CVS Lecture 10 Structure of the Blood Vessels
CVS Lecture – 10
Structure of the Blood Vessels (fig. 1) I. Tunica Interna (Intima) § Consists of a lining of simple squamous epithelium called endothelium supported by a subendothelial layer of loose connective tissue containing few smooth muscle cells. § An internal elastic lamina, a thick sheet of elastic tissue which in histological section has a characteristic wavy appearance, exists between the tunica intima and media. 1
II. Tunica Media § In general consists of concentric layers of helically arranged smooth muscle cells, interposed by variable amount of elastic fibers and lamellae, reticular fibers, glycoproteins, and proteoglycans. § It is separated from the tunica adventitia by an external elastic lamina. 2

III. Tunica Externa (Adventitia) § Consists mainly of connective tissue rich in collagene and elastic fibers. § It becomes continuous with the connective tissue of the organ through which the vessel runs. 3
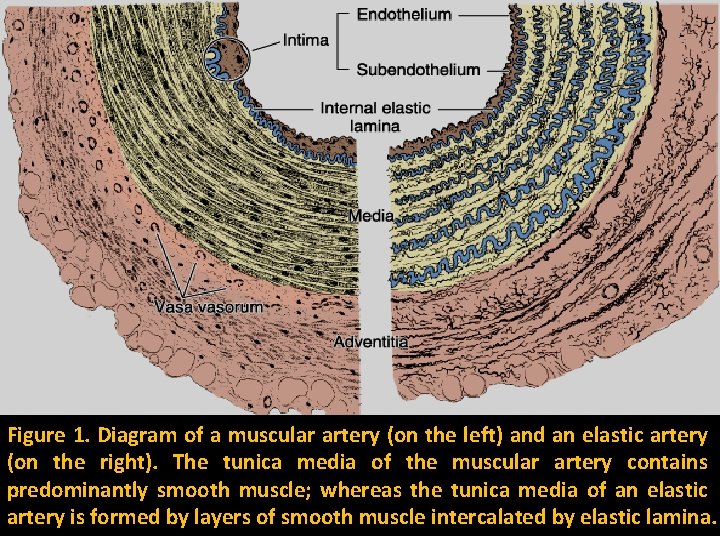
Figure 1. Diagram of a muscular artery (on the left) and an elastic artery (on the right). The tunica media of the muscular artery contains predominantly smooth muscle; whereas the tunica media of an elastic artery is formed by layers of smooth muscle intercalated by elastic lamina.
Larger (Elastic) Arteries (fig. 2) a. Tunica Intima: § Is thicker than the corresponding tunic of a muscular artery. § The internal elastic lamina, although present, may not be easily distinguished from the elastic layer of tunica media. § The several elastic lamina helps to maintain arterial pressure. 4
b. Tunica Media: § Consists of elastic fibers and a series of concentrically arranged, perforated (fenestrated) elastic lamina whose number increases with age. § The reason for the fenestration is not clear, but it may possibly facilitate the passage of the fine nerves and blood vessels which ramify in the wall of the artery. § In these arteries, the smooth muscle fibers are little; as these arteries divide, muscle fibers appear in increasing numbers, while elastic tissue diminishes. 5
c. Tunica Externa: It is relatively undeveloped. 6
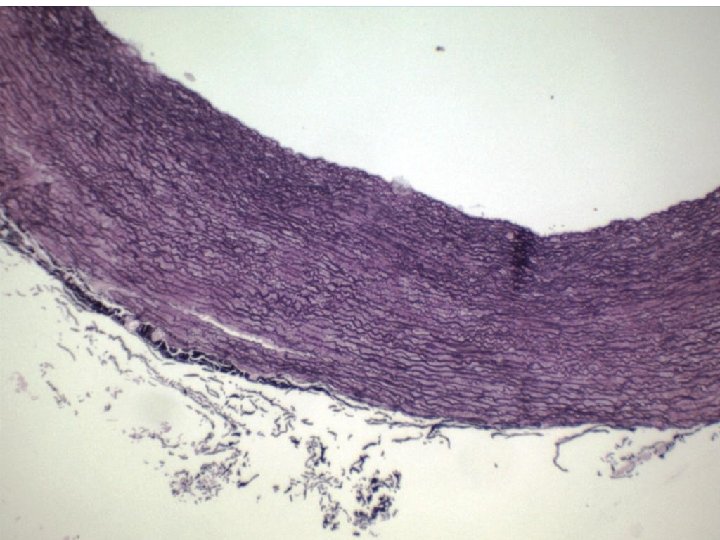
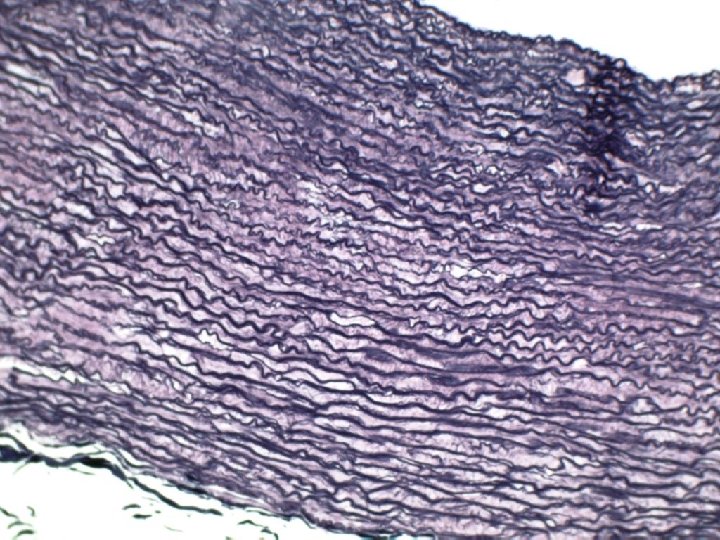
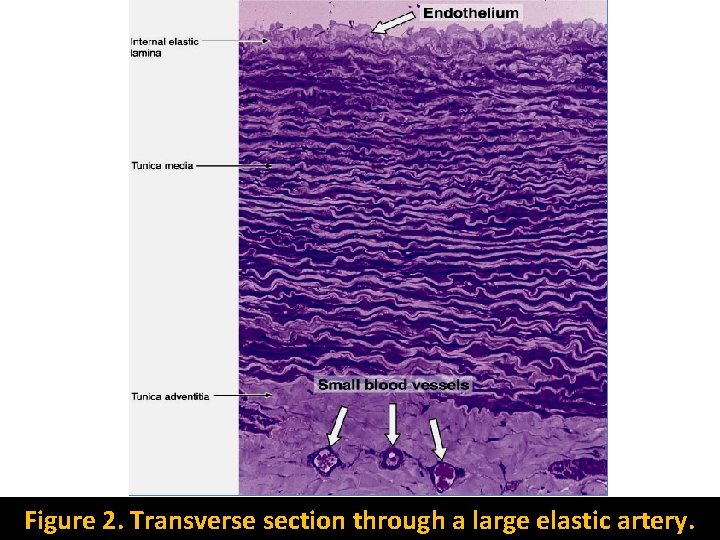
Figure 2. Transverse section through a large elastic artery.

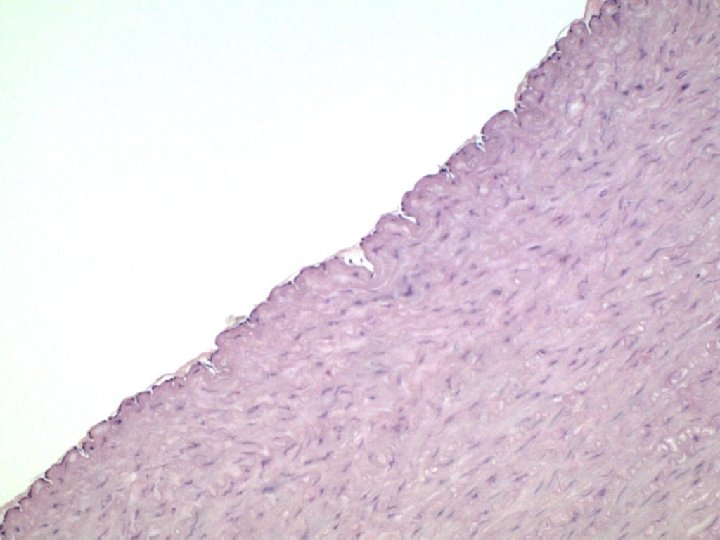
Medium (Muscular) Arteries (fig. 3) a. Tunica Intima : § The subendothelial layer Is thicker than that of the small arteries and arterioles. § The internal elastic lamina Is prominent. b. Tunica Media: § In the muscular arteries, this layer contains up to 40 layers of smooth muscle cells. § These cells are intermingled with various number of elastic lamellae, reticular fibers, and proteoglycans, all synthesized by the smooth muscle fibers. § An external lamina is present in the large muscular arteries. 7

c. Tunica Externa: In addition to the connective tissue, the adventitia contains lymphatic capillaries, vasa vasorum and nerves. 8
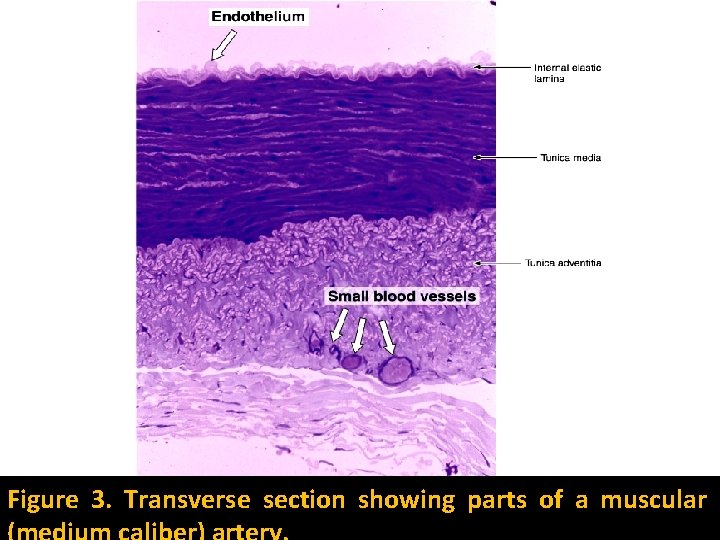
Figure 3. Transverse section showing parts of a muscular
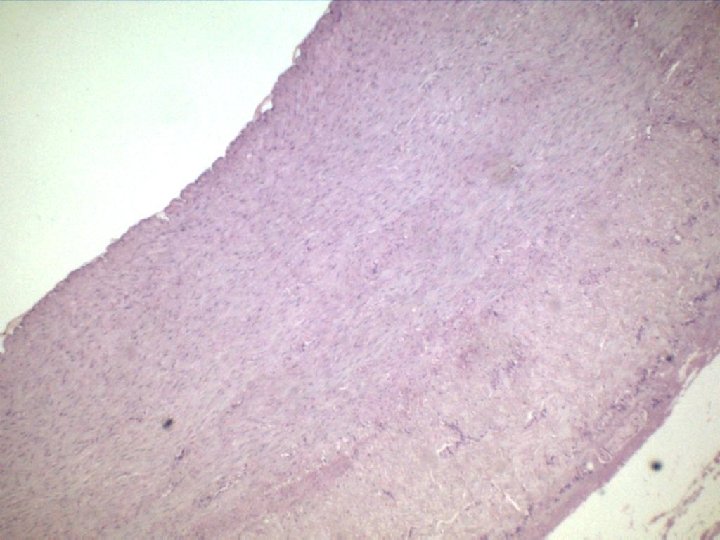
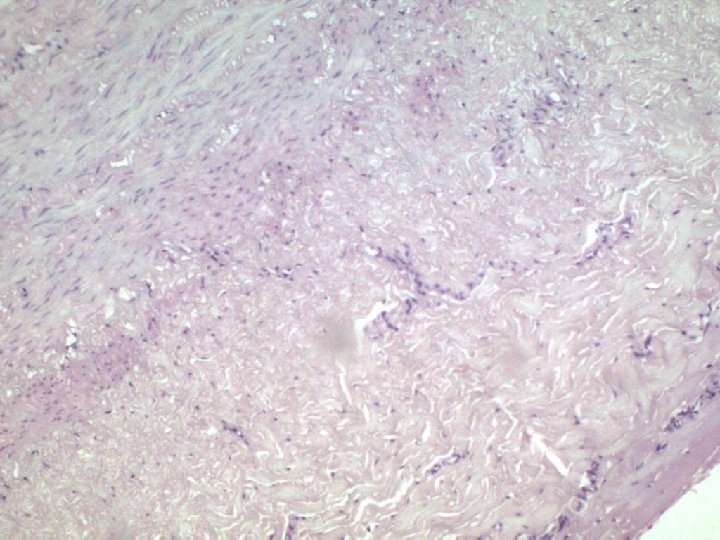
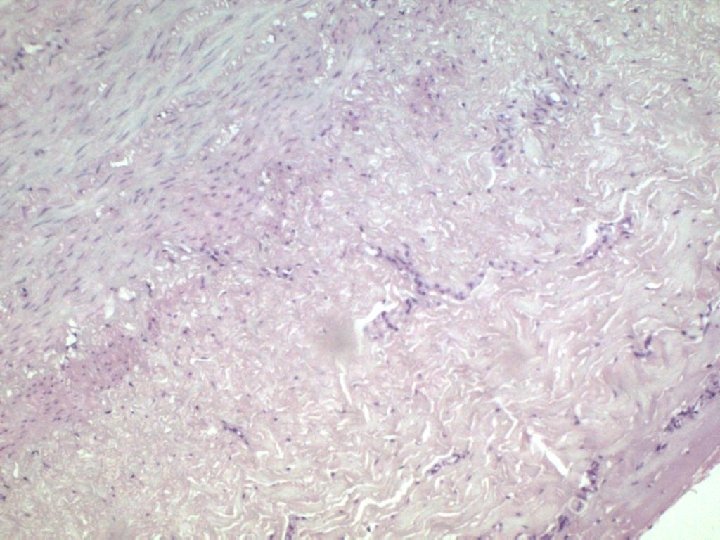
Smaller Arteries & Arterioles (fig. 4, 5, 6, and 7) a. Tunica Intima: § The subendothelial layer is relatively very thin. § In the very small arterioles, the internal elastic lamina is absent. b. Tunica Media: Is almost exclusively muscular and very thin. c. Tunica Externa: It is very thin. 9

Figure 4. Cross section of small artery: The elastic lamina is not stained and is seen as a pallid lamina of scalloped appearance just below the endothelium (arrowhead) – Medium magnification.
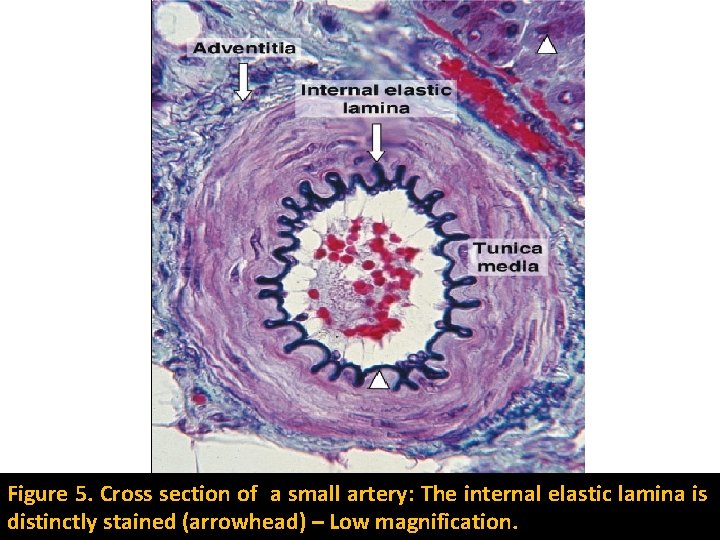
Figure 5. Cross section of a small artery: The internal elastic lamina is distinctly stained (arrowhead) – Low magnification.

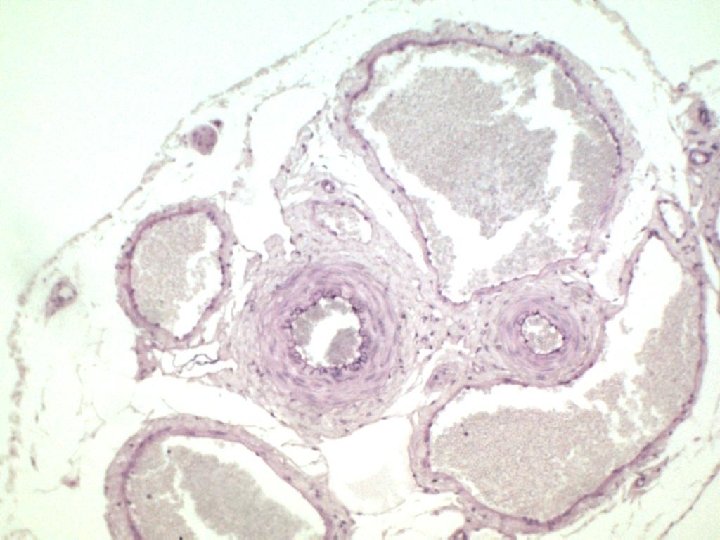
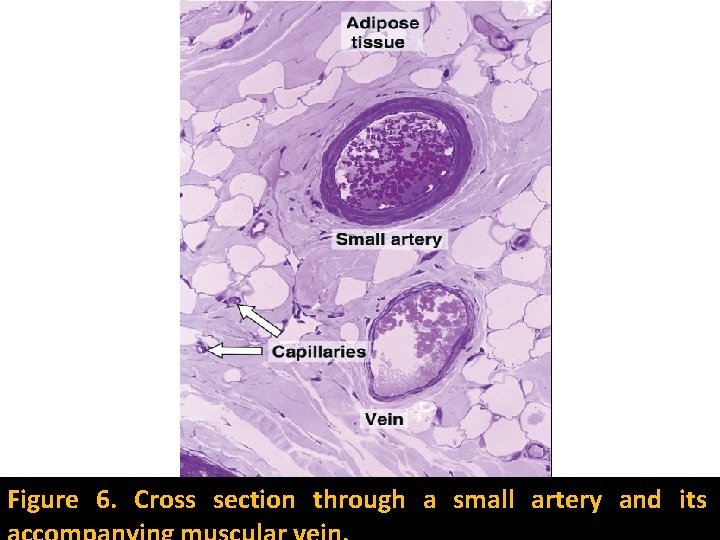
Figure 6. Cross section through a small artery and its
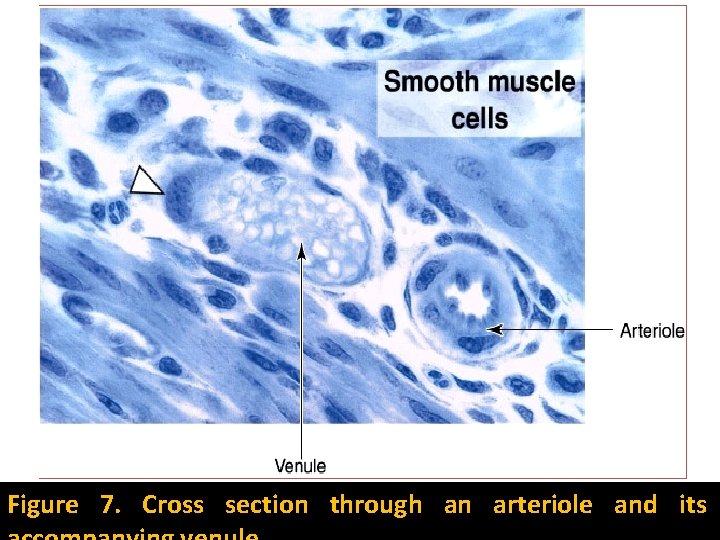
Figure 7. Cross section through an arteriole and its
Large Venous Trunks (fig. 8) a. Tunica intima: § Is well developed § They have valves in their interior. § The valves consist of two semilunar folds of the tunica intima that project into the lumen. § They are composed of connective tissue rich in elastic fibers and are lined on both sides by endothelium. § The valves are especially numerous in veins of the limbs, direct the venous blood toward the heart. 10
b. Tunica Media: Is relatively thin, consists of few layer of smooth muscle cells and abundant connective tissue. c. Tunica Externa: It is the thick and well developed layer, and frequently contains longitudinal bundles of smooth muscle. 11
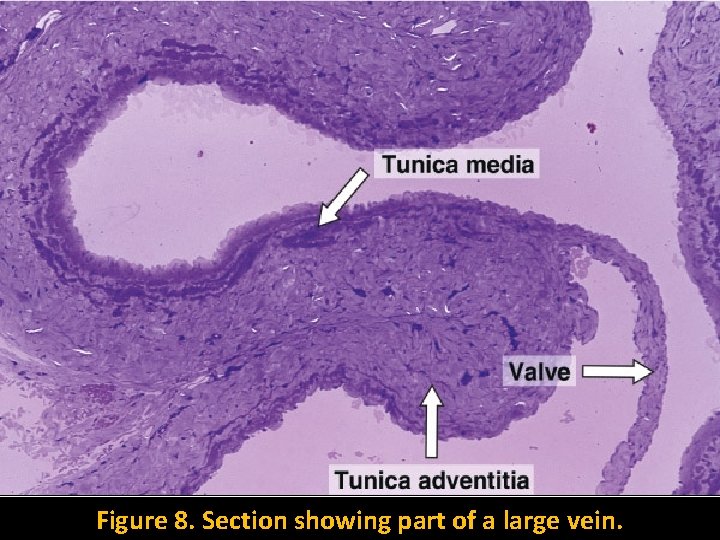
Figure 8. Section showing part of a large vein.
Medium and Small-sized Veins (fig. 6) a. Tunica Intima: Has a thin subendothelial layer, which may be absent at time. b. Tunica Media: Consists of small bundles of smooth muscle cells intermixed with reticular fibers and a delicate network of elastic fibers. It may contain only contractile pericytes. c. Tunica Externa: Is well developed, has abundant collagen fibers. 12
Venules (fig. 7) § Most venules are muscular, and are easily distinguished in section tissues because their thinner wall and irregular and collaps lumen. § These venules may also influence blood flow in the arterioles by producing and secreting diffusible vasoactive substances. § The tunica adventitia and the outer part of the tunica media of the large vessels have their metabolites via vasorum ("vessels of the vessel"). § These arterioles, capillaries, and venules that enter the vessels and branch profusely in the adventitia and media. 13
§ The most internal region of the media and the intema receive oxygen and nutrition by diffusion from the blood that passes through the lumen of these vessels. 14
Structures of the Capillaries § The capillaries are composed of a single layer of endothelial cells rolled up in the form of a tube. § In cross section, the walls of these vessels appear to consist of portions of 1 – 3 cells. § The external surfaces of these cells usually rest on a basal lamina. § The endothelial cells, in general are polygonal and elongated in the direction of the blood flow. § The nucleus causes the cell to bulge into the capillary lumen. § The cytoplasm contains few cisternae of rough endoplasmic reticulum, small Golgi complex, free ribosomes and few mitochondria. 15
§ Tight junctions (Zonula occludentes) type of cell junctions exist between these cells. § These junctions offer variable permeability to the macromolecules that play a significant role in both physiological and pathological conditions. 16
§ Pericyte cells of mesenchymal origin are distributed at various locations along capillaries and post capillary venules. § These cells have long cytoplasmic processes that partly surround the endothelial cells. § Pericytes are enclosed in their own basal lamina, which may fuse with that of the endothelial cells. § After tissue injuries, pericytes participates in the repair process. § They proliferate and differentiate to form new blood vessels and connective tissue cells. § Depending on the continuity of both the endothelial sheet and the basal lamina, capillaries can be classified into three groups: 17

A. Fenestrated capillaries (fig. 10) § Are found in some tissue where there is extensive change with blood; such as small intestine, endocrine glands and the kidney. § These capillaries have several circular transcellular openings (fenestrae) in the endothelium membrane (arrows). § These fenestrae are limited by the cell membrane, resulting in a continuous cell membrane channel from the blood front to the tissue front. § Each fenestra is closed by a diaphragm, which is thinner than a cell membrane. § The basal lamina in these capillaries is continuous (double arrows). 18
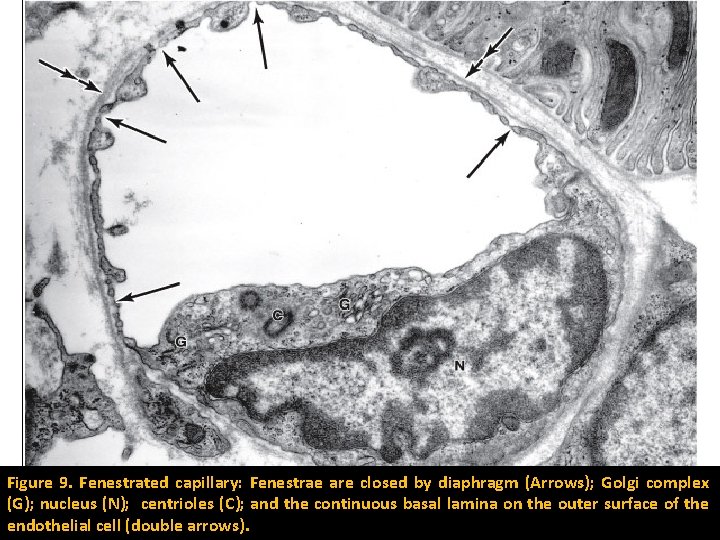
Figure 9. Fenestrated capillary: Fenestrae are closed by diaphragm (Arrows); Golgi complex (G); nucleus (N); centrioles (C); and the continuous basal lamina on the outer surface of the endothelial cell (double arrows).
B. Continuous or somatic capillaries (fig. 10) § These capillaries are present in all types of muscle tissue, connective tissue, exocrine glands, and nervous tissue. § They have no fenestrae in their wall. § Numerous pinocytotic vesicles are found in the cytoplasm of endothelial cells of this type of capillary, except in the nervous system. 19
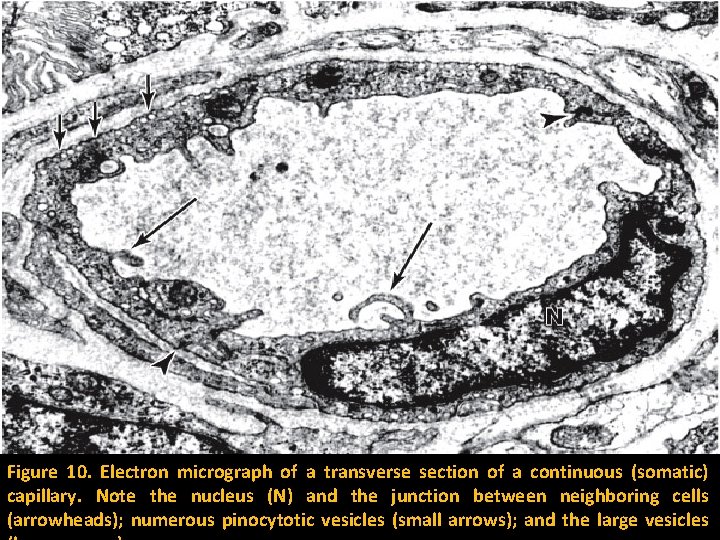
Figure 10. Electron micrograph of a transverse section of a continuous (somatic) capillary. Note the nucleus (N) and the junction between neighboring cells (arrowheads); numerous pinocytotic vesicles (small arrows); and the large vesicles

C. Discontinuous sinusoidal capillaries § These capillaries are found mainly in the liver and in hematopoietic organs such as bone marrow and spleen. § They have large diameter and a tortuous path, which slows the circulation of blood. § Their endothelial cells form a discontinuous layer, and are separated from one another by wide spaces. § The cytoplasm of these endothelial cells has multiple fenestrations without diaphragms. § Unlike fenestrated capillaries, the basal lamina in the sinusoidal is discontinuous. § Macrophages are seen either among or outside the endothelial cells. 20
Embryology of the Heart § The CVS is the first major system to function in the embryo. § The system appears in the middle of the 3 rd week of embryonic life. § The heart starts to function at the beginning of the 4 th week. 1
Development of the Heart § At the middle of the 3 rd week of fetal development, two endothelial strands, the angioblstic cords, appear in the cardiogenic mesoderm. § The angioblastic cords canalize to form the endocardial heart tube. § About end of the 3 rd week the endocardial heart tube approach each other and fuse to form a single tube, the tubular heart (fig. 3 and 4). § The heart begins to beat at 22 to 23 days. § During the formation of the tubular heart, the primordial myocardium is formed from splanchnic mesoderm surrounding the pericardial coelom (fig. 3 and 4). 2
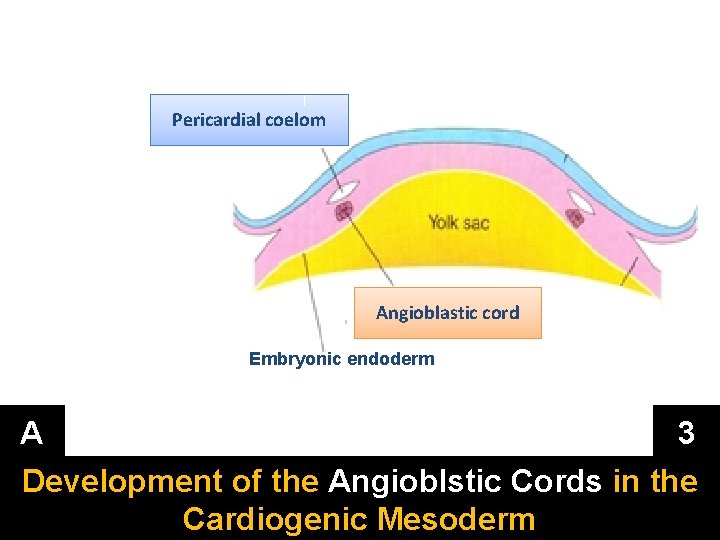
Pericardial coelom Angioblastic cord Embryonic endoderm A 3 Development of the Angioblstic Cords in the Cardiogenic Mesoderm
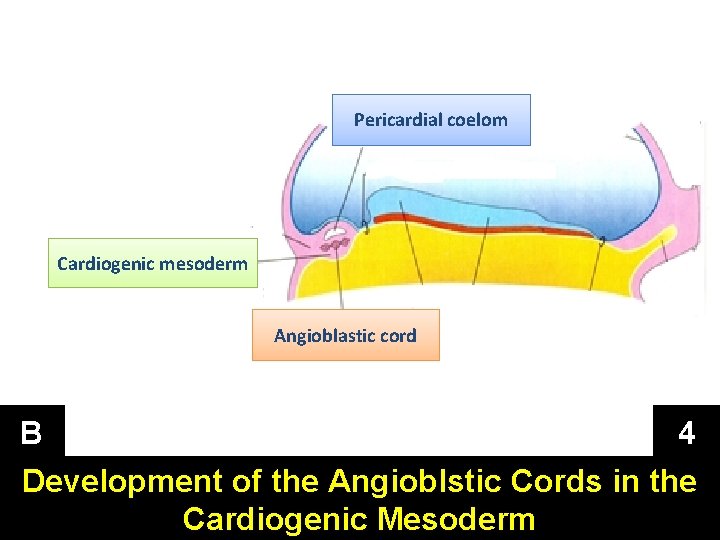
Pericardial coelom Cardiogenic mesoderm Angioblastic cord B 4 Development of the Angioblstic Cords in the Cardiogenic Mesoderm
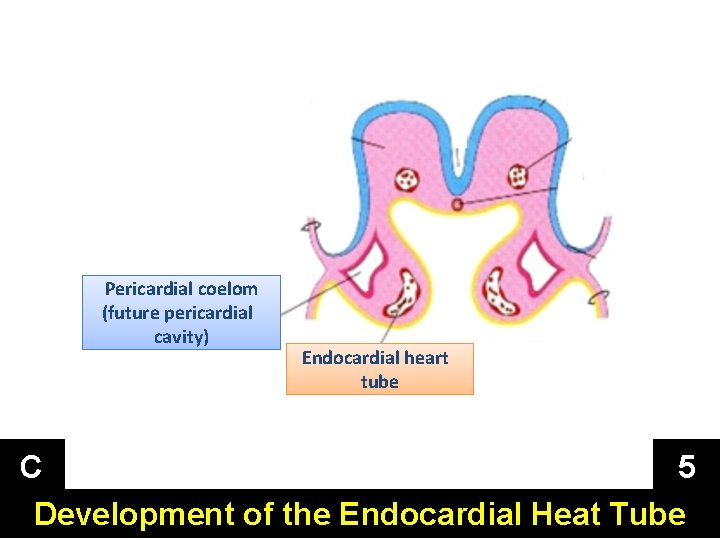
Pericardial coelom (future pericardial cavity) Endocardial heart tube C 5 Development of the Endocardial Heat Tube
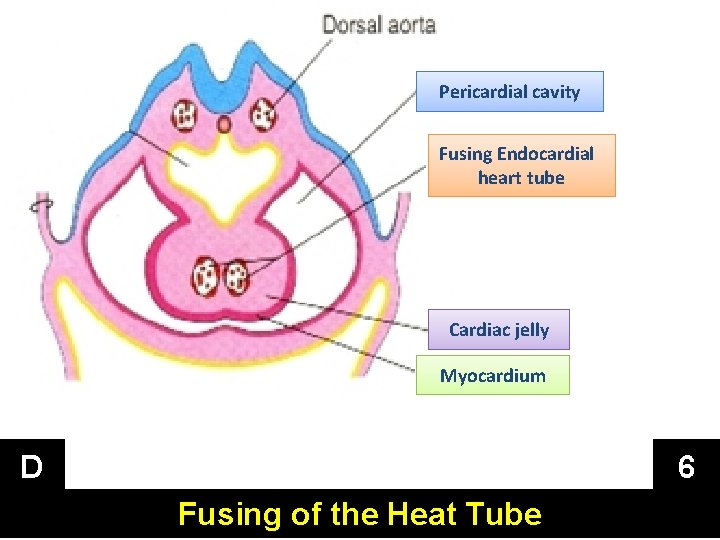
Pericardial cavity Fusing Endocardial heart tube Cardiac jelly Myocardium D 6 Fusing of the Heat Tube
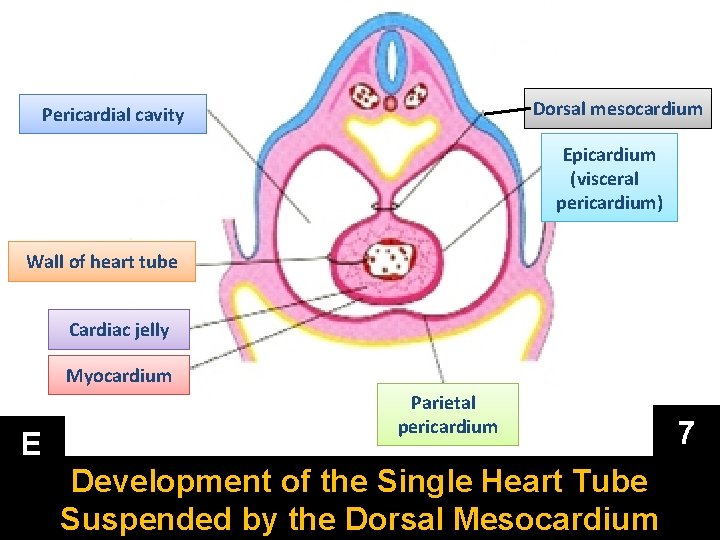
Dorsal mesocardium Pericardial cavity Epicardium (visceral pericardium) Wall of heart tube Cardiac jelly Myocardium E Parietal pericardium Development of the Single Heart Tube Suspended by the Dorsal Mesocardium 7
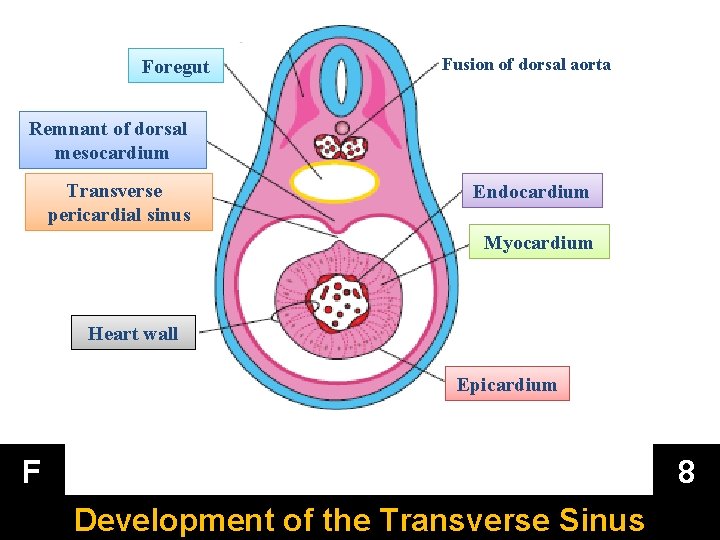
Foregut Fusion of dorsal aorta Remnant of dorsal mesocardium Transverse pericardial sinus Endocardium Myocardium Heart wall Epicardium F 8 Development of the Transverse Sinus
§ At this stage, the developing heart is composed of endothelial tube (tubular heart) that is separated from a thick muscular tube (the primordial myocardium) by gelatinous connective tissue called cardiac jelly. § The endothelial tube (tubular heart) becomes the internal endothelial lining of the heart, the endocardium, and the primordium myocardium becomes the muscular wall of the heart, the myocardium. § The visceral serous pericardium, or epicardium is derived from mesothelial cells that arise from the external surface of the sinus venosus. § The heart and pericardial cavity come to lie ventral to the foregut and caudal to the oropharyngeal membrane. 9
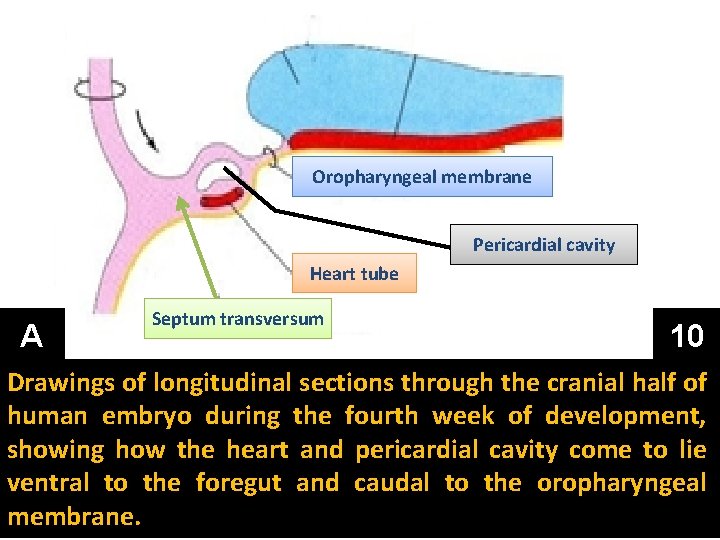
Oropharyngeal membrane Pericardial cavity Heart tube A Septum transversum 10 Drawings of longitudinal sections through the cranial half of human embryo during the fourth week of development, showing how the heart and pericardial cavity come to lie ventral to the foregut and caudal to the oropharyngeal membrane.
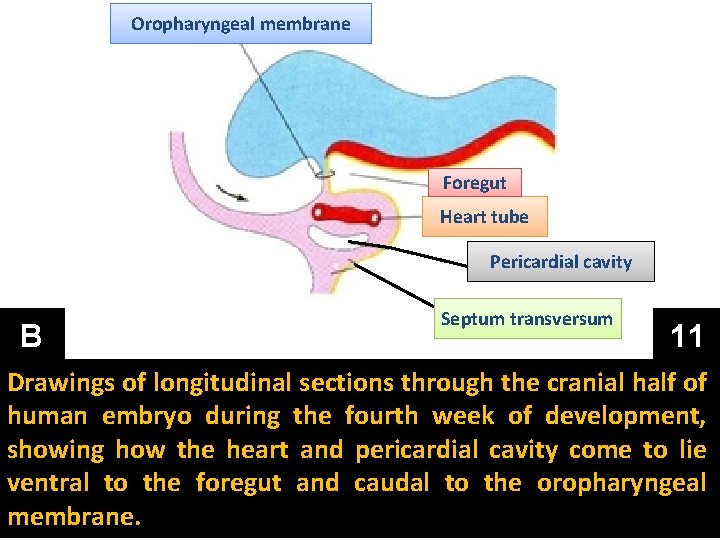
Oropharyngeal membrane Foregut Heart tube Pericardial cavity B Septum transversum 11 Drawings of longitudinal sections through the cranial half of human embryo during the fourth week of development, showing how the heart and pericardial cavity come to lie ventral to the foregut and caudal to the oropharyngeal membrane.
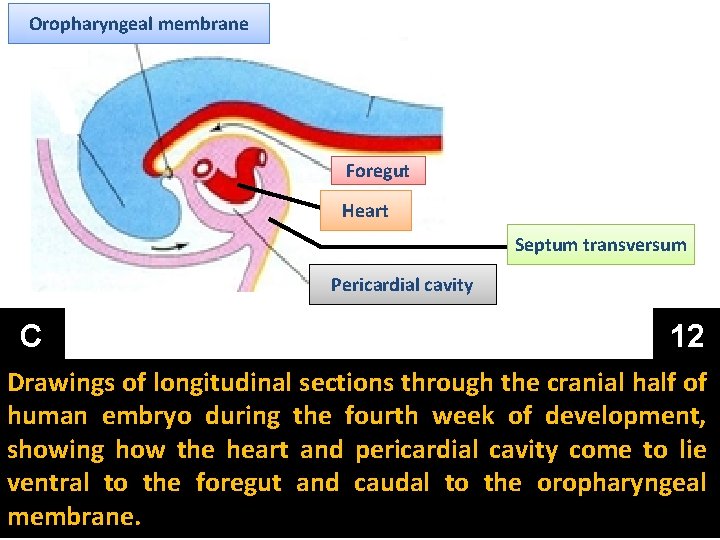
Oropharyngeal membrane Foregut Heart Septum transversum Pericardial cavity C 12 Drawings of longitudinal sections through the cranial half of human embryo during the fourth week of development, showing how the heart and pericardial cavity come to lie ventral to the foregut and caudal to the oropharyngeal membrane.
- Slides: 52