Current and Emerging Treatments for Chronic Spontaneous Urticaria
- Slides: 13
Current and Emerging Treatments for Chronic Spontaneous Urticaria Kirti J. Johal, MD Sarbjit S. Saini, MD Ann Allergy Asthma Immunol. October 2020; 125(4): 380 -387
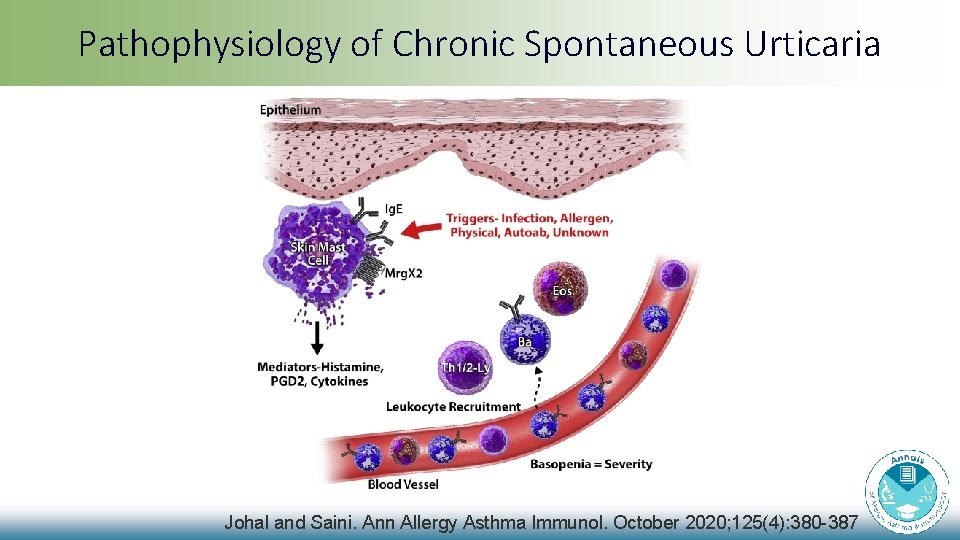
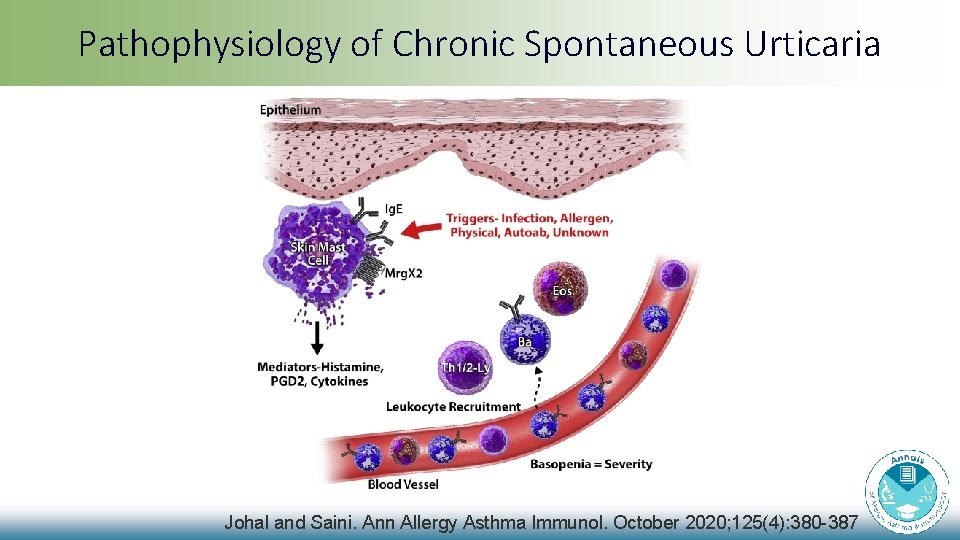
Pathophysiology of Chronic Spontaneous Urticaria Johal and Saini. Ann Allergy Asthma Immunol. October 2020; 125(4): 380 -387
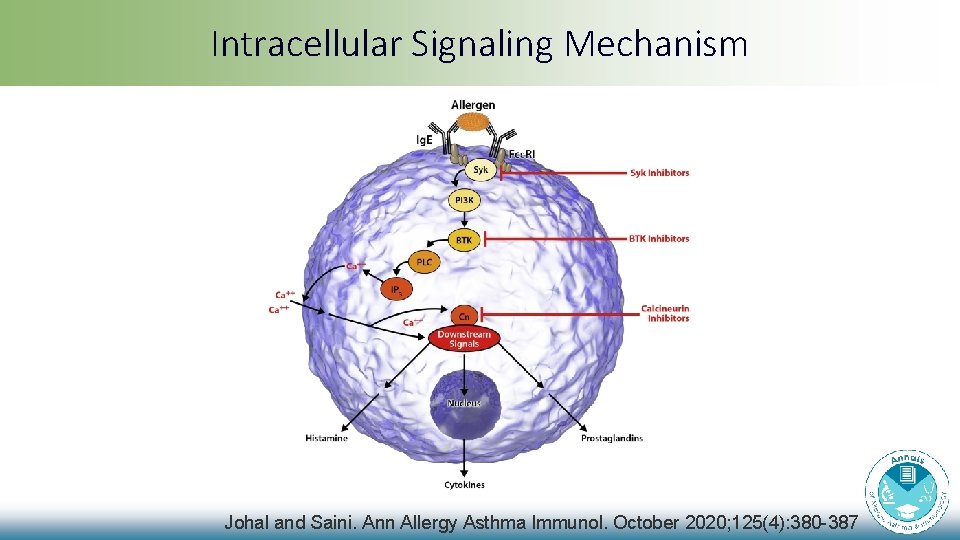
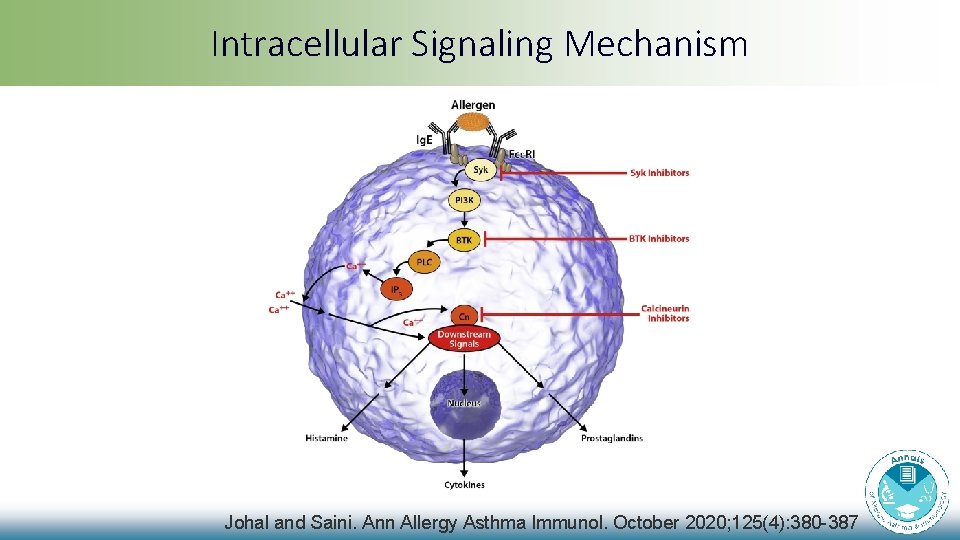
Intracellular Signaling Mechanism Johal and Saini. Ann Allergy Asthma Immunol. October 2020; 125(4): 380 -387
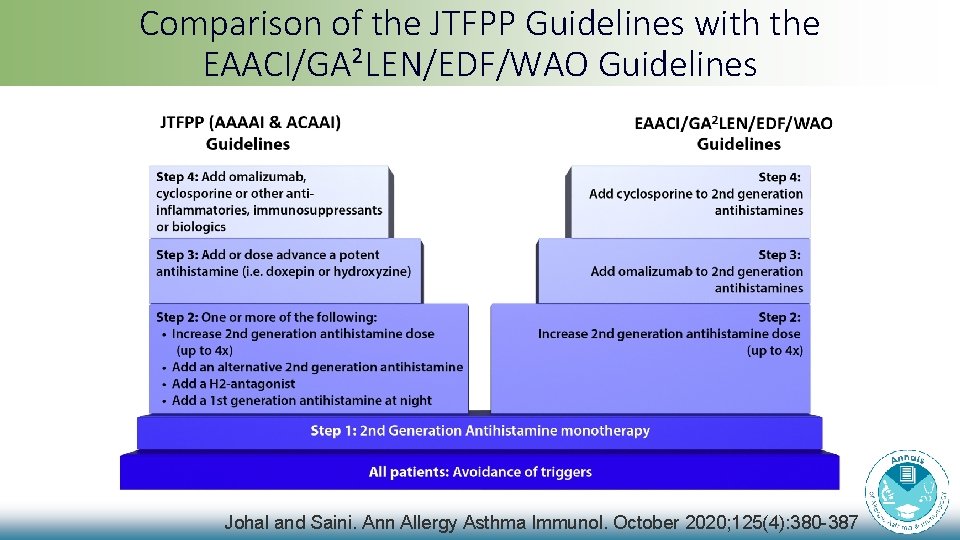
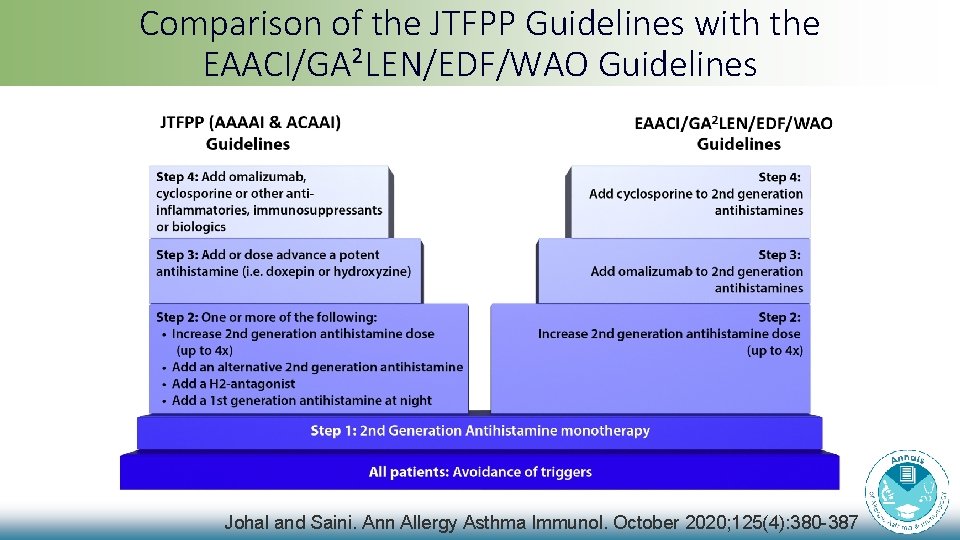
Comparison of the JTFPP Guidelines with the EAACI/GA²LEN/EDF/WAO Guidelines Johal and Saini. Ann Allergy Asthma Immunol. October 2020; 125(4): 380 -387
The Impact of Psychological Stress on Mast Cells Theoharis C. Theoharides, MS, MPhil, Ph. D, MD Ann Allergy Asthma Immunol. October 2020; 125(4): 388 -392
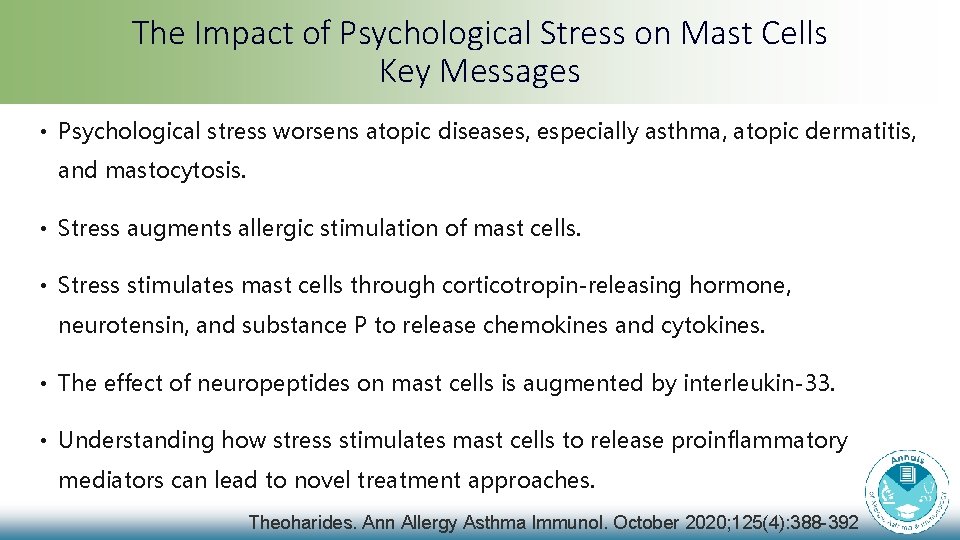
The Impact of Psychological Stress on Mast Cells Key Messages • Psychological stress worsens atopic diseases, especially asthma, atopic dermatitis, and mastocytosis. • Stress augments allergic stimulation of mast cells. • Stress stimulates mast cells through corticotropin-releasing hormone, neurotensin, and substance P to release chemokines and cytokines. • The effect of neuropeptides on mast cells is augmented by interleukin-33. • Understanding how stress stimulates mast cells to release proinflammatory mediators can lead to novel treatment approaches. Theoharides. Ann Allergy Asthma Immunol. October 2020; 125(4): 388 -392
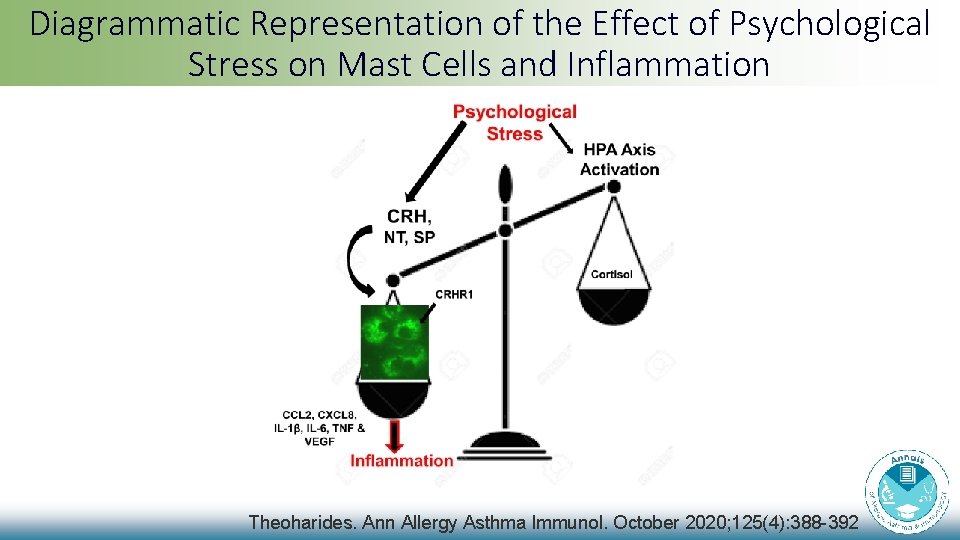
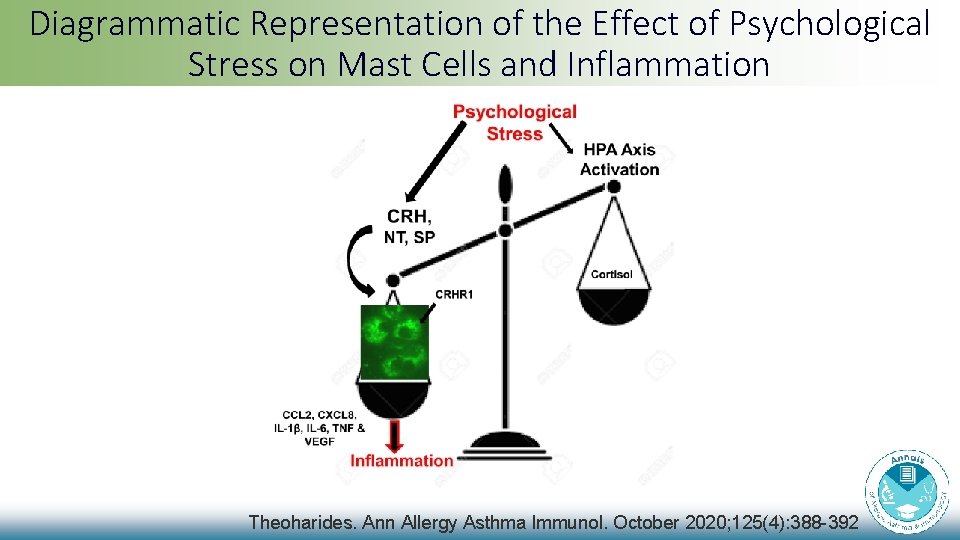
Diagrammatic Representation of the Effect of Psychological Stress on Mast Cells and Inflammation Theoharides. Ann Allergy Asthma Immunol. October 2020; 125(4): 388 -392
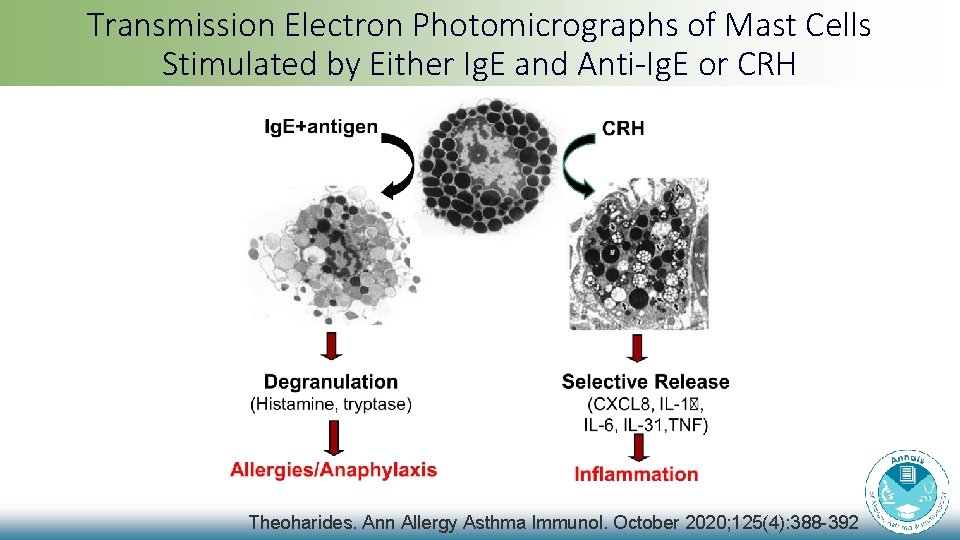
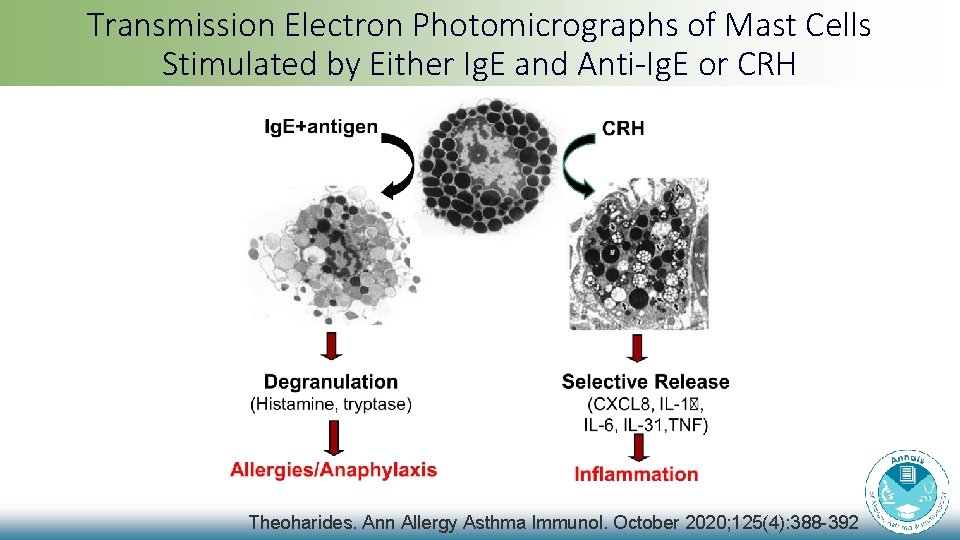
Transmission Electron Photomicrographs of Mast Cells Stimulated by Either Ig. E and Anti-Ig. E or CRH Theoharides. Ann Allergy Asthma Immunol. October 2020; 125(4): 388 -392
Chronic Stress and Asthma in Adolescents Jeremy Landeo-Gutierrez, MD, MPH Juan C. Celedón, MD, Dr. PH Ann Allergy Asthma Immunol. October 2020; 125(4): 393 -398
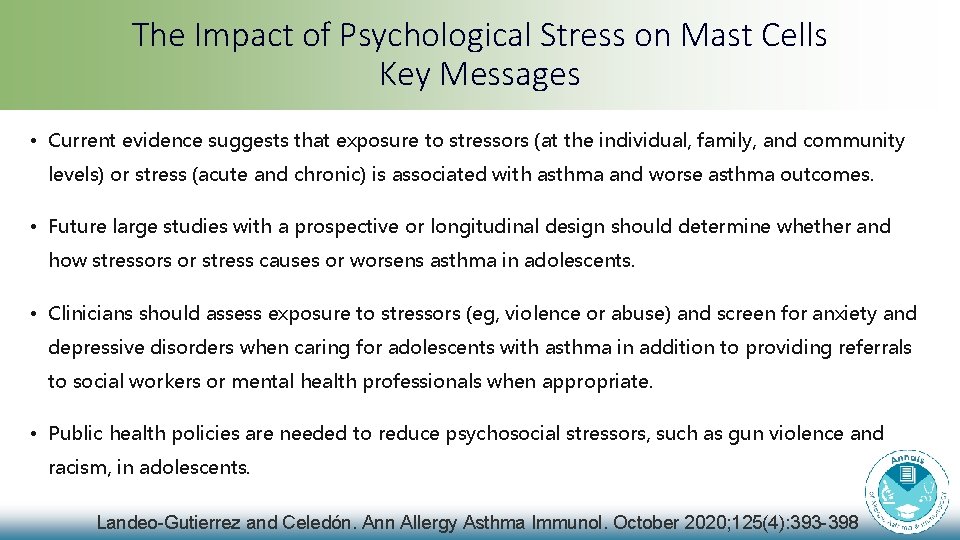
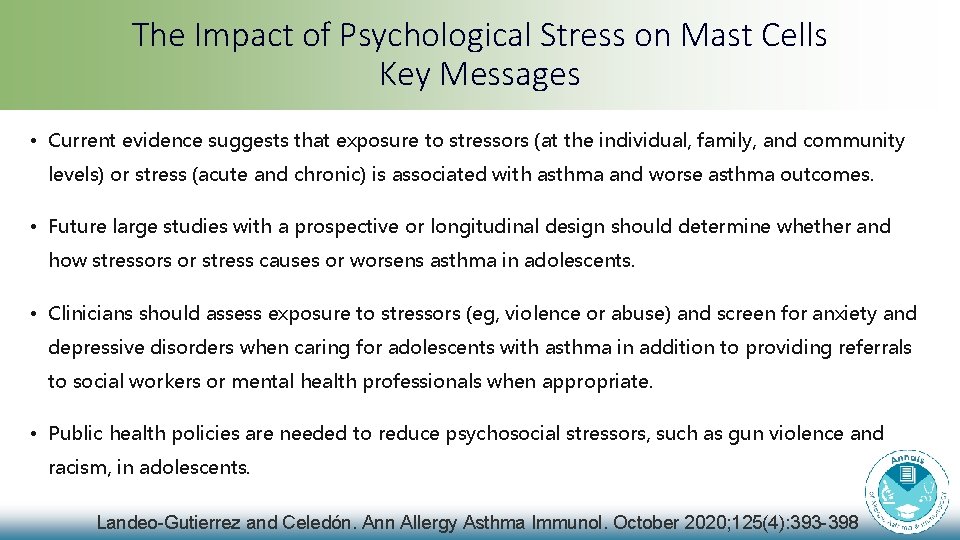
The Impact of Psychological Stress on Mast Cells Key Messages • Current evidence suggests that exposure to stressors (at the individual, family, and community levels) or stress (acute and chronic) is associated with asthma and worse asthma outcomes. • Future large studies with a prospective or longitudinal design should determine whether and how stressors or stress causes or worsens asthma in adolescents. • Clinicians should assess exposure to stressors (eg, violence or abuse) and screen for anxiety and depressive disorders when caring for adolescents with asthma in addition to providing referrals to social workers or mental health professionals when appropriate. • Public health policies are needed to reduce psychosocial stressors, such as gun violence and racism, in adolescents. Landeo-Gutierrez and Celedón. Ann Allergy Asthma Immunol. October 2020; 125(4): 393 -398
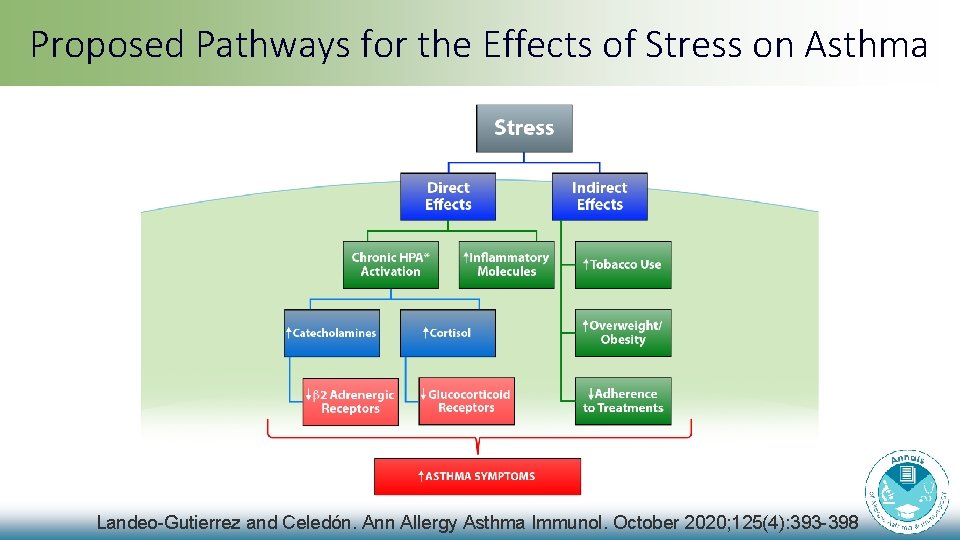
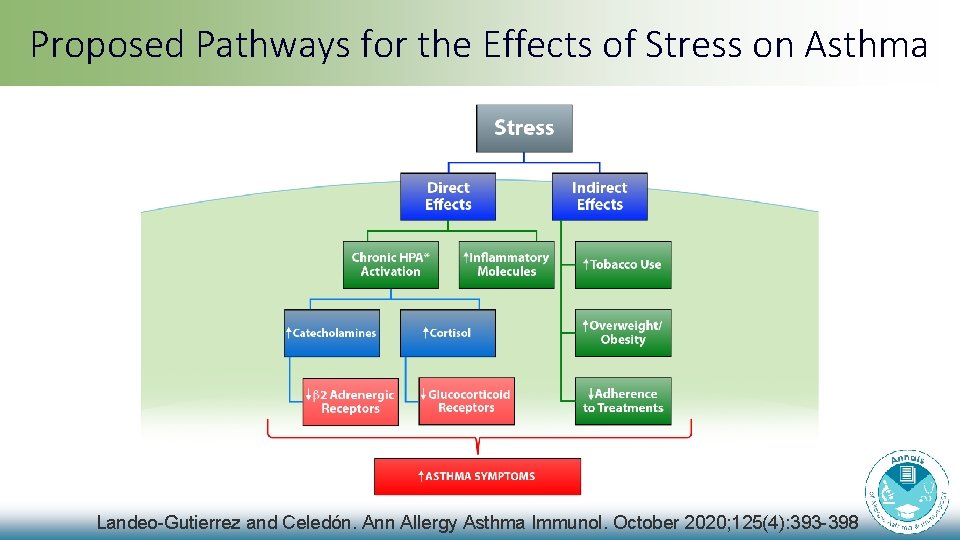
Proposed Pathways for the Effects of Stress on Asthma Landeo-Gutierrez and Celedón. Ann Allergy Asthma Immunol. October 2020; 125(4): 393 -398
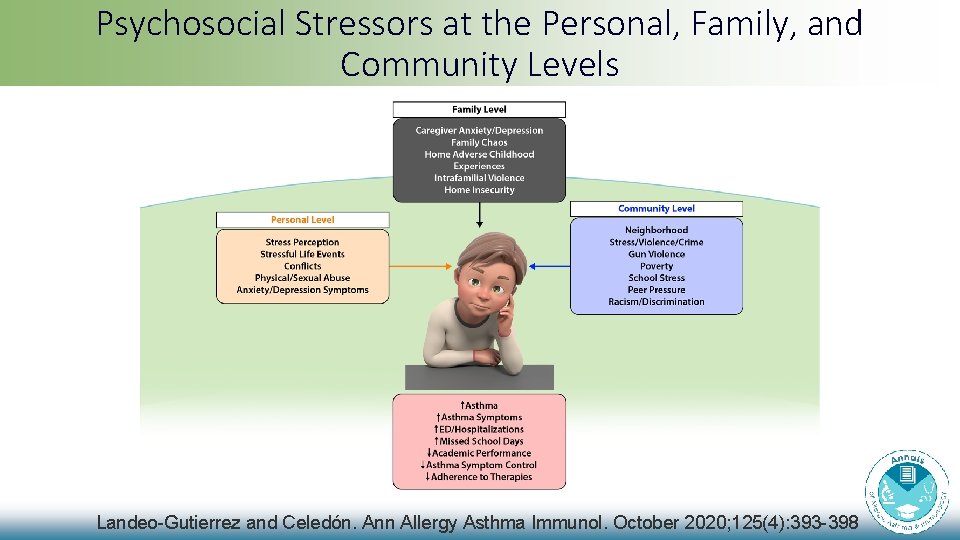
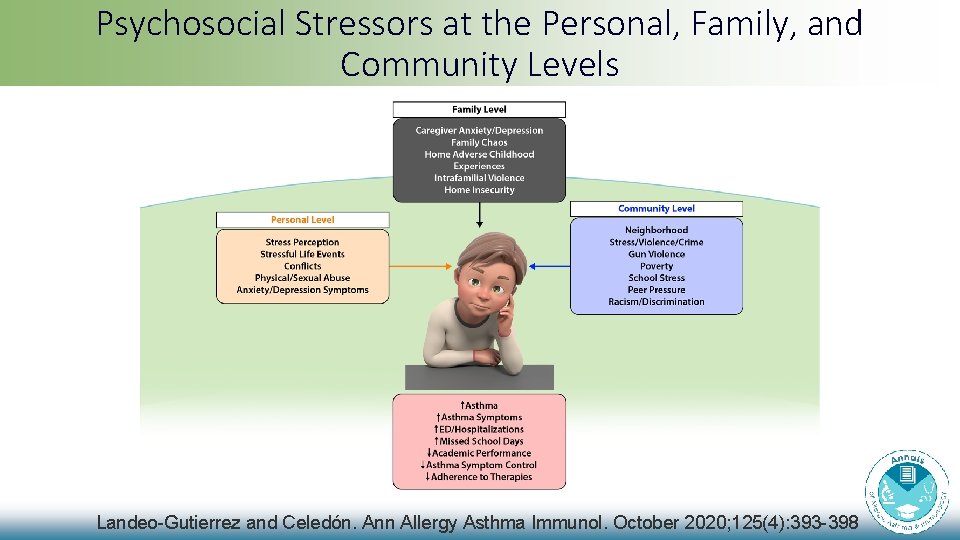
Psychosocial Stressors at the Personal, Family, and Community Levels Landeo-Gutierrez and Celedón. Ann Allergy Asthma Immunol. October 2020; 125(4): 393 -398