Cysts part 1 DR MARIYAM FIDHA CONTENTS INTRODUCTION





















- Slides: 85
Cysts – part 1 DR. MARIYAM FIDHA

CONTENTS • • INTRODUCTION HISTORY CLASSIFICATION DEVELOPMENT OF CYST • • • RADICULAR CYST DENTIGEROUS CYST GINGIVAL CYST OF ADULTS GINGIVAL CYST OF INFANT CALCIFYING ODONTOGENIC CYST LATERAL PERIODONTAL CYST ANEURYSMAL BONE CYST SOLITARY BONE CYST ODONTOGENIC KERATOCYST • ODONTOGENIC KERATOCYST • REFERENCES DR. MARIYAM FIDHA
INTRODUCTION ü Greek word – “kystis” means bladder ü Unilocular or Multilocular sac like lesions enclosed by a capsule DR. MARIYAM FIDHA
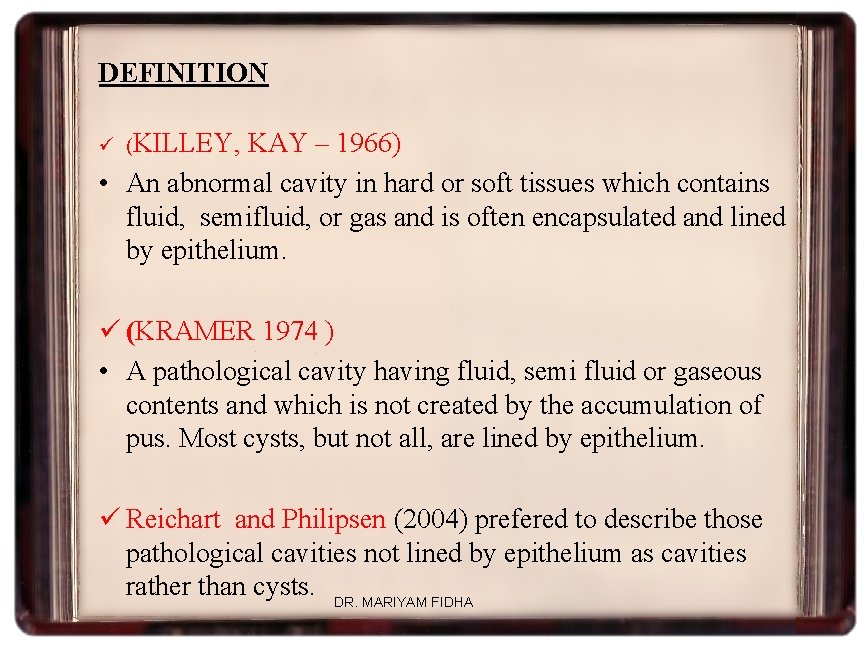
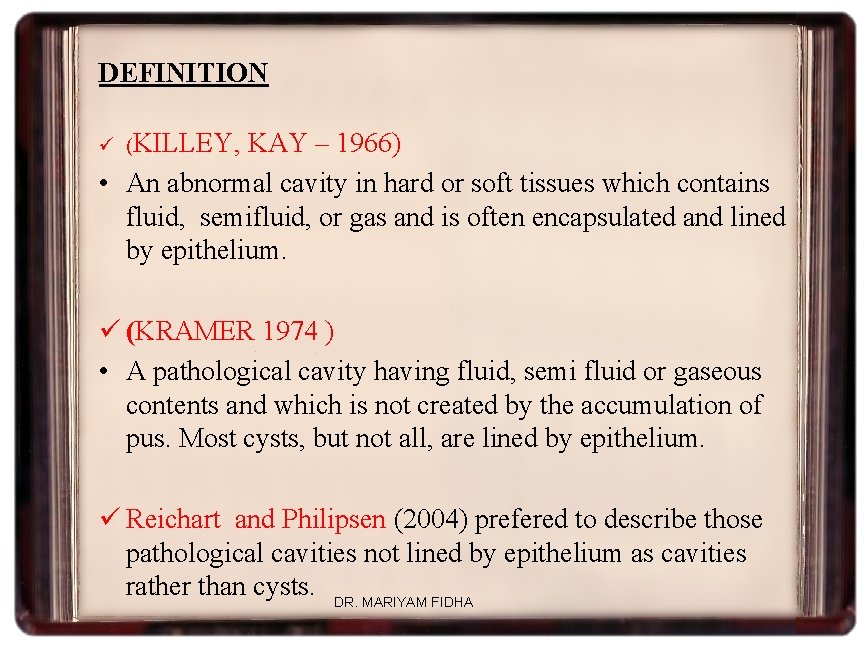
DEFINITION ü (KILLEY, KAY – 1966) • An abnormal cavity in hard or soft tissues which contains fluid, semifluid, or gas and is often encapsulated and lined by epithelium. ü (KRAMER 1974 ) • A pathological cavity having fluid, semi fluid or gaseous contents and which is not created by the accumulation of pus. Most cysts, but not all, are lined by epithelium. ü Reichart and Philipsen (2004) prefered to describe those pathological cavities not lined by epithelium as cavities rather than cysts. DR. MARIYAM FIDHA
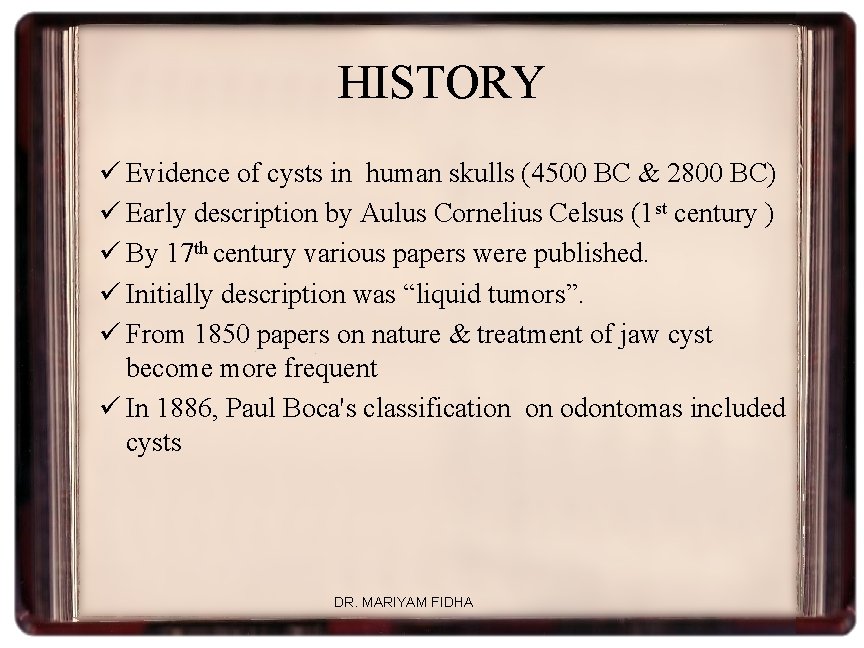
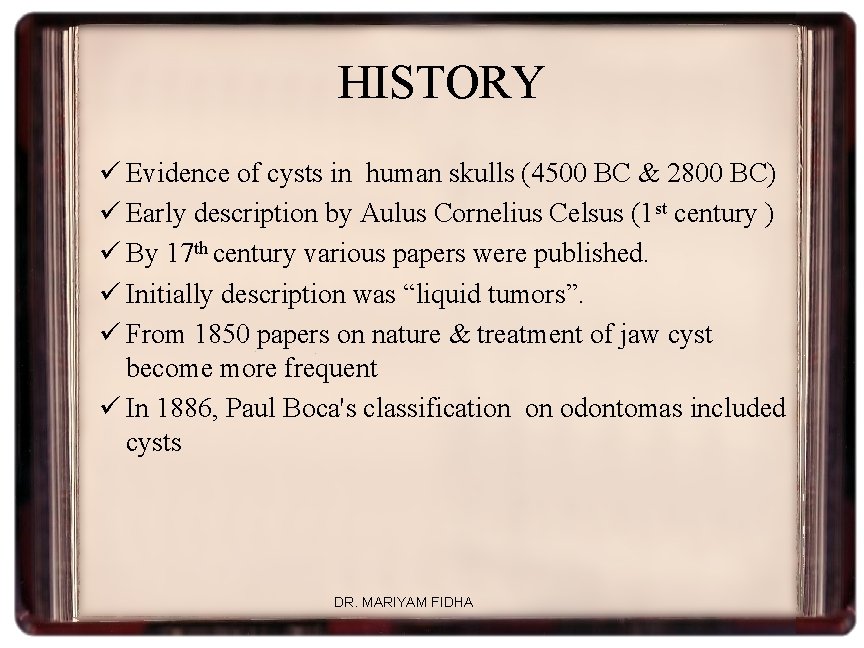
HISTORY ü Evidence of cysts in human skulls (4500 BC & 2800 BC) ü Early description by Aulus Cornelius Celsus (1 st century ) ü By 17 th century various papers were published. ü Initially description was “liquid tumors”. ü From 1850 papers on nature & treatment of jaw cyst become more frequent ü In 1886, Paul Boca's classification on odontomas included cysts DR. MARIYAM FIDHA
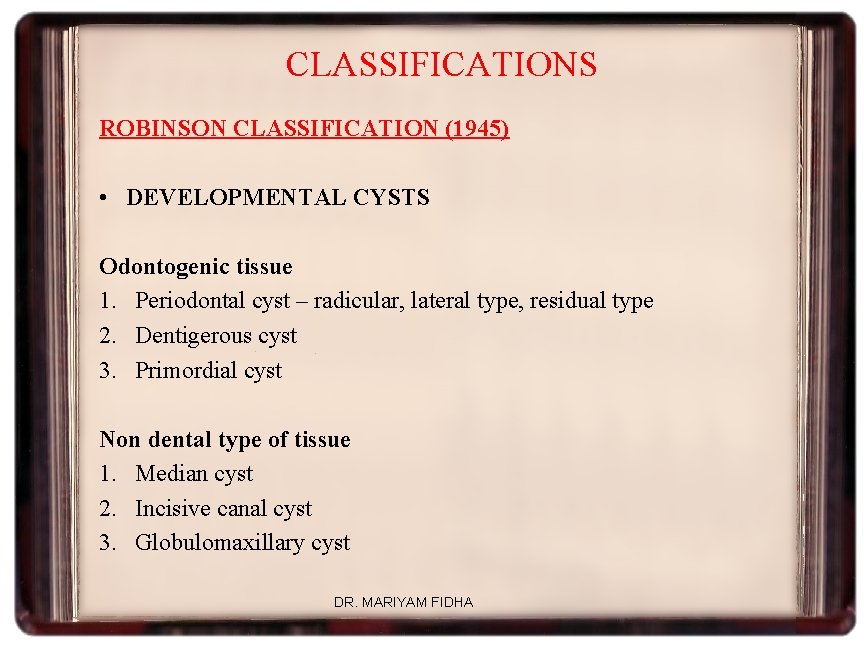
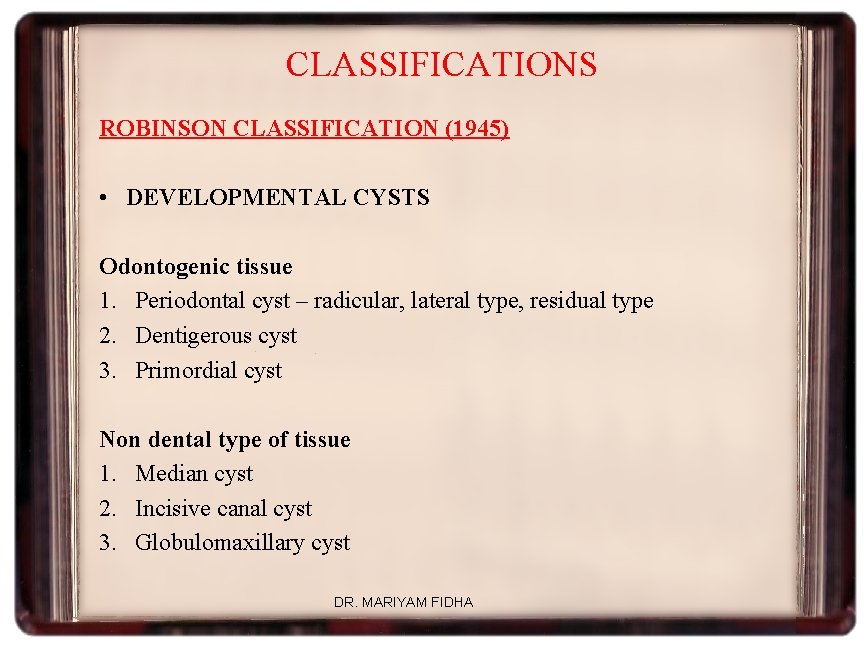
CLASSIFICATIONS ROBINSON CLASSIFICATION (1945) • DEVELOPMENTAL CYSTS Odontogenic tissue 1. Periodontal cyst – radicular, lateral type, residual type 2. Dentigerous cyst 3. Primordial cyst Non dental type of tissue 1. Median cyst 2. Incisive canal cyst 3. Globulomaxillary cyst DR. MARIYAM FIDHA

KRUGER CLASSIFICATION (1964) CONGENITAL CYST 1. Thyroglossal 2. Branchiogenic 3. Dermoid DEVELOPMENTAL 1. NON DENTAL ORIGIN a) Fissural type : nasoalveolar, median, incisive canal & globlomaxillary cysts b) Retention type: mucocele, ranula 2. DENTAL ORIGIN a) Periodontal b) Primordial c) Dentigerous DR. MARIYAM FIDHA
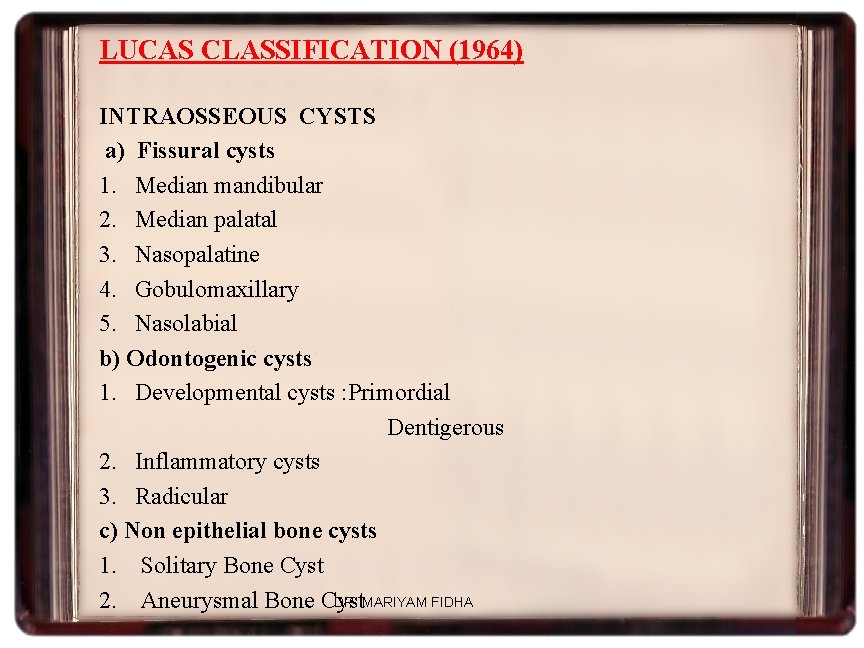
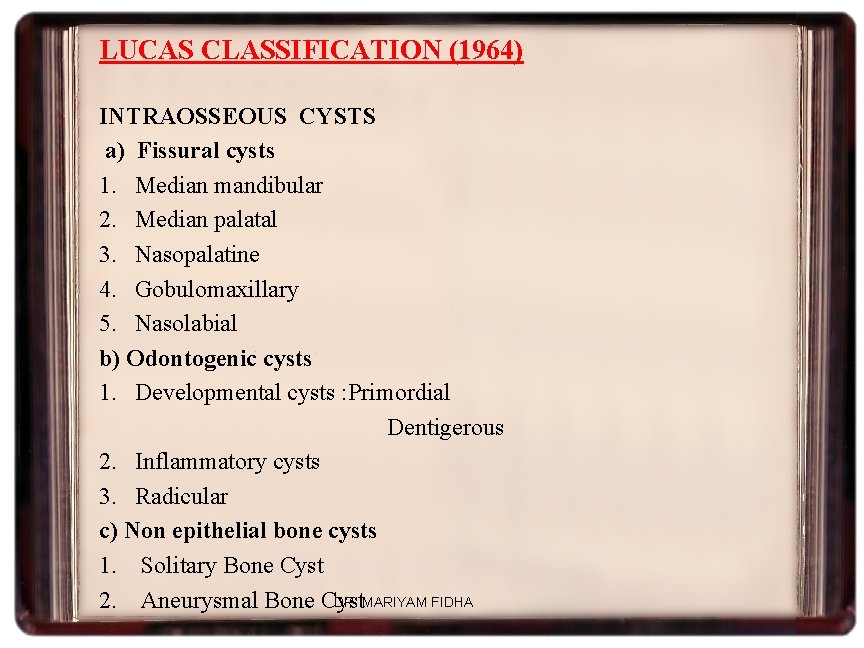
LUCAS CLASSIFICATION (1964) INTRAOSSEOUS CYSTS a) Fissural cysts 1. Median mandibular 2. Median palatal 3. Nasopalatine 4. Gobulomaxillary 5. Nasolabial b) Odontogenic cysts 1. Developmental cysts : Primordial Dentigerous 2. Inflammatory cysts 3. Radicular c) Non epithelial bone cysts 1. Solitary Bone Cyst DR. MARIYAM FIDHA 2. Aneurysmal Bone Cyst
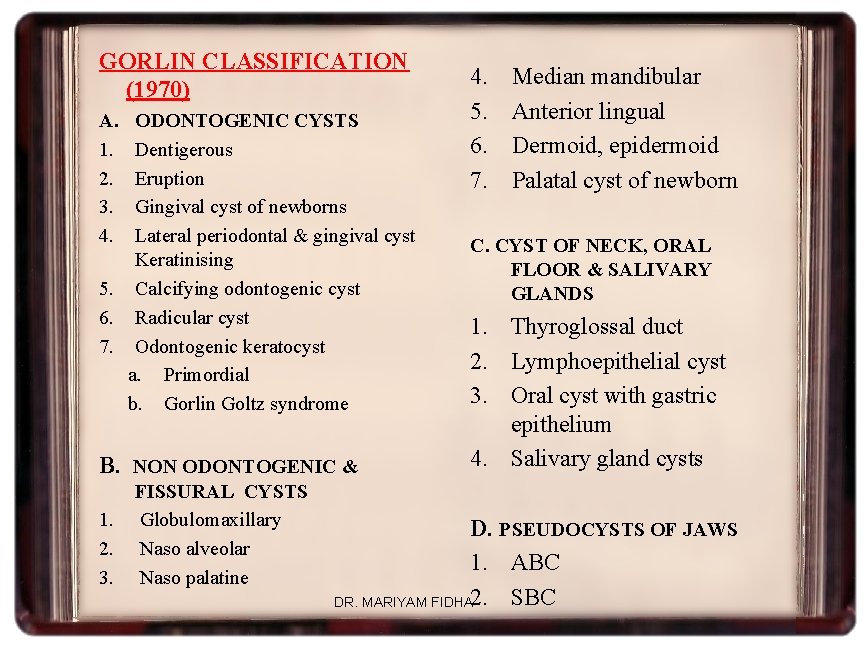
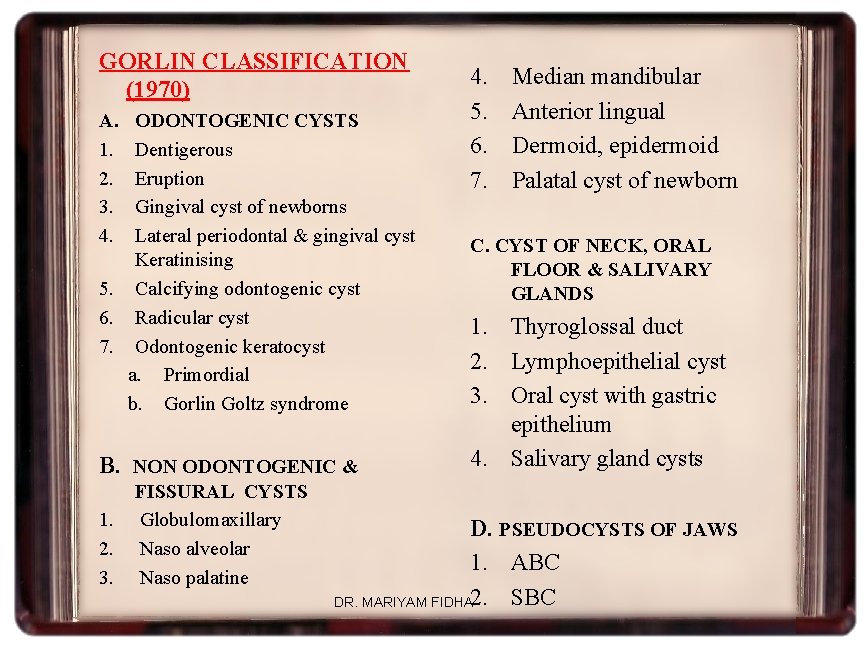
GORLIN CLASSIFICATION (1970) A. 1. 2. 3. 4. ODONTOGENIC CYSTS Dentigerous Eruption Gingival cyst of newborns Lateral periodontal & gingival cyst Keratinising 5. Calcifying odontogenic cyst 6. Radicular cyst 7. Odontogenic keratocyst a. Primordial b. Gorlin Goltz syndrome B. NON ODONTOGENIC & 1. 2. 3. FISSURAL CYSTS Globulomaxillary Naso alveolar Naso palatine 4. 5. 6. 7. Median mandibular Anterior lingual Dermoid, epidermoid Palatal cyst of newborn C. CYST OF NECK, ORAL FLOOR & SALIVARY GLANDS 1. Thyroglossal duct 2. Lymphoepithelial cyst 3. Oral cyst with gastric epithelium 4. Salivary gland cysts D. PSEUDOCYSTS OF JAWS 1. ABC SBC DR. MARIYAM FIDHA 2.
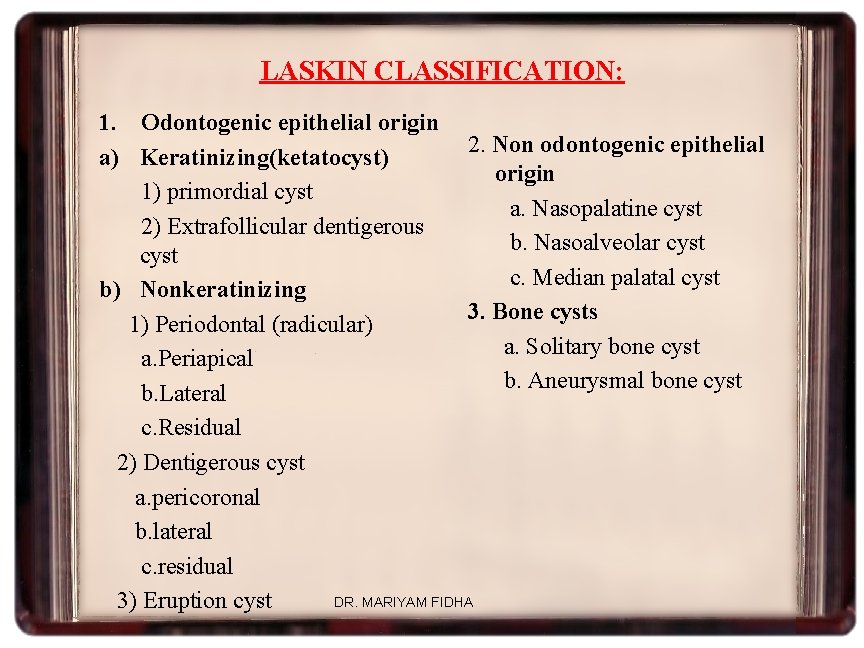
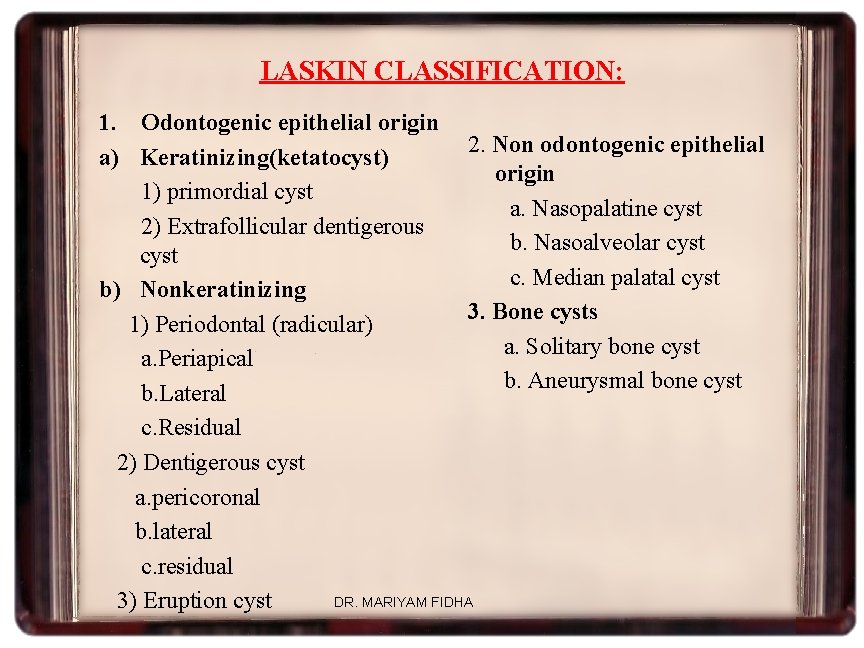
LASKIN CLASSIFICATION: 1. Odontogenic epithelial origin 2. Non odontogenic epithelial a) Keratinizing(ketatocyst) origin 1) primordial cyst a. Nasopalatine cyst 2) Extrafollicular dentigerous b. Nasoalveolar cyst c. Median palatal cyst b) Nonkeratinizing 3. Bone cysts 1) Periodontal (radicular) a. Solitary bone cyst a. Periapical b. Aneurysmal bone cyst b. Lateral c. Residual 2) Dentigerous cyst a. pericoronal b. lateral c. residual DR. MARIYAM FIDHA 3) Eruption cyst
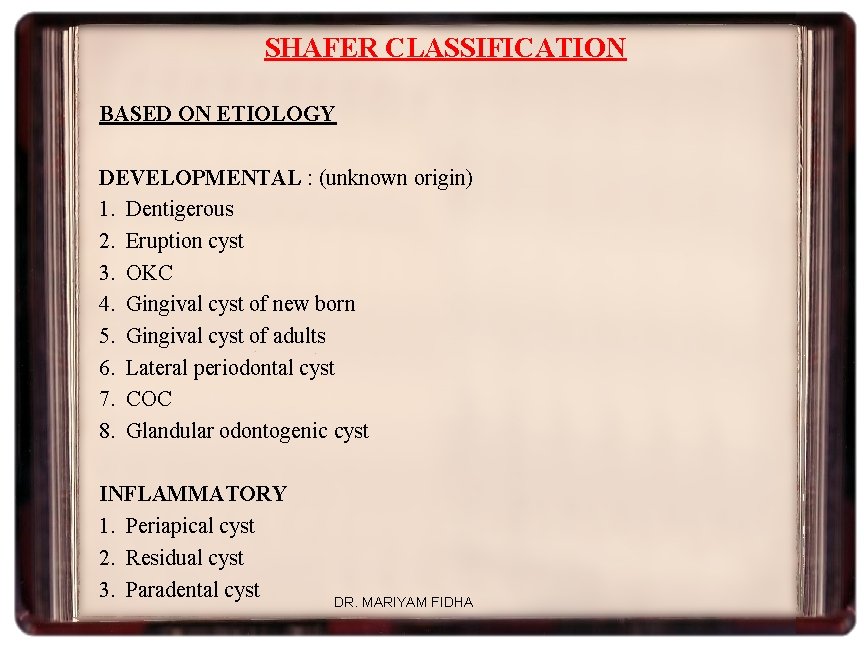
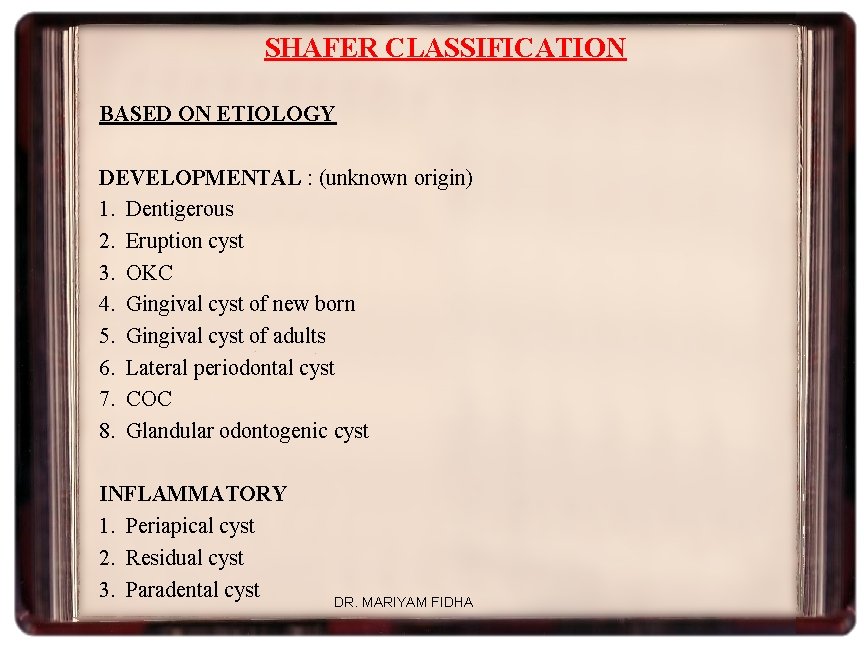
SHAFER CLASSIFICATION BASED ON ETIOLOGY DEVELOPMENTAL : (unknown origin) 1. Dentigerous 2. Eruption cyst 3. OKC 4. Gingival cyst of new born 5. Gingival cyst of adults 6. Lateral periodontal cyst 7. COC 8. Glandular odontogenic cyst INFLAMMATORY 1. Periapical cyst 2. Residual cyst 3. Paradental cyst DR. MARIYAM FIDHA
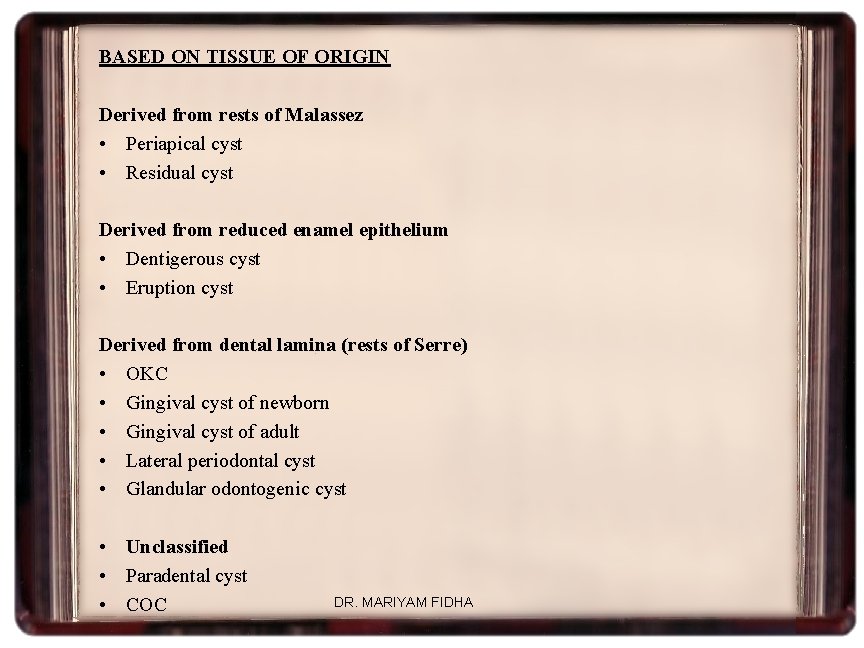
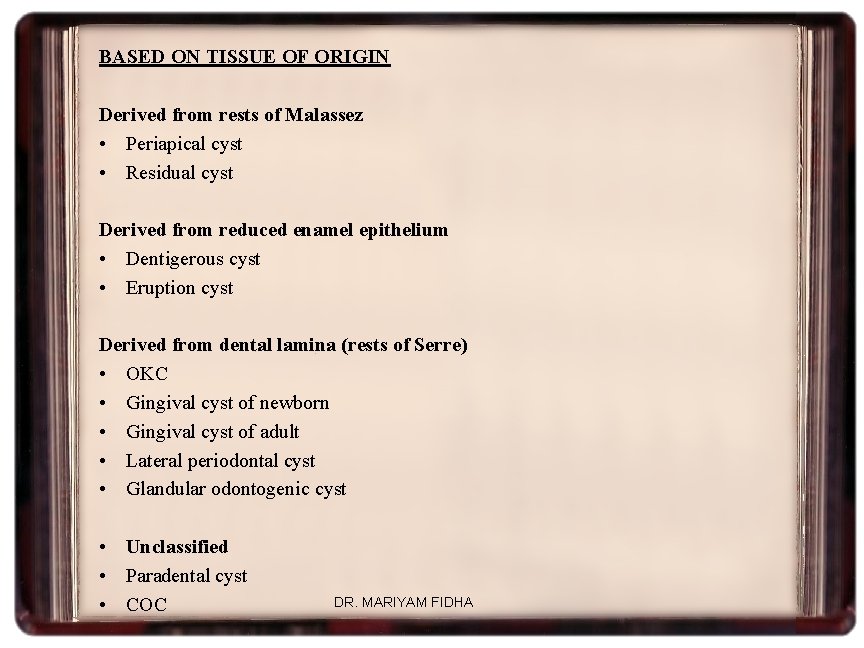
BASED ON TISSUE OF ORIGIN Derived from rests of Malassez • Periapical cyst • Residual cyst Derived from reduced enamel epithelium • Dentigerous cyst • Eruption cyst Derived from dental lamina (rests of Serre) • OKC • Gingival cyst of newborn • Gingival cyst of adult • Lateral periodontal cyst • Glandular odontogenic cyst • Unclassified • Paradental cyst • COC DR. MARIYAM FIDHA
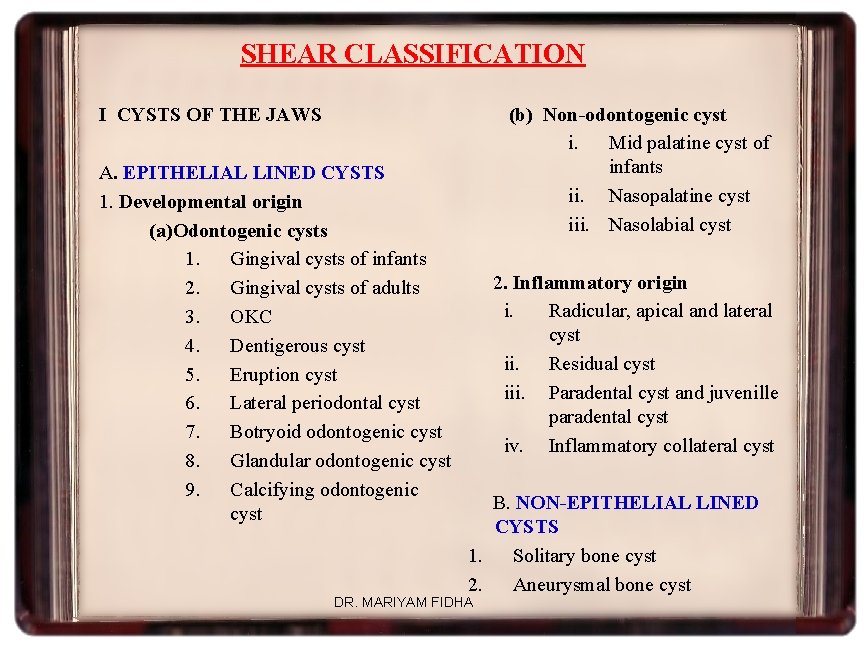
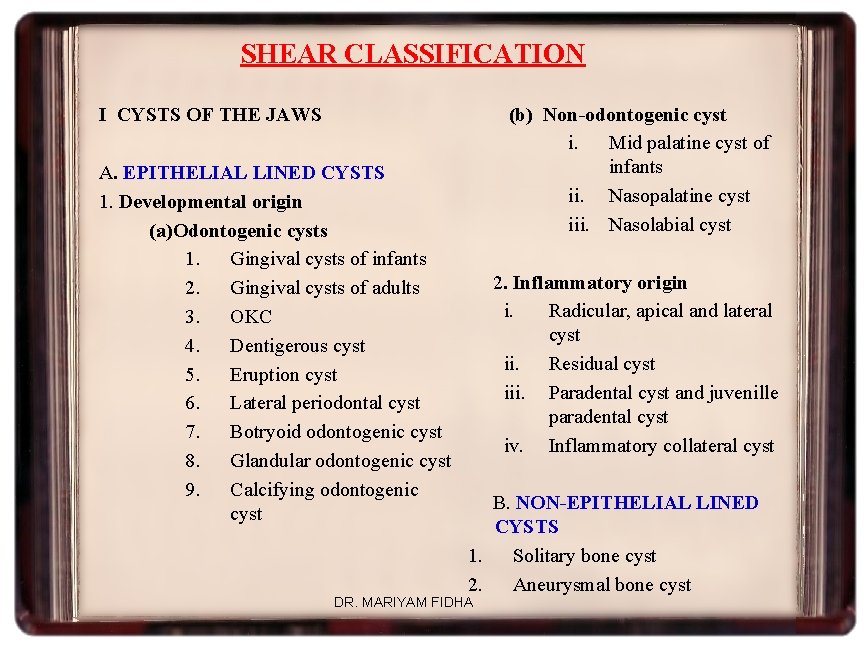
SHEAR CLASSIFICATION (b) Non-odontogenic cyst i. Mid palatine cyst of infants ii. Nasopalatine cyst iii. Nasolabial cyst I CYSTS OF THE JAWS A. EPITHELIAL LINED CYSTS 1. Developmental origin (a)Odontogenic cysts 1. Gingival cysts of infants 2. Gingival cysts of adults 3. OKC 4. Dentigerous cyst 5. Eruption cyst 6. Lateral periodontal cyst 7. Botryoid odontogenic cyst 8. Glandular odontogenic cyst 9. Calcifying odontogenic cyst 2. Inflammatory origin i. Radicular, apical and lateral cyst ii. Residual cyst iii. Paradental cyst and juvenille paradental cyst iv. Inflammatory collateral cyst B. NON-EPITHELIAL LINED CYSTS 1. Solitary bone cyst 2. Aneurysmal bone cyst DR. MARIYAM FIDHA
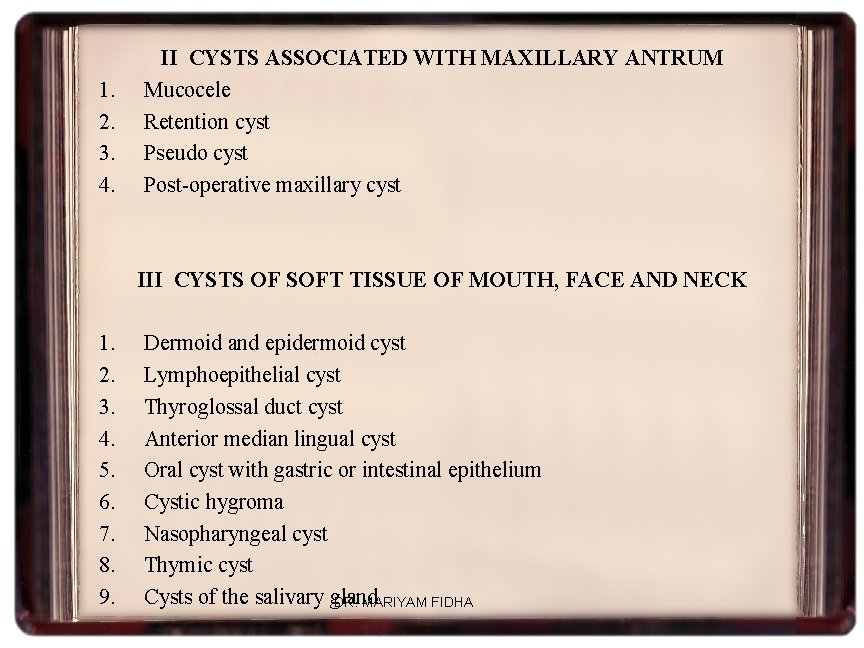
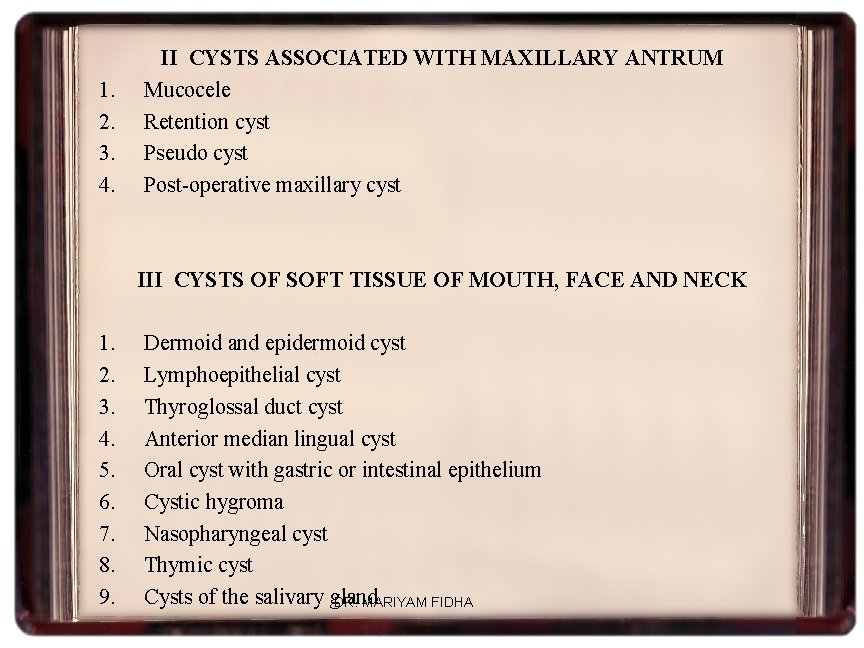
1. 2. 3. 4. II CYSTS ASSOCIATED WITH MAXILLARY ANTRUM Mucocele Retention cyst Pseudo cyst Post-operative maxillary cyst III CYSTS OF SOFT TISSUE OF MOUTH, FACE AND NECK 1. 2. 3. 4. 5. 6. 7. 8. 9. Dermoid and epidermoid cyst Lymphoepithelial cyst Thyroglossal duct cyst Anterior median lingual cyst Oral cyst with gastric or intestinal epithelium Cystic hygroma Nasopharyngeal cyst Thymic cyst Cysts of the salivary gland DR. MARIYAM FIDHA
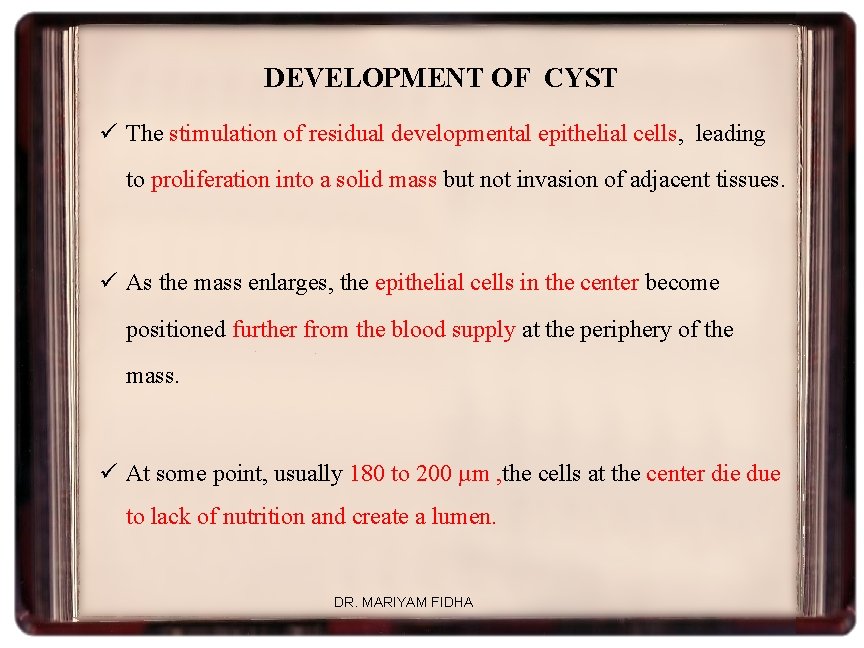
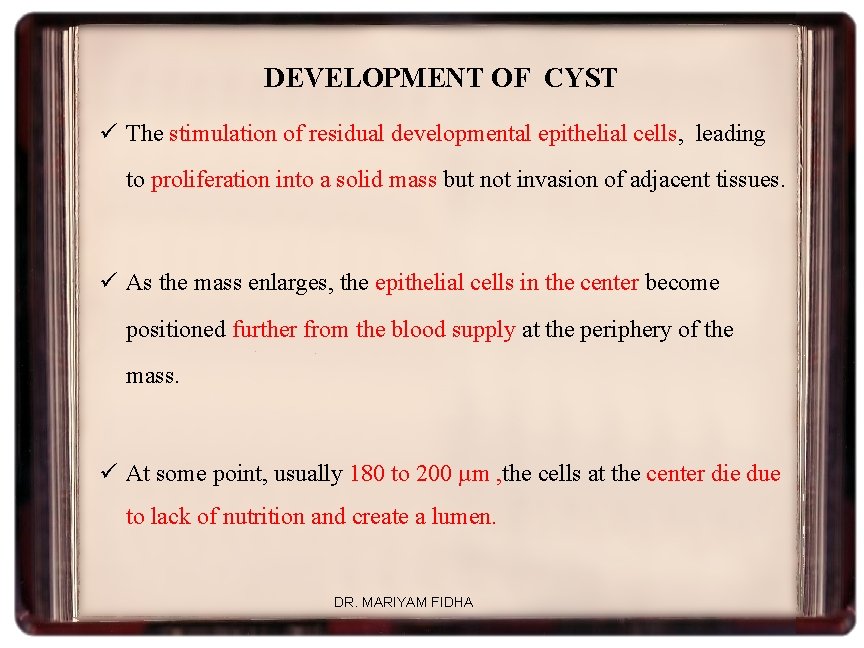
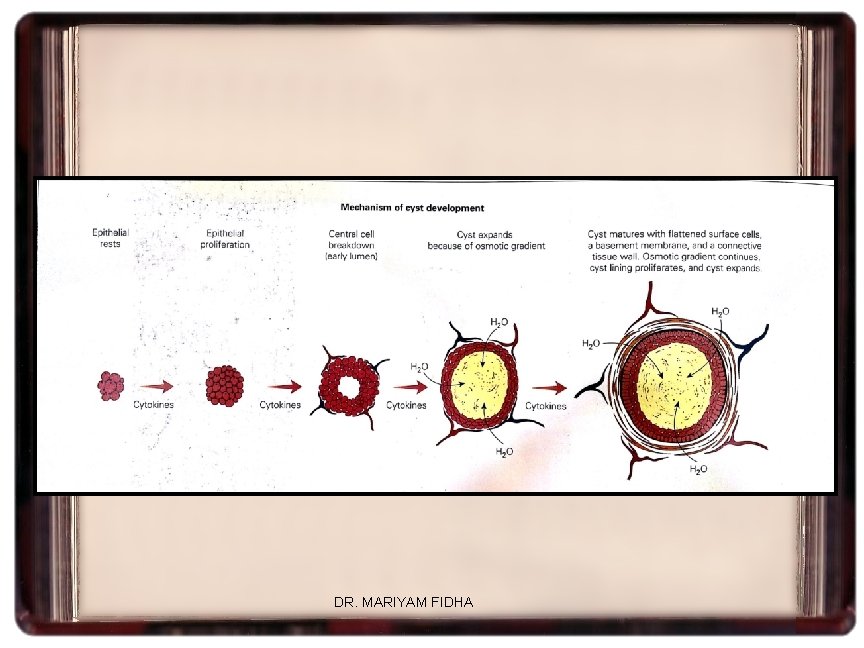
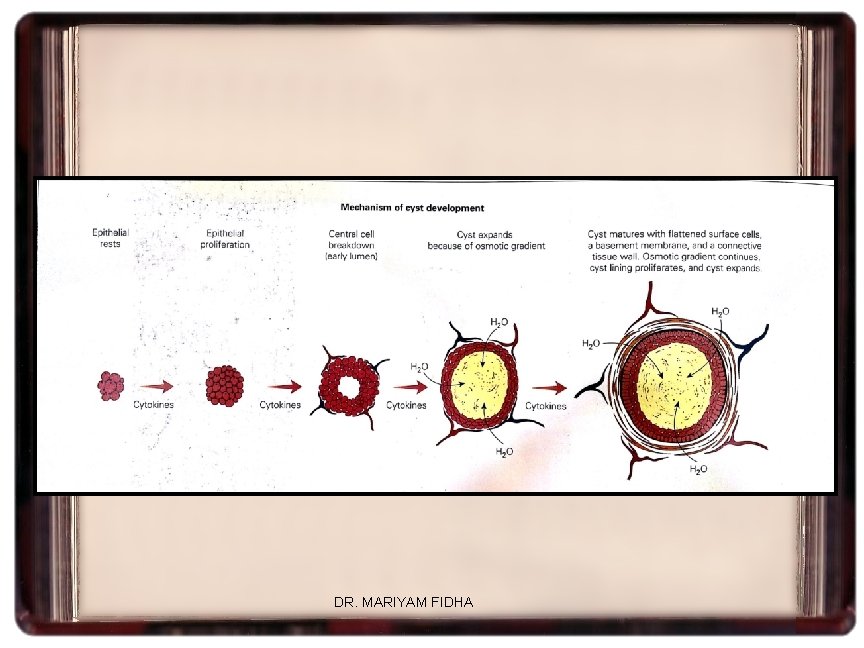
DEVELOPMENT OF CYST ü The stimulation of residual developmental epithelial cells, leading to proliferation into a solid mass but not invasion of adjacent tissues. ü As the mass enlarges, the epithelial cells in the center become positioned further from the blood supply at the periphery of the mass. ü At some point, usually 180 to 200 µm , the cells at the center die due to lack of nutrition and create a lumen. DR. MARIYAM FIDHA
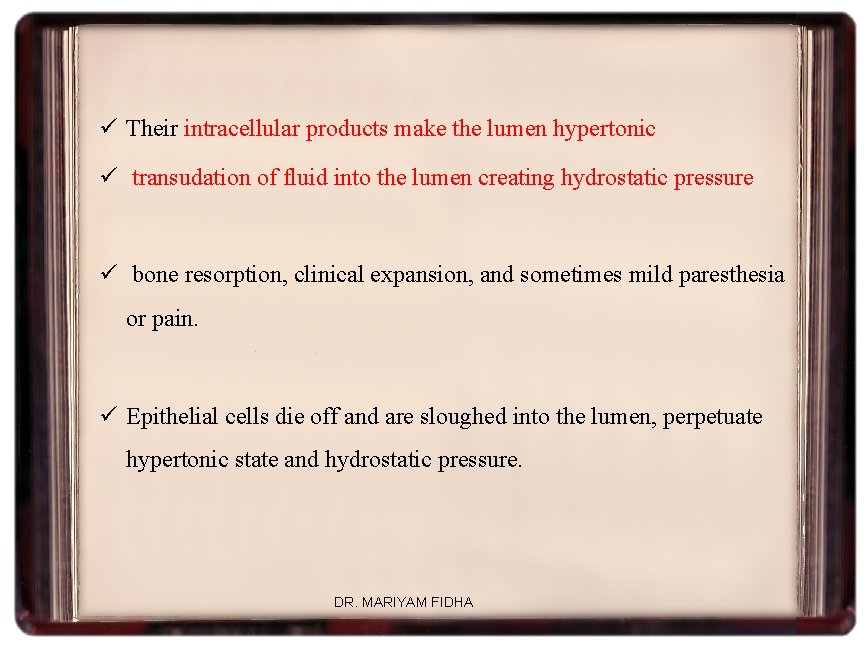
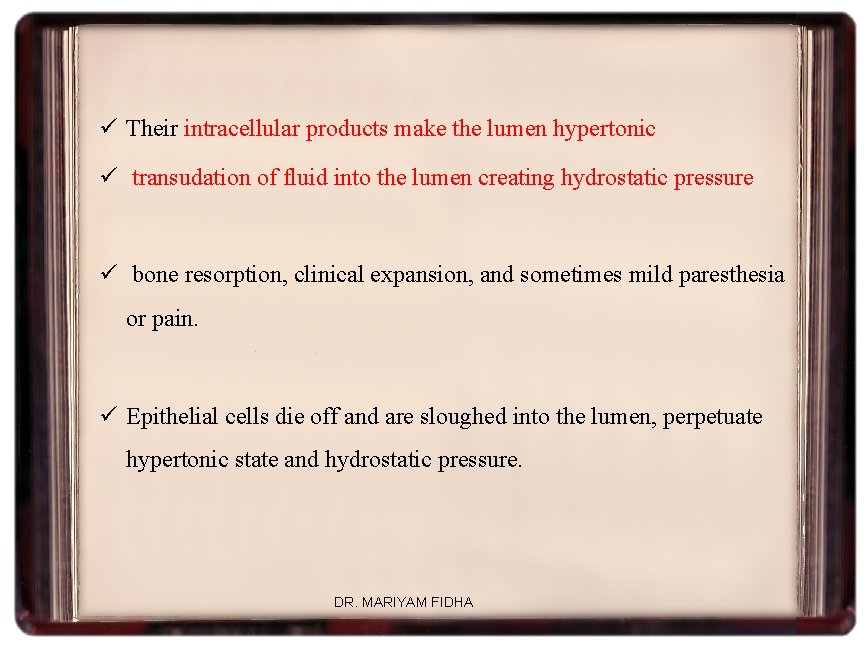
ü Their intracellular products make the lumen hypertonic ü transudation of fluid into the lumen creating hydrostatic pressure ü bone resorption, clinical expansion, and sometimes mild paresthesia or pain. ü Epithelial cells die off and are sloughed into the lumen, perpetuate hypertonic state and hydrostatic pressure. DR. MARIYAM FIDHA

ü The cell membranes and nuclear membranes of these sloughed cells are high in cholesterol hence the common finding of cholesterol clefts in the lumen or even in the wall of the cyst. ü As the cyst enlarges, it compresses surrounding connective tissue into a connective tissue wall. ü The epithelial lining matures and develops a basement membrane DR. MARIYAM FIDHA
DR. MARIYAM FIDHA
RADICULAR CYST Etiology : INFLAMMATION KEY FACTORS: a) Bacterial endotoxins from necrotic pulp (Meghji et al 1992) b) Inflammatory cytokines (humoral immunity) ü Ig. G is predominant class of immunoglobulin ü Smith et al (1987) - 85% Ig. G, 14% Ig A & 2% Ig. M in RC ü C 3 complement c) Cellular immune reactions: ü T lymphocytes > B lymphocytes ü Liapatas et al 2003 : CD 4 > CD 8 DR. MARIYAM FIDHA
d) Bone resorbing factors • • Meghji et al 1989 - Bone resorbing factor that had IL-1 activity Bando et al 1993 – IHC – IL 1α, IL 1β & IL 6 – epithelial lining & vascular endothelial cells. – TNF & IL 8 – macrophages – ICAM & ELAM 1 – endothelial cells e) Local changes in supporting CT - Grupe et al 1987 DR. MARIYAM FIDHA
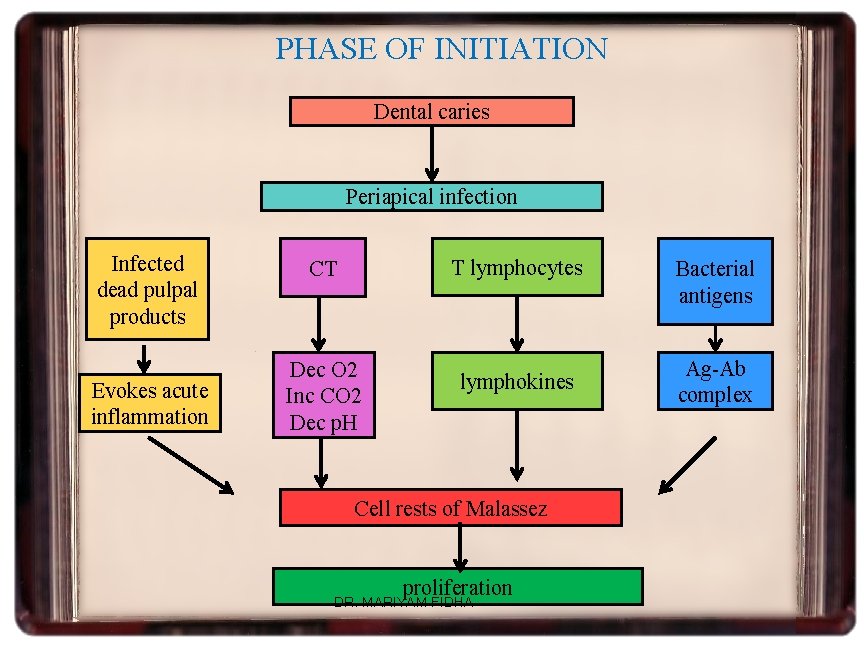
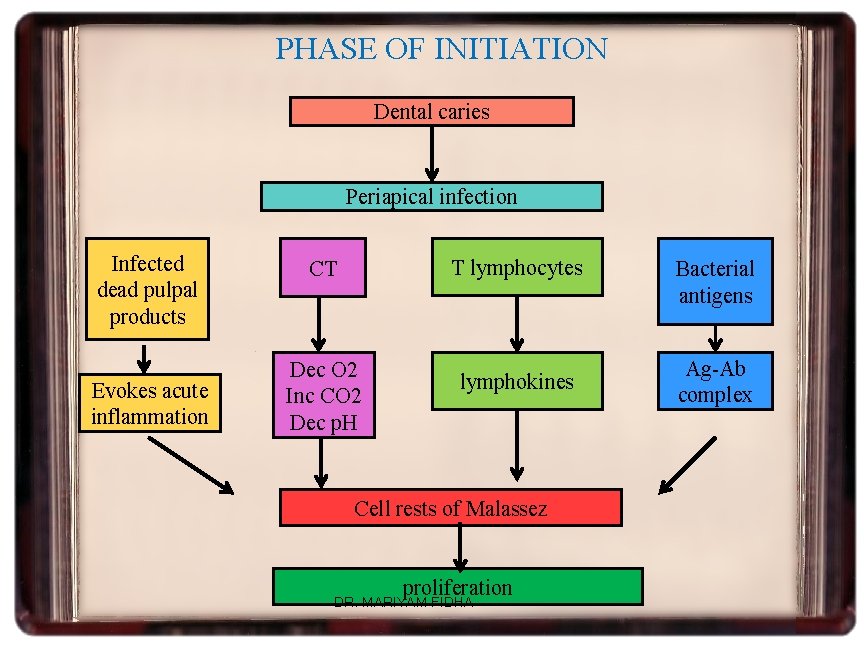
PHASE OF INITIATION Dental caries Periapical infection Infected dead pulpal products Evokes acute inflammation T lymphocytes CT Dec O 2 Inc CO 2 Dec p. H lymphokines Cell rests of Malassez proliferation DR. MARIYAM FIDHA Bacterial antigens Ag-Ab complex
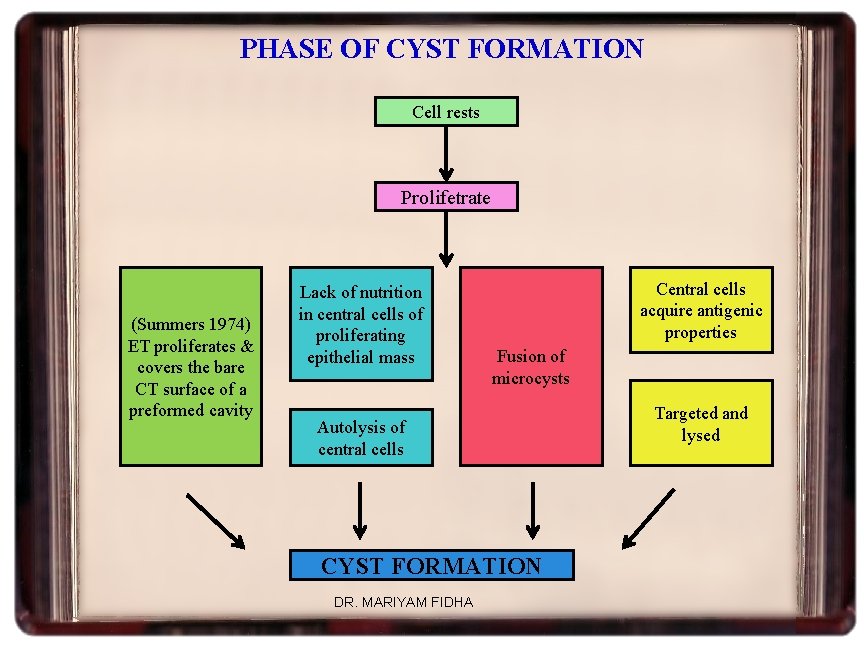
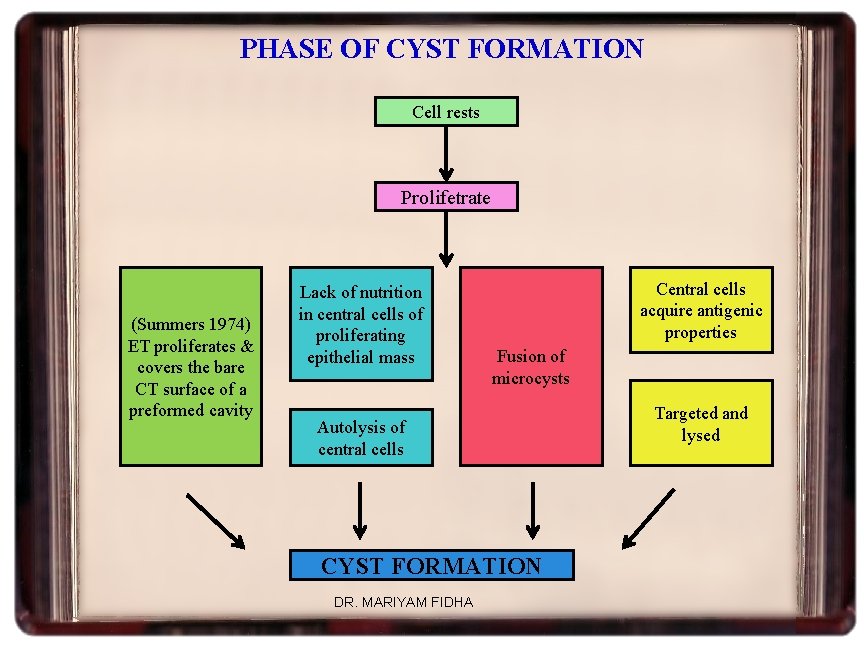
PHASE OF CYST FORMATION Cell rests Prolifetrate (Summers 1974) ET proliferates & covers the bare CT surface of a preformed cavity Lack of nutrition in central cells of proliferating epithelial mass Central cells acquire antigenic properties Fusion of microcysts Autolysis of central cells CYST FORMATION DR. MARIYAM FIDHA Targeted and lysed
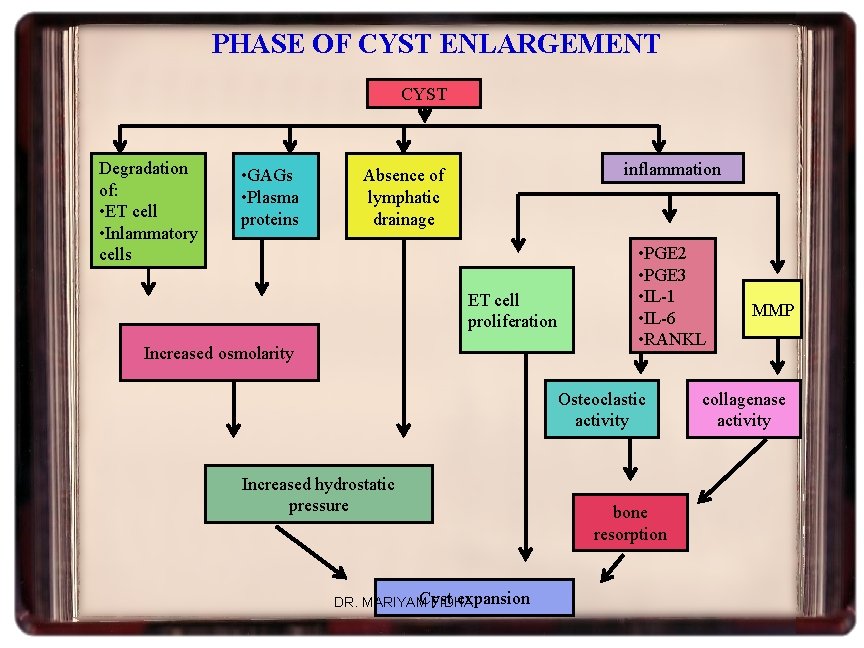
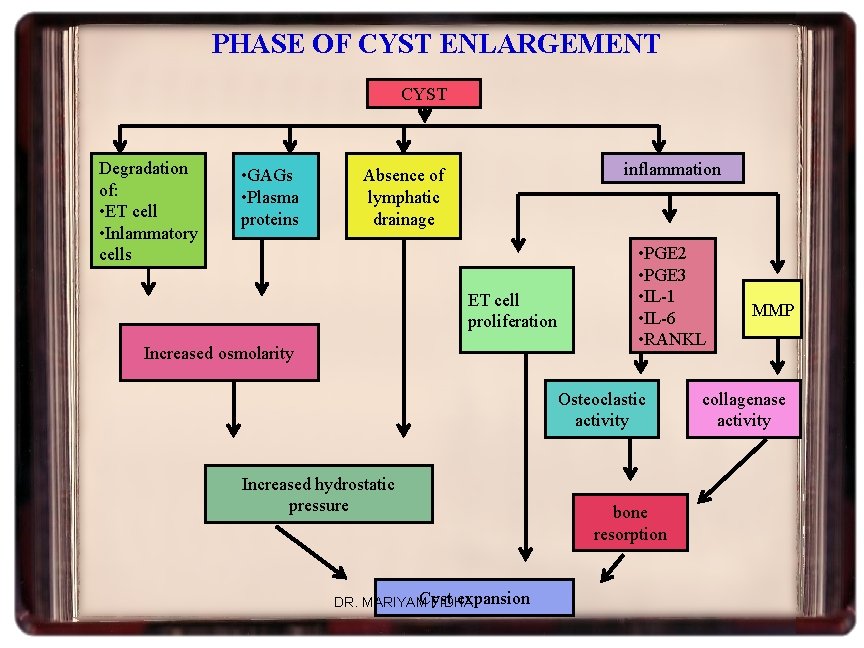
PHASE OF CYST ENLARGEMENT CYST Degradation of: • ET cell • Inlammatory cells • GAGs • Plasma proteins inflammation Absence of lymphatic drainage ET cell proliferation Increased osmolarity • PGE 2 • PGE 3 • IL-1 • IL-6 • RANKL Osteoclastic activity Increased hydrostatic pressure Cyst expansion DR. MARIYAM FIDHA bone resorption MMP collagenase activity
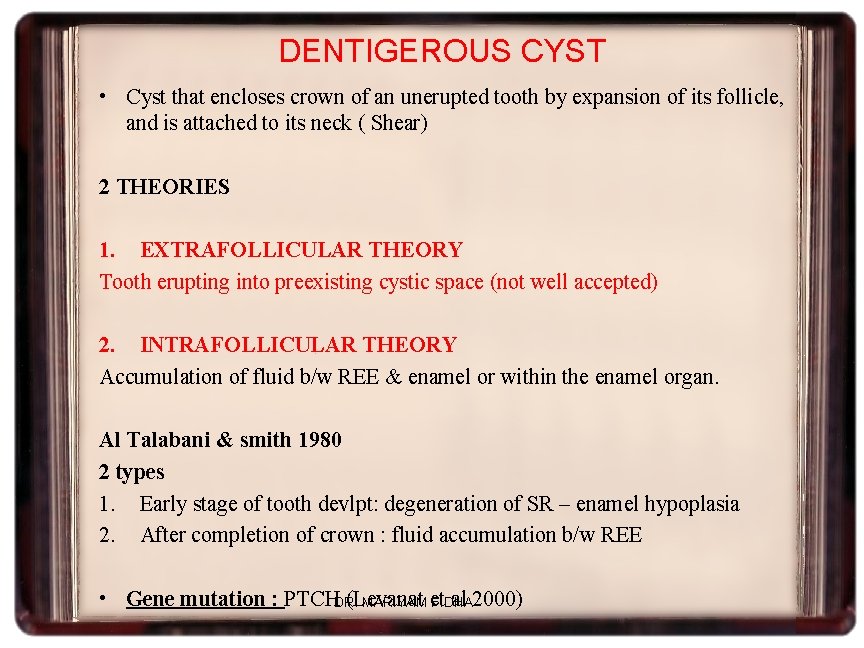
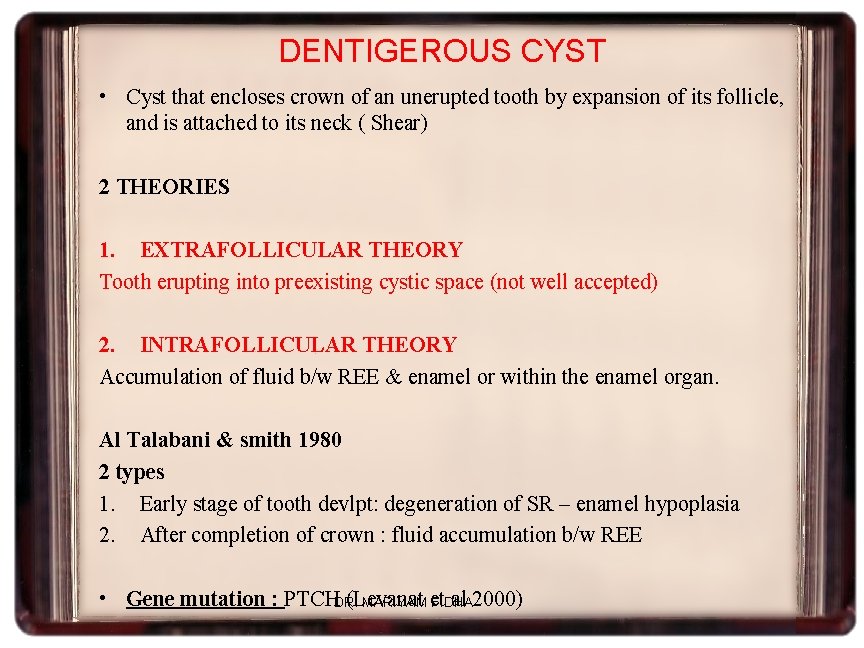
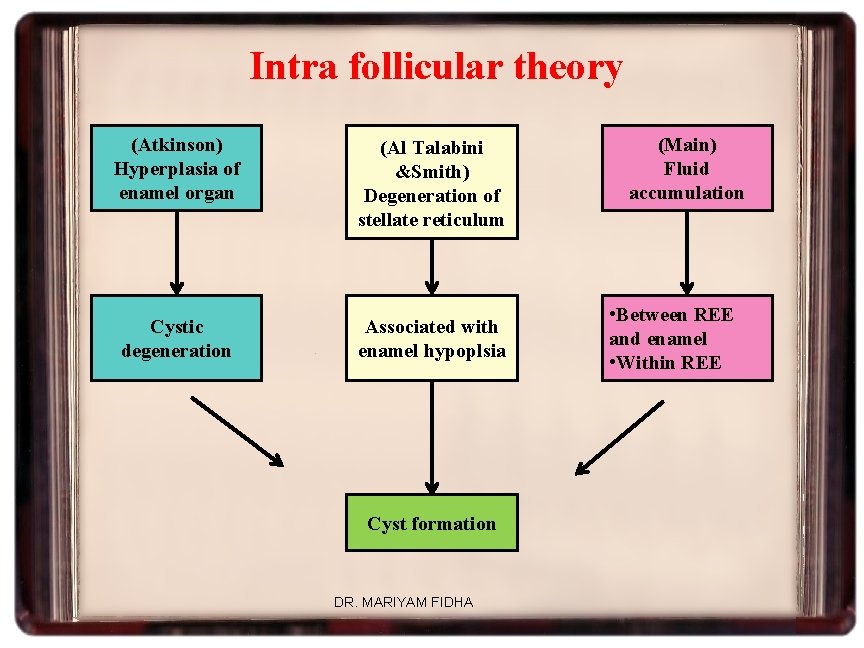
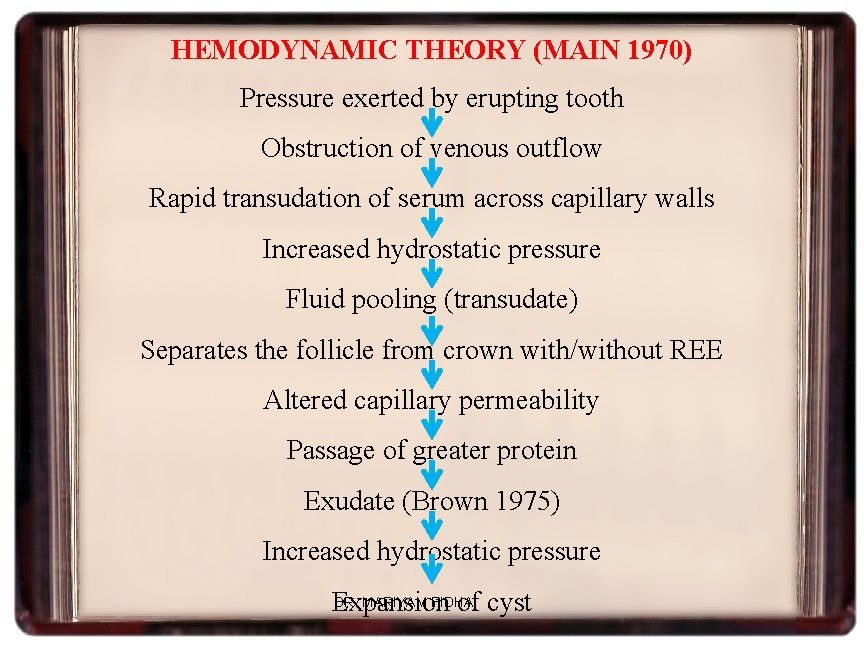
DENTIGEROUS CYST • Cyst that encloses crown of an unerupted tooth by expansion of its follicle, and is attached to its neck ( Shear) 2 THEORIES 1. EXTRAFOLLICULAR THEORY Tooth erupting into preexisting cystic space (not well accepted) 2. INTRAFOLLICULAR THEORY Accumulation of fluid b/w REE & enamel or within the enamel organ. Al Talabani & smith 1980 2 types 1. Early stage of tooth devlpt: degeneration of SR – enamel hypoplasia 2. After completion of crown : fluid accumulation b/w REE • Gene mutation : PTCHDR. (Levanat al 2000) MARIYAM et FIDHA
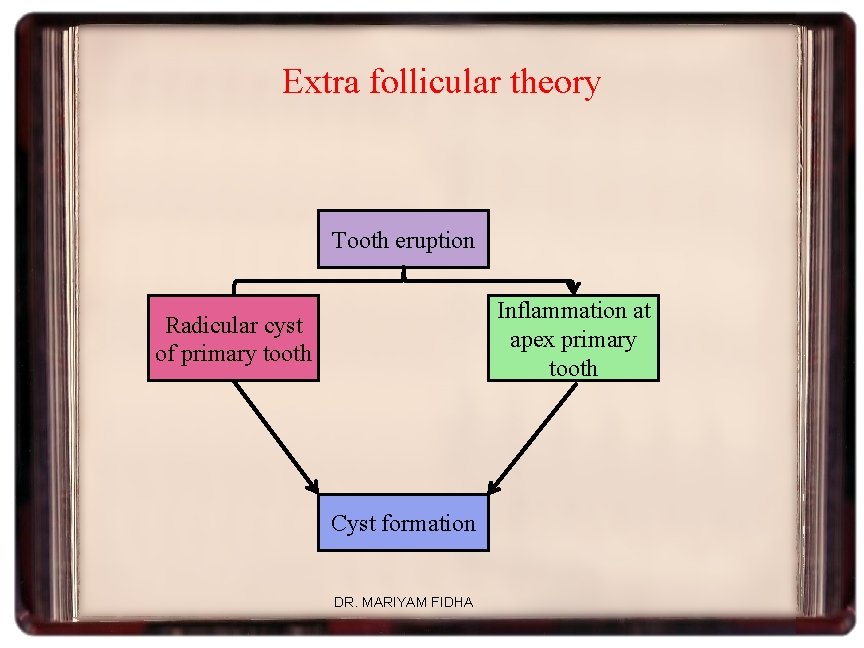
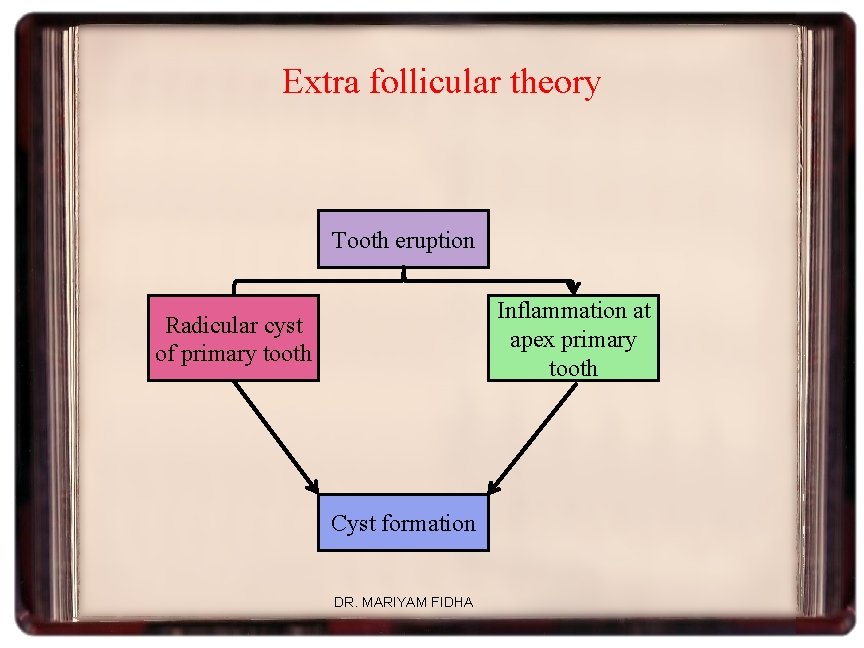
Extra follicular theory Tooth eruption Inflammation at apex primary tooth Radicular cyst of primary tooth Cyst formation DR. MARIYAM FIDHA
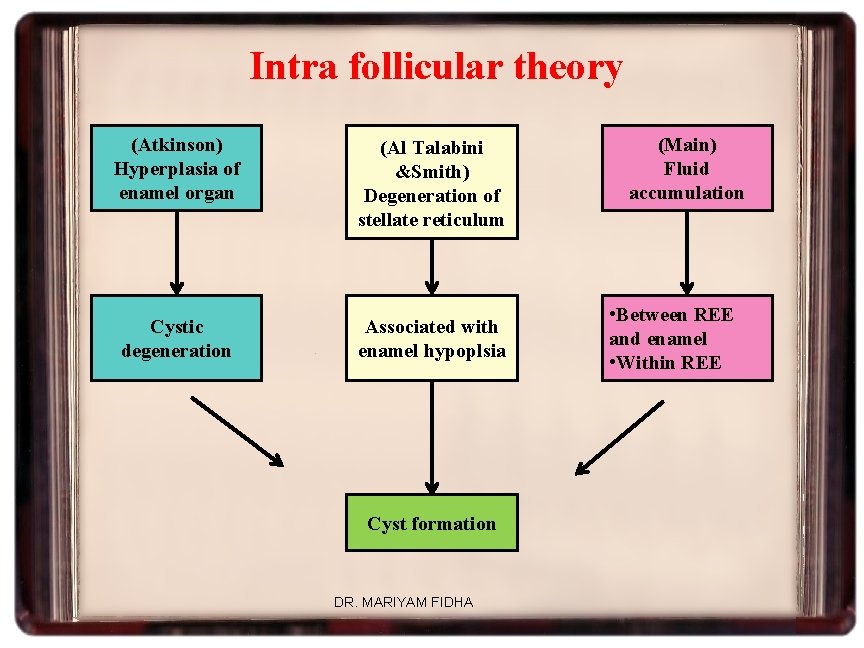
Intra follicular theory (Atkinson) Hyperplasia of enamel organ (Al Talabini &Smith) Degeneration of stellate reticulum Cystic degeneration Associated with enamel hypoplsia Cyst formation DR. MARIYAM FIDHA (Main) Fluid accumulation • Between REE and enamel • Within REE
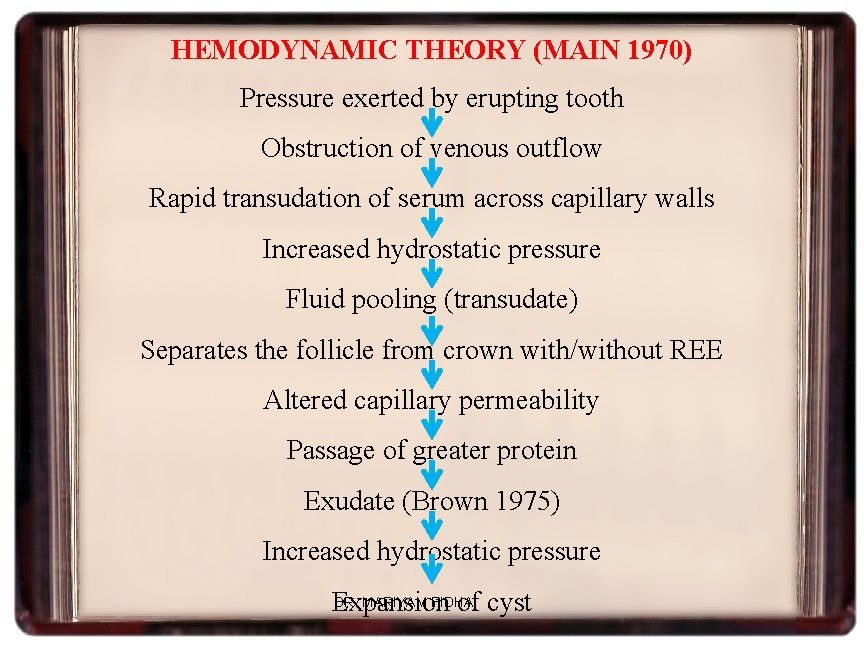
HEMODYNAMIC THEORY (MAIN 1970) Pressure exerted by erupting tooth Obstruction of venous outflow Rapid transudation of serum across capillary walls Increased hydrostatic pressure Fluid pooling (transudate) Separates the follicle from crown with/without REE Altered capillary permeability Passage of greater protein Exudate (Brown 1975) Increased hydrostatic pressure DR. MARIYAM FIDHA Expansion of cyst
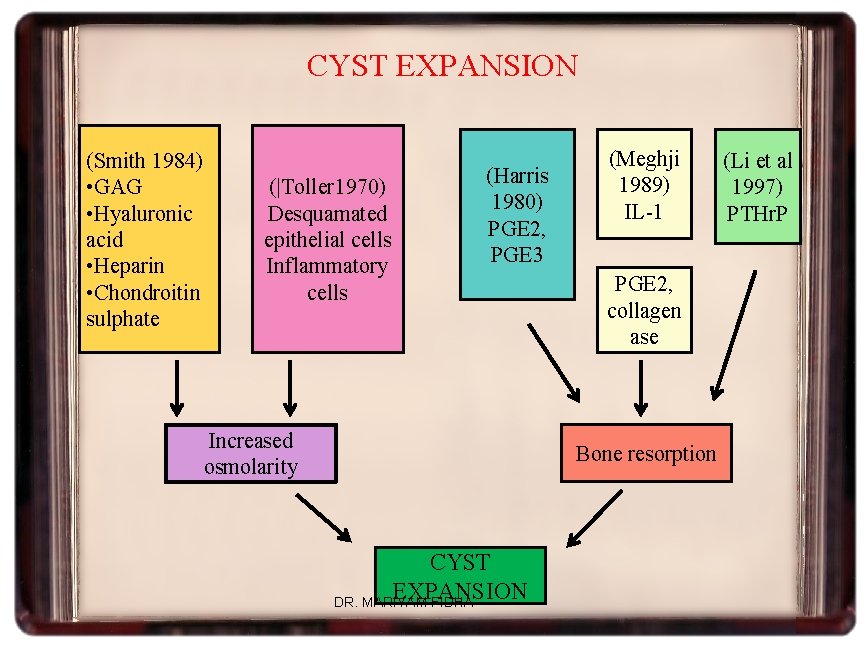
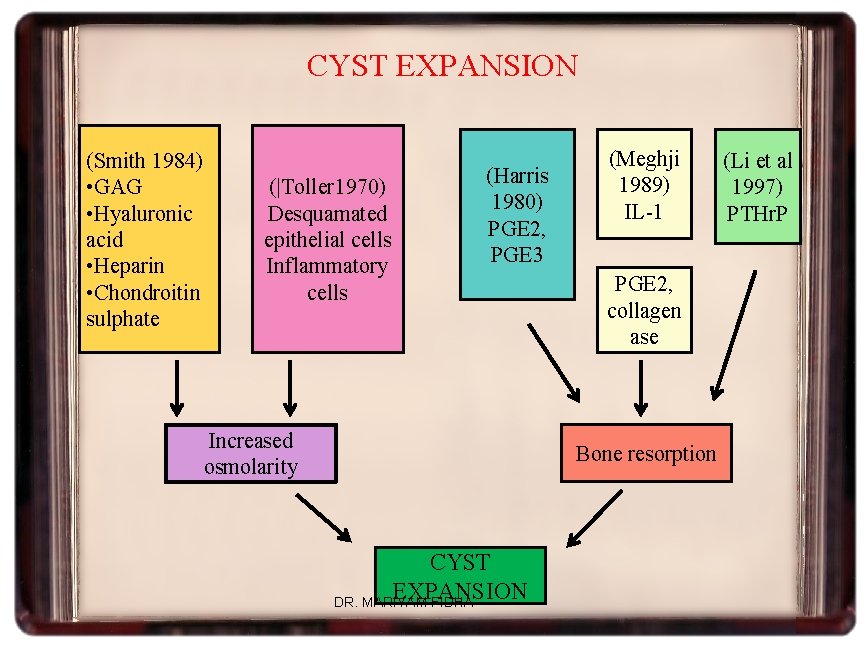
CYST EXPANSION (Smith 1984) • GAG • Hyaluronic acid • Heparin • Chondroitin sulphate (|Toller 1970) Desquamated epithelial cells Inflammatory cells (Harris 1980) PGE 2, PGE 3 Increased osmolarity (Meghji 1989) IL-1 PGE 2, collagen ase Bone resorption CYST EXPANSION DR. MARIYAM FIDHA (Li et al 1997) PTHr. P
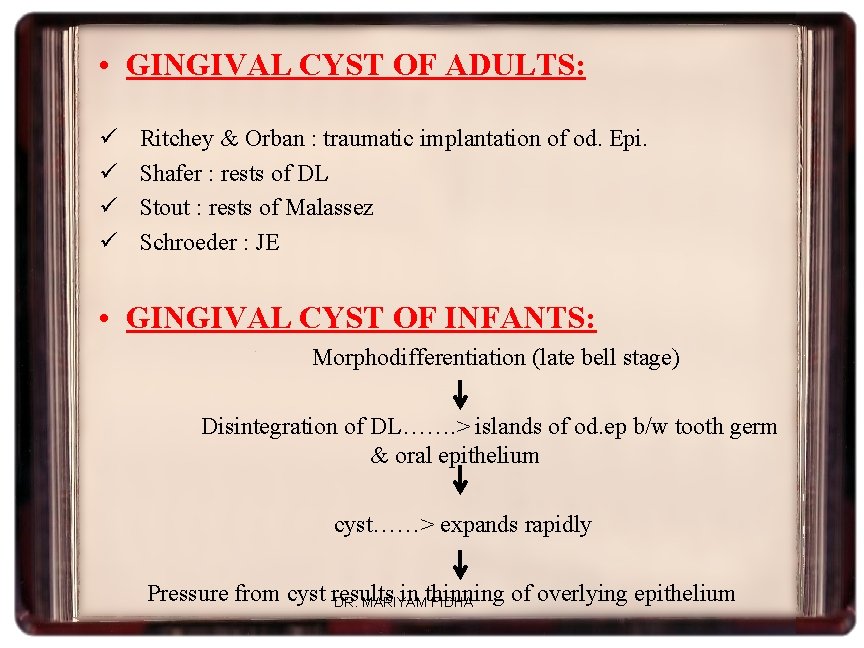
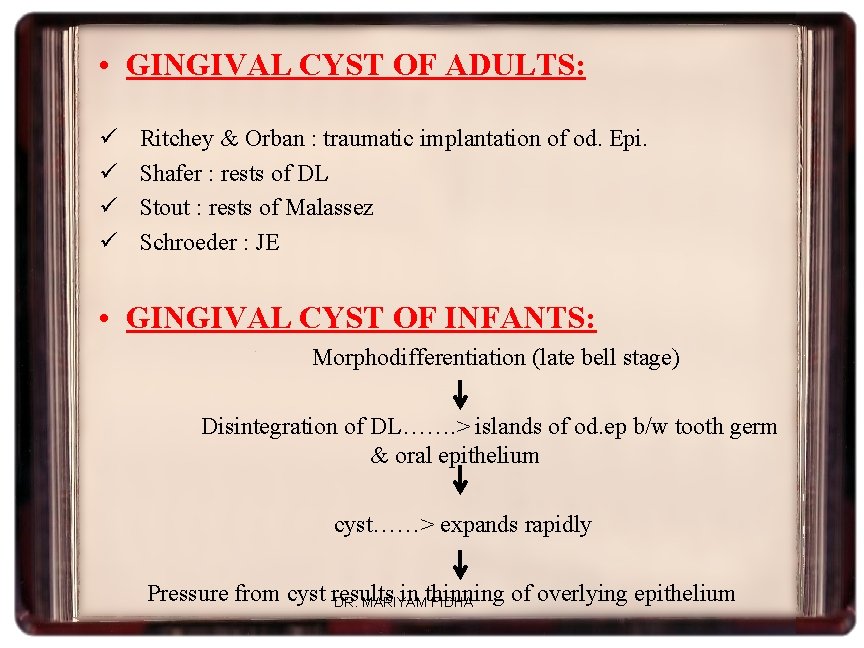
• GINGIVAL CYST OF ADULTS: ü ü Ritchey & Orban : traumatic implantation of od. Epi. Shafer : rests of DL Stout : rests of Malassez Schroeder : JE • GINGIVAL CYST OF INFANTS: Morphodifferentiation (late bell stage) Disintegration of DL……. > islands of od. ep b/w tooth germ & oral epithelium cyst……> expands rapidly Pressure from cyst results in thinning of overlying epithelium DR. MARIYAM FIDHA
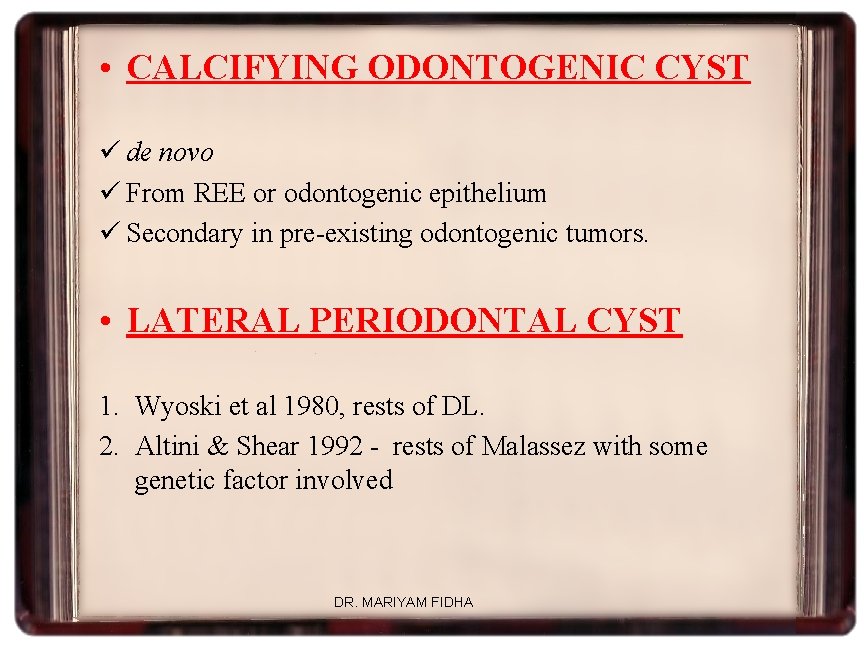
• CALCIFYING ODONTOGENIC CYST ü de novo ü From REE or odontogenic epithelium ü Secondary in pre-existing odontogenic tumors. • LATERAL PERIODONTAL CYST 1. Wyoski et al 1980, rests of DL. 2. Altini & Shear 1992 - rests of Malassez with some genetic factor involved DR. MARIYAM FIDHA
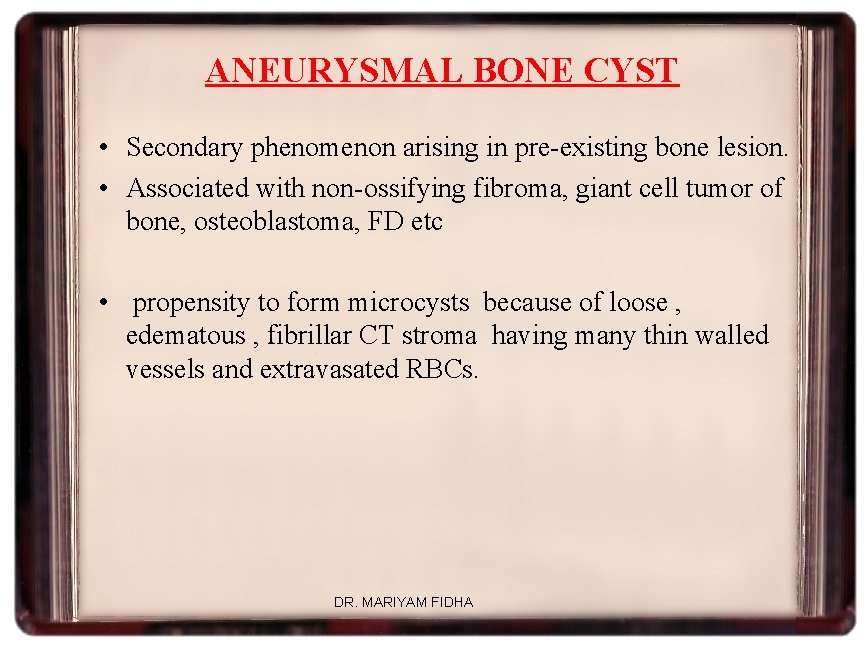
ANEURYSMAL BONE CYST • Secondary phenomenon arising in pre-existing bone lesion. • Associated with non-ossifying fibroma, giant cell tumor of bone, osteoblastoma, FD etc • propensity to form microcysts because of loose , edematous , fibrillar CT stroma having many thin walled vessels and extravasated RBCs. DR. MARIYAM FIDHA

Stagnation & ischaemia Localised areas of necrosis Microcysts– lined by stromal CT& Giant cells ( in GC lesions) Further stromal breakdown– microcysts coalasce & enlarge Dilalatation & rupture of thin walled vessels--haemorrahge into stroma & microcysts Connection established between microcyst & larger vessel --- enlargement due to haemodynamic changes Macrocyst --- surrounded by layers of compressed stroma---expanding cysts produce pressure resorbing bone Cortical bone breached -- “blow out” of lesion – covered with periosteum DR. MARIYAM FIDHA
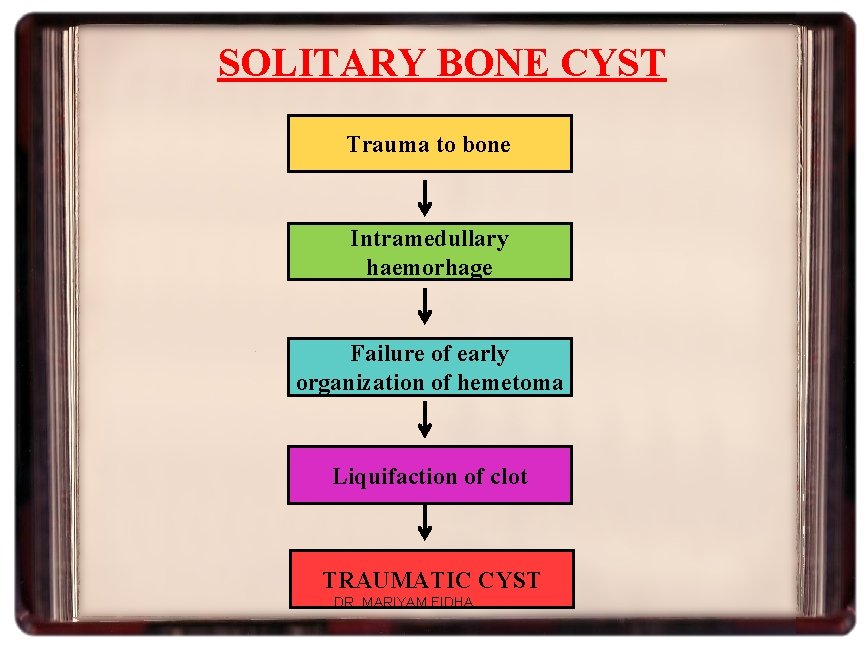
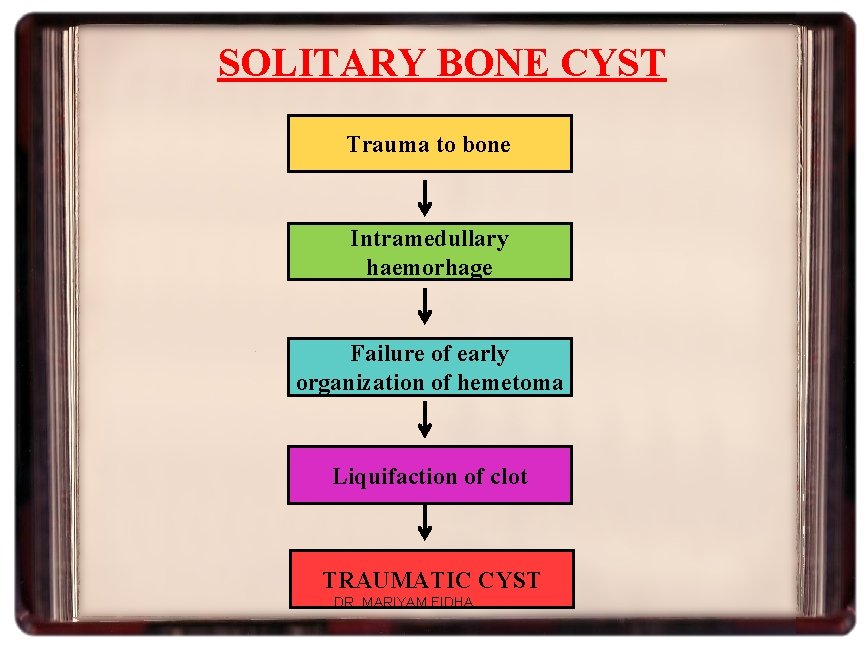
SOLITARY BONE CYST Trauma to bone Intramedullary haemorhage Failure of early organization of hemetoma Liquifaction of clot TRAUMATIC CYST DR. MARIYAM FIDHA
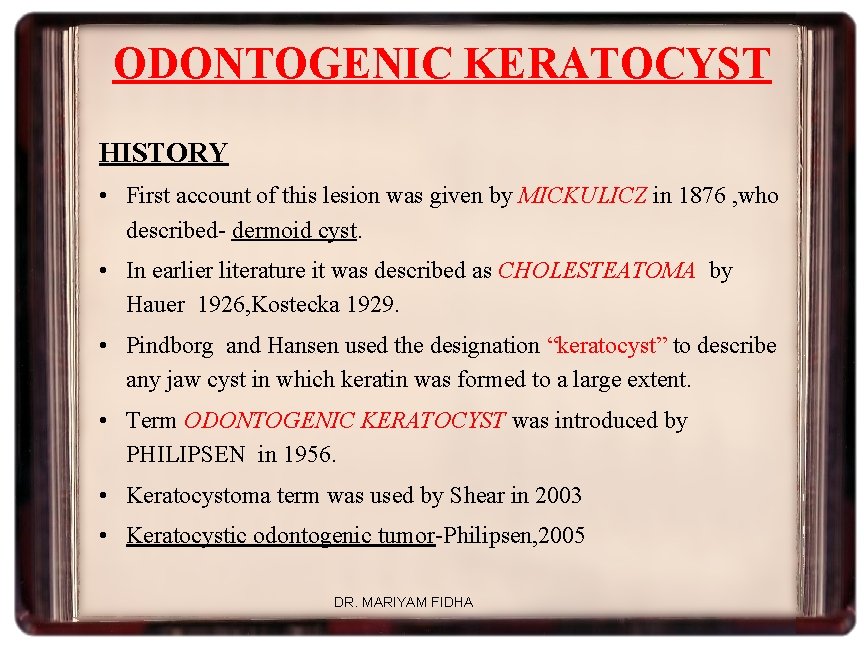
ODONTOGENIC KERATOCYST HISTORY • First account of this lesion was given by MICKULICZ in 1876 , who described- dermoid cyst. • In earlier literature it was described as CHOLESTEATOMA by Hauer 1926, Kostecka 1929. • Pindborg and Hansen used the designation “keratocyst” to describe any jaw cyst in which keratin was formed to a large extent. • Term ODONTOGENIC KERATOCYST was introduced by PHILIPSEN in 1956. • Keratocystoma term was used by Shear in 2003 • Keratocystic odontogenic tumor-Philipsen, 2005 DR. MARIYAM FIDHA
• TOLLER suggested that OKC might be regarded as benign cystic neoplasm based on its clinical behaviour. • Latest 2005, WHO classification of odontogenic tumors, considered OKC as “Keratocystic Odontogenic Tumor” or KCOT DR. MARIYAM FIDHA
Several factors form the basis of this decision. • Behaviour: KCOT is locally destructive and high recurrence rate • Histopathology: basal layer of the KCOT budding into connective tissue mitotic figures are frequently found in the suprabasal layers. • Genetics: association with PTCH gene. DR. MARIYAM FIDHA
• PTCH (“patched”), a tumour suppressor gene involved in both NBCCS and sporadic KCOTs, occurs on chromosome 9 q 22. 3 -q 31. • Normally, PTCH forms a receptor complex with the oncogene SMO (“smoothened”) for the SHH (“sonic hedgehog”) ligand. • PTCH binding to SMO inhibits growth-signal transduction • SHH binding to PTCH releases this inhibition • If normal functioning of PTCH is lost, the proliferationstimulating effects of SMO are permitted to predominate. DR. MARIYAM FIDHA

• PTCH diagram DR. MARIYAM FIDHA
• WHO, 2005 defines KCOT as Benign uni/multicystic intraosseous tumor of odontogenic origin with characteristic lining of parakeratinized stratified squamous epithelium and potential for aggressive, infiltrative behaviour. DR. MARIYAM FIDHA
Why is the recognition of this cyst is important? • OKC tends to act more aggressive • higher recurrence rate • specific cyst sometimes asso. with Nevoid Basal Cell Carcinoma Syndrome DR. MARIYAM FIDHA

PATHOGENESIS Earlier OKCs were considered to originate from the primordium of a tooth before mineralization had taken placeprimordial cysts Robinson 1945 The dental lamina or its remnants : satellite microcysts in the wall of the amin cystsapparantly arising from |DL ØWooglar et al 1987 genetically abnormal & prone to exuberant proliferation Basal cells of oral epithelium– OKC in ascending ramus have no relationship to tooth follicle or dental lamina--- arise from basal cell hamartias (proliferation of basal cells of oral mucosa) Soskolne and Shear, Toller-1967 Browne-1975 Stoelinga 1971 & Voorsmit 1981 DR. MARIYAM FIDHA
• • Shear & Altini 1976: induced by residual ectomesenchymal influence Ostrofsky 1980: 1. Mature rest cells – dental lamina 2. Immature rest cells – basal layer PTCH Gene mutation Nevoid basal cell carcinoma syndrome DR. MARIYAM FIDHA
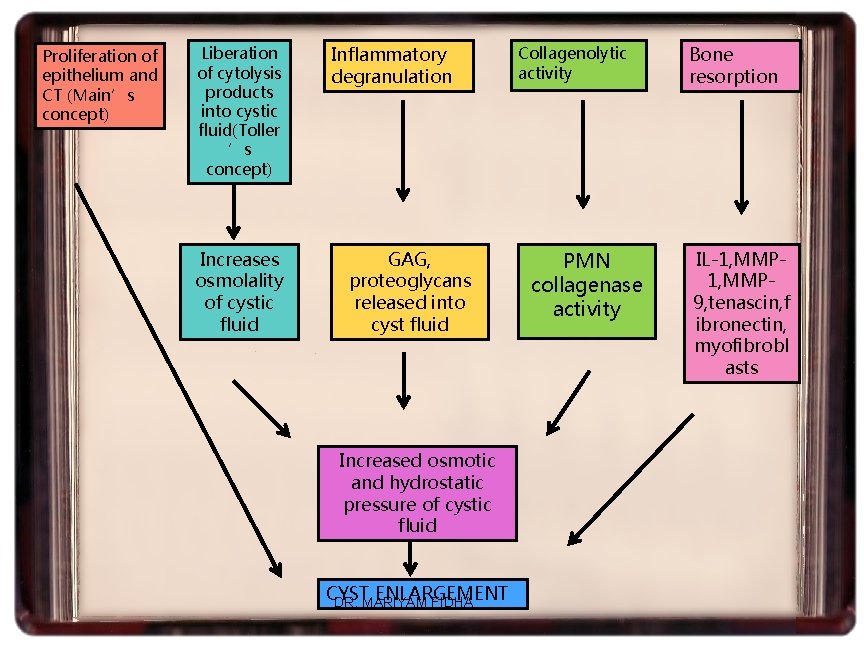
GROWTH AND ENLARGEMENT 1. RATE OF GROWTH: ü Inflammation has negligible role ( Toller, Browne, Smith et al) ü Rate of growth : 2 -14 mm/year average of 7 mm (Forselle 1980) • Causes: 1. higher mitotic activity ( Main 1970) – mitotic value ranged from 0 to 19 with a mean of 8 2. higher proliferation of cells (Scharffetter et al 1989) 3. irregular proliferation of epithelium & CT 4. active growth of CT wall DR. MARIYAM FIDHA

2. ROLE OF OSMOLALITY – limited role ü Toller 1970 : mean osmolality greater than serum § Not related to proteins but by products of cell lysis § Important, if not sole role, in expansive growth ü Main 1970: epithelial proliferation – major role in expansion & evidence of osmotic diffusion inconclusive ü Brown 1970 & Kramer 1974 – multilocular and loculated outlines of some OKC dificult to interpret on the basis of unicentric hydrostatic expansion § multicentric growth of cyst --- due to proliferation of local groups DR. MARIYAM FIDHA cyst content. of epithelial cells against semi-solid
3. INFLAMMATORY EXUDATES – LIMITED ROLE • Inflammatory exudate played a negligible role in OKC enlargement. • Cavity fluid contains low quantities of soluble protein Browne & Toller, 1976 • Cyst walls are free of inflammatory cell infiltrate except for occasional foci. • More or less continuous epithelial wall of OKC less permeable than other cysts-Smith et al, 1983 DR. MARIYAM FIDHA
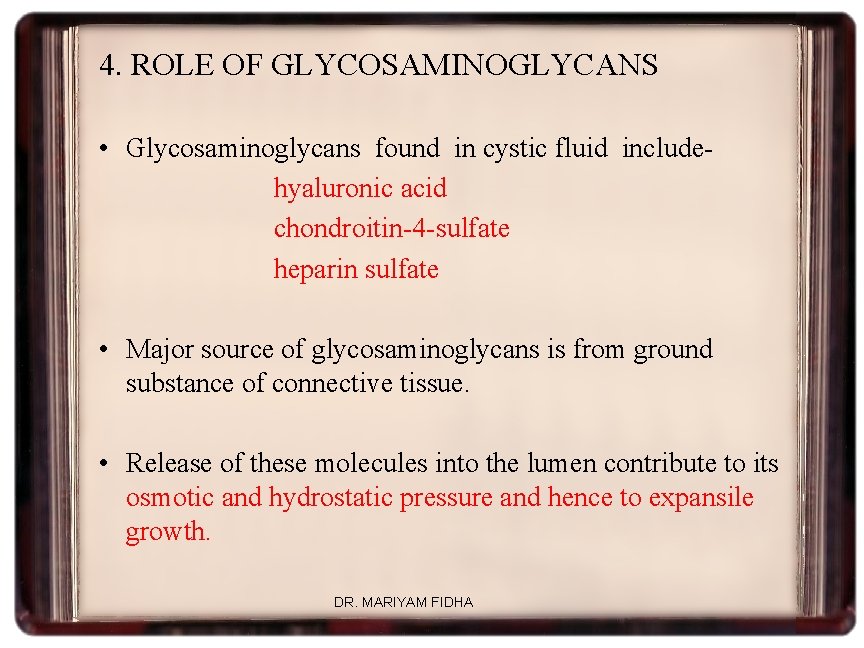
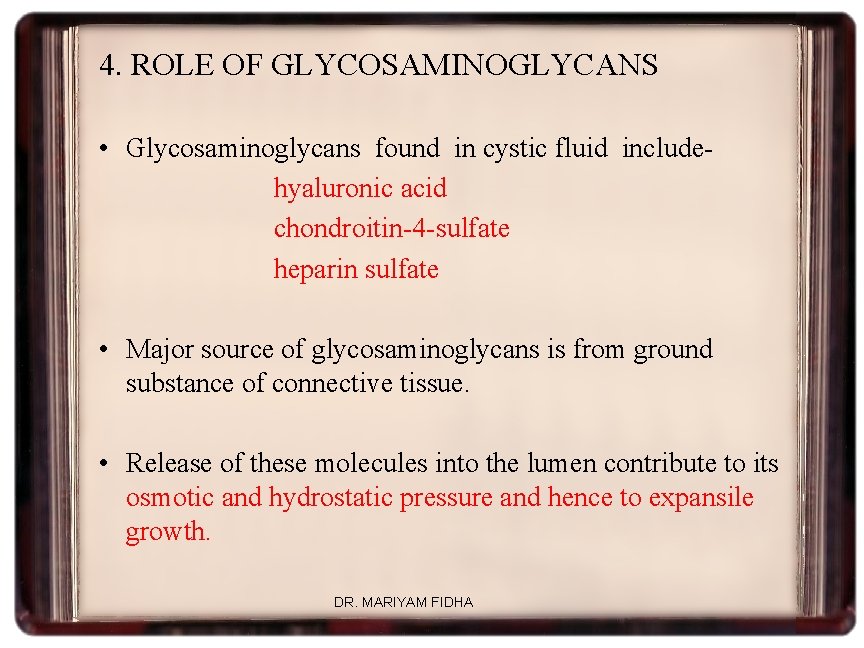
4. ROLE OF GLYCOSAMINOGLYCANS • Glycosaminoglycans found in cystic fluid includehyaluronic acid chondroitin-4 -sulfate heparin sulfate • Major source of glycosaminoglycans is from ground substance of connective tissue. • Release of these molecules into the lumen contribute to its osmotic and hydrostatic pressure and hence to expansile growth. DR. MARIYAM FIDHA

BONE RESORPTION AND OKC GROWTH 1. Collagenolytic activity ü Enzymatic mechanism is importnt for growth of OKC ü OKC collagenase – PMN type – degrade colagen type 1 & 2 (Sorsa et al) ü Connective tissue destruction leading to growth of OKC 2. Interleukins : IL 1 & IL 6 3. MMPS : Increased MMP 9 activity 4. Smooth muscle actin positivity : aggressive behavior 5. PTHrp positivity : increase bone resorption DR. MARIYAM FIDHA
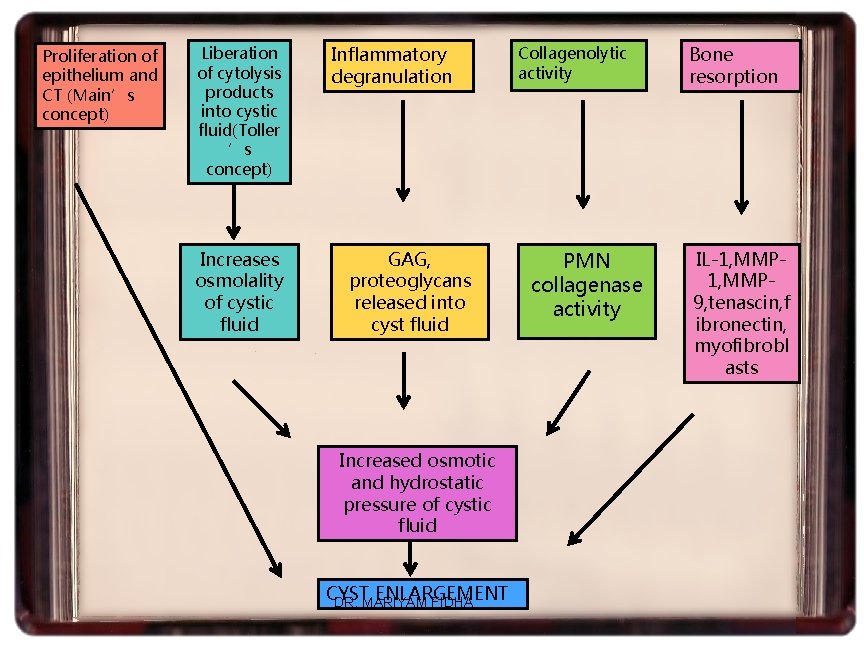
Proliferation of epithelium and CT (Main’s concept) Liberation of cytolysis products into cystic fluid(Toller ’s concept) Increases osmolality of cystic fluid Inflammatory degranulation GAG, proteoglycans released into cyst fluid Increased osmotic and hydrostatic pressure of cystic fluid CYST ENLARGEMENT DR. MARIYAM FIDHA Collagenolytic activity PMN collagenase activity Bone resorption IL-1, MMP 9, tenascin, f ibronectin, myofibrobl asts
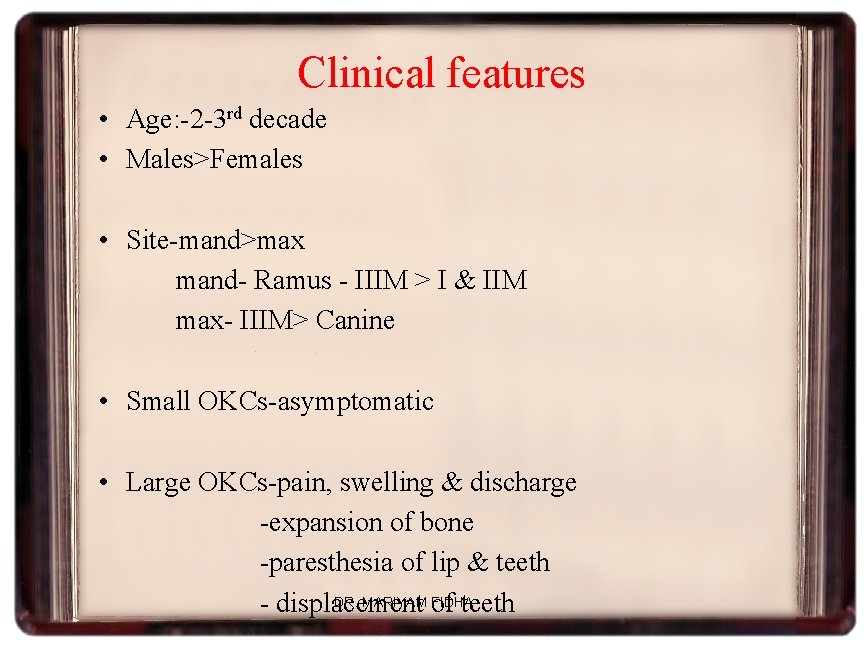
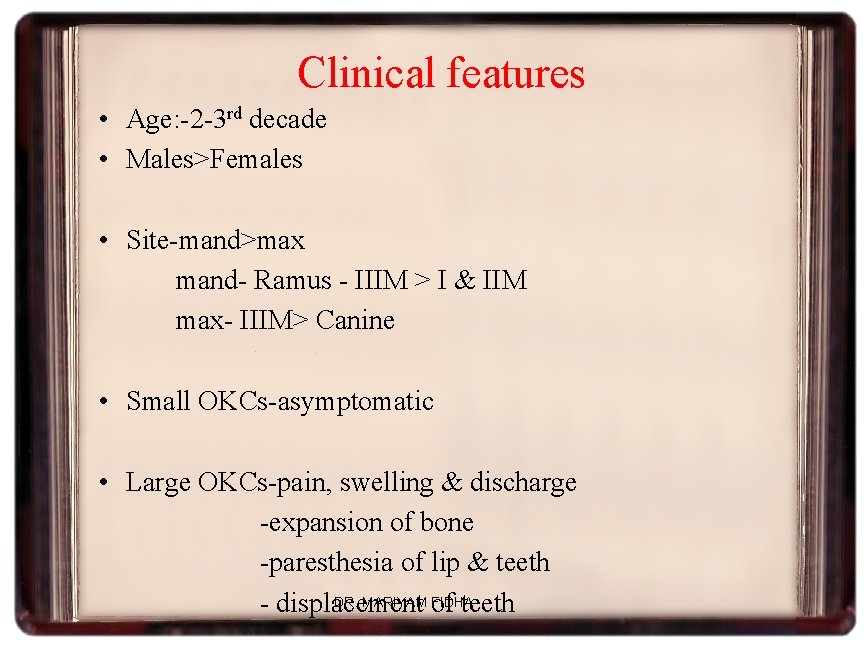
Clinical features • Age: -2 -3 rd decade • Males>Females • Site-mand>max mand- Ramus - IIIM > I & IIM max- IIIM> Canine • Small OKCs-asymptomatic • Large OKCs-pain, swelling & discharge -expansion of bone -paresthesia of lip & teeth DR. MARIYAM of FIDHA - displacement teeth
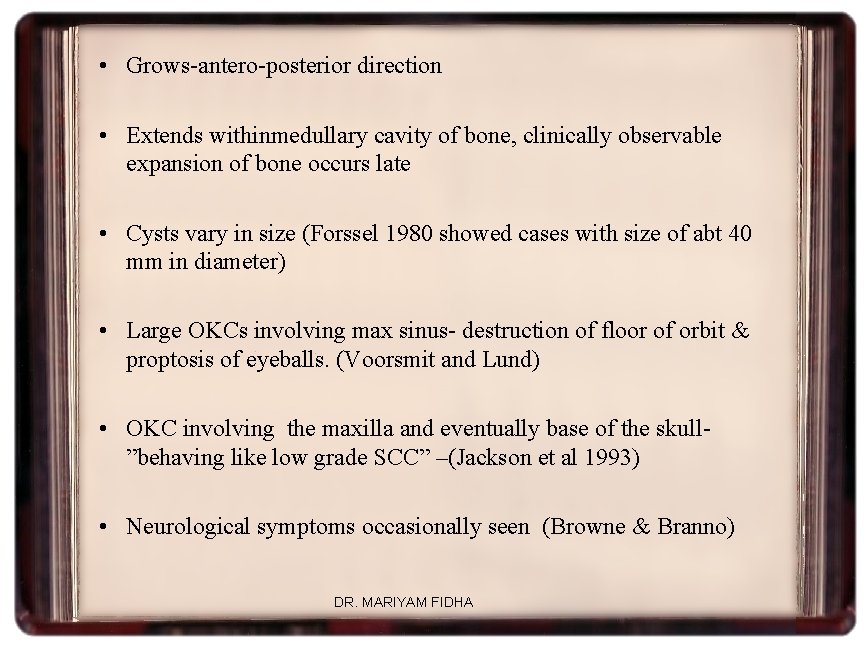
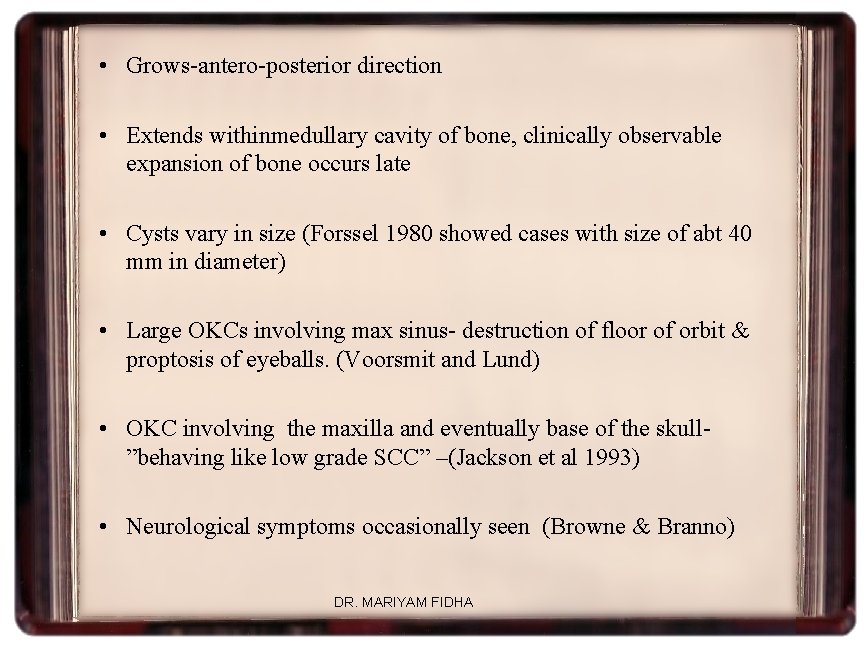
• Grows-antero-posterior direction • Extends withinmedullary cavity of bone, clinically observable expansion of bone occurs late • Cysts vary in size (Forssel 1980 showed cases with size of abt 40 mm in diameter) • Large OKCs involving max sinus- destruction of floor of orbit & proptosis of eyeballs. (Voorsmit and Lund) • OKC involving the maxilla and eventually base of the skull”behaving like low grade SCC” –(Jackson et al 1993) • Neurological symptoms occasionally seen (Browne & Branno) DR. MARIYAM FIDHA
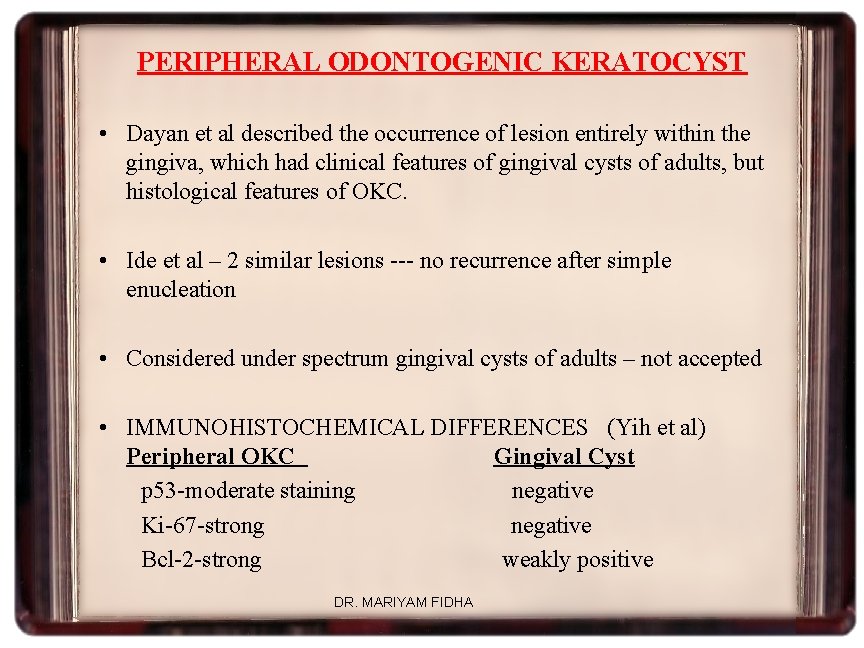
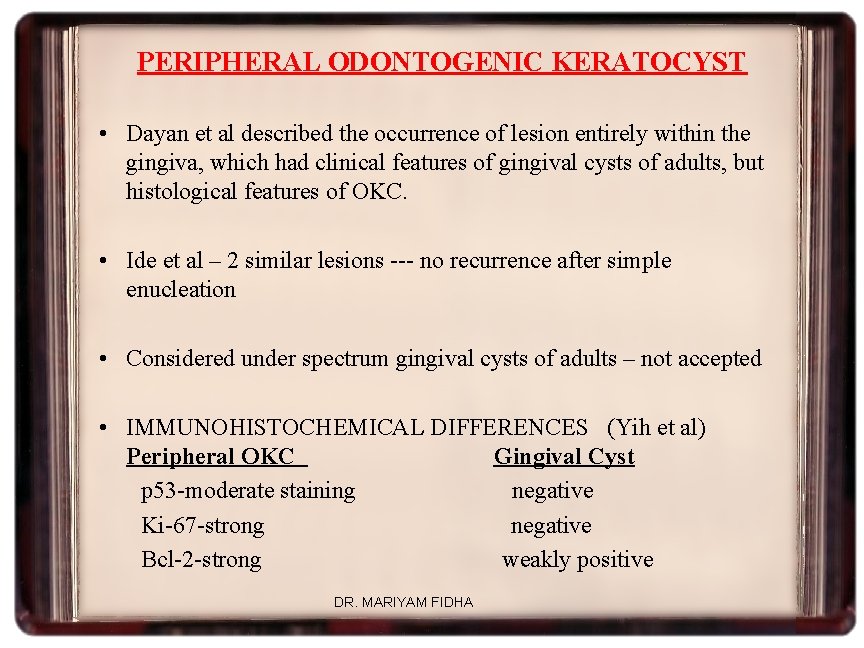
PERIPHERAL ODONTOGENIC KERATOCYST • Dayan et al described the occurrence of lesion entirely within the gingiva, which had clinical features of gingival cysts of adults, but histological features of OKC. • Ide et al – 2 similar lesions --- no recurrence after simple enucleation • Considered under spectrum gingival cysts of adults – not accepted • IMMUNOHISTOCHEMICAL DIFFERENCES (Yih et al) Peripheral OKC Gingival Cyst p 53 -moderate staining negative Ki-67 -strong negative Bcl-2 -strong weakly positive DR. MARIYAM FIDHA
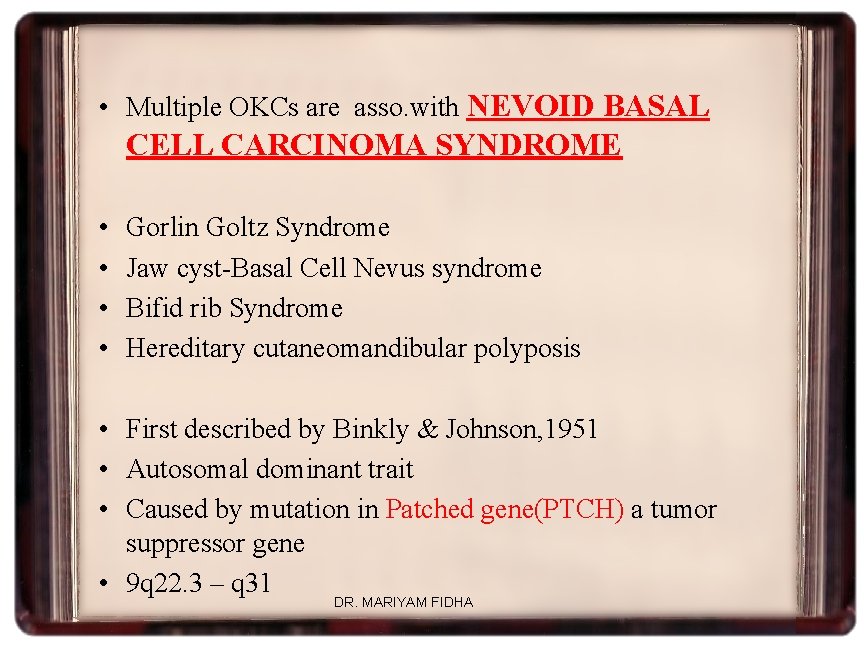
• Multiple OKCs are asso. with NEVOID BASAL CELL CARCINOMA SYNDROME • • Gorlin Goltz Syndrome Jaw cyst-Basal Cell Nevus syndrome Bifid rib Syndrome Hereditary cutaneomandibular polyposis • First described by Binkly & Johnson, 1951 • Autosomal dominant trait • Caused by mutation in Patched gene(PTCH) a tumor suppressor gene • 9 q 22. 3 – q 31 DR. MARIYAM FIDHA
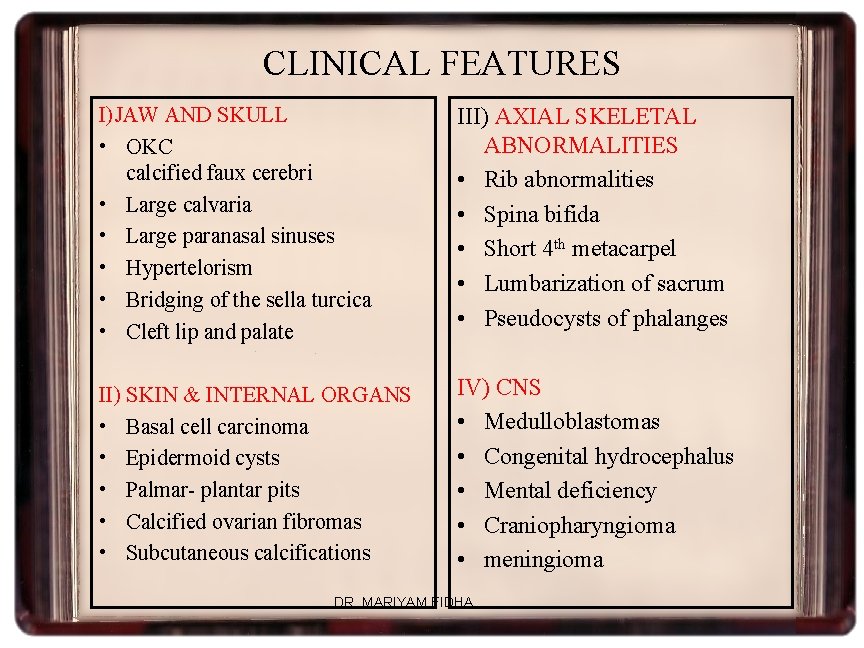
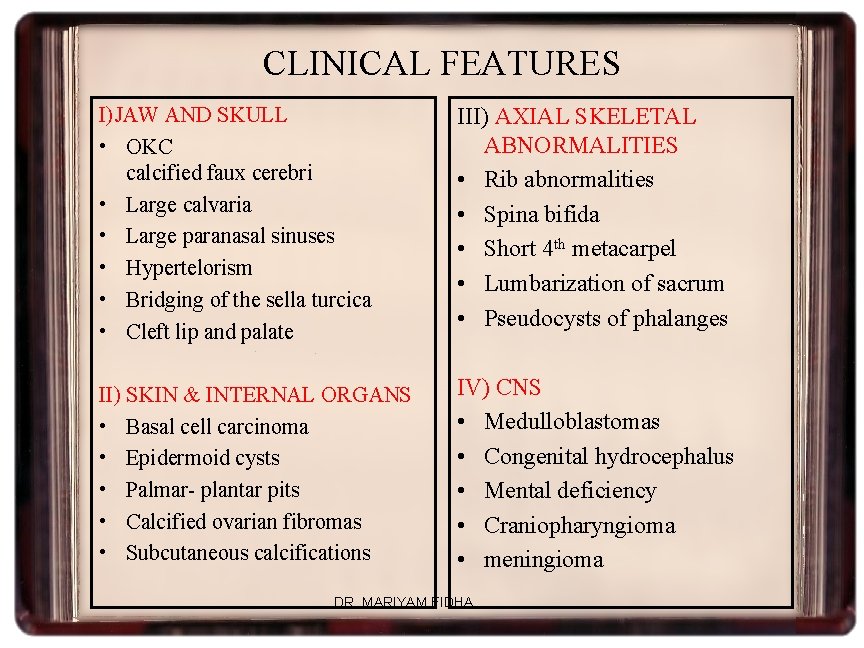
CLINICAL FEATURES I)JAW AND SKULL • OKC calcified faux cerebri • Large calvaria • Large paranasal sinuses • Hypertelorism • Bridging of the sella turcica • Cleft lip and palate III) AXIAL SKELETAL ABNORMALITIES • Rib abnormalities • Spina bifida • Short 4 th metacarpel • Lumbarization of sacrum • Pseudocysts of phalanges II) SKIN & INTERNAL ORGANS • Basal cell carcinoma • Epidermoid cysts • Palmar- plantar pits • Calcified ovarian fibromas • Subcutaneous calcifications IV) CNS • Medulloblastomas • Congenital hydrocephalus • Mental deficiency • Craniopharyngioma • meningioma DR. MARIYAM FIDHA

DR. MARIYAM FIDHA

Multiple cysts Calcification of Faux Cerebri Bifid Ribs Ribbon shaped Ribs DR. MARIYAM FIDHA
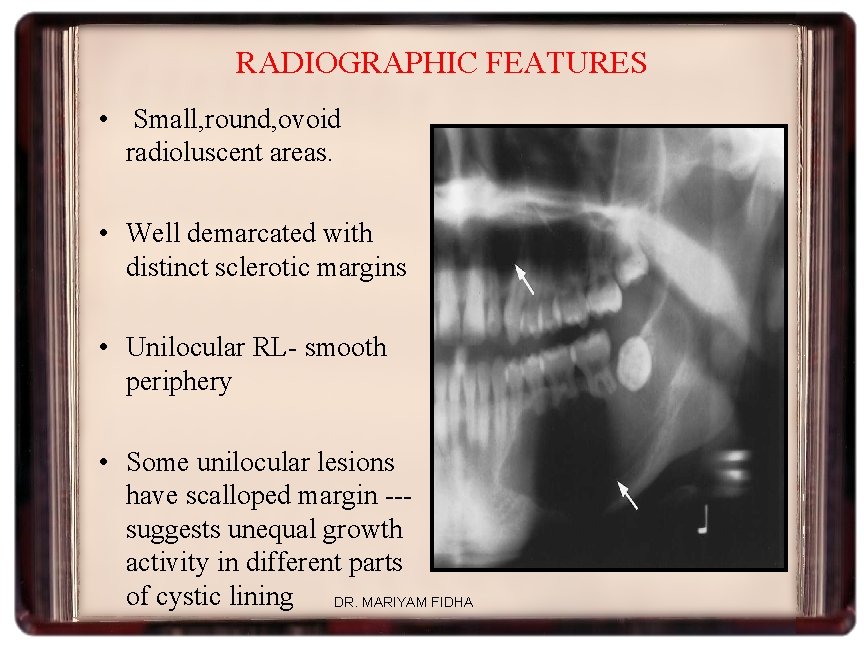
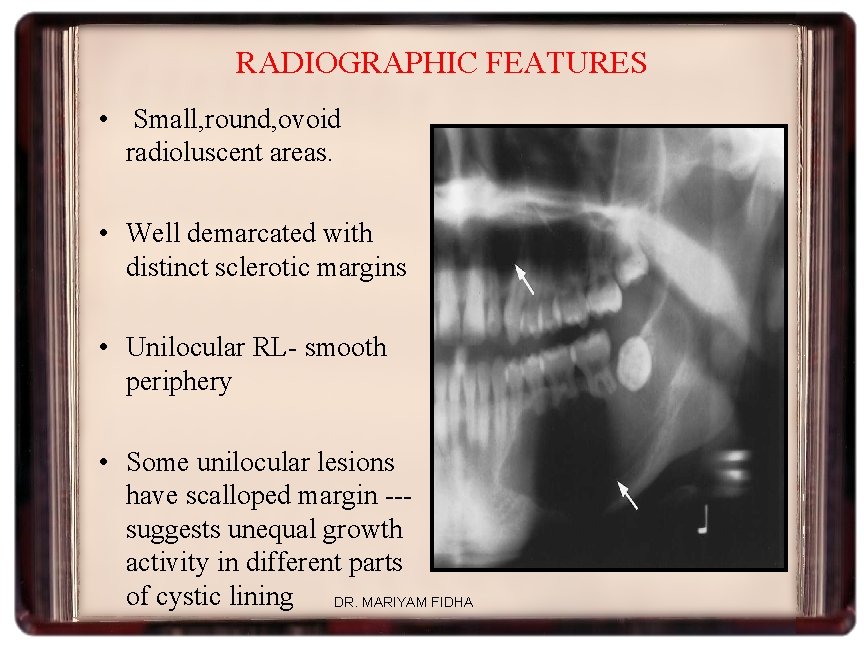
RADIOGRAPHIC FEATURES • Small, round, ovoid radioluscent areas. • Well demarcated with distinct sclerotic margins • Unilocular RL- smooth periphery • Some unilocular lesions have scalloped margin --suggests unequal growth activity in different parts of cystic lining DR. MARIYAM FIDHA
• Large multilocular lesions – especially in posterior mandible--- mimics amelobalstoma • Expansion of cortical plates less compared to others • Downward displacement of inferior alveolar canal • Resorption of lower cortical pate of mandible • Deflection of roots of teeth • Root resorption rare occurence DR. MARIYAM FIDHA
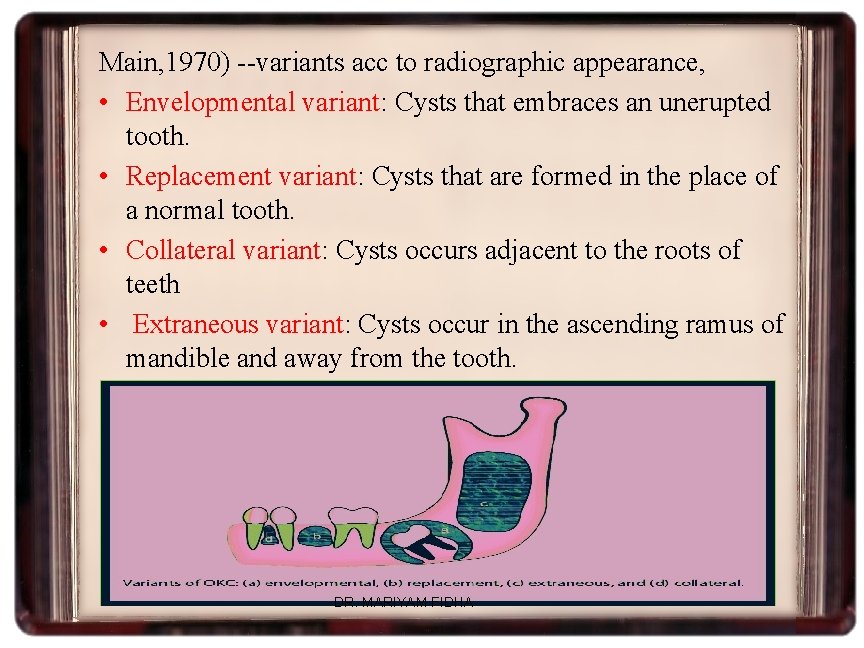
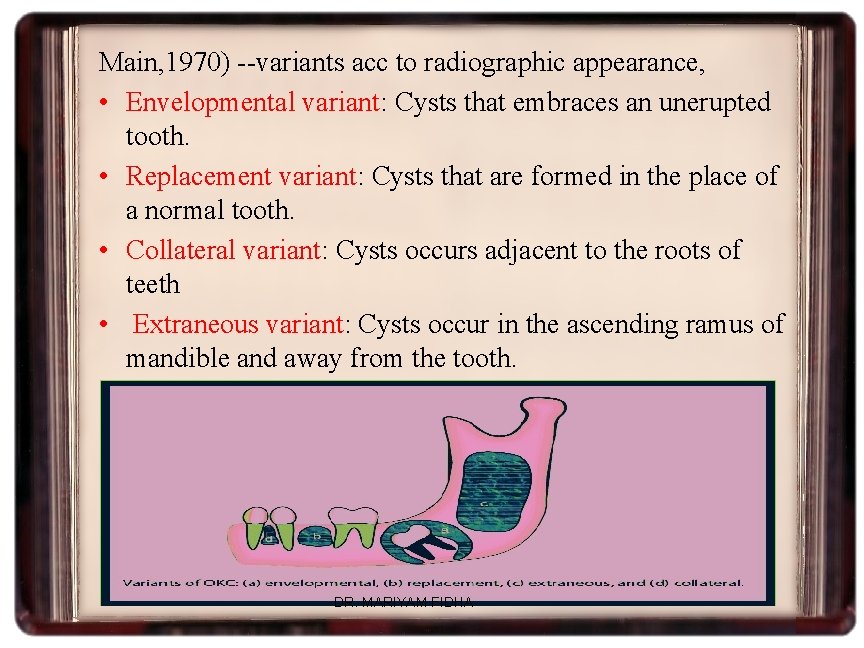
Main, 1970) --variants acc to radiographic appearance, • Envelopmental variant: Cysts that embraces an unerupted tooth. • Replacement variant: Cysts that are formed in the place of a normal tooth. • Collateral variant: Cysts occurs adjacent to the roots of teeth • Extraneous variant: Cysts occur in the ascending ramus of mandible and away from the tooth. • . DR. MARIYAM FIDHA
• OKC may occur in periapical region of vital standing teeth --- giving appearance of RC • May impede the eruption of related teeth--- dentigerous appearance radiographically • Such lesions frequently misdiagnosed as DC • Given rise to 2 misconceptions: (Gillette & Weinmann) 1. DC has keratinizing epithelail lining like OKC 2. DC may have extra-follicular origin DR. MARIYAM FIDHA

• Very occasionally the lining of a cyst in a true dentigerous relationship maybe identical to that of an OKC. • Browne suggested – occurred when an enlarging OKC involved the follicle of an unerupted tooth and fused with the REE DR. MARIYAM FIDHA
• Concept developed by Altini & Cohen--“FOLLICULAR KERATOCYST” • Cases in which cystic lining was typically OKC--- but completely surrounded crown of tooth & firmly attached to neck • Arise due to eruption of tooth into a pre-existing OKC cavity • Eithelium of cyst close to neck of tooth– REE • Reminder of the wall --- typical OKC epithelium DR. MARIYAM FIDHA
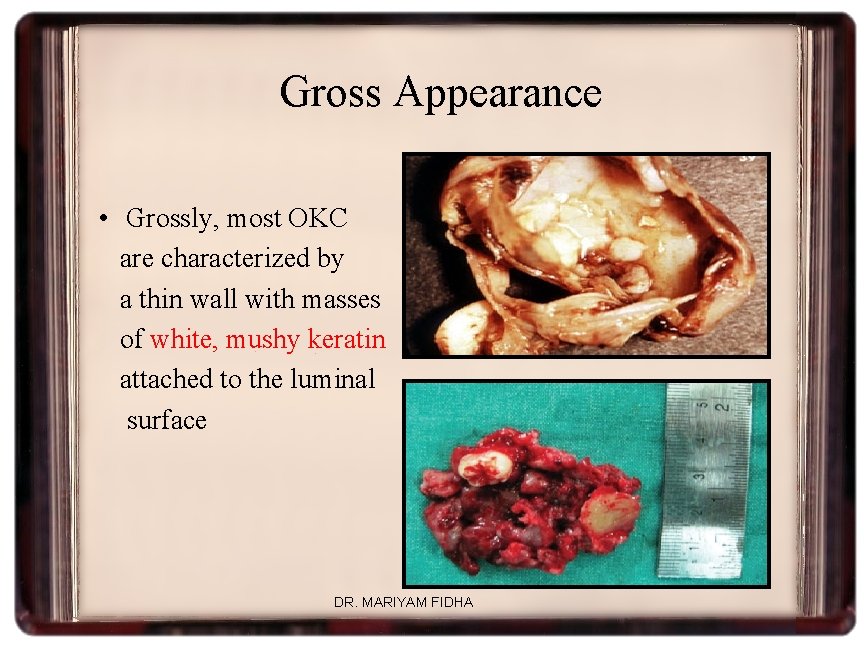
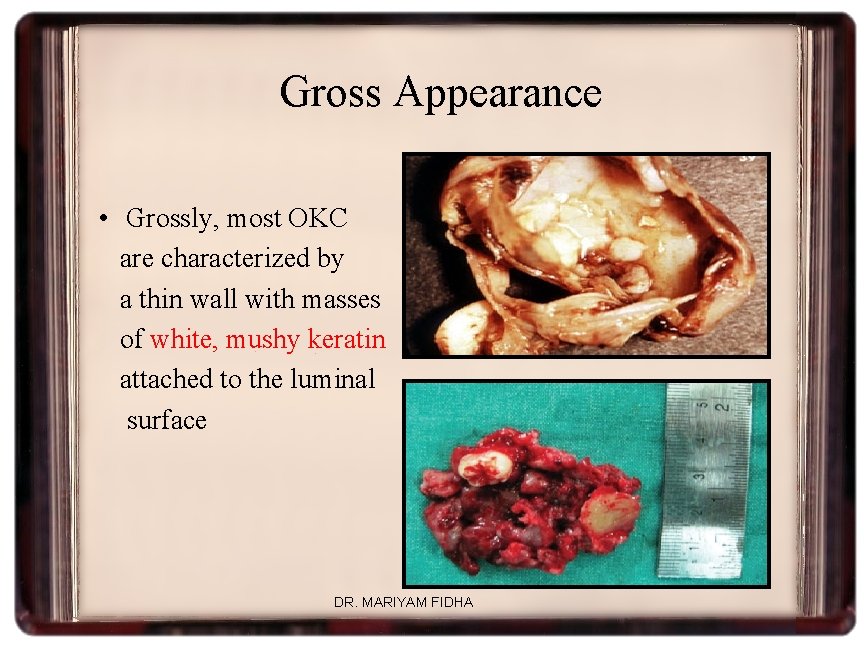
Gross Appearance • Grossly, most OKC are characterized by a thin wall with masses of white, mushy keratin attached to the luminal surface DR. MARIYAM FIDHA
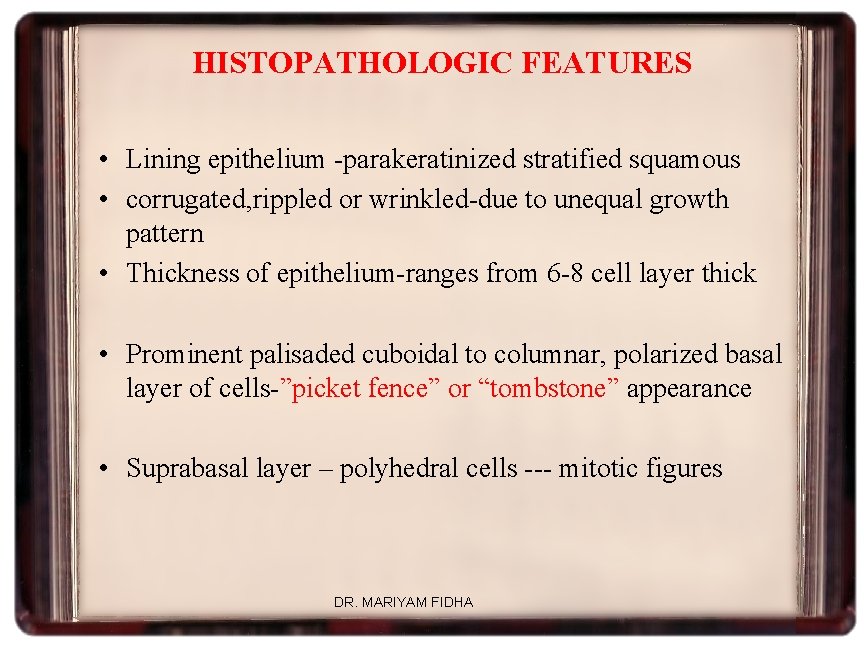
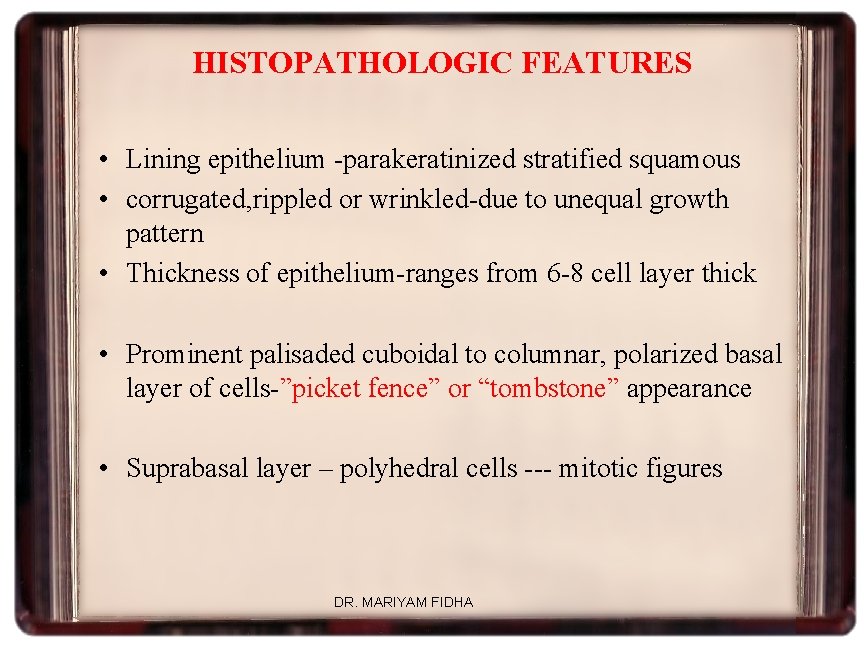
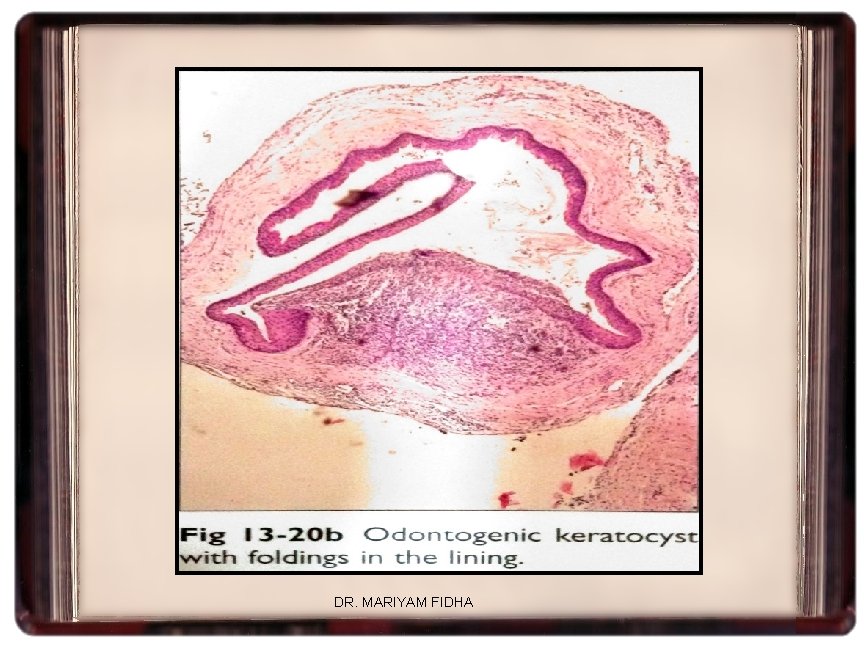
HISTOPATHOLOGIC FEATURES • Lining epithelium -parakeratinized stratified squamous • corrugated, rippled or wrinkled-due to unequal growth pattern • Thickness of epithelium-ranges from 6 -8 cell layer thick • Prominent palisaded cuboidal to columnar, polarized basal layer of cells-”picket fence” or “tombstone” appearance • Suprabasal layer – polyhedral cells --- mitotic figures DR. MARIYAM FIDHA
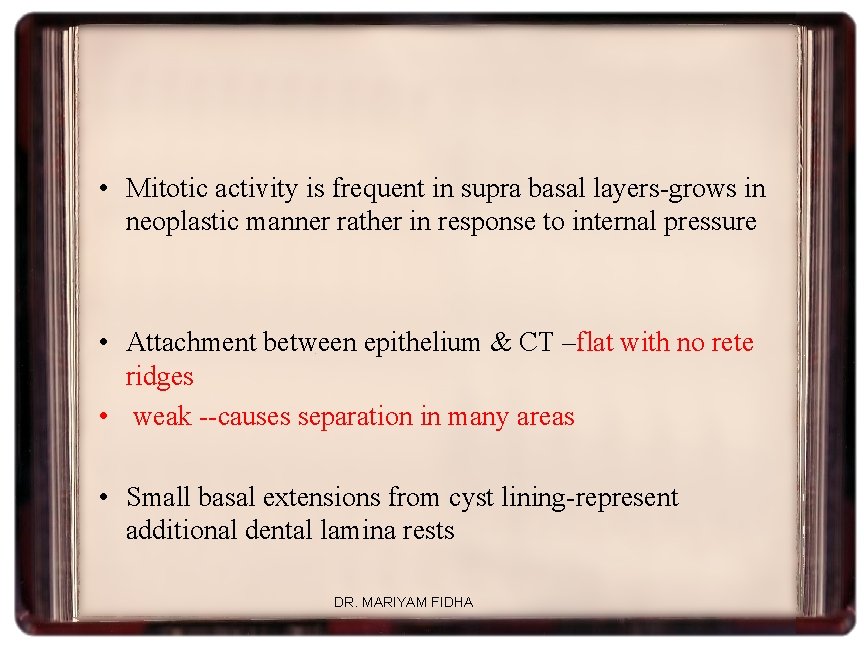
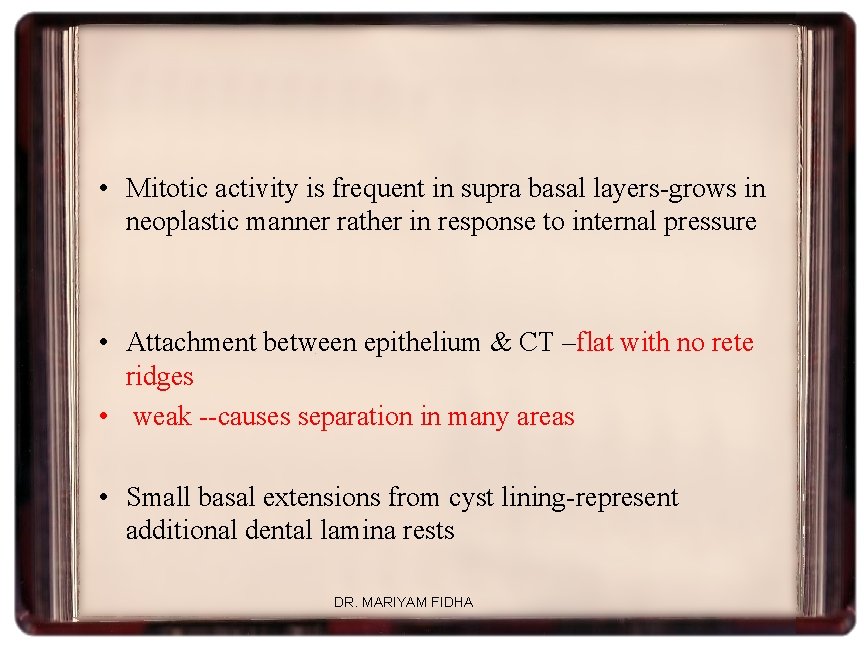
• Mitotic activity is frequent in supra basal layers-grows in neoplastic manner rather in response to internal pressure • Attachment between epithelium & CT –flat with no rete ridges • weak --causes separation in many areas • Small basal extensions from cyst lining-represent additional dental lamina rests DR. MARIYAM FIDHA

DR. MARIYAM FIDHA

DR. MARIYAM FIDHA
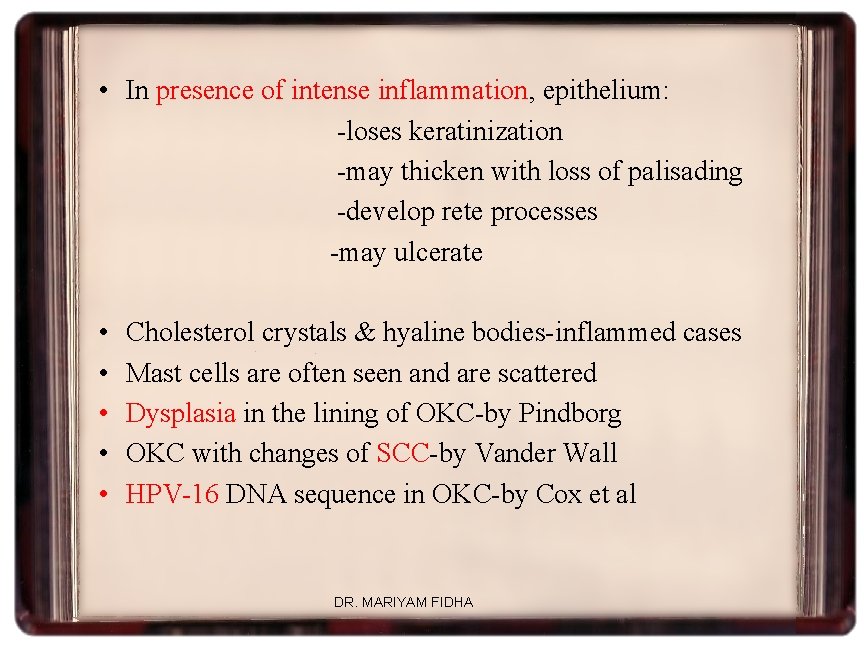
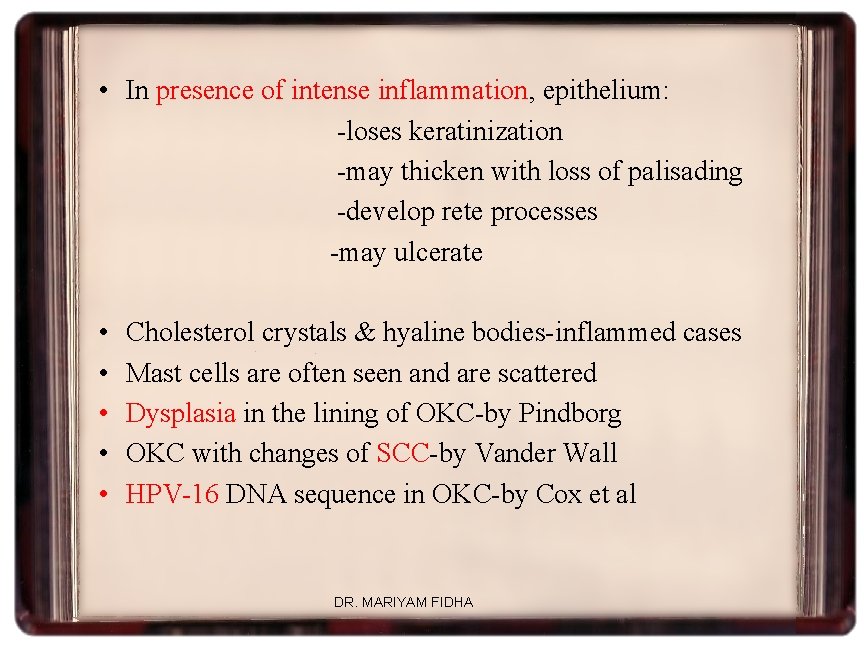
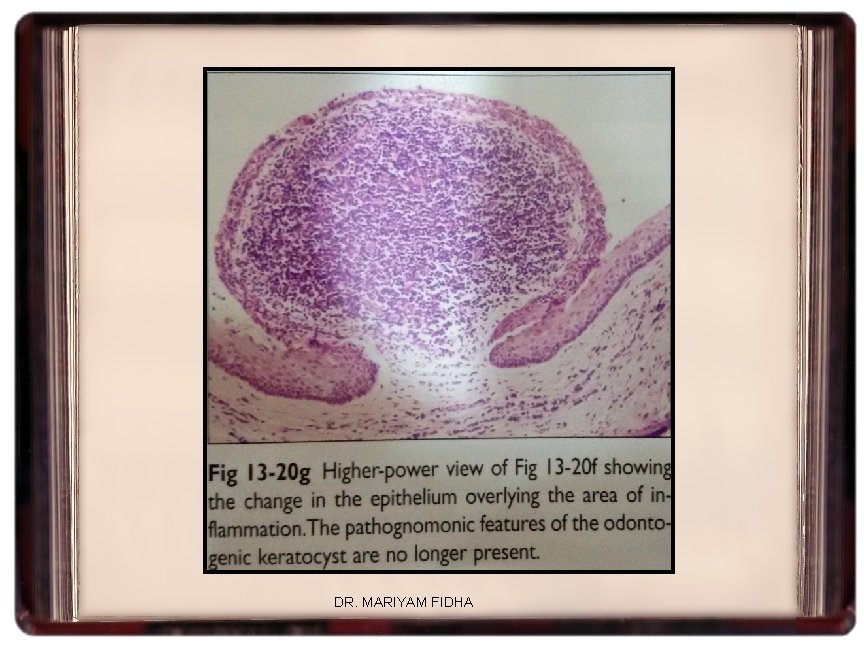
• In presence of intense inflammation, epithelium: -loses keratinization -may thicken with loss of palisading -develop rete processes -may ulcerate • • • Cholesterol crystals & hyaline bodies-inflammed cases Mast cells are often seen and are scattered Dysplasia in the lining of OKC-by Pindborg OKC with changes of SCC-by Vander Wall HPV-16 DNA sequence in OKC-by Cox et al DR. MARIYAM FIDHA
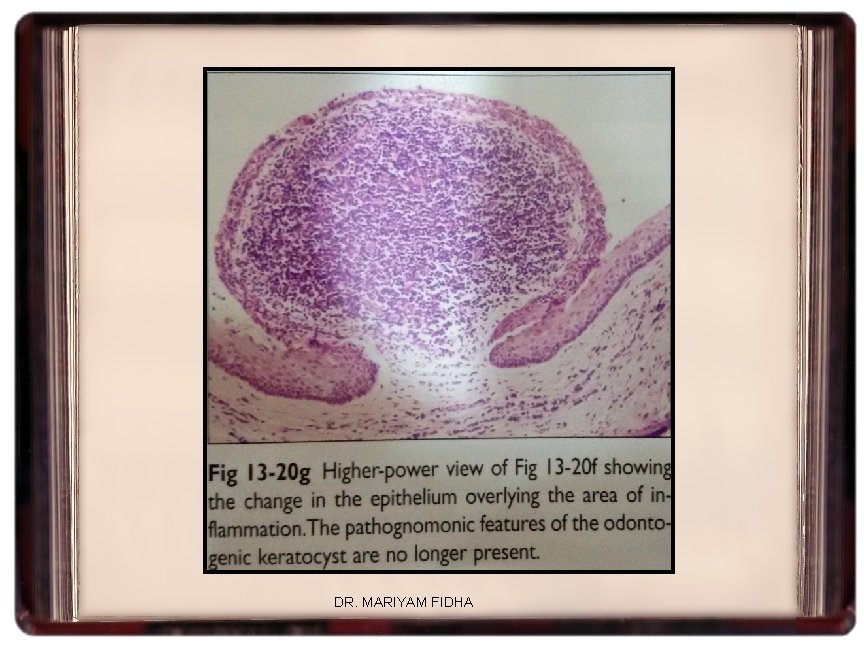
DR. MARIYAM FIDHA
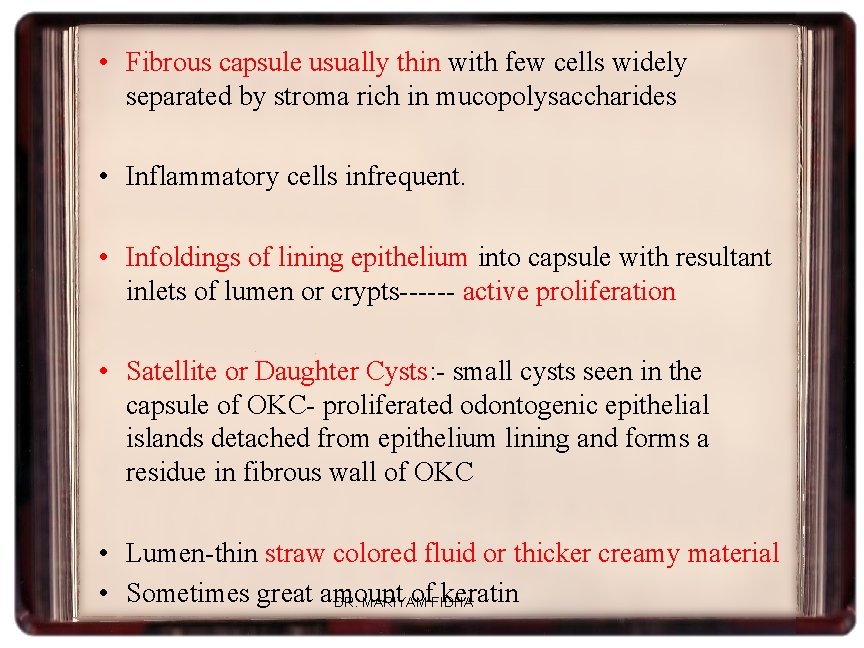
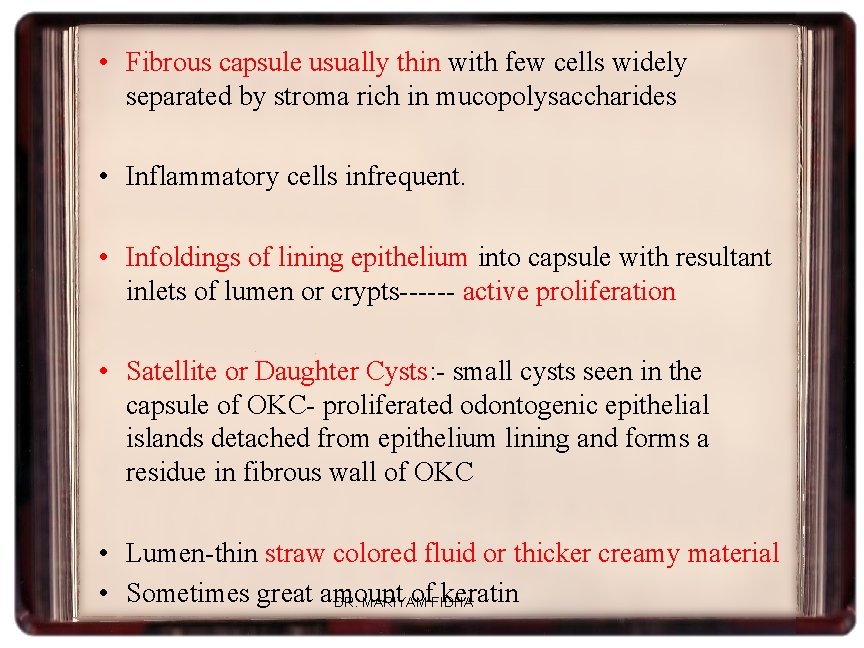
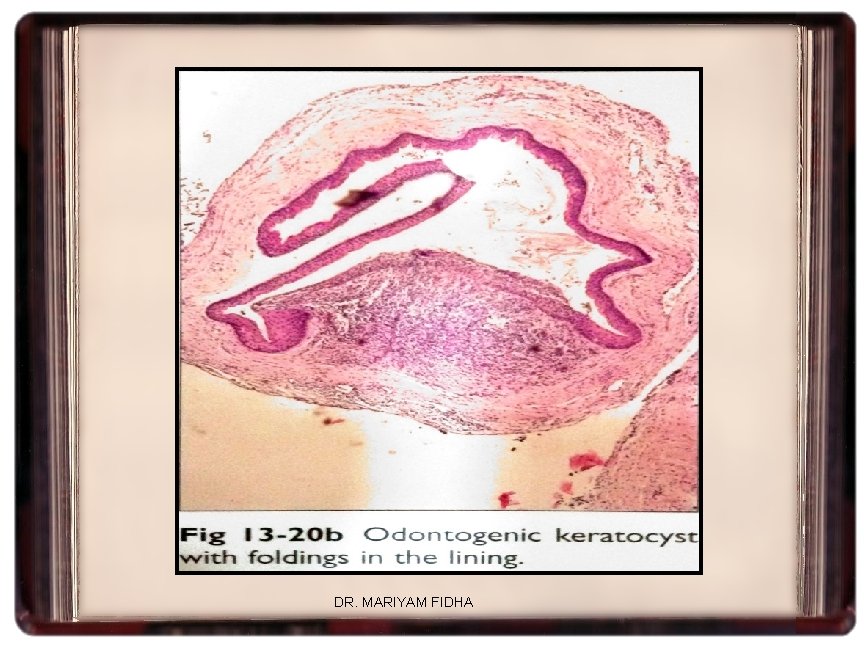
• Fibrous capsule usually thin with few cells widely separated by stroma rich in mucopolysaccharides • Inflammatory cells infrequent. • Infoldings of lining epithelium into capsule with resultant inlets of lumen or crypts------ active proliferation • Satellite or Daughter Cysts: - small cysts seen in the capsule of OKC- proliferated odontogenic epithelial islands detached from epithelium lining and forms a residue in fibrous wall of OKC • Lumen-thin straw colored fluid or thicker creamy material • Sometimes great amount of. FIDHA keratin DR. MARIYAM
DR. MARIYAM FIDHA

DR. MARIYAM FIDHA

EARLY ATTEMPTS AT LAB DIAGNOSIS OF OKC -Examining the cystic fluids from OKCs have soluble protein levels below 3. 5 g/dl and for nonkeratinizing cysts it is in the range of 5 -11 g/dl -A keratocyst antigen Kussela et al, 1982 showed an antigen in the fluid of OKCs that is not present in other cyst fluids nor in plasma or saliva Double antigen fluorescent tech localised the antigen to the epithelial cells of OKC and named it keratocyst antigen(KCA) -lactoferrin in OKC fluid Impermeable nature of OKC lining accounted for high concentratin of lactoferrin in the fluid and neutropils being the source-response to keratin in cyst lining-mediated by IL-1, chemotactic to neutrophils DR. MARIYAM FIDHA

Ultrastructural studies • Acc to Hansen, Philipsen and Ross ØSEM of parakeratinized forms shows complex series of elevations and depressions on cell surface Øorthokeratinized shows uniform, flat surface covered with a thick layer of leafy squames of orthokeratin with no epithelial infoldings ØTEM confirms presence of cytoplasmic interdigitations and desmosomal junctions-complex surface morphology Øjuxtaepithelially deep to lamina densa collagen shows dissolution (Philipsen et al) --- collagenase or other proteases --- responsible for ready separation of lining from CT DR. MARIYAM FIDHA

Immunohistochemistry -CK 7, 19 -all layers -CK 13, 16 -suprabasal layers -CK 8, 19 -basal layers -CK 1, 9, 10, 11 -absent -CEA and EMA-weak and patchy -BCL-2 ---strong in basal layer --PCNA, Ki-67, p 53 and IPO-38 are expressed more strongly in OKCs compared to other cysts DR. MARIYAM FIDHA
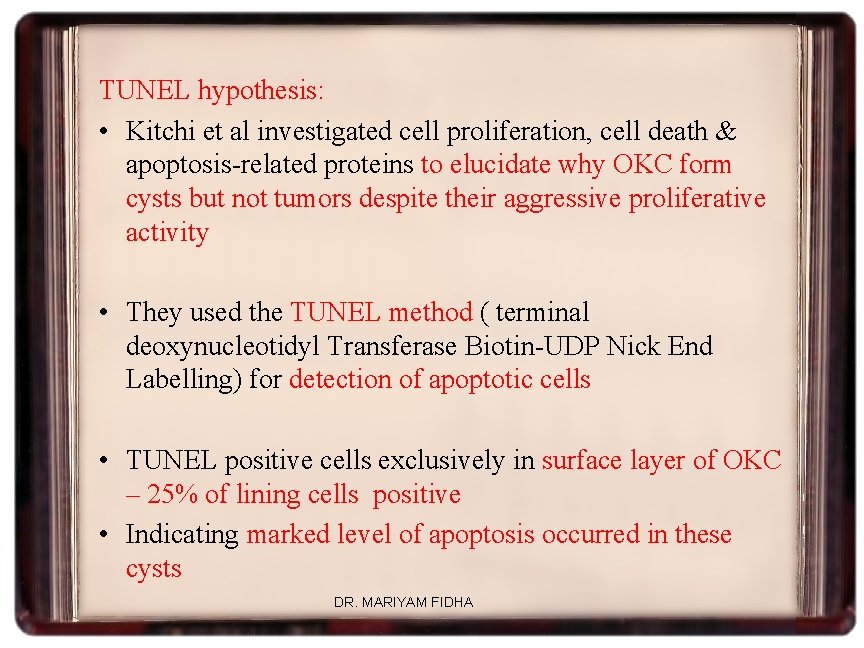
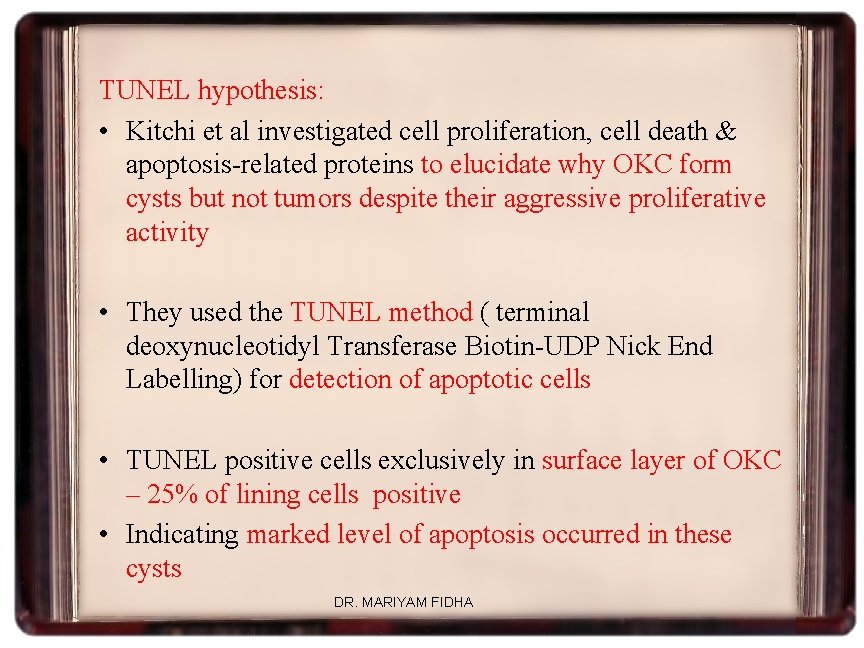
TUNEL hypothesis: • Kitchi et al investigated cell proliferation, cell death & apoptosis-related proteins to elucidate why OKC form cysts but not tumors despite their aggressive proliferative activity • They used the TUNEL method ( terminal deoxynucleotidyl Transferase Biotin-UDP Nick End Labelling) for detection of apoptotic cells • TUNEL positive cells exclusively in surface layer of OKC – 25% of lining cells positive • Indicating marked level of apoptosis occurred in these cysts DR. MARIYAM FIDHA

• Bcl 2 almost exclusively found in basal cell layer of OKC • Inhibited apoptosis to facilitate cellular proliferation in basal layer • Apoptosis in surface layer maintained the homeostasis of thickness of lining epithelium and allowed the synthesis of keratin • This way even though active proliferation occurred in lining of OKC – regulated by apoptosis – so lesions manifested as cysts rather than tumor masses DR. MARIYAM FIDHA
Differential Diagnosis • Cystic ameloblastoma- tall columnar basal cells that show nuclear polarization away from BM and sub epithelial hyalinization is seen, but in contrast to OKC, keratinization is never a feature • Lateral periodontal cyst- believed to arise from dental lamina, lined by st. sq. nonkeratinized epithelium contains focal thickenings or plques, like OKC it may be multiloculated but never shows keratinization • Glandular odontogenic cyst –multiloculated and show recurrence but lined by nonkeratinized epithelium with cuboidal cells in lining epithelium, with cilia and mucus cells that are not seen in OKC DR. MARIYAM FIDHA
Treatment • • Marsupialization Enucleation and curettage Peripheral ostectomy with bone bur-prevent recurrence Cyst broken through cortical plate and adhering to mucosa -excision of mucosa indicated • Large and aggressive lesion-resection and bone grafts • Chemical cautery of bony cavity or IL inj. of Carnoy’s solution to free the cyst from bony wall-easy removal • Insertion of polyethylene drainage tube-decompression and reduction-thick lining-easy removal DR. MARIYAM FIDHA
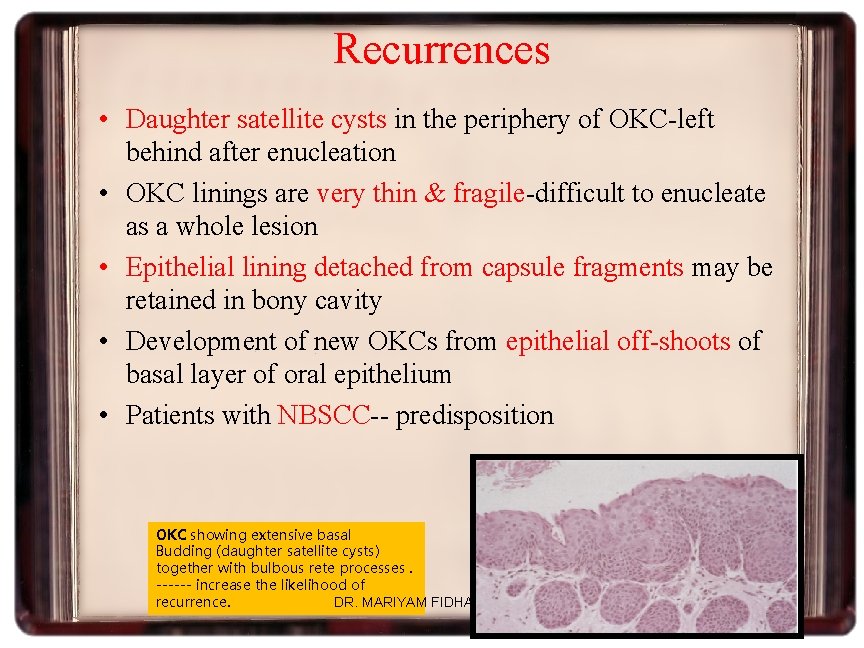
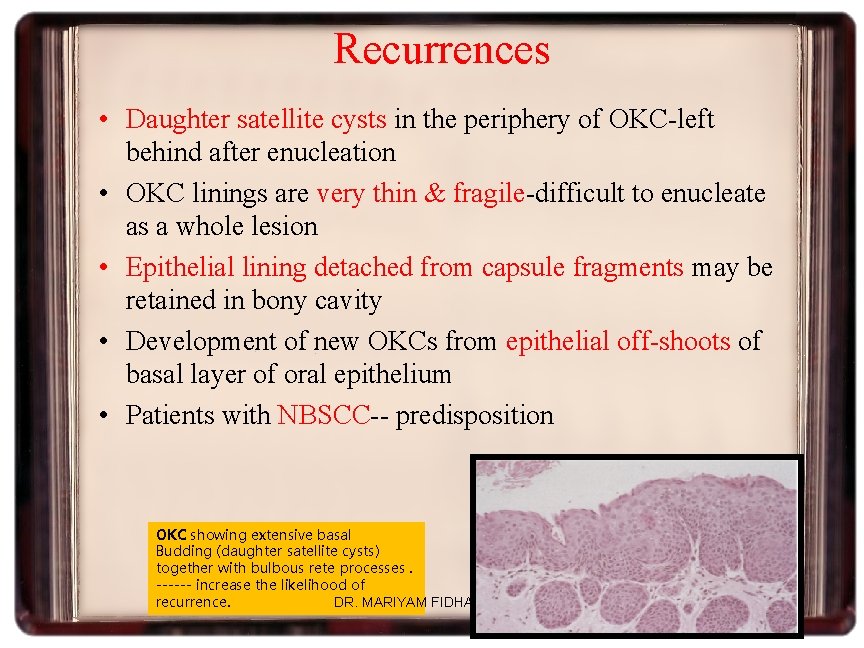
Recurrences • Daughter satellite cysts in the periphery of OKC-left behind after enucleation • OKC linings are very thin & fragile-difficult to enucleate as a whole lesion • Epithelial lining detached from capsule fragments may be retained in bony cavity • Development of new OKCs from epithelial off-shoots of basal layer of oral epithelium • Patients with NBSCC-- predisposition OKC showing extensive basal Budding (daughter satellite cysts) together with bulbous rete processes. ------ increase the likelihood of recurrence. DR. MARIYAM FIDHA
Orthokeratinized Odontogenic Cyst • • Orthokeratinized variant of OKC Less aggressive Represent 12 -13% of keratinizing odontogenic cysts Not asso. with NBCCS Clinical features • Teenagers and young adults • Male>females • Mand>max • Posterior areas of jaws • Approx 75% asso. with impacted tooth-clinically mimics dentigerous cyst DR. MARIYAM FIDHA

• Usually asymptomatic discovered in routine radiographs • Some cases-pain and swelling • Radiographically usually presents as a unilocular radiolucency • Size varies from 1 -7 cm in diameter DR. MARIYAM FIDHA

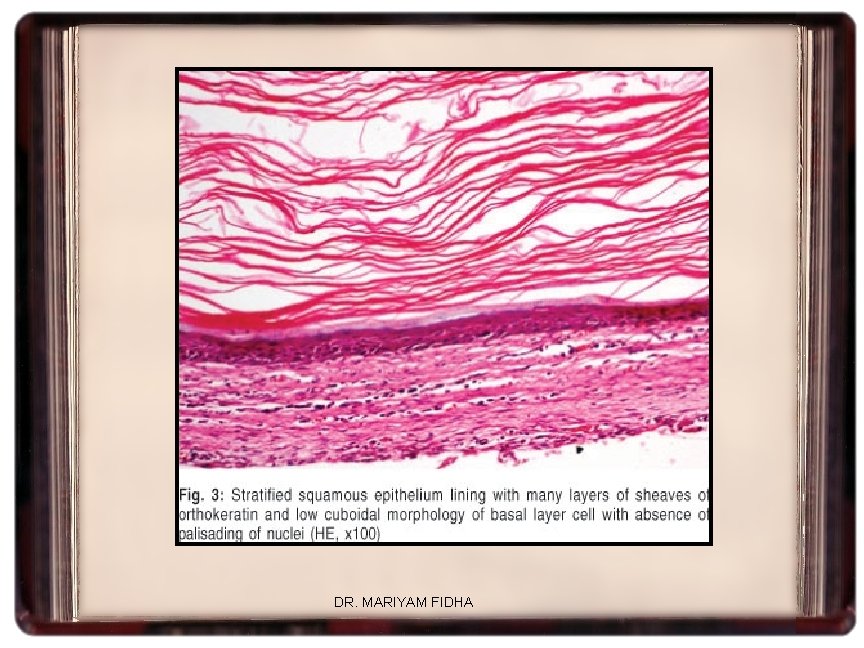
Histopathology • Lined by a thin, uniform layer of st. sq epithelium covered with orthokeratin • 4 -8 cell layer thickness • Prominent granular layer • No hyperchromatic basal layer • No satellite cysts • Basal layer consist of row of flattened to cuboidal cells with infrequent rete ridge formation • Orthokeratin is produced on epithelial surface and asso. with subjacent granular cell layer DR. MARIYAM FIDHA
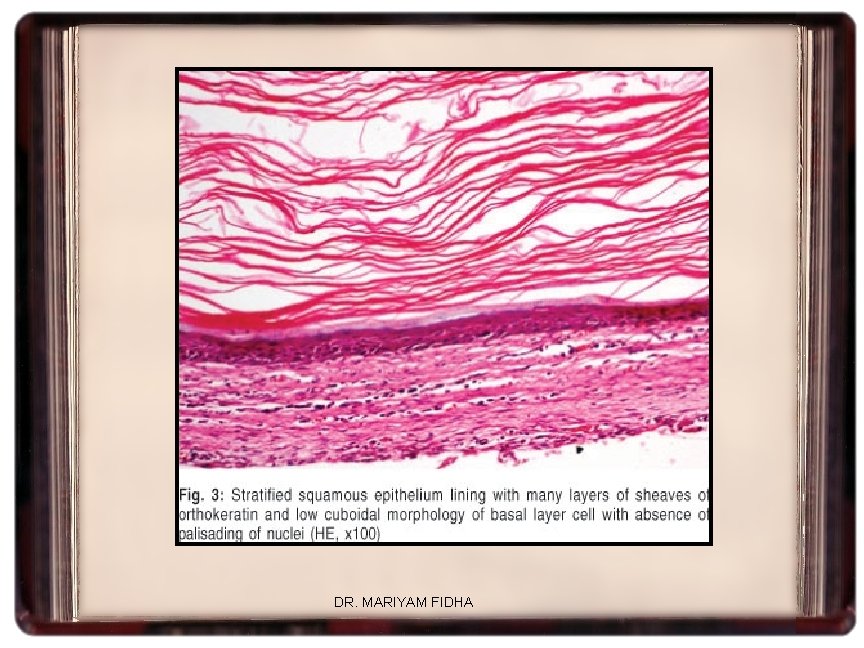
DR. MARIYAM FIDHA

• Abundant desquamated keratin in cyst lumen • Rare occasions-focal sebaceous glands found • Acc to Shear M, 2002, orthokeratinized variety is a different entity and should bear a different name -differences in immunoreactivity: -cytokeratin -epithelial membrane antigen(EMA) -carcinoembryonic antigen(CEA) • D/D -True odontogenic keratocyst -palisaded basal layer of columnar cells -hyperchromatic basal layer -corrugated layer of parakeratin on surface -no granular cell layer DR. MARIYAM FIDHA
REFERENCES DR. MARIYAM FIDHA
 Dr mariyam walls
Dr mariyam walls Mariyam visam
Mariyam visam Cavum vellum interpositum
Cavum vellum interpositum Sedimentation technique for stool concentration
Sedimentation technique for stool concentration Sru consensus ovarian cysts
Sru consensus ovarian cysts Sebaceous cyst vs dermoid cyst
Sebaceous cyst vs dermoid cyst Tapeworm
Tapeworm Contents introduction
Contents introduction Part whole model subtraction
Part whole model subtraction Unit ratio definition
Unit ratio definition Part part whole
Part part whole What is a technical description
What is a technical description Parts of front bar
Parts of front bar The phase of the moon you see depends on ______.
The phase of the moon you see depends on ______. Two way anova minitab 17
Two way anova minitab 17 The odyssey and epic poetry an introduction part 1
The odyssey and epic poetry an introduction part 1 Who was homer
Who was homer The odyssey and epic poetry: an introduction, part 1
The odyssey and epic poetry: an introduction, part 1 Hamlet part 1 an introduction to elizabethan theater
Hamlet part 1 an introduction to elizabethan theater Good introduction paragraph
Good introduction paragraph The odyssey and epic poetry an introduction part 1
The odyssey and epic poetry an introduction part 1 The odyssey and epic poetry an introduction part 1
The odyssey and epic poetry an introduction part 1 Homers epic poem
Homers epic poem An introduction to the odyssey
An introduction to the odyssey Hamlet, part 1: an introduction to elizabethan theater
Hamlet, part 1: an introduction to elizabethan theater Benvolio quotes act 1, scene 1
Benvolio quotes act 1, scene 1 The odyssey and epic poetry an introduction part 1
The odyssey and epic poetry an introduction part 1 Mrcog registration
Mrcog registration The odyssey and epic poetry an introduction part 1
The odyssey and epic poetry an introduction part 1 The odyssey and epic poetry an introduction part 1
The odyssey and epic poetry an introduction part 1 Introduction for portfolio
Introduction for portfolio Deep perineal pouch contents
Deep perineal pouch contents Febrile non hemolytic transfusion reaction
Febrile non hemolytic transfusion reaction Fresh frozen plasma vs platelets
Fresh frozen plasma vs platelets Level of the sternal angle
Level of the sternal angle Tabique intermuscular vastoaductor
Tabique intermuscular vastoaductor Posterior mediastinum
Posterior mediastinum The immortal life of henrietta lacks table of contents
The immortal life of henrietta lacks table of contents Medial lemniscus
Medial lemniscus Muscles of scapula region
Muscles of scapula region Contents of the ark of the covenant
Contents of the ark of the covenant Anatomy of a comic
Anatomy of a comic Right colic flexure
Right colic flexure Mla table of contents
Mla table of contents Stylistic lexicology
Stylistic lexicology School magazine contents page
School magazine contents page Research methodology contents
Research methodology contents Report appendix example
Report appendix example Ffp vs platelets
Ffp vs platelets Contents of the middle mediastinum
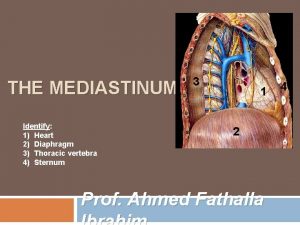
Contents of the middle mediastinum Pericardium mediastinum
Pericardium mediastinum Indicative abstract example
Indicative abstract example Persepolis table
Persepolis table Persepolis table of contents
Persepolis table of contents Interactive notebook table of contents
Interactive notebook table of contents Fresh frozen plasma contents
Fresh frozen plasma contents Cerebellum nuclei
Cerebellum nuclei Processus vaginalis anatomy
Processus vaginalis anatomy Greater sciatic foramen contents
Greater sciatic foramen contents Swot analysis event management
Swot analysis event management Anterior mediastinum contents
Anterior mediastinum contents Mediastinum image
Mediastinum image Carotid triangle contents
Carotid triangle contents Triangular space contents
Triangular space contents Curriculum vitaem
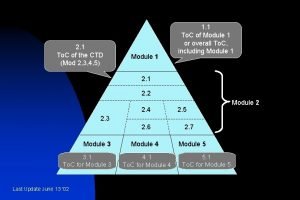
Curriculum vitaem Module 3 ctd table contents
Module 3 ctd table contents Annexure to cost audit report
Annexure to cost audit report Civics interactive notebook
Civics interactive notebook The city of ember poppy
The city of ember poppy Fresh frozen plasma transfusion time
Fresh frozen plasma transfusion time Air pollution contents
Air pollution contents Content page magazine
Content page magazine Nerve in cubital fossa
Nerve in cubital fossa Fossa in elbow joint
Fossa in elbow joint Triangle
Triangle Quadriceps femoral
Quadriceps femoral Cubital fossa boundaries
Cubital fossa boundaries Content of femoral triangle
Content of femoral triangle Coracohumeral
Coracohumeral Historical context of hamlet
Historical context of hamlet Mnemonic operation code
Mnemonic operation code Ctd module 5 table of contents
Ctd module 5 table of contents Urogenital triangle borders
Urogenital triangle borders Importance of edp
Importance of edp Scrapbook table of contents
Scrapbook table of contents Erb point neck
Erb point neck