CWFT Strategy for Clinical Systems and IT Executive


- Slides: 43
CWFT Strategy for Clinical Systems and IT
Executive Summary ( 1 / 2 ) This Strategy for Clinical Systems and IT (CS&IT) responds to the vision and ambitions of our Clinical Services Strategy, the commitments made in our Integrated Business Plan, the financial plan set out in our Long Term Financial Model, and other internal and external factors. The purpose of this document is to detail the emerging strategy for CS&IT. It outlines current plans and future priorities and raises a number of topics requiring further investigation / decision. It covers the following major elements: 1. Background and drivers sets out key local and national drivers and context that we need to respond to. We recognise that changes to deliver a sustainable health system across NW London will place demands on our clinical systems, and that in developing our clinical blueprint we must enable services to respond to the needs of our local population. We further recognise that new models of care will be patient centred and that our clinical systems and IT infrastructure / security models have to assume and encourage significantly greater direct interaction by / with our patients and the wider population. 2. The Analysis section considers how we will develop our clinical systems and IT in response to the context and drivers: • We must respond to the assessment of our current position (Section 3. 2) • We must respond to the seven priorities set out in our Clinical Services Strategy (Section 3. 3) • There are basic infrastructure and shared services that we need in place across both sites (Section 3. 4) • We need to take steps to rationalise systems across both sites (Section 3. 5) • We will enhance our systems to improve quality and realise cost savings and productivity benefits ahead of a full EPR (Section 3. 6) • New and transformed models of care likely to have significant implications on our clinical systems and IT (Section 3. 7) 2
Executive Summary ( 2 / 2 ) 3. The emerging forward plan consolidates the actions to support delivery of agreed priorities and sets out the key options for development and the decisions needed. It clearly articulates: • The five key elements of the CS&IT vision which will move us simple digitisation to using clinical systems to improve the health of the communities we serve (Section 4. 1) • The patient centric view of the EPR as an integrated source of Patient information (Section 4. 2) • The key principles underlying the strategy (Section 4. 3) • Benefits associated with the EPR (Section 4. 4) • The Clinical Systems & IT Roadmap (Section 4. 5) • Summary plans and options for Clinical System and IT projects / programmes of work (Section 4. 6) • The supporting Financial model (Section 4. 7) • Key risks and barriers (Section 4. 8) • Project delivery and governance (Section 4. 9) 4. The decisions and next steps section highlights key activity and areas for further consideration (Section 5. 1) Members of the Trust Board are asked to: • Support the overall direction of this strategy with delegated authority to the IT Directorate to develop options and plans • Agree the key decisions needed over the short, medium and long term • Provide endorsement in principle to the associated programme of work. 3
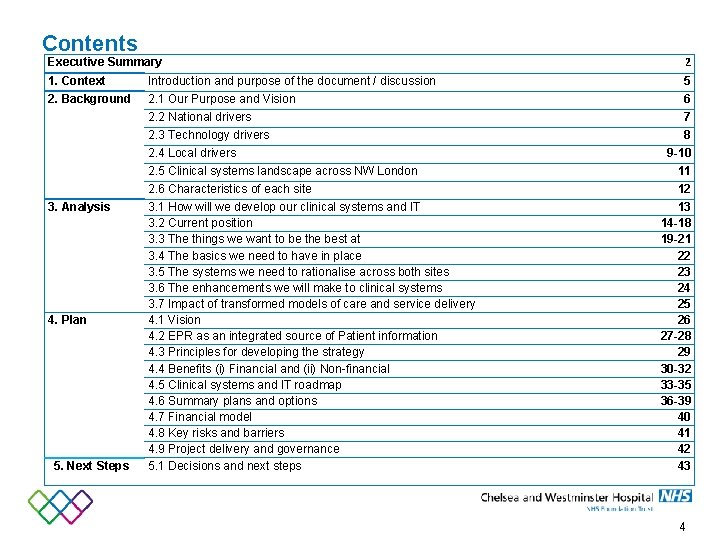
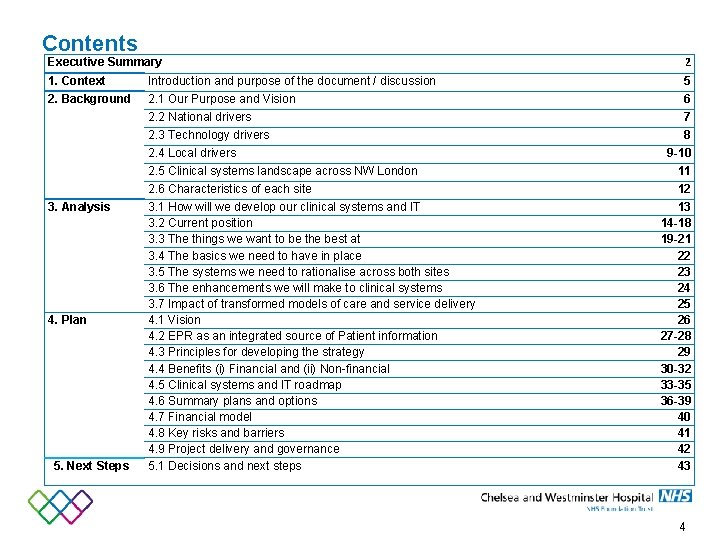
Contents Executive Summary 2 1. Context Introduction and purpose of the document / discussion 5 2. Background 2. 1 Our Purpose and Vision 6 2. 2 National drivers 7 2. 3 Technology drivers 8 2. 4 Local drivers 3. Analysis 4. Plan 5. Next Steps 9 -10 2. 5 Clinical systems landscape across NW London 11 2. 6 Characteristics of each site 12 3. 1 How will we develop our clinical systems and IT 3. 2 Current position 3. 3 The things we want to be the best at 3. 4 The basics we need to have in place 3. 5 The systems we need to rationalise across both sites 3. 6 The enhancements we will make to clinical systems 3. 7 Impact of transformed models of care and service delivery 4. 1 Vision 4. 2 EPR as an integrated source of Patient information 4. 3 Principles for developing the strategy 4. 4 Benefits (i) Financial and (ii) Non-financial 4. 5 Clinical systems and IT roadmap 4. 6 Summary plans and options 4. 7 Financial model 4. 8 Key risks and barriers 4. 9 Project delivery and governance 5. 1 Decisions and next steps 13 14 -18 19 -21 22 23 24 25 26 27 -28 29 30 -32 33 -35 36 -39 40 41 42 43 4
1. Context The purpose of this document is to set out the Strategy for Clinical Systems and IT and how this links to the Clinical Services Strategy and other drivers Our Clinical Services Strategy sets out how we deliver excellent experience and outcomes for patients through delivering services that are clinically, operationally and financially sustainable. The Strategy for Clinical Systems and IT describes how the Clinical and Informatics systems and technology solutions enable the Clinical Services Strategy, support the wider organisational vision and meet the demands of our commissioners and other stakeholders. The key enablers are: • Provision of resilient IT infrastructure in all locations where access to clinical and operational systems is required and provision of appropriate devices to access systems at the point of need; to include appropriate levels of security and Information Governance • Implementation of ‘intelligent’ clinical systems which enable adoption of standard pathways / evidence based care, provide clinical decision support, are fully integrated (e. g. with internal and external third party systems and Medical Devices / new technologies) and support learning, teaching and research • Provision of a single (where appropriate, summary) view of patient records to Trust staff, approved external stakeholders (e. g. Accountable Care Groups) and patients; including the ability for all authorised users (including patients) to interact with those records • Provision of live analytics, core reports (Operational / Management / Financial) and data mining for a range of secondary uses including clinical audit and research The Clinical Systems & IT Strategy was included within the Acquisition Business Case. It has been revised in line with the Clinical Services Strategy and within the context of developing national / local drivers and innovative technologies. This strategy remains largely aligned with the direction of travel and funding assumed within the LTFM. 5
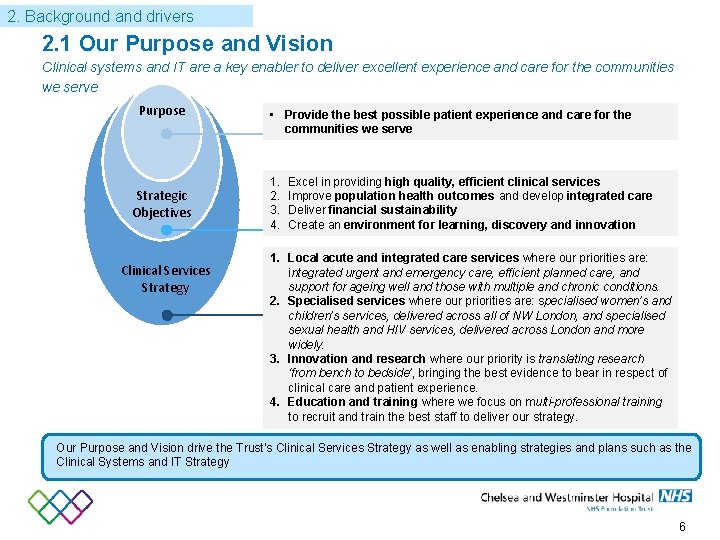
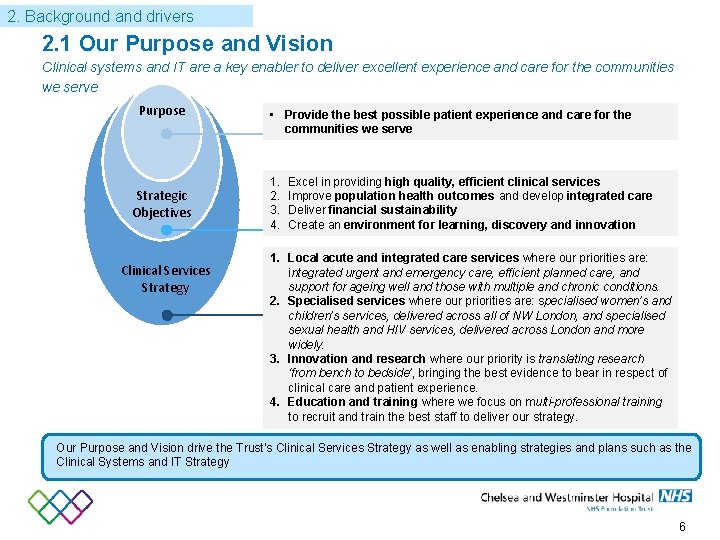
2. Background and drivers 2. 1 Our Purpose and Vision Clinical systems and IT are a key enabler to deliver excellent experience and care for the communities we serve Purpose Strategic Objectives Clinical Services Strategy • Provide the best possible patient experience and care for the communities we serve 1. 2. 3. 4. Excel in providing high quality, efficient clinical services Improve population health outcomes and develop integrated care Deliver financial sustainability Create an environment for learning, discovery and innovation 1. Local acute and integrated care services where our priorities are: integrated urgent and emergency care, efficient planned care, and support for ageing well and those with multiple and chronic conditions. 2. Specialised services where our priorities are: specialised women’s and children’s services, delivered across all of NW London, and specialised sexual health and HIV services, delivered across London and more widely. 3. Innovation and research where our priority is translating research ‘from bench to bedside’, bringing the best evidence to bear in respect of clinical care and patient experience. 4. Education and training where we focus on multi-professional training to recruit and train the best staff to deliver our strategy. Our Purpose and Vision drive the Trust’s Clinical Services Strategy as well as enabling strategies and plans such as the Clinical Systems and IT Strategy 6
2. Background and drivers 2. 2 National drivers Our strategy for developing our clinical systems and IT must respond to significant national drivers Pressures on NHS services • The Five Year Forward View recognised the need for the NHS and Social Care to exploit the information revolution to meet a number of fundamental challenges: • the health and wellbeing gap • the care and quality gap • the funding and efficiency gap • The NHS Services, Seven Days a Week Forum (2014) reported to NHS England on how NHS services can be improved to provide a more responsive and patient centred service across the seven-day week, with an initial focus on urgent and emergency care. Making these improvements will require significant changes to how we work and to the enabling clinical systems and technology solutions that support service transformation. Using Information and Technology to meet these challenges • In November 2014 the National Information Board produced “Personalised Health & Care 2020, Using Data and Technology to Transform Outcomes for Patients and Citizens – A framework for action”. It stated: “Better use of data and technology has the power to improve health, transforming the quality and reducing the cost of health and care services. It can give patients and citizens more control over their health and wellbeing , empower carers, reduce the administrative burden for care professionals, and support the development of new medicines and treatments”. • This document committed that local health and care economies would, by April 2016: • produce detailed roadmaps highlighting how, amongst a range of digital service capabilities, they will ensure clinicians in all care settings will be operating without the need to find or complete paper records by 2018; and • that by 2020 all patient and care records will be digital, real time and interoperable. The NHS must make best use of technology and data to enable improved health and outcomes for patients, better quality of care, and greater efficiency of services. The themes of digitising data and putting patients at the centre of service provision are core elements of this Clinical Systems & IT Strategy 7
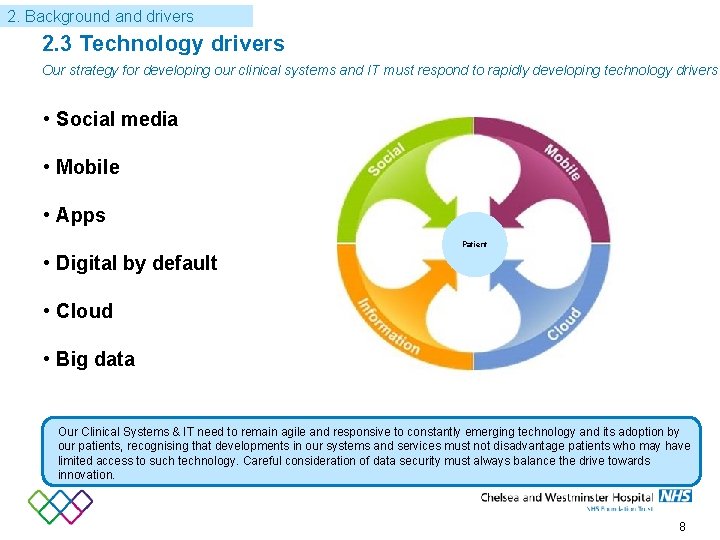
2. Background and drivers 2. 3 Technology drivers Our strategy for developing our clinical systems and IT must respond to rapidly developing technology drivers • Social media • Mobile • Apps Patient • Digital by default • Cloud • Big data Our Clinical Systems & IT need to remain agile and responsive to constantly emerging technology and its adoption by our patients, recognising that developments in our systems and services must not disadvantage patients who may have limited access to such technology. Careful consideration of data security must always balance the drive towards innovation. 8
2. Background and drivers 2. 4 Local drivers (1 / 2) Local strategies and fixed points will inform our approach – in particular Sa. HF and Accountable Care Local commissioning landscape • NW London’s Shaping a Healthier Future (Sa. HF) aims to consolidate A&E and major acute services across the region, combined with the strengthening out of hospital care. Both CWFT and WMUH are designated as ‘major acute hospitals’ under Sa. HF and would see them retaining their A&Es with significant activity growth • Sa. HF’s vision of ‘whole systems integrated care’ requires a new way of delivering care. It is a model of care that starts with people’s needs, whether social, physical or mental, and makes sure that the whole system’s resources are directed to those needs. This model will mean self-empowerment, use of community capital, networks of GPs, networks of providers and the system enablers such as the right information, the right workforce, and the right estate to support it: a whole system of care. Pathways of care will need to be seamlessly managed across organisational boundaries • The post acquisition landscape is significantly more complex for CWFT with key relationships now to be maintained with 7 CCGs (and associated Local Authorities) as well as NHS England other commissioner and customer relationships Development of local plans for Integrated Care and Accountable Care • There are plans for the development of integrated care and the growth of accountable care models throughout the local health system. These are being driven locally through Sa. HF (including NW London’s Integrated Care Pioneer Pilot) and SW London’s equivalent whole system Strategy, but are also being catalysed by emerging plans in relation to the 5 YFV • The figure overleaf sets out the emerging collaborative landscape for Accountable Care. This is focused on four sectors: West, South, Upper East and Lower East. Having high quality, agile Clinical systems and IT will enable the Trust to collaborate on NW London’s ‘whole systems integrated care’ vision, whilst strengthening the quality and efficiency of hospital based services. It will enable the Trust to respond to rising patient expectations of healthcare and their role as consumers and to the emerging development of personlased medicine (e. g. Silico medicine and Genomics) 9
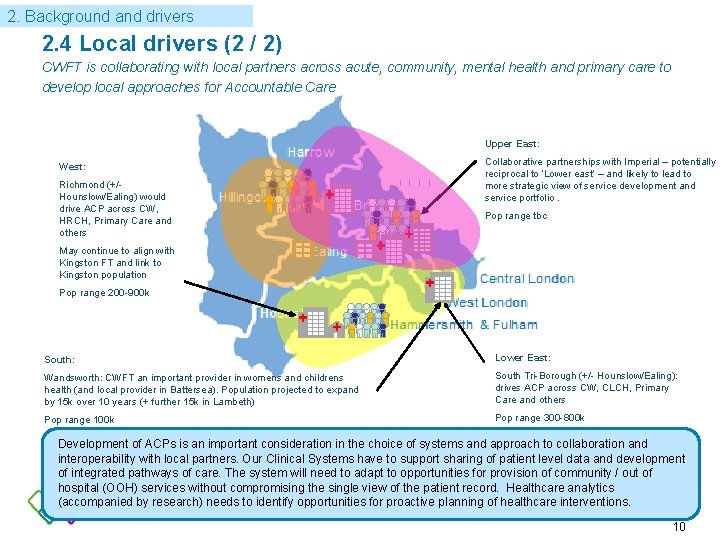
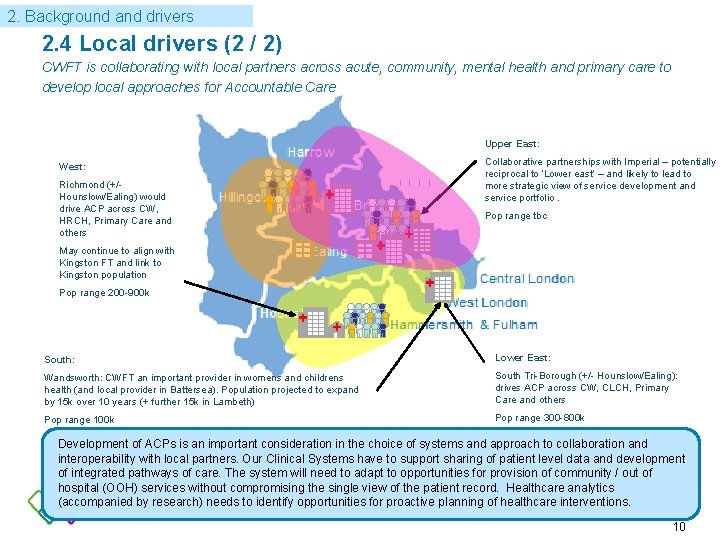
2. Background and drivers 2. 4 Local drivers (2 / 2) CWFT is collaborating with local partners across acute, community, mental health and primary care to develop local approaches for Accountable Care Upper East: West: Richmond (+/- Hounslow/Ealing) would drive ACP across CW, HRCH, Primary Care and others Collaborative partnerships with Imperial – potentially reciprocal to ‘Lower east’ – and likely to lead to more strategic view of service development and service portfolio. Pop range tbc May continue to align with Kingston FT and link to Kingston population Pop range 200 -900 k South: Lower East: Wandsworth: CWFT an important provider in womens and childrens health (and local provider in Battersea). Population projected to expand by 15 k over 10 years (+ further 15 k in Lambeth) South Tri-Borough (+/- Hounslow/Ealing): drives ACP across CW, CLCH, Primary Care and others Pop range 100 k Pop range 300 -800 k Development of ACPs is an important consideration in the choice of systems and approach to collaboration and interoperability with local partners. Our Clinical Systems have to support sharing of patient level data and development of integrated pathways of care. The system will need to adapt to opportunities for provision of community / out of hospital (OOH) services without compromising the single view of the patient record. Healthcare analytics (accompanied by research) needs to identify opportunities for proactive planning of healthcare interventions. 10
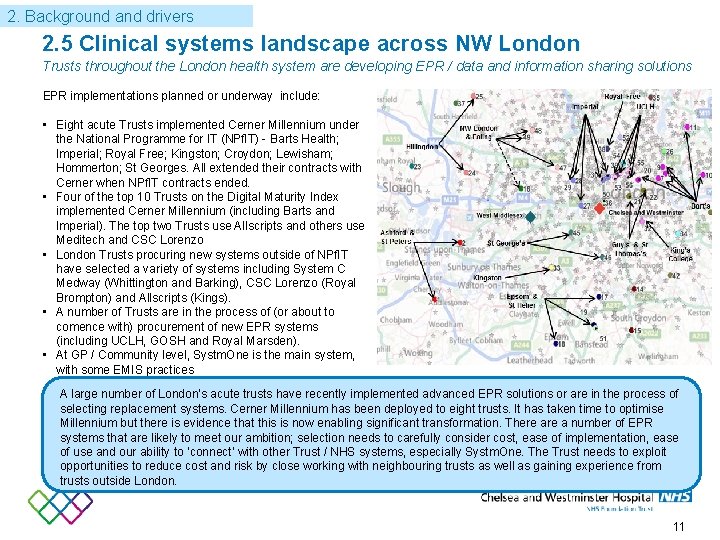
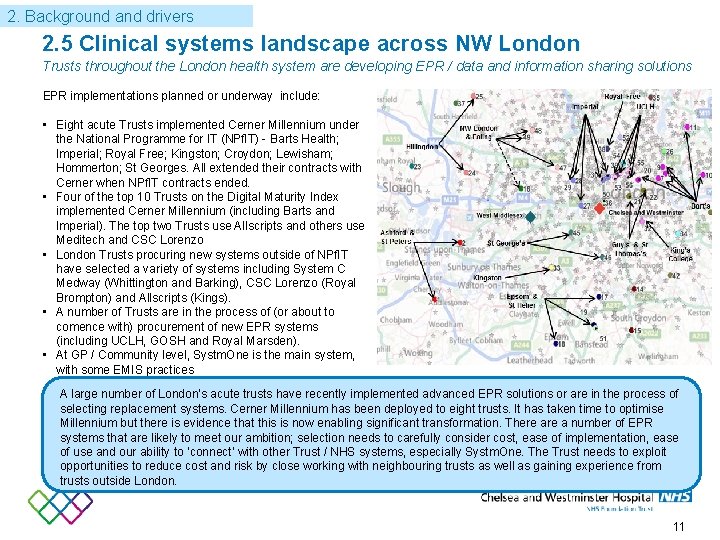
2. Background and drivers 2. 5 Clinical systems landscape across NW London Trusts throughout the London health system are developing EPR / data and information sharing solutions EPR implementations planned or underway include: • Eight acute Trusts implemented Cerner Millennium under the National Programme for IT (NPf. IT) - Barts Health; Imperial; Royal Free; Kingston; Croydon; Lewisham; Hommerton; St Georges. All extended their contracts with Cerner when NPf. IT contracts ended. • Four of the top 10 Trusts on the Digital Maturity Index implemented Cerner Millennium (including Barts and Imperial). The top two Trusts use Allscripts and others use Meditech and CSC Lorenzo • London Trusts procuring new systems outside of NPf. IT have selected a variety of systems including System C Medway (Whittington and Barking), CSC Lorenzo (Royal Brompton) and Allscripts (Kings). • A number of Trusts are in the process of (or about to comence with) procurement of new EPR systems (including UCLH, GOSH and Royal Marsden). • At GP / Community level, Systm. One is the main system, with some EMIS practices A large number of London‘s acute trusts have recently implemented advanced EPR solutions or are in the process of selecting replacement systems. Cerner Millennium has been deployed to eight trusts. It has taken time to optimise Millennium but there is evidence that this is now enabling significant transformation. There a number of EPR systems that are likely to meet our ambition; selection needs to carefully consider cost, ease of implementation, ease of use and our ability to ‘connect‘ with other Trust / NHS systems, especially Systm. One. The Trust needs to exploit opportunities to reduce cost and risk by close working with neighbouring trusts as well as gaining experience from trusts outside London. 11
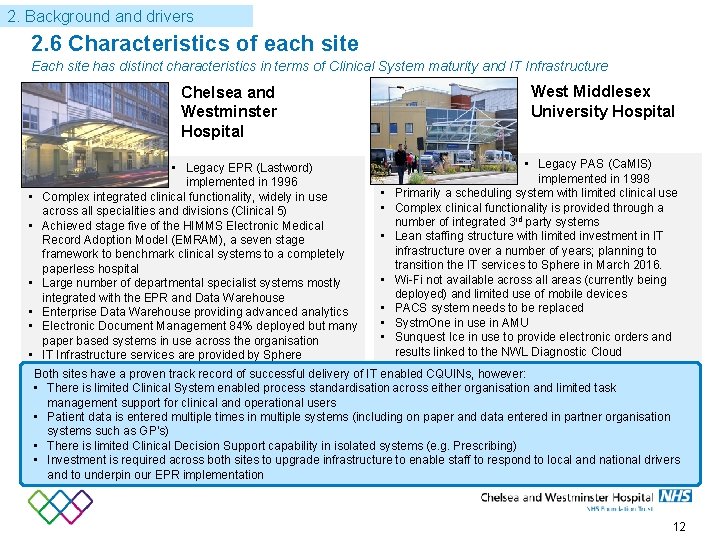
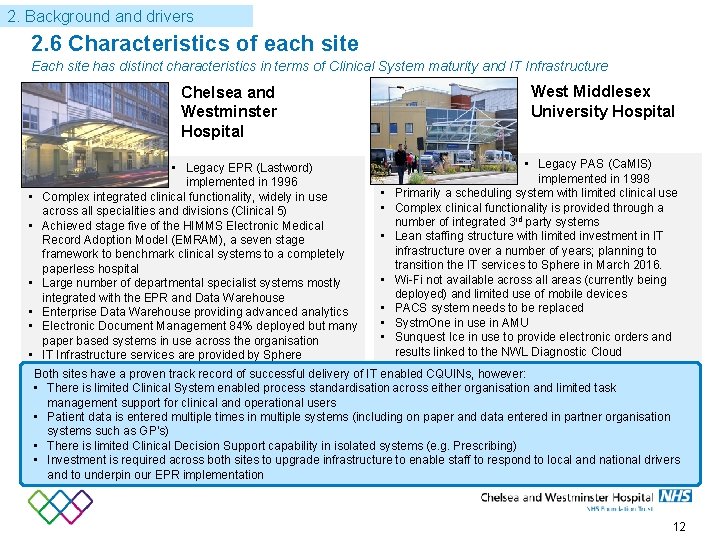
2. Background and drivers 2. 6 Characteristics of each site Each site has distinct characteristics in terms of Clinical System maturity and IT Infrastructure Chelsea and Westminster Hospital West Middlesex University Hospital • Legacy PAS (Ca. MIS) • Legacy EPR (Lastword) implemented in 1998 implemented in 1996 • Primarily a scheduling system with limited clinical use • Complex integrated clinical functionality, widely in use • Complex clinical functionality is provided through a across all specialities and divisions (Clinical 5) number of integrated 3 rd party systems • Achieved stage five of the HIMMS Electronic Medical • Lean staffing structure with limited investment in IT Record Adoption Model (EMRAM), a seven stage infrastructure over a number of years; planning to framework to benchmark clinical systems to a completely transition the IT services to Sphere in March 2016. paperless hospital • Wi-Fi not available across all areas (currently being • Large number of departmental specialist systems mostly deployed) and limited use of mobile devices integrated with the EPR and Data Warehouse • PACS system needs to be replaced • Enterprise Data Warehouse providing advanced analytics • Systm. One in use in AMU • Electronic Document Management 84% deployed but many • Sunquest Ice in use to provide electronic orders and paper based systems in use across the organisation results linked to the NWL Diagnostic Cloud • IT Infrastructure services are provided by Sphere Both sites have a proven track record of successful delivery of IT enabled CQUINs, however: • There is limited Clinical System enabled process standardisation across either organisation and limited task management support for clinical and operational users • Patient data is entered multiple times in multiple systems (including on paper and data entered in partner organisation systems such as GP’s) • There is limited Clinical Decision Support capability in isolated systems (e. g. Prescribing) • Investment is required across both sites to upgrade infrastructure to enable staff to respond to local and national drivers and to underpin our EPR implementation 12
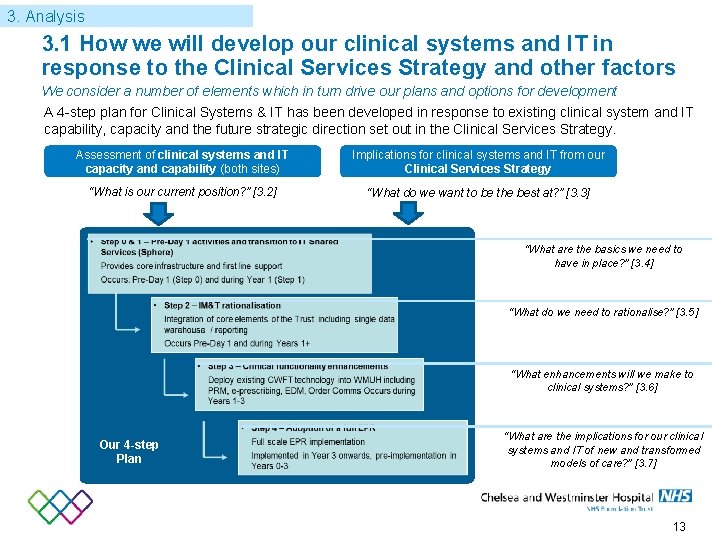
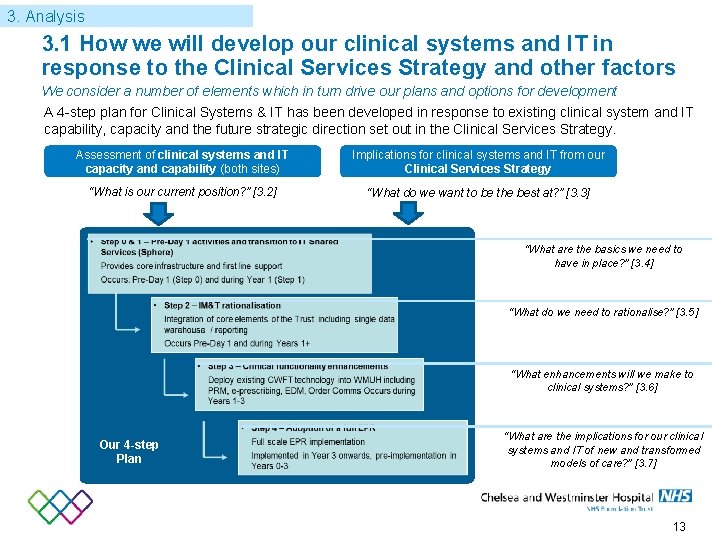
3. Analysis 3. 1 How we will develop our clinical systems and IT in response to the Clinical Services Strategy and other factors We consider a number of elements which in turn drive our plans and options for development A 4 -step plan for Clinical Systems & IT has been developed in response to existing clinical system and IT capability, capacity and the future strategic direction set out in the Clinical Services Strategy. Assessment of clinical systems and IT capacity and capability (both sites) Implications for clinical systems and IT from our Clinical Services Strategy “What is our current position? ” [3. 2] “What do we want to be the best at? ” [3. 3] “What are the basics we need to have in place? ” [3. 4] “What do we need to rationalise? ” [3. 5] “What enhancements will we make to clinical systems? ” [3. 6] Our 4 -step Plan “What are the implications for our clinical systems and IT of new and transformed models of care? ” [3. 7] 13
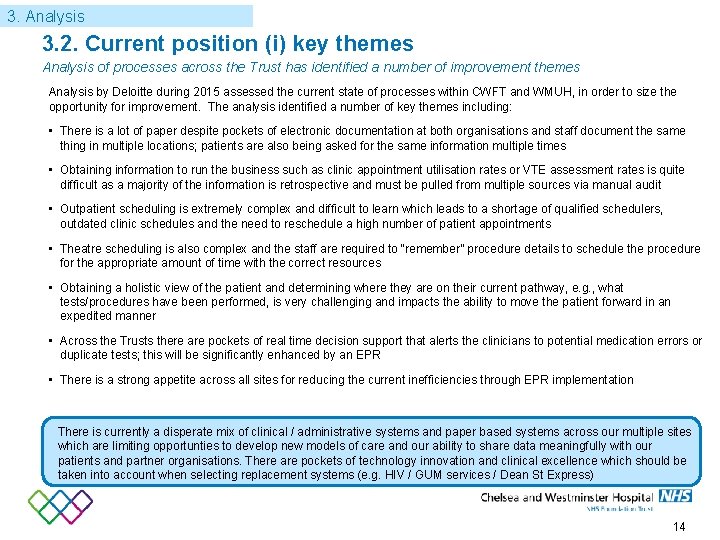
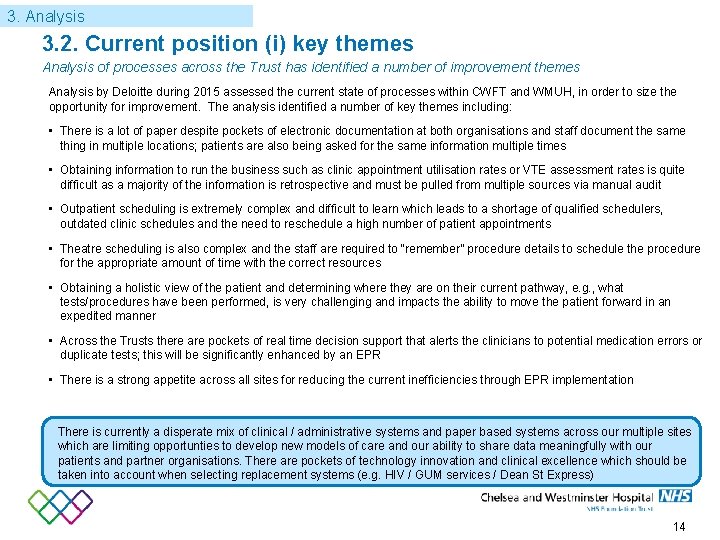
3. Analysis 3. 2. Current position (i) key themes Analysis of processes across the Trust has identified a number of improvement themes Analysis by Deloitte during 2015 assessed the current state of processes within CWFT and WMUH, in order to size the opportunity for improvement. The analysis identified a number of key themes including: • There is a lot of paper despite pockets of electronic documentation at both organisations and staff document the same thing in multiple locations; patients are also being asked for the same information multiple times • Obtaining information to run the business such as clinic appointment utilisation rates or VTE assessment rates is quite difficult as a majority of the information is retrospective and must be pulled from multiple sources via manual audit • Outpatient scheduling is extremely complex and difficult to learn which leads to a shortage of qualified schedulers, outdated clinic schedules and the need to reschedule a high number of patient appointments • Theatre scheduling is also complex and the staff are required to “remember” procedure details to schedule the procedure for the appropriate amount of time with the correct resources • Obtaining a holistic view of the patient and determining where they are on their current pathway, e. g. , what tests/procedures have been performed, is very challenging and impacts the ability to move the patient forward in an expedited manner • Across the Trusts there are pockets of real time decision support that alerts the clinicians to potential medication errors or duplicate tests; this will be significantly enhanced by an EPR • There is a strong appetite across all sites for reducing the current inefficiencies through EPR implementation There is currently a disperate mix of clinical / administrative systems and paper based systems across our multiple sites which are limiting opportunties to develop new models of care and our ability to share data meaningfully with our patients and partner organisations. There are pockets of technology innovation and clinical excellence which should be taken into account when selecting replacement systems (e. g. HIV / GUM services / Dean St Express) 14
3. Analysis 3. 2. Current position (ii) process maturity Benchmarking against a maturity model has identified opportunities to transform business functions to leading practices while implementing an EPR system 15 EPR Functionality Succesful implementation of a highly functional EPR system is a key enabler to developing our process and digital maturity. It is not the first or the final step on the journey. 15
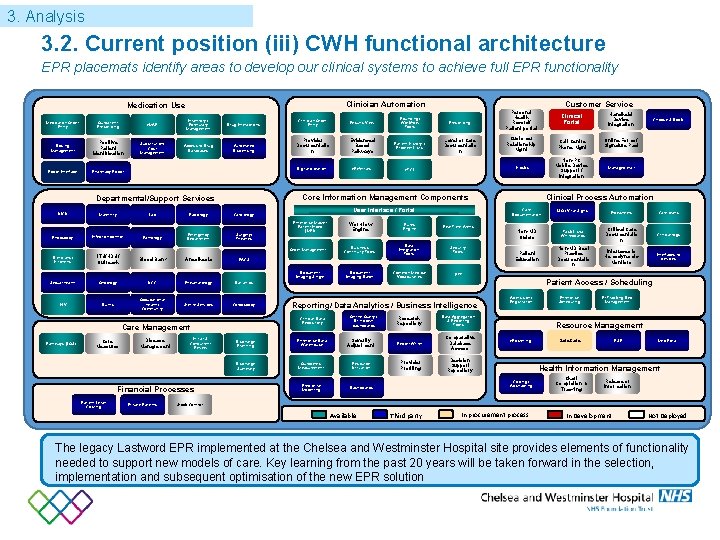
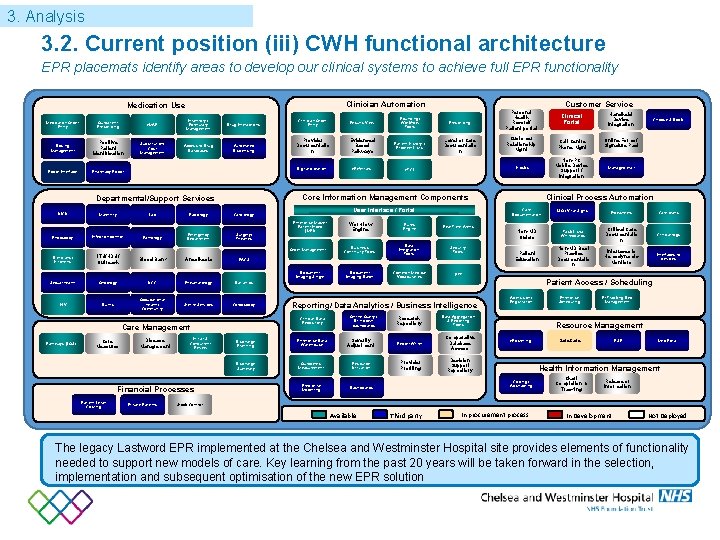
3. Analysis 3. 2. Current position (iii) CWH functional architecture EPR placemats identify areas to develop our clinical systems to achieve full EPR functionality Clinician Automation Medication Use Medication Order Entry Outpatient Prescribing e. MAR Inventory / Formulary Management Drug Interactions Clinician Order Entry Results View Rounding/ Workflow Tools Dosing Management Positive Patient Identification Substitution/ Cost Management Access to Drug Databases Automated Dispensing Provider Documentatio n Evidenced Based Pathways Patient History / Problem Lists Robot Interface Pharmacy Robot e. Referrals e. TCI Digital dictation Endoscopy Maternity Lab Infection control Pathology Radiology Emergency Department Surgery/ Theatres Enterprise Master Patient Index (MPI) Order Management ITU/HDU/ Outreach Blood Bank Anesthesia PACS Sexual health Oncology UCC Rheumatology Bariatrics Document Imaging Single Occupational health/ Community Burns Sterile Services Colposcopy Core Measures Disease Management Initial & Concurrent Review Financial Processes Patient Level Costing Private Patients Workflow Engine Rules Engine Business Continuity Tools Data Integration Tools Security Tools Document Imaging Batch Common Medical Vocabularies RTT Real Time Alerts Handheld Device Integration Customer Relationship Mgnt Call Centre Phone Mgnt Online Forms/ Signature Pad Kiosks Non-PC Mobile Device Support / Integration Managed mail Online Query / Drill down dashboards Research Repository Data Aggregation & Reporting Tools Discharge Planning Enterprise Data Warehouse Severity Adjustment Report Writer Comparative Database Access Discharge Summary Outcomes Measurement Resource Utilization Provider Profiling Decision Support Repository Predictive Modelling Clinical Process Automation Care Documentation I&O / Vital Signs Flowsheets Care plans Non-MD Orders Task Lists/ Whiteboards Critical Care Documentatio n Clinical logs Patient Education Non-MD Best Practice Documentatio n Interfaces to Hemodynamic Monitors Interfaces to devices Admission/ Registration Enterprise Scheduling Pt Tracking Bed Management Resource Management e. Rostering Safe. Care ESR Medi. Rota Health Information Management Coding / Abstracting Dashboards Choose & Book Patient Access / Scheduling Reporting/ Data Analytics / Business Intelligence Clinical Data Repository Care Management Pathways (LOS) Level of Care Documentatio n User Interface / Portal Cardiology Dieticians/ Kitchens HIV Prescribing Clinical Portal Core Information Management Components Departmental/Support Services NICU Customer Service Personal Health Record/ Patient portal Chart Completion & Tracking Release of Information 16 Stock Control Available Third party In procurement process In Development Not Deployed The legacy Lastword EPR implemented at the Chelsea and Westminster Hospital site provides elements of functionality needed to support new models of care. Key learning from the past 20 years will be taken forward in the selection, implementation and subsequent optimisation of the new EPR solution
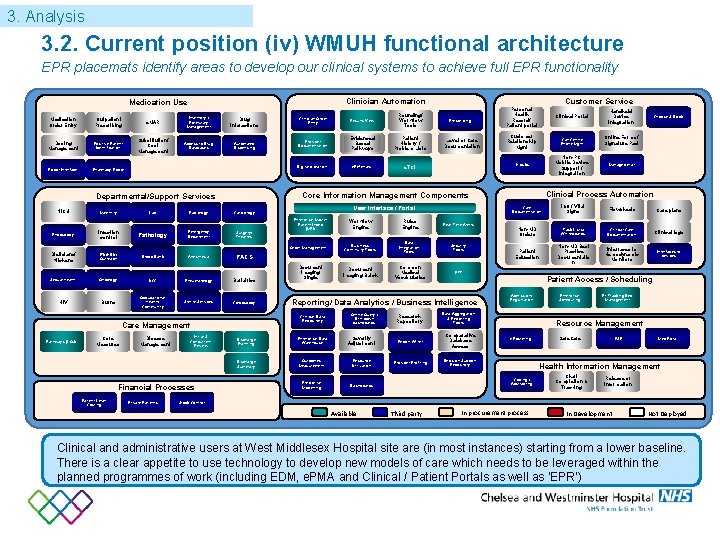
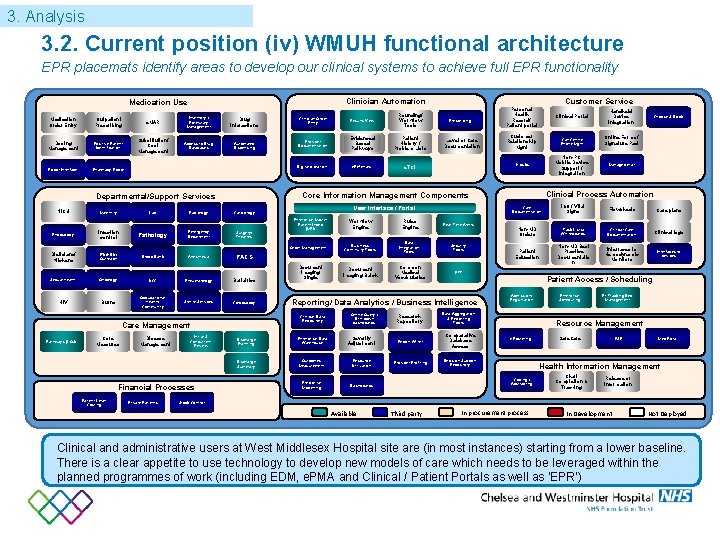
3. Analysis 3. 2. Current position (iv) WMUH functional architecture EPR placemats identify areas to develop our clinical systems to achieve full EPR functionality Clinician Automation Medication Use Medication Order Entry Outpatient Prescribing e. MAR Inventory / Formulary Management Dosing Management Positive Patient Identification Substitution/ Cost Management Access to Drug Databases Robot Interface Pharmacy Robot Drug Interactions Automated Dispensing Endoscopy Maternity Lab Infection control Pathology Radiology Emergency Department Results View Rounding/ Workflow Tools Provider Documentation Evidenced Based Pathways Patient History / Problem Lists Digital dictation e. Referrals e. TCI Surgery/ Theatres Enterprise Master Patient Index (MPI) Order Management ITU/HDU/ Outreach Blood Bank Anesthesia PACS Sexual health Oncology UCC Rheumatology Bariatrics HIV Burns Occupational health/ Community Sterile Services Colposcopy Core Measures Disease Management Financial Processes Patient Level Costing Private Patients Document Imaging Single Level of Care Documentation Workflow Engine Rules Engine Real Time Alerts Business Continuity Tools Data Integration Tools Security Tools Document Imaging Batch Common Medical Vocabularies RTT Clinical Portal Handheld Device Integration Customer Relationship Mgnt Call Centre Phone Mgnt Online Forms/ Signature Pad Kiosks Non-PC Mobile Device Support / Integration Managed mail Online Query / Drill down dashboards Research Repository Data Aggregation & Reporting Tools Discharge Planning Enterprise Data Warehouse Severity Adjustment Report Writer Comparative Database Access Discharge Summary Outcomes Measurement Resource Utilization Provider Profiling Decision Support Repository Predictive Modelling Clinical Process Automation Care Documentation I&O / Vital Signs Flowsheets Care plans Non-MD Orders Task Lists/ Whiteboards Critical Care Documentation Clinical logs Patient Education Non-MD Best Practice Documentatio n Interfaces to Hemodynamic Monitors Interfaces to devices Admission/ Registration Enterprise Scheduling Pt Tracking Bed Management Resource Management e. Rostering Safe. Care ESR Medi. Rota Health Information Management Coding / Abstracting Dashboards Choose & Book Patient Access / Scheduling Reporting/ Data Analytics / Business Intelligence Clinical Data Repository Care Management Pathways (LOS) Prescribing User Interface / Portal Cardiology Dieticians/ Kitchens Initial & Concurrent Review Customer Service Personal Health Record/ Patient portal Core Information Management Components Departmental/Support Services NICU Clinician Order Entry Chart Completion & Tracking Release of Information Stock Control Available Third party In procurement process In Development Not Deployed Clinical and administrative users at West Middlesex Hospital site are (in most instances) starting from a lower baseline. There is a clear appetite to use technology to develop new models of care which needs to be leveraged within the planned programmes of work (including EDM, e. PMA and Clinical / Patient Portals as well as ‘EPR’)
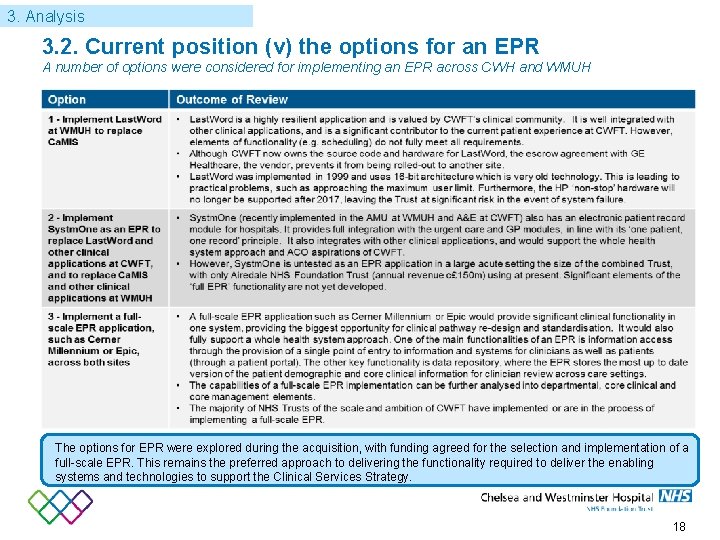
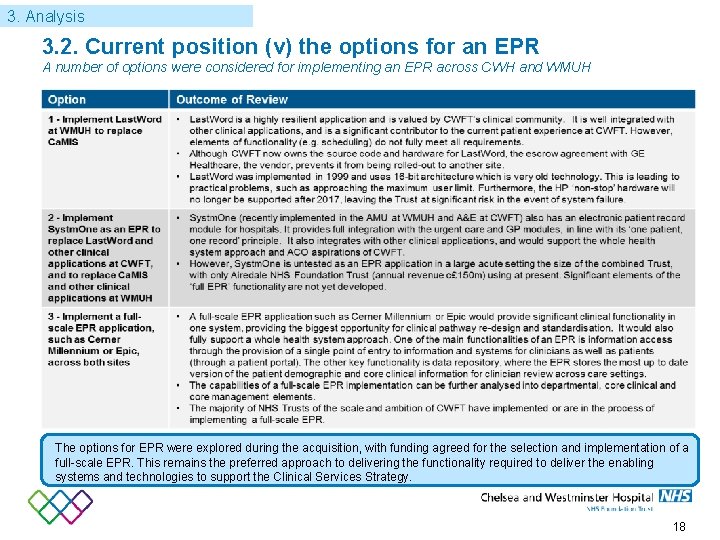
3. Analysis 3. 2. Current position (v) the options for an EPR A number of options were considered for implementing an EPR across CWH and WMUH The options for EPR were explored during the acquisition, with funding agreed for the selection and implementation of a full-scale EPR. This remains the preferred approach to delivering the functionality required to deliver the enabling systems and technologies to support the Clinical Services Strategy. 18
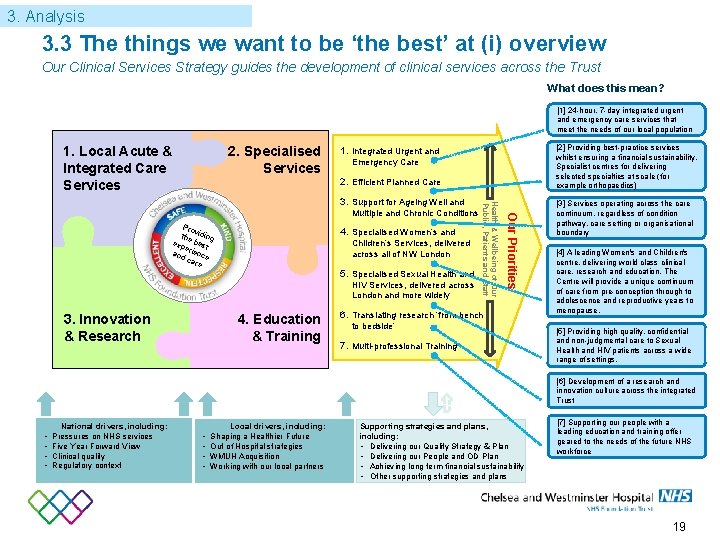
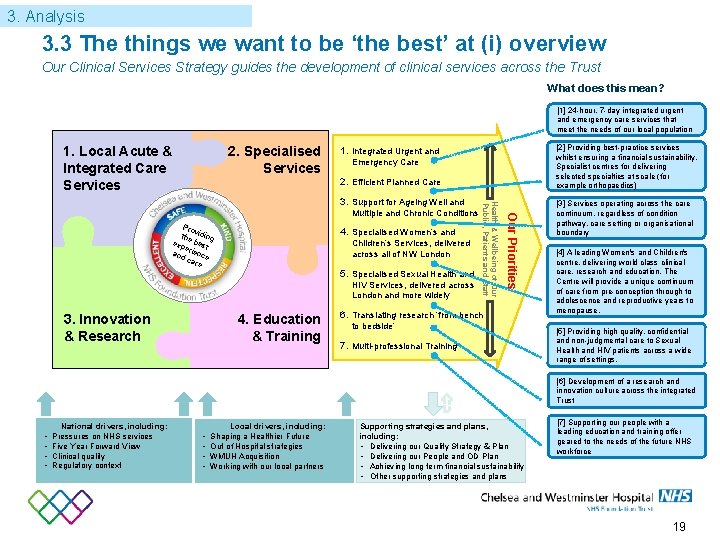
3. Analysis 3. 3 The things we want to be ‘the best’ at (i) overview Our Clinical Services Strategy guides the development of clinical services across the Trust What does this mean? [1] 24 -hour, 7 -day integrated urgent and emergency care services that meet the needs of our local population 1. Local Acute & Integrated Care Services 2. Specialised Services [2] Providing best-practice services whilst ensuring a financial sustainability. Specialist centres for delivering selected specialties at scale (for example orthopaedics) 1. Integrated Urgent and Emergency Care 2. Efficient Planned Care Pro v the iding exp best e and rience ca re 4. Specialised Women’s and Children’s Services, delivered across all of NW London 5. Specialised Sexual Health and HIV Services, delivered across London and more widely 3. Innovation & Research 4. Education & Training Our Priorities Multiple and Chronic Conditions Health & Wellbeing of Our Public, Patients and Staff 3. Support for Ageing Well and 6. Translating research ‘from bench to bedside’ 7. Multi-professional Training [3] Services operating across the care continuum, regardless of condition pathway, care setting or organisational boundary [4] A leading Women's and Children's centre, delivering world class clinical care, research and education. The Centre will provide a unique continuum of care from pre-conception through to adolescence and reproductive years to menopause. [5] Providing high quality, confidential and non-judgmental care to Sexual Health and HIV patients across a wide range of settings. [6] Development of a research and innovation culture across the integrated Trust • • National drivers, including: Pressures on NHS services Five Year Forward View Clinical quality Regulatory context • • Local drivers, including: Shaping a Healthier Future Out of Hospital strategies WMUH Acquisition Working with our local partners Supporting strategies and plans, including: • Delivering our Quality Strategy & Plan • Delivering our People and OD Plan • Achieving long term financial sustainability • Other supporting strategies and plans [7] Supporting our people with a leading education and training offer geared to the needs of the future NHS workforce 19

3. Analysis 3. 3 The things we want to be ‘the best’ at (ii) implications Delivering the Clinical Services Strategy will have significant implications for our clinical systems and IT Clinical Services Strategy priority / ambition Implications for the development of our clinical systems and IT 1. 24 -hour, 7 -day integrated urgent and emergency care services that meet the needs of our local population • Technology and systems innovation that supports real time monitoring of vital observations and early identification of deteriorating patients • Effective rostering of clinical and admin staff embedded within the core system, responsive to patient acuity and demand 2. Providing best-practice planned care services whilst ensuring a financial sustainability. • Supporting best practice planned care through best in class processes for booking, theatre and outpatient scheduling, diagnostics, discharge. (i. e. ; enterprise wide scheduling) • Enable patient participation in scheduling their planned care • Flexibility and agility of clinical systems to adapt to new models of outpatient care and diagnostics Specialist centres for delivering selected specialties at scale (for example orthopaedics) Shared across multiple priorities • Putting in place an EPR system that supports our vision for the best care and experience through enabling improvements in quality, safety and efficiency of care 3. Services operating across the care continuum, regardless of condition pathway, care setting or organisational boundary • Clinical system linkage to enable standardisation and access to a single care record accessible by GPs and care homes • Electronic medical record accessible by all partners • Sharing of information across health and social care partners 4. A leading Women's and Children's centre, delivering world class clinical care, research and education. The Centre will provide a unique continuum of care from pre-conception through to adolescence and reproductive years to menopause. • Supporting best practice women’s and children’s services through best in class processes for care management • Innovative access to care providers by patients using secure apps / patient portal / emerging technologies • State of the art technology and systems to support specialist care for children 5. Providing high quality, confidential and nonjudgmental care to Sexual Health and HIV patients across a wide range of settings. • Developing our innovative use of technology and clinical systems to enable our award winning patient centred ‘Express Model’ model for sexual health testing, as well as deploying this model to all our sexual health clinics 6. Development of a research and innovation culture across the integrated Trust • Developing a research portal that will support and manage all data and expand opportunities for patients to directly contribute to research 7. Supporting our people with a leading education and training offer geared to the needs of the future NHS workforce • Having an electronic staff record which enables our education and training capabilities, including interfacing to professional registration bodies, e-Learning functionality, compliance tools that enable tracking of statutory and mandatory training requirements, appraisals, absence management and self service 20

3. Analysis 3. 3 The things we want to be ‘the best’ at (ii) implications Delivering the Clinical Services Strategy will have significant implications for our clinical systems and IT Clinical Services Strategy priority / ambition Implications for the development of our clinical systems and IT 1. 24 -hour, 7 -day integrated urgent and emergency care services that meet the needs of our local population • Technology and systems innovation that supports real time monitoring of vital observations and early identification of deteriorating patients 2. Providing best-practice planned care services whilst ensuring a financial sustainability. • Supporting best practice planned care through best in class processes for booking, theatre and outpatient scheduling, diagnostics, discharge • Flexibility and agility of clinical systems to adapt to new models of outpatient care and diagnostics Specialist centres for delivering selected specialties at scale (for example orthopaedics) Shared across multiple priorities • Putting in place an EPR system that supports our vision for the best care and experience through enabling improvements in quality, safety and efficiency of care 3. Services operating across the care continuum, regardless of condition pathway, care setting or organisational boundary • IT/information system linkage to enable standardisation and access to a single care record accessible by GPs and care homes • EPR accessible by all partners • Sharing of information across health and social care partners 4. A leading Women's and Children's centre, delivering world class clinical care, research and education. The Centre will provide a unique continuum of care from pre-conception through to adolescence and reproductive years to menopause. • Supporting best practice women’s and children’s services through best in class processes for booking, care management, diagnostics, discharge • State of the art technology and systems to support specialist care for children 5. Providing high quality, confidential and nonjudgmental care to Sexual Health and HIV patients across a wide range of settings. • Developing our innovative use of technology and clinical systems to enable our award winning patient centred ‘Express Model’ model for sexual health testing, as well as deploying this model to all our sexual health clinics 6. Development of a research and innovation culture across the integrated Trust • Developing a research portal that will support and manage all data and expand opportunities for patients to directly contribute to research 7. Supporting our people with a leading education and training offer geared to the needs of the future NHS workforce • Having an electronic staff record which enables our education and training capabilities, including interfacing to professional registration bodies, e-Learning functionality, compliance tools that enable tracking of statutory and mandatory training requirements, appraisals, absence management and self service • Standardised, decision support, task management and auditable workflow will support and enforce education and training 21
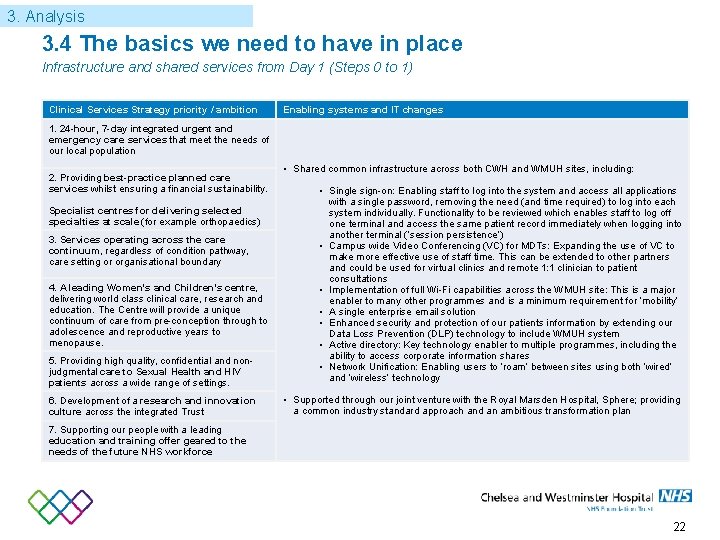
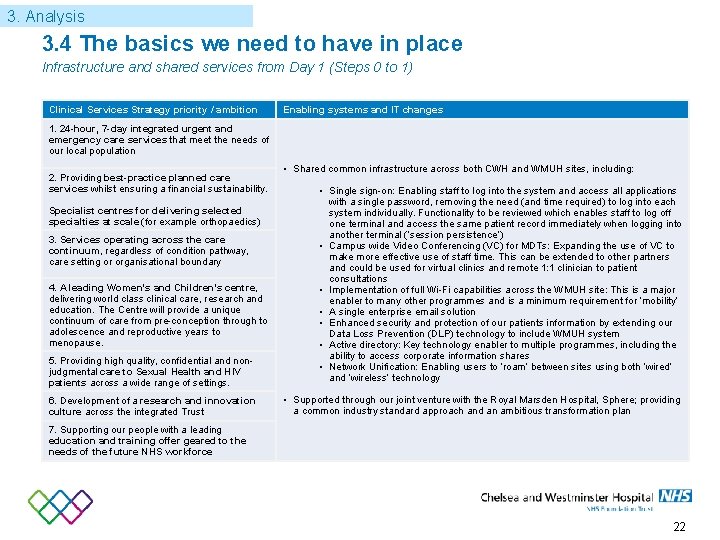
3. Analysis 3. 4 The basics we need to have in place Infrastructure and shared services from Day 1 (Steps 0 to 1) Clinical Services Strategy priority / ambition Enabling systems and IT changes 1. 24 -hour, 7 -day integrated urgent and emergency care services that meet the needs of our local population 2. Providing best-practice planned care services whilst ensuring a financial sustainability. • Shared common infrastructure across both CWH and WMUH sites, including: 5. Providing high quality, confidential and nonjudgmental care to Sexual Health and HIV patients across a wide range of settings. • Single sign-on: Enabling staff to log into the system and access all applications with a single password, removing the need (and time required) to log into each system individually. Functionality to be reviewed which enables staff to log off one terminal and access the same patient record immediately when logging into another terminal (‘session persistence’) • Campus wide Video Conferencing (VC) for MDTs: Expanding the use of VC to make more effective use of staff time. This can be extended to other partners and could be used for virtual clinics and remote 1: 1 clinician to patient consultations • Implementation of full Wi-Fi capabilities across the WMUH site: This is a major enabler to many other programmes and is a minimum requirement for ‘mobility’ • A single enterprise email solution • Enhanced security and protection of our patients information by extending our Data Loss Prevention (DLP) technology to include WMUH system • Active directory: Key technology enabler to multiple programmes, including the ability to access corporate information shares • Network Unification: Enabling users to ‘roam’ between sites using both ‘wired’ and ‘wireless’ technology 6. Development of a research and innovation culture across the integrated Trust • Supported through our joint venture with the Royal Marsden Hospital, Sphere; providing a common industry standard approach and an ambitious transformation plan Specialist centres for delivering selected specialties at scale (for example orthopaedics) 3. Services operating across the care continuum, regardless of condition pathway, care setting or organisational boundary 4. A leading Women's and Children's centre, delivering world class clinical care, research and education. The Centre will provide a unique continuum of care from pre-conception through to adolescence and reproductive years to menopause. 7. Supporting our people with a leading education and training offer geared to the needs of the future NHS workforce 22
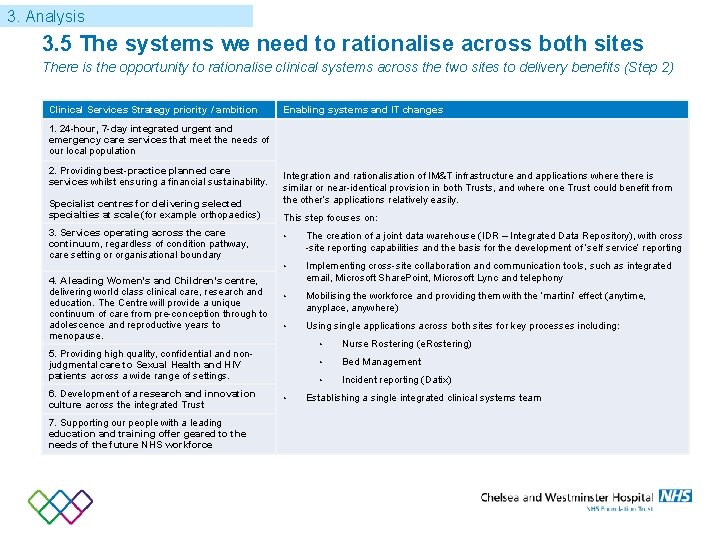
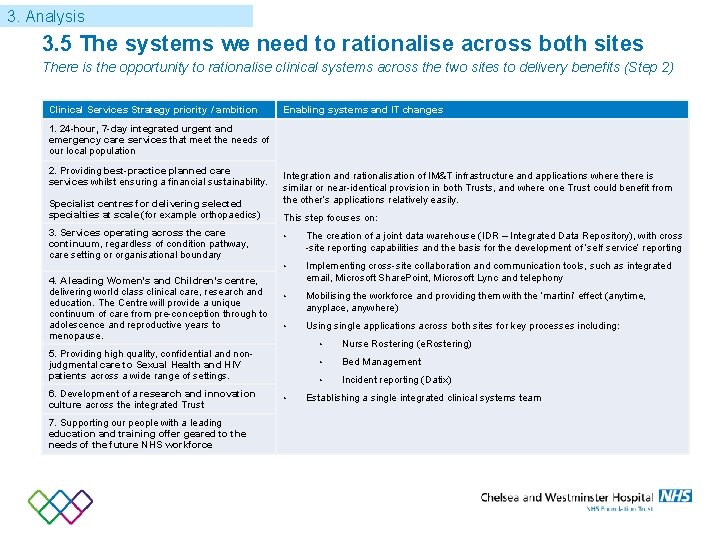
3. Analysis 3. 5 The systems we need to rationalise across both sites There is the opportunity to rationalise clinical systems across the two sites to delivery benefits (Step 2) Clinical Services Strategy priority / ambition Enabling systems and IT changes 1. 24 -hour, 7 -day integrated urgent and emergency care services that meet the needs of our local population 2. Providing best-practice planned care services whilst ensuring a financial sustainability. Specialist centres for delivering selected specialties at scale (for example orthopaedics) 3. Services operating across the care continuum, regardless of condition pathway, care setting or organisational boundary 4. A leading Women's and Children's centre, delivering world class clinical care, research and education. The Centre will provide a unique continuum of care from pre-conception through to adolescence and reproductive years to menopause. Integration and rationalisation of IM&T infrastructure and applications where there is similar or near-identical provision in both Trusts, and where one Trust could benefit from the other’s applications relatively easily. This step focuses on: • The creation of a joint data warehouse (IDR – Integrated Data Repository), with cross -site reporting capabilities and the basis for the development of ‘self service’ reporting • Implementing cross-site collaboration and communication tools, such as integrated email, Microsoft Share. Point, Microsoft Lync and telephony • Mobilising the workforce and providing them with the ‘martini’ effect (anytime, anyplace, anywhere) • Usingle applications across both sites for key processes including: 5. Providing high quality, confidential and nonjudgmental care to Sexual Health and HIV patients across a wide range of settings. 6. Development of a research and innovation culture across the integrated Trust 7. Supporting our people with a leading education and training offer geared to the needs of the future NHS workforce • • Nurse Rostering (e. Rostering) • Bed Management • Incident reporting (Datix) Establishing a single integrated clinical systems team
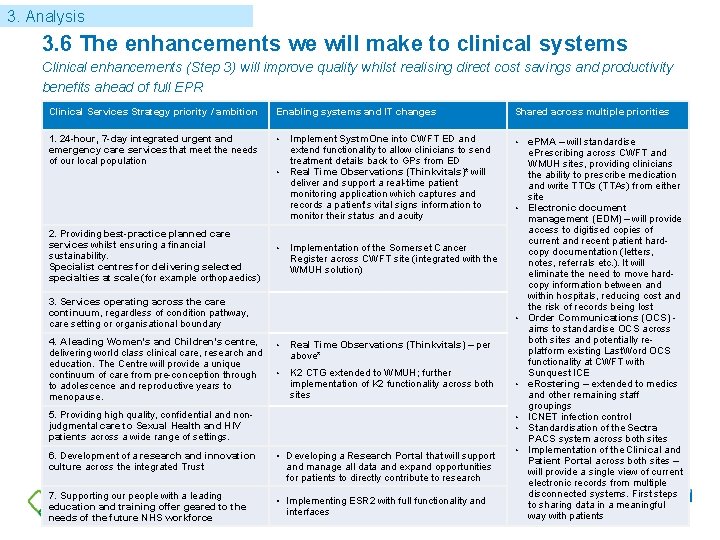
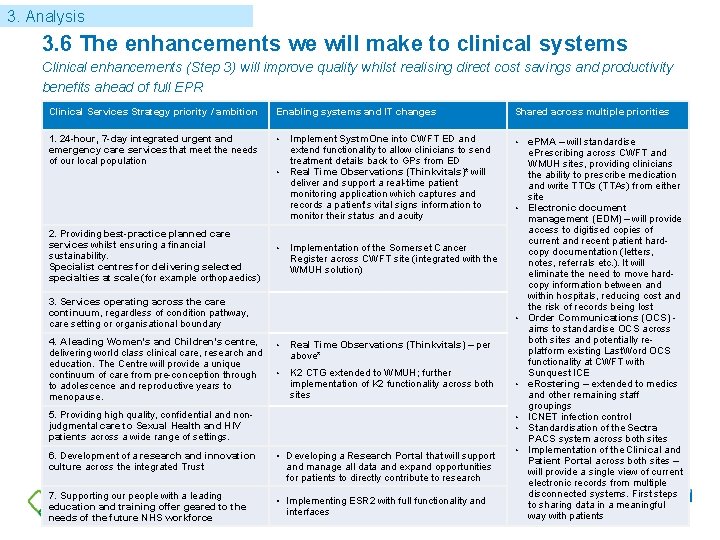
3. Analysis 3. 6 The enhancements we will make to clinical systems Clinical enhancements (Step 3) will improve quality whilst realising direct cost savings and productivity benefits ahead of full EPR Clinical Services Strategy priority / ambition Enabling systems and IT changes 1. 24 -hour, 7 -day integrated urgent and emergency care services that meet the needs of our local population • • 2. Providing best-practice planned care services whilst ensuring a financial sustainability. Specialist centres for delivering selected specialties at scale (for example orthopaedics) • Implement Systm. One into CWFT ED and extend functionality to allow clinicians to send treatment details back to GPs from ED Real Time Observations (Thinkvitals)* will deliver and support a real-time patient monitoring application which captures and records a patient’s vital signs information to monitor their status and acuity 7. Supporting our people with a leading education and training offer geared to the needs of the future NHS workforce • • • Real Time Observations (Thinkvitals) – per above* • K 2 CTG extended to WMUH; further implementation of K 2 functionality across both sites 5. Providing high quality, confidential and nonjudgmental care to Sexual Health and HIV patients across a wide range of settings. 6. Development of a research and innovation culture across the integrated Trust • Implementation of the Somerset Cancer Register across CWFT site (integrated with the WMUH solution) 3. Services operating across the care continuum, regardless of condition pathway, care setting or organisational boundary 4. A leading Women's and Children's centre, delivering world class clinical care, research and education. The Centre will provide a unique continuum of care from pre-conception through to adolescence and reproductive years to menopause. Shared across multiple priorities • • Developing a Research Portal that will support and manage all data and expand opportunities for patients to directly contribute to research • Implementing ESR 2 with full functionality and interfaces • e. PMA – will standardise e. Prescribing across CWFT and WMUH sites, providing clinicians the ability to prescribe medication and write TTOs (TTAs) from either site Electronic document management (EDM) – will provide access to digitised copies of current and recent patient hardcopy documentation (letters, notes, referrals etc. ). It will eliminate the need to move hardcopy information between and within hospitals, reducing cost and the risk of records being lost Order Communications (OCS) - aims to standardise OCS across both sites and potentially replatform existing Last. Word OCS functionality at CWFT with Sunquest ICE e. Rostering – extended to medics and other remaining staff groupings ICNET infection control Standardisation of the Sectra PACS system across both sites Implementation of the Clinical and Patient Portal across both sites – will provide a single view of current electronic records from multiple disconnected systems. First steps to sharing data in a meaningful way with patients
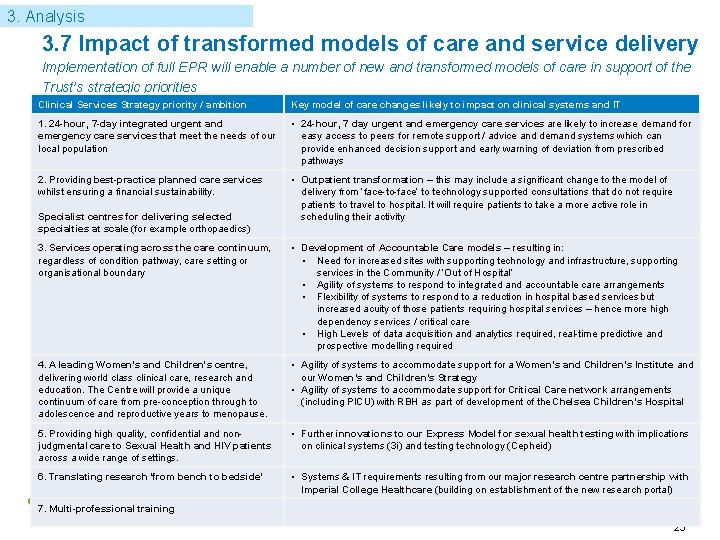
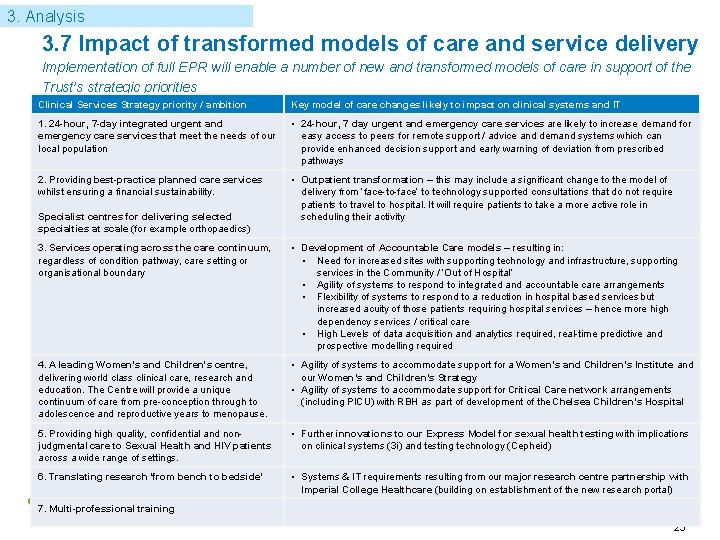
3. Analysis 3. 7 Impact of transformed models of care and service delivery Implementation of full EPR will enable a number of new and transformed models of care in support of the Trust’s strategic priorities Clinical Services Strategy priority / ambition Key model of care changes likely to impact on clinical systems and IT 1. 24 -hour, 7 -day integrated urgent and emergency care services that meet the needs of our local population • 24 -hour, 7 day urgent and emergency care services are likely to increase demand for easy access to peers for remote support / advice and demand systems which can provide enhanced decision support and early warning of deviation from prescribed pathways 2. Providing best-practice planned care services whilst ensuring a financial sustainability. • Outpatient transformation – this may include a significant change to the model of delivery from ‘face-to-face’ to technology supported consultations that do not require patients to travel to hospital. It will require patients to take a more active role in scheduling their activity Specialist centres for delivering selected specialties at scale (for example orthopaedics) 3. Services operating across the care continuum, regardless of condition pathway, care setting or organisational boundary • Development of Accountable Care models – resulting in: • Need for increased sites with supporting technology and infrastructure, supporting services in the Community / ‘Out of Hospital’ • Agility of systems to respond to integrated and accountable care arrangements • Flexibility of systems to respond to a reduction in hospital based services but increased acuity of those patients requiring hospital services – hence more high dependency services / critical care • High Levels of data acquisition and analytics required, real-time predictive and prospective modelling required 4. A leading Women's and Children's centre, delivering world class clinical care, research and education. The Centre will provide a unique continuum of care from pre-conception through to adolescence and reproductive years to menopause. • Agility of systems to accommodate support for a Women’s and Children’s Institute and our Women’s and Children’s Strategy • Agility of systems to accommodate support for Critical Care network arrangements (including PICU) with RBH as part of development of the Chelsea Children’s Hospital 5. Providing high quality, confidential and nonjudgmental care to Sexual Health and HIV patients across a wide range of settings. • Further innovations to our Express Model for sexual health testing with implications on clinical systems (3 i) and testing technology (Cepheid) 6. Translating research ‘from bench to bedside’ • Systems & IT requirements resulting from our major research centre partnership with Imperial College Healthcare (building on establishment of the new research portal) 7. Multi-professional training 25
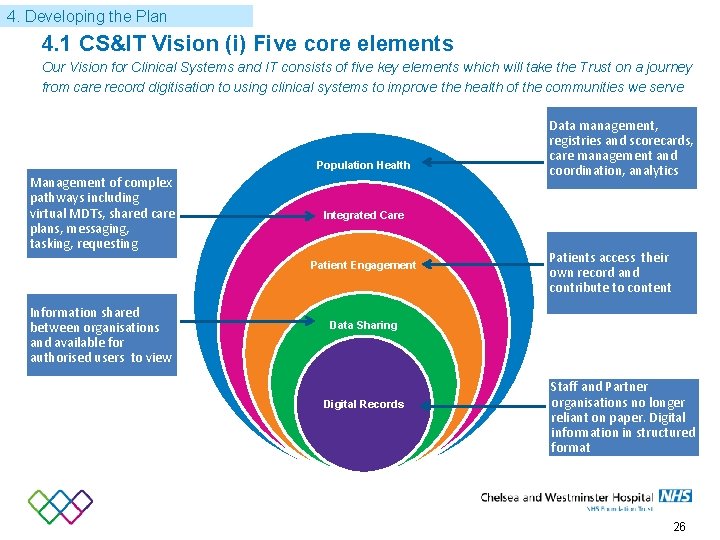
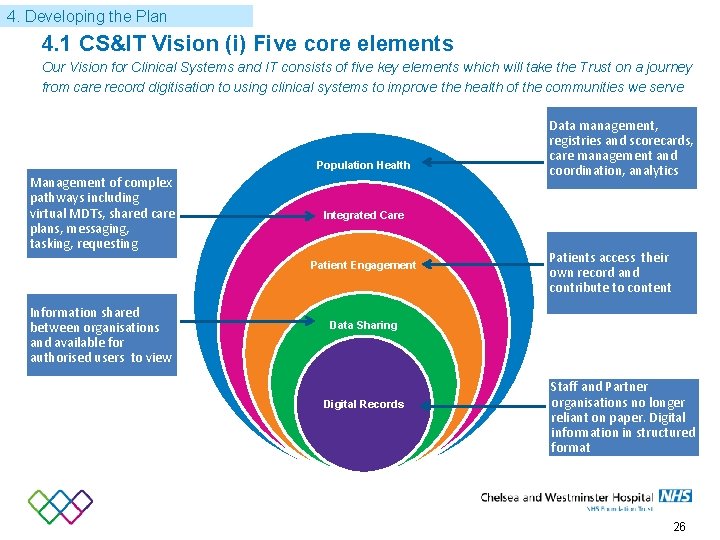
4. Developing the Plan 4. 1 CS&IT Vision (i) Five core elements Our Vision for Clinical Systems and IT consists of five key elements which will take the Trust on a journey from care record digitisation to using clinical systems to improve the health of the communities we serve Population Health Management of complex pathways including virtual MDTs, shared care plans, messaging, tasking, requesting Integrated Care Patient Engagement Information shared between organisations and available for authorised users to view Data management, registries and scorecards, care management and coordination, analytics Patients access their own record and contribute to content Data Sharing Digital Records Staff and Partner organisations no longer reliant on paper. Digital information in structured format 26
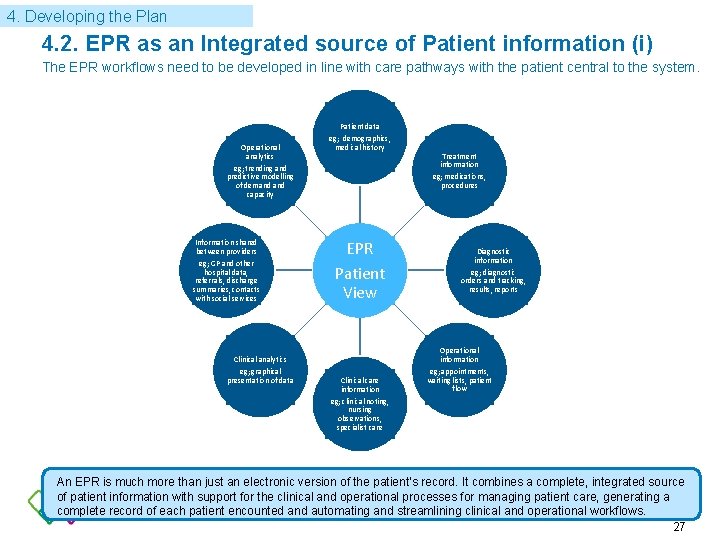
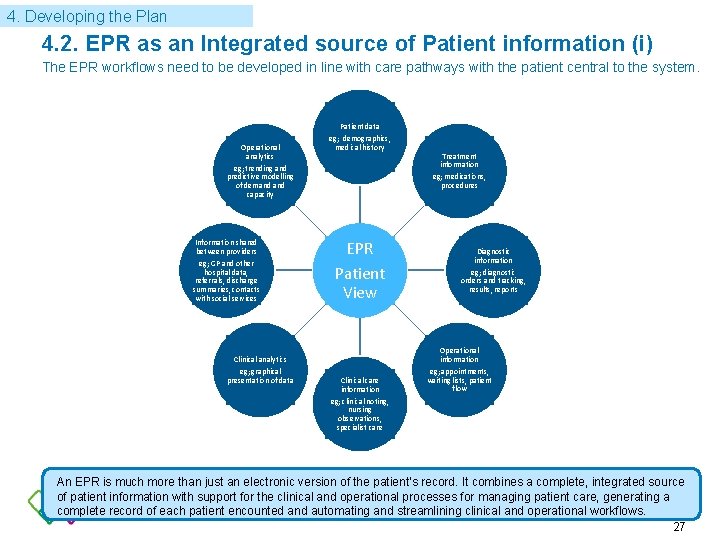
3. Analysis 4. Developing the Plan 4. 2. EPR as an Integrated source of Patient information (i) The EPR workflows need to be developed in line with care pathways with the patient central to the system. Operational analytics eg; trending and predictive modelling of demand capacity Information shared between providers eg; GP and other hospital data, referrals, discharge summaries, contacts with social services Clinical analytics eg; graphical presentation of data Patient data eg; demographics, medical history Treatment information eg; medications, procedures EPR Patient View Clinical care information eg; clinical noting, nursing observations, specialist care Diagnostic information eg; diagnostic orders and tracking, results, reports Operational information eg; appointments, waiting lists, patient flow An EPR is much more than just an electronic version of the patient‘s record. It combines a complete, integrated source of patient information with support for the clinical and operational processes for managing patient care, generating a complete record of each patient encounted and automating and streamlining clinical and operational workflows. 27
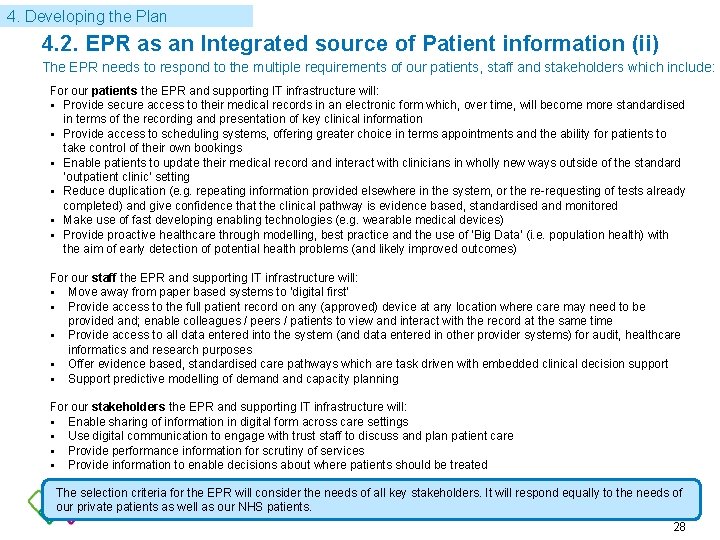
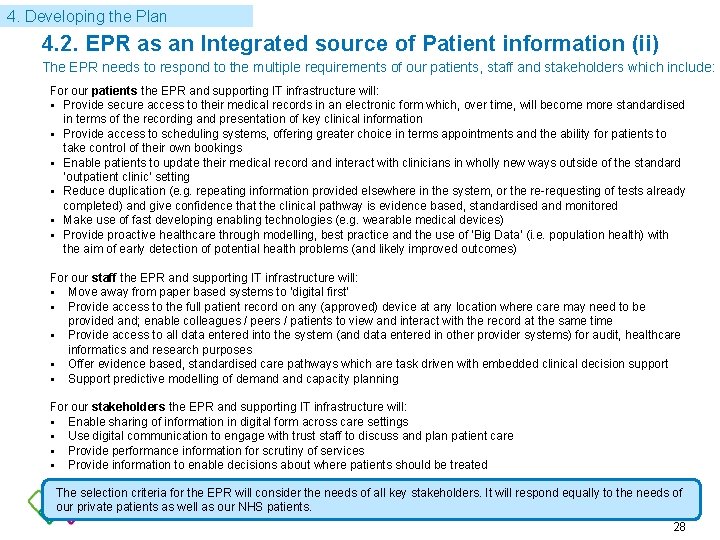
3. Analysis 4. Developing the Plan 4. 2. EPR as an Integrated source of Patient information (ii) The EPR needs to respond to the multiple requirements of our patients, staff and stakeholders which include: For our patients the EPR and supporting IT infrastructure will: Provide secure access to their medical records in an electronic form which, over time, will become more standardised in terms of the recording and presentation of key clinical information Provide access to scheduling systems, offering greater choice in terms appointments and the ability for patients to take control of their own bookings Enable patients to update their medical record and interact with clinicians in wholly new ways outside of the standard ‘outpatient clinic’ setting Reduce duplication (e. g. repeating information provided elsewhere in the system, or the re-requesting of tests already completed) and give confidence that the clinical pathway is evidence based, standardised and monitored Make use of fast developing enabling technologies (e. g. wearable medical devices) Provide proactive healthcare through modelling, best practice and the use of ‘Big Data’ (i. e. population health) with the aim of early detection of potential health problems (and likely improved outcomes) For our staff the EPR and supporting IT infrastructure will: Move away from paper based systems to ‘digital first’ Provide access to the full patient record on any (approved) device at any location where care may need to be provided and; enable colleagues / peers / patients to view and interact with the record at the same time Provide access to all data entered into the system (and data entered in other provider systems) for audit, healthcare informatics and research purposes Offer evidence based, standardised care pathways which are task driven with embedded clinical decision support Support predictive modelling of demand capacity planning For our stakeholders the EPR and supporting IT infrastructure will: Enable sharing of information in digital form across care settings Use digital communication to engage with trust staff to discuss and plan patient care Provide performance information for scrutiny of services Provide information to enable decisions about where patients should be treated The selection criteria for the EPR will consider the needs of all key stakeholders. It will respond equally to the needs of our private patients as well as our NHS patients. 28
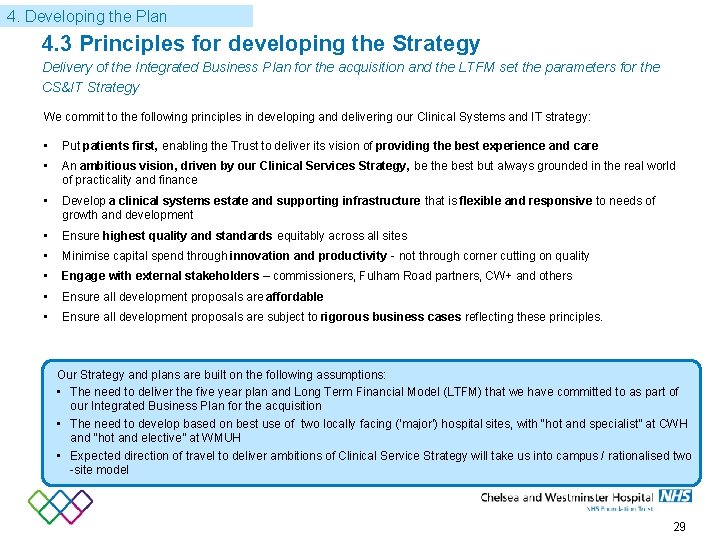
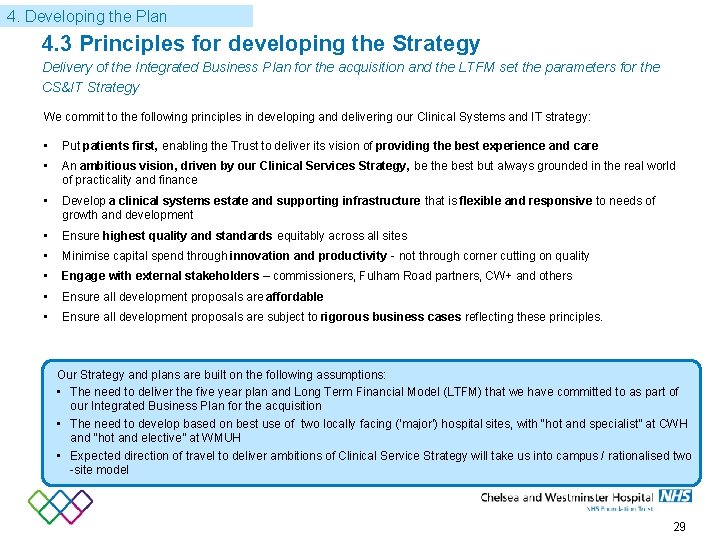
4. Developing the Plan 4. 3 Principles for developing the Strategy Delivery of the Integrated Business Plan for the acquisition and the LTFM set the parameters for the CS&IT Strategy We commit to the following principles in developing and delivering our Clinical Systems and IT strategy: • Put patients first, enabling the Trust to deliver its vision of providing the best experience and care • An ambitious vision, driven by our Clinical Services Strategy, be the best but always grounded in the real world of practicality and finance • Develop a clinical systems estate and supporting infrastructure that is flexible and responsive to needs of growth and development • Ensure highest quality and standards equitably across all sites • Minimise capital spend through innovation and productivity - not through corner cutting on quality • Engage with external stakeholders – commissioners, Fulham Road partners, CW+ and others • Ensure all development proposals are affordable • Ensure all development proposals are subject to rigorous business cases reflecting these principles. Our Strategy and plans are built on the following assumptions: • The need to deliver the five year plan and Long Term Financial Model (LTFM) that we have committed to as part of our Integrated Business Plan for the acquisition • The need to develop based on best use of two locally facing (‘major’) hospital sites, with “hot and specialist” at CWH and “hot and elective” at WMUH • Expected direction of travel to deliver ambitions of Clinical Service Strategy will take us into campus / rationalised two -site model 29
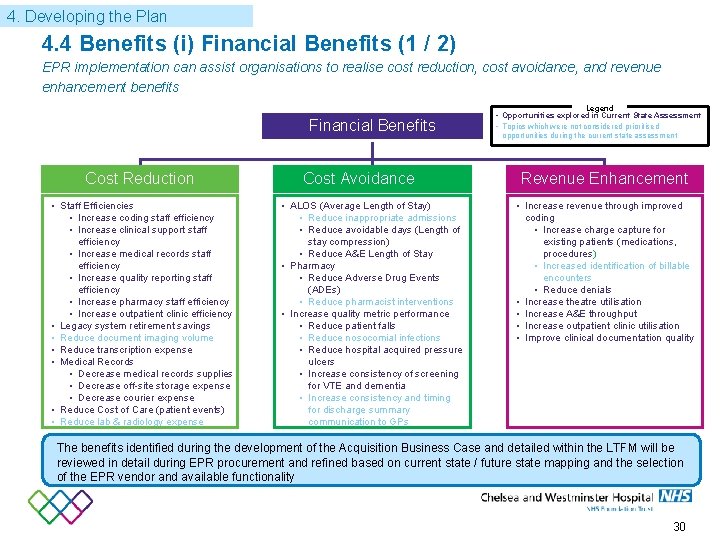
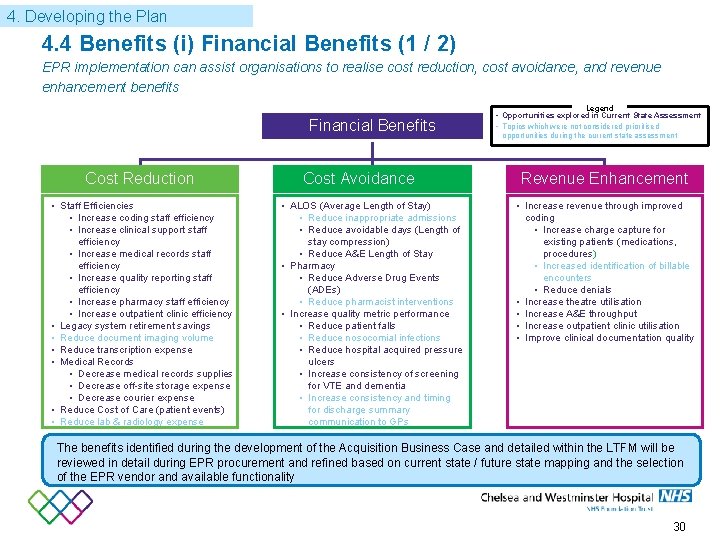
4. Developing the Plan 4. 4 Benefits (i) Financial Benefits (1 / 2) EPR implementation can assist organisations to realise cost reduction, cost avoidance, and revenue enhancement benefits Legend Financial Benefits Cost Reduction • Staff Efficiencies • Increase coding staff efficiency • Increase clinical support staff efficiency • Increase medical records staff efficiency • Increase quality reporting staff efficiency • Increase pharmacy staff efficiency • Increase outpatient clinic efficiency • Legacy system retirement savings • Reduce document imaging volume • Reduce transcription expense • Medical Records • Decrease medical records supplies • Decrease off-site storage expense • Decrease courier expense • Reduce Cost of Care (patient events) • Reduce lab & radiology expense Cost Avoidance • ALOS (Average Length of Stay) • Reduce inappropriate admissions • Reduce avoidable days (Length of stay compression) • Reduce A&E Length of Stay • Pharmacy • Reduce Adverse Drug Events (ADEs) • Reduce pharmacist interventions • Increase quality metric performance • Reduce patient falls • Reduce nosocomial infections • Reduce hospital acquired pressure ulcers • Increase consistency of screening for VTE and dementia • Increase consistency and timing for discharge summary communication to GPs • Opportunities explored in Current State Assessment • Topics which were not considered prioritised opportunities during the current state assessment Revenue Enhancement • Increase revenue through improved coding • Increase charge capture for existing patients (medications, procedures) • Increased identification of billable encounters • Reduce denials • Increase theatre utilisation • Increase A&E throughput • Increase outpatient clinic utilisation • Improve clinical documentation quality The benefits identified during the development of the Acquisition Business Case and detailed within the LTFM will be reviewed in detail during EPR procurement and refined based on current state / future state mapping and the selection of the EPR vendor and available functionality 30
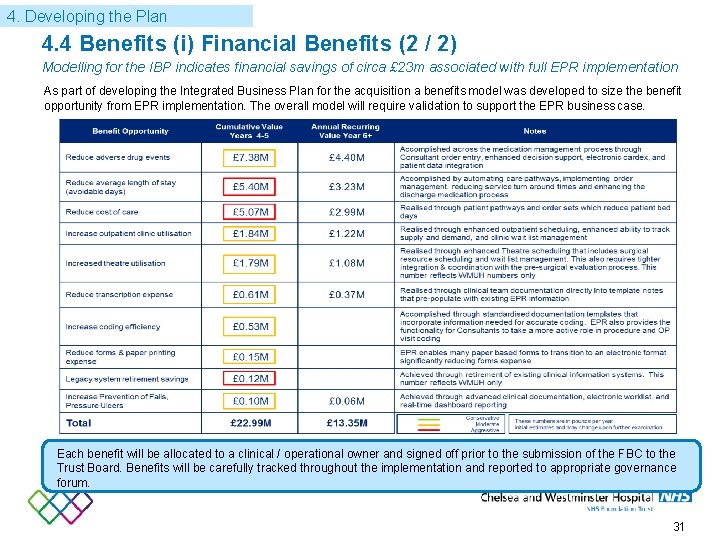
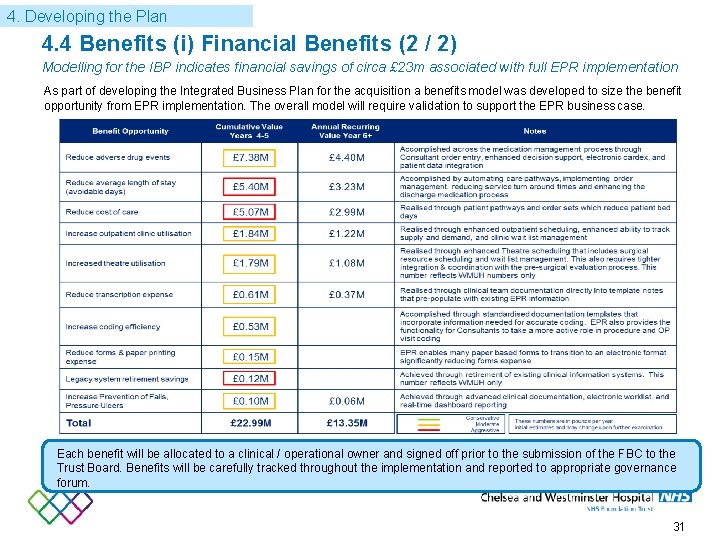
4. Developing the Plan 4. 4 Benefits (i) Financial Benefits (2 / 2) Modelling for the IBP indicates financial savings of circa £ 23 m associated with full EPR implementation … As part of developing the Integrated Business Plan for the acquisition a benefits model was developed to size the benefit opportunity from EPR implementation. The overall model will require validation to support the EPR business case. Each benefit will be allocated to a clinical / operational owner and signed off prior to the submission of the FBC to the Trust Board. Benefits will be carefully tracked throughout the implementation and reported to appropriate governance forum. 31
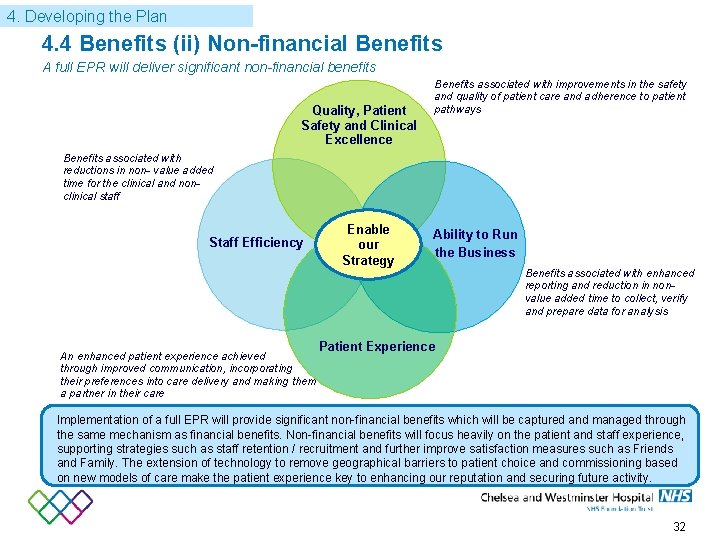
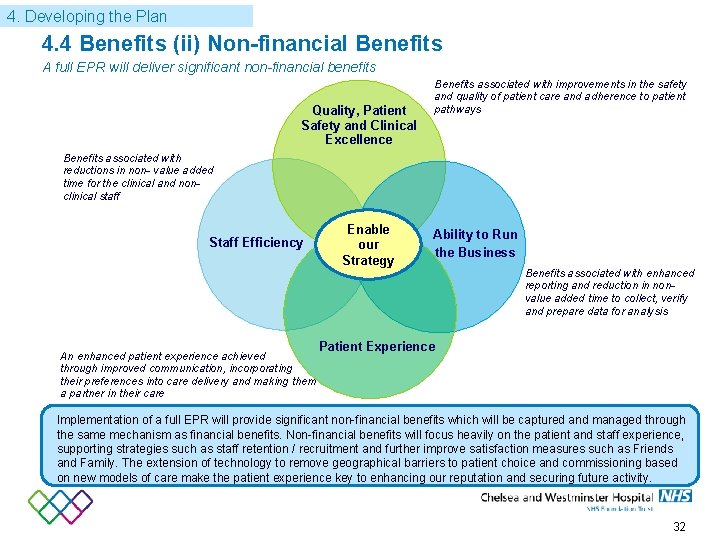
4. Developing the Plan 4. 4 Benefits (ii) Non-financial Benefits A full EPR will deliver significant non-financial benefits Quality, Patient Safety and Clinical Excellence Benefits associated with improvements in the safety and quality of patient care and adherence to patient pathways Benefits associated with reductions in non- value added time for the clinical and nonclinical staff Staff Efficiency An enhanced patient experience achieved through improved communication, incorporating their preferences into care delivery and making them a partner in their care Enable our Strategy Ability to Run the Business Benefits associated with enhanced reporting and reduction in nonvalue added time to collect, verify and prepare data for analysis Patient Experience Implementation of a full EPR will provide significant non-financial benefits which will be captured and managed through the same mechanism as financial benefits. Non-financial benefits will focus heavily on the patient and staff experience, supporting strategies such as staff retention / recruitment and further improve satisfaction measures such as Friends and Family. The extension of technology to remove geographical barriers to patient choice and commissioning based on new models of care make the patient experience key to enhancing our reputation and securing future activity. 32
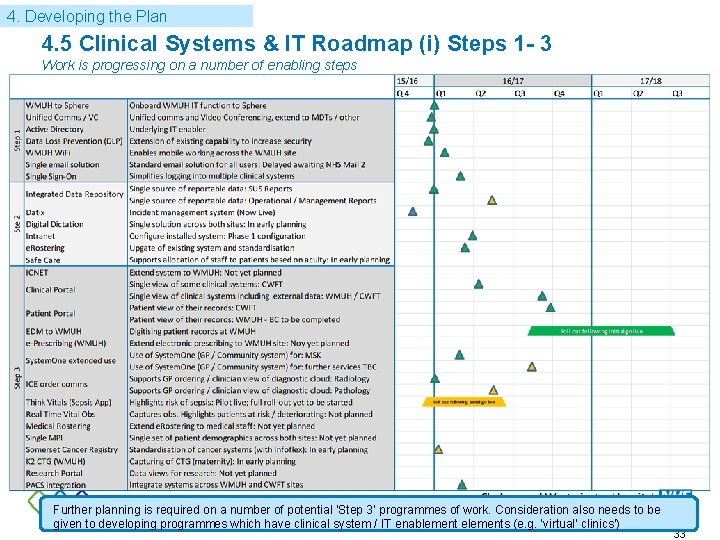
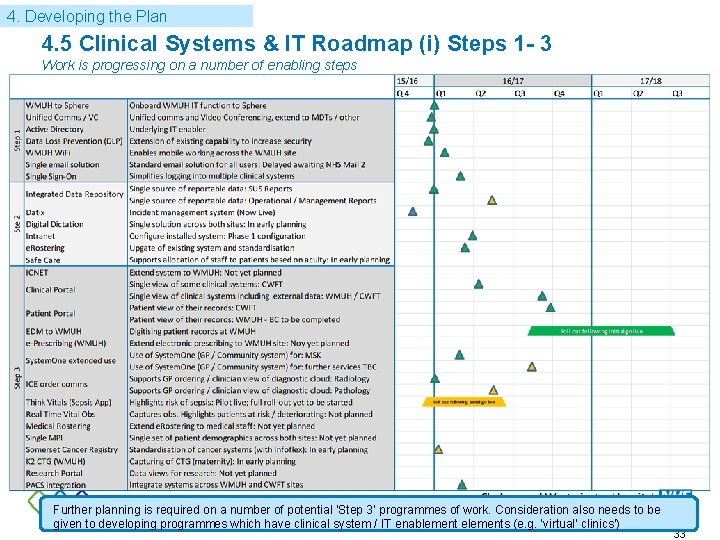
4. Developing the Plan 4. 5 Clinical Systems & IT Roadmap (i) Steps 1 - 3 Work is progressing on a number of enabling steps Further planning is required on a number of potential ‘Step 3’ programmes of work. Consideration also needs to be given to developing programmes which have clinical system / IT enablement elements (e. g. ‘virtual’ clinics’) 33
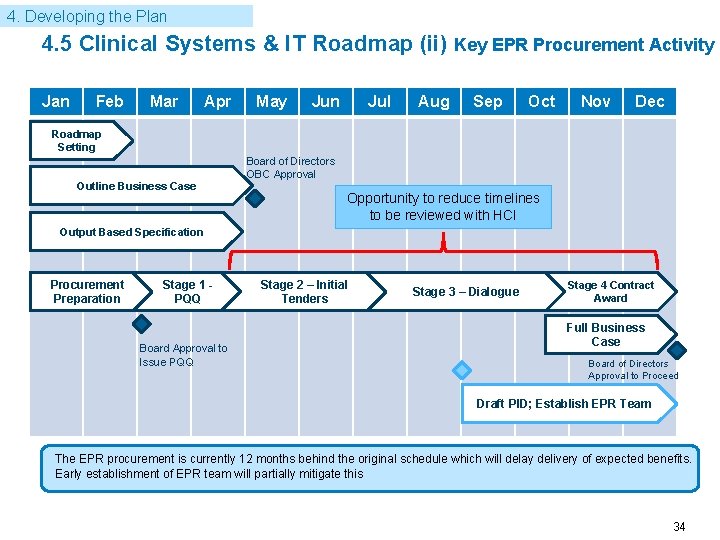
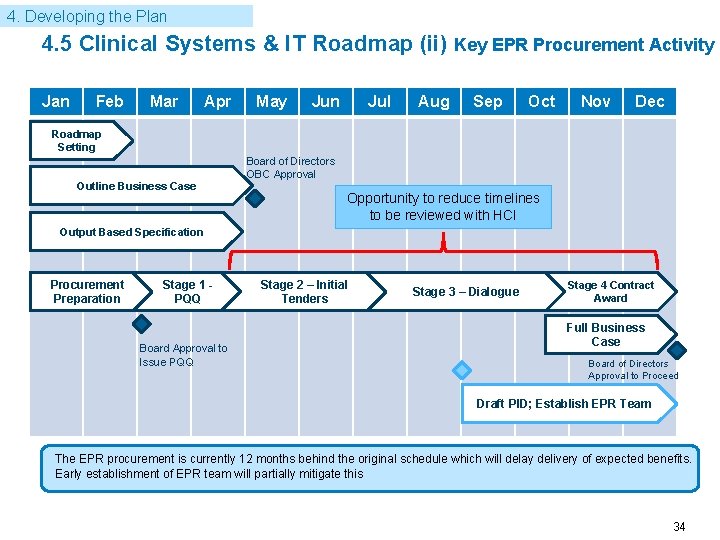
4. Developing the Plan 4. 5 Clinical Systems & IT Roadmap (ii) Key EPR Procurement Activity Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Roadmap Setting Outline Business Case Board of Directors OBC Approval Opportunity to reduce timelines to be reviewed with HCI Output Based Specification Procurement Preparation Stage 1 PQQ Board Approval to Issue PQQ Stage 2 – Initial Tenders Stage 3 – Dialogue Stage 4 Contract Award Full Business Case Board of Directors Approval to Proceed Draft PID; Establish EPR Team The EPR procurement is currently 12 months behind the original schedule which will delay delivery of expected benefits. Early establishment of EPR team will partially mitigate this 34
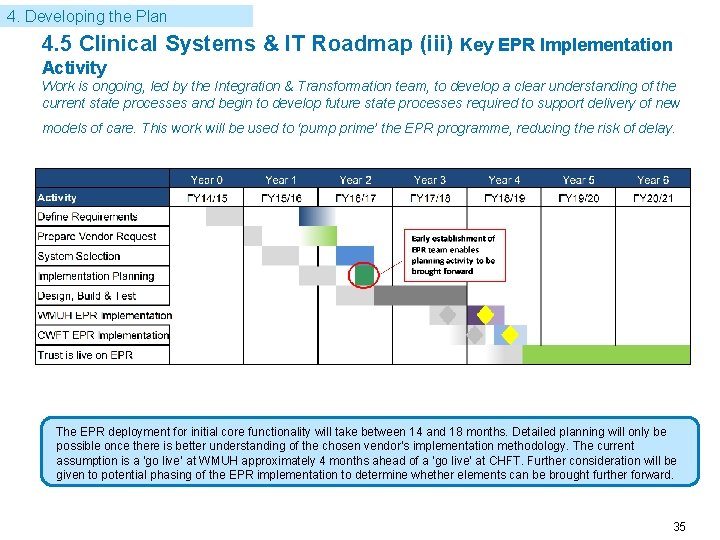
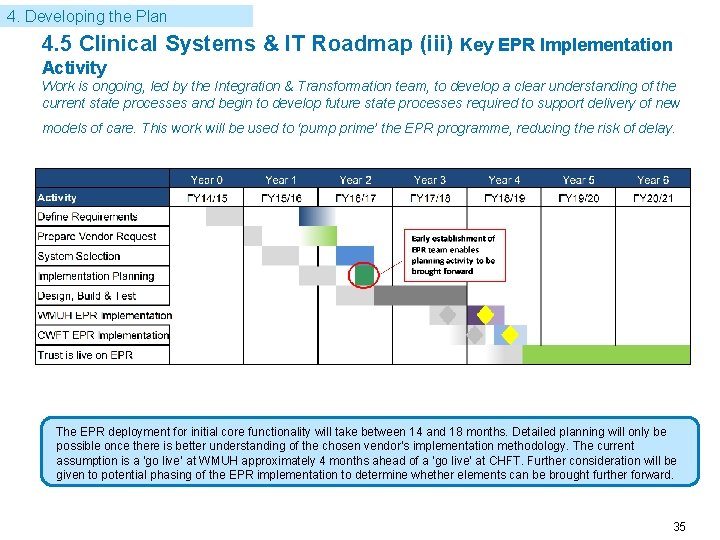
4. Developing the Plan 4. 5 Clinical Systems & IT Roadmap (iii) Key EPR Implementation Activity Work is ongoing, led by the Integration & Transformation team, to develop a clear understanding of the current state processes and begin to develop future state processes required to support delivery of new models of care. This work will be used to ‘pump prime’ the EPR programme, reducing the risk of delay. The EPR deployment for initial core functionality will take between 14 and 18 months. Detailed planning will only be possible once there is better understanding of the chosen vendor’s implementation methodology. The current assumption is a ‘go live’ at WMUH approximately 4 months ahead of a ‘go live’ at CHFT. Further consideration will be given to potential phasing of the EPR implementation to determine whether elements can be brought further forward. 35
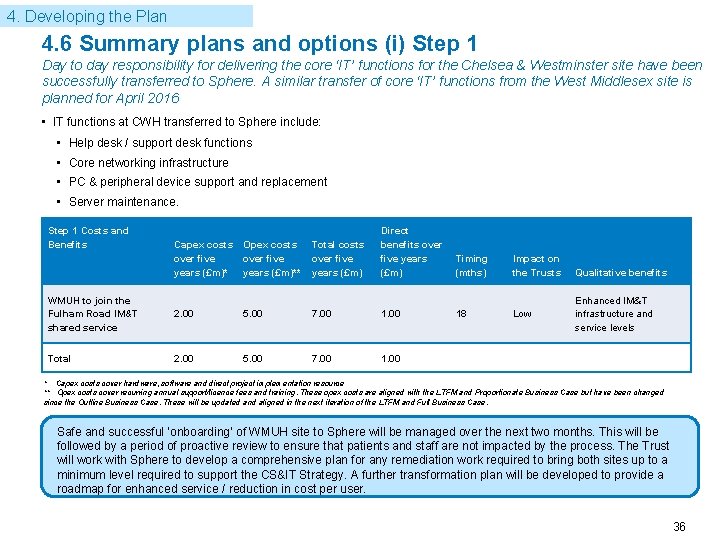
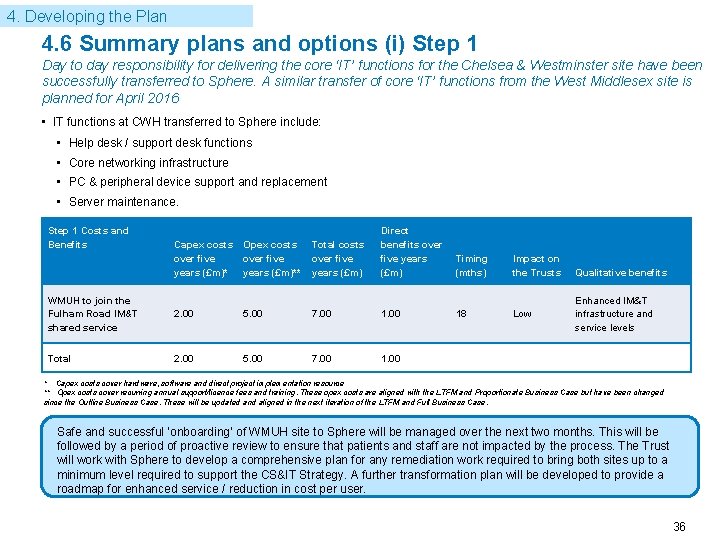
4. Developing the Plan 4. 6 Summary plans and options (i) Step 1 Day to day responsibility for delivering the core ‘IT’ functions for the Chelsea & Westminster site have been successfully transferred to Sphere. A similar transfer of core ‘IT’ functions from the West Middlesex site is planned for April 2016 • IT functions at CWH transferred to Sphere include: • Help desk / support desk functions • Core networking infrastructure • PC & peripheral device support and replacement • Server maintenance. Step 1 Costs and Benefits Capex costs over five years (£m)* Opex costs over five years (£m)** Total costs over five years (£m) Direct benefits over five years (£m) Timing (mths) Impact on the Trusts Qualitative benefits WMUH to join the Fulham Road IM&T shared service 2. 00 5. 00 7. 00 18 Low Enhanced IM&T infrastructure and service levels Total 2. 00 5. 00 7. 00 1. 00 * Capex costs cover hardware, software and direct project implementation resource ** Opex costs cover recurring annual support/licence fees and training. These opex costs are aligned with the LTFM and Proportionate Business Case but have been changed since the Outline Business Case. These will be updated and aligned in the next iteration of the LTFM and Full Business Case. Safe and successful ‘onboarding’ of WMUH site to Sphere will be managed over the next two months. This will be followed by a period of proactive review to ensure that patients and staff are not impacted by the process. The Trust will work with Sphere to develop a comprehensive plan for any remediation work required to bring both sites up to a minimum level required to support the CS&IT Strategy. A further transformation plan will be developed to provide a roadmap for enhanced service / reduction in cost per user. 36
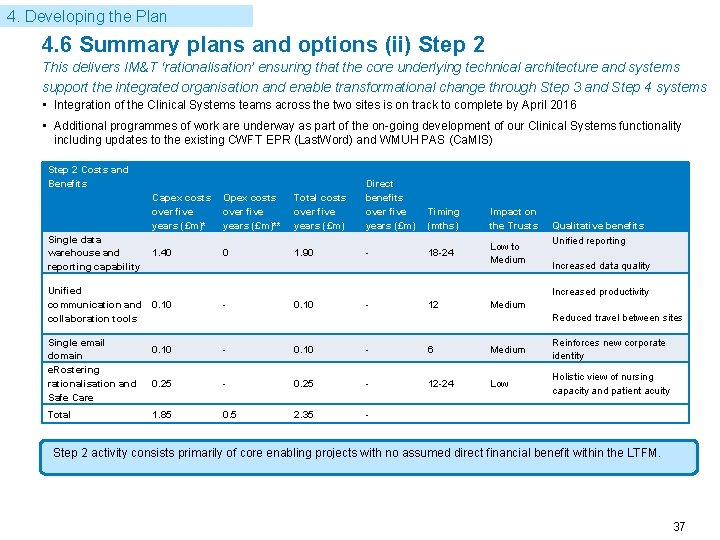
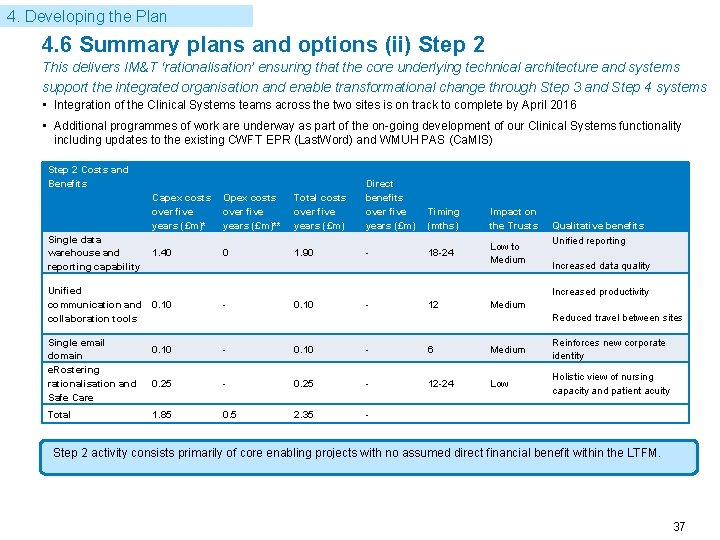
4. Developing the Plan 4. 6 Summary plans and options (ii) Step 2 This delivers IM&T ‘rationalisation’ ensuring that the core underlying technical architecture and systems support the integrated organisation and enable transformational change through Step 3 and Step 4 systems • Integration of the Clinical Systems teams across the two sites is on track to complete by April 2016 • Additional programmes of work are underway as part of the on-going development of our Clinical Systems functionality including updates to the existing CWFT EPR (Last. Word) and WMUH PAS (Ca. MIS) Step 2 Costs and Benefits Capex costs over five years (£m)* Opex costs over five years (£m)** Total costs over five years (£m) Direct benefits over five years (£m) Single data warehouse and reporting capability 1. 40 0 1. 90 - Unified communication and collaboration tools 0. 10 Single email domain e. Rostering rationalisation and Safe Care Total Timing (mths) Impact on the Trusts 18 -24 Low to Medium Qualitative benefits Unified reporting Increased data quality Increased productivity - 0. 10 - 12 Medium Reduced travel between sites 0. 10 - 6 Medium Reinforces new corporate identity 0. 25 - 12 -24 Low Holistic view of nursing capacity and patient acuity 1. 85 0. 5 2. 35 - Step 2 activity consists primarily of core enabling projects with no assumed direct financial benefit within the LTFM. 37
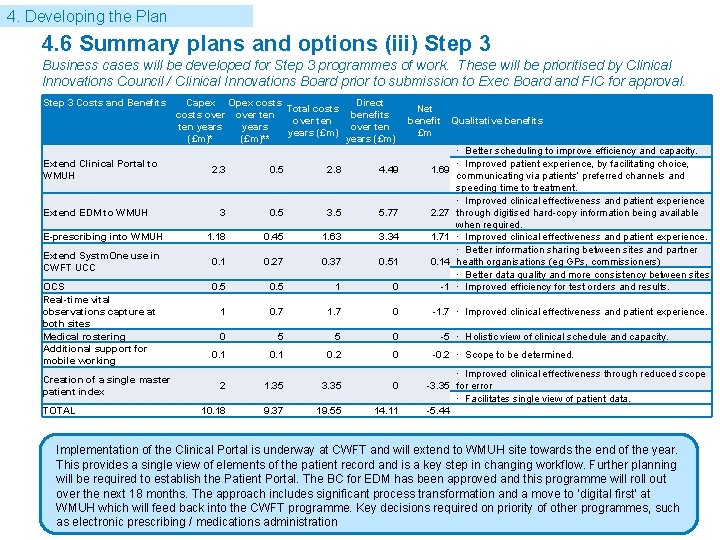
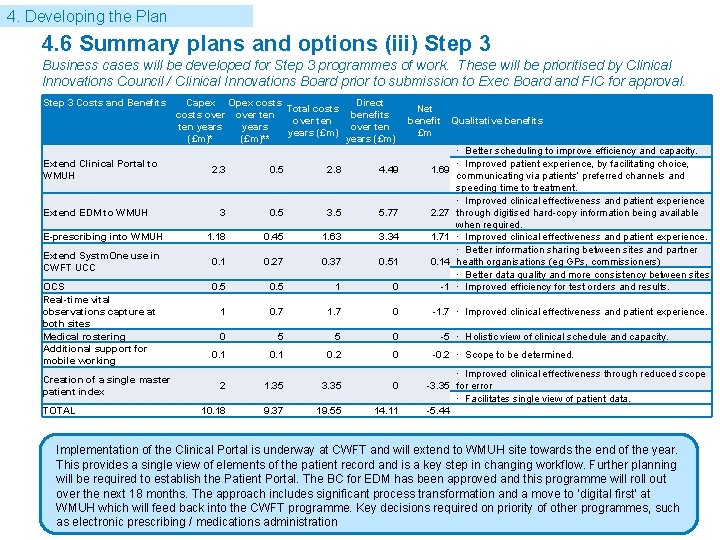
4. Developing the Plan 4. 6 Summary plans and options (iii) Step 3 Business cases will be developed for Step 3 programmes of work. These will be prioritised by Clinical Innovations Council / Clinical Innovations Board prior to submission to Exec Board and FIC for approval. Step 3 Costs and Benefits Extend Clinical Portal to WMUH Capex Opex costs Direct Total costs over ten benefits over ten years (£m)** years (£m) Net benefit Qualitative benefits £m 2. 3 0. 5 2. 8 4. 49 1. 69 3 0. 5 3. 5 5. 77 2. 27 E-prescribing into WMUH 1. 18 0. 45 1. 63 3. 34 1. 71 Extend Systm. One use in CWFT UCC 0. 1 0. 27 0. 37 0. 51 0. 14 0. 5 1 0 -1 1 0. 7 1. 7 0 0 5 5 0 0. 1 0. 2 0 2 1. 35 3. 35 0 10. 18 9. 37 19. 55 14. 11 Extend EDM to WMUH OCS Real-time vital observations capture at both sites Medical rostering Additional support for mobile working Creation of a single master patient index TOTAL · Better scheduling to improve efficiency and capacity. · Improved patient experience, by facilitating choice, communicating via patients’ preferred channels and speeding time to treatment. · Improved clinical effectiveness and patient experience through digitised hard-copy information being available when required. · Improved clinical effectiveness and patient experience. · Better information sharing between sites and partner health organisations (eg GPs, commissioners) · Better data quality and more consistency between sites. · Improved efficiency for test orders and results. -1. 7 · Improved clinical effectiveness and patient experience. -5 · Holistic view of clinical schedule and capacity. -0. 2 · Scope to be determined. · Improved clinical effectiveness through reduced scope -3. 35 for error · Facilitates single view of patient data. -5. 44 Implementation of the Clinical Portal is underway at CWFT and will extend to WMUH site towards the end of the year. This provides a single view of elements of the patient record and is a key step in changing workflow. Further planning will be required to establish the Patient Portal. The BC for EDM has been approved and this programme will roll out over the next 18 months. The approach includes significant process transformation and a move to ‘digital first’ at WMUH which will feed back into the CWFT programme. Key decisions required on priority of other programmes, such as electronic prescribing / medications administration 38
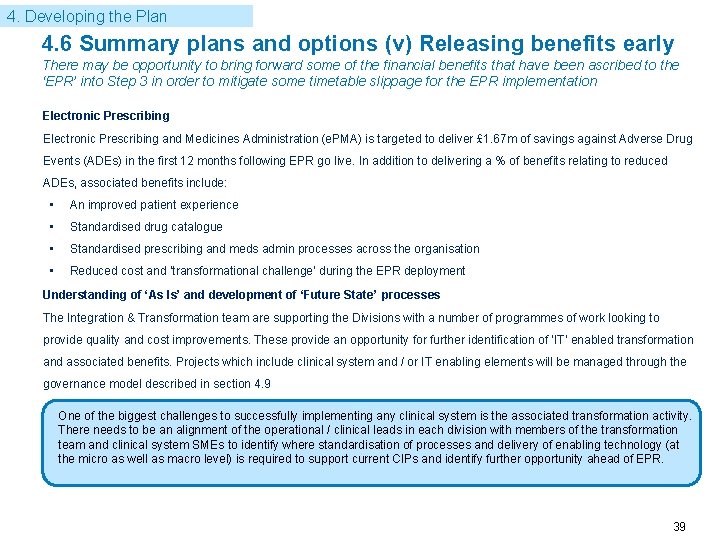
4. Developing the Plan 4. 6 Summary plans and options (v) Releasing benefits early There may be opportunity to bring forward some of the financial benefits that have been ascribed to the ‘EPR’ into Step 3 in order to mitigate some timetable slippage for the EPR implementation Electronic Prescribing and Medicines Administration (e. PMA) is targeted to deliver £ 1. 67 m of savings against Adverse Drug Events (ADEs) in the first 12 months following EPR go live. In addition to delivering a % of benefits relating to reduced ADEs, associated benefits include: • An improved patient experience • Standardised drug catalogue • Standardised prescribing and meds admin processes across the organisation • Reduced cost and ‘transformational challenge’ during the EPR deployment Understanding of ‘As Is’ and development of ‘Future State’ processes The Integration & Transformation team are supporting the Divisions with a number of programmes of work looking to provide quality and cost improvements. These provide an opportunity for further identification of ‘IT’ enabled transformation and associated benefits. Projects which include clinical system and / or IT enabling elements will be managed through the governance model described in section 4. 9 One of the biggest challenges to successfully implementing any clinical system is the associated transformation activity. There needs to be an alignment of the operational / clinical leads in each division with members of the transformation team and clinical system SMEs to identify where standardisation of processes and delivery of enabling technology (at the micro as well as macro level) is required to support current CIPs and identify further opportunity ahead of EPR. 39
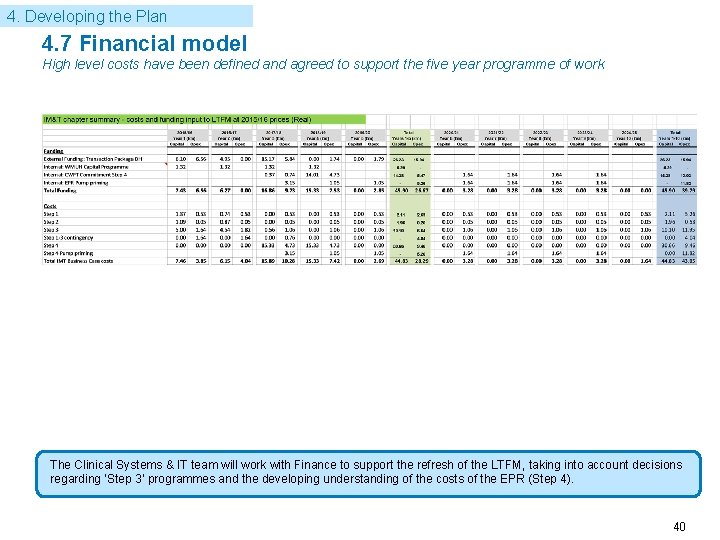
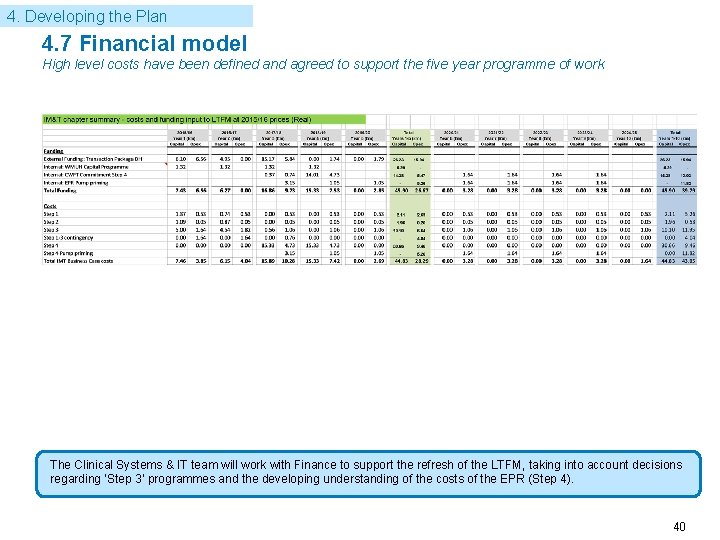
4. Developing the Plan 4. 7 Financial model High level costs have been defined and agreed to support the five year programme of work The Clinical Systems & IT team will work with Finance to support the refresh of the LTFM, taking into account decisions regarding ‘Step 3’ programmes and the developing understanding of the costs of the EPR (Step 4). 40
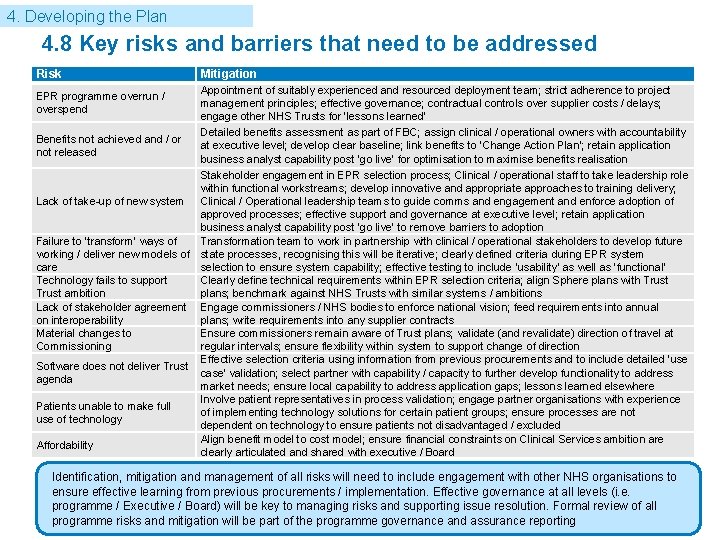
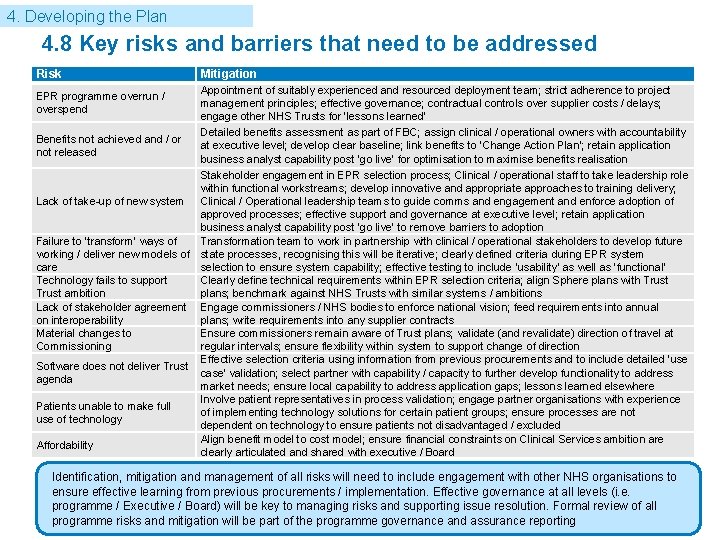
4. Developing the Plan 4. 8 Key risks and barriers that need to be addressed Risk Mitigation Appointment of suitably experienced and resourced deployment team; strict adherence to project management principles; effective governance; contractual controls over supplier costs / delays; engage other NHS Trusts for ‘lessons learned’ Detailed benefits assessment as part of FBC; assign clinical / operational owners with accountability Benefits not achieved and / or at executive level; develop clear baseline; link benefits to ‘Change Action Plan’; retain application not released business analyst capability post ‘go live’ for optimisation to maximise benefits realisation Stakeholder engagement in EPR selection process; Clinical / operational staff to take leadership role within functional workstreams; develop innovative and appropriate approaches to training delivery; Lack of take-up of new system Clinical / Operational leadership teams to guide comms and engagement and enforce adoption of approved processes; effective support and governance at executive level; retain application business analyst capability post ‘go live’ to remove barriers to adoption Failure to ‘transform’ ways of Transformation team to work in partnership with clinical / operational stakeholders to develop future working / deliver new models of state processes, recognising this will be iterative; clearly defined criteria during EPR system care selection to ensure system capability; effective testing to include ‘usability’ as well as ‘functional’ Technology fails to support Clearly define technical requirements within EPR selection criteria; align Sphere plans with Trust ambition plans; benchmark against NHS Trusts with similar systems / ambitions Lack of stakeholder agreement Engage commissioners / NHS bodies to enforce national vision; feed requirements into annual on interoperability plans; write requirements into any supplier contracts Material changes to Ensure commissioners remain aware of Trust plans; validate (and revalidate) direction of travel at Commissioning regular intervals; ensure flexibility within system to support change of direction Effective selection criteria using information from previous procurements and to include detailed ‘use Software does not deliver Trust case’ validation; select partner with capability / capacity to further develop functionality to address agenda market needs; ensure local capability to address application gaps; lessons learned elsewhere Involve patient representatives in process validation; engage partner organisations with experience Patients unable to make full of implementing technology solutions for certain patient groups; ensure processes are not use of technology dependent on technology to ensure patients not disadvantaged / excluded Align benefit model to cost model; ensure financial constraints on Clinical Services ambition are Affordability clearly articulated and shared with executive / Board EPR programme overrun / overspend Identification, mitigation and management of all risks will need to include engagement with other NHS organisations to ensure effective learning from previous procurements / implementation. Effective governance at all levels (i. e. programme / Executive / Board) will be key to managing risks and supporting issue resolution. Formal review of all programme risks and mitigation will be part of the programme governance and assurance reporting 41
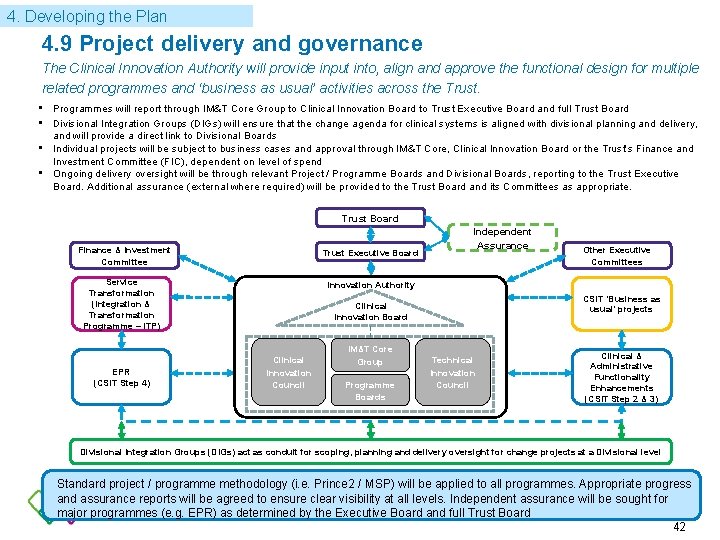
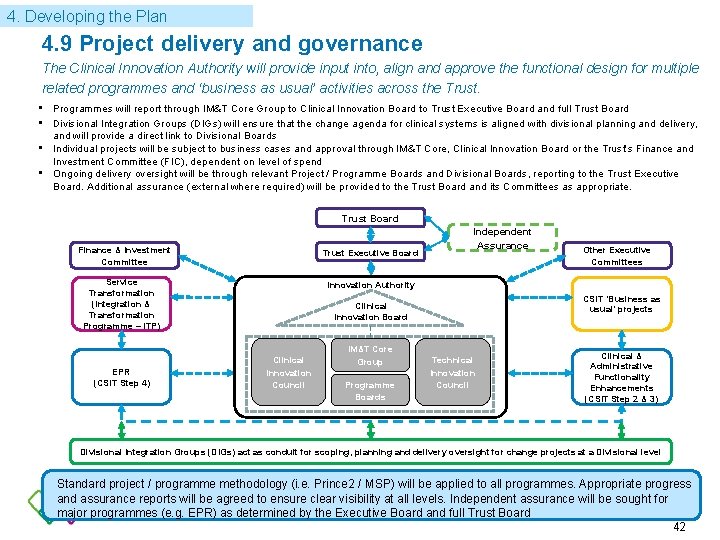
4. Developing the Plan 4. 9 Project delivery and governance The Clinical Innovation Authority will provide input into, align and approve the functional design for multiple related programmes and ‘business as usual’ activities across the Trust. • Programmes will report through IM&T Core Group to Clinical Innovation Board to Trust Executive Board and full Trust Board • Divisional Integration Groups (DIGs) will ensure that the change agenda for clinical systems is aligned with divisional planning and delivery, and will provide a direct link to Divisional Boards • Individual projects will be subject to business cases and approval through IM&T Core, Clinical Innovation Board or the Trust’s Finance and Investment Committee (FIC), dependent on level of spend • Ongoing delivery oversight will be through relevant Project / Programme Boards and Divisional Boards, reporting to the Trust Executive Board. Additional assurance (external where required) will be provided to the Trust Board and its Committees as appropriate. Trust Board Finance & Investment Committee Trust Executive Board Service Transformation (Integration & Transformation Programme – ITP) EPR (CSIT Step 4) Independent Assurance Other Executive Committees Innovation Authority CSIT ‘Business as usual’ projects Clinical Innovation Board Clinical Innovation Council IM&T Core Group Programme Boards Technical Innovation Council Clinical & Administrative Functionality Enhancements (CSIT Step 2 & 3) Divisional Integration Groups (DIGs) act as conduit for scoping, planning and delivery oversight for change projects at a Divisional level Standard project / programme methodology (i. e. Prince 2 / MSP) will be applied to all programmes. Appropriate progress and assurance reports will be agreed to ensure clear visibility at all levels. Independent assurance will be sought for major programmes (e. g. EPR) as determined by the Executive Board and full Trust Board 42
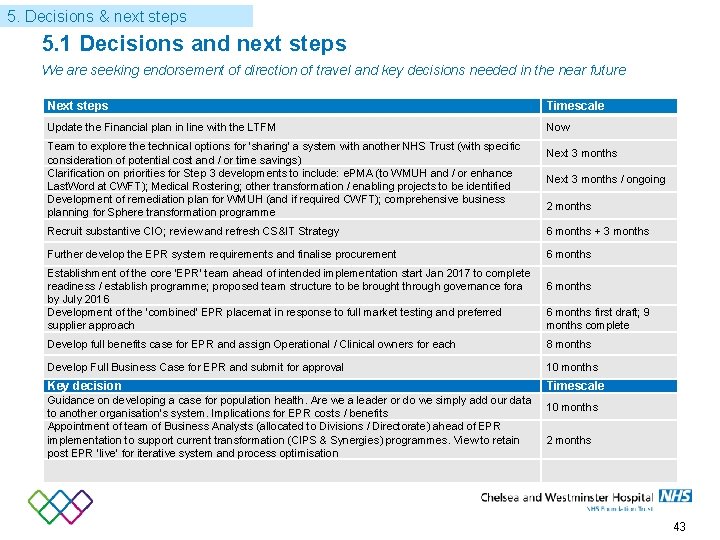
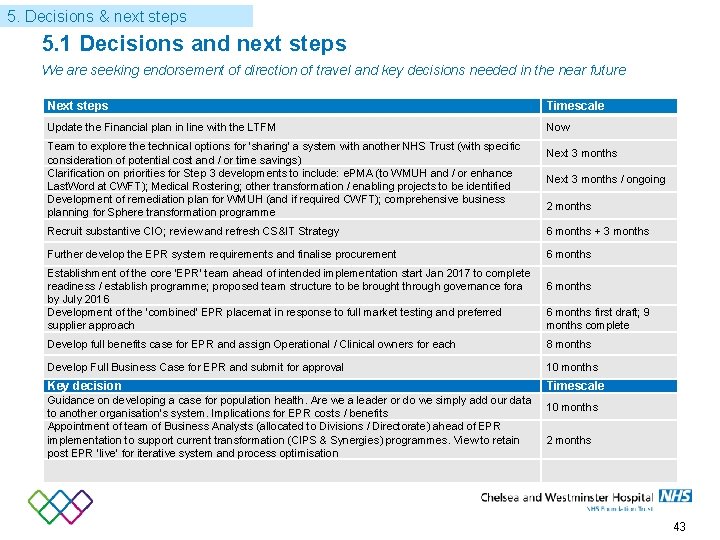
5. Decisions & next steps 5. 1 Decisions and next steps We are seeking endorsement of direction of travel and key decisions needed in the near future Next steps Timescale Update the Financial plan in line with the LTFM Now Team to explore the technical options for ‘sharing’ a system with another NHS Trust (with specific consideration of potential cost and / or time savings) Clarification on priorities for Step 3 developments to include: e. PMA (to WMUH and / or enhance Last. Word at CWFT); Medical Rostering; other transformation / enabling projects to be identified Development of remediation plan for WMUH (and if required CWFT); comprehensive business planning for Sphere transformation programme Next 3 months / ongoing 2 months Recruit substantive CIO; review and refresh CS&IT Strategy 6 months + 3 months Further develop the EPR system requirements and finalise procurement 6 months Establishment of the core ‘EPR’ team ahead of intended implementation start Jan 2017 to complete readiness / establish programme; proposed team structure to be brought through governance fora by July 2016 Development of the ‘combined’ EPR placemat in response to full market testing and preferred supplier approach 6 months first draft; 9 months complete Develop full benefits case for EPR and assign Operational / Clinical owners for each 8 months Develop Full Business Case for EPR and submit for approval 10 months Key decision Timescale Guidance on developing a case for population health. Are we a leader or do we simply add our data to another organisation’s system. Implications for EPR costs / benefits Appointment of team of Business Analysts (allocated to Divisions / Directorate) ahead of EPR implementation to support current transformation (CIPS & Synergies) programmes. View to retain post EPR ‘live’ for iterative system and process optimisation 10 months 2 months 43