CYSTIC FIBROSIS Is a complex metabolic disorder characterized
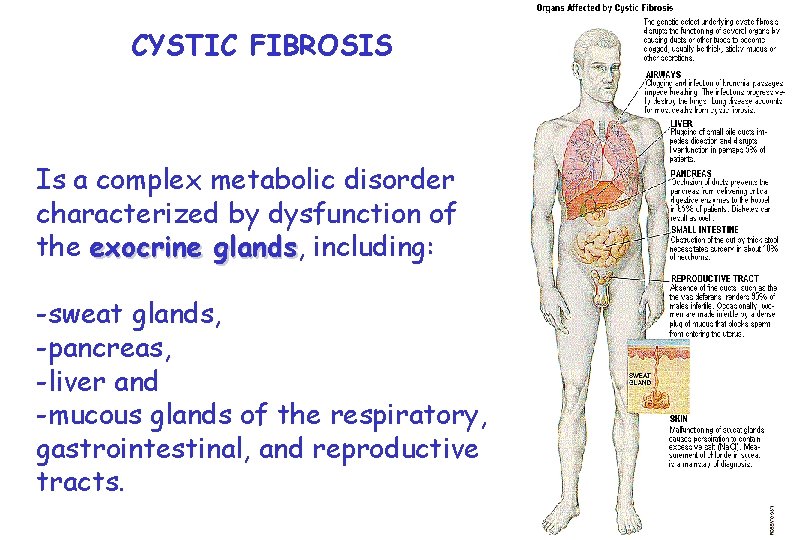
CYSTIC FIBROSIS Is a complex metabolic disorder characterized by dysfunction of the exocrine glands, glands including: -sweat glands, -pancreas, -liver and -mucous glands of the respiratory, gastrointestinal, and reproductive tracts.
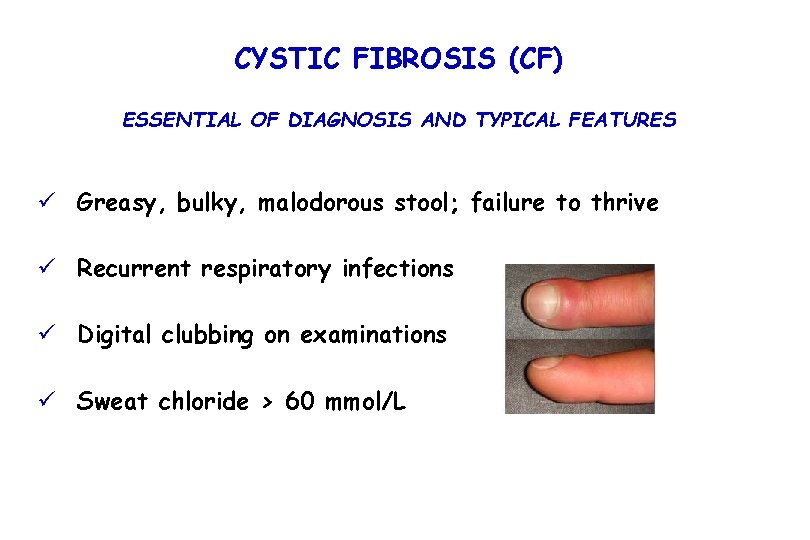
CYSTIC FIBROSIS (CF) ESSENTIAL OF DIAGNOSIS AND TYPICAL FEATURES ü Greasy, bulky, malodorous stool; failure to thrive ü Recurrent respiratory infections ü Digital clubbing on examinations ü Sweat chloride > 60 mmol/L
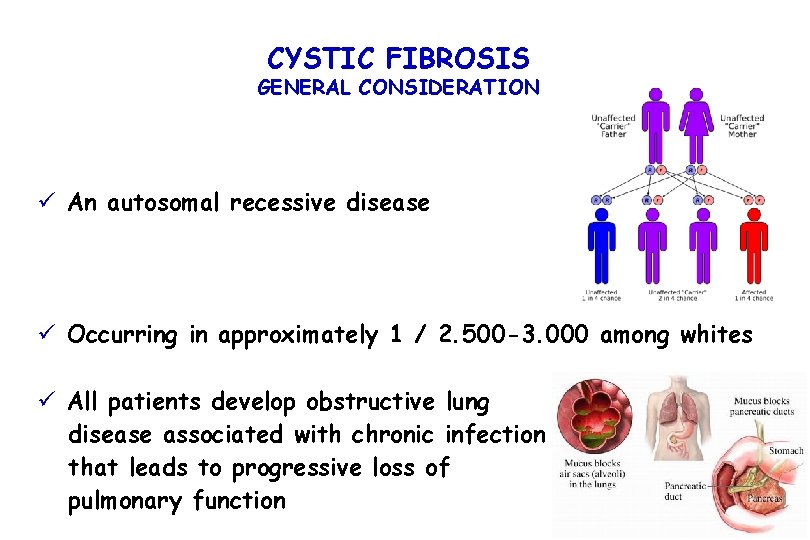
CYSTIC FIBROSIS GENERAL CONSIDERATION ü An autosomal recessive disease ü Occurring in approximately 1 / 2. 500 -3. 000 among whites ü All patients develop obstructive lung disease associated with chronic infection that leads to progressive loss of pulmonary function
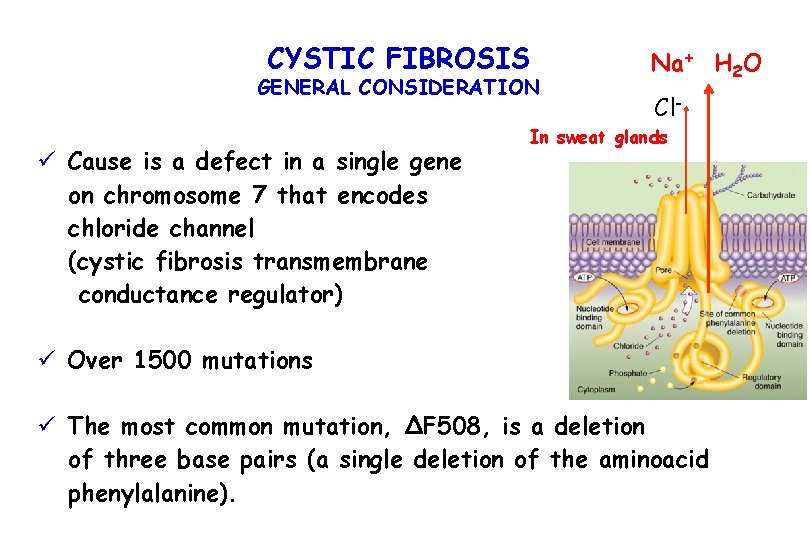
CYSTIC FIBROSIS GENERAL CONSIDERATION ü Cause is a defect in a single gene on chromosome 7 that encodes chloride channel (cystic fibrosis transmembrane conductance regulator) Na+ H 2 O Cl- In sweat glands ü Over 1500 mutations ü The most common mutation, ΔF 508, is a deletion of three base pairs (a single deletion of the aminoacid phenylalanine).
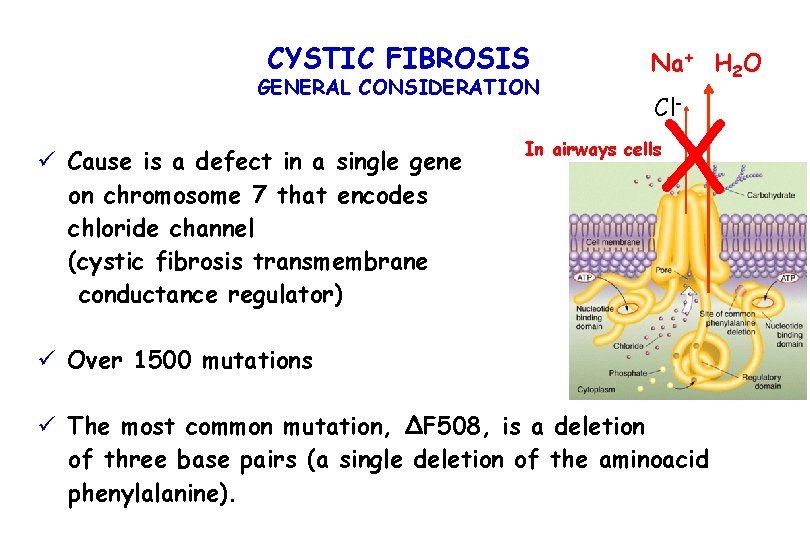
CYSTIC FIBROSIS GENERAL CONSIDERATION ü Cause is a defect in a single gene on chromosome 7 that encodes chloride channel (cystic fibrosis transmembrane conductance regulator) Na+ H 2 O X Cl- In airways cells ü Over 1500 mutations ü The most common mutation, ΔF 508, is a deletion of three base pairs (a single deletion of the aminoacid phenylalanine).
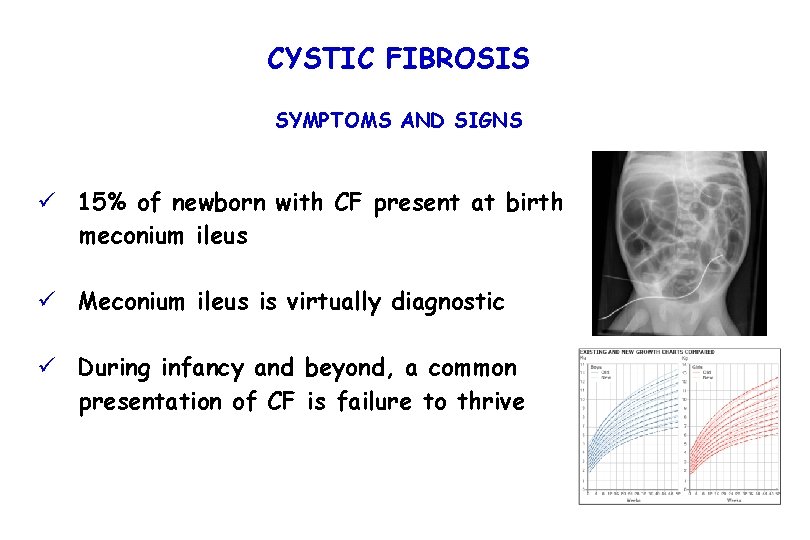
CYSTIC FIBROSIS SYMPTOMS AND SIGNS ü 15% of newborn with CF present at birth meconium ileus ü Meconium ileus is virtually diagnostic ü During infancy and beyond, a common presentation of CF is failure to thrive
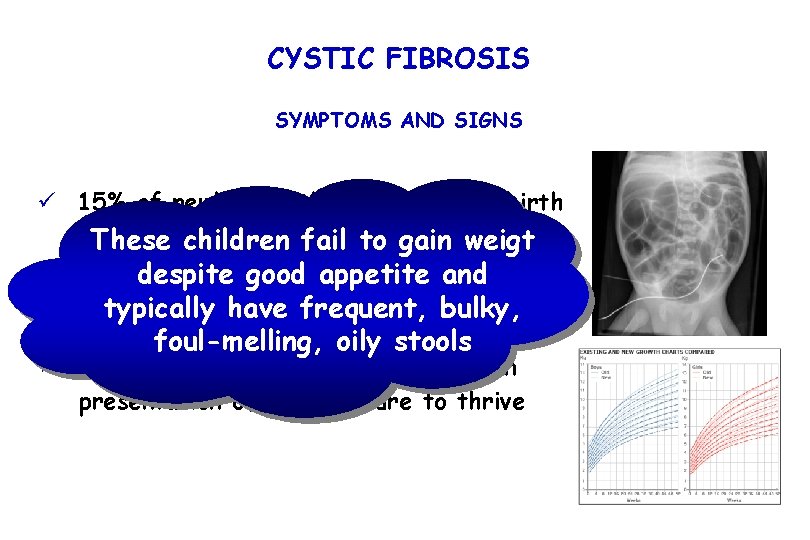
CYSTIC FIBROSIS SYMPTOMS AND SIGNS ü 15% of newborn with CF present at birth meconium ileus These children fail to gain weigt despite good appetite and ü Meconium ileus is virtually diagnostic typically have frequent, bulky, foul-melling, oily stools ü During infancy and beyond, a common presentation of CF is failure to thrive
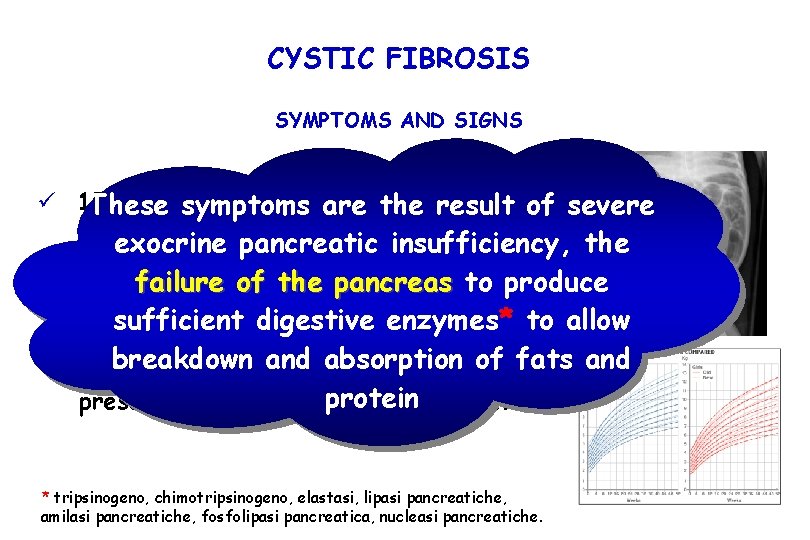
CYSTIC FIBROSIS SYMPTOMS AND SIGNS ü 15% of newborn withare CF present at birth These symptoms the result of severe meconium ileuspancreatic insufficiency, the exocrine failure of the pancreas to produce ü Meconium ileus is virtually diagnostic sufficient digestive enzymes* to allow breakdown andbeyond, absorption of fats and ü During infancy and a common presentation of CF isprotein failure to thrive * tripsinogeno, chimotripsinogeno, elastasi, lipasi pancreatiche, amilasi pancreatiche, fosfolipasi pancreatica, nucleasi pancreatiche.
CYSTIC FIBROSIS SYMPTOMS AND SIGNS ü Pancreatic insufficiency occurs in over 85% of person with CF ü Infants with undiagnosed CF may also present with hypoproteinemia with or without edema, anemia, and deficiency of the fat-soluble vitamins A, D, E, and K, because of ongoing steatorrhea.
CYSTIC FIBROSIS SYMPTOMS AND SIGNS ü Respiratory symptoms: - chronic productive cough - wheezing - exercise intolerance ü Recurrent pneumonia and or bronchitis ü Digital clubbing ü Pulmonary exacerbations with increased cough and sputum production, increased dyspnea, poor appetite, weight loss, occasionally fever, fatigue, reduction in pulmonary function, increased hemoptisis
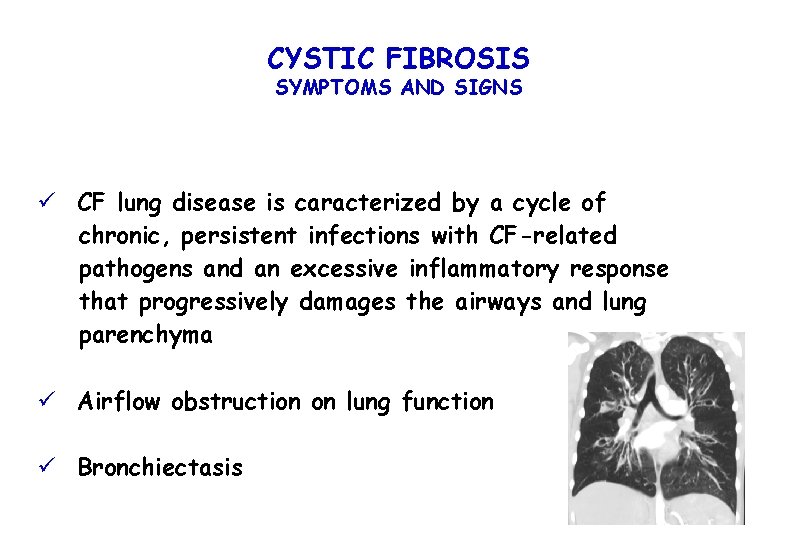
CYSTIC FIBROSIS SYMPTOMS AND SIGNS ü CF lung disease is caracterized by a cycle of chronic, persistent infections with CF-related pathogens and an excessive inflammatory response that progressively damages the airways and lung parenchyma ü Airflow obstruction on lung function ü Bronchiectasis
CYSTIC FIBROSIS related DISEASES üAltered growth and nutrition, üAllergic bronchopulmonary aspergillosis üDiabetes mellitus and liver diseases (both seen in approximately 15 -20% of adolescents and adults), üOsteoporosis, Arthropaty and arthritis, üInfertility in men due to bilateral absence of the vas deferens, X üWomen are fertile but pregancy is risky both for the mother and fetus.
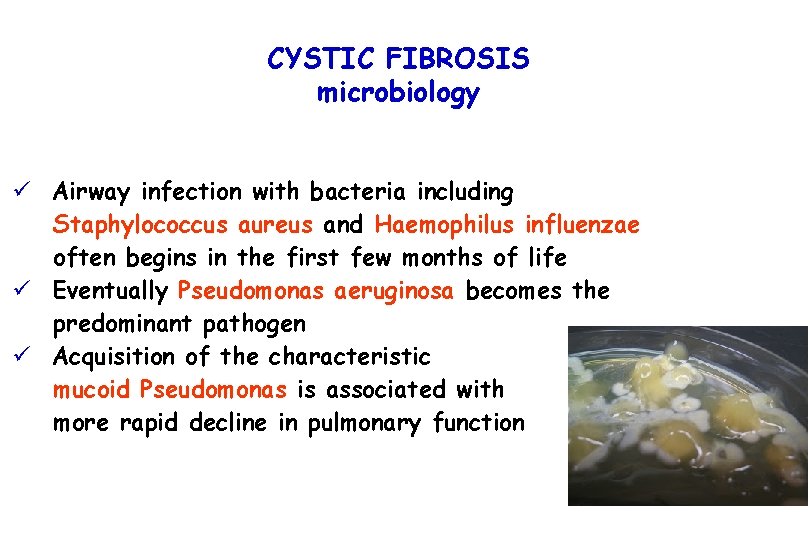
CYSTIC FIBROSIS microbiology ü Airway infection with bacteria including Staphylococcus aureus and Haemophilus influenzae often begins in the first few months of life ü Eventually Pseudomonas aeruginosa becomes the predominant pathogen ü Acquisition of the characteristic mucoid Pseudomonas is associated with more rapid decline in pulmonary function
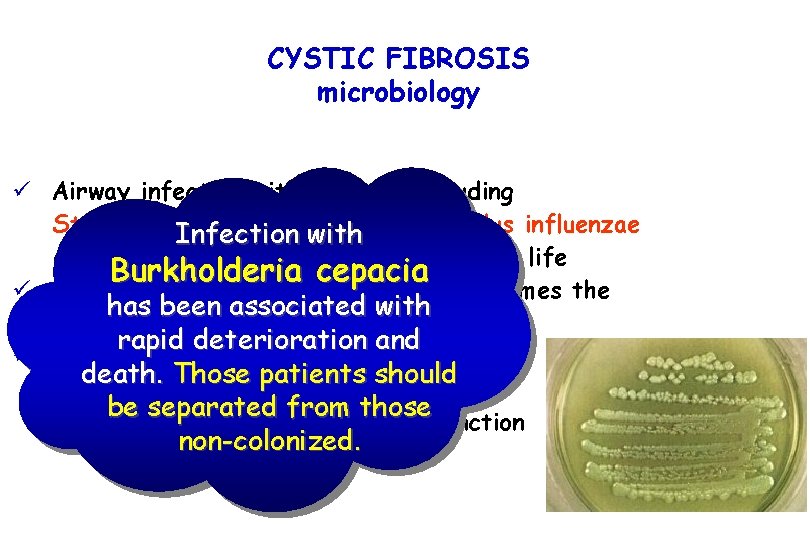
CYSTIC FIBROSIS microbiology ü Airway infection with bacteria including Staphylococcus aureuswith and Haemophilus influenzae Infection often begins in the first few months of life Burkholderia cepacia ü Eventually Pseudomonas aeruginosa becomes the has been associated with predominant pathogen rapid deterioration and ü Acquisition of the characteristic death. Those patients should mucoid Pseudomonas is associated with be separated from those more rapid decline in pulmonary function non-colonized.
CYSTIC FIBROSIS diagnosis ü CF should also be considered in infants and children who present with severe dehydration and hypochloremic alkalosis ü Other findings that should prompt a diagnostic evaluation for Cf include: - unexplained bronchiectasis, - rectal prolapse, - nasal polyps, - chronic sinusitis and - unexplained pancreatitis or cirrhosis
CYSTIC FIBROSIS diagnosis ü Sweat Chloride concentrations > 60 mmol/l * - in the presence of some appropriate clinical manifestation: -chronic pulmonary disease -pancreatic insufficiency - or an appropriate family history: -sibling or first cousin who has CF. * Borderline sweat test results are more commonly seen in patients with retained pancreatic function
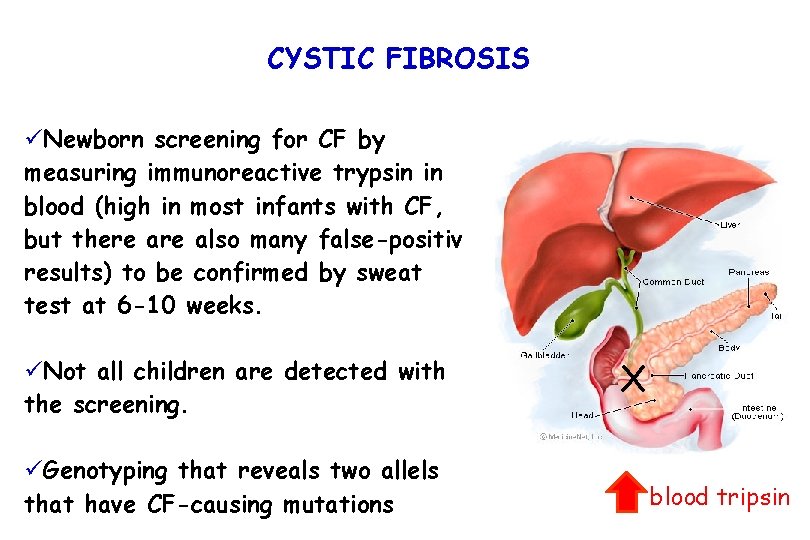
CYSTIC FIBROSIS üNewborn screening for CF by measuring immunoreactive trypsin in blood (high in most infants with CF, but there also many false-positive results) to be confirmed by sweat test at 6 -10 weeks. üNot all children are detected with the screening. üGenotyping that reveals two allels that have CF-causing mutations X blood tripsin
CYSTIC FIBROSIS üNewborn screening for CF by Therefore diagnosis measuring immunoreactive trypsin in blood (high in most infants with CF, must be confirmed by but there also many false-positive sweat test or by genotyping results) to be confirmed by sweat test at 6 -10 weeks. üNot all children are detected with the screening. üGenotyping that reveals two allels that have CF-causing mutations X blood tripsin
CYSTIC FIBROSIS TREATMENT ü Followed at a accredited CF care center ü Pancreatic enzyme supplementation immediately prior to each meal and with snacks ü Daily multivitamins that contain vitamins A, D, E, K ü Caloric supplements
CYSTIC FIBROSIS TREATMENT ü Airway clearance ü Aggressive antibiotic use ü Inhaled mucolitic agent ü Recombinant human DNase (Pulmozyme) ü Inhaled tobramycin ü Oral azitromycin
CYSTIC FIBROSIS PROGNOSIS ü Median life expectancy is around 35 -45 years of age ü Lung transplantation ( As many as 90% of people with CF are alive 1 year after transplantation, and 50% are alive after 5 years. ) ü Gene therapy (under research)
CYSTIC FIBROSIS PROGNOSIS Once the person has received a lung transplant, does CF "go away? " Transplanted lungs come from people who do not have CF, so the new lungs do not have CF. However, after the transplant, the recipient still has CF in the sinuses, pancreas, intestines, sweat glands, and reproductive tract. The new lungs do not “get” CF, but immunosuppressive drugs may decrease the ability to fight germs like Pseudomonas aeruginosa and Burkholderia cepacia (B. cepacia ). These germs may stay in the upper airways after a transplant and can infect the new lungs. The risks of infection are highest right after the transplant operation when immunosuppressive drugs are given at the highest doses so the body will not reject the new lungs. However, these drugs also make it hard for the body to fight infections, which can lead to lung disease.
CYSTIC FIBROSIS PROGNOSIS Can a person with CF who has B. cepacia receive a lung transplant? Survival for people with B. cepacia after a transplant is not as good as for those without these bacteria. Many lung transplant centers will not accept people with CF who have B. cepacia. The lung transplant coordinator at the center will know if it will transplant someone with B. cepacia.
- Slides: 23