Current management of COPD and when to refer
- Slides: 24
Current management of COPD and when to refer? Dr Maxine Hardinge Consultant Respiratory Medicine Oxford University Hospitals NHS Foundation Trust
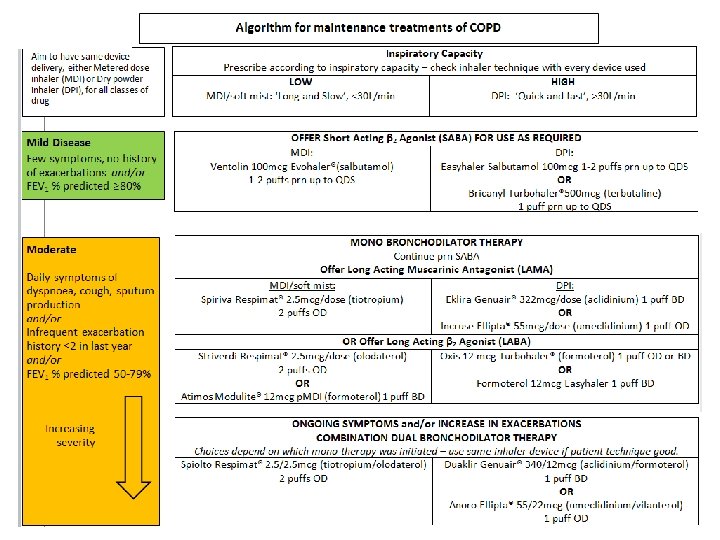
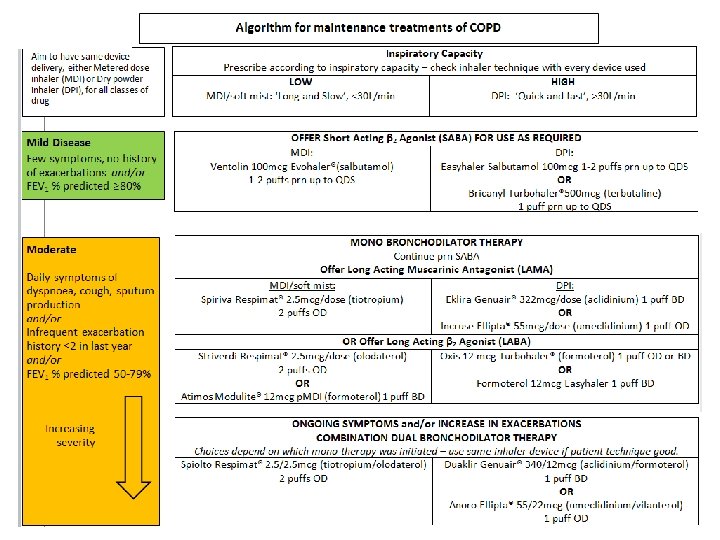
• Aims of treatment – reducing risk and reducing symptoms • Inhaled therapy – new Oxfordshire guidance • Severe COPD – home oxygen therapy, palliative measures, surgical interventions • Out-patient referrals - who to refer and who is being referred?
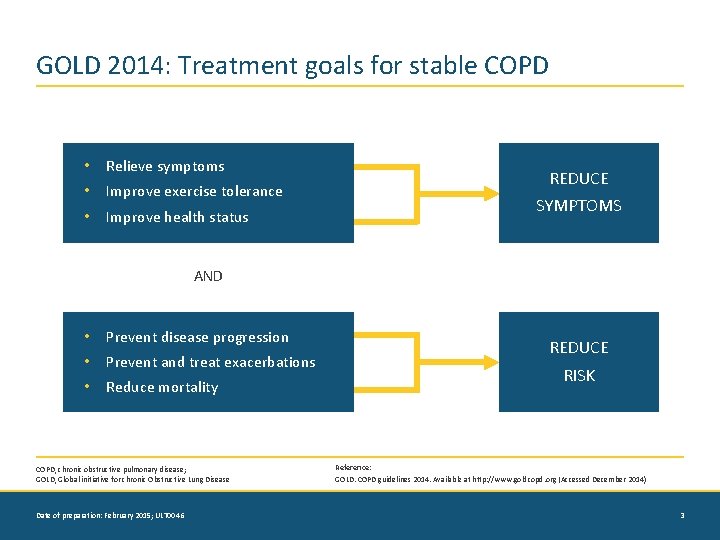
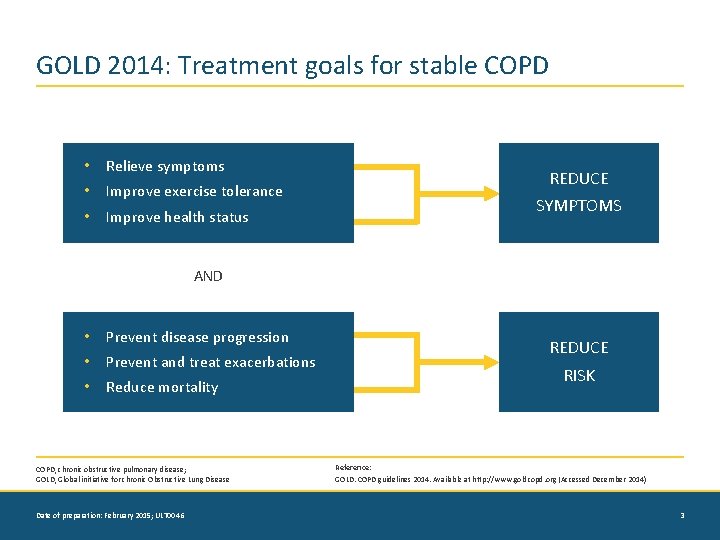
GOLD 2014: Treatment goals for stable COPD • Relieve symptoms • Improve exercise tolerance • Improve health status REDUCE SYMPTOMS AND • Prevent disease progression • Prevent and treat exacerbations • Reduce mortality COPD, chronic obstructive pulmonary disease; GOLD, Global initiative for chronic Obstructive Lung Disease Date of preparation: February 2015; ULT 0046 REDUCE RISK Reference: GOLD. COPD guidelines 2014. Available at http: //www. goldcopd. org (Accessed December 2014) 3
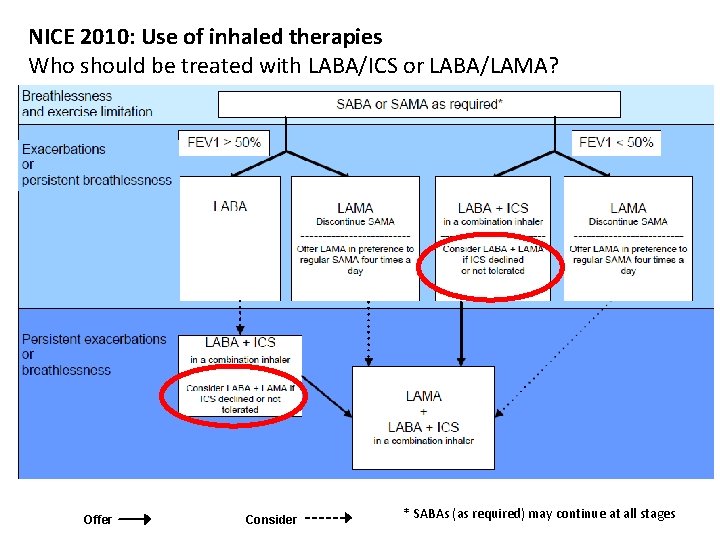
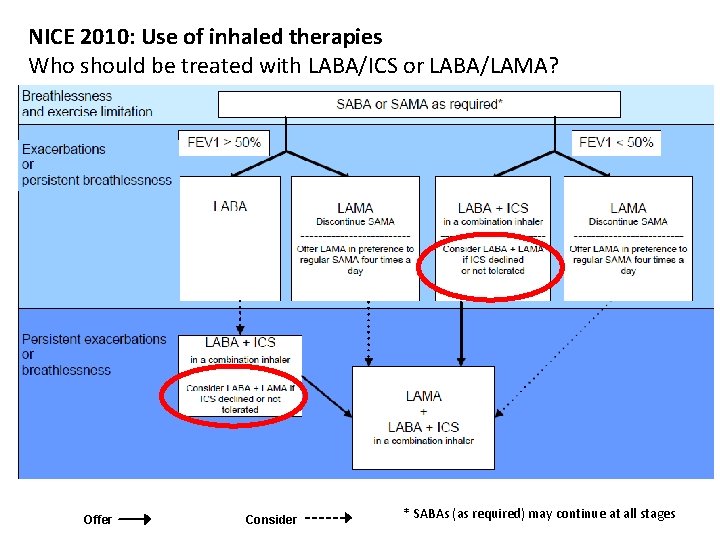
NICE 2010: Use of inhaled therapies Who should be treated with LABA/ICS or LABA/LAMA? Offer Consider * SABAs (as required) may continue at all stages
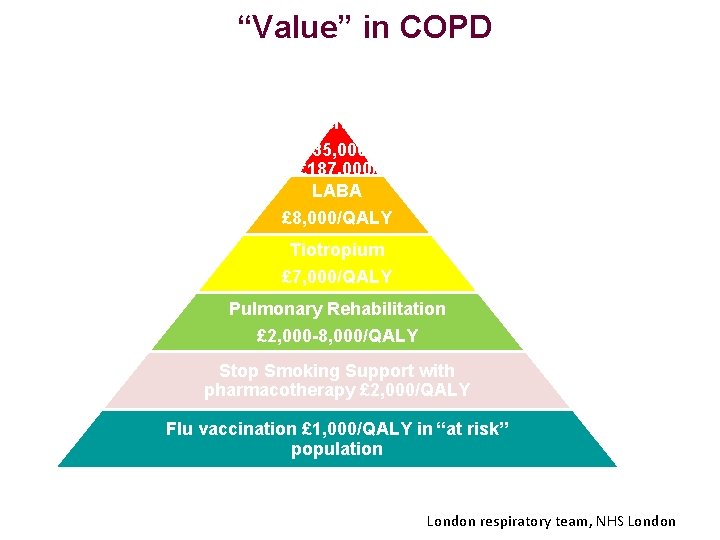
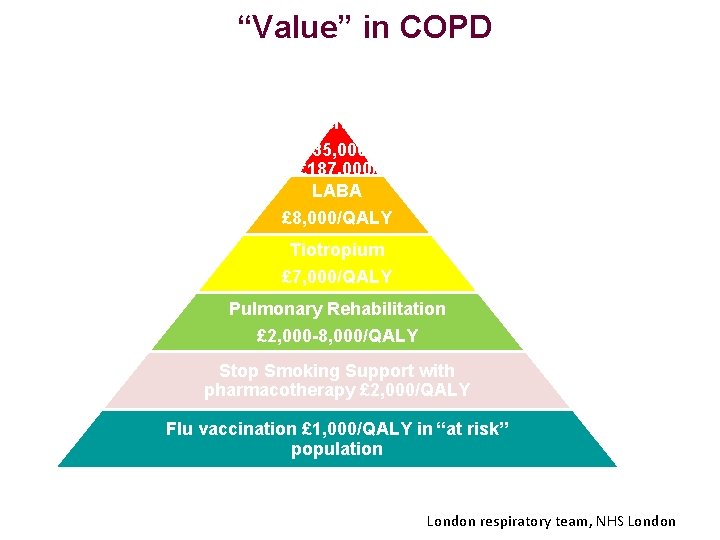
“Value” in COPD Triple Therapy £ 35, 000£ 187, 000/ QALY LABA £ 8, 000/QALY Tiotropium £ 7, 000/QALY Pulmonary Rehabilitation £ 2, 000 -8, 000/QALY Stop Smoking Support with pharmacotherapy £ 2, 000/QALY Flu vaccination £ 1, 000/QALY in “at risk” population London respiratory team, NHS London
Getting the basics right • • Diagnosis – quality assured spirometry Vaccination Smoking cessation Physical activity – pulmonary rehabilitation Diet Self management Depression/ anxiety
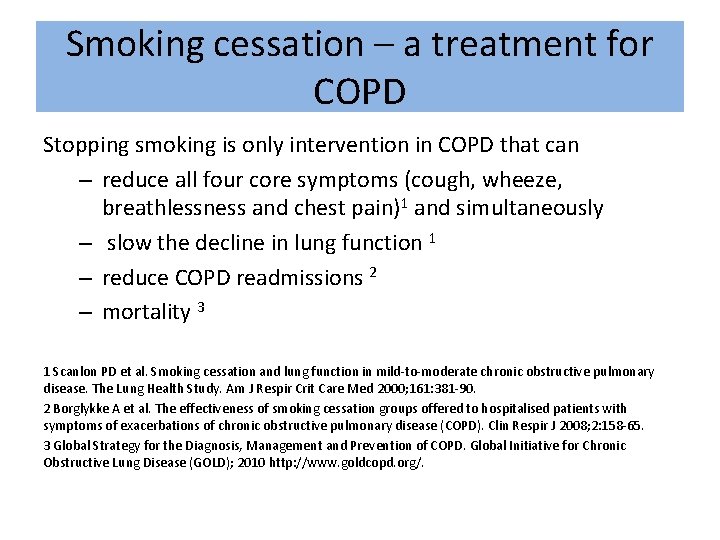
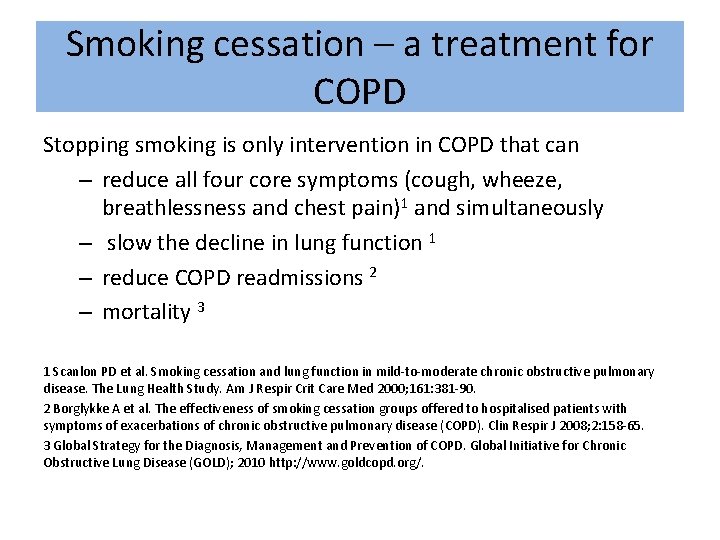
Smoking cessation – a treatment for COPD Stopping smoking is only intervention in COPD that can – reduce all four core symptoms (cough, wheeze, breathlessness and chest pain)1 and simultaneously – slow the decline in lung function 1 – reduce COPD readmissions 2 – mortality 3 1 Scanlon PD et al. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease. The Lung Health Study. Am J Respir Crit Care Med 2000; 161: 381 -90. 2 Borglykke A et al. The effectiveness of smoking cessation groups offered to hospitalised patients with symptoms of exacerbations of chronic obstructive pulmonary disease (COPD). Clin Respir J 2008; 2: 158 -65. 3 Global Strategy for the Diagnosis, Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD); 2010 http: //www. goldcopd. org/.
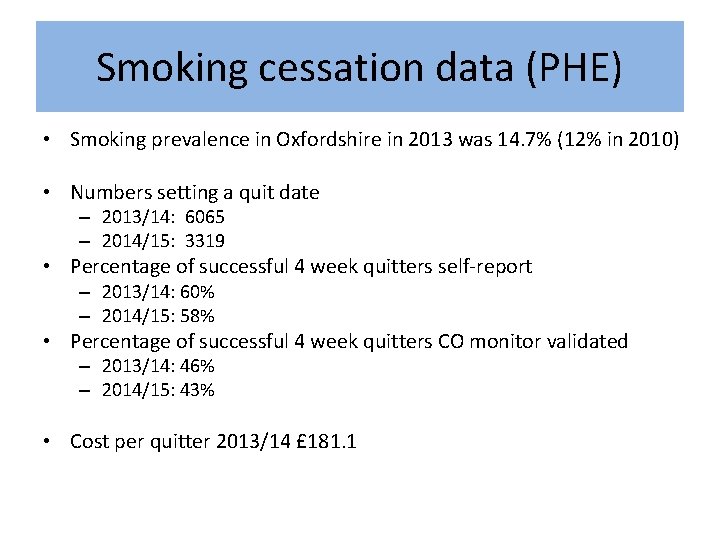
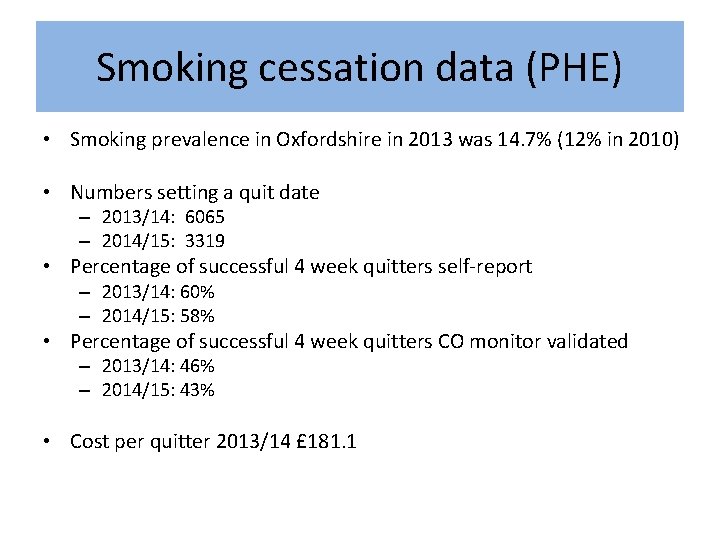
Smoking cessation data (PHE) • Smoking prevalence in Oxfordshire in 2013 was 14. 7% (12% in 2010) • Numbers setting a quit date – 2013/14: 6065 – 2014/15: 3319 • Percentage of successful 4 week quitters self-report – 2013/14: 60% – 2014/15: 58% • Percentage of successful 4 week quitters CO monitor validated – 2013/14: 46% – 2014/15: 43% • Cost per quitter 2013/14 £ 181. 1
NICE 2010: Pulmonary rehabilitation Offer to all appropriate people with COPD • those who consider themselves functionally disabled by COPD (usually MRC grade 3 and above) • including those who have had a recent hospitalisation for an exacerbation – early post discharge pulmonary rehabilitation
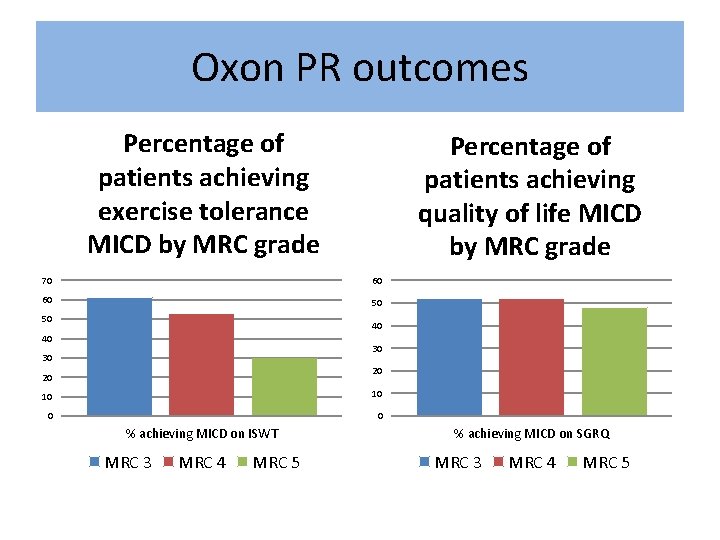
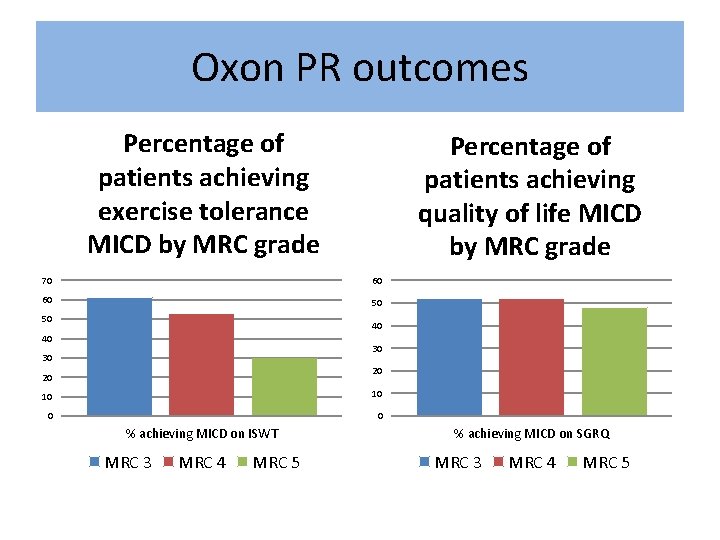
Oxon PR outcomes Percentage of patients achieving exercise tolerance MICD by MRC grade Percentage of patients achieving quality of life MICD by MRC grade 70 60 60 50 50 40 40 30 30 20 20 10 10 0 0 % achieving MICD on ISWT MRC 3 MRC 4 MRC 5 % achieving MICD on SGRQ MRC 3 MRC 4 MRC 5
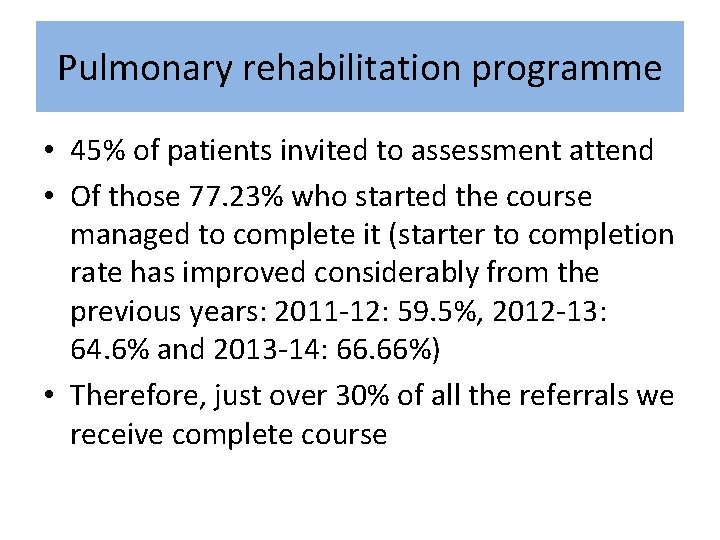
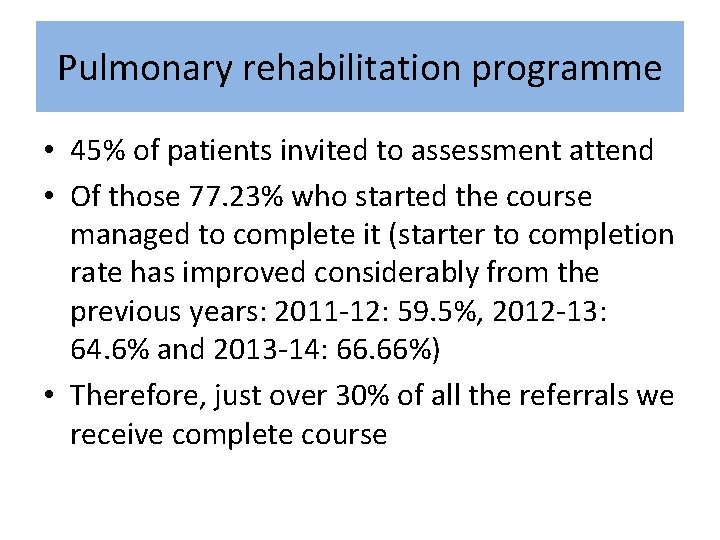
Pulmonary rehabilitation programme • 45% of patients invited to assessment attend • Of those 77. 23% who started the course managed to complete it (starter to completion rate has improved considerably from the previous years: 2011 -12: 59. 5%, 2012 -13: 64. 6% and 2013 -14: 66. 66%) • Therefore, just over 30% of all the referrals we receive complete course
Self management • Need to take a variety of approaches tailored to individual
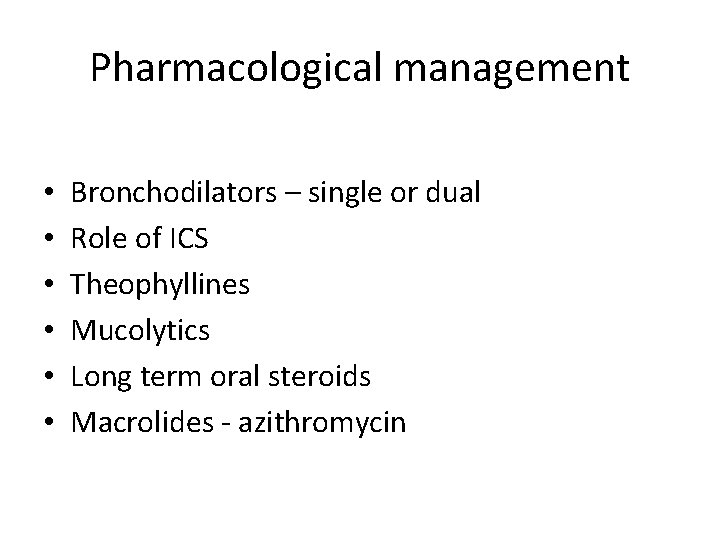
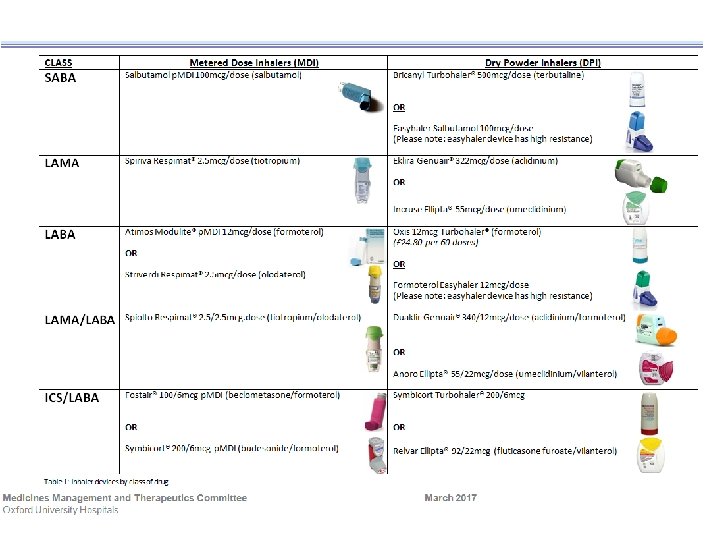
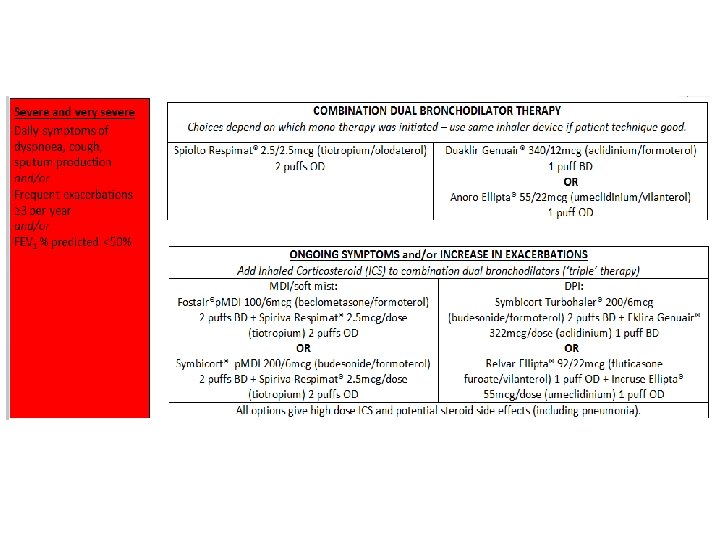
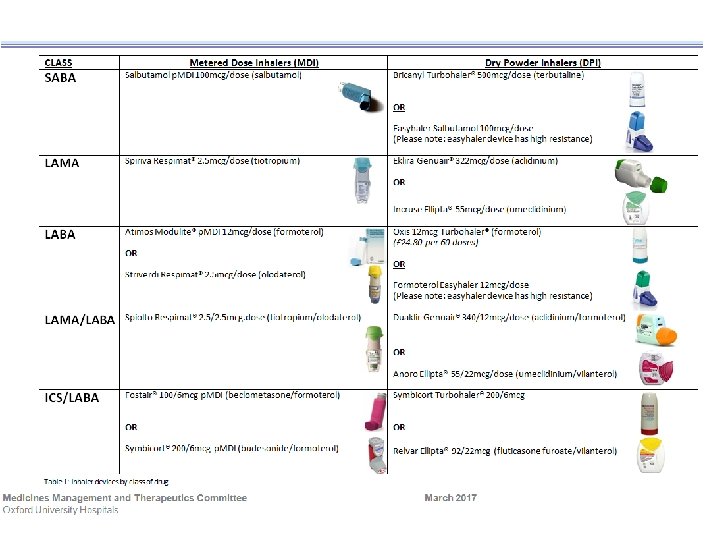
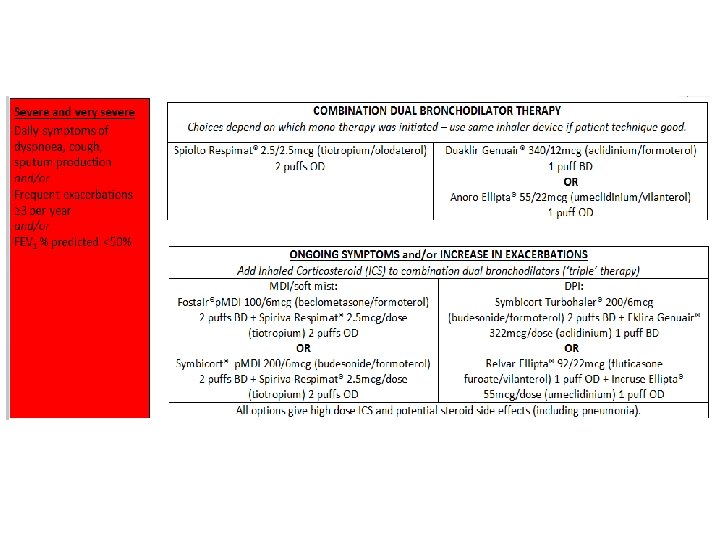
Pharmacological management • • • Bronchodilators – single or dual Role of ICS Theophyllines Mucolytics Long term oral steroids Macrolides - azithromycin
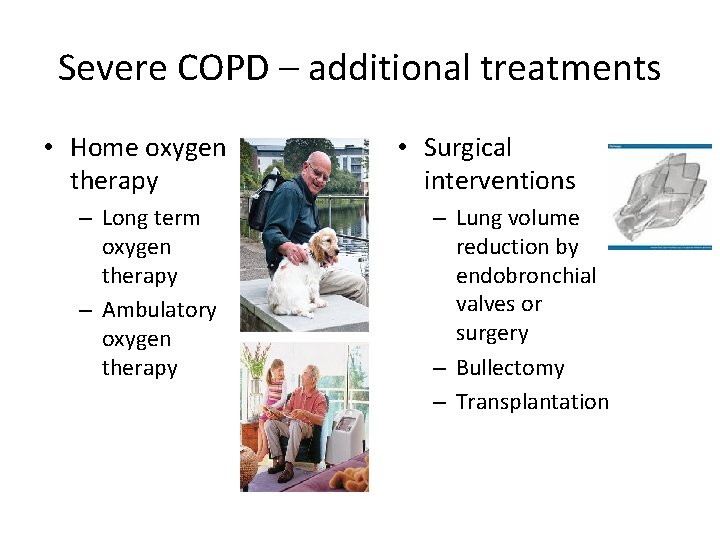
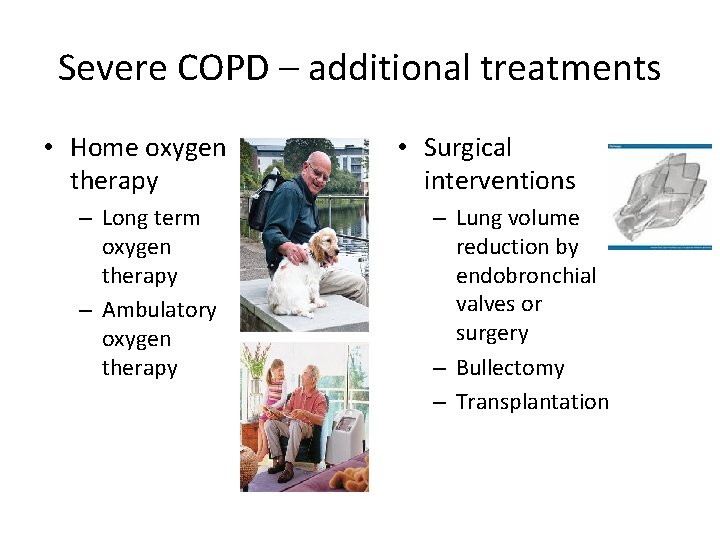
Severe COPD – additional treatments • Home oxygen therapy – Long term oxygen therapy – Ambulatory oxygen therapy • Surgical interventions – Lung volume reduction by endobronchial valves or surgery – Bullectomy – Transplantation
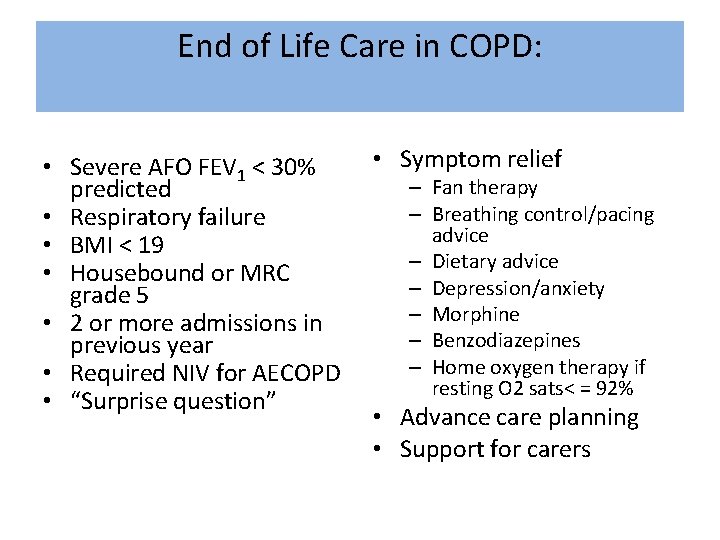
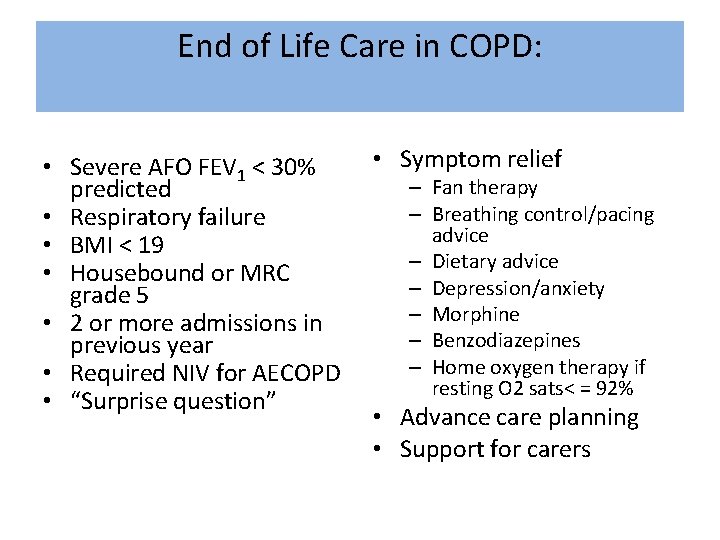
End of Life Care in COPD: • Severe AFO FEV 1 < 30% predicted • Respiratory failure • BMI < 19 • Housebound or MRC grade 5 • 2 or more admissions in previous year • Required NIV for AECOPD • “Surprise question” • Symptom relief – Fan therapy – Breathing control/pacing advice – Dietary advice – Depression/anxiety – Morphine – Benzodiazepines – Home oxygen therapy if resting O 2 sats< = 92% • Advance care planning • Support for carers
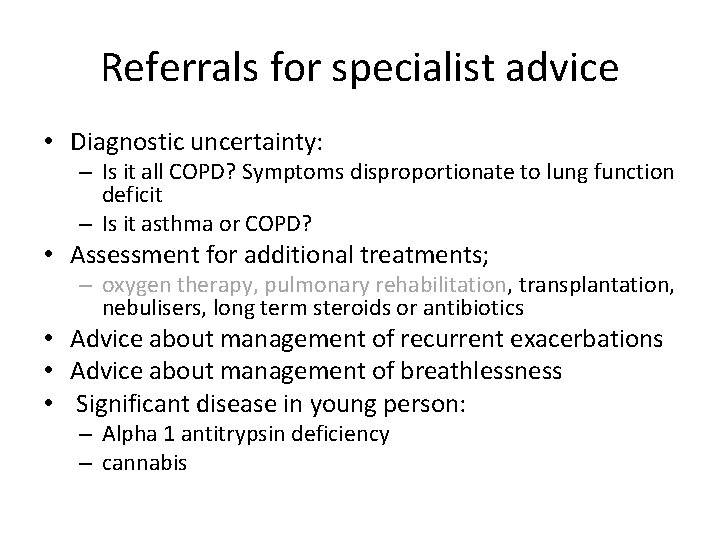
NICE 1. 1. 8 Referral for specialist advice (2004, 2010) • should be made when clinically indicated • may be appropriate at all stages and not solely in most severely disabled patients
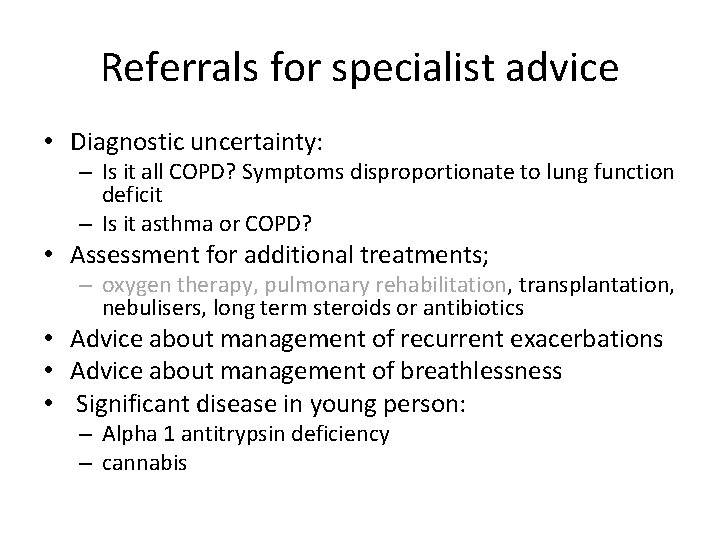
Referrals for specialist advice • Diagnostic uncertainty: – Is it all COPD? Symptoms disproportionate to lung function deficit – Is it asthma or COPD? • Assessment for additional treatments; – oxygen therapy, pulmonary rehabilitation, transplantation, nebulisers, long term steroids or antibiotics • Advice about management of recurrent exacerbations • Advice about management of breathlessness • Significant disease in young person: – Alpha 1 antitrypsin deficiency – cannabis
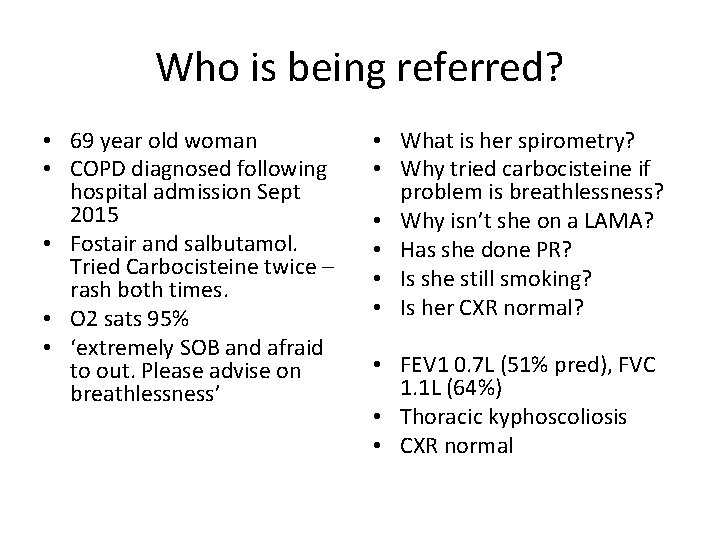
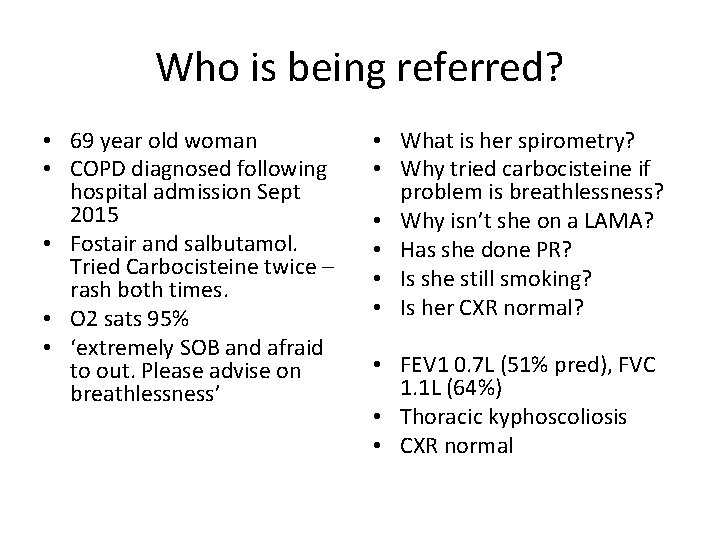
Who is being referred? • 69 year old woman • COPD diagnosed following hospital admission Sept 2015 • Fostair and salbutamol. Tried Carbocisteine twice – rash both times. • O 2 sats 95% • ‘extremely SOB and afraid to out. Please advise on breathlessness’ • What is her spirometry? • Why tried carbocisteine if problem is breathlessness? • Why isn’t she on a LAMA? • Has she done PR? • Is she still smoking? • Is her CXR normal? • FEV 1 0. 7 L (51% pred), FVC 1. 1 L (64%) • Thoracic kyphoscoliosis • CXR normal
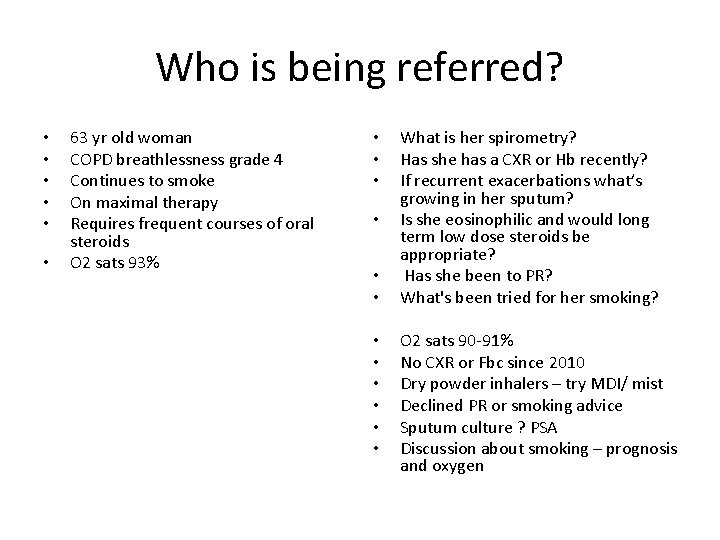
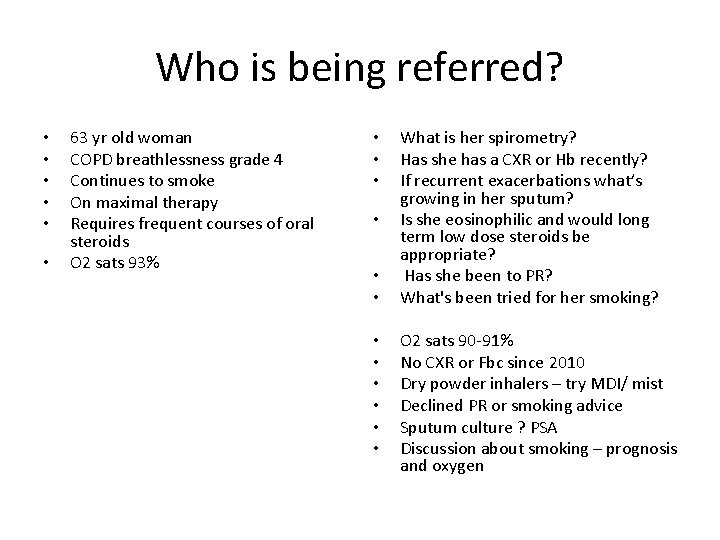
Who is being referred? • • • 63 yr old woman COPD breathlessness grade 4 Continues to smoke On maximal therapy Requires frequent courses of oral steroids O 2 sats 93% • • • What is her spirometry? Has she has a CXR or Hb recently? If recurrent exacerbations what’s growing in her sputum? Is she eosinophilic and would long term low dose steroids be appropriate? Has she been to PR? What's been tried for her smoking? O 2 sats 90 -91% No CXR or Fbc since 2010 Dry powder inhalers – try MDI/ mist Declined PR or smoking advice Sputum culture ? PSA Discussion about smoking – prognosis and oxygen
Summary • Treatments as risk reduction and symptom treatment • New inhaler guidance • Smoking cessation is a treatment for COPD • Championing exercise and PR • Tailoring self-management • Referrals – overview of COPD severity and problem which needs addressing