Cutaneous Fungal Infections DR NOUF TALAL MILEH DERMATOLOGY





- Slides: 61
Cutaneous Fungal Infections DR. NOUF TALAL MILEH DERMATOLOGY DEMONSTRATOR
Cutaneous Fungal Infections o Dermatomycosis - general name for any skin disease caused by a fungus. o Dermatophytosis - "ringworm" disease of the nails, hair, and/or stratum corneum of the skin caused by fungi called dermatophytes.
Cutaneous Fungal Infections �Etiological agents are called dermatophytes. �Three important anamorphic genera are involved in ringworm. 1)Microsporum. 2)Trichophyton. 3) Epidermophyton.
Cutaneous Fungal Infections �Dermatophytes are keratinophilic - "keratin loving". Digest keratin by their keratinases � Keratin is a major protein found in horns, hooves, nails, hair, and skin. �Ringworm - disease called ‘herpes' by the Greeks, and by the Romans ‘tinea' (which means small insect larvae).
DERMATOPHYTES �Classified into three groups depending on their usual habitat ANTROPOPHILIC keratin-utilizing on hosts - humans (e. g. , M. audounii, T. tonsurans, Trichophyton rubrum ) GEOPHILIC keratin-utilizing soil saprophytes (e. g. , M. gypseum…). ZOOPHILIC keratin-utilizing on hosts - living animals (e. g. , M. canis, T. verrucosum).
DERMATOPHYTOSIS Pathogenesis and Immunity �Contact and trauma. �Moisture. �Crowded living conditions. �Cellular immunodeficiency (chronic inf. ). �Re-infection is possible (but, larger inoculum is needed, the course is shorter ).
Major sources of ringworm infection �Schools, military camps, prisons. �Warm damp areas (e. g. , tropics, moisture accumulation in clothing and shoes). �Animals (e. g. , dogs, cattle, poultry, etc. ). �Historical note: More people were shipped out of the Pacific Theater in WWII back to U. S. because of ringworm infection then through injury.
Transmission �Close human contact. �Sharing clothes, combs, brushes, towels, bedsheets. . . (fomites). �Animal-to-human contact (Zoophilic).
DERMATOPHYTOSIS Clinical Classification Infection is named according to the anatomic location involved: �Tinea capitis - ringworm infection of the head, scalp, eyebrows, eyelashes. �Tinea facialis - of the face. �Tinea corporis - of the body. �Tinea cruris - of the groin (jock itch). �Tinea unguium - of the nails. �Tinea barbae - of the beard. �Tinea manuum - of the hand. �Tinea pedis - of the foot (athlete's foot).
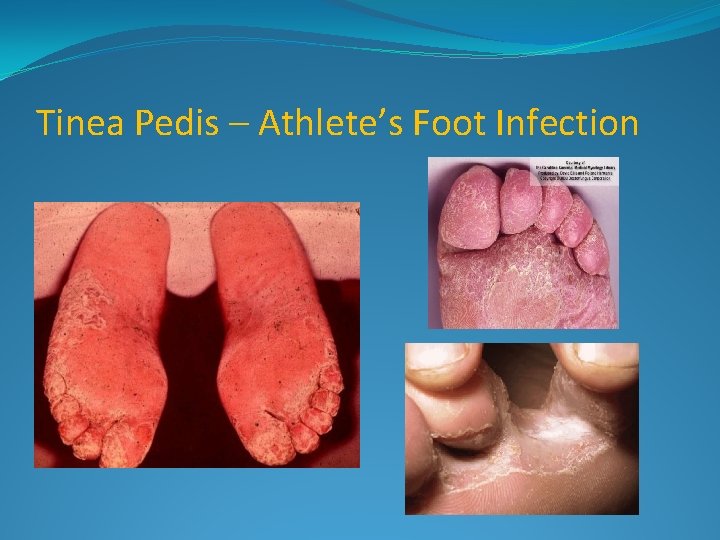
CLINICAL MANIFESTATIONS OF RINGWORM Tinea pedis - Athletes' foot infection �Between toes or toe webs (releasing of clear fluid) - 4 th and 5 th toes are most common, sole. �Commonly, patients describe pruritic, scaly soles and, often, painful fissures between the toes. � Most frequently due to: - Trichophyton (T. ) rubrum - T. interdigitale, previously called T. mentagrophytes var. interdigitale - Epidermophyton floccosum
Tinea pedis - Athletes' foot infection � 3 possible clinical presentations: ( Interdigital, Chronic hyperkeratotic (moccasin) Inflammatory or vesiculobullous ) �Allergic reactions are sometimes associated with tinea pedis and other ringworm infections.
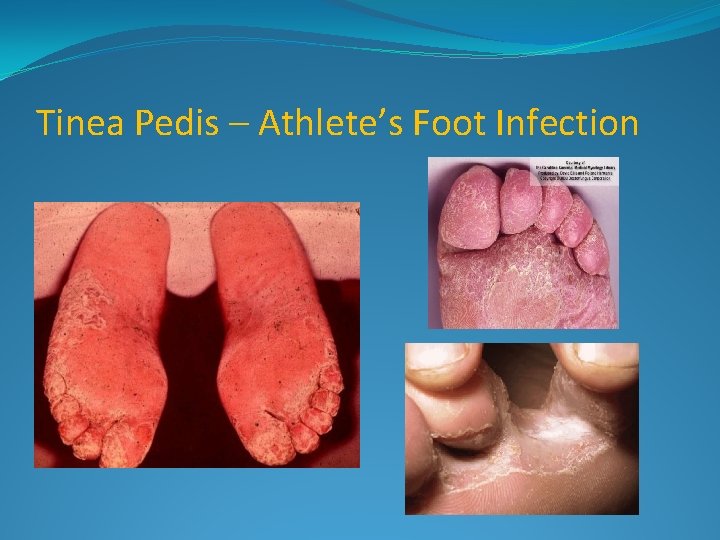
Tinea Pedis – Athlete’s Foot Infection

Dermatophytid Reaction
Tinea corporis - body ringworm �Generally restricted to stratum corneum of the smooth skin. �Symptoms result form fungi metabolites such as toxin/allergens. �Produces concentric or ring-like lesions on skin (annular plaques), and in severe cases these are raised and may become inflamed.
Tinea corporis - body ringworm �All forms of tinea corporis caused by T. rubrum, T. mentagrophytes, T. tonsurans, M. canis, and M. audouinii are treatable with topical agent containing ketoconazole, miconazole, etc. . . �Widespread tinea corporis and more severe types (lesions) require systemic griseofulvin treatment (about 6 weeks for effective treatment).

Tinea corporis – body ringworm
Tinea cruris - ringworm of the groin and surrounding region �More common in men than women. �Infection seen on scrotum and inner thigh, the penis is usually not infected. �Several causes of tinea cruris include T. rubrum , E. flocossum. �Predisposing factors include persistent perspiration, high humidity, tight clothing , diabetes and obesity, topical glucocorticoid application.
Tinea cruris - ringworm of the groin and surrounding region �Symptom: none, prurits. �Signs: large, scaling well demarcated red / tan/ brown/ plaques. �Diagnosis �If lesion "weep", it is likely caused by a yeast, such as, Candida albicans, and not by a dermatophyte, especially if infections are seen in a woman.

Tinea Cruris – Jock Itch
Tinea unguium - ringworm of the nails Tinea unguium or onychomycosis can take 4 forms : �Distal subungual onychomycosis �Proximal subungual onychomycosis �Superficial white onychomycosis �Candidal onychomycosis
Tinea unguium - ringworm of the nails �Most commonly caused by T. rubrum, then E. floccosum or other Trichophyton species. �Resistant to treatment, rarely resolves spontaneously.
Tinea unguium - ringworm of the nails �Topical treatments - poor record of cure. �If the disease involve one or two nails loceryl nail loquer ( amorolfiene ). �If the disease involve multable nails lamfine (terbinafine) 250 mg (6 w for fingure nail, 12 w for toe nail ) �Systemic griseofulvin therapy can lead to remission.

Tinea Unguium – Nail Infection
Tinea facialis �Dermatophytosis of the glabrous facial skin. �More common in children. �Etiology : T. tonsurans , T. rubrum, T. mentagrophytes , M. audouinii, M. canis. �Predisposing factors : animal exposure, topical application of glucocorticoid. �Symptoms : asymptomatic �Characterized by a well-circumscribed erythematous patch, minimal scaling.
Tinea Barbae �Involving the beard and moustache areas. �Males only, adult. �Etiology : T. verrucosum, T. mentagrophytes. �Predisposing factors : more common in farmers. �Symptoms : pruritus, tenderness, pain. �Signs : scattered, discrete follicular pustules and papules. �D. D. : Beard folliculitis ( s. aures ) �Treatment : see tinea capitis.
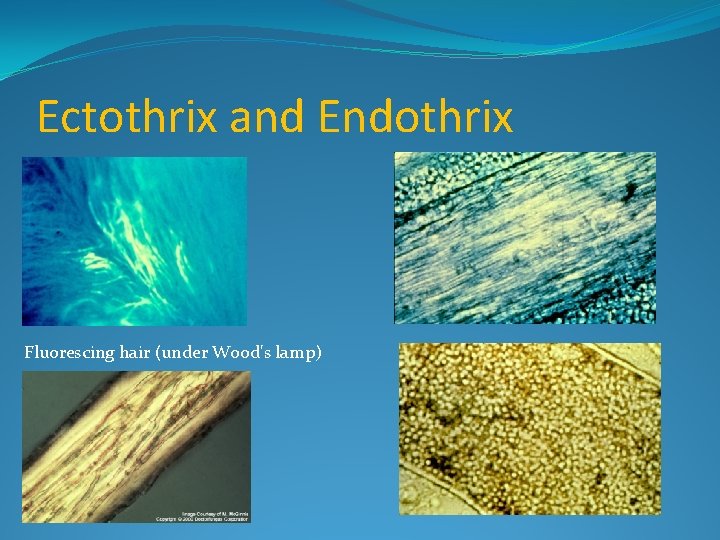
Tinea capitis - ringworm of the scalp, eyebrows and eyelashes �Predominantly a disease of preadolescent children �Caused by species of Microsporum and Trichophyton. �Fungus grows into hair follicle. �Using a Wood's lamp, on hair Microsporum species tend to fluoresce green while Trichophyton species generally do not fluoresce. �Lack of fluorescence does not mean it isn't Microsporum.
Tinea capitis �classified according to the microscopic pattern of fungal invasion as endothrix, ectothrix, and favus. Endothrix : �Fungi invade the inside of the hair shaft. �composed of fungal arthroconidie and hyphae, without cuticle destruction. �The causative organisms TVS.
Tinea capitis Ectothrix : �Fungi invade the outside of the hair shfat. �The process of ectothrix invasion is similar to endothrix invasion, with the exception that the hyphae destroy the hair cuticle, then convert into infectious arthroconidia. �The causative organisms are M. audouinii, M. canis, M distortum, T. ferrugineum. All these organisms cause fluorescence under Wood light. ( to remamber, SEE CATS AND DOGS FIGHT)
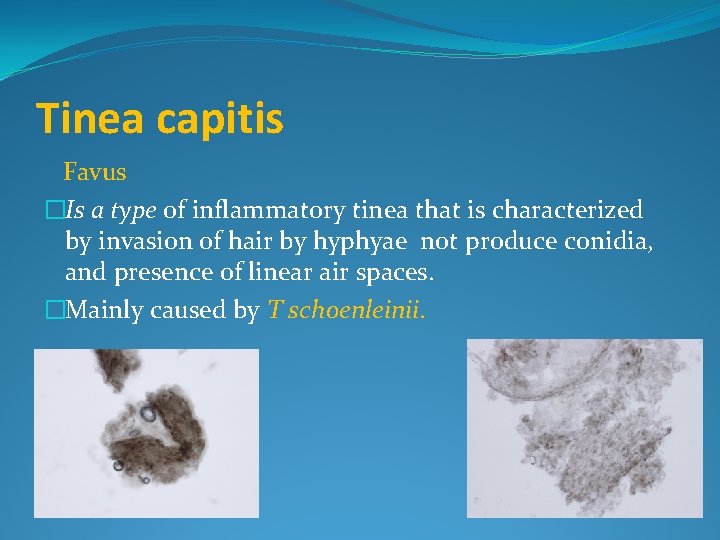
Tinea capitis Favus �Is a type of inflammatory tinea that is characterized by invasion of hair by hyphyae not produce conidia, and presence of linear air spaces. �Mainly caused by T schoenleinii.
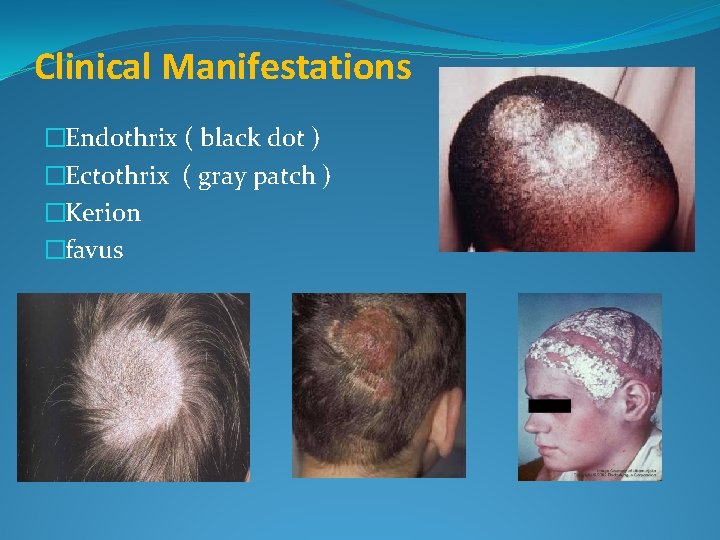
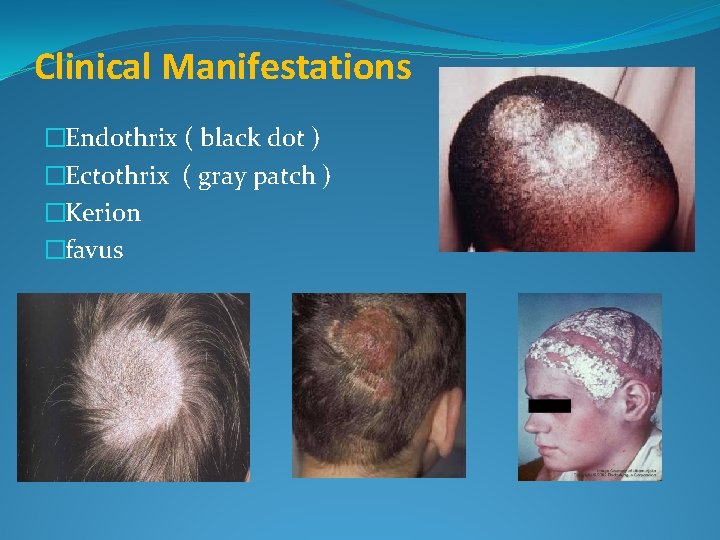
Clinical Manifestations �Endothrix ( black dot ) �Ectothrix ( gray patch ) �Kerion �favus
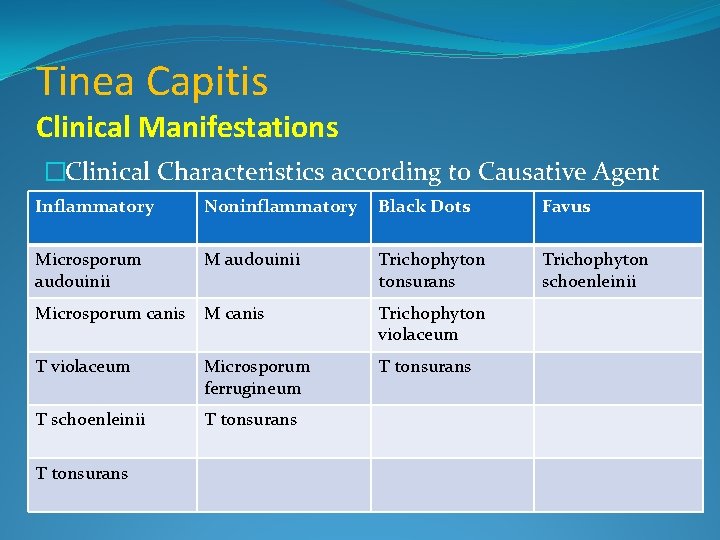
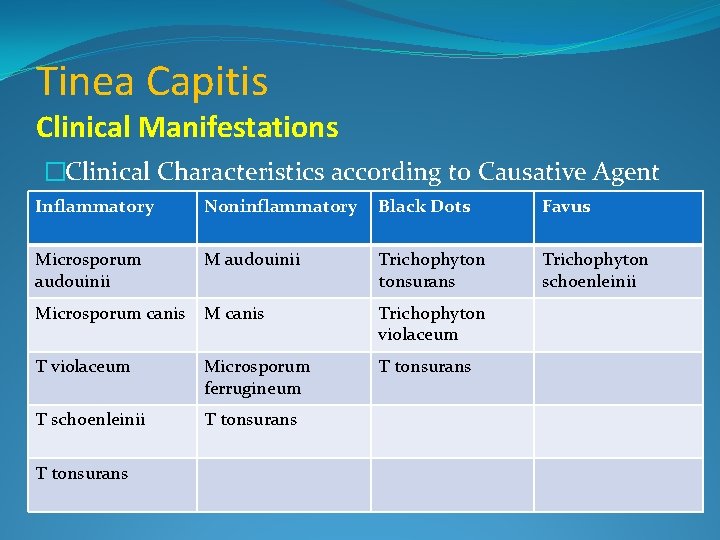
Tinea Capitis Clinical Manifestations �Clinical Characteristics according to Causative Agent Inflammatory Noninflammatory Black Dots Favus Microsporum audouinii M audouinii Trichophyton tonsurans Trichophyton schoenleinii Microsporum canis M canis Trichophyton violaceum T violaceum Microsporum ferrugineum T tonsurans T schoenleinii T tonsurans
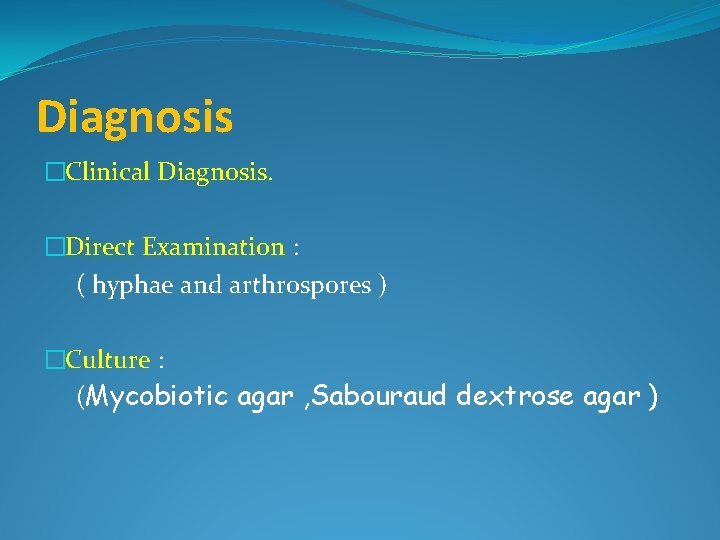
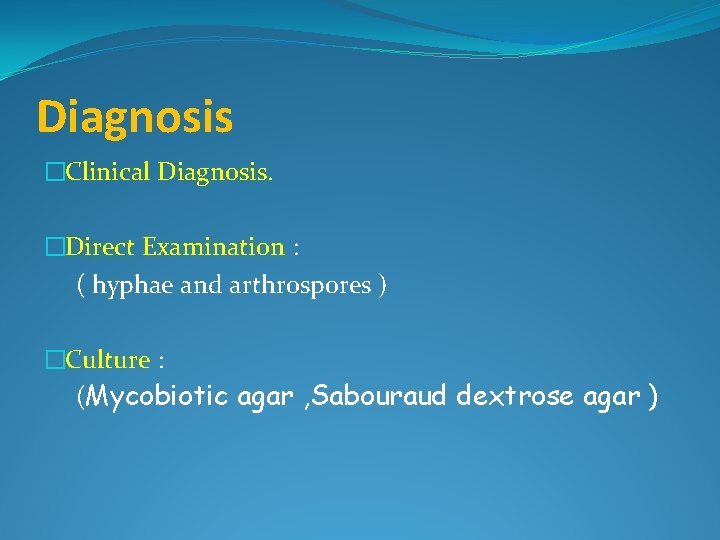
Diagnosis �Clinical Diagnosis. �Direct Examination : ( hyphae and arthrospores ) �Culture : (Mycobiotic agar , Sabouraud dextrose agar )
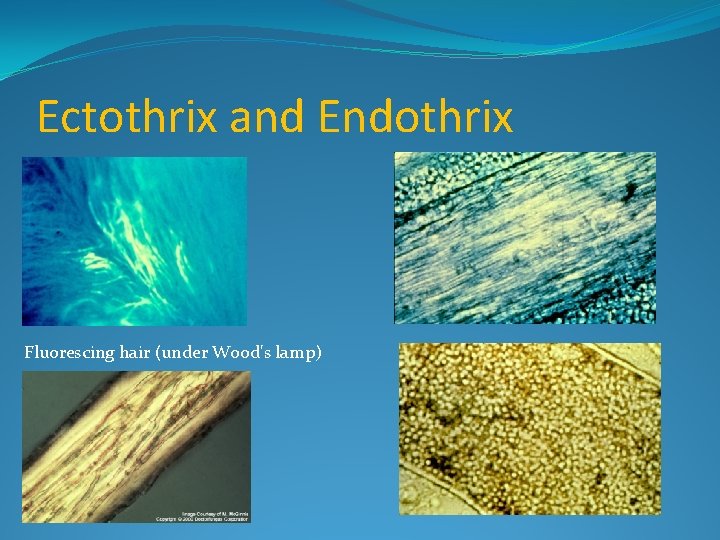
Ectothrix and Endothrix Fluorescing hair (under Wood's lamp)
Diagnosis �Immunologic Study : ( type I response and a delayed type IV response ) �Histopathology : ( growth of hyphae and formation of arthroconidia )
Rapid identification and differentiation of fungal DNA in dermatological specimens by Light. Cycler PCR Ralf Gutzmer, Susanne Mommert, Uta Ku¨ ttler, Thomas Werfel and Alexander Kapp �In conclusion, we developed a fast and simple Light. Cyclerbased PCR to detect DNA of the dermatologically most relevant fungi and to differentiate dermatophytes, yeasts and nondermatophyte moulds. �This can complement mycological culture and direct microscopy in the diagnosis of fungal skin disease and provides additional diagnostic information in a substantial number of patients. Journal of Medical Microbiology (2004), 53, 1207– 1214 ormation in a substantial number of patients
Differential Diagnosis According to Clinical Presentation �Diffuse scaling (noninflammatory) : Seborrheic and atopic dermatitis, psoriasis. �Alopecia plaque (noninflammatory) : Seborrheic and atopic dermatitis, psoriasis. �Black dots : Alopecia areata, trichotillomania. �Diffuse pustular (inflammatory) : Bacterial folliculitis �kerion celsi (inflammatory): Abscess, tumor.
Treatment Topical Treatment : �Shampoo containing 2% selenium sulfide. �shampoos containing 2% ketoconazole. �Topical antifungal cream : ketoconazole (nezoral), micinazole ( daktarin)
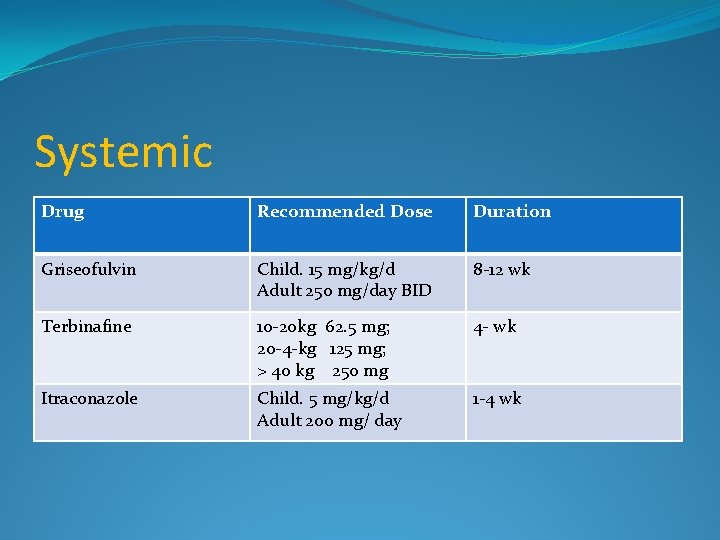
Oral Griseofulvin ( treatment of choice ) �Fungistatic, and inhibits nucleic acid synthesis, arresting cell division at metaphase and impairing fungal cell wall synthesis. � It is also anti-inflammatory �Tablet or suspension form �Recommended dose: for pediatric microsized 15 mg/kg/day, ultramicrosized 10 mg/kg/day �For adults up to 250 mg/ day, Bid.
Griseofulvin �between 8 and 12 weeks. �Side effects nausea and rashes in 8 -15%. �contra-indicated in pregnancy, lupus erythematosus, porphyria and severe liver disease. �Advantages inexpensive, effective, safe. �Disadvantages: Prolonged treatment required. �Drug interactions : warfarin, cyclosporin and the oral contraceptive pill.
Terbinafine �Acts on fungal cell membranes and is fungicidal. � It is effective against all dermatophytes �Effective as griseofulvin and is safe for the management of scalp ringworm due to Trichophyton sp. �Dosage : 250 mg qd, depends on the weight of the patient ( if the weight 10 -20 kg 62. 5 mg, between 20 -40 kg 125 mg, > 40 kg 250 mg.
Terbinafine �Side-effects include; gastrointestinal disturbances and rashes in 5% and 3% of cases, �Advantages. Fungicidal so shorter therapy required (cf. griseofulvin) so increased compliance more likely. �Disadvantages. No suspension formulation.
Itraconazole �exhibits both fungistatic and fungicidal activity �Fungistatic through depletion of cell membrane ergosterol, which interferes with membrane permeability. �Doses in children 5 mg/kg per day. � in adult 200 mg/day. �Duration 4 weeks.
Itraconazole �Advantage. Pulsed shorter treatment regimens are possible. �Disadvantage. possible side-effects. Potential drug interactions. �Drug interactions. Enhanced toxicity of anticoagulants (warfarin), antihistamines (terfenadine and astemizole), antipsychotics (sertindole), anxiolytics (midazolam), digoxin.
Fluconazole �Doses : for pediatric 6 mg/kg per day for 4 weeks for adult : 200 mg/ day Ketoconazole �Doses : for pediatric 5 mg/kg per day for adult 200 -400 mg / day its use in children is limited by hepatotoxicity
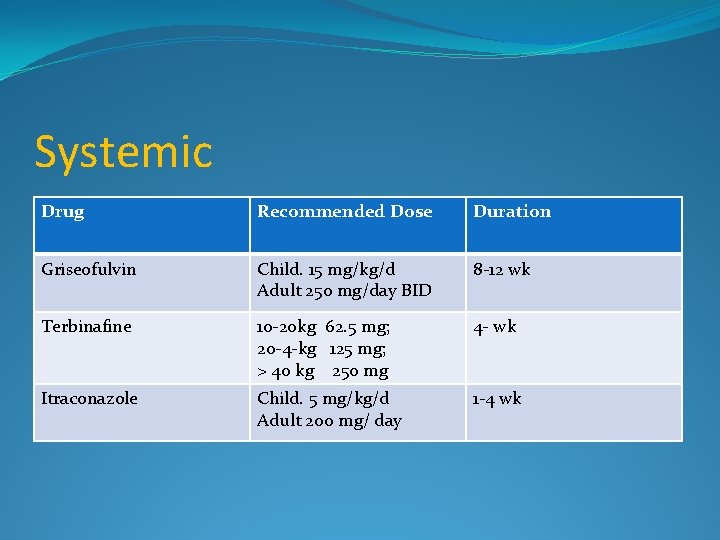
Systemic Drug Recommended Dose Duration Griseofulvin Child. 15 mg/kg/d Adult 250 mg/day BID 8 -12 wk Terbinafine 10 -20 kg 62. 5 mg; 20 -4 -kg 125 mg; > 40 kg 250 mg 4 - wk Itraconazole Child. 5 mg/kg/d Adult 200 mg/ day 1 -4 wk
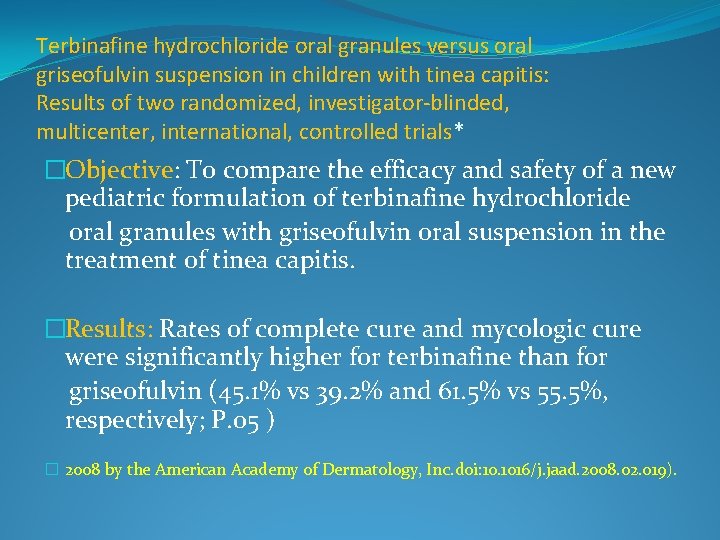
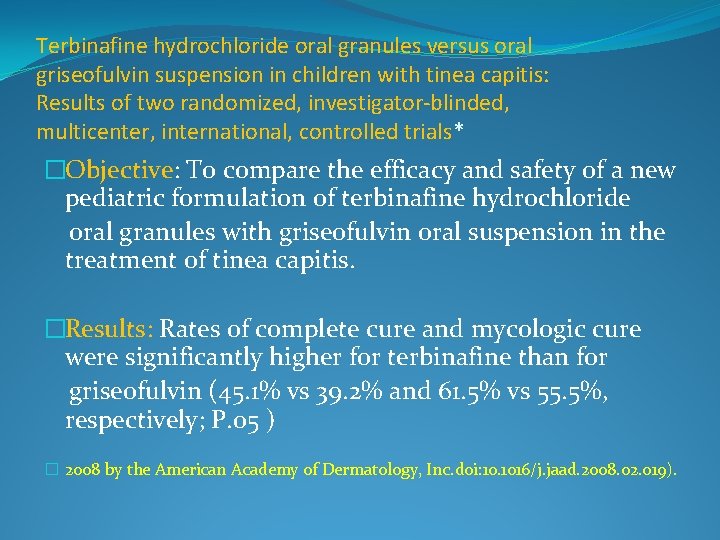
Terbinafine hydrochloride oral granules versus oral griseofulvin suspension in children with tinea capitis: Results of two randomized, investigator-blinded, multicenter, international, controlled trials* �Objective: To compare the efficacy and safety of a new pediatric formulation of terbinafine hydrochloride oral granules with griseofulvin oral suspension in the treatment of tinea capitis. �Results: Rates of complete cure and mycologic cure were significantly higher for terbinafine than for griseofulvin (45. 1% vs 39. 2% and 61. 5% vs 55. 5%, respectively; P. 05 ) � 2008 by the American Academy of Dermatology, Inc. doi: 10. 1016/j. jaad. 2008. 02. 019).
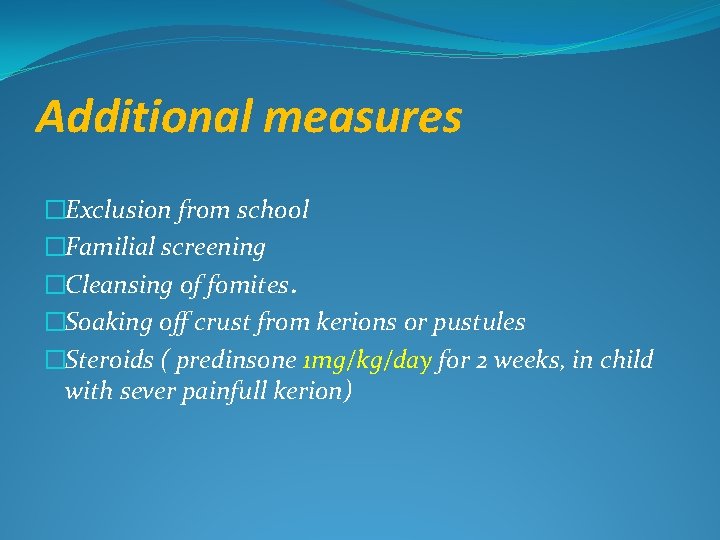
Additional measures �Exclusion from school �Familial screening �Cleansing of fomites. �Soaking off crust from kerions or pustules �Steroids ( predinsone 1 mg/kg/day for 2 weeks, in child with sever painfull kerion)
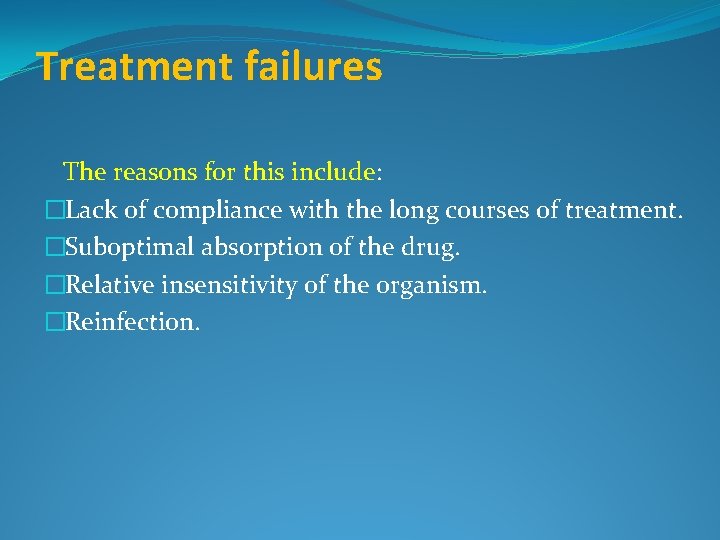
Treatment failures The reasons for this include: �Lack of compliance with the long courses of treatment. �Suboptimal absorption of the drug. �Relative insensitivity of the organism. �Reinfection.
options include � Increase the dose or duration of the original drug. �Change to an alternative antifungal e. g. switch from griseofulvin to terbinafine or itraconazole. Carriers Person who does not have clinical signs of tinea capitis but has a positive fungal culture from the scalp Treatment : twice weekly selenium sulphide or povidone iodine shampoo
Follow-up �Repeat mycology sampling is recommended at the end of the standard treatment period and then monthly until mycological clearance is documented. � Or by clinical imporovment.
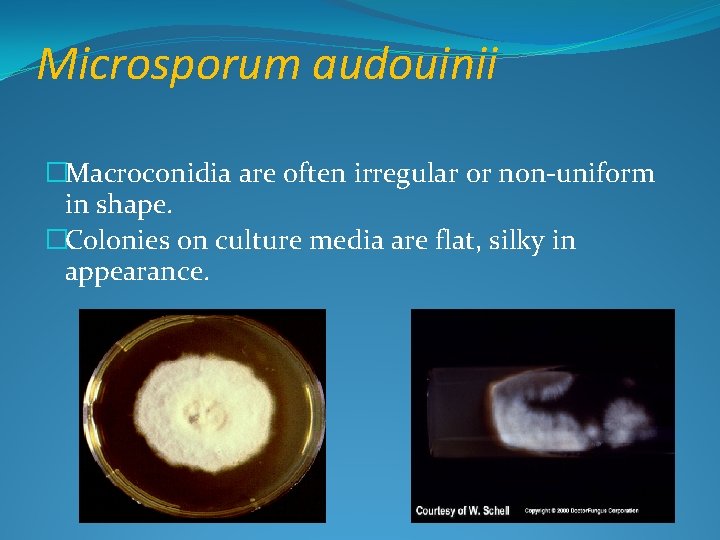
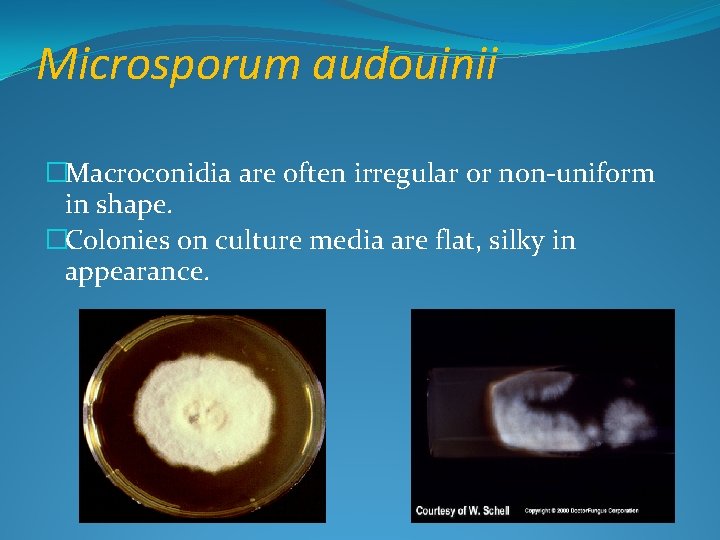
Microsporum audouinii �Macroconidia are often irregular or non-uniform in shape. �Colonies on culture media are flat, silky in appearance.
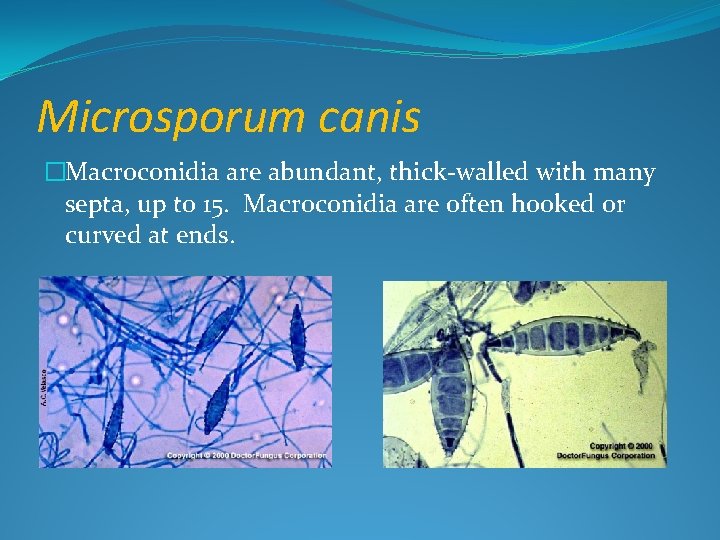
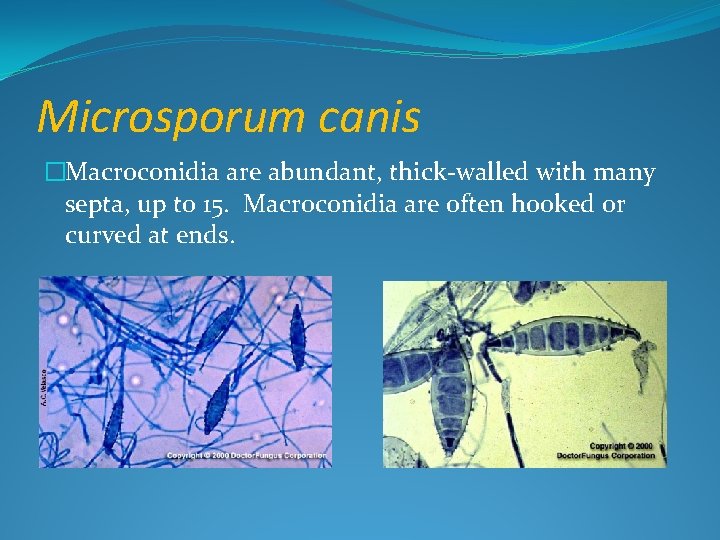
Microsporum canis �Macroconidia are abundant, thick-walled with many septa, up to 15. Macroconidia are often hooked or curved at ends.

Microsporum gypseum �Produces abundant macroconidia brownish-yellow due to large numbers macroconidia. Surface of culture colony often is powdery in appearance. �Macroconidia usually have 4 -6 septa or crosswalls. �Microconidia are smaller than in M. canis.
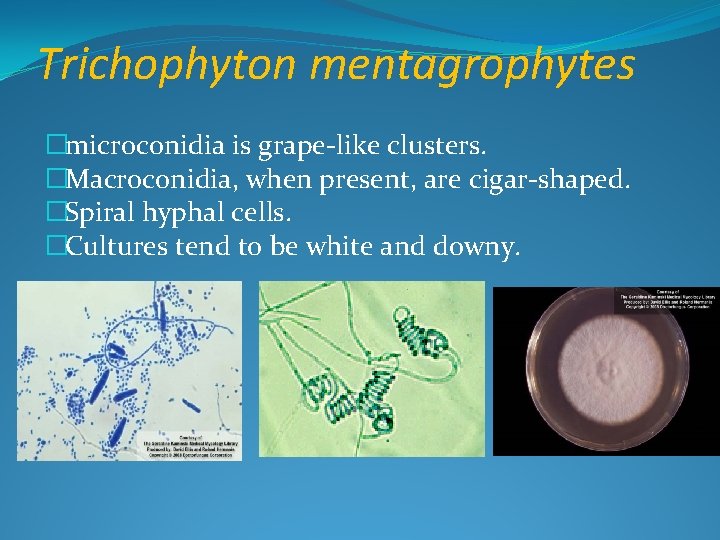
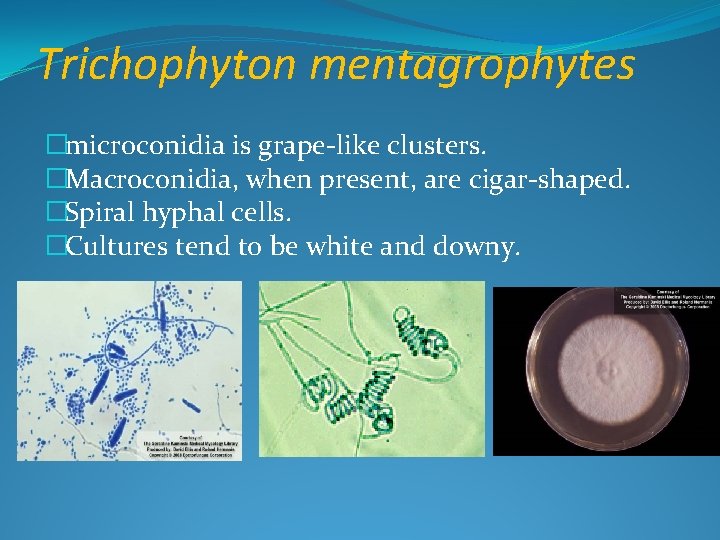
Trichophyton mentagrophytes �microconidia is grape-like clusters. �Macroconidia, when present, are cigar-shaped. �Spiral hyphal cells. �Cultures tend to be white and downy.
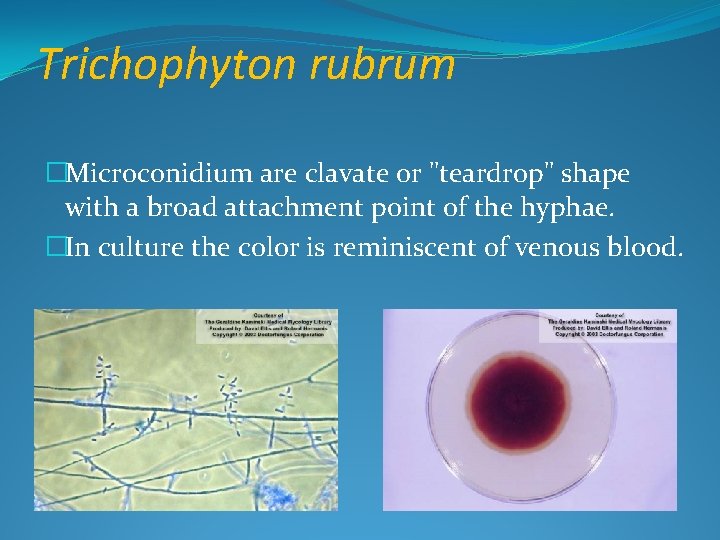
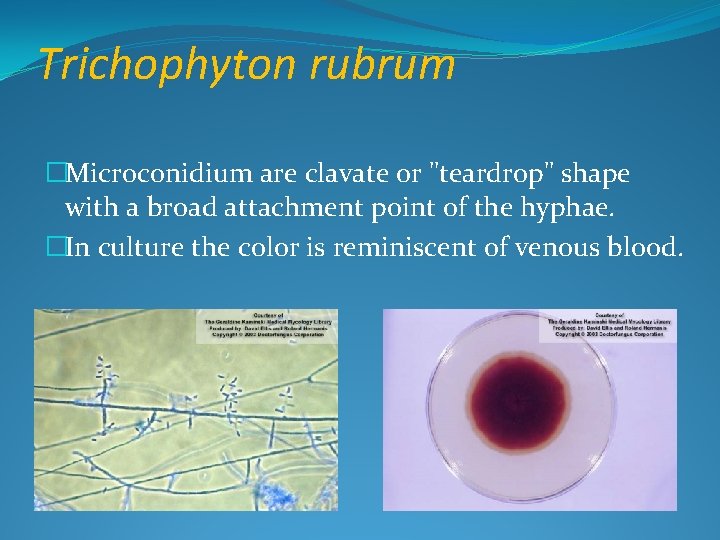
Trichophyton rubrum �Microconidium are clavate or "teardrop" shape with a broad attachment point of the hyphae. �In culture the color is reminiscent of venous blood.
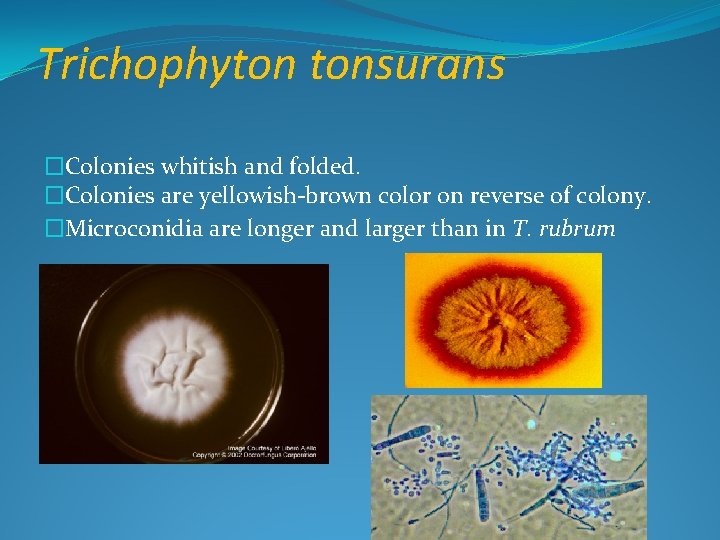
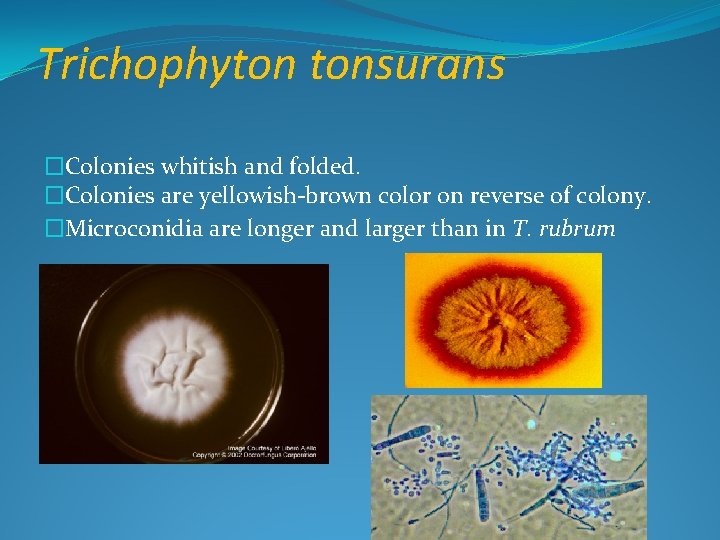
Trichophyton tonsurans �Colonies whitish and folded. �Colonies are yellowish-brown color on reverse of colony. �Microconidia are longer and larger than in T. rubrum
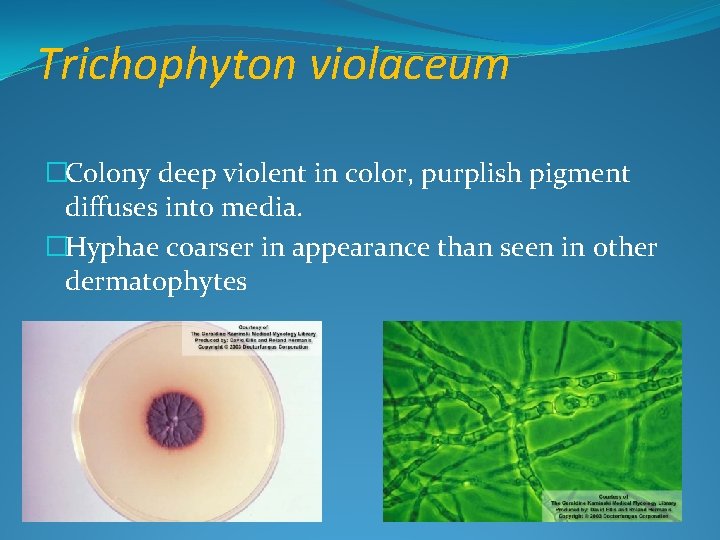
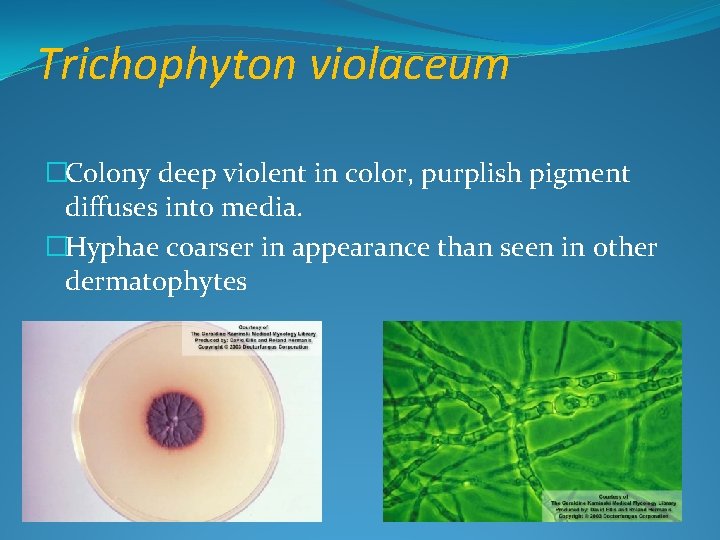
Trichophyton violaceum �Colony deep violent in color, purplish pigment diffuses into media. �Hyphae coarser in appearance than seen in other dermatophytes
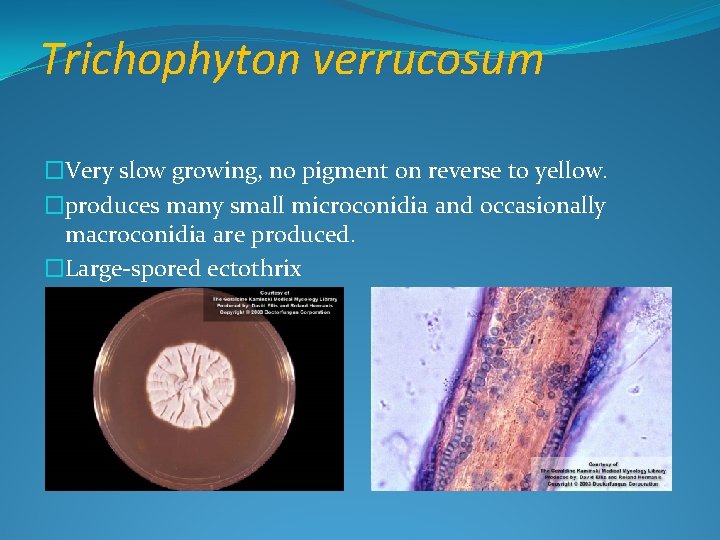
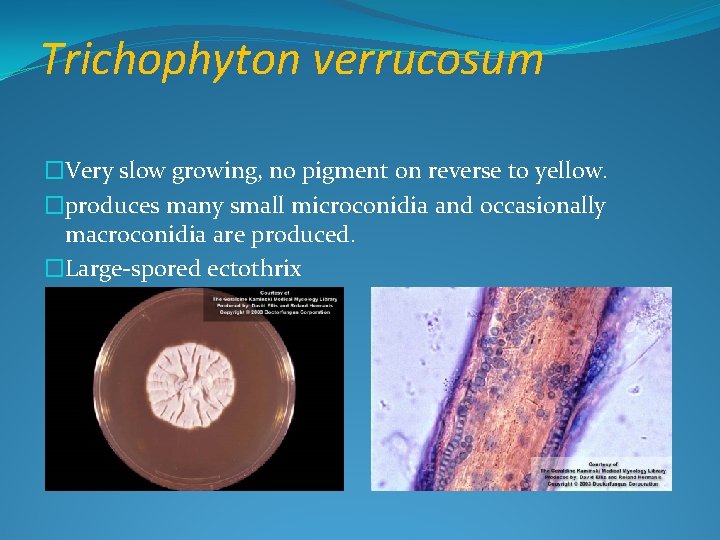
Trichophyton verrucosum �Very slow growing, no pigment on reverse to yellow. �produces many small microconidia and occasionally macroconidia are produced. �Large-spored ectothrix
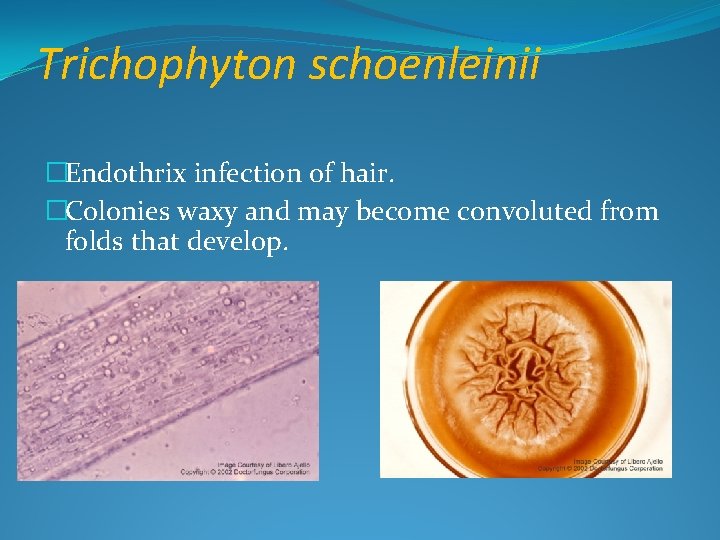
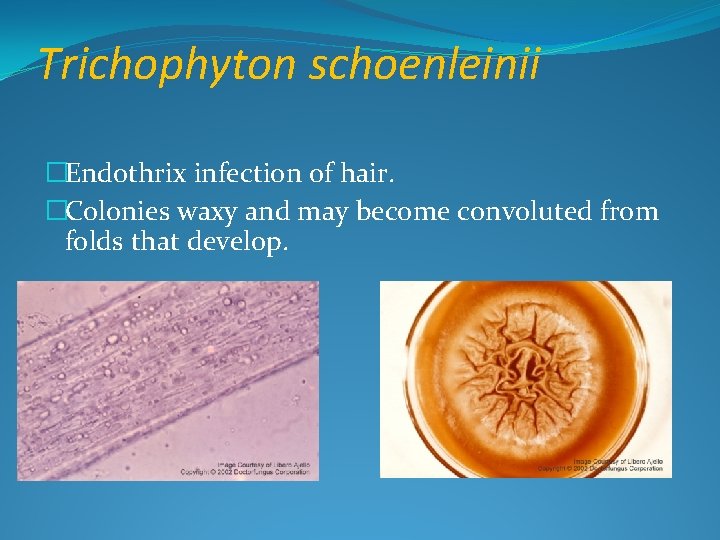
Trichophyton schoenleinii �Endothrix infection of hair. �Colonies waxy and may become convoluted from folds that develop.
THANK YOU
References �Fitzpatrick’s Dermatology in General Medicine. 6 th ed. New. York: Mc Graw Hill; 2003; �Elewski BE. Tinea capitis: A current perpspective. J Am Acad Dermatol. 2000; 42 1 Pt 1: 1 -20. �Jhangir M, Hussain I, Khushid K, Haroon TS. A �clinicoetiologic correlation in tinea capitis. Int J Dermatol. 2002; 38: 275 -8. �Ghannoum M, Isham N, Hajjeh R, Cano M, Al-Hasawi F, Yearick D, et al. Tinea capitis in Cleveland: Survey of elementary school students. J Am Acad Dermatol. 2003; 48: 189 -93.