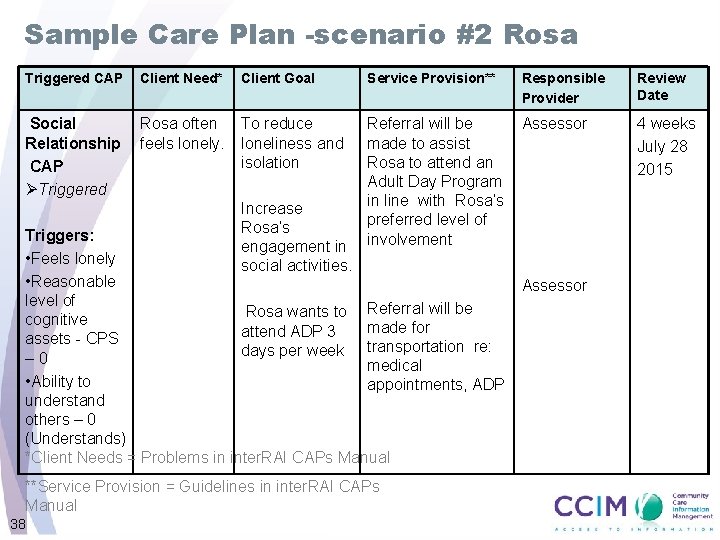
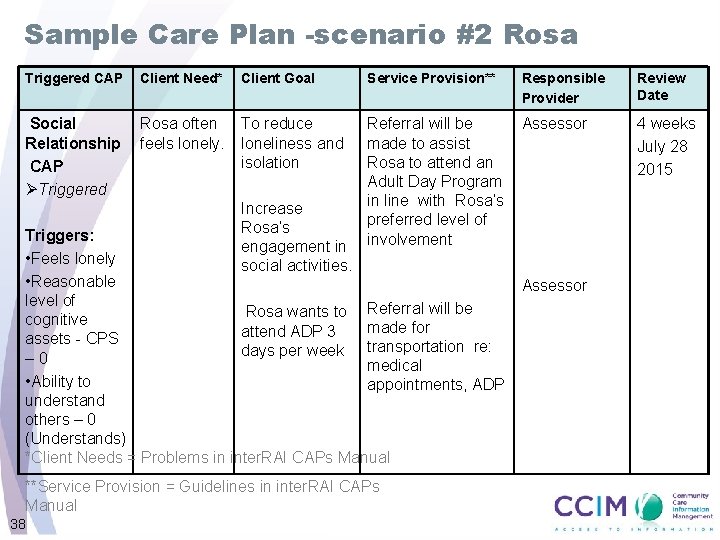
Sample Care Plan -scenario #2 Rosa Triggered CAP Client Need* Client Goal Service Provision** Responsible Provider Review Date Social Relationship CAP ØTriggered Rosa often feels lonely. To reduce loneliness and isolation Referral will be made to assist Rosa to attend an Adult Day Program in line with Rosa’s preferred level of involvement Assessor 4 weeks July 28 2015 Increase Rosa’s engagement in social activities. Triggers: • Feels lonely • Reasonable level of Rosa wants to Referral will be cognitive made for attend ADP 3 assets - CPS days per week transportation re: – 0 medical • Ability to appointments, ADP understand others – 0 (Understands) *Client Needs = Problems in inter. RAI CAPs Manual **Service Provision = Guidelines in inter. RAI CAPs Manual 38 Assessor
Summary: • Value and impact of using the CAPs and Outcomes Scale reports • Benefits of using inter. RAI CAPs Manual • Tips and examples of how use the outputs to inform care planning and improve client outcomes • Begin to include the outputs at your regular team meetings, client and family discussions
Resources inter. RAI CHA CAPs and Care Planning Binder ØReassessment Best Practices ØTrigger Level Categories inter. RAI Clinical Assessment Protocols - For Use with inter. RAI’s Community and Long Term Care Assessment Instruments Manual Website www. ccim. on. ca Service Desk csscap@ccim. on. ca 1 -866 -909 -5600 option 9
Wrap- up
Thank you! Service Desk Contact Information Email: Toll Free: Website: 42 csscap@ccim. on. ca 1 -866 -909 -5600, Option 9 www. ccim. on. ca