Cultural Diversity in Psychotherapy CulturallyTailored Interventions and Multicultural










- Slides: 39

Cultural Diversity in Psychotherapy: Culturally-Tailored Interventions and Multicultural Approaches 9/25/18 Arthur “Trey” Andrews, Ph. D
About This Series: Core Topics for Behavioral Health Providers • BHECN's webinar series designed to educate behavioral health trainees and providers about practical topics in behavioral health • Expert presenters provide a mixture of principles and case based application • All webinars are free of charge

Core Topics for Behavioral Health Providers Cultural Diversity in Psychotherapy CID 39838 September 25, 2018 Target Audience: Providers and trainees from the following fields: Physicians, psychologists, advanced practice providers, nurse, licensed mental health therapists, and social workers. Educational Objectives: • Discuss treatment disparities and common barriers to care • Describe the role and types of cultural adaptations to treatment • Identify strategies for implementing adaptations to treatment with examples focusing on Latinx populations.
Requirements for Successful Completion In order to receive continuing education credits or contact hours, you must: ØSign into Go to Webinar and attend the entire learning activity ØComplete the online evaluation by signing in to My Account at www. unmc. edu/cce ü Go to Evaluate a Course/Print Certificate ü Use CME Activity Code 39838 ü Save and print your certificate. Retain for future documentation. Certificates are available up to 60 -days post activity upon completion of the evaluation and attestation.
CREDIT The University of Nebraska Medical Center, Center for Continuing Education is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. The University of Nebraska Medical Center, Center for Continuing Education designates this live activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. The University of Nebraska Medical Center College of Nursing Continuing Nursing Education is accredited with distinction as a provider of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation. This activity is provided for 1. 0 contact hour under ANCC criteria. This activity has been planned and implemented in accordance with the accreditation requirements and policies of the American Nurses Credentialing Center’s Commission on Accreditation (ANCC) through the joint providership of the University of Nebraska Medical Center College of Nursing Continuing Nursing Education (UNMC CON CNE) (provider), University of Nebraska Medical Center, Center for Continuing Education (UNMC CCE), and Behavioral Health Education Center of Nebraska (BHECN). This program meets the criteria of an approved continuing education program for Licensed Mental Health Providers. This program meets the criteria of an approved continuing education program for Social Work.
DISCLOSURE DECLARATION As a provider accredited by ACCME, the University of Nebraska Medical Center, Center for Continuing Education, the University of Nebraska Medical Center, College of Nursing Continuing Nursing Education, and the American Nurses Credentialing Center’s Commission on Accreditation must ensure balance, objectivity, independence, and scientific rigor in its educational activities. Faculty are encouraged to provide a balanced view of therapeutic options by utilizing either generic names or the trade names of several to ensure impartiality. All speakers, planning committee members and others in a position to control continuing medical education content participating in a University of Nebraska Medical Center, Center for Continuing Education, University of Nebraska Medical Center, College of Nursing Continuing Nursing Education, and American Nurses Credentialing Center’s Commission on Accreditation activity are required to disclose relationships with commercial interests. A commercial interest is any entity producing, marketing, re-selling, or distributing health care goods or services consumed by, or used on, patients. Disclosure of these commitments and/or relationships is included in these course materials so that participants in the activity may formulate their own judgments in interpreting its content and evaluating its recommendations. This activity may include presentations in which faculty may discuss off-label and/or investigational use of pharmaceuticals or instruments not yet FDA-approved. Participants should note that the use of products outside currently FDA-approved labeling should be considered experimental and are advised to consult current prescribing information for FDA-approved indications. All materials are included with the permission of the authors. The opinions expressed are those of the authors and are not to be construed as those of the University of Nebraska Medical Center, Center for Continuing Education, University of Nebraska Medical Center, College of Nursing Continuing Nursing Education, or American Nurses Credentialing Center’s Commission on Accreditation.
FACULTY AND PLANNING COMMITTEE DISCLOSURES All faculty and planning committee members have no financial relationships to disclose. Arthur “Trey” Andrews, Ph. D Assistant Professor Department of Psychology University of Nebraska Lincoln Heidi Keeler, Ph. D, RN Assistant Professor College of Nursing-Omaha Division Director, Continuing Nursing Education Director, Office of Community Engagement University of Nebraska Medical Center Howard Liu, MD Associate Professor Department of Psychiatry Director, Behavioral Health Education Center of Nebraska University of Nebraska Medical Center Brenda Ram, CMP, CHCP Interim Director, Educational Programs Center for Continuing Education University of Nebraska Medical Center
About BHECN The Behavioral Health Education Center of Nebraska (BHECN), pronounced “beacon”, was established in 2009 by a legislative bill to address the shortage of behavioral health professionals in rural and underserved areas of the state. unmc. edu/bhecn MISSION: BHECN is dedicated to improving access to behavioral health care across the state of Nebraska by developing a skilled and passionate workforce.
Announcements • Attendees are muted • To ask a question, please type it in to the “Questions” box in your Go. To. Webinar control panel • Slides are available to download in “Handouts” section of control panel • Please complete survey after the webinar
Recording available Click the link to view a recording of today's webinar and information on future webinars https: //www. unmc. edu/bhecn/education/onlinetraining/core-topics-webinars. html

Next webinar Introduction to Social Anxiety: Identification and Treatment Options October 11 th 2 -3: 30 pm Dr. Deb Hope of UNL
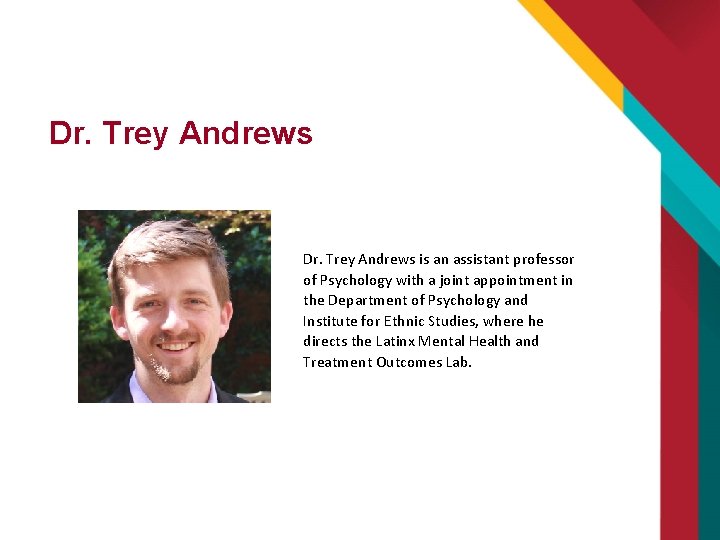
Dr. Trey Andrews is an assistant professor of Psychology with a joint appointment in the Department of Psychology and Institute for Ethnic Studies, where he directs the Latinx Mental Health and Treatment Outcomes Lab.
Cultural Diversity in Psychotherapy: Culturally-Tailored Interventions and Multicultural Approaches Arthur “Trey” Andrews, Ph. D. BHECN, 9/25/2018
A Little about Me Assistant Professor in Psychology and Ethnic Studies (Latina/o Studies) at UNL Established the Latinx Mental Health and Treatment Outcomes Lab Ph. D from Arkansas in 2014, internship and postdoc at MUSC All focused on addressing Latinx mental health disparities Conducted overwhelming majority of my clinical hours with Latinxs in Spanish
A Little about You What has your diversity/multicultural training been like? Any training on cultural adaptations? Biases or blindspots in clinical care? How has this influenced your approach to diversity issues in clinical care? For example, what issues do you pay attention to or maybe miss?

Overview for Today What we will focus on: Treatment disparities and common barriers to care Roles and types of cultural adaptations to treatment Strategies for implementing adaptations to treatment with examples focusing on Latinx populations
What is it? What do we mean when we say “cultural diversity”?
What is it? What do we mean when we say “cultural diversity”? Two potential meanings that we can use: 1) Working with individuals from traditionally marginalized groups – racial/ethnic minority populations, language, low SES, gender and gender identity, sexual orientation, religious minority, etc. Culture can incorporate any of these components 2) Working with individuals who differ from us across one of these dimensions, even if they are not necessarily marginalized or disempowered
Why You Should Care: Reason 1 Regardless of what you do, experiences with biases or discrimination will impact your patients/clients of marginalized backgrounds In matched samples and experiments, Latinxs, African Americans, and Native Americans are: Steered away from home financing More frequently denied rental applications Asked to pay more for housing Employed less often More often denied or provided inappropriate health care Less often tracked to gifted and talented programs More likely to be found guilty of comparable crimes Given longer sentences for similar crimes Despite being less likely to have drugs and weapons, Latinxs and African Americans were roughly four times as likely to be stopped during “stop and frisk”
The Individual Impact of Discrimination Stereotype threat Individuals perform closer to the stereotype when reminded of it Academics are most common example A variety of negative health outcomes are associated with experiencing discrimination of all kinds Cardiovascular stress response when experiencing discrimination Cardiovascular disease Depression Worse cancer outcomes A variety of anxiety disorders Poorer mental health treatment outcomes IAT scores within a given county are associated with that county’s: Access to healthcare among African Americans Death rate due to cardiovascular disease among African Americans IAT scores also predict the quality of care given by a physician
Psychologists aren’t Immune To test discrimination and biases, the author called 320 mental health practitioners Recipients were randomly chosen from phone listings of an insurance company All practitioners had Ph. Ds or equivalent degrees All calls were made at night so that scripted voice messages could be left
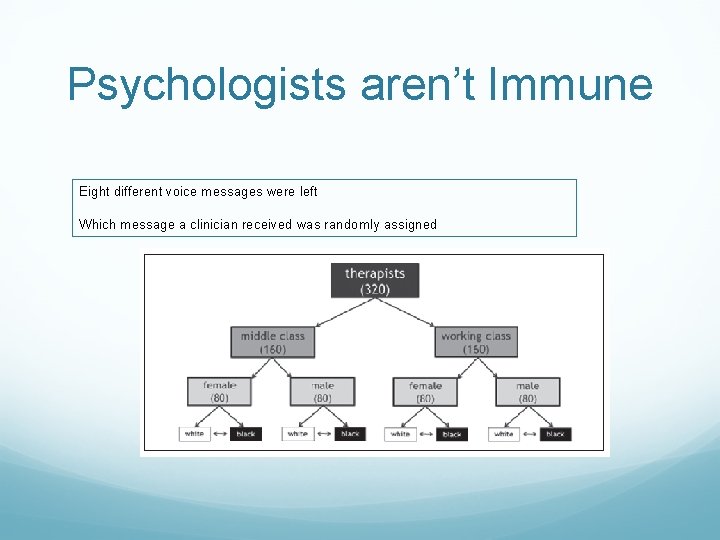
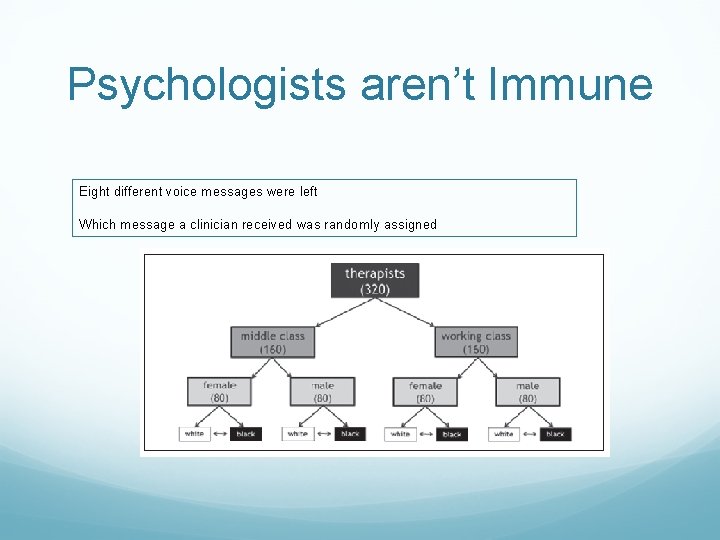
Psychologists aren’t Immune Eight different voice messages were left Which message a clinician received was randomly assigned
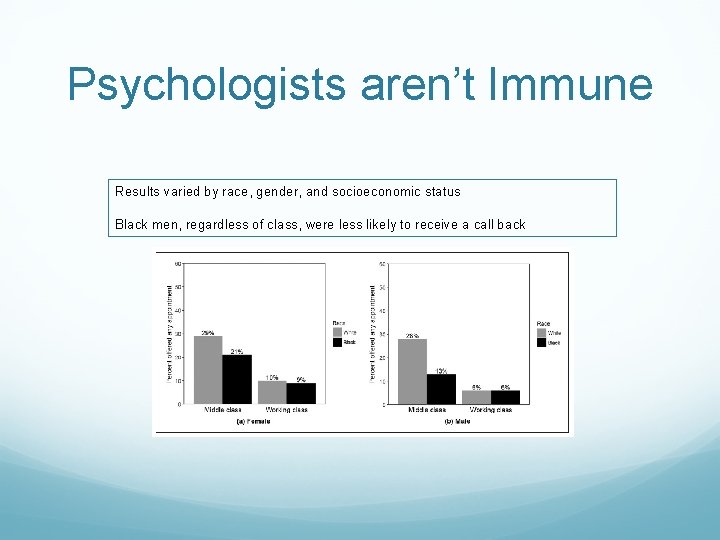
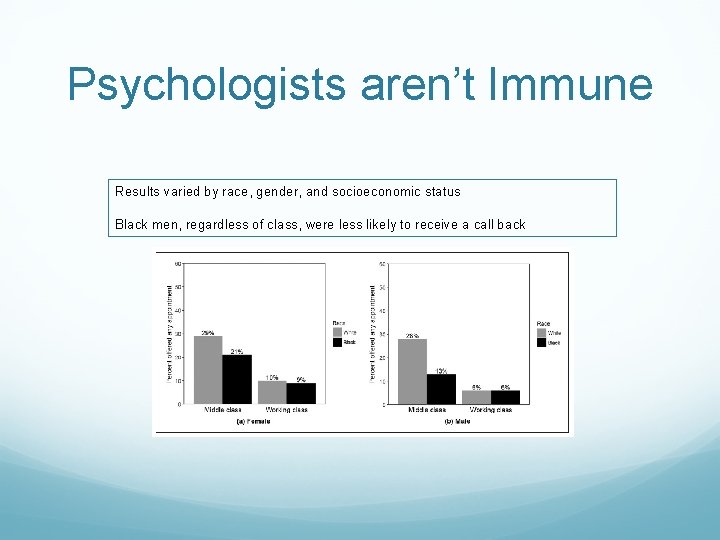
Psychologists aren’t Immune Results varied by race, gender, and socioeconomic status Black men, regardless of class, were less likely to receive a call back

Why You Should Care: Reason 2 Several minority and marginalized populations underutilize mental health services Enter into treatment less Drop out earlier Receive less quality care Barriers are varied Some systemic Some cultural Some due to interaction with clinician

Why You Should Care: Reason 2 Several minority and marginalized populations underutilize mental health services Enter into treatment less Drop out earlier Receive less quality care Barriers are varied Some systemic Some cultural Some due to interaction with clinician
What Clinicians Can Do Two cultural adaptation strategies for addressing disparities: 1. Develop empirically-supported treatments to address disparities 2. Adapt treatments or practice to accommodate individual differences as part of evidence-based practice
Some Culturally-Adapted Examples Safe. Care (adapted for Latinxs) CM-TFT (TF-CBT) GANA Program (PCIT for Mexican Americans) Psychotherapy Adaptation and Modification Framework (guidelines for general CBT) Culturally-adapted one-session treatment (multiple hour, single-session intervention)
Developing Adapted ESTs Numerous frameworks, but all follow similar recommendations: A – Assessment D – Decision making A – Adaptation P – Production T – Topical Experts I – Integration T – Training T – Testing Taken from: Wingood, G. M. , & Di. Clemente, R. J. (2008). The ADAPT-ITT model: a novel method of adapting evidence-based HIV Interventions. JAIDS Journal of Acquired Immune Deficiency Syndromes, 47, S 40 -S 46.
So, How about Individually-Tailored EBPP? There are many models for individually-tailoring evidence-based practice (e. g. , Sue & Sue) Some common recommendations to tailor practice based on culture: Greater inclusion of cultural values Client-therapist match (e. g. , ethnicity or language) Coordination with community agencies (e. g. , churches) Attention to group-specific issues
Inclusion of Cultural Values You do not need to be an expert, but using common recommendations with Latinxs as an example: Religion Understanding beliefs about mental illness, and what ultimately decides the future - fatalismo Role of family Including gender, parent, child, and extended family roles Machismo, marianismo, respecto Values could also impact approach to clinician May not be appropriate to voice disagreement with “expert”
Assessing Cultural Values Don’t be afraid to ask! Do ask about specific areas or values: “What does it mean to you to be a woman/mother…? ” When appropriate, don’t be afraid to acknowledge differences. It may be reassuring to model appropriate acknowledgement of different experiences Don’t assume you know. Culture varies tremendously within any underserved and under-researched group Do ask people from all backgrounds

Using Cultural Values in Treatment Instead of arguing or viewing them as a weakness, approach cultural values as a strength Enhancing family cohesion tends to improve treatment outcomes for depression and PTSD You can also utilize positive aspects of cultural values to enhance treatment components

Coordination with Community Agencies Reaching out to community leaders Could discuss complementarity of treatment with religious values with appropriate leader (e. g. , pastor or priest) Better assess community resources Support groups Religious services Financial/basic needs resources

Group-Specific Issues Latinx Immigrants First-generation immigrants likely experienced a traumatic event while immigrating Immigration itself can often be considered traumatic These issues may need to be directly assessed May be less likely to speak English fluently Second generation and generation 1. 5 Experience significantly more traumatic events than their parents Often have cultural conflicts with parents May more often recognize discrimination
Addressing Language Avoid using family as translators/interpreters at all cost. If unavoidable, remember: Children/partners become language broker roles and may have no training, may not feel comfortable discussing particular topics, and may have their own reactions to your communication When working with translators, speak in brief phrases and be mindful of colloquialisms. Check in with them after. Try to use a language that is common to the group if working with families (try not to have asides that others won’t understand)
Beyond Cultural Tailoring In addition to cultural tailoring, typical recommendations for reaching underserved populations: Flexible location Flexible hours Emphasis on case management Telemedicine Developing specialty services to address group-specific concerns Frequency of child trauma Lack of community resources Rurality Parenting groups for families at risk for physical abuse Sexual safety and related cultural issues

Example 1 - Eduardo Presented to integrated care clinic with social anxiety issues During assessment, became evident that social anxiety resulted from race-based bullying How should we approach it?
Example 2 - Blanca Presented to traditional care clinic for PTSD concerns Prolonged exposure and cognitive processing therapy were offered and client chose PE Client appeared as treatment resistant as client frequently verbalized her doubts about treatment in general Family plays a central role in her life (familismo) How might we approach this?
Example 3 - Jorge Presented for PTSD and traumatic grief Mother had passed away. She was very religious. Was told by religious leader that his mother was dying because he was gay. Treatment approach was a novel approach called Written Exposure Therapy How might we modify treatment/assessment?