Curriculum for the Hospitalized Aging Medical Patient CHAMP

- Slides: 63
Curriculum for the Hospitalized Aging Medical Patient CHAMP Drugs and Aging Paula M. Podrazik, MD University of Chicago
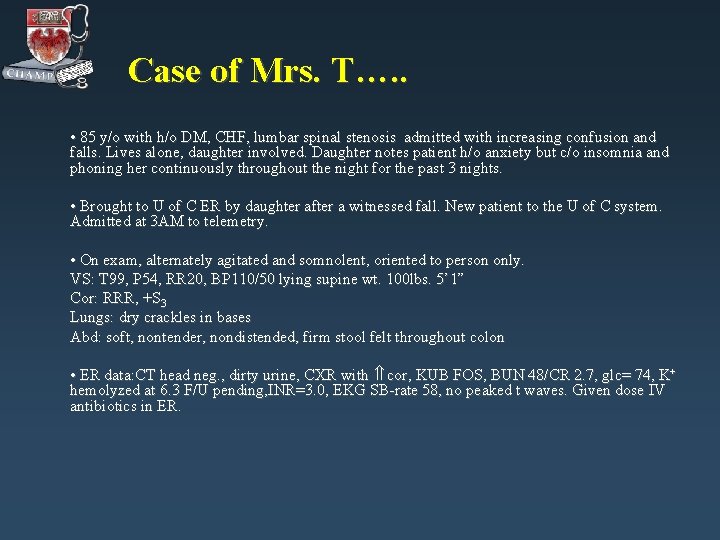
Case of Mrs. T…. . • 85 y/o with h/o DM, CHF, lumbar spinal stenosis admitted with increasing confusion and falls. Lives alone, daughter involved. Daughter notes patient h/o anxiety but c/o insomnia and phoning her continuously throughout the night for the past 3 nights. • Brought to U of C ER by daughter after a witnessed fall. New patient to the U of C system. Admitted at 3 AM to telemetry. • On exam, alternately agitated and somnolent, oriented to person only. VS: T 99, P 54, RR 20, BP 110/50 lying supine wt. 100 lbs. 5’ 1” Cor: RRR, +S 3 Lungs: dry crackles in bases Abd: soft, nontender, nondistended, firm stool felt throughout colon • ER data: CT head neg. , dirty urine, CXR with cor, KUB FOS, BUN 48/CR 2. 7, glc= 74, K+ hemolyzed at 6. 3 F/U pending, INR=3. 0, EKG SB-rate 58, no peaked t waves. Given dose IV antibiotics in ER.
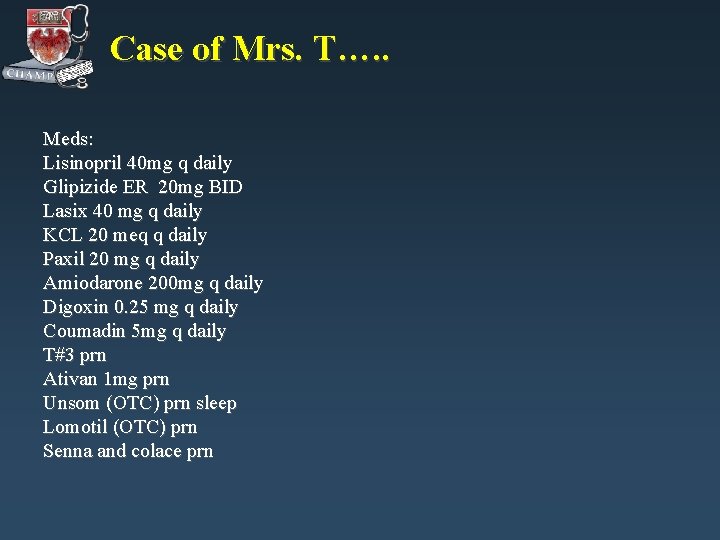
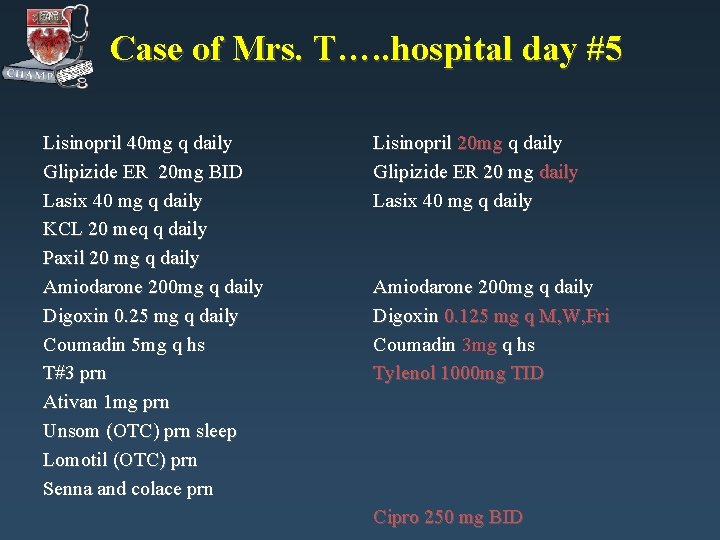
Case of Mrs. T…. . Meds: Lisinopril 40 mg q daily Glipizide ER 20 mg BID Lasix 40 mg q daily KCL 20 meq q daily Paxil 20 mg q daily Amiodarone 200 mg q daily Digoxin 0. 25 mg q daily Coumadin 5 mg q daily T#3 prn Ativan 1 mg prn Unsom (OTC) prn sleep Lomotil (OTC) prn Senna and colace prn
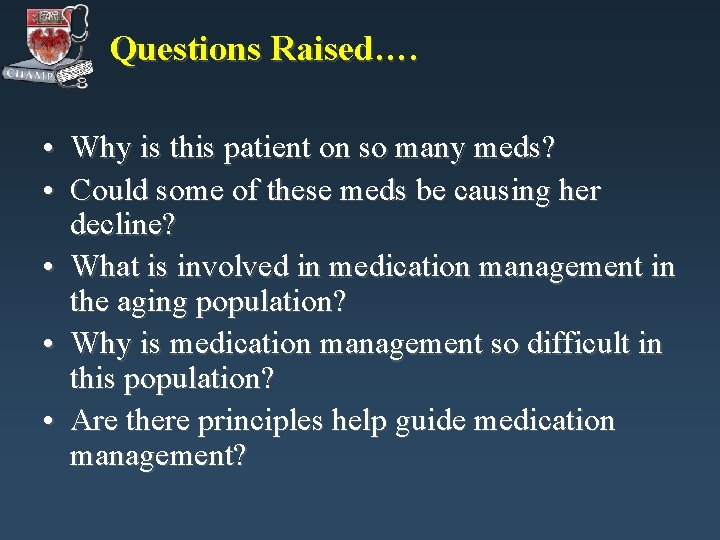
Questions Raised…. • Why is this patient on so many meds? • Could some of these meds be causing her decline? • What is involved in medication management in the aging population? • Why is medication management so difficult in this population? • Are there principles help guide medication management?

Drugs and Aging: Topics for Review • • Information Gap Aging Pharmacology Polypharmacy Drugs to Avoid Adverse Drug Reactions Cost Compliance Medication Review
Drugs and Aging • • Information Gap Aging Pharmacology Polypharmacy Drugs to Avoid Adverse Drug Reactions Cost Compliance Medication Review
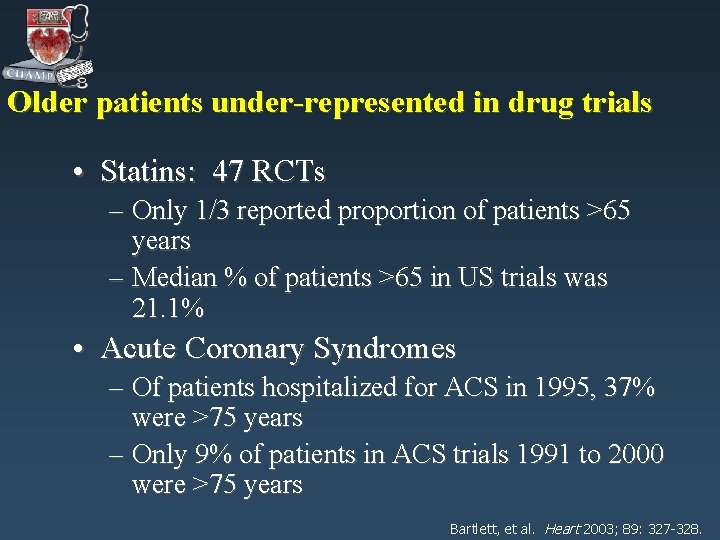
Older patients under-represented in drug trials • Statins: 47 RCTs – Only 1/3 reported proportion of patients >65 years – Median % of patients >65 in US trials was 21. 1% • Acute Coronary Syndromes – Of patients hospitalized for ACS in 1995, 37% were >75 years – Only 9% of patients in ACS trials 1991 to 2000 were >75 years Bartlett, et al. Heart 2003; 89: 327 -328.
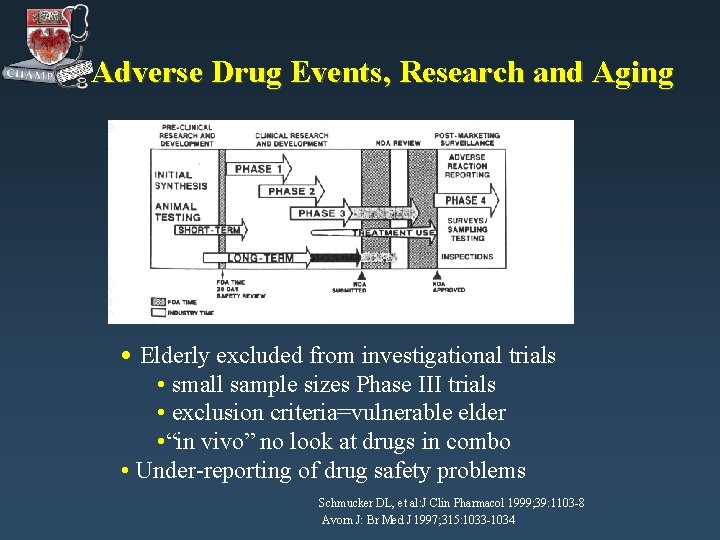
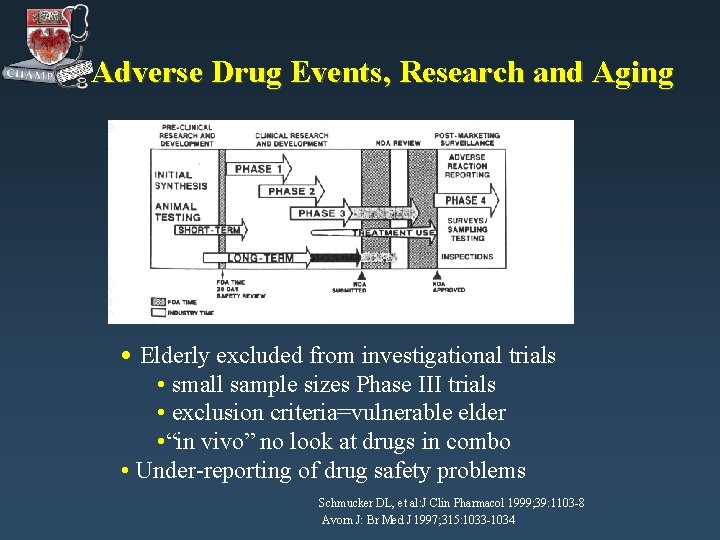
Adverse Drug Events, Research and Aging • Elderly excluded from investigational trials • small sample sizes Phase III trials • exclusion criteria=vulnerable elder • “in vivo” no look at drugs in combo • Under-reporting of drug safety problems Schmucker DL, et al: J Clin Pharmacol 1999; 39: 1103 -8 Avorn J: Br Med J 1997; 315: 1033 -1034
Drugs and Aging • • Information Gap Aging Pharmacology Adverse Drug Reactions Drugs to Avoid Polypharmacy Cost Compliance Medication Review
Aging Pharmacology: Objectives • Definitions • Pharmacokinetics – Aging & drug absorption – Aging drug distribution – Aging & Drug Clearance • Renal Metabolism • Hepatic Biotransformation • Pharmacodynamics
Drug Absorption with Normal Aging • • • in gastric p. H, motility, absorptive surface gastric emptying time May see slower absorption, time to effect Bottom line: No clinically sign. age-related change in drug absorption with normal aging.
Drug Distribution with Aging • • • body fat to age 60 -70 antipsychotics, TCAs in lean body mass and fat after 70 digoxin conc. protein-binding can effect Vd warfain + amiodarone, phenytoin, ketaconazole Bottom Line: Drug dosing is a dynamic process with aging.
Hepatic Biotransformation and Aging • Age- related decline – Reduction in liver blood flow • High-clearance drugs affected: propanolol, labetolol, esmolol, lidocaine – Reduction in hepatic oxidation: CYP 450 • No age-related changes – Hepatic acetylation – Hepatic conjugation
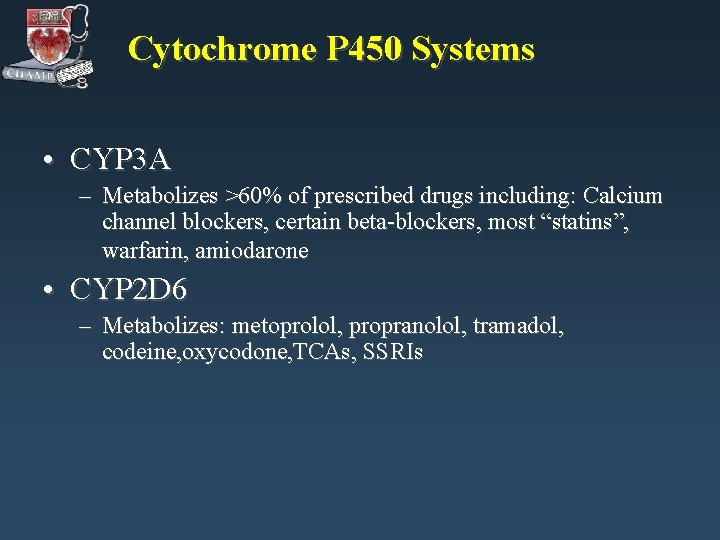
Cytochrome P 450 Systems • CYP 3 A – Metabolizes >60% of prescribed drugs including: Calcium channel blockers, certain beta-blockers, most “statins”, warfarin, amiodarone • CYP 2 D 6 – Metabolizes: metoprolol, propranolol, tramadol, codeine, oxycodone, TCAs, SSRIs
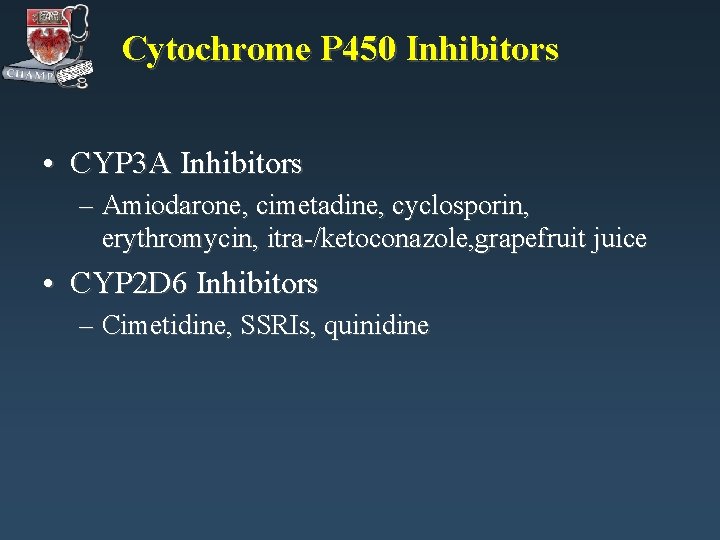
Cytochrome P 450 Inhibitors • CYP 3 A Inhibitors – Amiodarone, cimetadine, cyclosporin, erythromycin, itra-/ketoconazole, grapefruit juice • CYP 2 D 6 Inhibitors – Cimetidine, SSRIs, quinidine
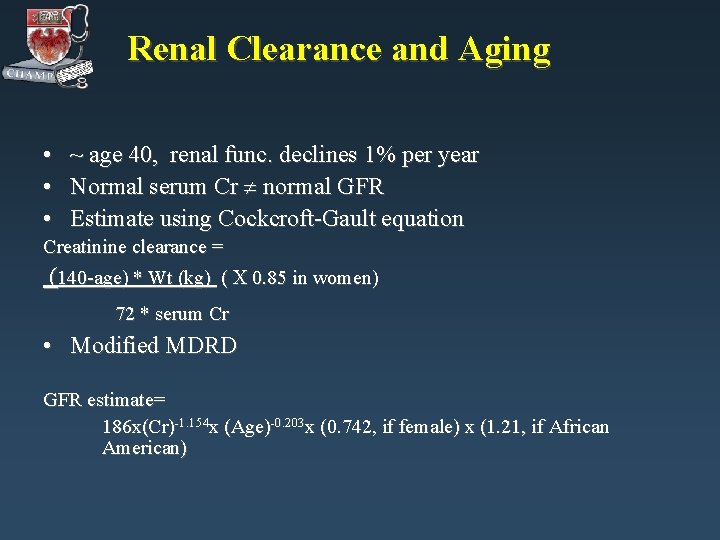
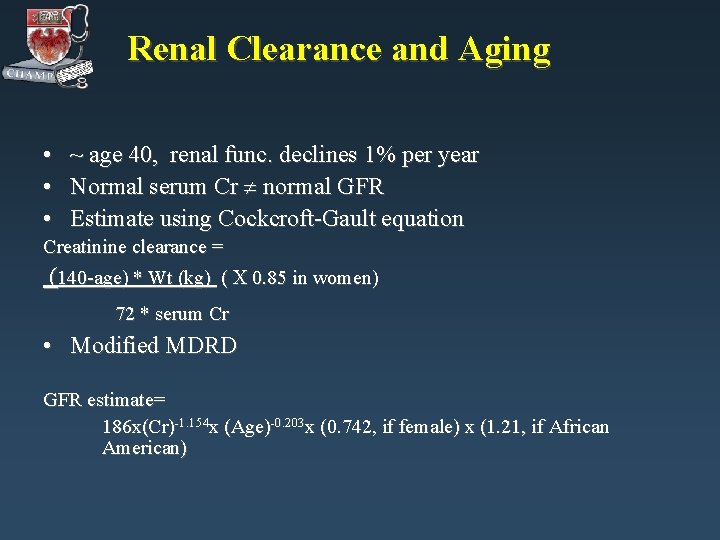
Renal Clearance and Aging • ~ age 40, renal func. declines 1% per year • Normal serum Cr normal GFR • Estimate using Cockcroft-Gault equation Creatinine clearance = (140 -age) * Wt (kg) ( 0. 85 in women) 72 * serum Cr • Modified MDRD GFR estimate= 186 x(Cr)-1. 154 x (Age)-0. 203 x (0. 742, if female) x (1. 21, if African American)
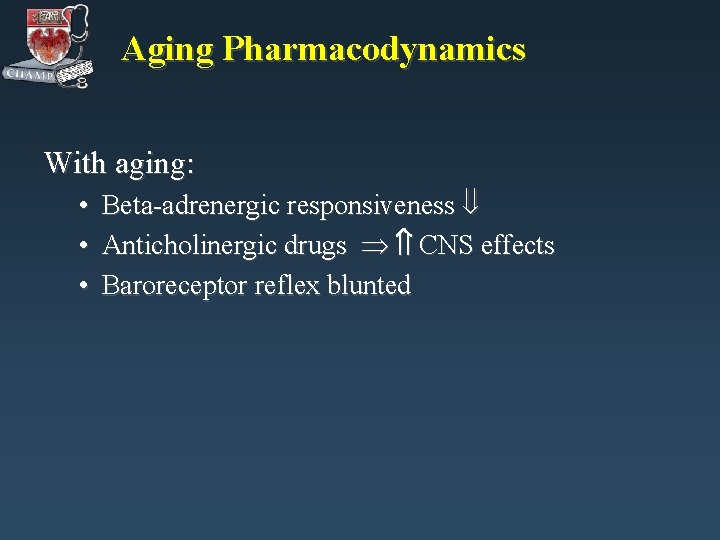
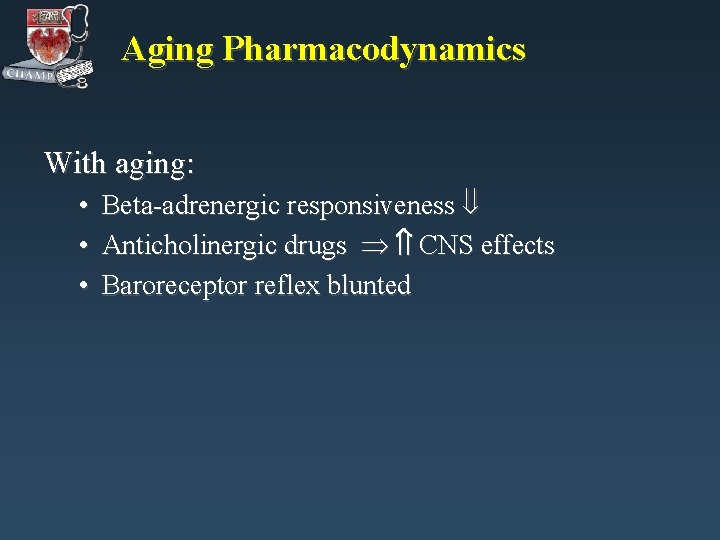
Aging Pharmacodynamics With aging: • Beta-adrenergic responsiveness • Anticholinergic drugs CNS effects • Baroreceptor reflex blunted
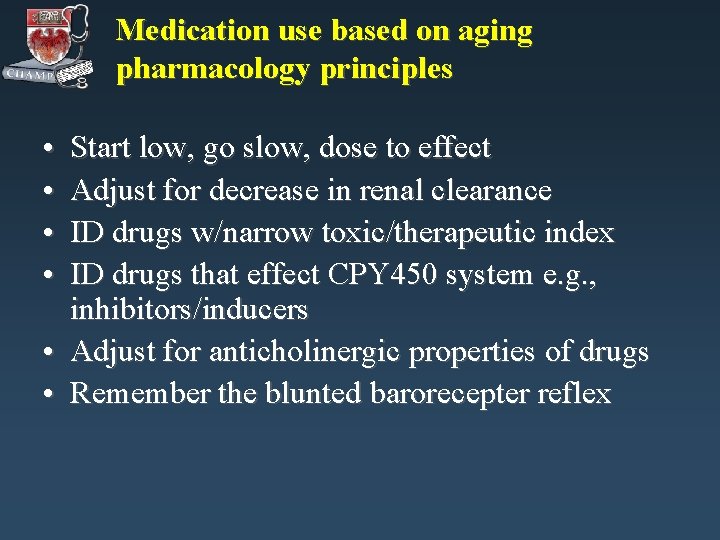
Medication use based on aging pharmacology principles • • Start low, go slow, dose to effect Adjust for decrease in renal clearance ID drugs w/narrow toxic/therapeutic index ID drugs that effect CPY 450 system e. g. , inhibitors/inducers • Adjust for anticholinergic properties of drugs • Remember the blunted barorecepter reflex
Drugs and Aging • • Information Gap Aging Pharmacology Polypharmacy Adverse Drug Reactions Drugs to Avoid Cost Compliance Medication Review
Case of Mrs. K…. . 75 y o F with CAD, HTN, OP, LBP Walks 1 mile 3 x per week & Tai Chi 2 x per week & water aerobics class 1 x per week Med list: asa 81 q day lisinopril 20 q day atenolol 25 q day hctz 25 q day lipitor (atorvastatin) 10 q day fosamax (alendronate) 70 mg q week MVI q day tums 3 q day vicodin (hydrocodone/acetaminophen) prn
What is the prevalence of drug use in the elderly? • Ambulatory adults > 65 surveyed – 12% take > 10 meds – 50% take 5 or > meds Kaufman DW, et al The Slone survey. JAMA 2002; 287: 337. .
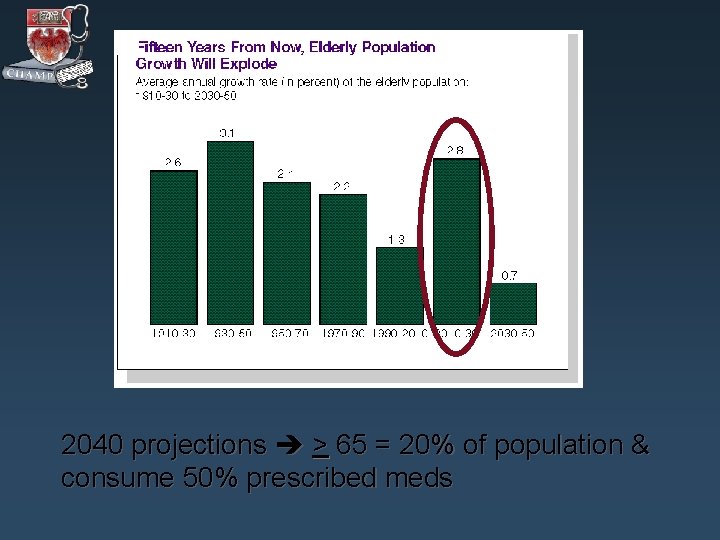
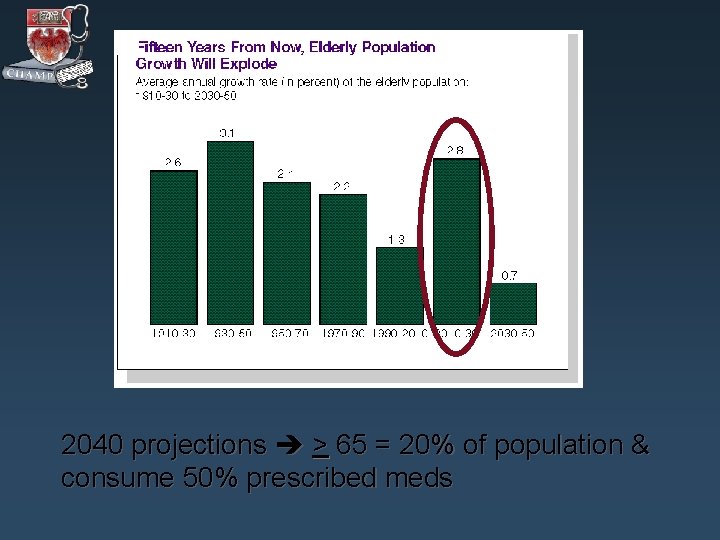
2040 projections > 65 = 20% of population & consume 50% prescribed meds
Will polypharmacy continue to escalate?
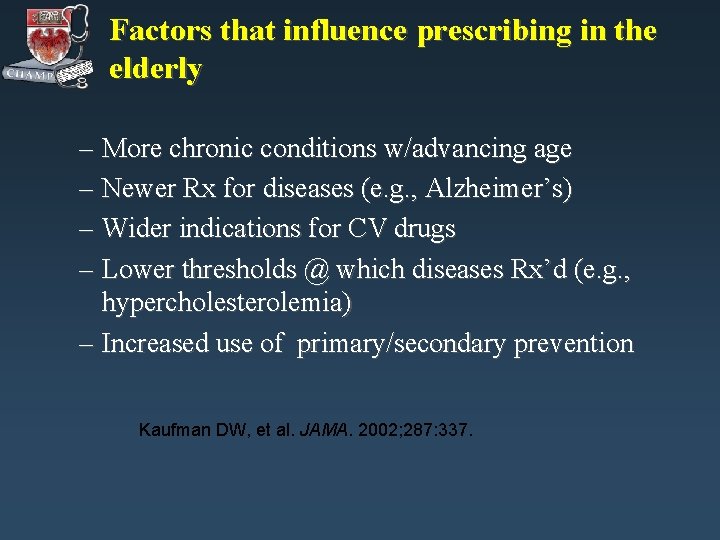
Factors that influence prescribing in the elderly – More chronic conditions w/advancing age – Newer Rx for diseases (e. g. , Alzheimer’s) – Wider indications for CV drugs – Lower thresholds @ which diseases Rx’d (e. g. , hypercholesterolemia) – Increased use of primary/secondary prevention Kaufman DW, et al. JAMA. 2002; 287: 337.
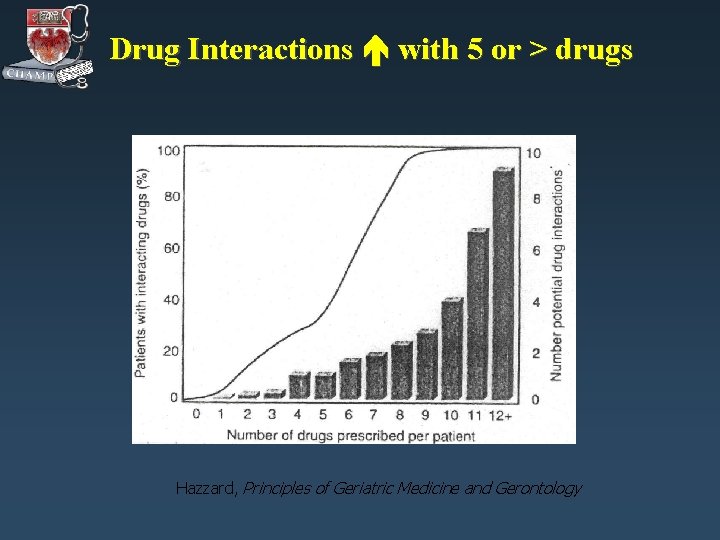
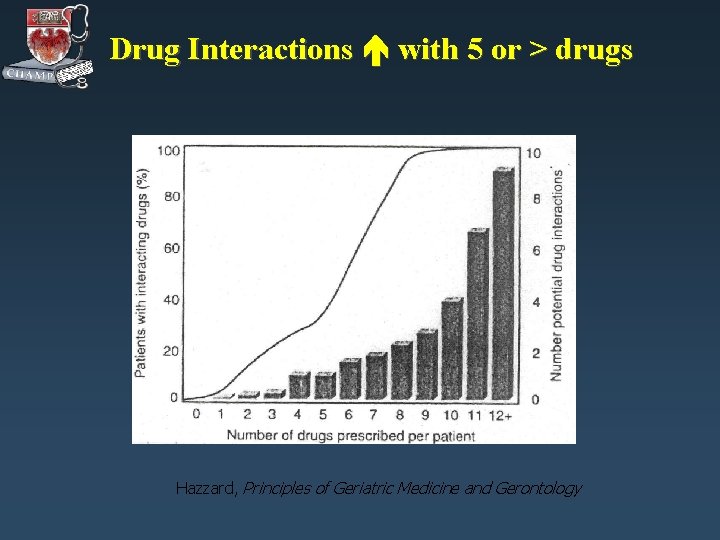
Drug Interactions with 5 or > drugs Hazzard, Principles of Geriatric Medicine and Gerontology
Polypharmacy definitions? • > 5 medications used • Concurrent use of multiple prescriptions & over-the-counter meds • Definitions w/measure of "appropriateness" – Use of one med to treat adverse effects of another – Medical regimen includes > one unnecessary med – Use of more meds than clinically indicated
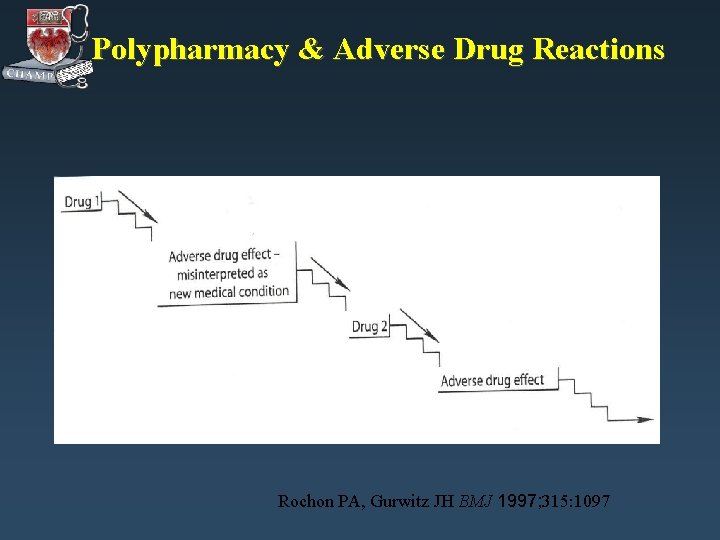
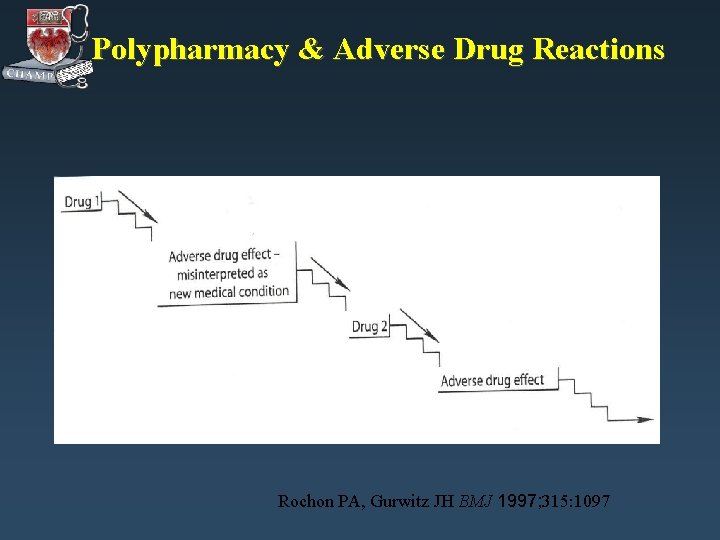
Polypharmacy & Adverse Drug Reactions Rochon PA, Gurwitz JH BMJ 1997; 315: 1097
What is the risk of polypharmacy? • Risk of drug-drug interactions increases with increasing # of meds • Up to 73% of ADRs involved unnecessary meds • 10 -17% of hospital admissions due to ADEs Bergendal L, et al. Pharm World Sci. 1995; 17: 152. Lindley CM. et al. Ageing. 1992; 21: 294. Beard K. Drugs Ageing. 1992; 2: 356.
Drugs and Aging • • Information Gap Aging Pharmacology Polypharmacy Drugs to Avoid Adverse Drug Reactions Cost Compliance Medication Review
Explicit Criteria --Beers • List of medications to avoid in elderly nursing home patients • Developed by consensus panel in 1991 • Updated in 1997 and 2002 Beers, et al. Arch Intern Med 1991; 151: 1825 -1832. Beers MH. Arch Intern Med 1997; 157(14): 1531 -1536. Fick DM, et al. Arch Int Med 2003; 163: 2716 -24.
Drugs to Avoid in the Elderly Drug Classes/Drugs • antihistamines • antispasmodics • certain CV meds – methyldopa, (Aldomet. TM), reserpine – disopyramide (Norpace. TM) – dipyridamole (Persantine. TM) • certain psychotropics – amitriptyline( Elavil. TM), doxepin (Sinequan. TM) – meprobamate(Miltown. TM), diazepam, flurazepam (Dalmane. TM), barbs Beers MH Arch Intern Med 1997; 157: 1531 -1536
Drugs to Avoid in the Elderly Drug Classes/Drugs • certain analgesics – propoxyphene (Darvon. TM) – merperidine (Demerol. TM) – pentazocine (Talwin. TM) • • • chlorpropamide (Diabenase. TM) trimethobenzamide (Tigan. TM) certain anti-inflammatory agents – indomethacin (Indocin. TM), ketorolac (Toradol. TM), piroxicam(Feldene. TM) Beers MH Arch Intern Med 1997; 157: 1531 -1536
Interactions to Beware Drug-Disease Interactions to Avoid dementia, falls + benzodiazepines BPH, constipation + antihistamines, antispasmodics, TCAs CRF, CHF, PUD + NSAIDS DM + steroids asthma, COPD, PVD, HB + beta blockers Beers MH Arch Intern Med 1997; 157: 1531 -1536
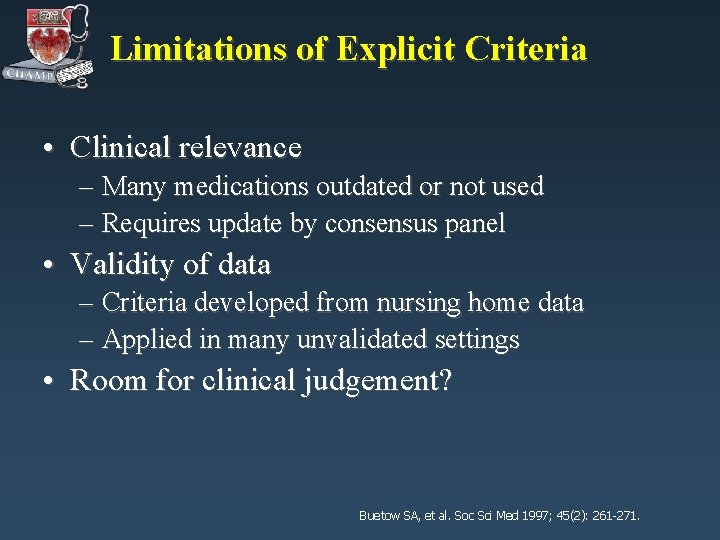
Limitations of Explicit Criteria • Clinical relevance – Many medications outdated or not used – Requires update by consensus panel • Validity of data – Criteria developed from nursing home data – Applied in many unvalidated settings • Room for clinical judgement? Buetow SA, et al. Soc Sci Med 1997; 45(2): 261 -271.
Drugs and Aging • • Information Gap Aging Pharmacology Polypharmacy Drugs to Avoid Adverse Drug Reactions Cost Compliance Medication Review
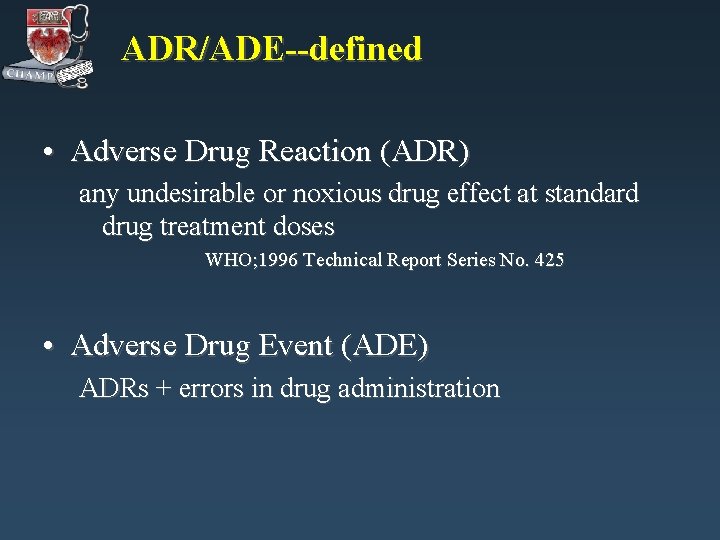
ADR/ADE--defined • Adverse Drug Reaction (ADR) any undesirable or noxious drug effect at standard drug treatment doses WHO; 1996 Technical Report Series No. 425 • Adverse Drug Event (ADE) ADRs + errors in drug administration
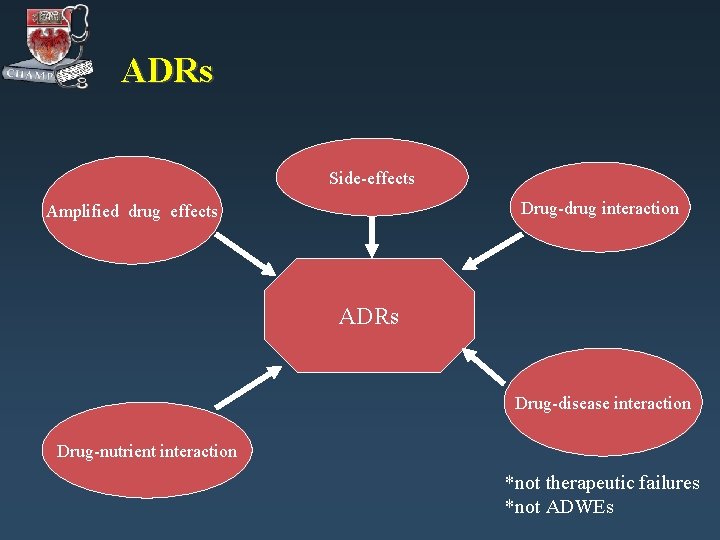
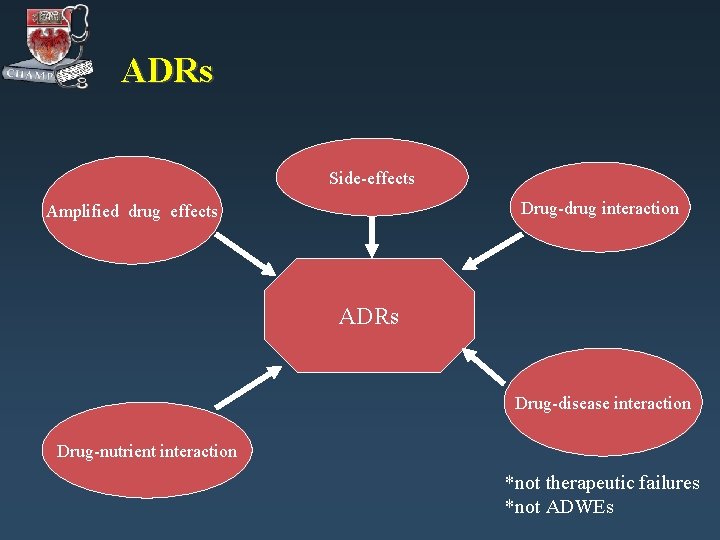
ADRs Side-effects Drug-drug interaction Amplified drug effects ADRs Drug-disease interaction Drug-nutrient interaction *not therapeutic failures *not ADWEs
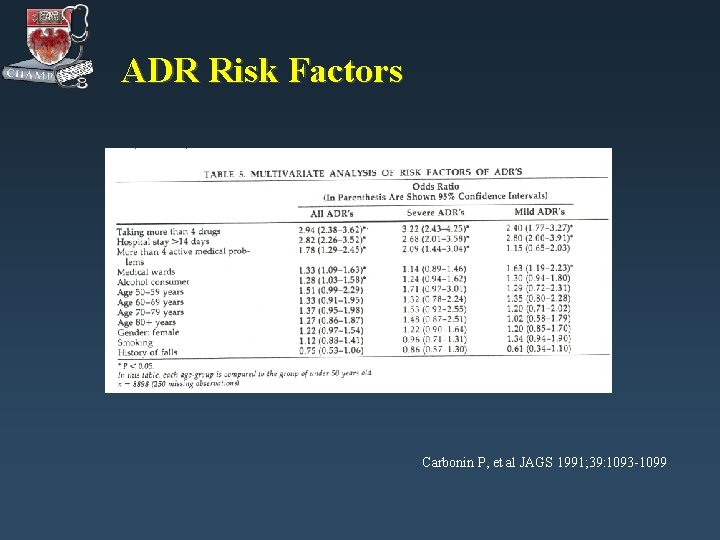
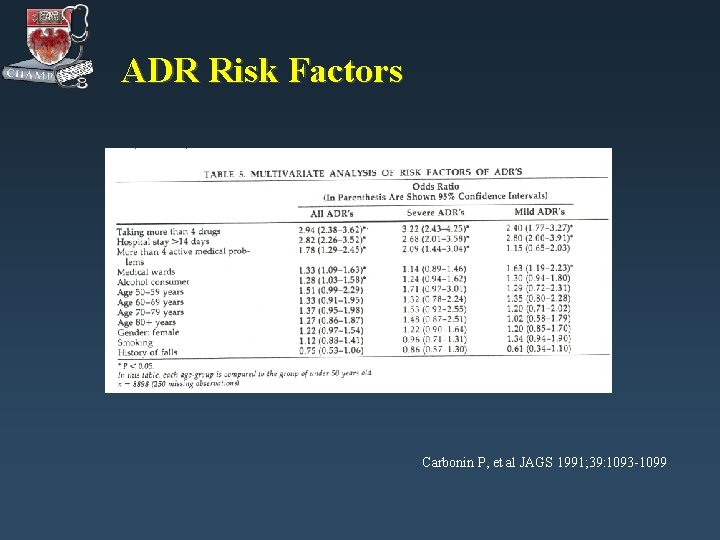
ADR Risk Factors Carbonin P, et al JAGS 1991; 39: 1093 -1099
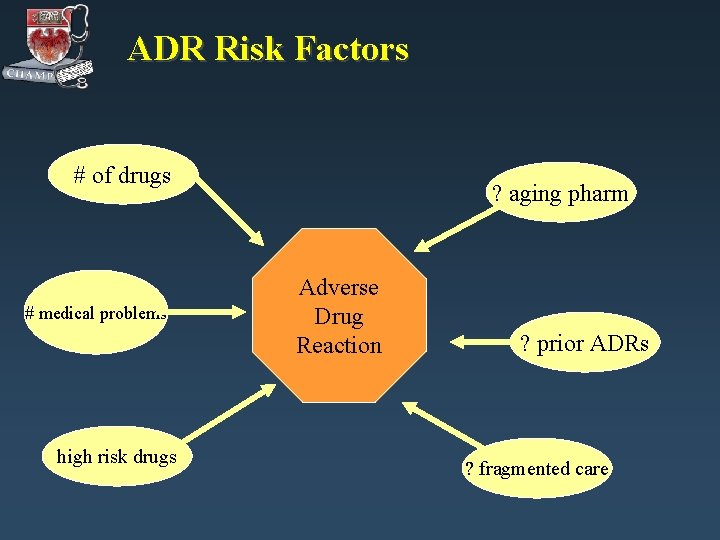
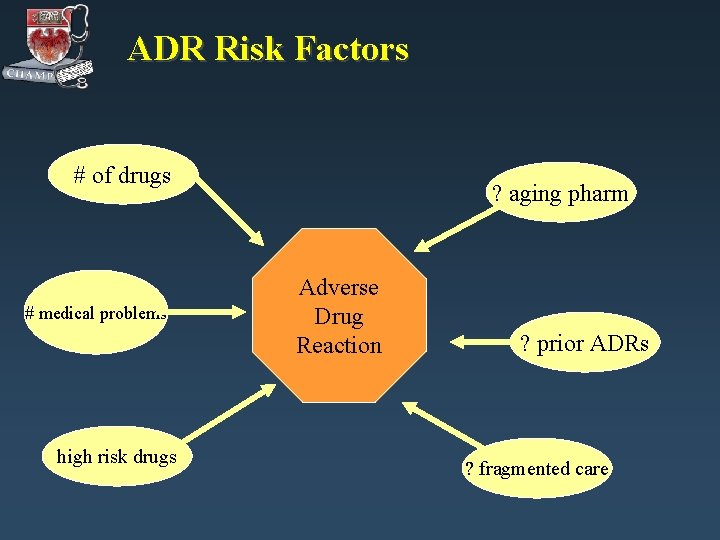
ADR Risk Factors # of drugs # medical problems high risk drugs ? aging pharm Adverse Drug Reaction ? prior ADRs ? fragmented care
ADEs and Hospitalization Recent inhospital studies look at ADEs How big a problem? • 4 th-6 th leading cause of hospital death (serious ADRs 6. 2%, fatal ADRs 0. 32%) • Increased length of stay • Increased cost Lazarou J, et al JAMA 1998; 280(20): 1741 -44 Classen D, et al JAMA 1997; 277(4): 301 -6
Drugs and Aging • • Information Gap Aging Pharmacology Adverse Drug Reactions Drugs to Avoid Polypharmacy Cost Compliance Medication Review
Drugs and Aging: Cost • Important to ask: “How do you pay for your medications? ” • Federal poverty level: $10, 400 for individual, $14, 000 for couple • Potential sources of aid: Medicare Part D, Medicaid, Circuit Breaker, Illinois Care Rx, Rx buying club, manufacturer-sponsored programs
Drugs and Aging • • Information Gap Aging Pharmacology Adverse Drug Reactions Drugs to Avoid Polypharmacy Cost Compliance Medication Review
Compliance • • • Compliance Adherence Concordance Non-adherence 25 to 59% in the elderly Factors associated with non-adherence – Physical impairment – Psychosocial risks – Medication related factors • Higher risk of re-hospitalization • Risk of noncompliance after discharge Ryan AA. Int’l J Nursing Studies 1999; 36: 153 -62. Van Eijken M, et al. Drugs & Aging 2003; 20: 229 -40.
Drugs and Aging • • Information Gap Aging Pharmacology Adverse Drug Reactions Drugs to Avoid Polypharmacy Cost Compliance Medication Review
Strategies for improving quality of medication use in the elderly • Medication Review – Implicit criteria vs. explicit criteria • • Enlisting the pharmacist Use of the CPOE Enlisting the patient Simplifying administration – – – Polypill Single daily dosing Pill organizers
Medication Review • Explicit criteria – Drugs/classes of drugs w/high risk/ low benefit – U. S. example: Beers drugs-to-avoid criteria • Requires updating • Validity of data in other settings? • ? Room for clinical judgment/ "patient-centered" care • Implicit criteria – IDs individual elements of prescribing as inappropriate e. g. , MAI – Time consuming, pharmacist driven Fick DM, et al. Arch Int Med. 2003; 163: 2716. Hanlon JT, et al. J Clin Epidemiol 1992; 45: 1045. Samsa GP, et al. J Clin Epidemiol 1994; 47: 891.
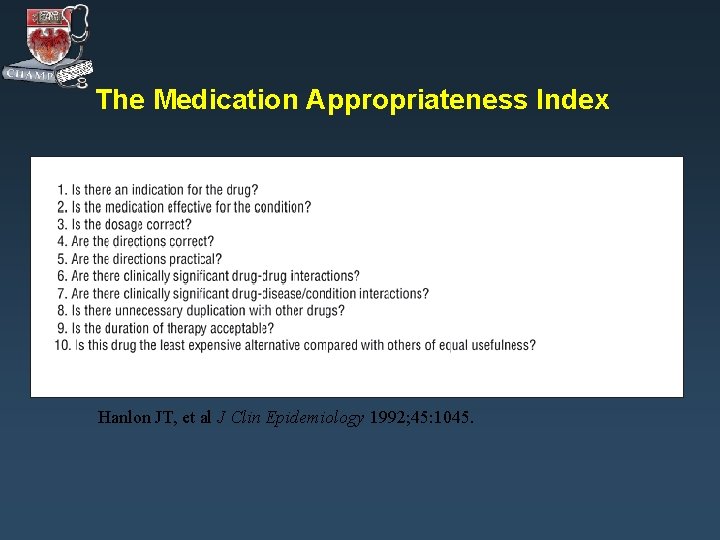
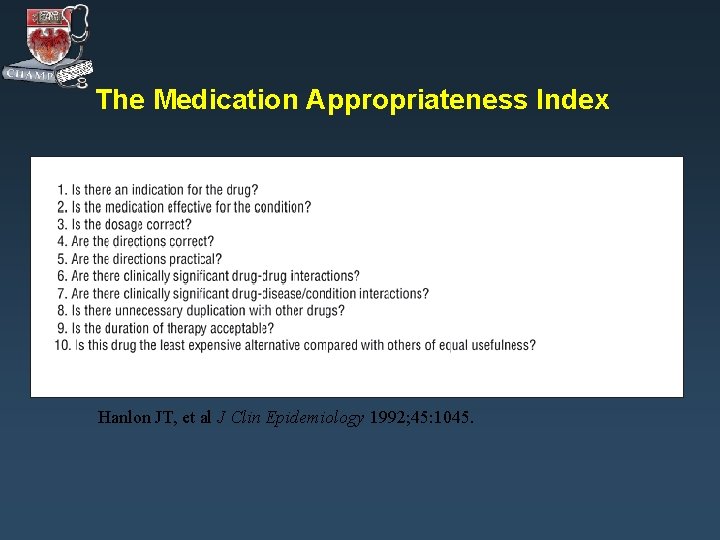
The Medication Appropriateness Index Hanlon JT, et al J Clin Epidemiology 1992; 45: 1045.
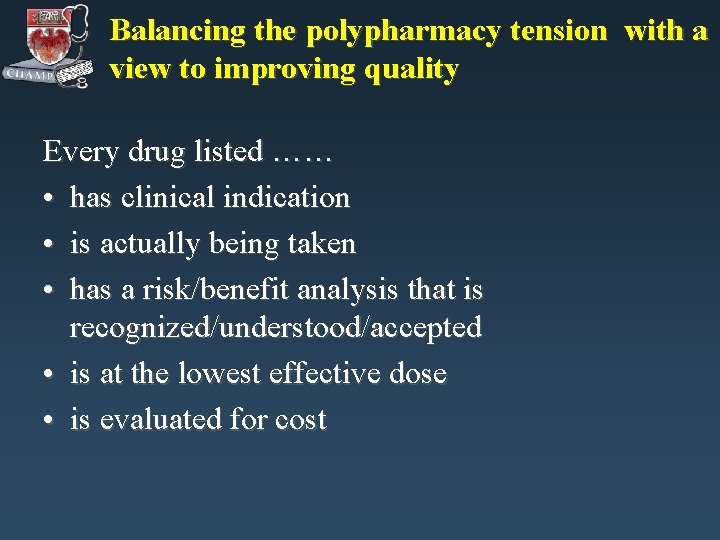
Balancing the polypharmacy tension with a view to improving quality Every drug listed …… • has clinical indication • is actually being taken • has a risk/benefit analysis that is recognized/understood/accepted • is at the lowest effective dose • is evaluated for cost
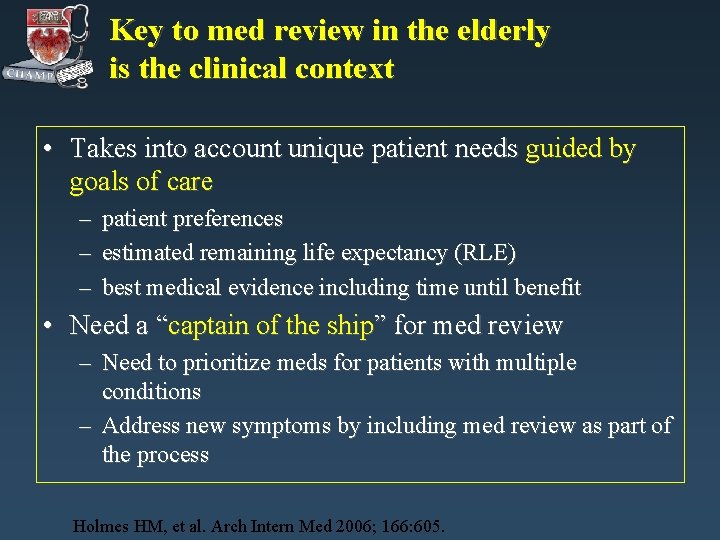
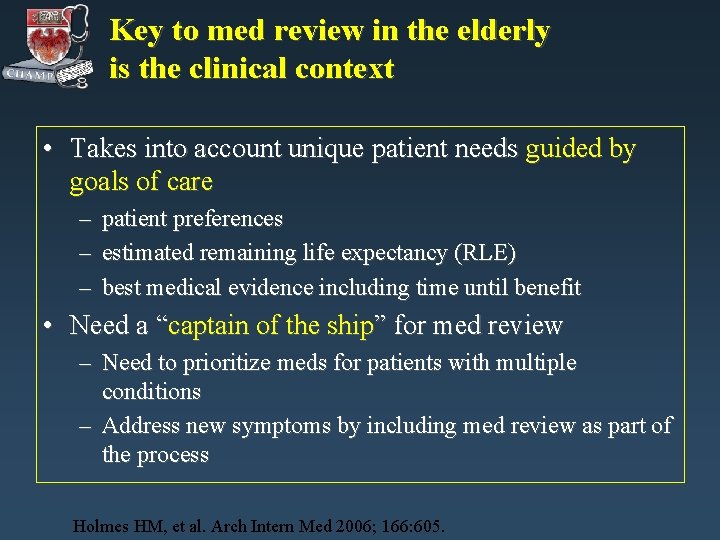
Key to med review in the elderly is the clinical context • Takes into account unique patient needs guided by goals of care – patient preferences – estimated remaining life expectancy (RLE) – best medical evidence including time until benefit • Need a “captain of the ship” for med review – Need to prioritize meds for patients with multiple conditions – Address new symptoms by including med review as part of the process Holmes HM, et al. Arch Intern Med 2006; 166: 605.
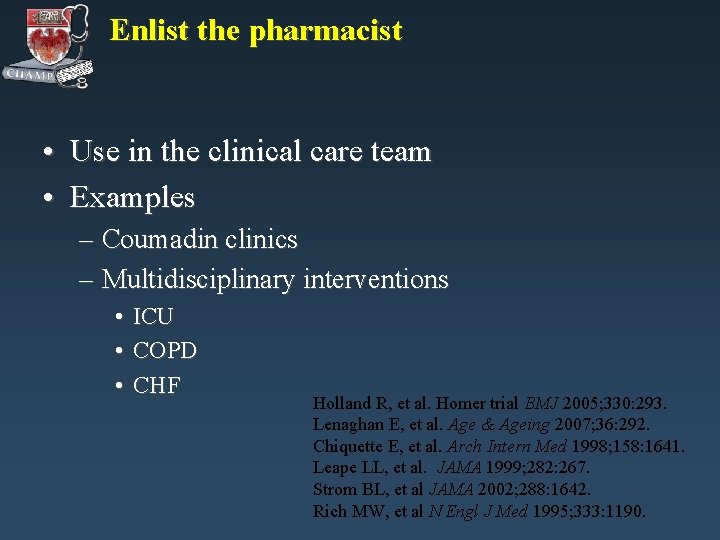
Enlist the pharmacist • Use in the clinical care team • Examples – Coumadin clinics – Multidisciplinary interventions • • • ICU COPD CHF Holland R, et al. Homer trial BMJ 2005; 330: 293. Lenaghan E, et al. Age & Ageing 2007; 36: 292. Chiquette E, et al. Arch Intern Med 1998; 158: 1641. Leape LL, et al. JAMA 1999; 282: 267. Strom BL, et al JAMA 2002; 288: 1642. Rich MW, et al N Engl J Med 1995; 333: 1190.
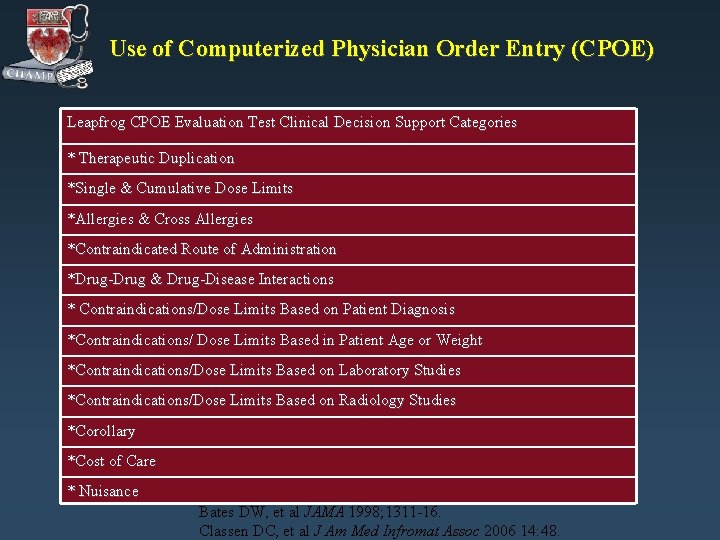
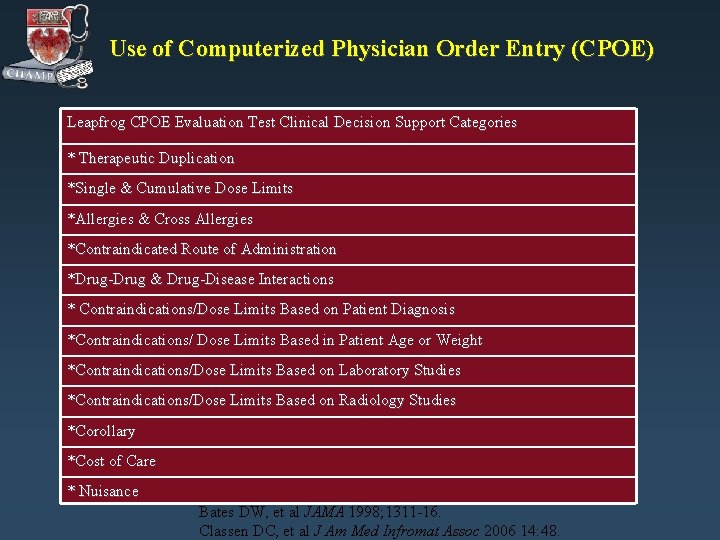
Use of Computerized Physician Order Entry (CPOE) Leapfrog CPOE Evaluation Test Clinical Decision Support Categories * Therapeutic Duplication *Single & Cumulative Dose Limits *Allergies & Cross Allergies *Contraindicated Route of Administration *Drug-Drug & Drug-Disease Interactions * Contraindications/Dose Limits Based on Patient Diagnosis *Contraindications/ Dose Limits Based in Patient Age or Weight *Contraindications/Dose Limits Based on Laboratory Studies *Contraindications/Dose Limits Based on Radiology Studies *Corollary *Cost of Care * Nuisance Bates DW, et al JAMA 1998; 1311 -16. Classen DC, et al J Am Med Infromat Assoc 2006 14: 48.
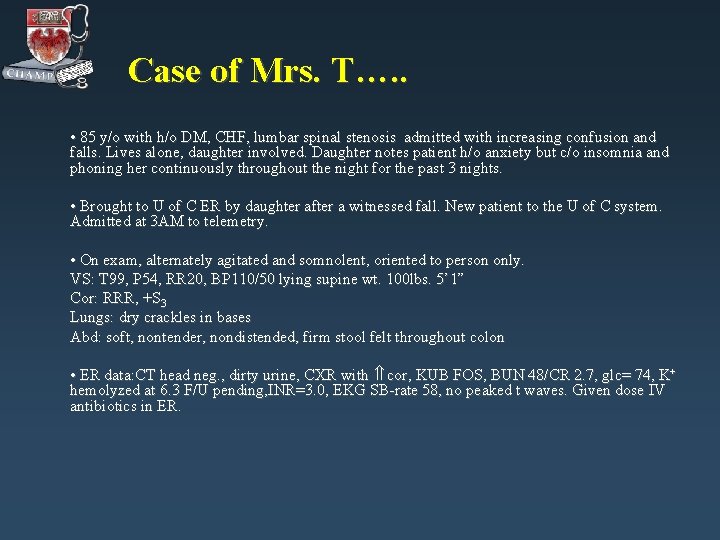
Case of Mrs. T…. . • 85 y/o with h/o DM, CHF, lumbar spinal stenosis admitted with increasing confusion and falls. Lives alone, daughter involved. Daughter notes patient h/o anxiety but c/o insomnia and phoning her continuously throughout the night for the past 3 nights. • Brought to U of C ER by daughter after a witnessed fall. New patient to the U of C system. Admitted at 3 AM to telemetry. • On exam, alternately agitated and somnolent, oriented to person only. VS: T 99, P 54, RR 20, BP 110/50 lying supine wt. 100 lbs. 5’ 1” Cor: RRR, +S 3 Lungs: dry crackles in bases Abd: soft, nontender, nondistended, firm stool felt throughout colon • ER data: CT head neg. , dirty urine, CXR with cor, KUB FOS, BUN 48/CR 2. 7, glc= 74, K+ hemolyzed at 6. 3 F/U pending, INR=3. 0, EKG SB-rate 58, no peaked t waves. Given dose IV antibiotics in ER.
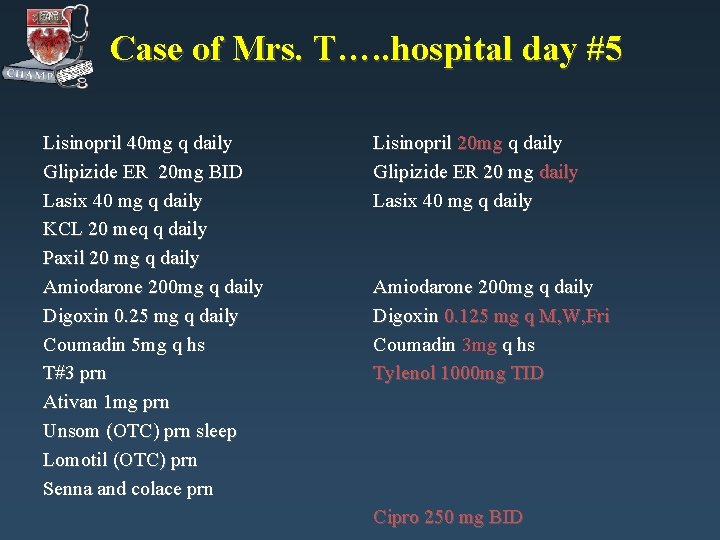
Case of Mrs. T…. . hospital day #5 Lisinopril 40 mg q daily Glipizide ER 20 mg BID Lasix 40 mg q daily KCL 20 meq q daily Paxil 20 mg q daily Amiodarone 200 mg q daily Digoxin 0. 25 mg q daily Coumadin 5 mg q hs T#3 prn Ativan 1 mg prn Unsom (OTC) prn sleep Lomotil (OTC) prn Senna and colace prn Lisinopril 20 mg q daily Glipizide ER 20 mg daily Lasix 40 mg q daily Amiodarone 200 mg q daily Digoxin 0. 125 mg q M, W, Fri Coumadin 3 mg q hs Tylenol 1000 mg TID Cipro 250 mg BID
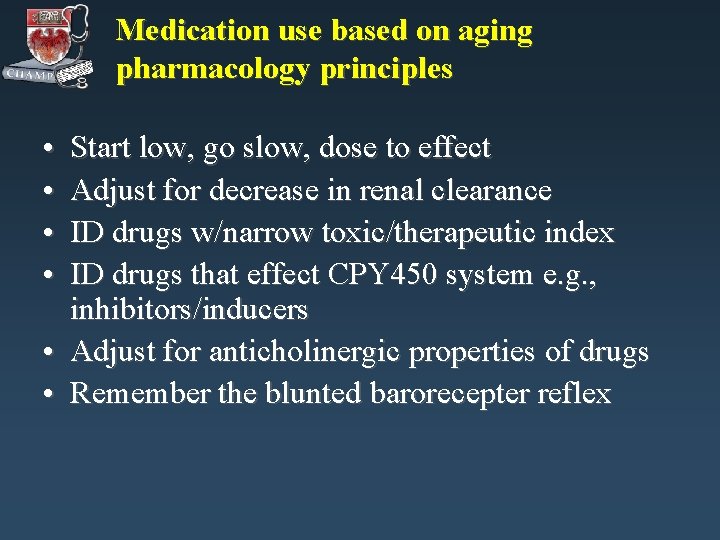
Medication use based on aging pharmacology principles • • Start low, go slow, dose to effect Adjust for decrease in renal clearance ID drugs w/narrow toxic/therapeutic index ID drugs that effect CPY 450 system e. g. , inhibitors/inducers • Adjust for anticholinergic properties of drugs • Remember the blunted barorecepter reflex
Med Review: Intersecting Safeties • • PCP plays key role in med review (prioritize & individualize) New symptom consider a medication in the D/Dx Meds on list guided by goals of care Review meds on list for – – – Indication Dose Interactions—drug/drug & drug/disease Duplications Adherence Cost • Enlist the pharmacist • Enlist a CPOE system • Review for medication underuse
Into the future…… • Increase knowledge base on drugs in the elderly – Clinical trials vs. post marketing surveillance • Broaden testing/implementation of technologies e. g. , CPOE • Multidisciplinary monitoring • Support continued affordable drug coverage
Special Thanks • CHAMP core faculty • Holly Holmes, MD • Visit our website @http: //champ. bsd. uchicago. edu
CHAMP: Drugs and Aging Bibliography 1. 2. 3. 4. 5. 6. 7. Bates DW, et al: The cost of adverse drug events in hospitalized patients. JAMA 1997; 277: 307 -11. Bates DW, et al: Incidence of adverse drug events and potential adverse drug events: implications for prevention. JAMA 1995; 274: 29 -34. Beers, MH, Ouslander JG, Rollingher I, Reuben DB, Brooks, J, Beck JC. : Explicit criteria for determining inappropriate medication use in nursing home residents. Arch Intern Med 1991; 151: 1825 -1832. . Beers MH: Explicit criteria for determining potentially inappropriate medication use by the elderly: an update Arch Intern Med 1997; 157(14): 1531 -36. Beers MH. : Inappropriate medication prescribing in skilled-nursing facilities. Ann Intern Med. 1992 Oct 15; 117(8): 684 -689. Buetow SA, Sibbald B, Cantrill JA, Halliwell S. : Appropriateness in health care: application to prescribing. Soc Sci Med 1997; 45(2): 261 -271. Beyth RJ, et al: Principles of drug therapy in older adults: rational drug prescribing. Clin Ger med 2002; 18: 577 -92.
CHAMP: Drugs and Aging Bibliography 8. Chrischilles EA, et al: Use of medications by persons 65 and over: data from the established populations for the epidemiologic studies of the elderly. J Gerontol 1992; M 137 M 144. 9. Chin MH, Wang LC, Jin L, Mulliken R, Walter J, Hayley DC, Karrison TG, Nerney MP, Miller A, Friedmann PD. : Appropriateness of medication selection for older persons in an urban academic emergency department. Academic Emergency Medicine 1999; 6: 1232 -1242. 10. Classen DC, et al: Adverse drug events in hospitalized patients: excess length of stay, extra costs, and attributable mortality. JAMA 1997; 277: 301 -6. 11. Doucet J, et al: Drug-drug interactions related to hospital admissions in older adults: a prospective study of 1000 patients. J Am Geriatr Soc 1996; 44: 944 -48.
CHAMP: Drugs and Aging Bibliography Fick DM, Cooper JW, Wade WE, Waller JL, Maclean R, Beers MH. Updating the Beers Criteria for potentially inappropriate medication use in older adults. Arch Int Med 2003; 163: 2716 -24. 13. Gurwitz JH, Field TS, Avorn J, Mc. Cormick D, Jain S, Eckler M, Benser M, Edmondson AC, Bates DW. Incidence and preventability of adverse drug events in nursing homes. Am J Med 2000; 109: 87 -94. 14. Hanlon JT, et al: A method for assssing drug therapy appropriateness. J Clin Epidemiol 1992; 45: 1045 -51. 15. Hanlon JT, Artz MB, Pieper CF, et al. Inappropriate medication use among frail elderly inpatients. Ann Pharmacother 2004; 38: 9 -14. 16. Inouye SK, et al: Precipitating factors for delirium in hospitalized elderly persons: predictive model and interrelationship with baseline vulnerability. JAMA 1996; 275: 852 -57. 17. Kroenke K: Polypharmacy : causes, consequences, and cure. Am J Med 1985; 79: 149 -52. 12.
CHAMP: Drugs and Aging Bibliography 18. 19. 20. 21. 22. 23. 24. Kaiser Family Foundation. Views of the new Medicare drug law: a survey of people on Medicare. August 2004. Lazarou J, et al: Incidence of adverse drug reactions inhospitalized patients: a meta-analysis of prospective studies. JAMA 1998; 279: 1200 -5. Leape L: Reporting of adverse events. NEJM 2002; 347: 1633 -38. Lipton HL, et al: The impact of clinical pharmacists’ consultations on physicians geriatric drug prescribing: a randomized controlled trial. Med Care 1992; 30: 646 -58. Ryan AA. Medication compliance and older people: a review of the literature. Int’l J Nursing Studies 1999; 36: 153 -162. Samsa GP, Hanlon JT, Schmader KE, Weinberger M, Clipp EC, Uttech KM, Lewis IK, Landsman PB, Cohen HJ. A summated score for the medication appropriateness index: development and assessment of clinimetric properties including content validity. J Clin Epidemiol 1994; 47(8): 891 -896. Schmader K, et al: Appropriateness of medication prescribing in ambulatory elderly patients. J Am Geriatr Soc 1994; 42: 1241 -47.
CHAMP: Drugs and Aging Bibliography 25. 26. 27. Stuck AE, Beers MH, Steiner A, Aronow HU, Rubenstein LZ, Beck JC. Inappropriate medication use in community-residing older persons. Arch Intern Med 1994; 154: 2195 -2200. Van Eijken M, Tsang S, Wensing M, de Smet PAGM, Grol RPTM. Interventions to improve medication compliance in older patients living in the community: a systematic review of the literature. Drugs & Aging 2003; 20: 229 -240. Illinois Department of Public Aid website, © 2004.