CURRENT CONCEPTS in perioperative FLUID MANAGEMENT Prof Mehdi


![THE KINETICS OF PVE Starlings Equiblirium Q=Ka[(Pc – Pi) + O-(IIi- IIc)] THE KINETICS OF PVE Starlings Equiblirium Q=Ka[(Pc – Pi) + O-(IIi- IIc)]](https://slidetodoc.com/presentation_image/252961507e115dd31b3b82b8d45284b0/image-5.jpg)



- Slides: 47

CURRENT CONCEPTS in peri-operative FLUID MANAGEMENT Prof. Mehdi Hasan Mumtaz

IMPORTANT ASPECTS The kinetics of water compartments. Recent developments colloid solutions. Components of crystalloids. Planning fluid therapy. Specific therapies.
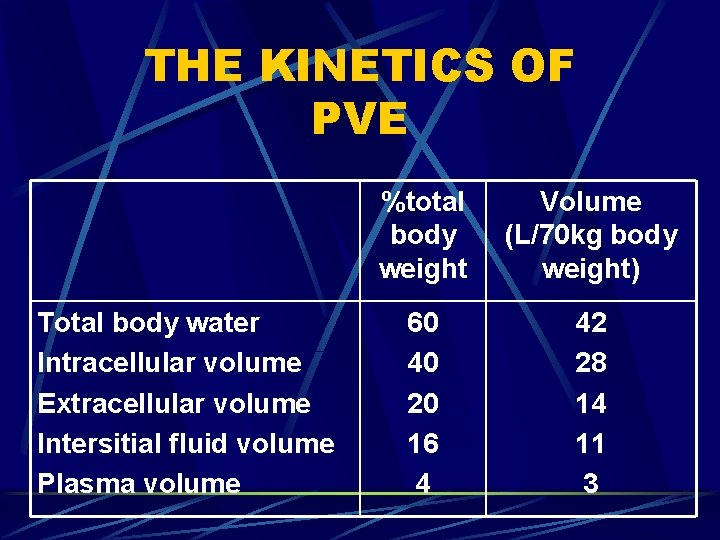
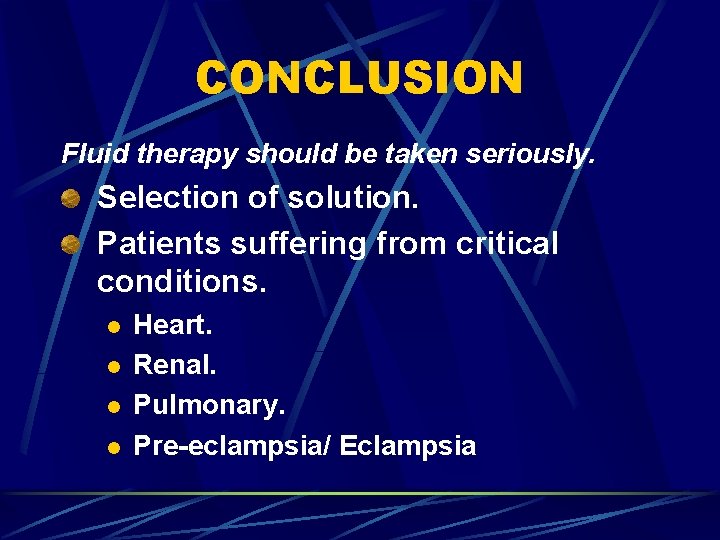
THE KINETICS OF PVE Total body water Intracellular volume Extracellular volume Intersitial fluid volume Plasma volume %total body weight Volume (L/70 kg body weight) 60 40 20 16 4 42 28 14 11 3
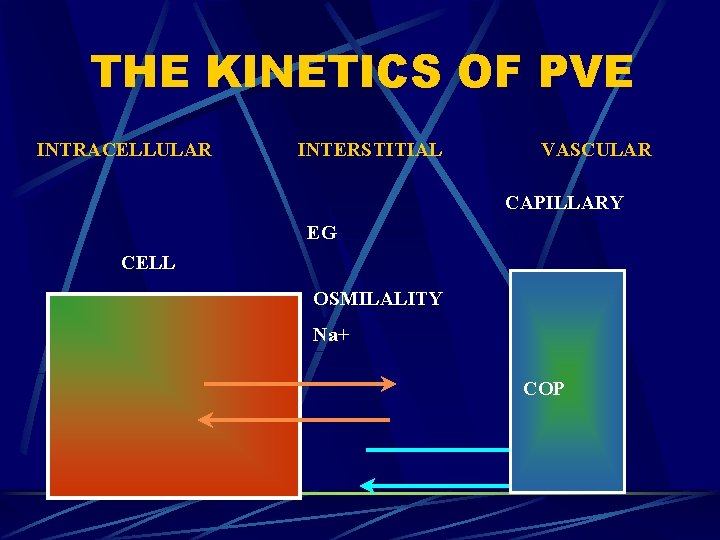
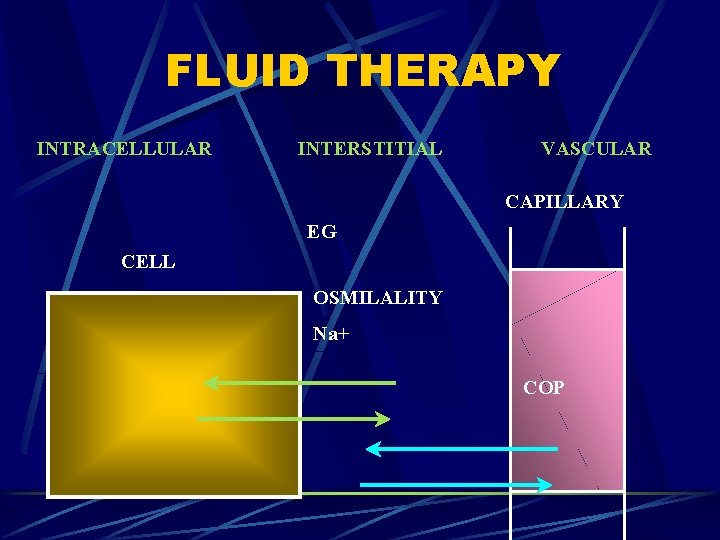
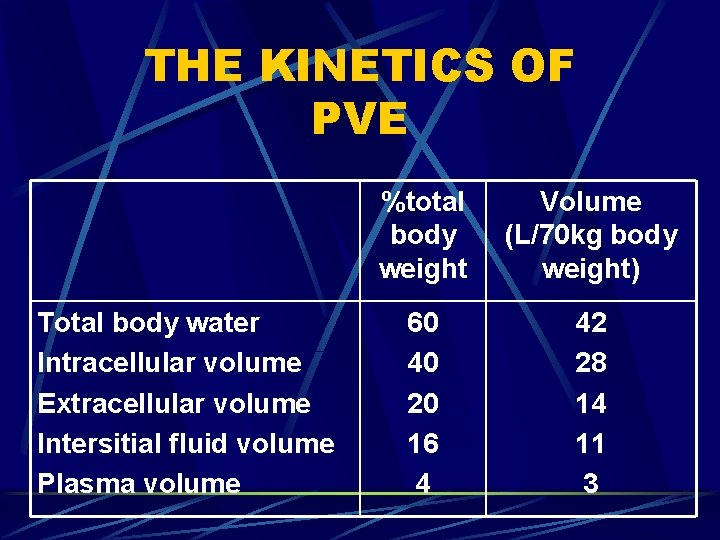
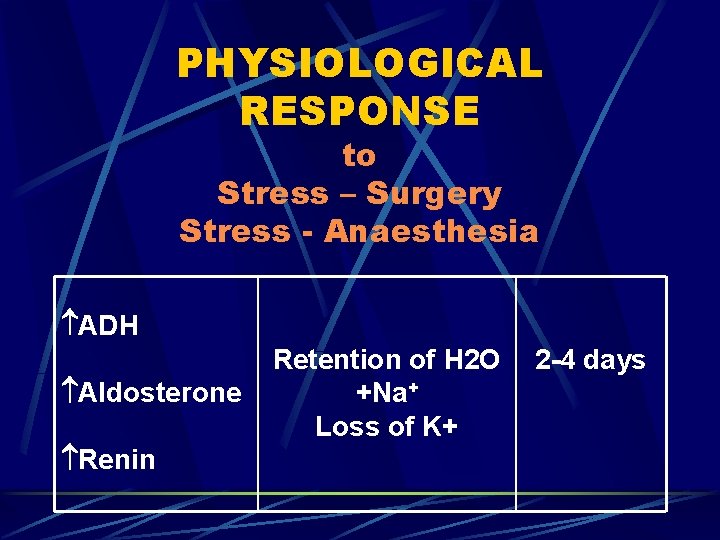
THE KINETICS OF PVE INTRACELLULAR INTERSTITIAL VASCULAR CAPILLARY EG CELL OSMILALITY Na+ COP
![THE KINETICS OF PVE Starlings Equiblirium QKaPc Pi OIIi IIc THE KINETICS OF PVE Starlings Equiblirium Q=Ka[(Pc – Pi) + O-(IIi- IIc)]](https://slidetodoc.com/presentation_image/252961507e115dd31b3b82b8d45284b0/image-5.jpg)
THE KINETICS OF PVE Starlings Equiblirium Q=Ka[(Pc – Pi) + O-(IIi- IIc)]
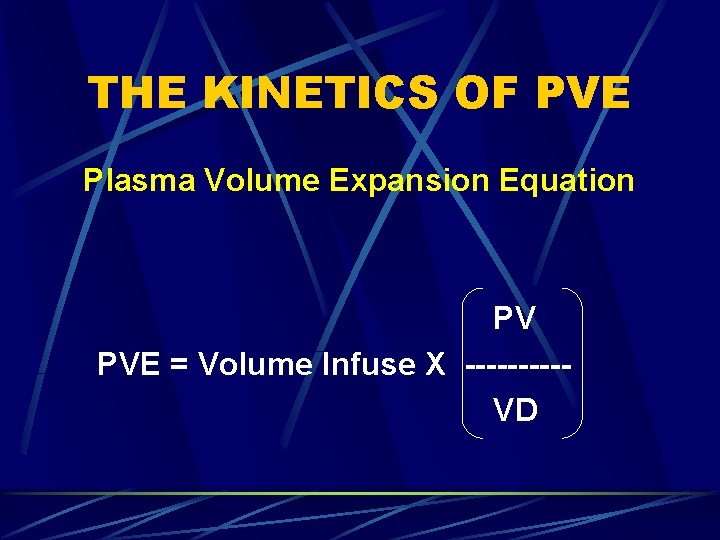
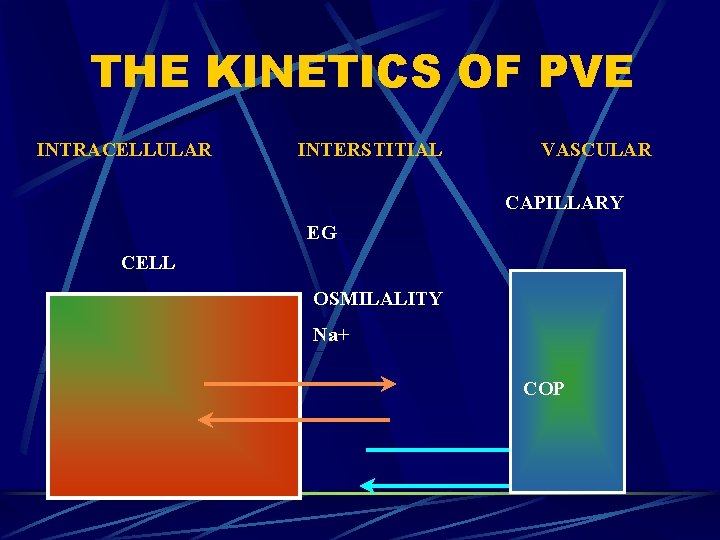
THE KINETICS OF PVE Plasma Volume Expansion Equation PV PVE = Volume Infuse X -----VD
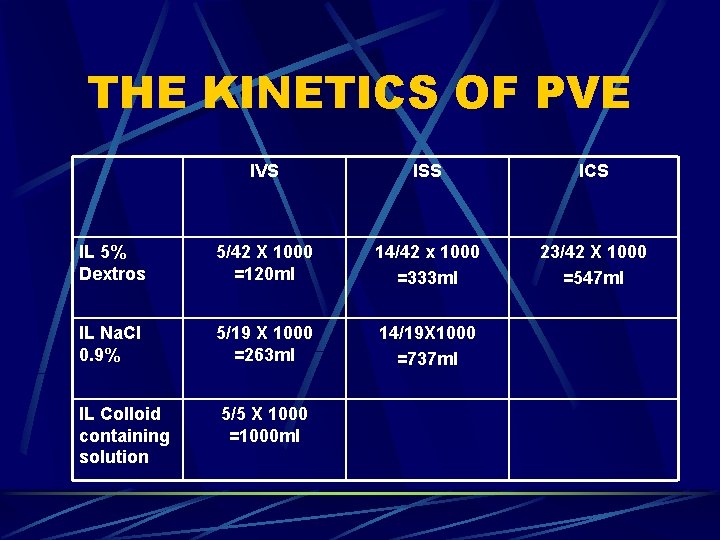
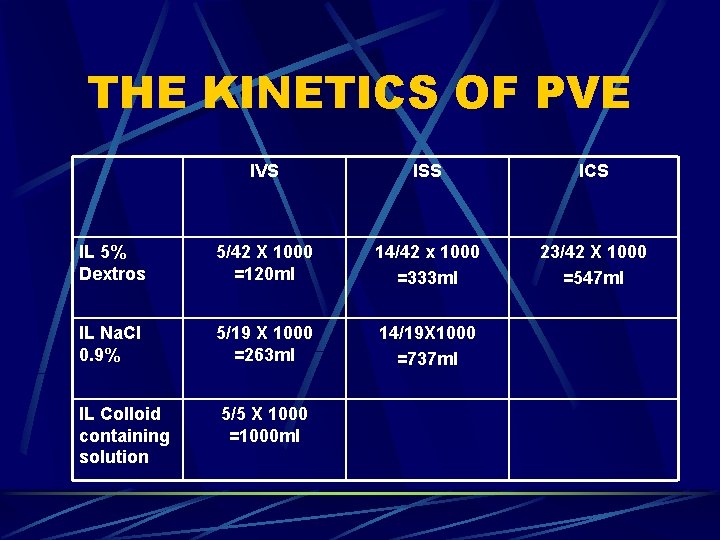
THE KINETICS OF PVE IVS ISS ICS IL 5% Dextros 5/42 X 1000 =120 ml 14/42 x 1000 =333 ml 23/42 X 1000 =547 ml IL Na. Cl 0. 9% 5/19 X 1000 =263 ml 14/19 X 1000 =737 ml IL Colloid containing solution 5/5 X 1000 =1000 ml
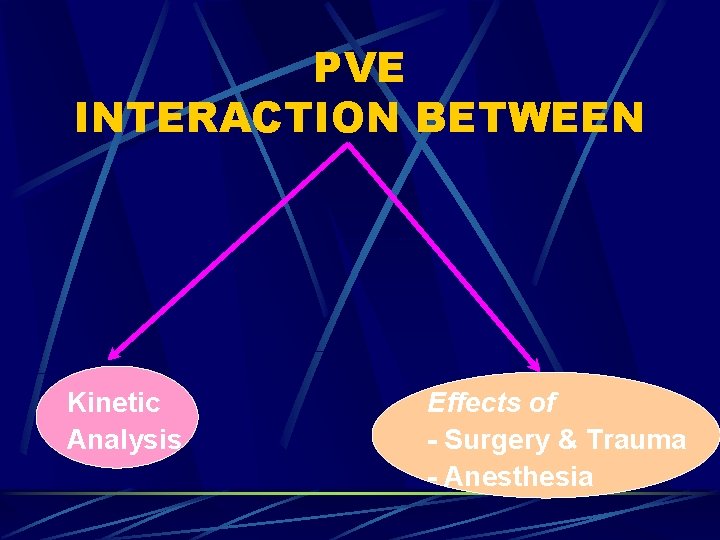
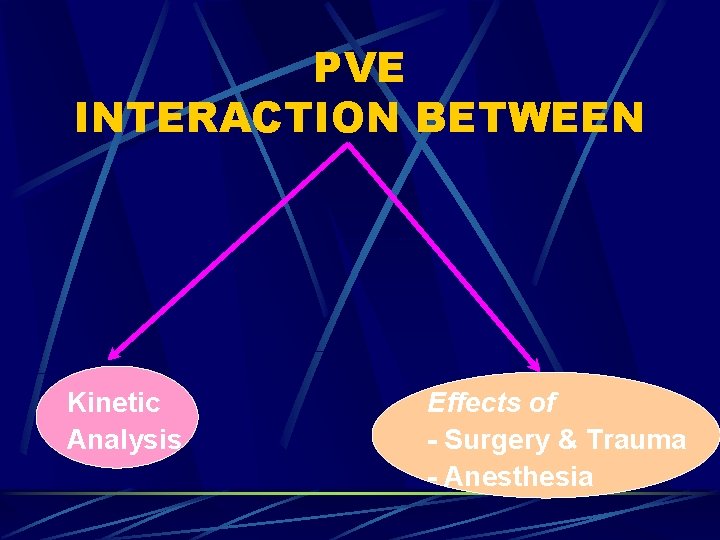
PVE INTERACTION BETWEEN Kinetic Analysis Effects of - Surgery & Trauma - Anesthesia
CURRENT PERIOPERATIVE FLUID MANAGEMENT “AVOID HYPOVOLAEMIA” But no tools are available to permit Precise matching of fluid Administration to fluid needs
REFERENCE Arieff Al. Fatal postoperative pulmonary edema: Pathogenesis and literature review. Chest 1999; 115: 1371 -7.
1 Restoration of Immune Function X --------Time Factor
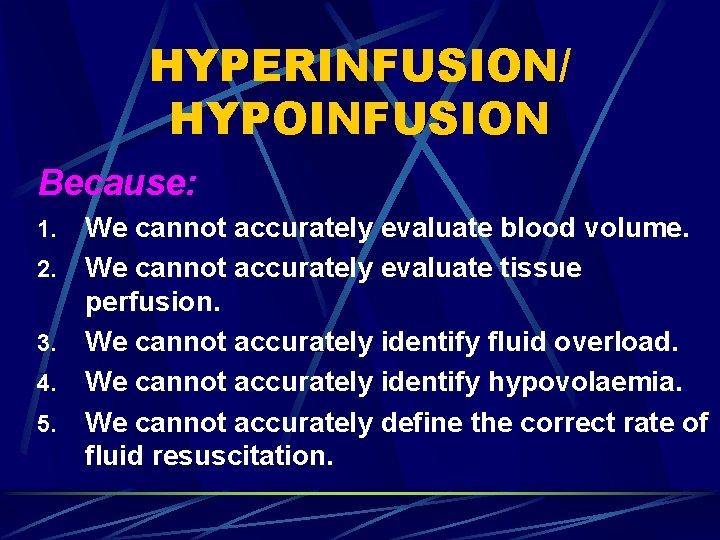
HYPERINFUSION/ HYPOINFUSION Because: 1. 2. 3. 4. 5. We cannot accurately evaluate blood volume. We cannot accurately evaluate tissue perfusion. We cannot accurately identify fluid overload. We cannot accurately identify hypovolaemia. We cannot accurately define the correct rate of fluid resuscitation.
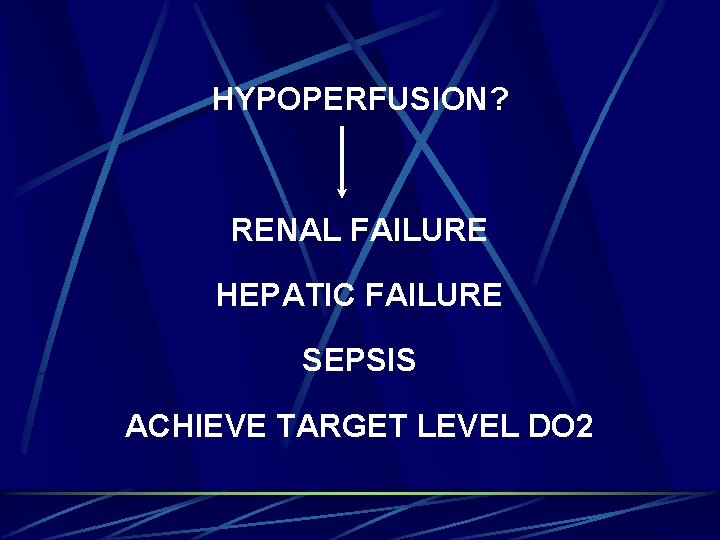
HYPOPERFUSION? RENAL FAILURE HEPATIC FAILURE SEPSIS ACHIEVE TARGET LEVEL DO 2
OXYGEN DELIVERY DO 2=Q x Ca. O 2 x 10
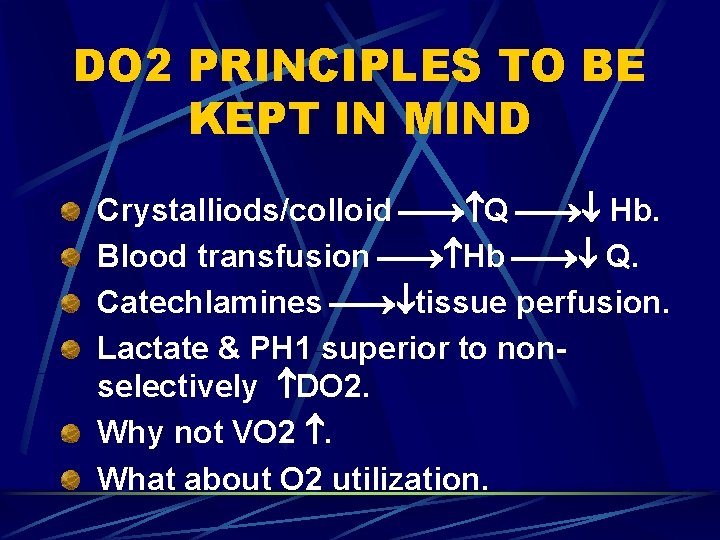
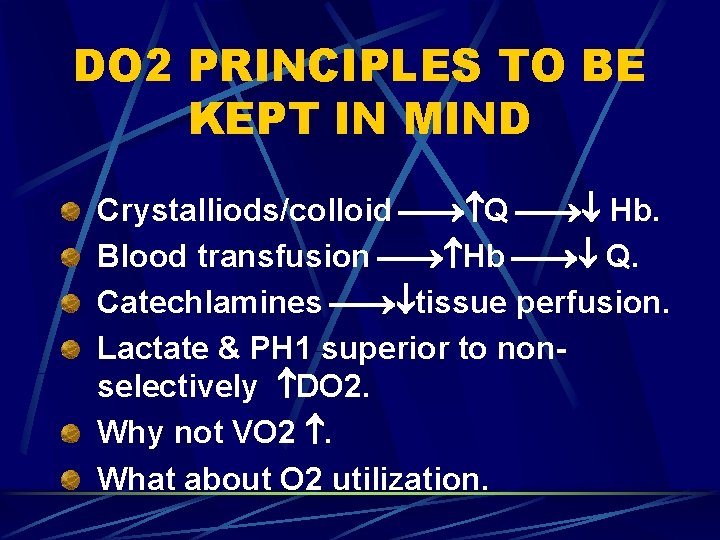
DO 2 PRINCIPLES TO BE KEPT IN MIND Crystalliods/colloid Q Hb. Blood transfusion Hb Q. Catechlamines tissue perfusion. Lactate & PH 1 superior to nonselectively DO 2. Why not VO 2 . What about O 2 utilization.
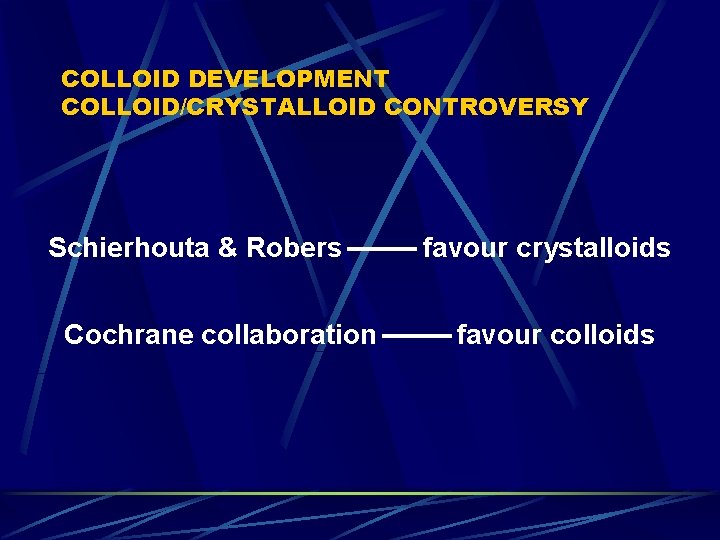
COLLOID DEVELOPMENT COLLOID/CRYSTALLOID CONTROVERSY Schierhouta & Robers favour crystalloids Cochrane collaboration favour colloids
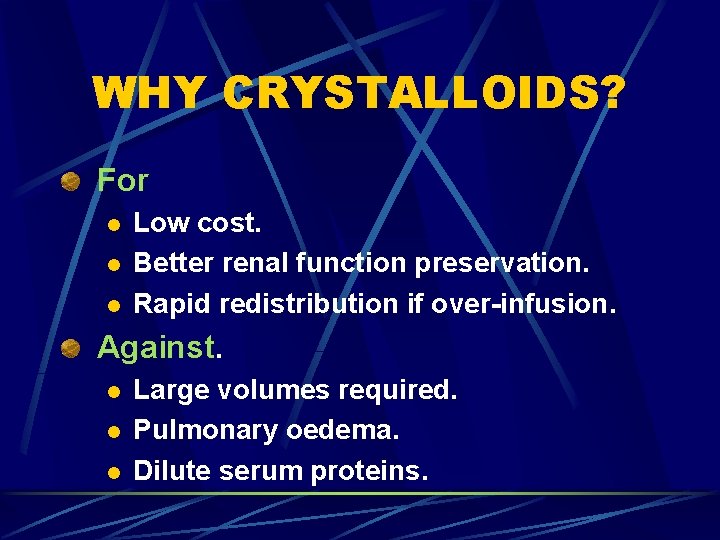
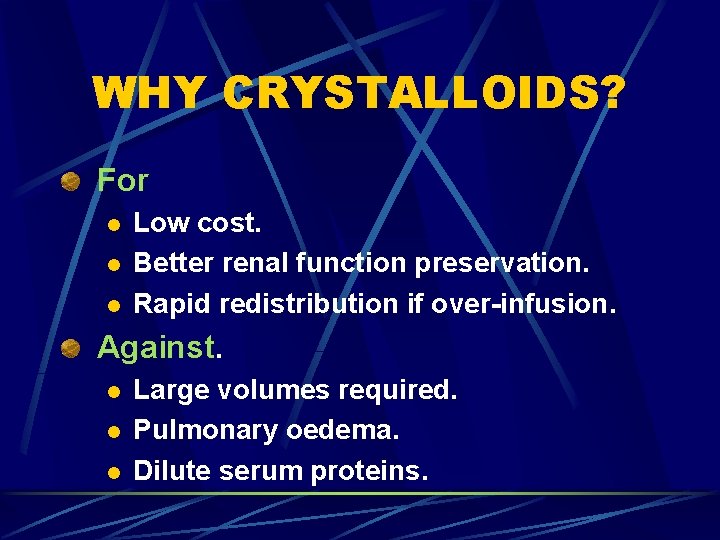
WHY CRYSTALLOIDS? For l l l Low cost. Better renal function preservation. Rapid redistribution if over-infusion. Against. l l l Large volumes required. Pulmonary oedema. Dilute serum proteins.
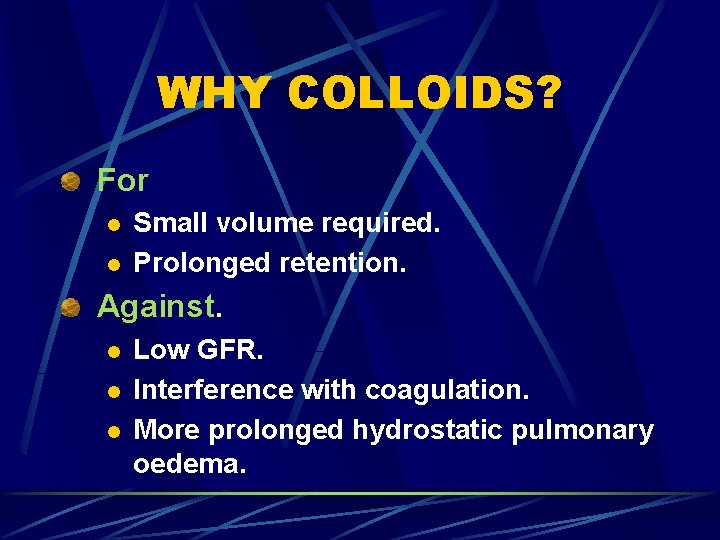
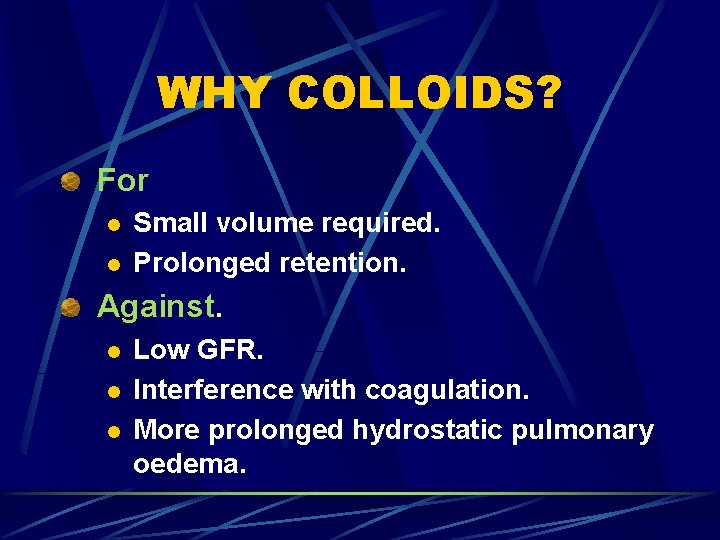
WHY COLLOIDS? For l l Small volume required. Prolonged retention. Against. l l l Low GFR. Interference with coagulation. More prolonged hydrostatic pulmonary oedema.
SOLUTION More prolonged expansion of IV volume with colloids in situation of major fluid loss (extensive surgery). Lower cost of crystalloids for most routine cases.
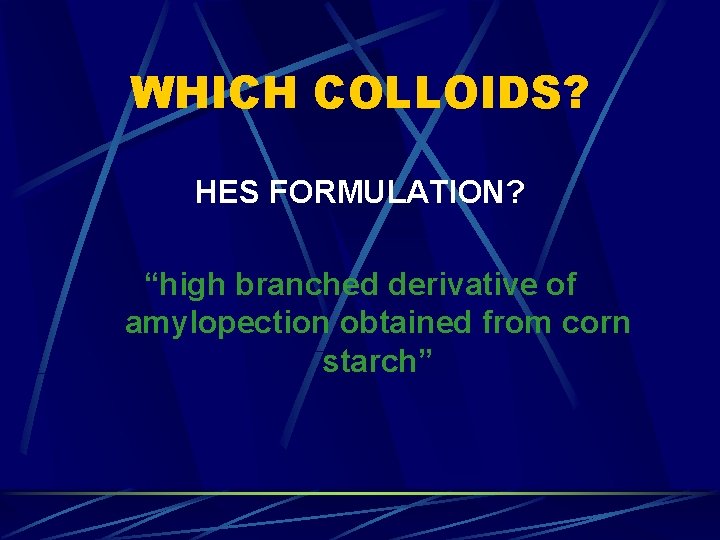
WHICH COLLOIDS? HES FORMULATION? “high branched derivative of amylopection obtained from corn starch”
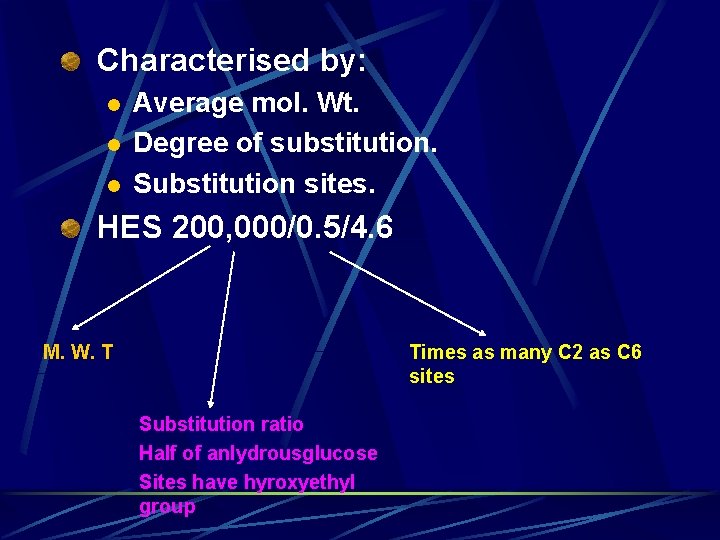
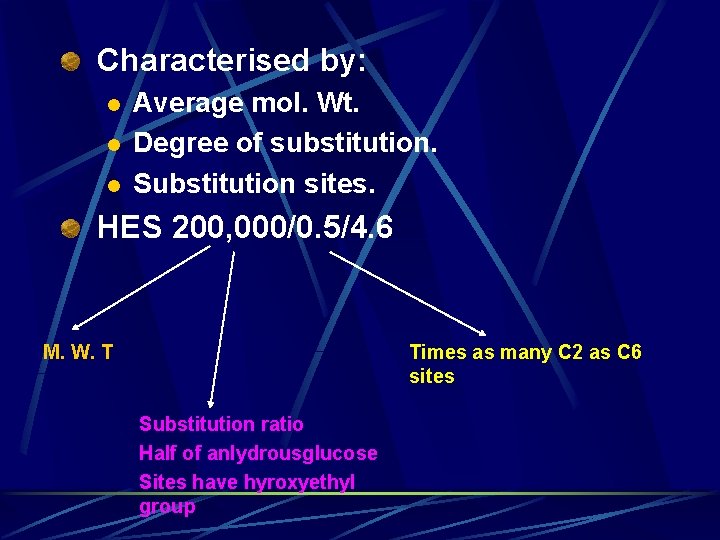
Characterised by: l l l Average mol. Wt. Degree of substitution. Substitution sites. HES 200, 000/0. 5/4. 6 M. W. T Times as many C 2 as C 6 sites Substitution ratio Half of anlydrousglucose Sites have hyroxyethyl group
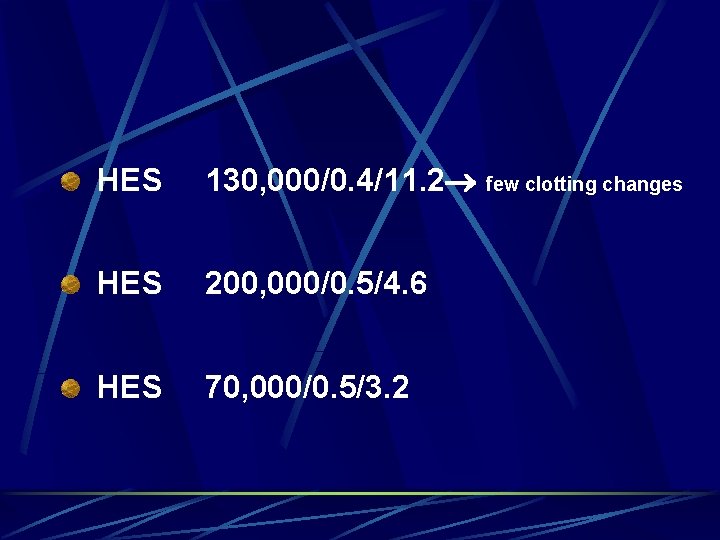
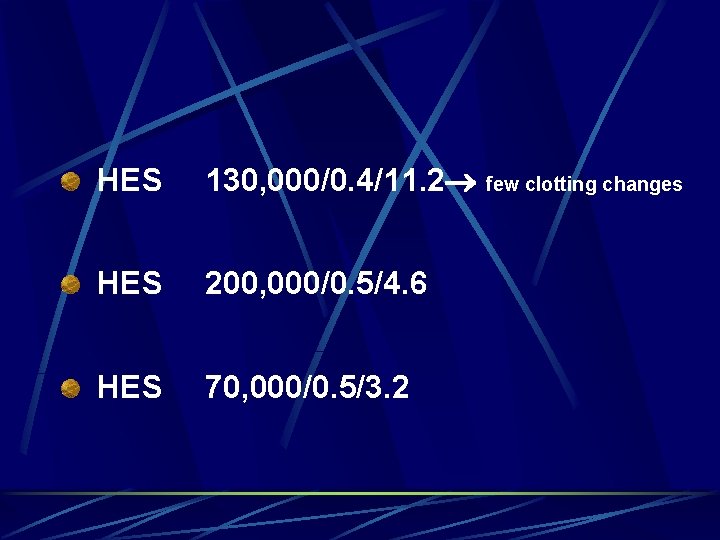
HES 130, 000/0. 4/11. 2 few clotting changes HES 200, 000/0. 5/4. 6 HES 70, 000/0. 5/3. 2
SPECIFIC COMPONENTS OF IV CRYSTALLOIDS Sodium. Lactate. Chloride. Potassium. Bicarbonate. Glucose. Water.
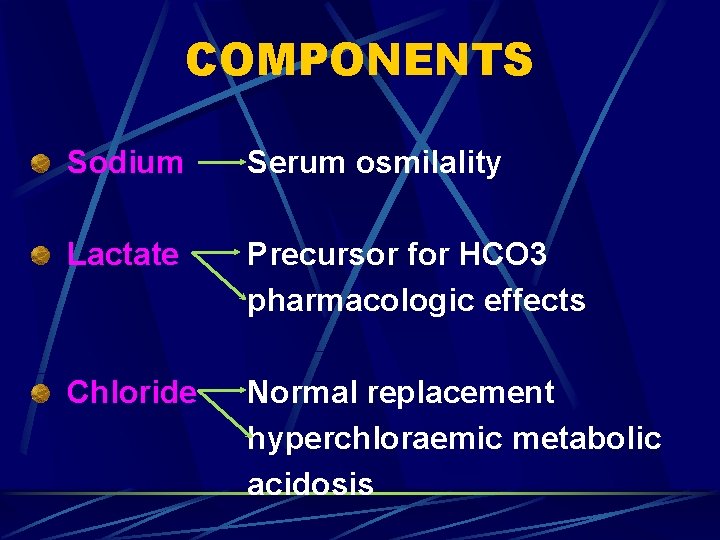
COMPONENTS Sodium Serum osmilality Lactate Precursor for HCO 3 pharmacologic effects Chloride Normal replacement hyperchloraemic metabolic acidosis
COMPONENTS - Sodium Reference: Zornow MH, Todd MM, Moore SS. The acute cerebral effects of changes in plasma osmolality and oncotic pressure. Anesthesiology 1987; 67: 946 -41.
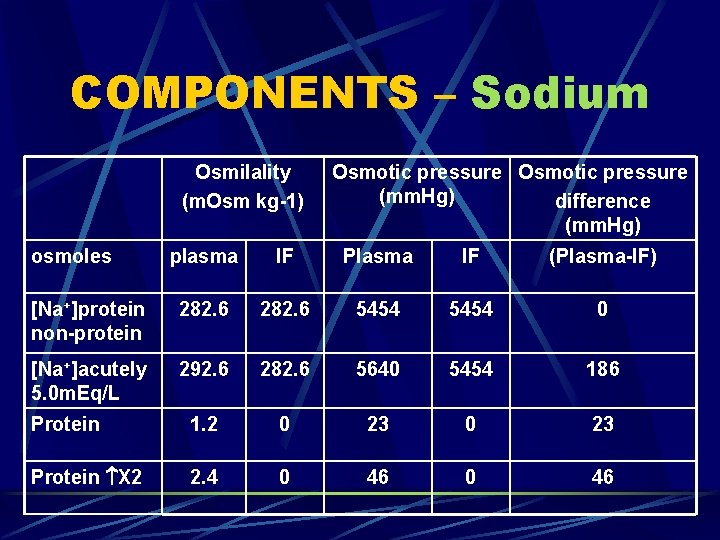
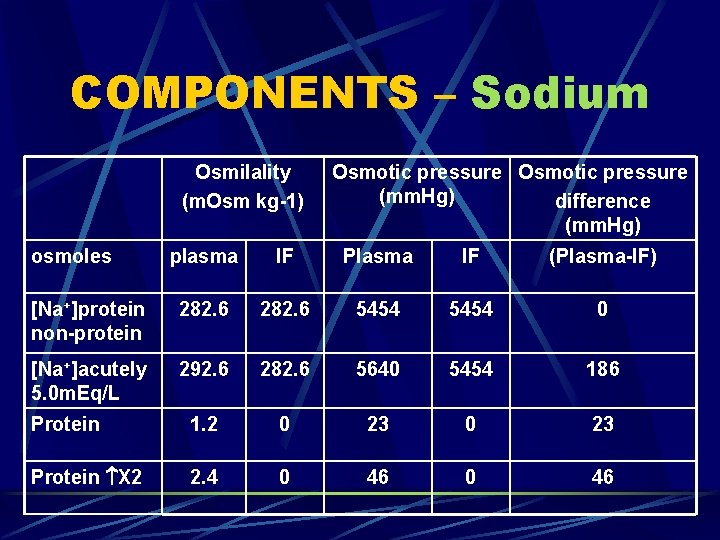
COMPONENTS – Sodium Osmilality (m. Osm kg-1) osmoles Osmotic pressure (mm. Hg) difference (mm. Hg) plasma IF Plasma IF (Plasma-IF) [Na+]protein non-protein 282. 6 5454 0 [Na+]acutely 5. 0 m. Eq/L 292. 6 282. 6 5640 5454 186 Protein 1. 2 0 23 Protein X 2 2. 4 0 46
REFERENCE Drumond JC, Patel PM, Cole DJ, Kelly PJ. The effect of the reduction of colloid oncotic pressure, with and without reduction of osmolailty, on post-traumatic cerebral edema. Anesthesiology 1998; 88: 993 -1002.
REFERENCE Fisher B, Thomas D, Peterson B. Hypertonic saline lowers raised intracranial pressure in children after head trauma. J Neurosurg. Anesthesiology 1992; 4: 4 -10.
COMPONENTS – Lactate PRECURSOR FOR BICARBONATE. APOPTOSIS IN GIT & LIVER. IMMUNE SUPRESSION.
COMPONENTS – Chloride Reference: l l Liskaser Fj, Bellomo R, Hayhoe M, et al. the role of pump prime in the etiology and pathogenesis of cardiopulmonary bypass associated acidosis. Anestheology 2000; 93: 1170 -3 Waters JH, Bernstein CA. Dilutional acidosis following hetastarch or albumin in healthy volunteers. Anesthesiology 2000 -93: 1184 -7. Hyperchloraemic metabolic acidosis
COMPONENTS – Chloride Reference: l l Prough DS, Bidani A. Hyperchloremic metabolic acidosis is a predictable consequence of intraoperative infusion of 0. 9% saline. Anesthesiology 1999; 90: 1247 -9 Prough DS, Acidosis associated with peri-operative saline administration: dilution or delusion? . Anesthesiology 2000; 93: 1167 -9 Fluid containing no bicarbonate
COMPONENTS – Chloride Reference: l Sevensen C, Hahn RG. Volume kinetics of ringer solution, dextran 70, and hypertonic saline in male volunteers. Anesthesiology 1997; 87: 204 -12 Acidosis is resolves more quickly if solution contains bicarbonates
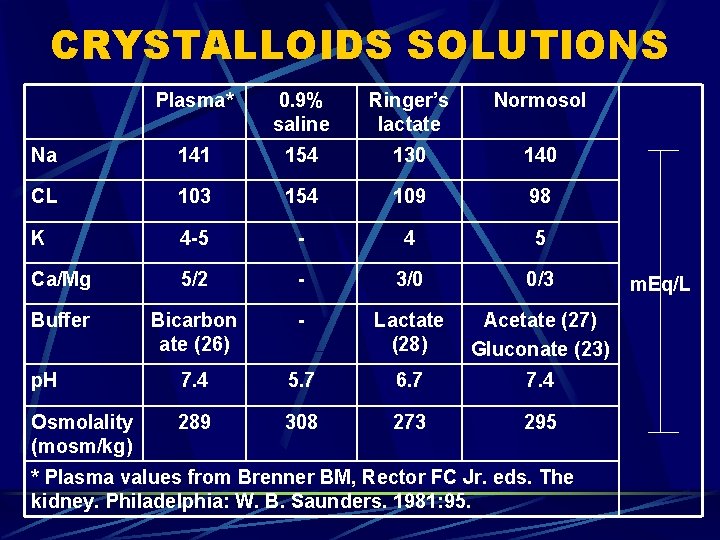
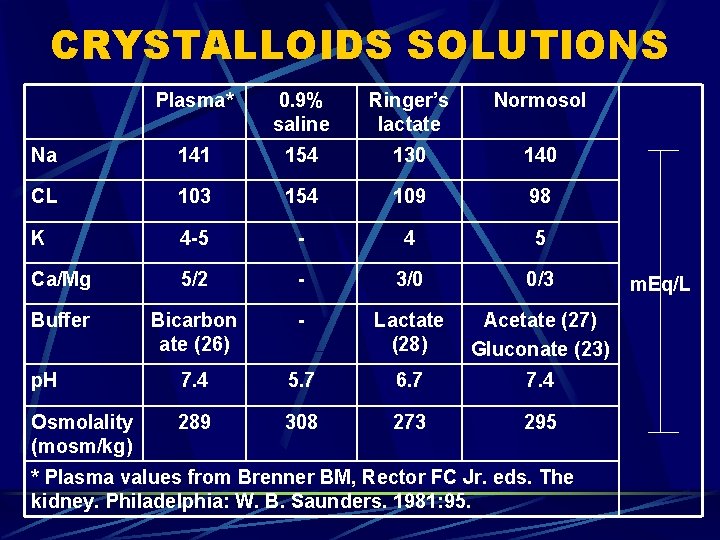
CRYSTALLOIDS SOLUTIONS Plasma* 0. 9% saline Ringer’s lactate Normosol Na 141 154 130 140 CL 103 154 109 98 K 4 -5 - 4 5 Ca/Mg 5/2 - 3/0 0/3 Buffer Bicarbon ate (26) - Lactate (28) Acetate (27) Gluconate (23) p. H 7. 4 5. 7 6. 7 7. 4 Osmolality (mosm/kg) 289 308 273 295 * Plasma values from Brenner BM, Rector FC Jr. eds. The kidney. Philadelphia: W. B. Saunders. 1981: 95. m. Eq/L
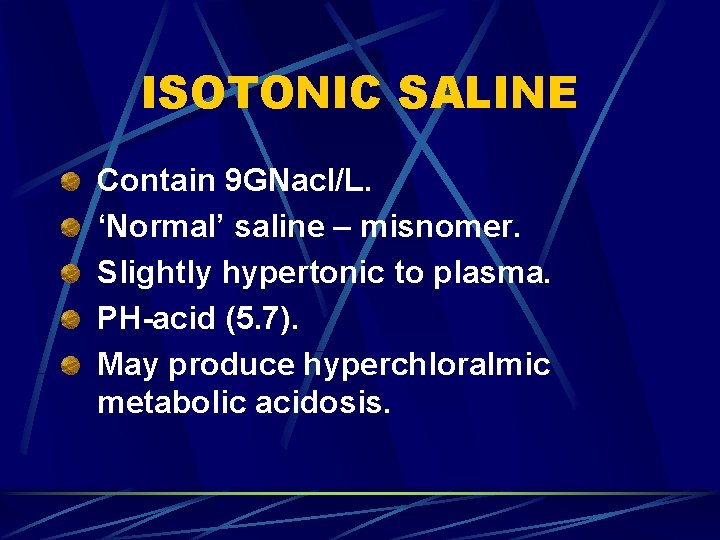
ISOTONIC SALINE Contain 9 GNacl/L. ‘Normal’ saline – misnomer. Slightly hypertonic to plasma. PH-acid (5. 7). May produce hyperchloralmic metabolic acidosis.
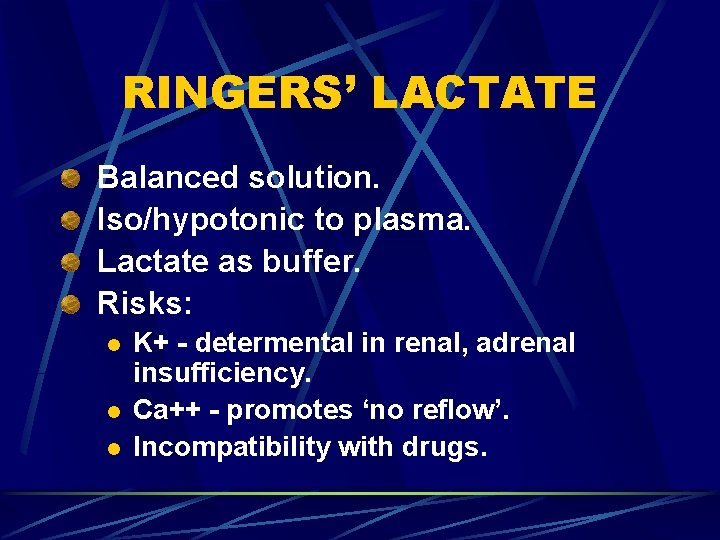
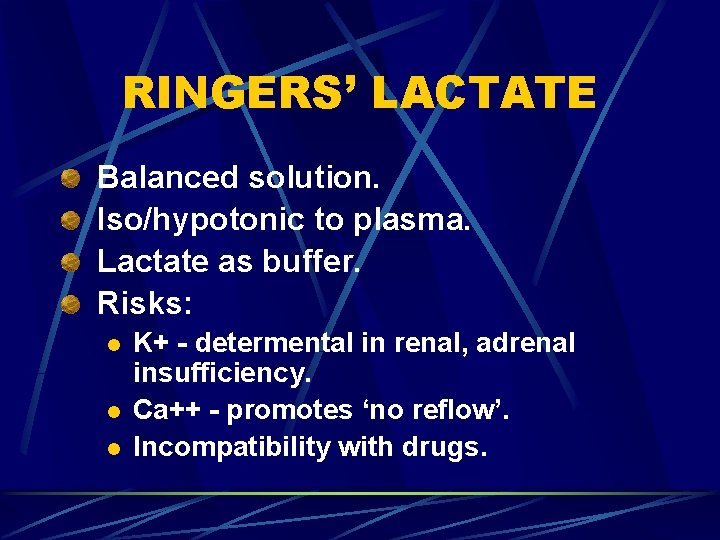
RINGERS’ LACTATE Balanced solution. Iso/hypotonic to plasma. Lactate as buffer. Risks: l l l K+ - determental in renal, adrenal insufficiency. Ca++ - promotes ‘no reflow’. Incompatibility with drugs.
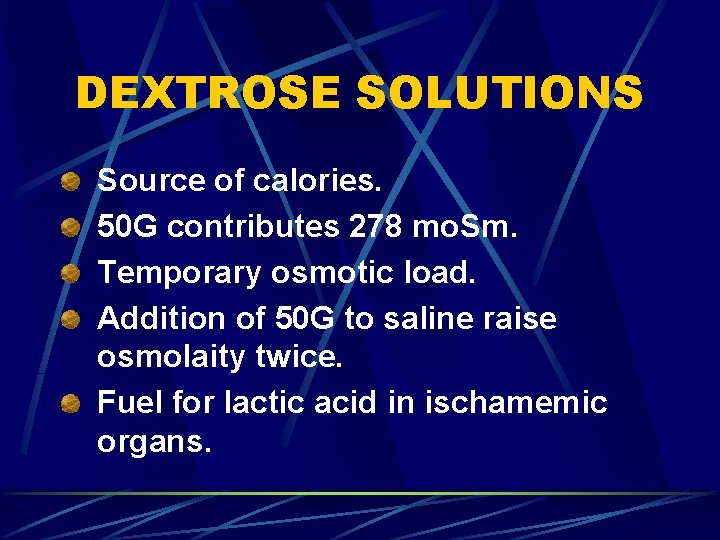
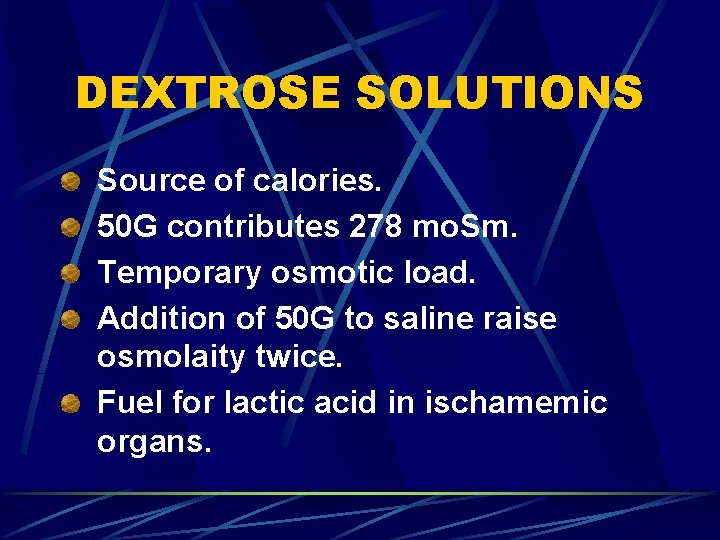
DEXTROSE SOLUTIONS Source of calories. 50 G contributes 278 mo. Sm. Temporary osmotic load. Addition of 50 G to saline raise osmolaity twice. Fuel for lactic acid in ischamemic organs.
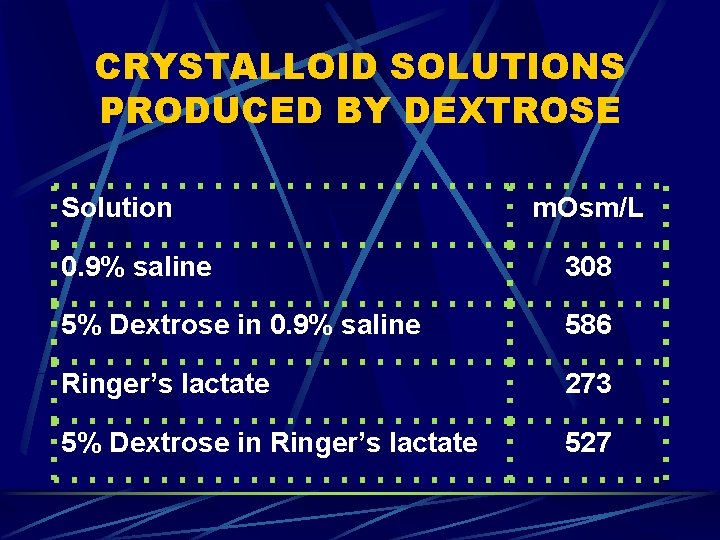
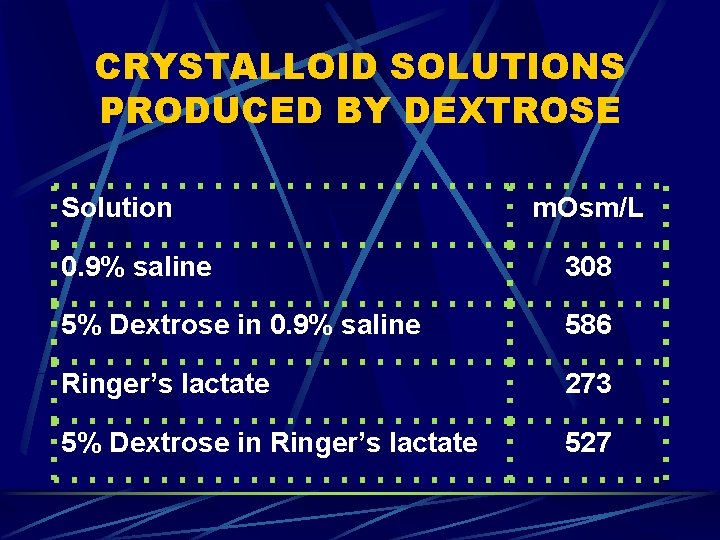
CRYSTALLOID SOLUTIONS PRODUCED BY DEXTROSE Solution m. Osm/L 0. 9% saline 308 5% Dextrose in 0. 9% saline 586 Ringer’s lactate 273 5% Dextrose in Ringer’s lactate 527
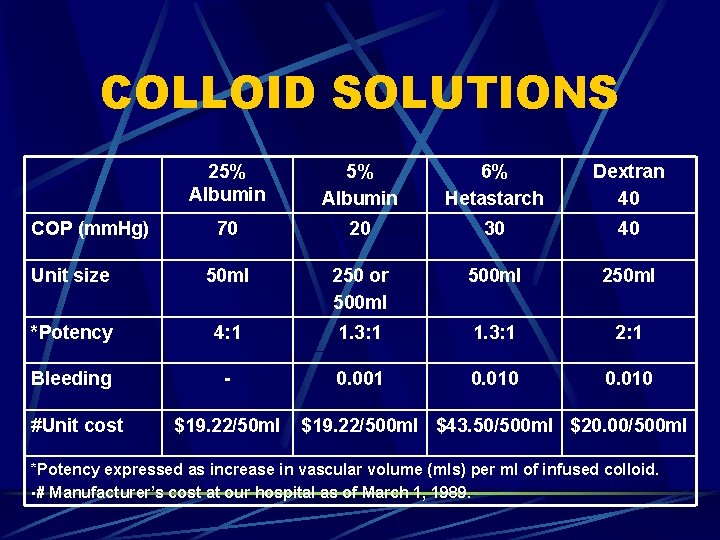
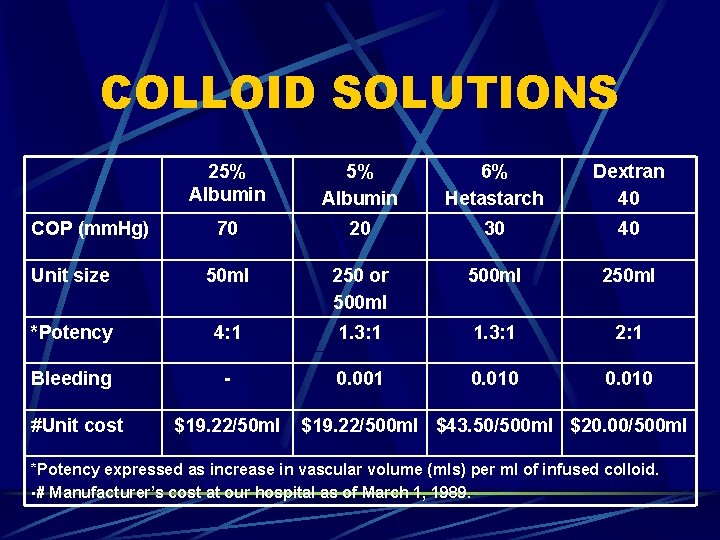
COLLOID SOLUTIONS 25% Albumin 6% Hetastarch Dextran 40 70 20 30 40 Unit size 50 ml 250 or 500 ml 250 ml *Potency 4: 1 1. 3: 1 2: 1 Bleeding - 0. 001 0. 010 COP (mm. Hg) #Unit cost $19. 22/50 ml $19. 22/500 ml $43. 50/500 ml $20. 00/500 ml *Potency expressed as increase in vascular volume (mls) per ml of infused colloid. • # Manufacturer’s cost at our hospital as of March 1, 1989.

FLUID DURING OPERATION CONTROVERSIAL? Benefit Drawback No renal failure Blood coaguability
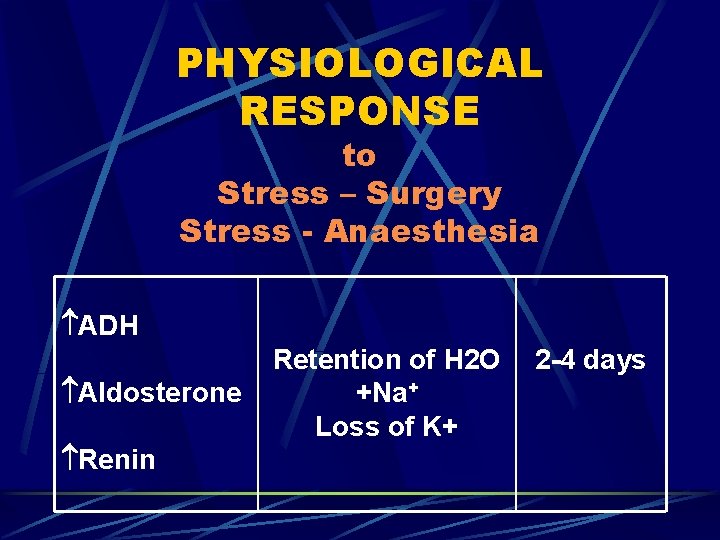
PHYSIOLOGICAL RESPONSE to Stress – Surgery Stress - Anaesthesia ADH Aldosterone Renin Retention of H 2 O +Na+ Loss of K+ 2 -4 days
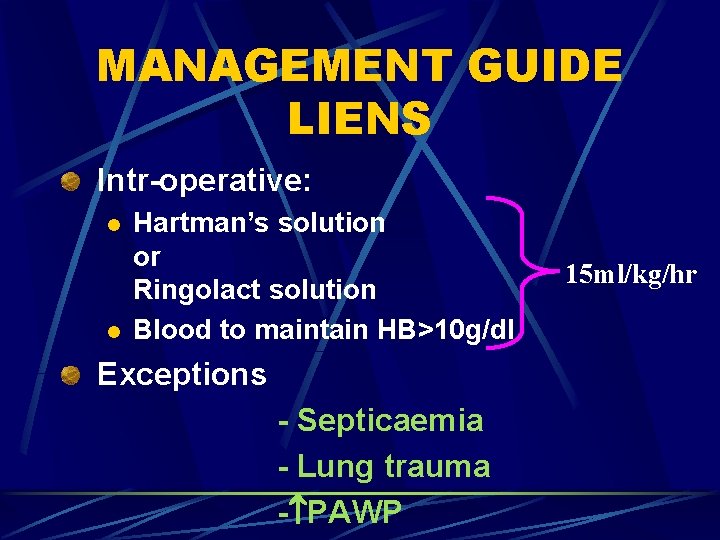
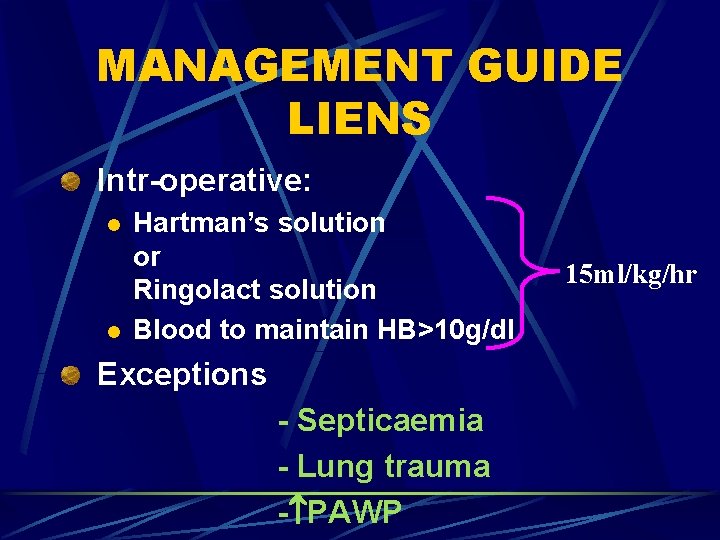
MANAGEMENT GUIDE LIENS Intr-operative: l l Hartman’s solution or Ringolact solution Blood to maintain HB>10 g/dl Exceptions - Septicaemia - Lung trauma - PAWP 15 ml/kg/hr

POSTOPERATIVE PERIOD 1. (24 -48 hrs) 5% Dextrose/water = 30 ml/kg/day + 30 mmol K+/L. l l Replace specific losses. Maintain urine output > 0. 5 ml/kg/hr.

POSTOPERATIVE PERIOD 2. After 48 hrs. l l l Add sodium. 4% D/W 0. 18% saline 30 ml/kg/day. or 5% D/W 7 ml/kg/day. + Normal saline 23 ml/kg/day. Assess serum K+ level. Consider parenteral nutrition.
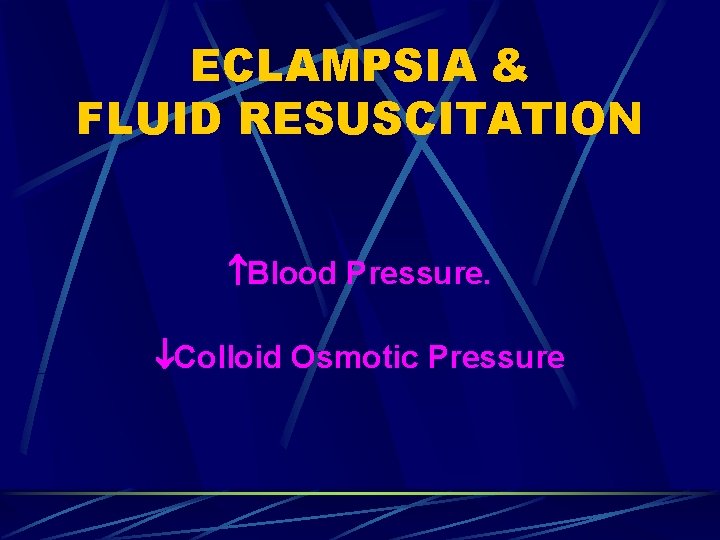
ECLAMPSIA & FLUID RESUSCITATION Blood Pressure. Colloid Osmotic Pressure
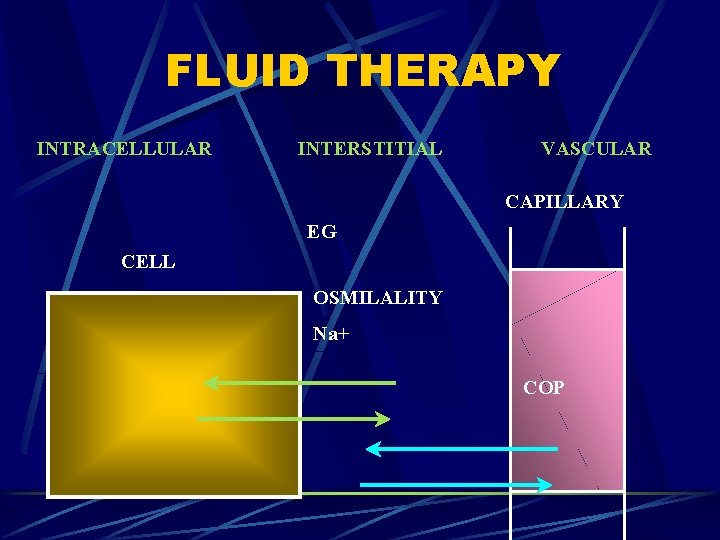
FLUID THERAPY INTRACELLULAR INTERSTITIAL VASCULAR CAPILLARY EG CELL OSMILALITY Na+ COP
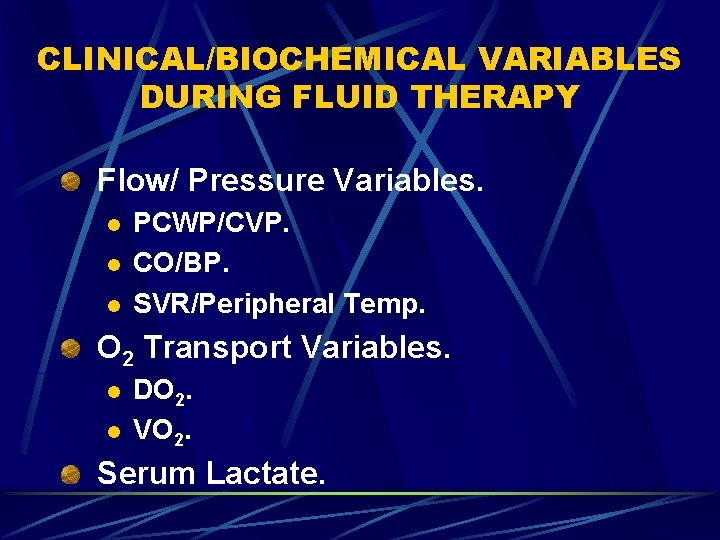
CLINICAL/BIOCHEMICAL VARIABLES DURING FLUID THERAPY Flow/ Pressure Variables. l l l PCWP/CVP. CO/BP. SVR/Peripheral Temp. O 2 Transport Variables. l l DO 2. VO 2. Serum Lactate.
CONCLUSION Fluid therapy should be taken seriously. Selection of solution. Patients suffering from critical conditions. l l Heart. Renal. Pulmonary. Pre-eclampsia/ Eclampsia