Cultural and Religious Issues Impacting EndofLife Care Sheri





- Slides: 18
Cultural and Religious Issues Impacting End-of-Life Care Sheri Mila Gerson, LICSW, ACHP-SW Anne Roberts, MSSW, LSWAIC Mark Snelling, D. Min Washington State Hospice and Palliative Care Organization Fall Conference, Chelan, Washington October 10, 2017

Objectives What impact does culture play on end-of-life care? How can Hospice and Palliative Care staff respectfully support the diverse, multi-cultural patient populations being served? identify at least two ways cultural backgrounds or religious beliefs impact current hospice or palliative care practice describe at least three cultural and religious practices at end of life which may be “outside usual experience” identify several measures to implement in work setting to facilitate a more open and accepting response to others’ cultural or religious practices.

What is culture?
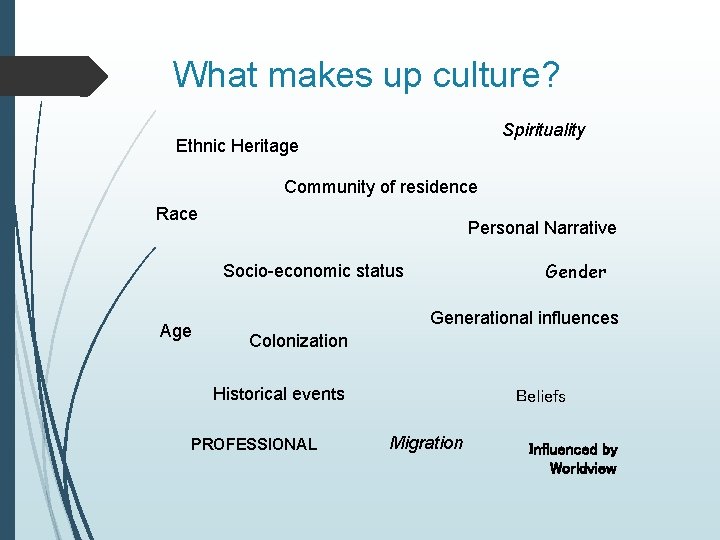
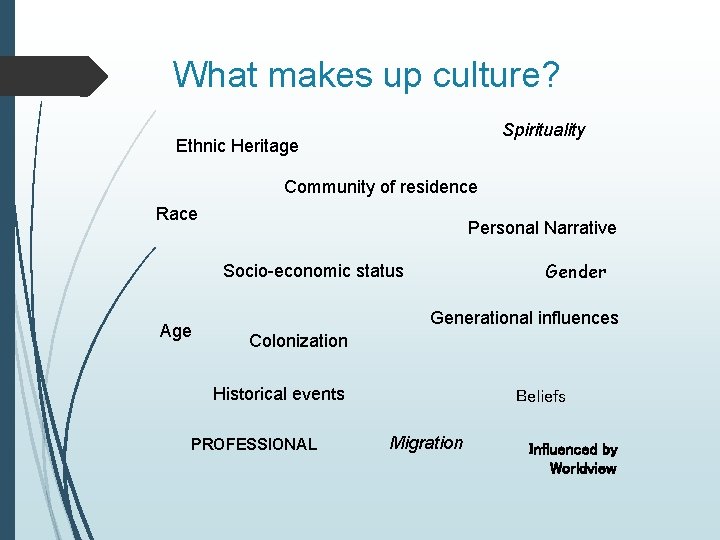
What makes up culture? Spirituality Ethnic Heritage Community of residence Race Personal Narrative Gender Socio-economic status Age Generational influences Colonization Historical events PROFESSIONAL Beliefs Migration Influenced by Worldview
Palliative Care Challenges: The culture of the individual requesting hospice/palliative care Emotional expression/experience of grief by patient/family Requests by family regarding disclosure to patient Conflicted or diverse perspectives of family members Use of interpreters After death plans and rituals Organizational policy regarding end of life options or treatments Home and community resources
Patient Self Determination Act: 1. Patient autonomy people have the inherent right to make treatment decisions and should be active participants in their own care. 2. Informed decision making people have access to all the information relevant to the particular decision. 3. Truth telling information provided will be provided openly by health professionals 4. Control over the dying process people should and can have control over their own life and death. (Giger et al. , 2006)
Values vary among people: Informed-decision making Not all believe patient should be involved in decision making Autonomy Decision making may lie within community or family rather than a patient-centered model that values autonomy Truth-telling In some cultures or traditions, to say that death is near eliminates hope and there is a belief that it can hasten death Attitude and experience of pain/suffering Desire for pain avoidance is not a universally shared belief (Giger et al. , 2006; Lubimir & Wen, 2011; Zager & Yancy 2011)
Cultural Sensitivity ”In order to communicate respect for culturally different patients, it is important to assess the relevance of specific cultural values for a particular patient or family using cultural sensitivity” (Zager & Yancy 2011).
Cultural Competence Asking culturally sensitive questions to promote values and beliefs enhance cultural competence, . . . education may increase clinician awareness of cultural differences among patients. (Zager & Yancy, 2011) “lack of evidenced outcomes in which health disparities are indeed reduced through the implementation of cultural competence programs” (Chang & Dong, 2012)
Bias: • An inclination of temperament or outlook: personal or unreasoned judgment Stereotype: • Assumption that all members of a group possess similar attributes

Generalizations and stereotyping lead to: • False assumptions • Broad generalizations • Misunderstanding • Poor communication
Cultural Humility “Encourages individuals to identify their own biases and to acknowledge that those biases must be recognized. It is the “ability to maintain a stance that is otheroriented in relation to aspects of cultural identity that are most important to the [person]”
Elements of Cultural Humility “Cultivate a reflective and humble mind” Self-Questioning Cultural Immersion acknowledge assumptions and beliefs that are embedded in our own understanding, rather than delving into patient’s belief system Every patient encounter is a cross-cultural exercise – “even if you grew up on the same street” (Chang & Dong, 2012)
Elements of Cultural Humility “Cultivate a reflective and humble mind” Active listening A life-long process Learn from patients narrative without jumping to conclusions to avoid cultural stereotyping Cultural humility becomes not an end point but an active process of being in the world and being in relationships with others and self (Chang & Dong, 2012)

Asking culturally sensitive questions: ? ? ?
LANGUAGE MATTERS “When professional interpreters were not used, . . patients and families had inadequate understanding about diagnosis and prognosis during goals of care conversations, and patients had worse symptom management at the end of life, including pain and anxiety. " (Silva et al. , 2016)

• A caring stance can overcome almost anything • A continuous process based on listening • Begins with self
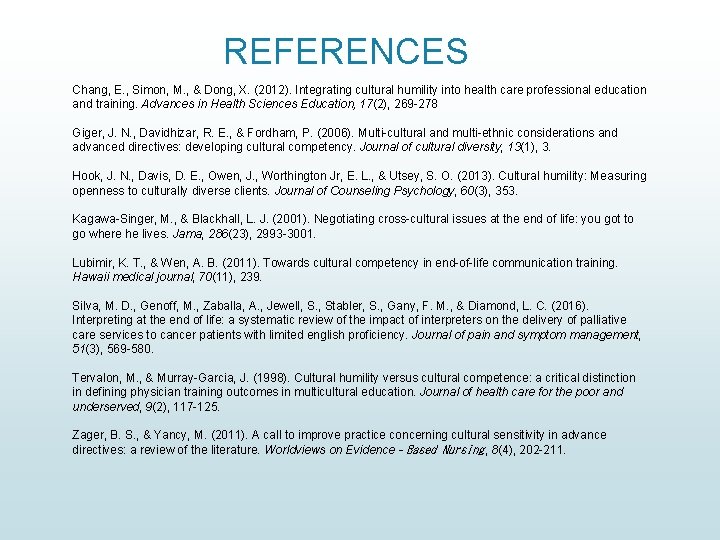
REFERENCES Chang, E. , Simon, M. , & Dong, X. (2012). Integrating cultural humility into health care professional education and training. Advances in Health Sciences Education, 17(2), 269 -278 Giger, J. N. , Davidhizar, R. E. , & Fordham, P. (2006). Multi-cultural and multi-ethnic considerations and advanced directives: developing cultural competency. Journal of cultural diversity, 13(1), 3. Hook, J. N. , Davis, D. E. , Owen, J. , Worthington Jr, E. L. , & Utsey, S. O. (2013). Cultural humility: Measuring openness to culturally diverse clients. Journal of Counseling Psychology, 60(3), 353. Kagawa-Singer, M. , & Blackhall, L. J. (2001). Negotiating cross-cultural issues at the end of life: you got to go where he lives. Jama, 286(23), 2993 -3001. Lubimir, K. T. , & Wen, A. B. (2011). Towards cultural competency in end-of-life communication training. Hawaii medical journal, 70(11), 239. Silva, M. D. , Genoff, M. , Zaballa, A. , Jewell, S. , Stabler, S. , Gany, F. M. , & Diamond, L. C. (2016). Interpreting at the end of life: a systematic review of the impact of interpreters on the delivery of palliative care services to cancer patients with limited english proficiency. Journal of pain and symptom management, 51(3), 569 -580. Tervalon, M. , & Murray-Garcia, J. (1998). Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. Journal of health care for the poor and underserved, 9(2), 117 -125. Zager, B. S. , & Yancy, M. (2011). A call to improve practice concerning cultural sensitivity in advance directives: a review of the literature. Worldviews on Evidence‐Based Nursing , 8(4), 202 -211.