CVS DISEASES Lecture 1 Dr NADIA ALANI Vasculitis

- Slides: 33
CVS DISEASES Lecture 1 Dr. NADIA ALANI
Vasculitis Inflammation of the vessel wall. Affect large & small vessels: Ex. : Large, Medium-sized muscular arteries, Arterioles, Capillaries & Venules. Etiology: Two most common pathogenic mechanisms: 1. Infectious mechanism: Direct vascular invasion by infectious pathogens. 2. Immunologic mechanism: Immune-mediated inflammation.
1. Infectious Vasculitis: Localized arteritis. Cause: Bacteria or fungi: Aspergillus & Mucor spp. Source of vascular invasion: 1. Part of general infection: Ex. Bacterial pneumonia or adjacent to abscesse. 2. Hematogenous spread of bacteria: Septicemia & embolization from infective endocarditis. Concequences of vascular infections: 1. Weaken arterial walls Aneurysms. 2. Induce thrombosis & infarction. Ex. Bacterial meningitis Infl. of vessels Thrombosis & infarction of brain.
2. Immunological vasculitis: (Noninfectious) Main immunologic mechanisms: 1. Immune complex deposition: Polyarteritis nodosa. 2. Anti-neutrophil cytoplasmic antibodies. 3. Anti-endothelial cell antibodies Vasculitis. Ex. Kawasaki disease. 4. Auto-reactive T cells: Activated T lymphocyte in the absence of any identifiable foreign antigen granulomatous vasculitis. Ex. Giant cells (Temporal) arteritis.
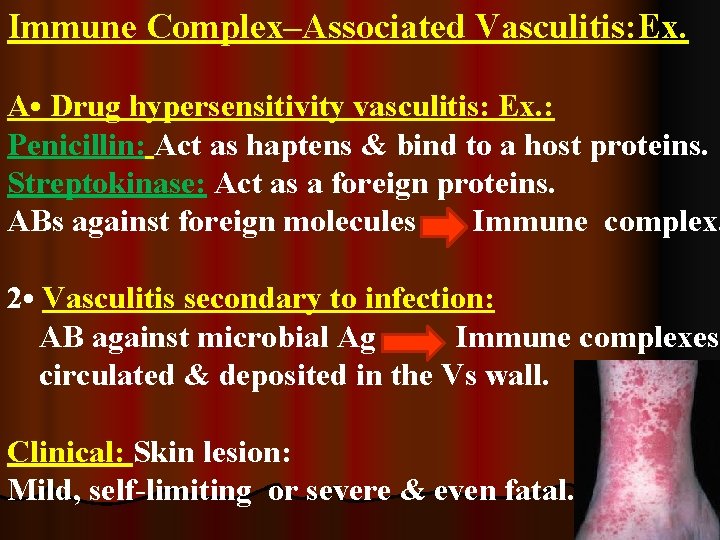
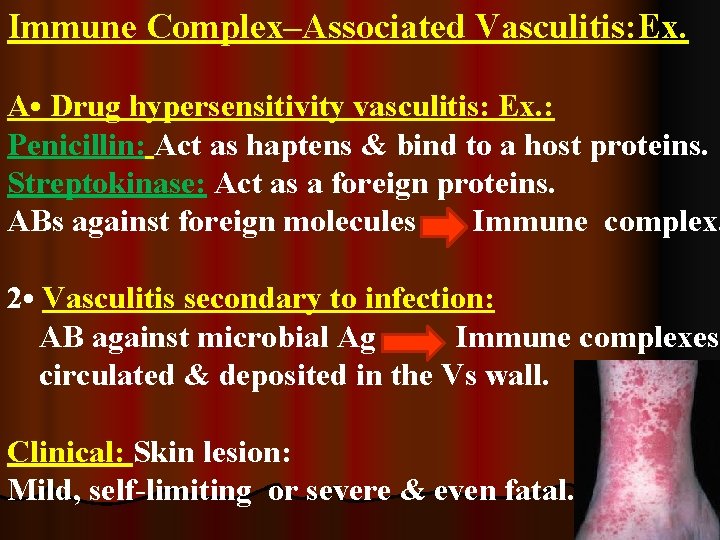
Immune Complex–Associated Vasculitis: Ex. A • Drug hypersensitivity vasculitis: Ex. : Penicillin: Act as haptens & bind to a host proteins. Streptokinase: Act as a foreign proteins. ABs against foreign molecules Immune complex. 2 • Vasculitis secondary to infection: AB against microbial Ag Immune complexes circulated & deposited in the Vs wall. Clinical: Skin lesion: Mild, self-limiting or severe & even fatal.
Anti-Neutrophil Cytoplasmic Antibodies: (ANCAs) Circulating auto-ABs react with Ags in neutrophil cytoplasm Endothelial cell injury. Mainly 2 enzymes represents ANCA: 1 • Antiproteinase-3 (PR 3 -ANCA): Wegener granulomatosis. 2 • Anti-myeloperoxidase (MPO-ANCA): Microscopic polyangiitis. Churg-Strauss syndrome.
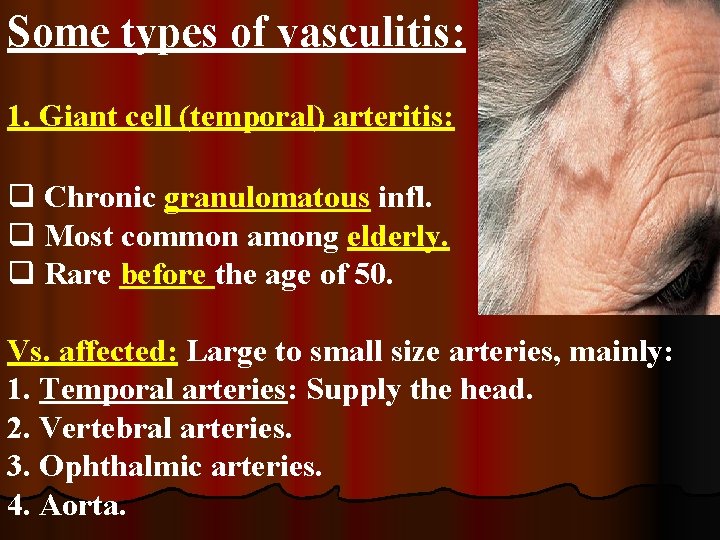
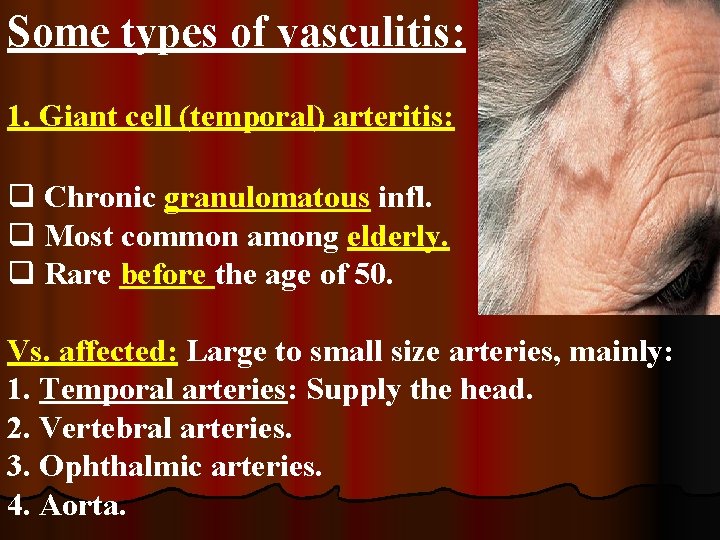
Some types of vasculitis: 1. Giant cell (temporal) arteritis: q Chronic granulomatous infl. q Most common among elderly. q Rare before the age of 50. Vs. affected: Large to small size arteries, mainly: 1. Temporal arteries: Supply the head. 2. Vertebral arteries. 3. Ophthalmic arteries. 4. Aorta.
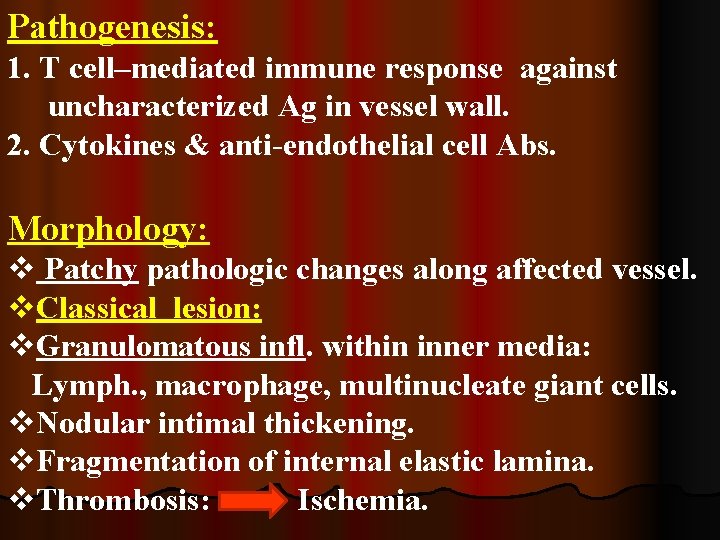
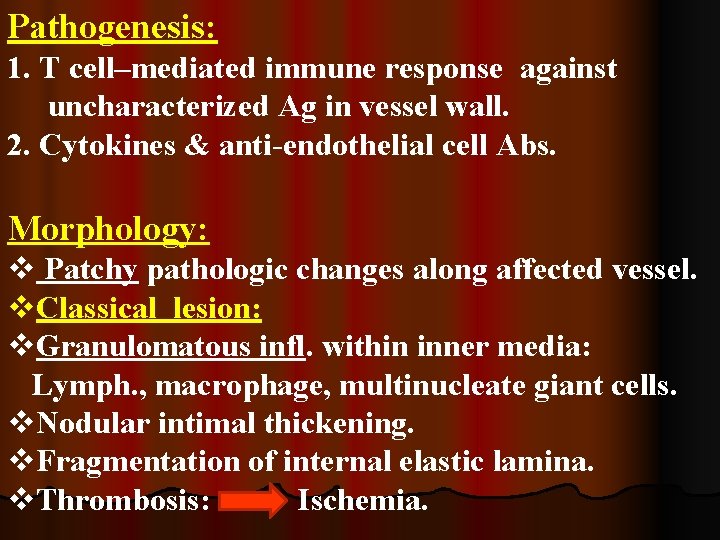
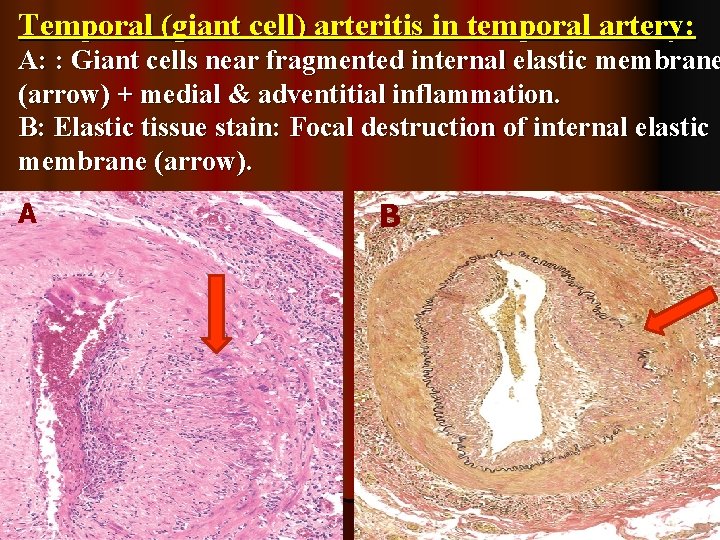
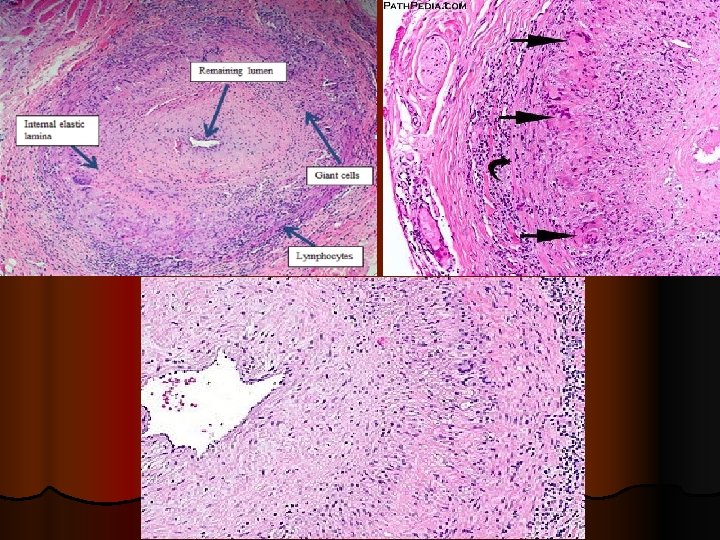
Pathogenesis: 1. T cell–mediated immune response against uncharacterized Ag in vessel wall. 2. Cytokines & anti-endothelial cell Abs. Morphology: v Patchy pathologic changes along affected vessel. v. Classical lesion: v. Granulomatous infl. within inner media: Lymph. , macrophage, multinucleate giant cells. v. Nodular intimal thickening. v. Fragmentation of internal elastic lamina. v. Thrombosis: Ischemia.
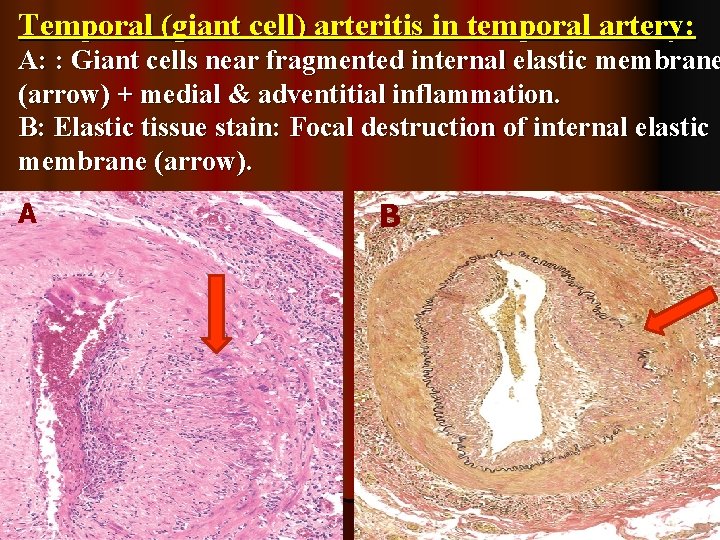
Temporal (giant cell) arteritis in temporal artery: A: : Giant cells near fragmented internal elastic membrane (arrow) + medial & adventitial inflammation. B: Elastic tissue stain: Focal destruction of internal elastic membrane (arrow). A B
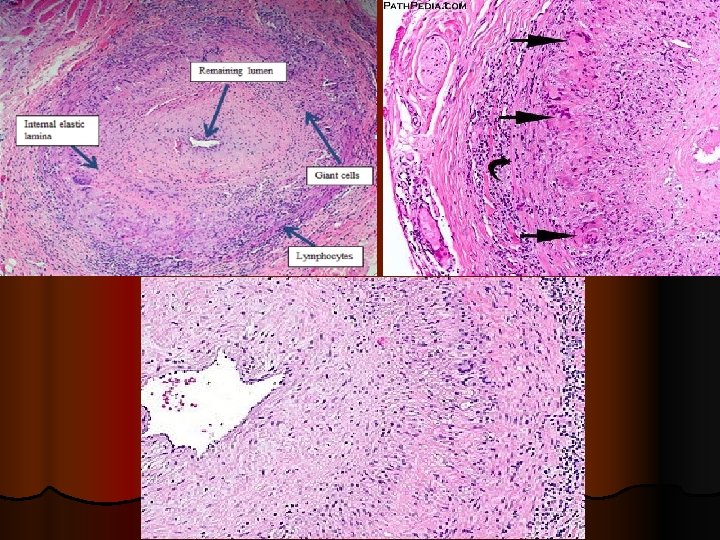
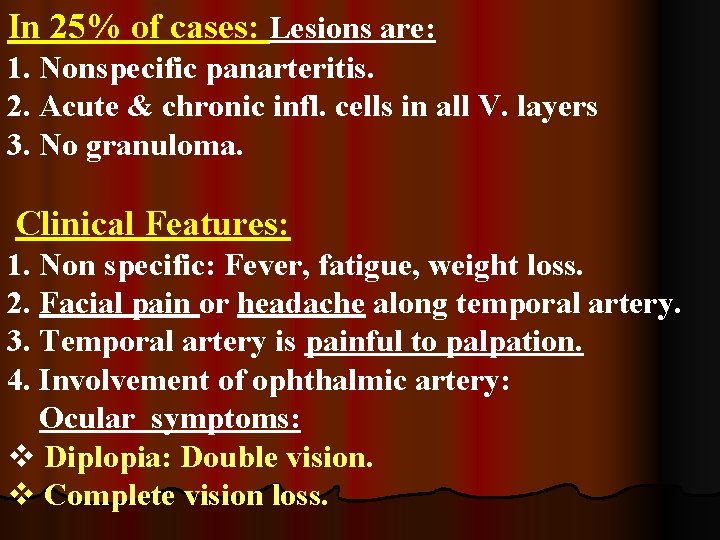
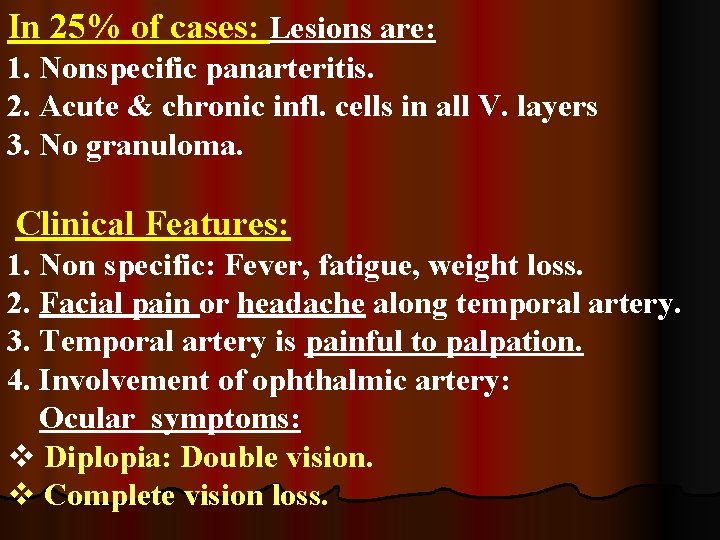
In 25% of cases: Lesions are: 1. Nonspecific panarteritis. 2. Acute & chronic infl. cells in all V. layers 3. No granuloma. Clinical Features: 1. Non specific: Fever, fatigue, weight loss. 2. Facial pain or headache along temporal artery. 3. Temporal artery is painful to palpation. 4. Involvement of ophthalmic artery: Ocular symptoms: v Diplopia: Double vision. v Complete vision loss.
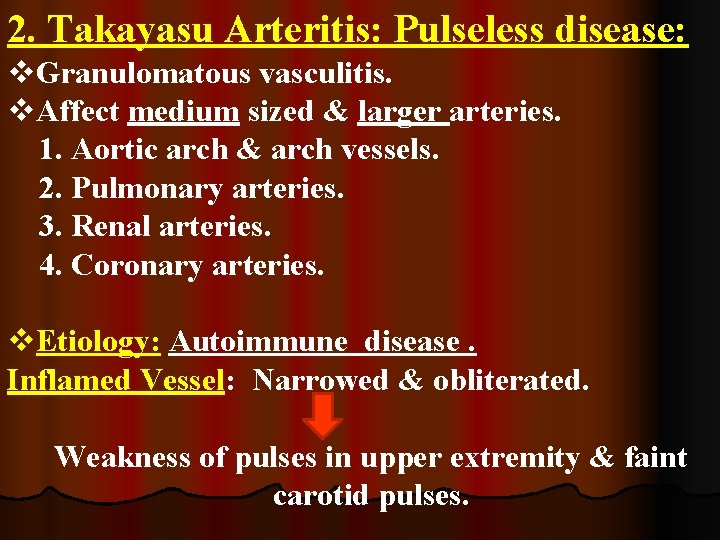
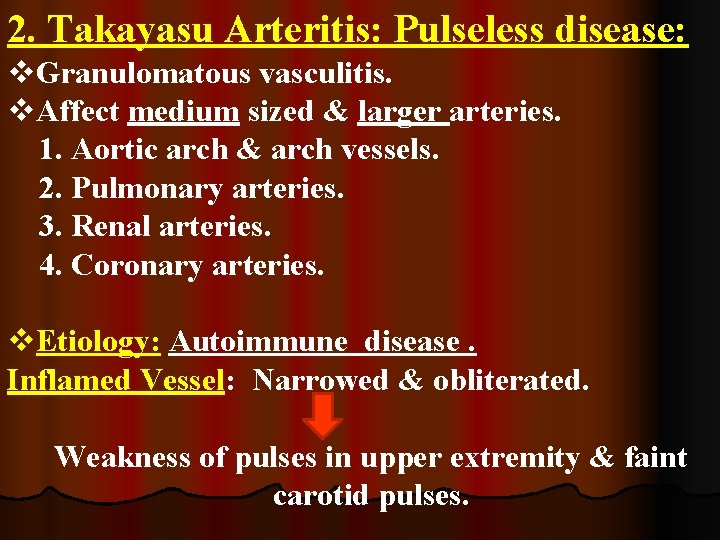
2. Takayasu Arteritis: Pulseless disease: v. Granulomatous vasculitis. v. Affect medium sized & larger arteries. 1. Aortic arch & arch vessels. 2. Pulmonary arteries. 3. Renal arteries. 4. Coronary arteries. v. Etiology: Autoimmune disease. Inflamed Vessel: Narrowed & obliterated. Weakness of pulses in upper extremity & faint carotid pulses.

Characteristic features: 1. Marked weakening of pulses in upper extremities (So named pulseless disease). 2. Ocular disturbances. 3. Transmural thickening & scarring of aorta. 4. Severe luminal narrowing of major branch vessel. Aortic lesions in Takayasu Arteritis & giant cell aortitis: Share many of clinical & histologic features. Distinction: Depends on patient’s age: v. Older than 50 year: Giant cell aortitis. v. Younger than 50 year: Takayasu aortitis.
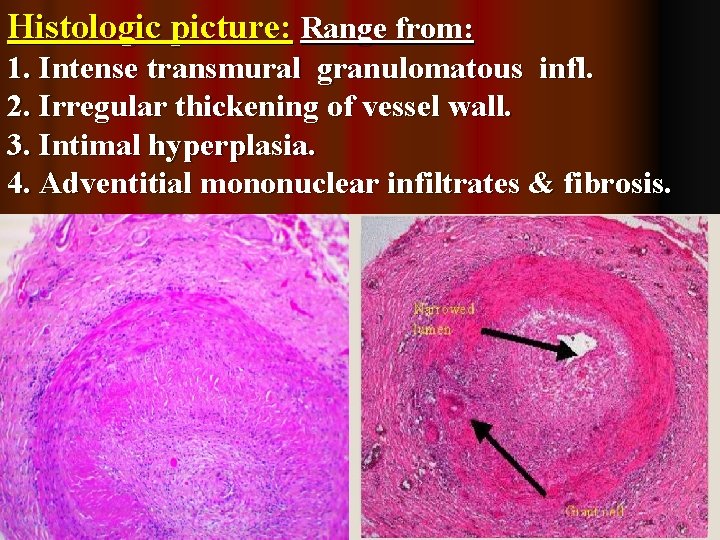
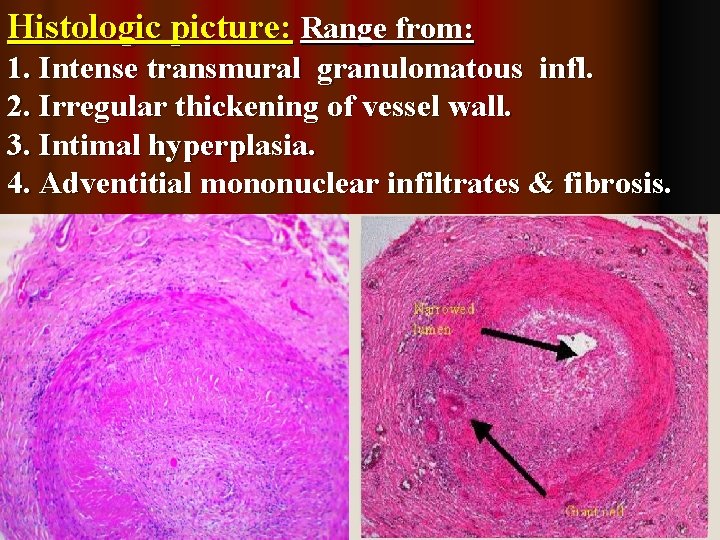
Histologic picture: Range from: 1. Intense transmural granulomatous infl. 2. Irregular thickening of vessel wall. 3. Intimal hyperplasia. 4. Adventitial mononuclear infiltrates & fibrosis.
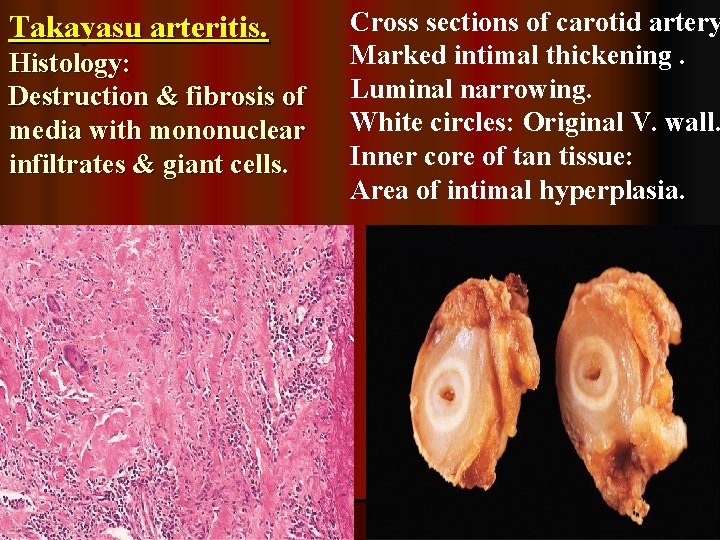
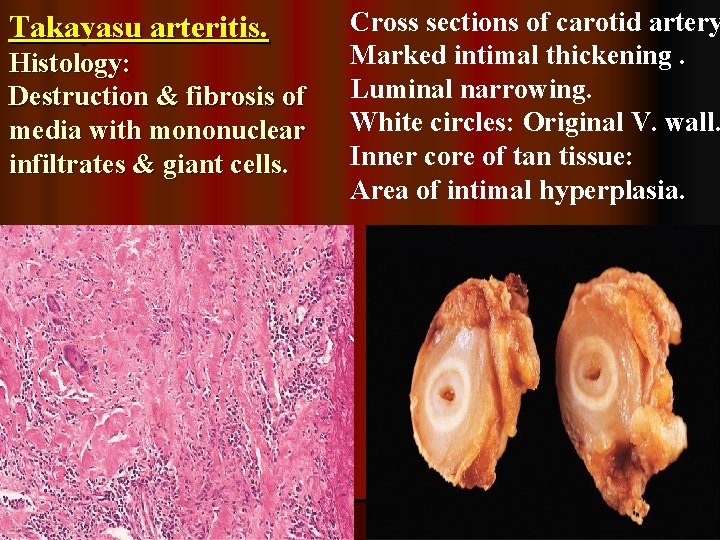
Takayasu arteritis. Histology: Destruction & fibrosis of media with mononuclear infiltrates & giant cells. Cross sections of carotid artery Marked intimal thickening. Luminal narrowing. White circles: Original V. wall. Inner core of tan tissue: Area of intimal hyperplasia.
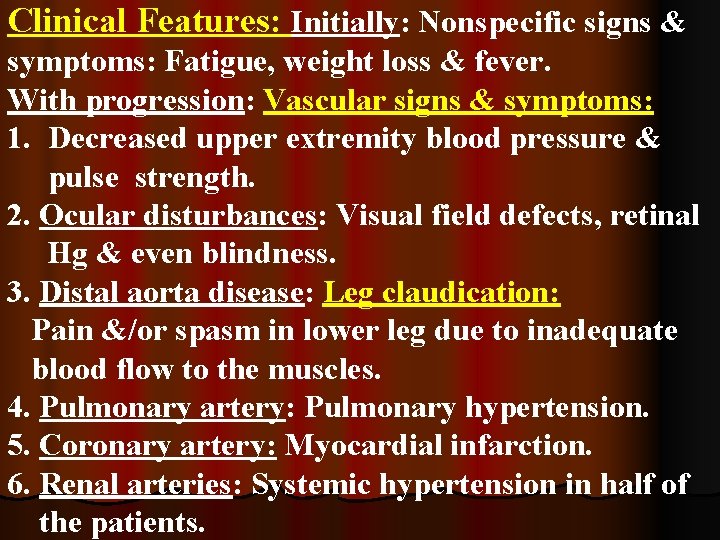
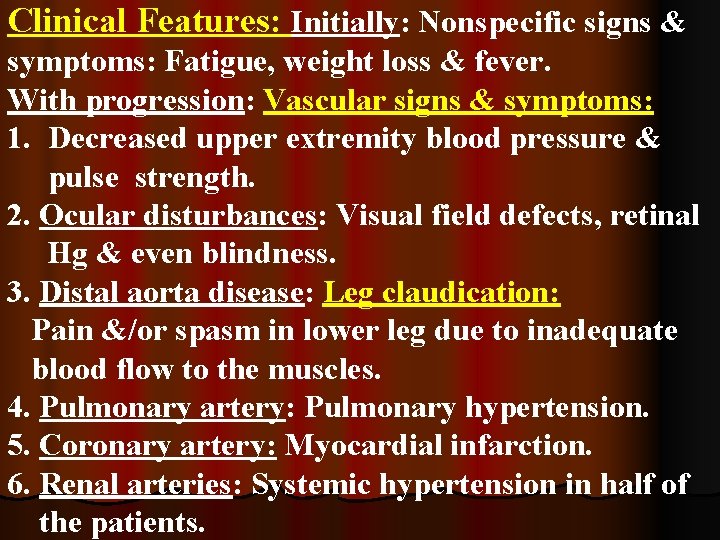
Clinical Features: Initially: Nonspecific signs & symptoms: Fatigue, weight loss & fever. With progression: Vascular signs & symptoms: 1. Decreased upper extremity blood pressure & pulse strength. 2. Ocular disturbances: Visual field defects, retinal Hg & even blindness. 3. Distal aorta disease: Leg claudication: Pain &/or spasm in lower leg due to inadequate blood flow to the muscles. 4. Pulmonary artery: Pulmonary hypertension. 5. Coronary artery: Myocardial infarction. 6. Renal arteries: Systemic hypertension in half of the patients.
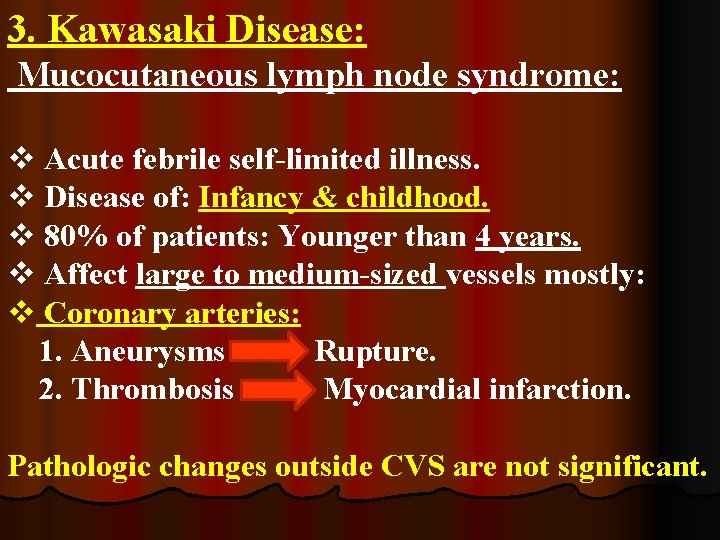
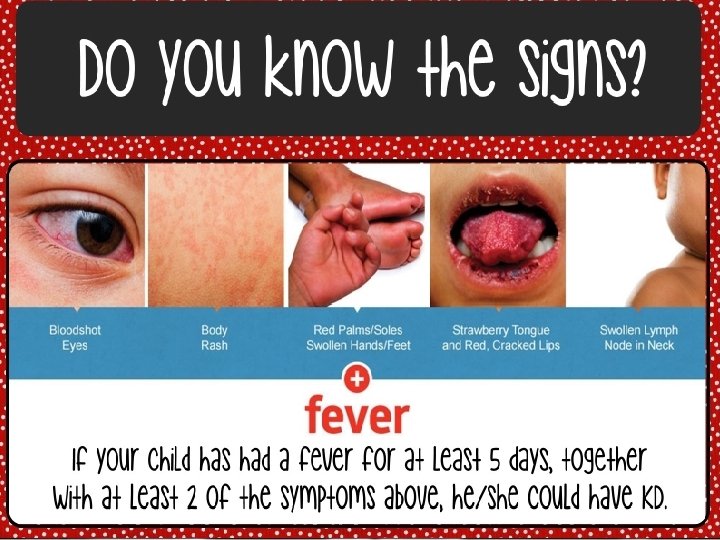
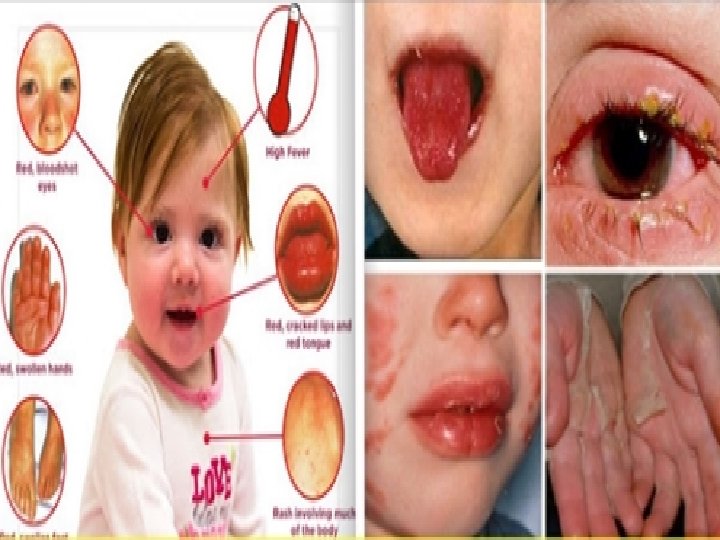
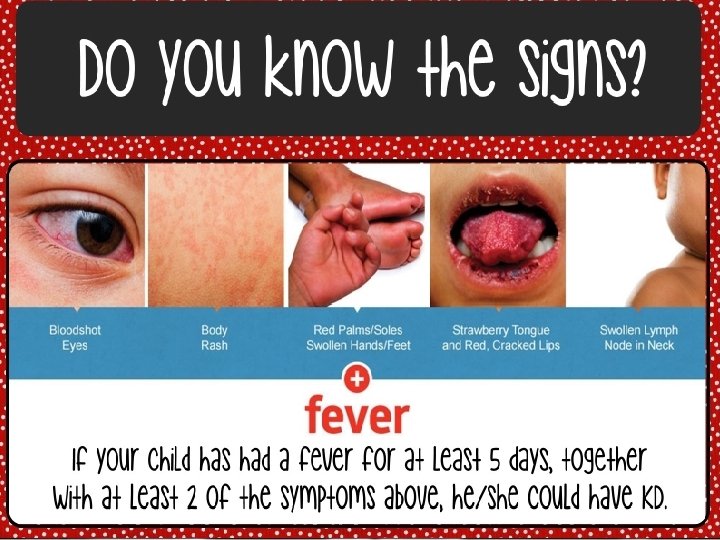
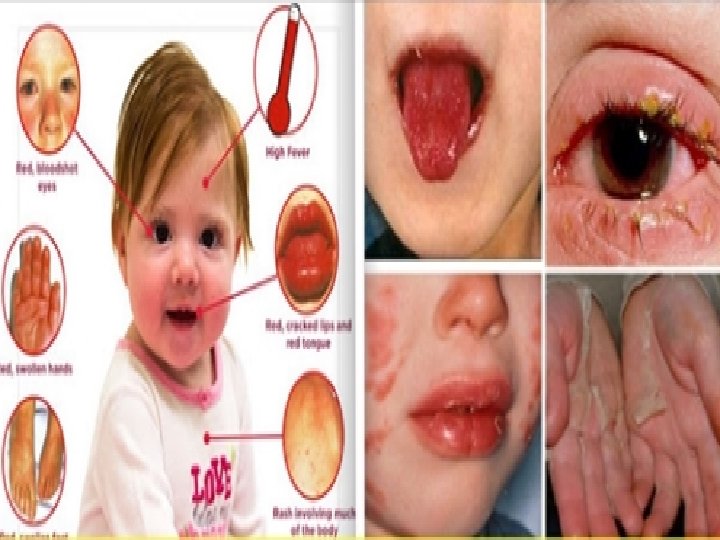
3. Kawasaki Disease: Mucocutaneous lymph node syndrome: v Acute febrile self-limited illness. v Disease of: Infancy & childhood. v 80% of patients: Younger than 4 years. v Affect large to medium-sized vessels mostly: v Coronary arteries: 1. Aneurysms Rupture. 2. Thrombosis Myocardial infarction. Pathologic changes outside CVS are not significant.
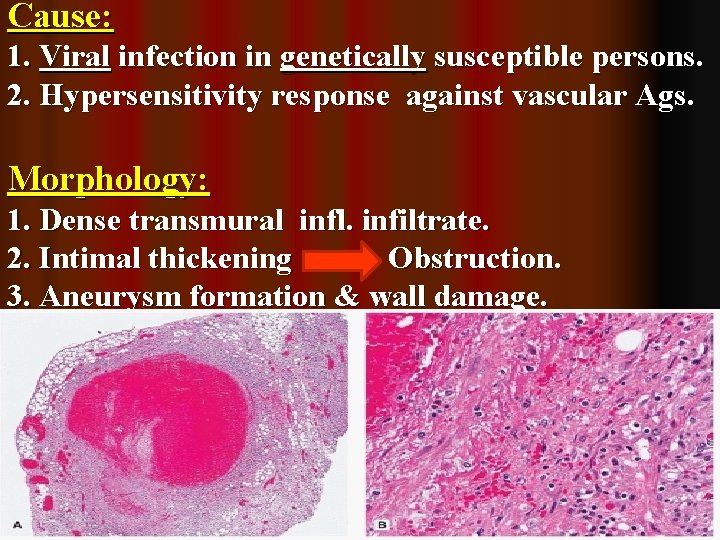
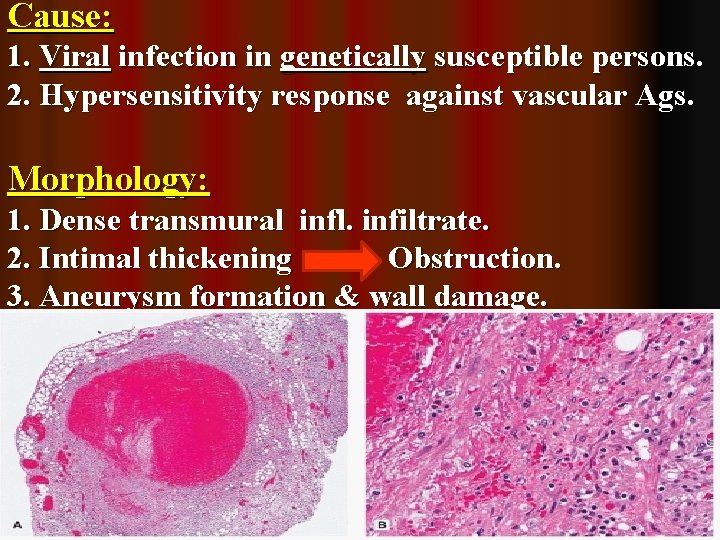
Cause: 1. Viral infection in genetically susceptible persons. 2. Hypersensitivity response against vascular Ags. Morphology: 1. Dense transmural infl. infiltrate. 2. Intimal thickening Obstruction. 3. Aneurysm formation & wall damage.
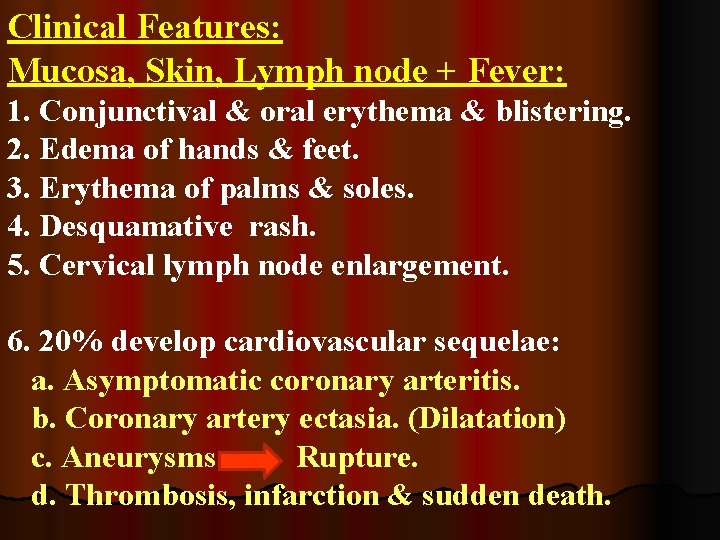
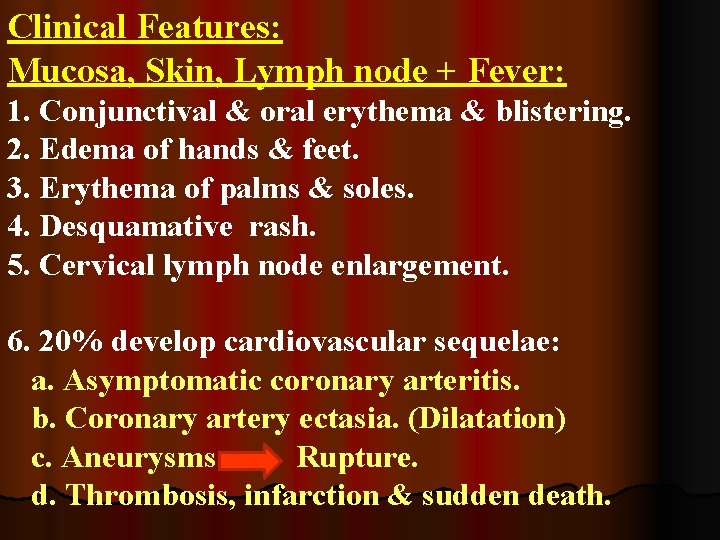
Clinical Features: Mucosa, Skin, Lymph node + Fever: 1. Conjunctival & oral erythema & blistering. 2. Edema of hands & feet. 3. Erythema of palms & soles. 4. Desquamative rash. 5. Cervical lymph node enlargement. 6. 20% develop cardiovascular sequelae: a. Asymptomatic coronary arteritis. b. Coronary artery ectasia. (Dilatation) c. Aneurysms Rupture. d. Thrombosis, infarction & sudden death.
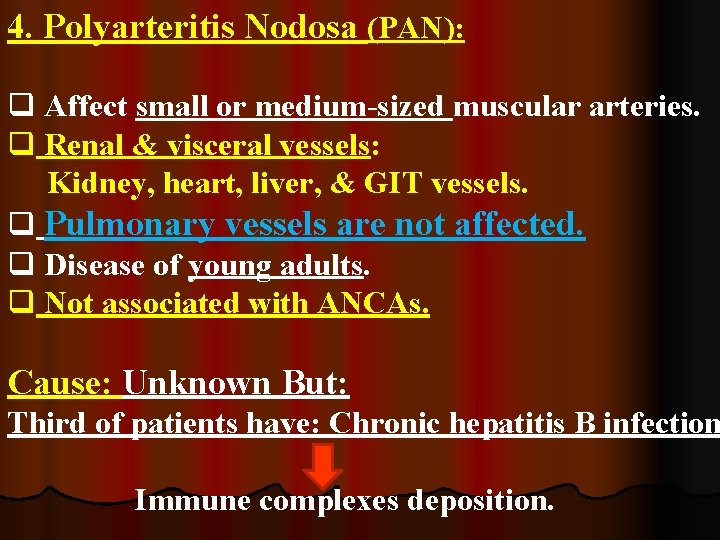
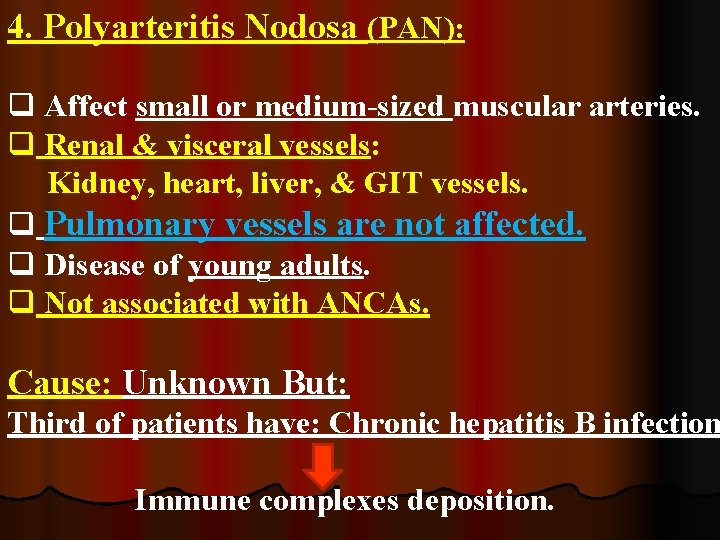
4. Polyarteritis Nodosa (PAN): q Affect small or medium-sized muscular arteries. q Renal & visceral vessels: Kidney, heart, liver, & GIT vessels. q Pulmonary vessels are not affected. q Disease of young adults. q Not associated with ANCAs. Cause: Unknown But: Third of patients have: Chronic hepatitis B infection Immune complexes deposition.
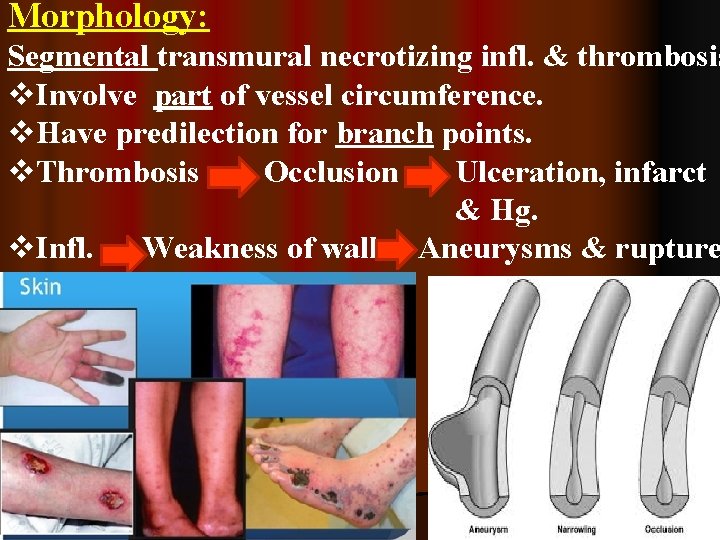
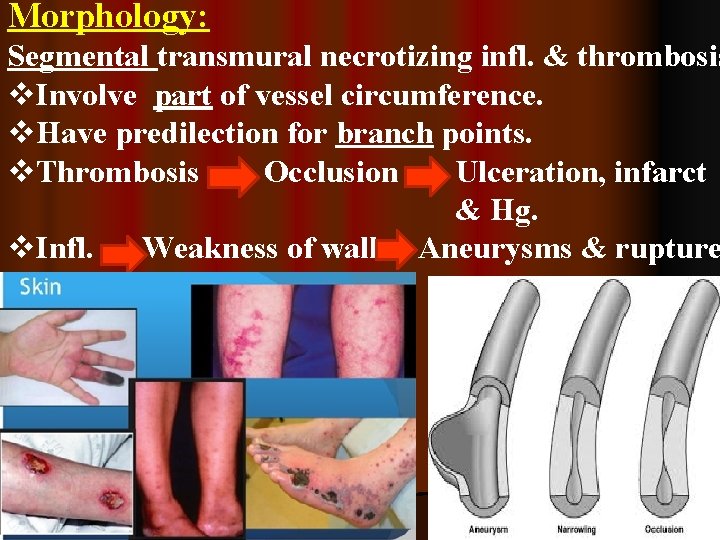
Morphology: Segmental transmural necrotizing infl. & thrombosis v. Involve part of vessel circumference. v. Have predilection for branch points. v. Thrombosis Occlusion Ulceration, infarct & Hg. v. Infl. Weakness of wall Aneurysms & rupture
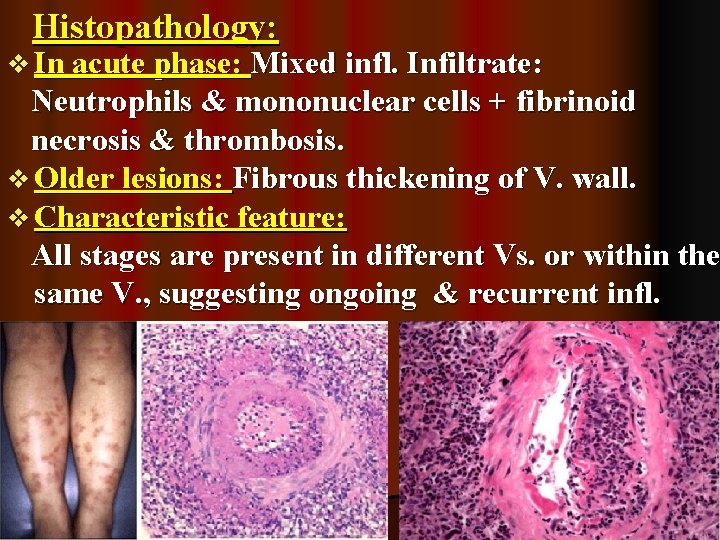
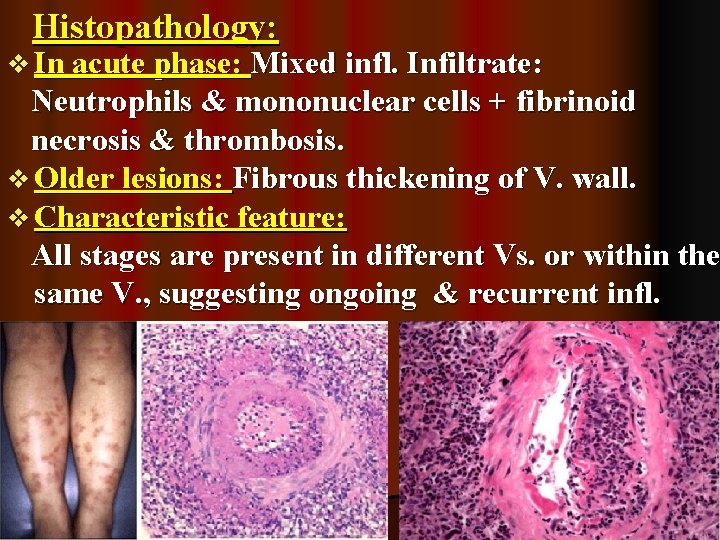
Histopathology: v In acute phase: Mixed infl. Infiltrate: Neutrophils & mononuclear cells + fibrinoid necrosis & thrombosis. v Older lesions: Fibrous thickening of V. wall. v Characteristic feature: All stages are present in different Vs. or within the same V. , suggesting ongoing & recurrent infl.
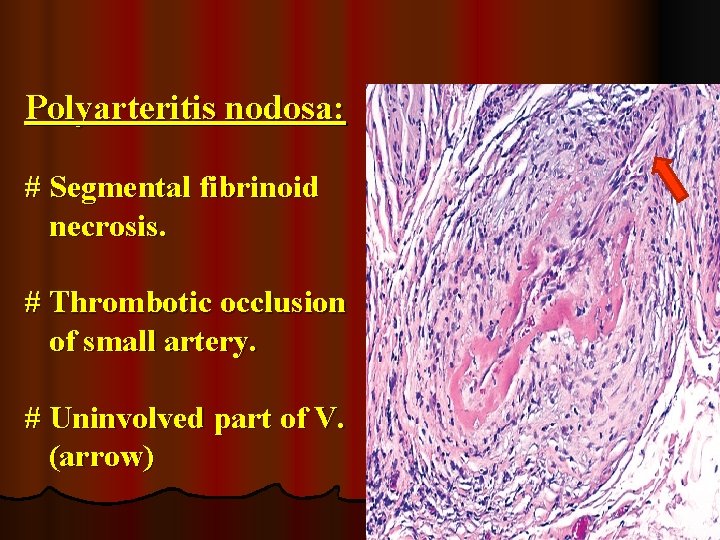
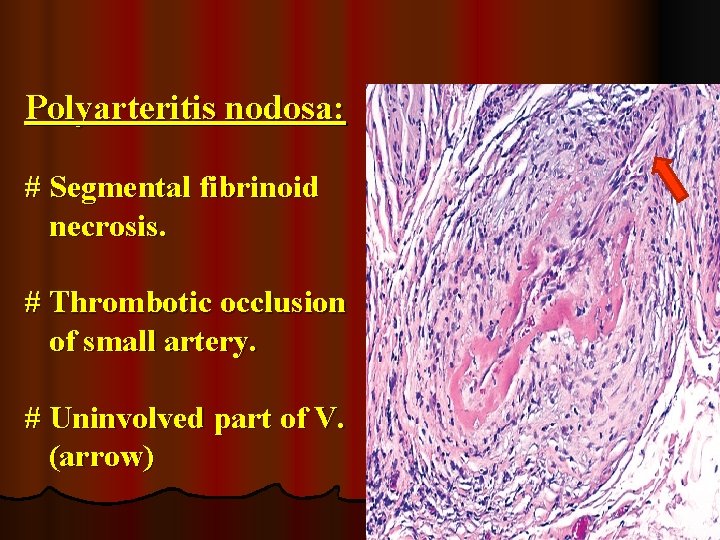
Polyarteritis nodosa: # Segmental fibrinoid necrosis. # Thrombotic occlusion of small artery. # Uninvolved part of V. (arrow)
Clinical Features of PAN: Range from: Acute to chronic inflammation. Typically: Episodic with long symptom-free intervals Systemic findings: Nonspecific. Vessels involvement: Classical presentation: 1. Renal artery: Rapidly accelerating hypertension Death. 2. GIT V. : Abdominal pain & bloody stools. 3. Muscular V. : Diffuse muscular pains. 4. Motor nerves: Peripheral neuritis. 5. Skin: Hg. & ulceration. (Patients have combination of these symptoms)
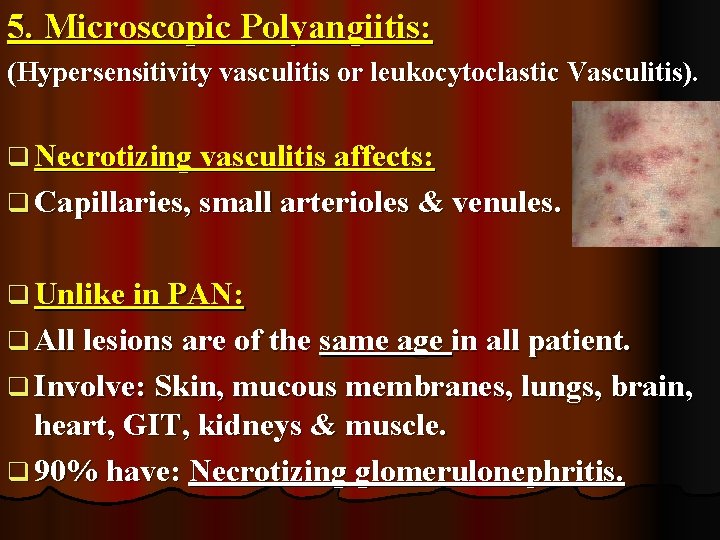
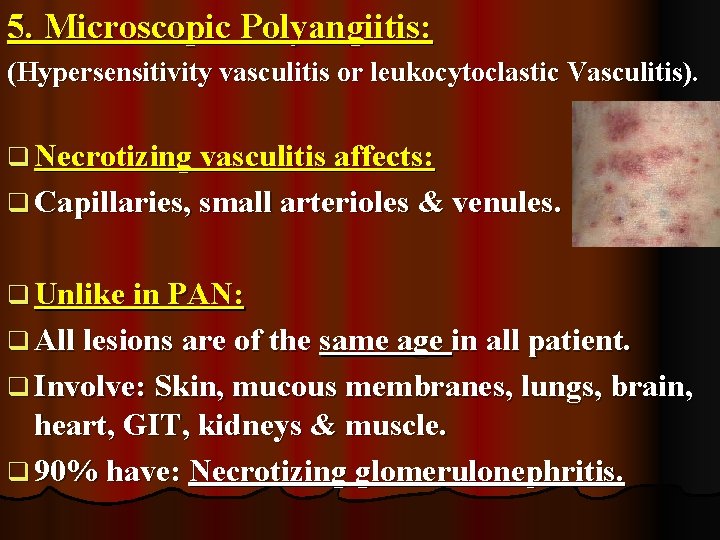
5. Microscopic Polyangiitis: (Hypersensitivity vasculitis or leukocytoclastic Vasculitis). q Necrotizing vasculitis affects: q Capillaries, small arterioles & venules. q Unlike in PAN: q All lesions are of the same age in all patient. q Involve: Skin, mucous membranes, lungs, brain, heart, GIT, kidneys & muscle. q 90% have: Necrotizing glomerulonephritis.
Cause: 1. It can be a feature of other immune disease. 2. AB-Ags reaction: Drugs (penicillin). Microorganisms (streptococci). Immune complex Deposition Or Trigger secondary immune responses: e. g. : Development of MPO ANCAs. (Most cases) Disease manifestations occurs due to: Recruitment & activation of neutrophils.
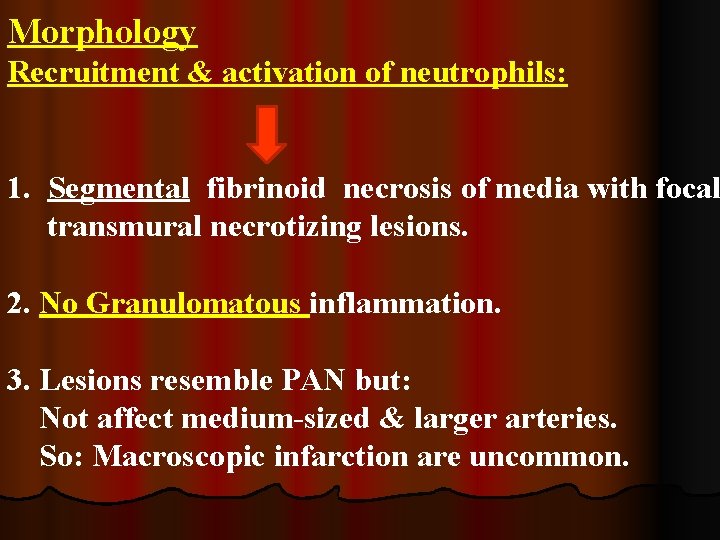
Morphology Recruitment & activation of neutrophils: 1. Segmental fibrinoid necrosis of media with focal transmural necrotizing lesions. 2. No Granulomatous inflammation. 3. Lesions resemble PAN but: Not affect medium-sized & larger arteries. So: Macroscopic infarction are uncommon.
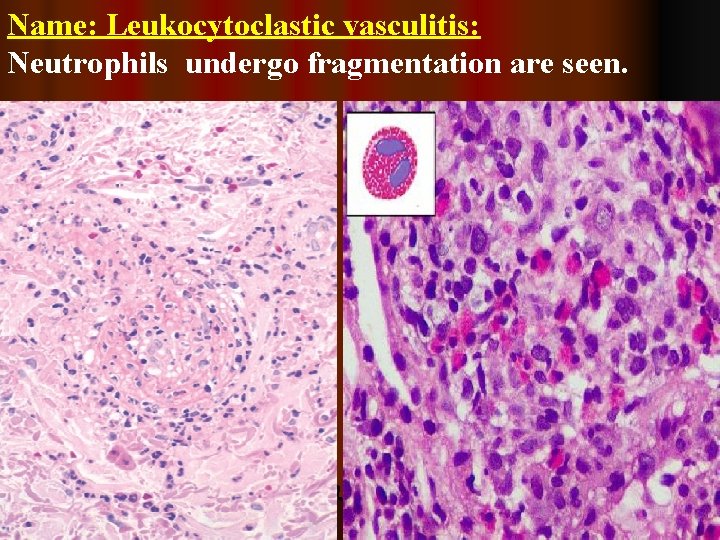
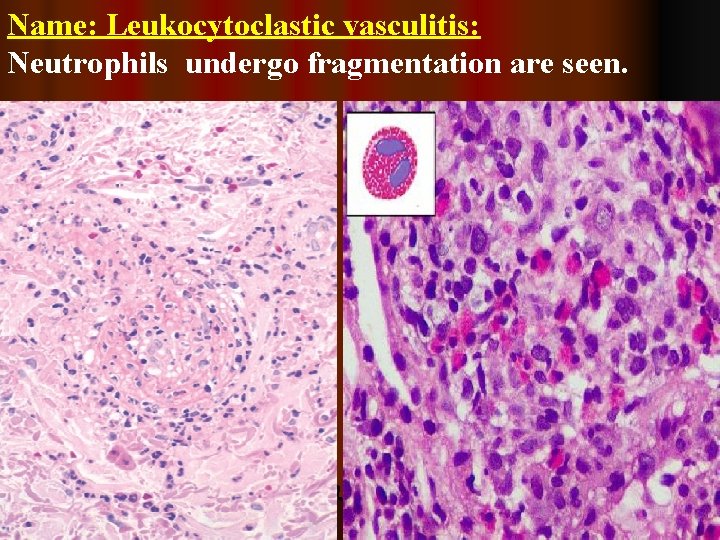
Name: Leukocytoclastic vasculitis: Neutrophils undergo fragmentation are seen.
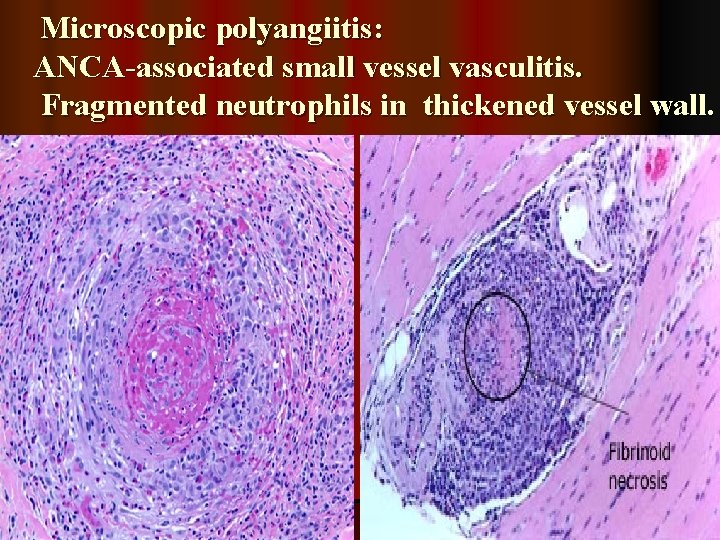
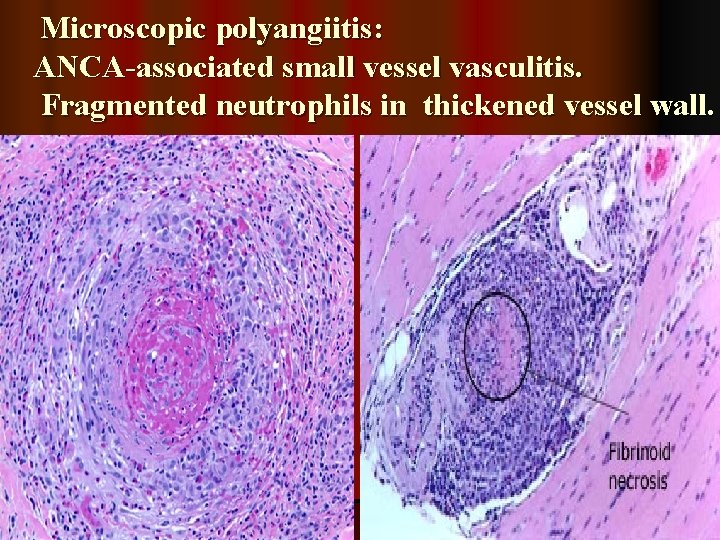
Microscopic polyangiitis: ANCA-associated small vessel vasculitis. Fragmented neutrophils in thickened vessel wall.
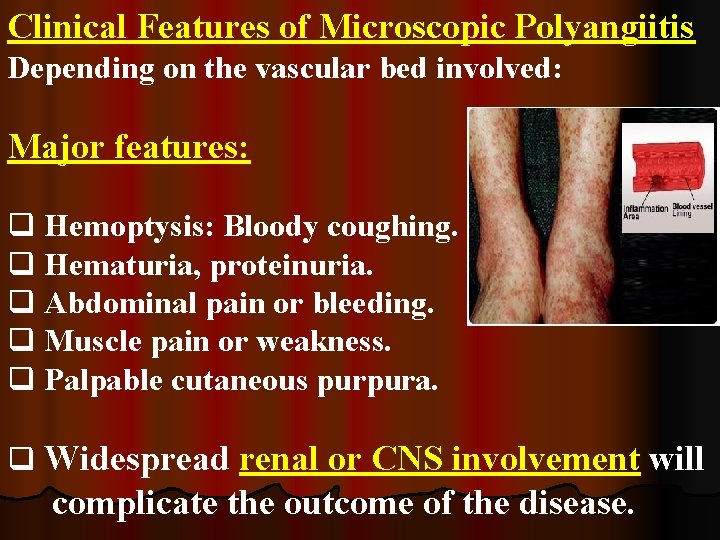
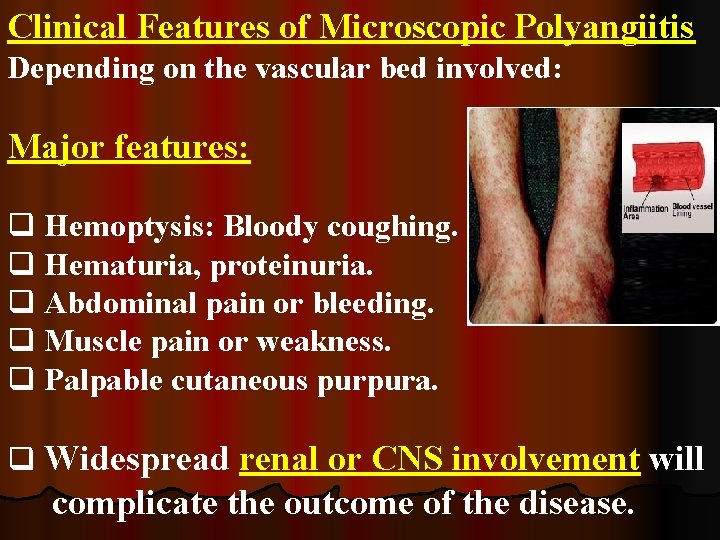
Clinical Features of Microscopic Polyangiitis Depending on the vascular bed involved: Major features: q Hemoptysis: Bloody coughing. q Hematuria, proteinuria. q Abdominal pain or bleeding. q Muscle pain or weakness. q Palpable cutaneous purpura. q Widespread renal or CNS involvement will complicate the outcome of the disease.
THANK YOU