Curriculum Update Crime Scenes Behavioral Emergencies Toxic Exposure
Curriculum Update: Crime Scenes Behavioral Emergencies Toxic Exposure Abuse and Assault Condell Medical Center EMS System September 2006 Site code #10 -7200 -E-1206 Revisions by S Hopkins, RN, BSN 1
Objectives n Upon completion of the module, the EMS provider should be able to: n describe approach to a crime scene and steps taken to preserve evidence n describe what a behavioral emergency is and medical legal considerations n list drugs that are abused and field interventions that may be necessary 2 2
Objectives cont’d n list types of abuse and assault and the legal considerations n actively participate in case scenario discussion n review activation of cardizem syringe n successfully complete the quiz with a score of 80% or greater 3
Crime Scenes 4

Crime Scenes n Crime Scene Definition A location where any part of a criminal act occurred n A location where evidence relating to a crime may be found n 5
Crime Scenes n EMS personnel may be mistaken for police Uniform colors n Badges n Exiting a vehicle with lights and sirens n Can initiate aggression toward an authority figure n 6
Approach to the Scene n Approach is part of scene size-up Identification of possible hazards is part of scene size-up n Key point – identify and respond to dangers before they threaten n Safety concerns begin with dispatch information n Use available resources before arrival n n Do not enter the scene until it is safe and secured 7
Approach to the Scene n. A secured scene can become unsafe again - be on guard n Retreat from the scene if the scene cannot be made safe; there is no such thing as a dead hero! n Know local protocols n Begin observation several blocks before the scene 8
Use of Red Lights & Sirens Urban areas - excess use may draw crowds n Highway scene - lights required for safety nlights can also be hypnotizing and cause drivers to drive into the lights n 9
Known Violent Scenes n Stage safe distance from the scene until police advise scene “secure” n Out of sight of the scene n If you can be seen, people will come to you n Entering an unsafe scene adds another potential victim n You may be injured, killed, or taken as hostage n You may become another patient 10

Violent Scenes n Coordinate your approach with police n n n Approach potentially unsafe environments single file If holding a flashlight, hold from the side n n You do not want to be misidentified Armed assailants often aim at the light Stand to the side of doorways when knocking n Standing directly in front of a door makes you a target 11
Approach to the Scene n n Remember non-violent dangers such as hazardous materials, power lines, dangerous pets, etc Scene safety considerations must continue throughout the call Others could expect you to intervene in violent situations Remember to include “escape and strategic escape plans” in your protocols 12
Crime Scene Preservation n Evidence n Prints Fingerprints - ridge characteristics are left behind on a surface with oils & moisture from the skin; unique in that no 2 people have identical fingerprints n Footprints n n Blood and body fluids DNA and ABO blood typing possible n Blood splatter pattern is evidence n n Particulate evidence n Hairs, carpet & clothing fibers - leave sheets under 13 the patient in the ED (may hold evidence)
Crime Scene Observations n n n Patient (victim) position Patient injuries versus marks you added (ie: IV attempts) Conditions at the scene “He done it!” n lights, curtains, signs of forced entry, anything moved or touched by EMS Statements of persons at the scene Statements of the patient/ victim Dying declarations 14 n place in quotation marks
Evidence Preservation at Crime Scenes n Patient care is the ultimate priority n n Evidence protection is performed while caring for the patient n n You may be restricted to only 1 team member for initial scene entrance Carry in only necessary equipment Evidence preservation techniques Be observant n Touch only what is necessary for patient care n 15
Use of Gloves At Crime Scenes n Wear latex gloves Used for infection control n Prevents you from leaving your fingerprints n Prevents smudging of other fingerprints n 16
Crime Scene Documentation n n Note observations objectively, not subjectively (ie: note color of bruising and not “new” bruise) Put patient’s or bystander’s words in quotes Patient care records are legal documents Avoid opinions not relevant to patient care Patient care records will be used in court will 17 your charting stand up?
Mandatory Reporting n EMS providers are required to report certain types of crimes n n n Child abuse - DCFS must be notified Suspected elder abuse (age 60 or older) and/or neglect Domestic violence n If a refusal, EMS is mandated by the State to report all cases of domestic violence to the local police n Offer an informational brochure to the patient n Document your actions Certain violent crimes (i. e. sexual assault, gunshot, etc. ) Confidentiality needs to be maintained 18
19
BEHAVIORAL EMERGENCIES 20
BEHAVIORAL EMERGENCEIS n “Normal Behavior” n n n No clear definition or ideal model Ideas vary by culture or ethnic group What society accepts at the moment n “Abnormal Behavior” n n n Deviates from society’s expectations Interferes with well being and ability to function Harmful to individual or group 21
What Is A BEHAVIORAL EMERGENCY? n n General term to describe a broad range of conditions of varying severity including unanticipated or maladaptive behavioral episode Use of the word “abnormal” is very subjective Recognized as behavior requiring immediate intervention Not always a clear cut EMS call 22
Behavioral Calls n Indications of a behavioral or psychological condition include: interference with core life functions (eating, sleeping, ability to maintain housing, interpersonal or sexual relations n posing a threat to the life or well-being of themselves or others n significant deviation from the expectations or norms of society n 23
Responses to Behavioral Emergencies n n n Most of your assessment skills will depend on your interpersonal & people skills more than use of diagnostic tools Remember, on all calls your safety is #1 and your partner’s is #2 Will need to exercise observational skills patient n family n bystanders n 24
BEHAVIORAL EMERGENCIES n Incidence Estimates vary with as much as 20% of the population experiencing some type of mental problem n Incapacitates more people than all other health problems combined n 1 person out of 7 will require treatment for an emotional disturbance n 25
BEHAVIORAL EMERGENCIES n Common misconceptions Abnormal behavior is always bizarre n All mental patients are unstable and dangerous n Mental disorders are incurable n Having a mental disorder is cause for embarrassment and shame n 26
Specific Psychiatric Disorders ü Cognitive disorders Organic causes such as brain injury or disease n Includes delirium (rapid onset disorganized thought) and dementia (gradual development memory & cognitive impairment) n ü Schizophrenia loss of contact with reality n hallucinations, delusions, depression n ü Anxiety & related Disorders panic attacks n phobias n post-traumatic stress syndrome n 27
ü Mood disorders depression n bipolar disorder (manic-depressive episodes) n Substance use/abuse ü Physical symptoms with no apparent physiological cause ü Factitious disorders ü intentional production of signs/symptoms n motivation to assume the sick role n external incentives are absent (ie: avoid police) n 28
ü Dissociate disorders failure to recall (psychogenic amnesia) n physically moving miles away (fugue state) n multiple personality disorder (2 or more compete personalities) n depersonalization (loss of one’s self) n ü Eating disorders anorexia - loss of appetite; excessive fasting n bulimia - uncontrollable bingeing & vomiting or diarrhea n these patients are at risk for electrolyte imbalance and dysrhythmia n 29
ü Personality disorders acting odd or eccentric n dramatic, emotional, fearful, anxious patients n ü Impulse control disorders n ü failure to control certain impulses that may be harmful to the patient or others Suicide/suicidal attempts 30
BEHAVIORAL EMERGENCIES n Management considerations Treat existing medical problems n Maintain safety n Do not confront or argue with patient n Control violent situations n Remain with patient at all times n Avoid challenging the patient’s personal space n Avoid judgements n 31
BEHAVIORAL EMERGENCIES n Medical Legal Considerations Standard of care must always be followed n Obtaining consent may help avoid charges of assault or battery n assault - a verbal or physical threat n battery - patient force without consent n n Limitations of legal authority n n if in doubt regarding action, contact medical control Objective documentation will be your best defense 32
Use of Restraints n n n Methods of restraint n Verbal de-escalation n speaking in a calm manner n avoid patient’s “personal space” n Physical restraint n includes soft (ie: sheets) and hard restraints (ie: handcuffs, leathers) Have enough man-power available prior to beginning restraint procedure, if possible Restraint in a prone (face-down) position can make the patient susceptible to positional asphyxia - watch for airway compromise!!! 33
Restraints n n Once a patient is restrained, never leave them unattended Once restrained, frequently monitor and document neurovascular assessments of restrained extremities n n need to maintain adequate circulation EMS personnel need to contact medical control as soon as possible when restraints are being considered or have been used 34
Restraints n n n Never compromise the patient’s airway Do not further aggravate injuries or illness EMS to clearly document the behavior that led to use of restraints Handcuffs are to be applied by police only If handcuffed, a police officer must accompany the patient in the ambulance while being transported (CMC policy) 35
Taser Use By Law Enforcement n n Use of propelled wires to conduct energy that affects the sensory and motor functions of the central nervous system Overrides the central nervous system to achieve incapacitation n previous weapons worked on pain compliance which can be overcome by drugs, alcohol, or focused & combative patients 36
Taser Use n n n Static discharge on a doorknob - 35, 000 100, 000 volts Taser system - 50, 000 volts Does not cause electrocution in a wet environment Electricity will not pass to others in contact with the subject unless contact is made directly between or on the probes Patient can be touched while Taser is active n do not touch probes or step on wires 37
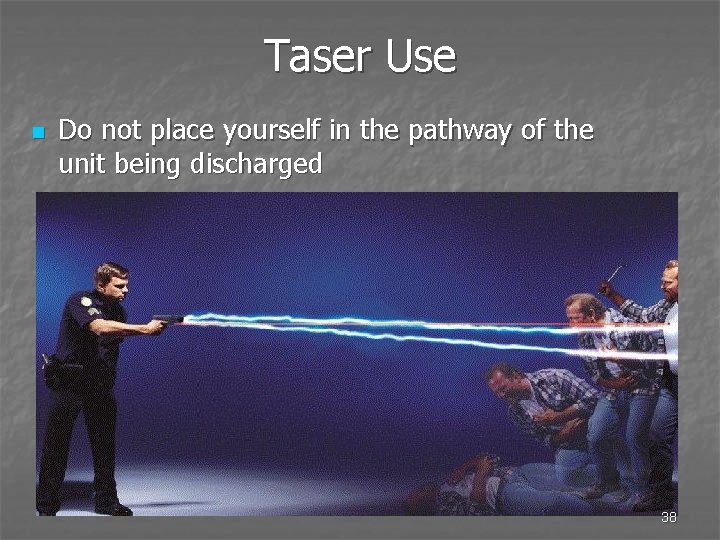
Taser Use n Do not place yourself in the pathway of the unit being discharged 38
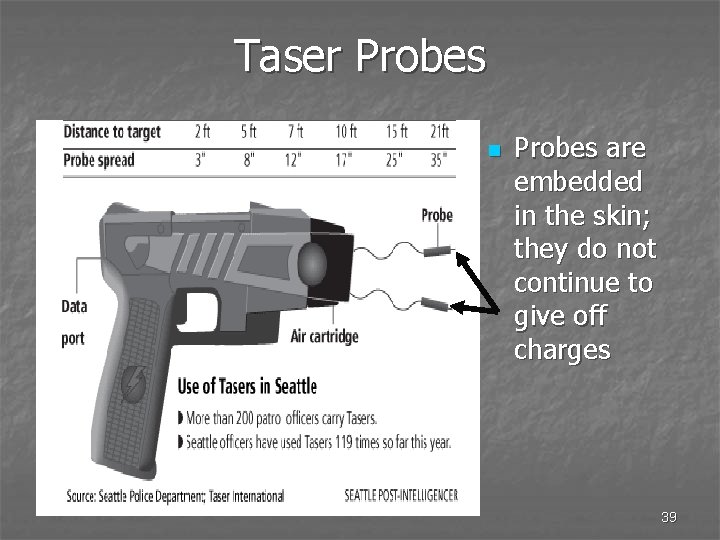
Taser Probes n Probes are embedded in the skin; they do not continue to give off charges 39
Taser Probes n n n Law enforcement may remove/break wires near probes CMC EMS have not been authorized to remove laser probes Removal of probes most commonly performed in the ED probed grabbed firmly and pulled straight out n skin wiped with alcohol pad n n Treat removed probes with precautions similar to contaminated sharps 40
Transportation Against The Patient’s Will n n n Patient presents as a threat to themselves or others When ordered by medical control Implemented by law enforcement authorities An incompetent patient will not be allowed to make health care decisions When in doubt, contact medical control and document the contact 41
Transportation of Patients with Psychiatric Issues n n n All patients must be evaluated in an ED before psych admission can occur Admission destination often based on many factors including but not limited to: diagnosis, available beds, insurance requests Just because one facility has a psych unit is no guarantee a patient stays at that facility if in the ED there 42
Petition for Involuntary Admission n n Completed by person(s) witnessing the behavior (ie: police, EMS, family, hospital) If petition not completed in ED and ED staff have not witnessed behavior, patient may be discharged Petition may be completed by family only if they witness behavior or conversation Transporting authority acting in good faith and without negligence shall incur no liability, civil or criminal, due to transport 43
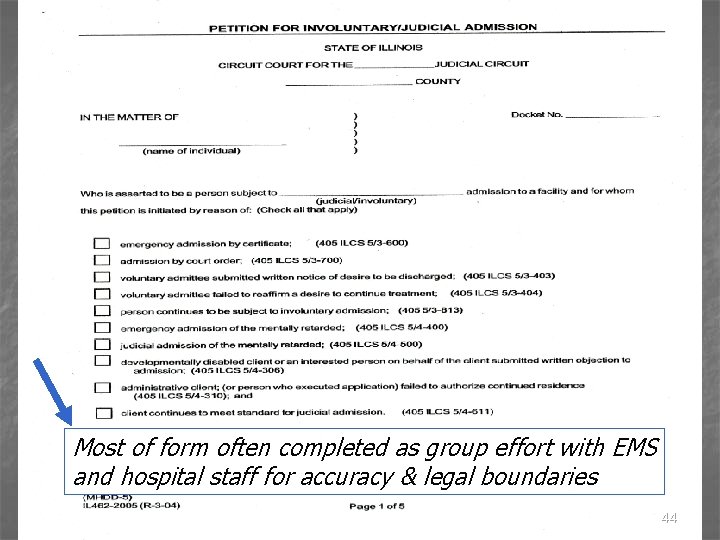
Most of form often completed as group effort with EMS and hospital staff for accuracy & legal boundaries 44
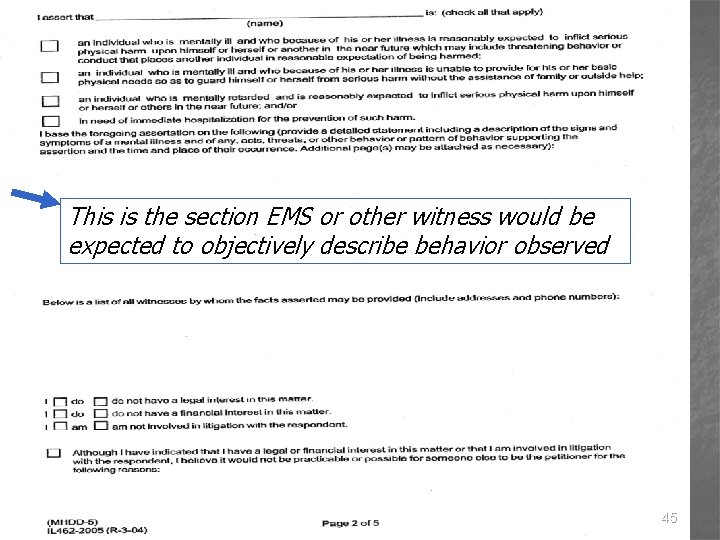
This is the section EMS or other witness would be expected to objectively describe behavior observed 45
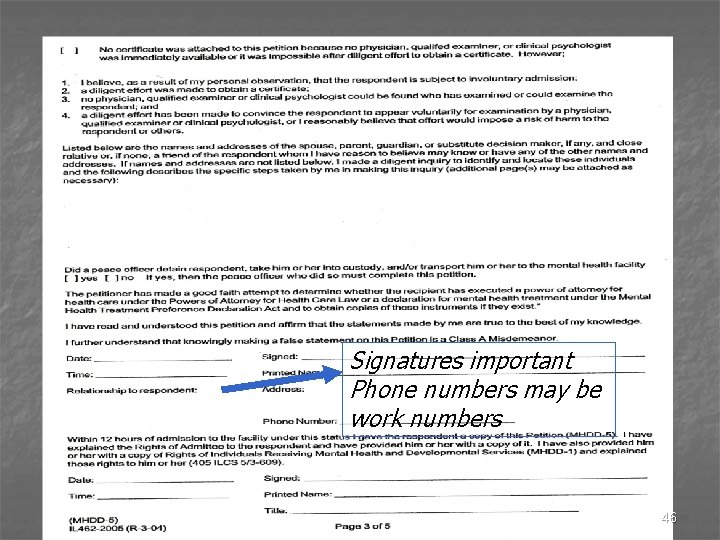
Signatures important Phone numbers may be work numbers 46

47
Toxic Exposure 48
Multiple Forms of Toxic Exposure Substances n n n n Biological Nuclear Irritants Chemical Nerve agents Blister agents Blood agents n n n Farm chemicals Cleaning agents Petroleum products and by-products Medicine/drugs Inert gases Explosion hazards 49
Alcohol n n n A central nervous system depressant A common & favorite mood-altering drug Affect on body influenced by: age n gender n physical condition n amount of food eaten n other medicines/drugs taken n n Is a toxic drug producing pathological changes in liver tissue (cirrhosis) and can cause death 50
Alcohol n Low dose effects relaxed feeling, reduces tension, lowers inhibition n impairs concentration; slows reflexes n reduces coordination; impairs reaction time n n Medium dose effects n n slurred speech, drowsiness, altered emotions Higher dose effects vomiting n breathing difficulties n unconsciousness n coma n 51
Chronic Use of Alcohol n n n Damage to frontal lobes of brain Brain shrinkage Vitamin deficiency (B-1 or thiamine) n Wernicke’s encephalopathy - impaired memory, confusion, lack of coordination n Korsakoff’s syndrome - amnesia, apathy, disorientation Health deterioration of multiple systems Fetal alcohol syndrome in newborn alcohol passes thru placenta n normal brain development disrupted n 52
Alcohol Withdrawal n Typically 6 - 48 hours after last drink Shaking (tremors) n Sleep problems n Decreased appetite, nausea n Anxiety n Increased heart rate, increased blood pressure n Hallucinations n Seizures n 53
Delirium Tremens (DTs) n n n n Usually start 48 - 96 hours after last drink 20% fatality when untreated DT's can produce fatal seizures, MI, stroke Hallucinations - usually visual Profound confusion, disorientation, hyperactivity Cardiac dysrhythmias Seizures - true emergency 54
Treatment of DT’s n n Valium to stop seizure activity Fluid resuscitation Treat dysrhythmias per SOP Increased risk of vomiting n protect airway from aspiration n have suction available n consider transport of patient side-lying 55
Marijuana n n n One of the world’s most commonly used illegal drugs Usually smoked; can be cooked/baked into food Interferes with normal function of certain receptors in the brain (memory, concentration, perception, movement) Effects in 1 -10 minutes; lasts 3 - 4 hours High doses cause: hallucination, delusions, impaired memory, disorientation Metabolites detected 45 -60 days after use 56
Inhalants n n Huffing or sniffing products which are easily found & available everywhere Damage the nervous system & other organs (ie: lungs, liver, heart, & kidneys) Vapors inhaled into lungs enter bloodstream then travel to brain & other tissues Immediate effects: relaxation, slurred speech, euphoria, hallucinations, drowsiness, dizziness, nausea, vomiting, DEATH from heart failure or suffocation from plastic bags 57 or aspiration of vomit
Inhalants n n Long term use effects: memory loss, concentration problems, visual disturbances, blindness, motor problems, peripheral nerve damage Products abused: hair spray, nitrous oxide, cleaning fluids, typewriter correction fluid, nail polish remover, gasoline, glue, rubber cement, paint & paint thinner, lighter fluid, room deodorizers, marker pens 58
Cocaine n n n A local anesthetic and central nervous system stimulant Can be chewed (leaves), smoked, inhaled (snorted), or injected Acts by blocking reuptake of neurotransmitters dopamine, norepinephrine & serotonin in brain Affects peripheral nervous system: constricts blood vessels, causes irregular heart beat, pupils dilate Risk of MI or stroke within 3 days of OD 59
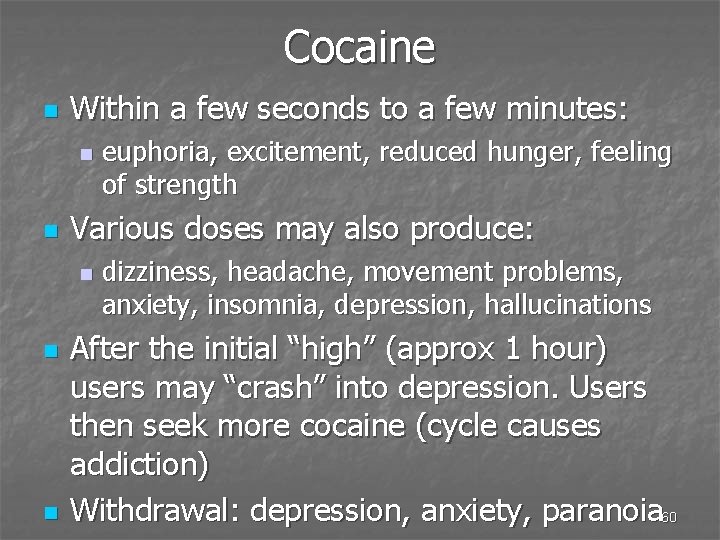
Cocaine n Within a few seconds to a few minutes: n n Various doses may also produce: n n n euphoria, excitement, reduced hunger, feeling of strength dizziness, headache, movement problems, anxiety, insomnia, depression, hallucinations After the initial “high” (approx 1 hour) users may “crash” into depression. Users then seek more cocaine (cycle causes addiction) Withdrawal: depression, anxiety, paranoia 60
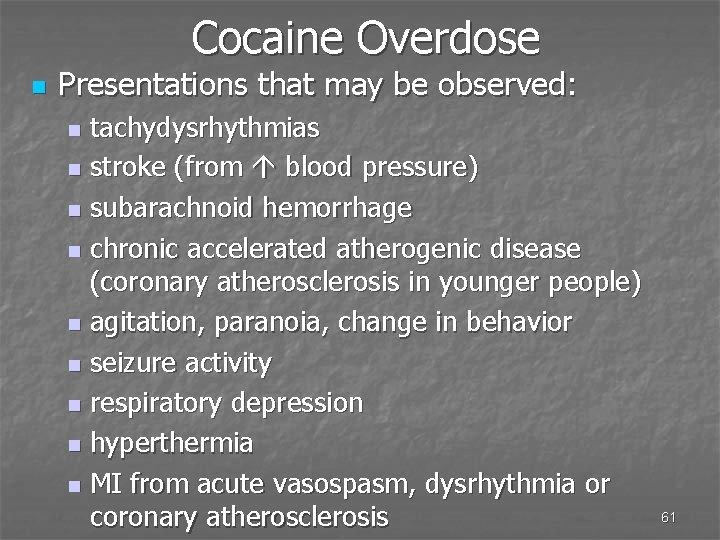
Cocaine Overdose n Presentations that may be observed: tachydysrhythmias n stroke (from blood pressure) n subarachnoid hemorrhage n chronic accelerated atherogenic disease (coronary atherosclerosis in younger people) n agitation, paranoia, change in behavior n seizure activity n respiratory depression n hyperthermia n MI from acute vasospasm, dysrhythmia or coronary atherosclerosis n 61
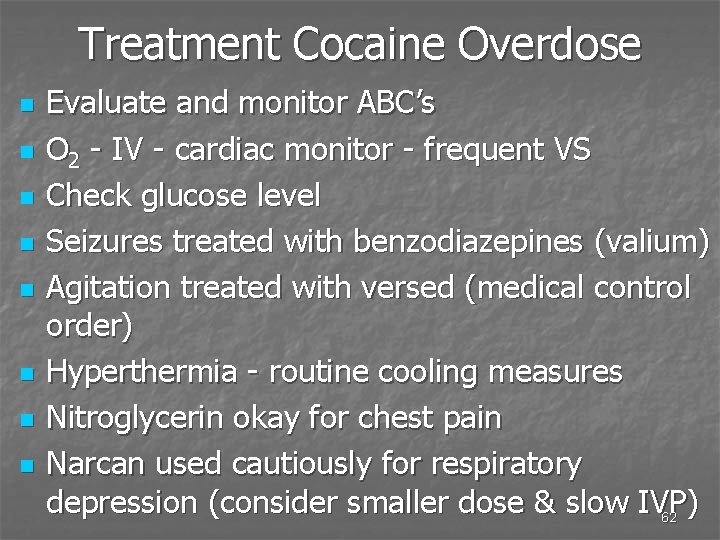
Treatment Cocaine Overdose n n n n Evaluate and monitor ABC’s O 2 - IV - cardiac monitor - frequent VS Check glucose level Seizures treated with benzodiazepines (valium) Agitation treated with versed (medical control order) Hyperthermia - routine cooling measures Nitroglycerin okay for chest pain Narcan used cautiously for respiratory depression (consider smaller dose & slow IVP) 62
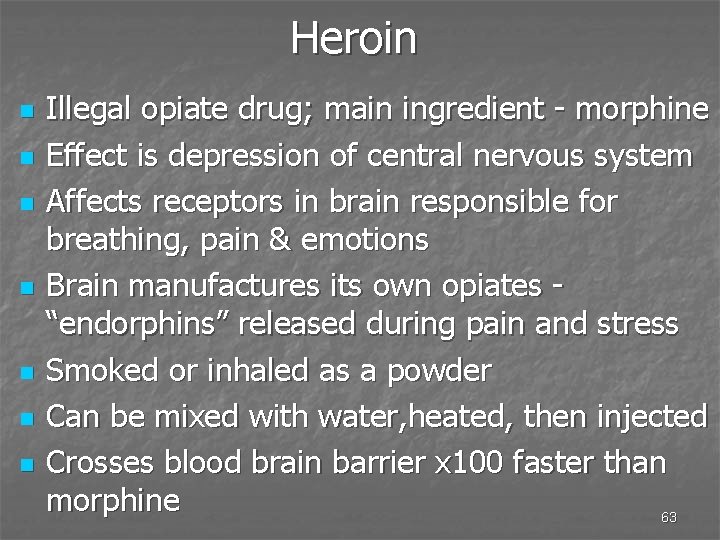
Heroin n n n Illegal opiate drug; main ingredient - morphine Effect is depression of central nervous system Affects receptors in brain responsible for breathing, pain & emotions Brain manufactures its own opiates “endorphins” released during pain and stress Smoked or inhaled as a powder Can be mixed with water, heated, then injected Crosses blood brain barrier x 100 faster than morphine 63
Heroin n Effects produced: IVP - 7 - 8 seconds n IM or SQ - 5 - 8 minutes n n Short term effects analgesia n brief euphoria (“rush”) n nausea n sedation/drowsiness n reduced anxiety n hypothermia n reduced respirations; reduced coughing n 64
Other Effects of Heroin n Long term: tolerance - need higher drug dosages n addiction - psychological & physiological need n withdrawal - 8 -12 hours after last dose are symptomatic n risk of HIV/AIDS, hepatitis, infections n poisoning - from added product to heroin n increased risk of stroke n collapsed veins n lung infections n 65
Speedballing n n Combining cocaine with heroin use Causes frequent & sometimes fatal complications because of combining these 2 drugs n n Deaths of John Belushi, River Phoenix, Chris Farley Heroin injected or smoked followed immediately by smoking cocaine 66
Treatment of Heroin Overdose n n Support ventilations Narcan May negate sedative effect of opioid (heroin) and leave stimulating effect of cocaine unopposed which worsens toxicity n Use narcan to treat respiratory depression n 2 mg slow IVP; repeated every 5 minutes to total of 10 mg n consult with medical control for possible smaller dose (to avoid increased agitation and uncontrollable behavior in the patient) 67 n
Amphetamines n n n Stimulants of the central nervous system Many effects similar to cocaine Addiction, withdrawal, & tolerance possible Taken orally, injected, smoked, snorted Common products dextroamphetamine - dexies n benzedrine n ritalin n methamphetamine - speed, meth, crystal n n OTC cold & allergy products no longer easily 68 accessible to the public due to abuse factor
Amphetamines n Originally developed to treat asthma n sleep disorders (narcolepsy) n hyperactivity n n Short term effects increased heart rate n increased blood pressure n reduced appetite n dilation of pupils n feelings of happiness and power n reduced fatigue n 69
Amphetamines n Long term use effects insomnia, restlessness n paranoid psychosis n hallucinations n violent & aggressive behavior n weight loss n tremors n n Popular abused drugs in the club and rave scenes n rave - all night underground party 70
Treatment of Amphetamine Use n Scene safety very important patients often agitated, hostile, paranoid n meth lab volatile environment with risk of explosion and fire n n Acute overdose produces n seizures n hypertension n tachycardia n hyperthermia n psychosis, hallucinations n stroke, death 71
Barbiturates n Depresses central nervous system n n n “sleeping pills” May lead to tolerance (need for increasing doses) and dependence (feeling you must use the drug; withdrawal symptoms occur when you stop using the drug) Easily cross blood/brain barrier 72
Barbiturate Effects n Low doses reduces anxiety n reduces blood pressure, respirations heart rate n reduces REM sleep n n Higher doses n n increase some types of behavior and actually act as a stimulant (depression of inhibitory brain circuits) Can cause excessive sedation, anesthesia, coma, death 73
Drugs Abused For Sexual Purposes n n n Added to drinks and food Can be forced on the person by coercion Known versus unknown ingestion of substances Self gratification or fulfillment of another person If called for one person at a “party, ” anticipate multiple patients affected 74
GHB (Gamma hydroxybutyrate) n n n Central nervous system depressant Takes minutes for user to lose control, have amnesia, or lose consciousness Colorless, odorless, slightly salty taste High can last 1 1/2 - 3 hours with a rapid return to normal with no hangover Can be extremely addictive Used by body builders 75
GHB n Low doses (similar to alcohol intoxication) drowsiness n hypnosis n dizziness n euphoria n n High doses vomiting n convulsions n hypotension, bradycardia, bradypnea n coma n 76
Assessment GHB Often called to a party of many unconscious young adults n Powerful CNS depressant (often GCS is 3) n Skin will be hot and in some cases dry n Pupils fixed and dilated n Nausea and uncontrollable vomiting n Gag reflex intact n Loss of recall of current events leading to present condition n Duration 1 -2 hours; full recovery 8 hours n 77
Ketamine n n Powerful anesthetic (tranquilizer) used for animals (derivative of PCP) CNS depressant, sedative & amnesic properties Can be injected, consumed in drinks, smoked, inhaled Renders victim physically helpless, unable to refuse sexual advances, unable to remember events 78
Ketamine Effects n Low doses impaired concentration, learning & memory functions n feeling of floating outside body n increased heart rate & blood pressure n n High doses hallucinations n sensation of rising above one’s body n potentially fatal n n Long term - flashbacks & shortened attention span 79
Rohypnol (Roofies) n n n Benzodiazepine but 10 times more powerful than equivalent of valium Outside USA used as sleep aid & presurgical sedative (sedative-hypnotic effect) Illegal in USA Tasteless, odorless, dissolves easily in food or drink Manufactured now to release a blue dye when dissolved in a liquid Onset 15 -30 minutes, peaks 2 hours, last 6 -8 80 hours
Rohypnol n n n n As date rape drug, causes blackouts, memory loss, removes inhibitions, long lasting Impairs judgement, confusion, amnesia Dilated pupils Respirations depressed (common) B/P decreased, pulse increased Impaired motor skills Slurred speech Seizures, coma 81
Assessment Drugs Abused for Sexual Purposes n n n Watch for decreasing level of responsiveness Anticipate slow, shallow respiratory rate Watch for apnea (dose dependant) Frequent monitoring vital signs and EKG Monitor level of responsiveness 82
Management Drugs Abused for Sexual Purposes n n Scene safety very important Activate triage if multiple patients Most EMS care is supportive Control the airway BVM use n Narcan may reverse respiratory depression n n Vomiting precautions Seizure precautions - valium as needed Be prepared for cardiac arrhythmias 83
84
Abuse and Assault 85
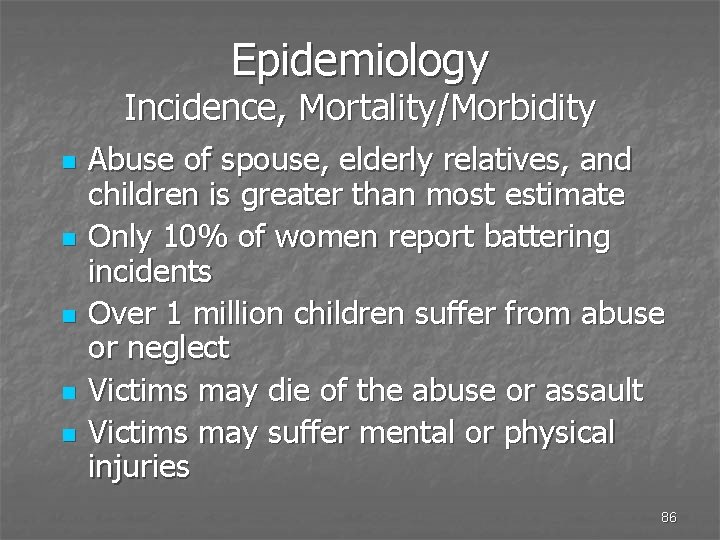
Epidemiology Incidence, Mortality/Morbidity n n n Abuse of spouse, elderly relatives, and children is greater than most estimate Only 10% of women report battering incidents Over 1 million children suffer from abuse or neglect Victims may die of the abuse or assault Victims may suffer mental or physical injuries 86
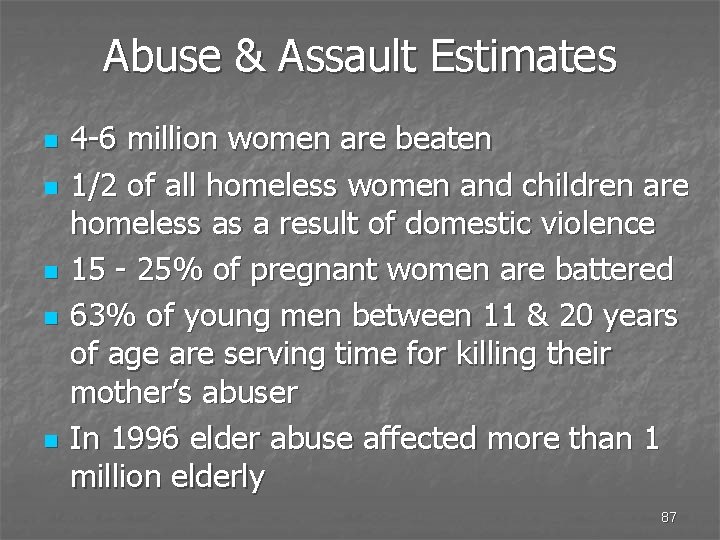
Abuse & Assault Estimates n n n 4 -6 million women are beaten 1/2 of all homeless women and children are homeless as a result of domestic violence 15 - 25% of pregnant women are battered 63% of young men between 11 & 20 years of age are serving time for killing their mother’s abuser In 1996 elder abuse affected more than 1 million elderly 87
Epidemiology Risk Factors n n Men and women who beat one another are most likely beating their children Children of abusive and unloving homes are more likely to become spouse or child batterers and later, abusers of their elderly parents 88
Types of Abuse n n n Physical abuse - physical force Sexual abuse - nonconsensual sexual contact Emotional abuse - anguish, pain, or distress Financial/material exploitation - illegal or improper use of funds, property, assets Neglect n failure to provide adequate medical or personal care or maintenance, which failure results in physical or mental injury to a person or in the deterioration of a person’s physical or mental condition 89
Battered Women Reasons for Not Reporting n n n Personal fear or fear for her children A belief that the offender’s behavior will change A lack of financial and/or emotional support A woman’s belief that she is the cause of the violent behavior A belief that battering is “part of the marriage” and must be endured to keep the family together 90
Battered Women Characteristics of Wife-Battering n n Beatings do not stop Beatings become more severe & frequent Beatings occur without provocation Violence can turn toward the children 91
Characteristics of Spousal Abusers n n n n Low self esteem Violence learned from their parents Believe they are demonstrating discipline They do not like being out of “control” Fail to see alternative behavior Unable to back down from conflict Feel powerless to change 92
Characteristics of Spousal Abusers n n n Alcohol abuse is often a factor Mental illness occurs in less than 10% of abusers Occurs in all socio-economic groups; but most abusers are in lower socio-economic groups 93
Characteristics of Spousal Abusers n n Abuser goes into sudden rages Abusers feel insecure and jealous May appear charming and loving after the incident History of financial problems, holding a job and possible legal problems 94
Risk Factors for Domestic Violence n n n Male is unemployed Male uses illegal drugs at least once a year Partners have different religious backgrounds Family income below poverty line Partners are unmarried n n n Violence toward children Male did not graduate from high school Blue collar job if employed Male age 18 -30 Male saw father hit mother 95
Battered Men Overview n n n Men also rarely report incident Humiliation is multiplied for a man Men feel as trapped as women do Same psychological & emotional effects Society is less empathetic toward men Fewer resources exist for men 96
Homosexual Relationships n n n Spouse battering occurs in homosexual relationships as well Homosexuals are conditioned the same as heterosexuals >150, 000 men in the US each year are victims of physical violence by a spouse or partner (both opposite and same sex relationships) 97
Legal Considerations for Battered Spouses n n n Spousal abuse is a crime Assault is a misdemeanor or a felony Attacker may be released within hours of arrest n n Patient must be aware of this for their protection Victim-witness assistance programs are available n Know resources in your community 98
Legal Considerations for Sexual Assault n Take steps to preserve any evidence n n n use paper not plastic bags Patient should not urinate, defecate, douche, bathe Notify law enforcement as soon as possible Remember there will be a “chain of evidence” Follow local & state protocols 99
Resources and Support n n Nationwide 24 hour hotline toll-free for domestic violence n 1 -800 -799 -SAFE (7233) n TDD # 1 -800 -787 -3224 Elder abuse hotline n Elder defined as 60 or older n 1 -800 -252 -8966 (M-F 0830 -1700) n 1 -800 -279 -0400 (all other times) n DCFS - 1 -800 -25 -abuse (800 -252 -2873) 100
EMS Responsibilities n n Document objectively EMS mandated by the State to report all cases of domestic violence to local police EMS mandated to offer a referral brochure to all patients that sign a release Document all efforts offered and all reports made to other non-EMS parties 101
102
- Slides: 102