D Cardiac Cycle Mechanical Events Systole Diastole BP
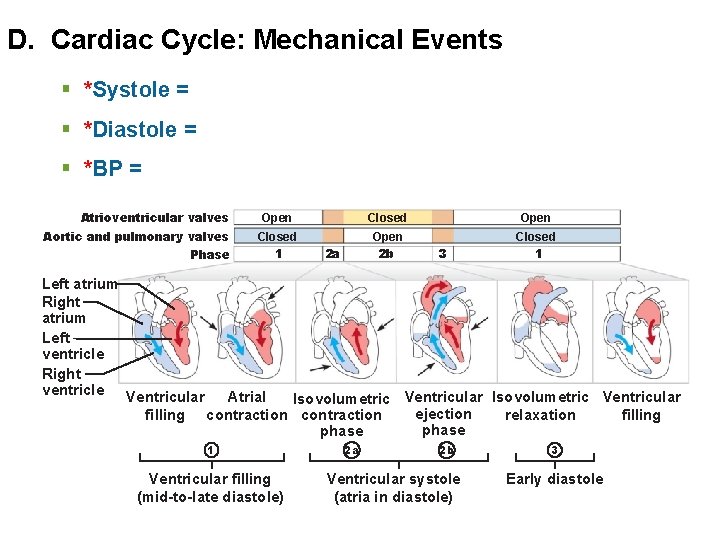
D. Cardiac Cycle: Mechanical Events § *Systole = § *Diastole = § *BP = Atrioventricular valves Aortic and pulmonary valves Phase Open Closed 1 Open 2 b Closed 1 2 a 3 Left atrium Right atrium Left ventricle Right ventricle Ventricular Atrial Isovolumetric Ventricular ejection filling contraction relaxation filling phase 1 Ventricular filling (mid-to-late diastole) 2 a 2 b Ventricular systole (atria in diastole) 3 Early diastole
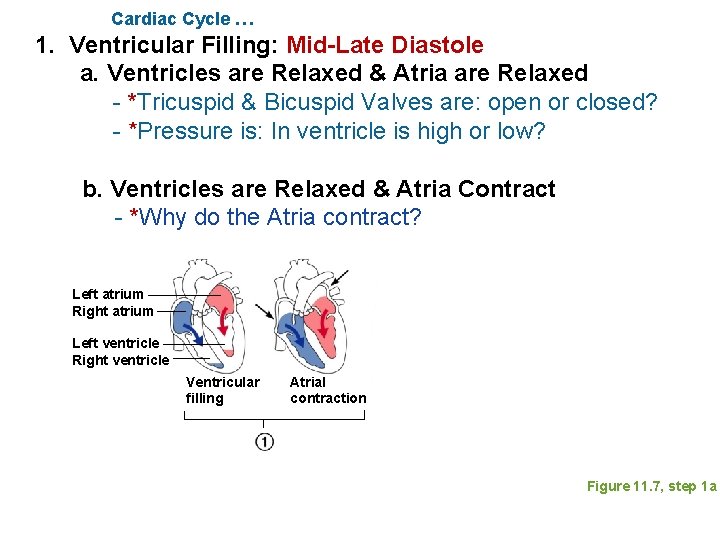
Cardiac Cycle … 1. Ventricular Filling: Mid-Late Diastole a. Ventricles are Relaxed & Atria are Relaxed - *Tricuspid & Bicuspid Valves are: open or closed? - *Pressure is: In ventricle is high or low? b. Ventricles are Relaxed & Atria Contract - *Why do the Atria contract? Left atrium Right atrium Left ventricle Right ventricle Ventricular filling Atrial contraction Figure 11. 7, step 1 a
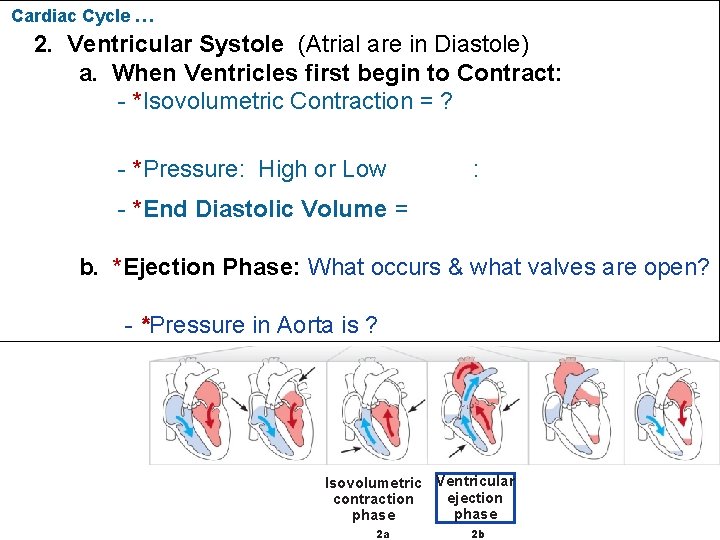
Cardiac Cycle … 2. Ventricular Systole (Atrial are in Diastole) a. When Ventricles first begin to Contract: - *Isovolumetric Contraction = ? - *Pressure: High or Low : - *End Diastolic Volume = b. *Ejection Phase: What occurs & what valves are open? - *Pressure in Aorta is ? Isovolumetric Ventricular ejection contraction phase 2 a 2 b
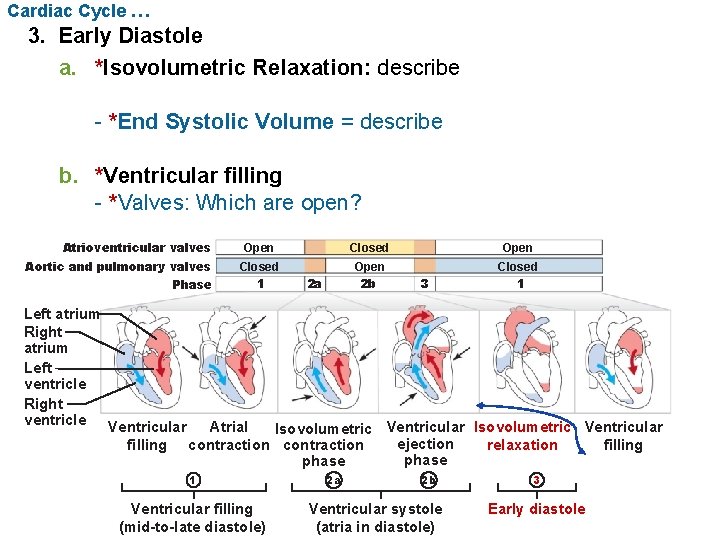
Cardiac Cycle … 3. Early Diastole a. *Isovolumetric Relaxation: describe - *End Systolic Volume = describe b. *Ventricular filling - *Valves: Which are open? Atrioventricular valves Aortic and pulmonary valves Phase Open Closed 1 Open 2 b Closed 1 2 a 3 Left atrium Right atrium Left ventricle Right ventricle Ventricular Atrial Isovolumetric Ventricular ejection filling contraction relaxation filling phase 1 Ventricular filling (mid-to-late diastole) 2 a 2 b Ventricular systole (atria in diastole) 3 Early diastole
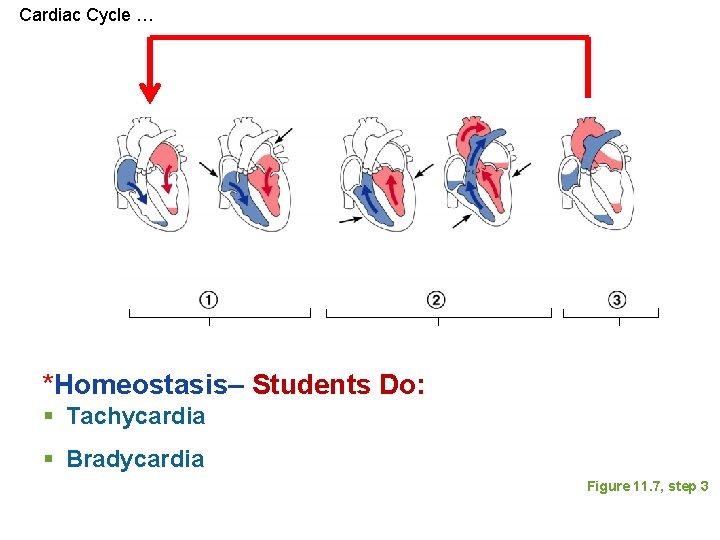
Cardiac Cycle … *Homeostasis– Students Do: § Tachycardia § Bradycardia Figure 11. 7, step 3

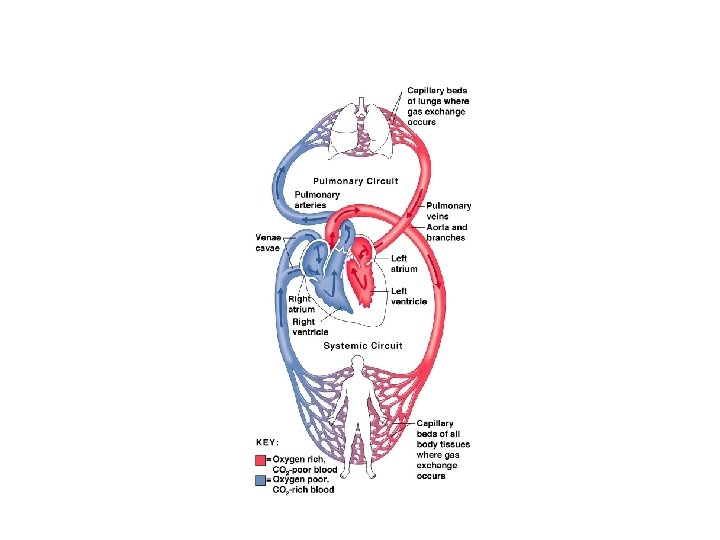
E. Control of Heart Function– Cardiac Output Is Controled by Stroke Volume & Heart Rate 1. Definition of Terms *CO = Volume of blood pumped: finish definition *Stroke Volume (SV) = Volume of blood: finish definition - The two ventricles eject the same volume *Heart Rate = CO = heart rate (HR) x stroke volume (SV) = 5. 25 L/min *Cardiac Reserve = CO maximum – CO at rest
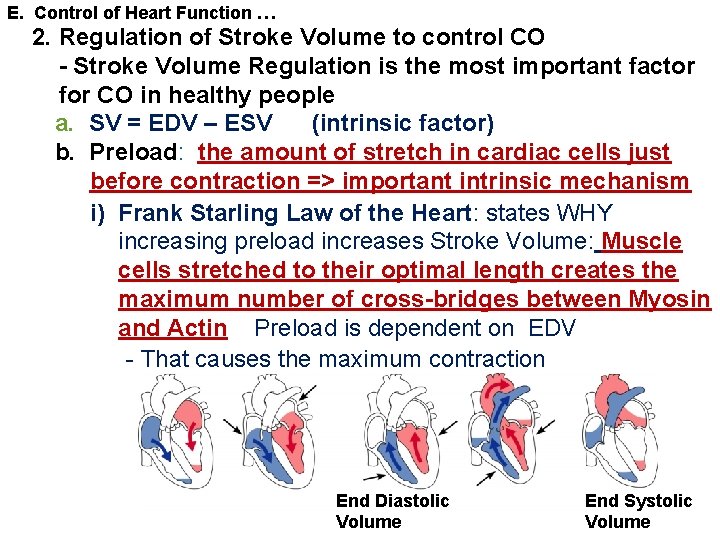
E. Control of Heart Function … 2. Regulation of Stroke Volume to control CO - Stroke Volume Regulation is the most important factor for CO in healthy people a. SV = EDV – ESV (intrinsic factor) b. Preload: the amount of stretch in cardiac cells just before contraction => important intrinsic mechanism i) Frank Starling Law of the Heart: states WHY increasing preload increases Stroke Volume: Muscle cells stretched to their optimal length creates the maximum number of cross-bridges between Myosin and Actin Preload is dependent on EDV - That causes the maximum contraction End Diastolic Volume End Systolic Volume
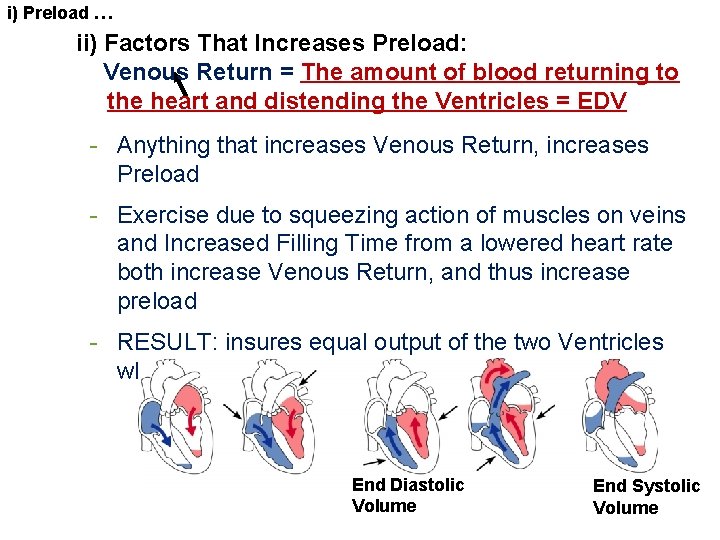
i) Preload … ii) Factors That Increases Preload: Venous Return = The amount of blood returning to the heart and distending the Ventricles = EDV - Anything that increases Venous Return, increases Preload - Exercise due to squeezing action of muscles on veins and Increased Filling Time from a lowered heart rate both increase Venous Return, and thus increase preload - RESULT: insures equal output of the two Ventricles which prevents back-up of blood End Diastolic Volume End Systolic Volume
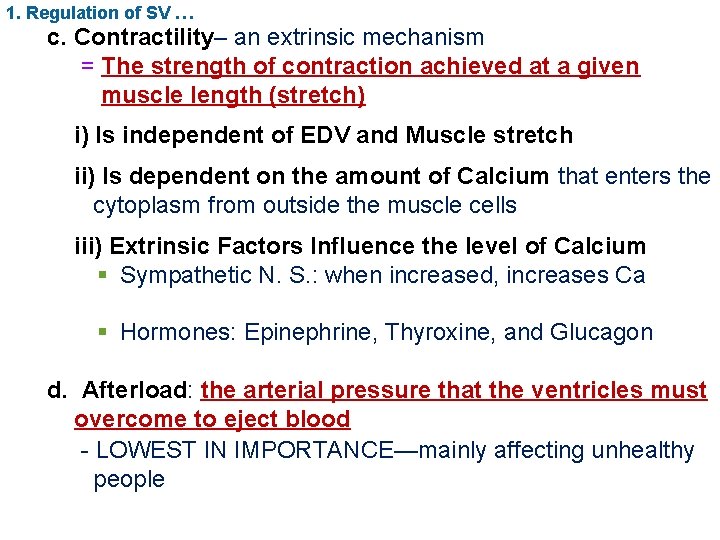
1. Regulation of SV … c. Contractility– an extrinsic mechanism = The strength of contraction achieved at a given muscle length (stretch) i) Is independent of EDV and Muscle stretch ii) Is dependent on the amount of Calcium that enters the cytoplasm from outside the muscle cells iii) Extrinsic Factors Influence the level of Calcium § Sympathetic N. S. : when increased, increases Ca § Hormones: Epinephrine, Thyroxine, and Glucagon d. Afterload: the arterial pressure that the ventricles must overcome to eject blood - LOWEST IN IMPORTANCE—mainly affecting unhealthy people
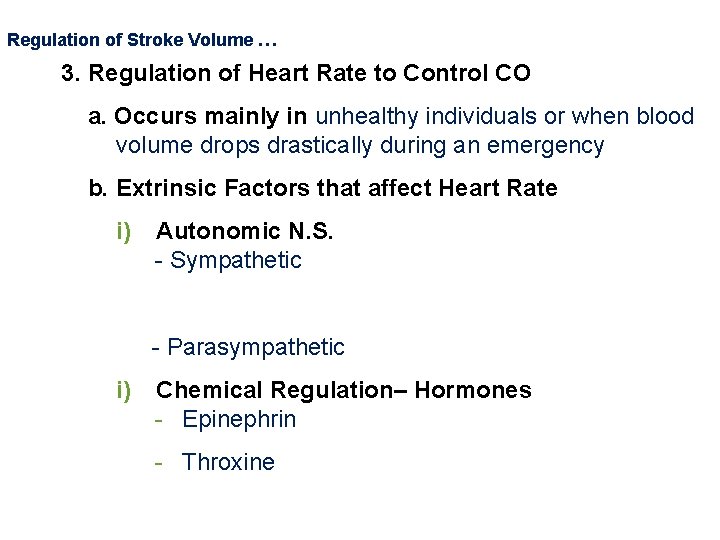
Regulation of Stroke Volume … 3. Regulation of Heart Rate to Control CO a. Occurs mainly in unhealthy individuals or when blood volume drops drastically during an emergency b. Extrinsic Factors that affect Heart Rate i) Autonomic N. S. - Sympathetic - Parasympathetic i) Chemical Regulation– Hormones - Epinephrin - Throxine

4. Autonomic Innervation of the HEART-- Overview § Parasympathetic NS § Cardioihibitory Center of Medulla § Vagus Nerve causes Vagal Tone § Sympathetic NS § Cardioacceleratory Center of Medulla § Vasomotor Center of Medulla § NEXT SLIDE
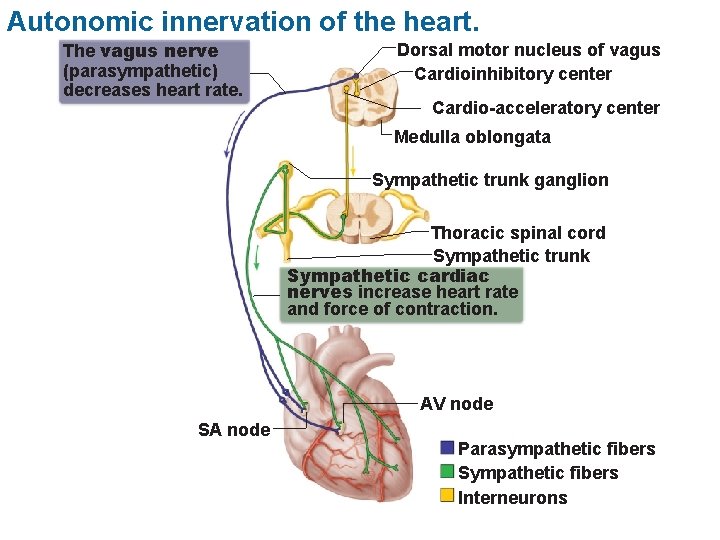
Autonomic innervation of the heart. The vagus nerve (parasympathetic) decreases heart rate. Dorsal motor nucleus of vagus Cardioinhibitory center Cardio-acceleratory center Medulla oblongata Sympathetic trunk ganglion Thoracic spinal cord Sympathetic trunk Sympathetic cardiac nerves increase heart rate and force of contraction. AV node SA node Parasympathetic fibers Sympathetic fibers Interneurons
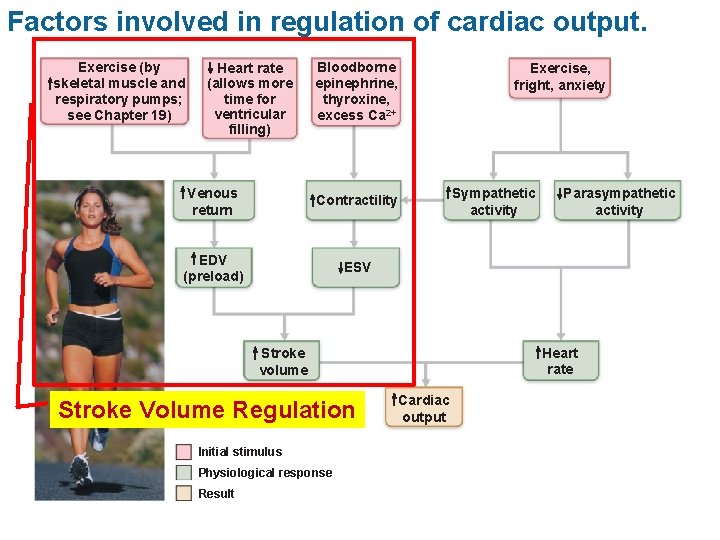
Factors involved in regulation of cardiac output. Exercise (by skeletal muscle and respiratory pumps; see Chapter 19) Heart rate (allows more time for ventricular filling) Bloodborne epinephrine, thyroxine, excess Ca 2+ Venous return Contractility EDV (preload) ESV Exercise, fright, anxiety Sympathetic activity Heart rate Stroke volume Stroke Volume Regulation Initial stimulus Physiological response Result Parasympathetic activity Cardiac output
END OF PPT NEXT § Review Questio
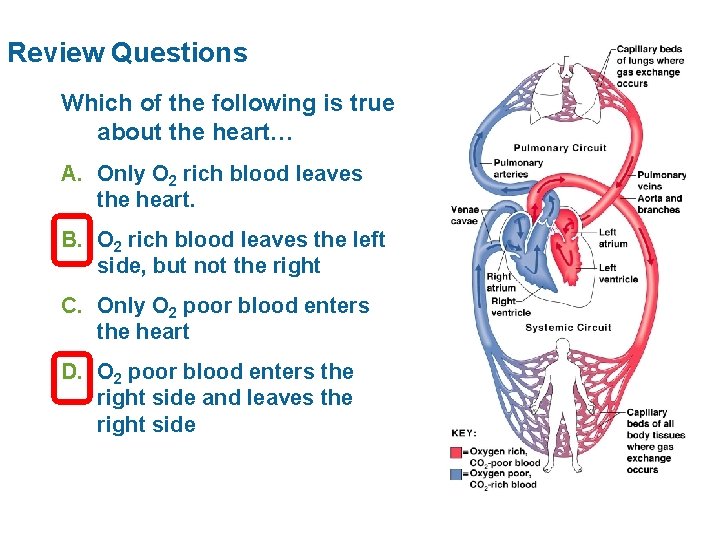
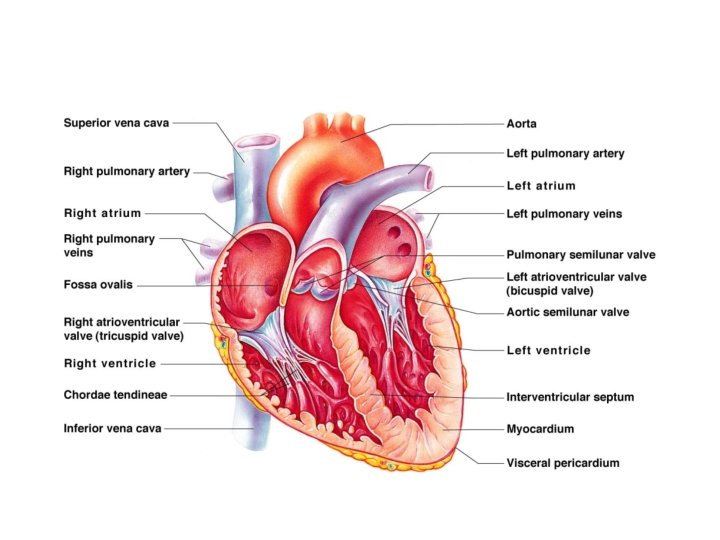
Review Questions Which of the following is true about the heart… A. Only O 2 rich blood leaves the heart. B. O 2 rich blood leaves the left side, but not the right C. Only O 2 poor blood enters the heart D. O 2 poor blood enters the right side and leaves the right side
Review Questions Atrioventricular (AV) valves prevent blood from _________ semilunar going back into the atria while _______ valves open to allow blood into arteries during pulmonary circuit ventricular contraction. The ______ systemic delivers blood to the lungs and the ______ circuit delivers to the rest of the body.
Review Questions SA node Heart rate is controlled primarily by the _____ because it spontaneously depolarizes at a faster rate than any other part of the conduction system. decreases Parasympathetic fibers ______ heart rate by hyper - polarizing the typical lower limit of the ______ opening extra K+ pacemaker potential by ______ channels. Sympathetic fibers increase ____ heart rate by, among depolarizing the pacemaker potential. other things, ______
Review Questions If the impulse from the SA node to the AV node is delayed, how would that effect the ECG? P-Q interval takes longer What does the QRS complex indicate? Ventricular depolarization Interference of signal transmission from SA to AV heart block node is known as ________.
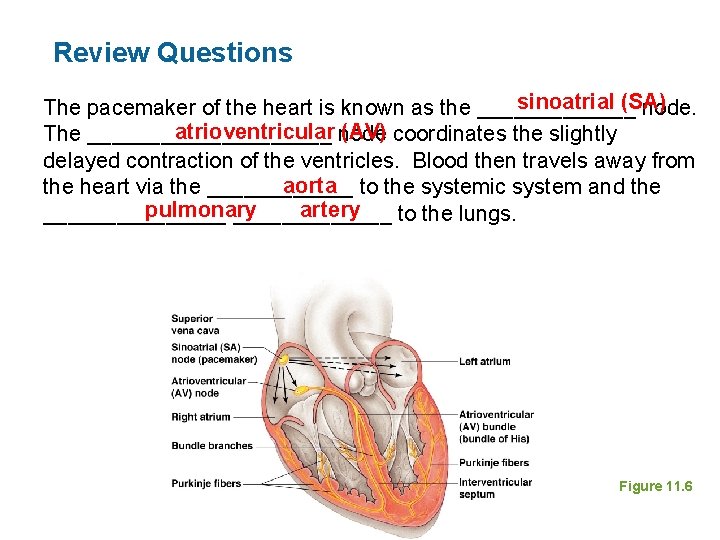
Review Questions sinoatrial (SA) The pacemaker of the heart is known as the _______ node. atrioventricular node (AV) coordinates the slightly The __________ delayed contraction of the ventricles. Blood then travels away from aorta to the systemic system and the heart via the ______ pulmonary artery ________ to the lungs. Figure 11. 6
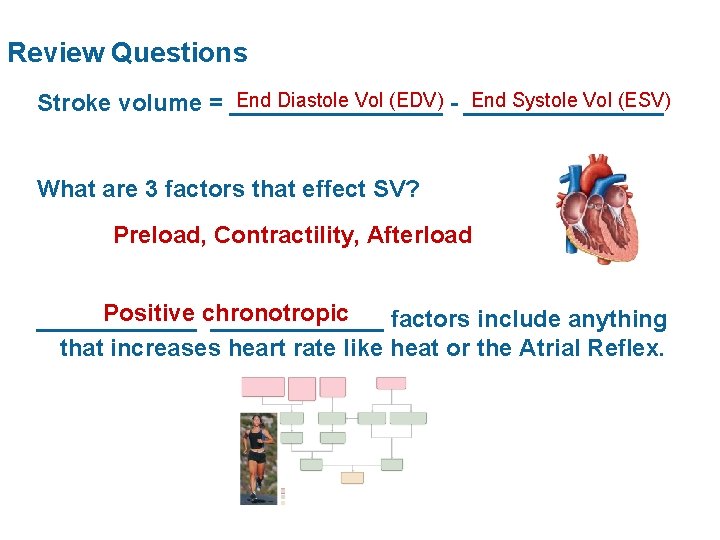
Review Questions End Diastole Vol (EDV) - ________ End Systole Vol (ESV) Stroke volume = ________ What are 3 factors that effect SV? Preload, Contractility, Afterload Positive chronotropic _____________ factors include anything that increases heart rate like heat or the Atrial Reflex.
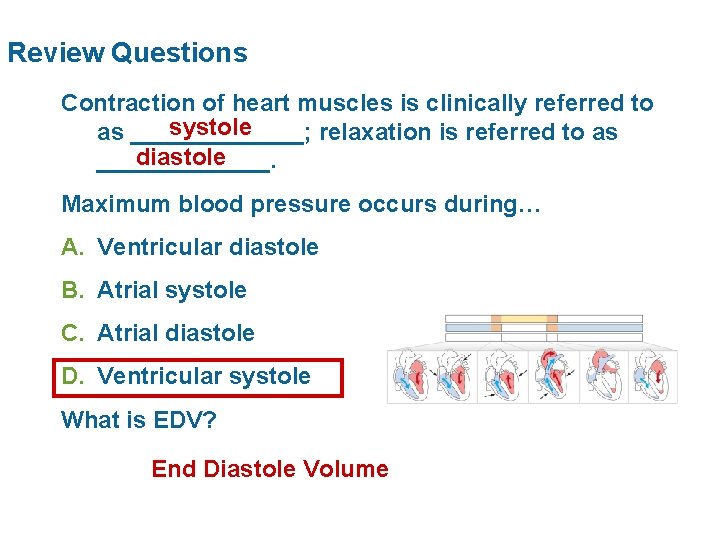
Review Questions Contraction of heart muscles is clinically referred to systole as _______; relaxation is referred to as diastole _______. Maximum blood pressure occurs during… A. Ventricular diastole B. Atrial systole C. Atrial diastole D. Ventricular systole What is EDV? End Diastole Volume
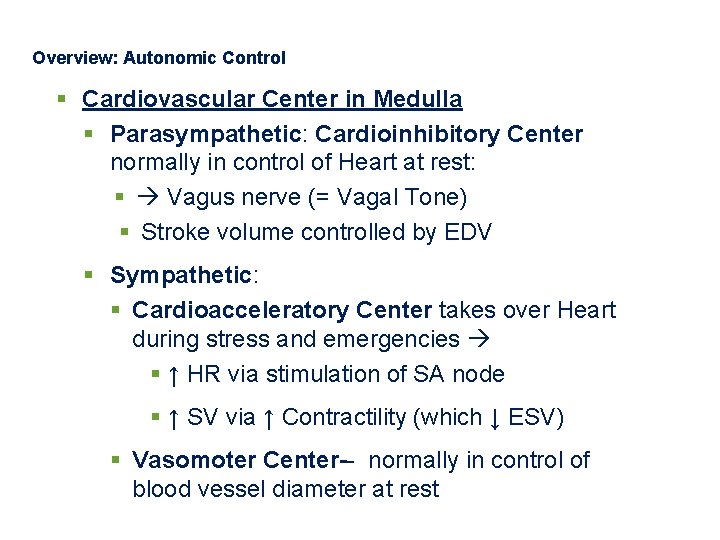
Overview: Autonomic Control § Cardiovascular Center in Medulla § Parasympathetic: Cardioinhibitory Center normally in control of Heart at rest: § Vagus nerve (= Vagal Tone) § Stroke volume controlled by EDV § Sympathetic: § Cardioacceleratory Center takes over Heart during stress and emergencies § ↑ HR via stimulation of SA node § ↑ SV via ↑ Contractility (which ↓ ESV) § Vasomoter Center-- normally in control of blood vessel diameter at rest
- Slides: 24