CTSN Trials of Mitral Valve Repair and Replacement


- Slides: 29
CTSN Trials of Mitral Valve Repair and Replacement Michael Mack, M. D. Baylor Scott & White Health Dallas, TX
Disclosure Statement of Financial Interest I, Michael. Mack DO NOT have a financial interest/arrangement or affiliation with one or more organizations that could be perceived as a real or apparent conflict of interest in the context of the subject of this presentation.
What is CTSN? • Cardiothoracic Surgical Trials Network • Goal – Evaluate surgical approaches to cardiovascular disease • Support- $50 M (2013 -2018) – NIH • NHLBI • NINDS – CIHR- Canadian Institute of Health Research • PI’s – Richard Weisel-Toronto – Patrick O’Gara-Boston

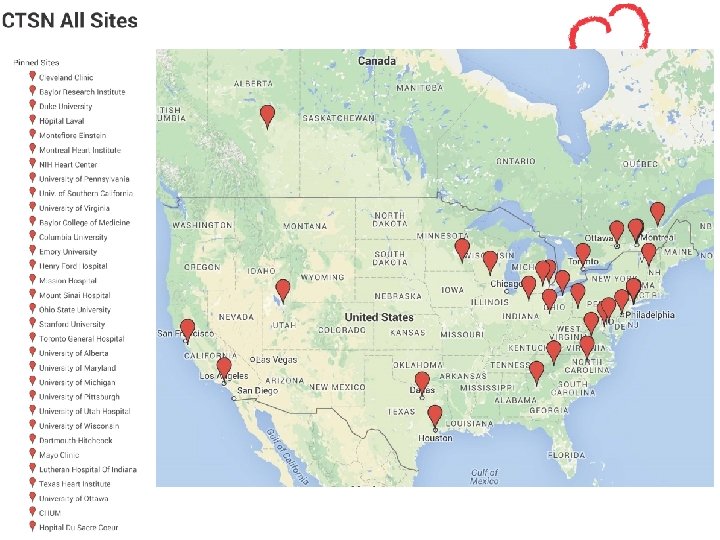
Core Sites • • • Baylor Research Institute Cleveland Clinic Foundation Duke University Hopital Laval de Quebec Montefiore Einstein Heart Center Montreal Heart Institute University of Pennsylvania University of Southern California University of Virginia Consortium Sites -12
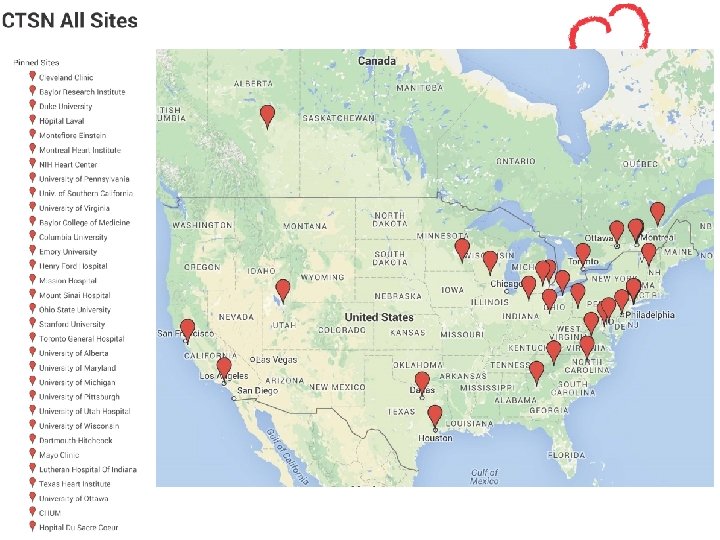

CTSN GERMAN SITES
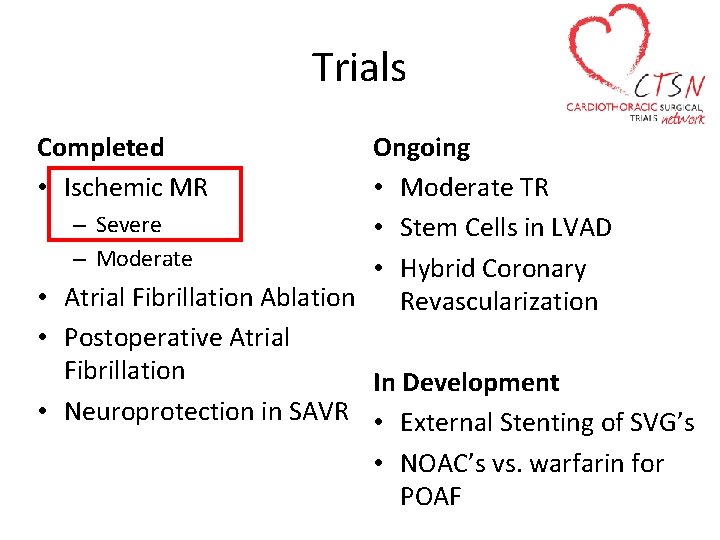
Trials Completed • Ischemic MR Ongoing • Moderate TR – Severe • Stem Cells in LVAD – Moderate • Hybrid Coronary • Atrial Fibrillation Ablation Revascularization • Postoperative Atrial Fibrillation In Development • Neuroprotection in SAVR • External Stenting of SVG’s • NOAC’s vs. warfarin for POAF
Ischemic MR • Severe MR: – Mitral valve repair with annuloplasty vs. mitral valve replacement with complete preservation of the subvalvular apparatus. • Moderate MR: – Mitral valve repair combined with coronary artery bypass grafting vs. coronary artery bypass grafting alone
For the last 20 years surgeons have considered that for all types of ischemia related mitral regurgitation mitral repair with a ring annuloplasty was better that an valve replacement However, because of the high mortality of this disease, it was time to find out - Was this the truth or a myth?
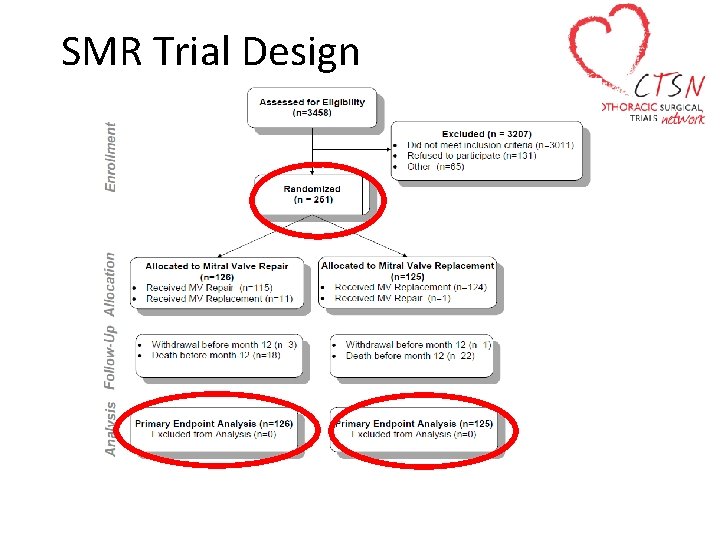
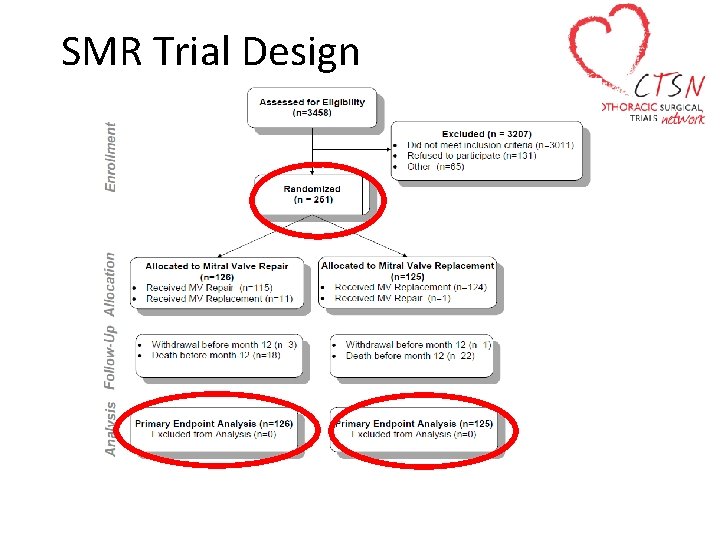
SMR Trial Design
Primary Endpoint • Degree of left ventricular reverse remodeling − Assessed by left ventricular end systolic volume index (LVESVI) using TTE at 12 months
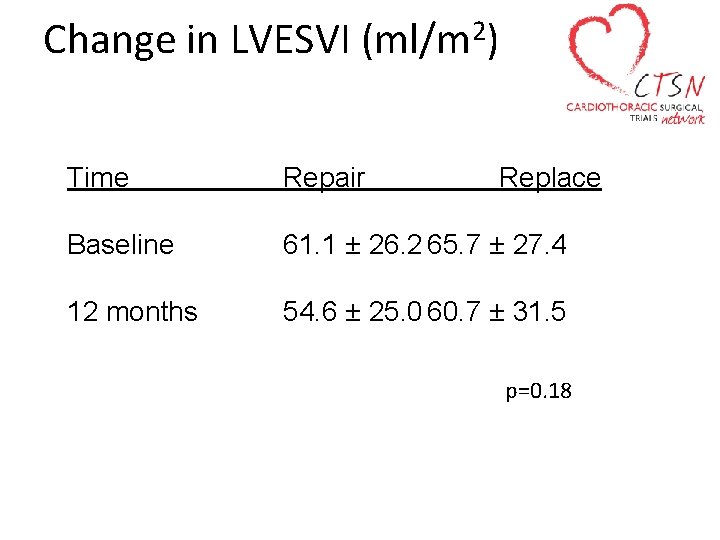
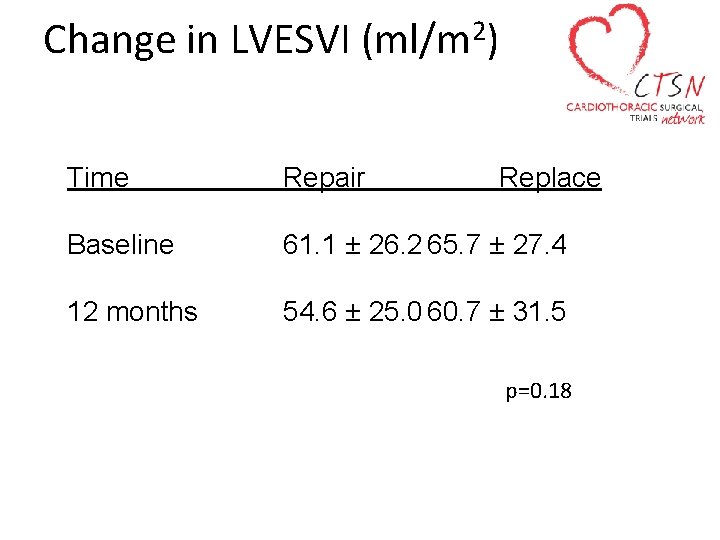
Change in LVESVI 2 (ml/m ) Time Repair Replace Baseline 61. 1 ± 26. 2 65. 7 ± 27. 4 12 months 54. 6 ± 25. 0 60. 7 ± 31. 5 p=0. 18
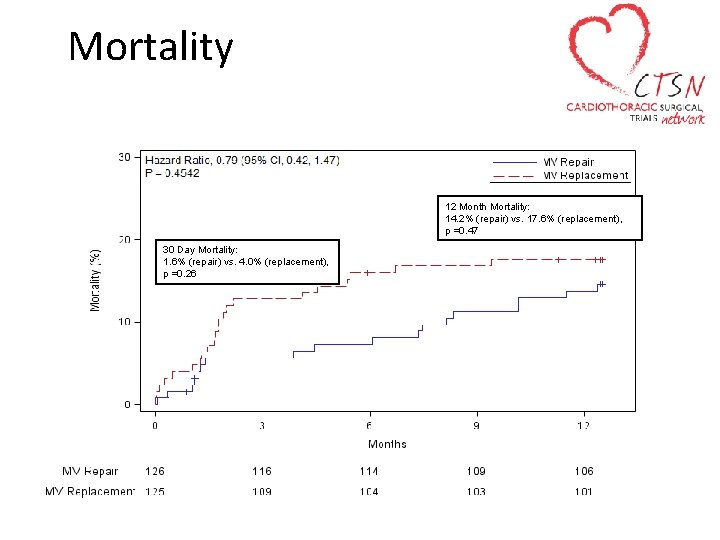
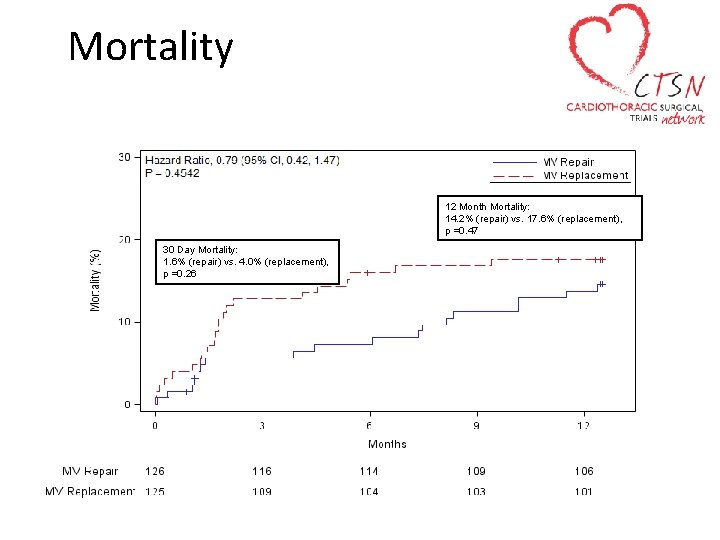
Mortality 12 Month Mortality: 14. 2% (repair) vs. 17. 6% (replacement), p =0. 47 30 Day Mortality: 1. 6% (repair) vs. 4. 0% (replacement), p =0. 26
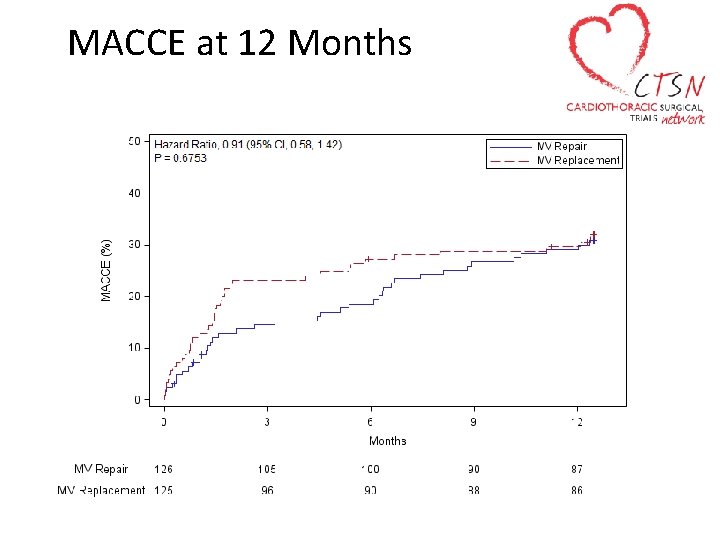
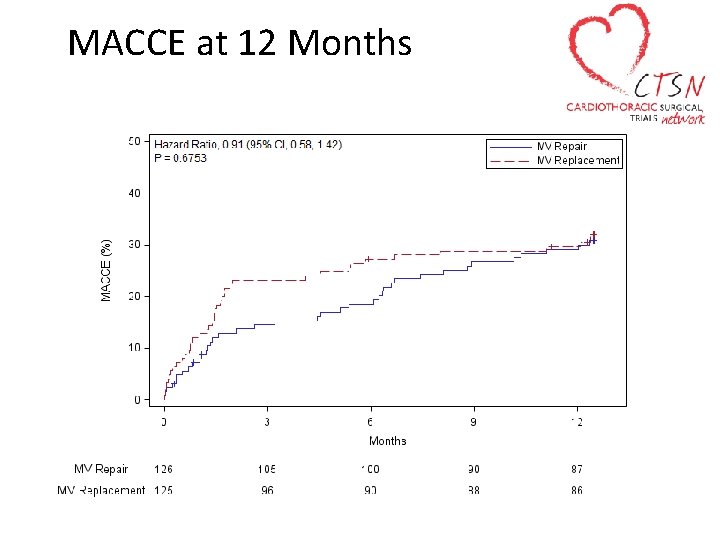
MACCE at 12 Months
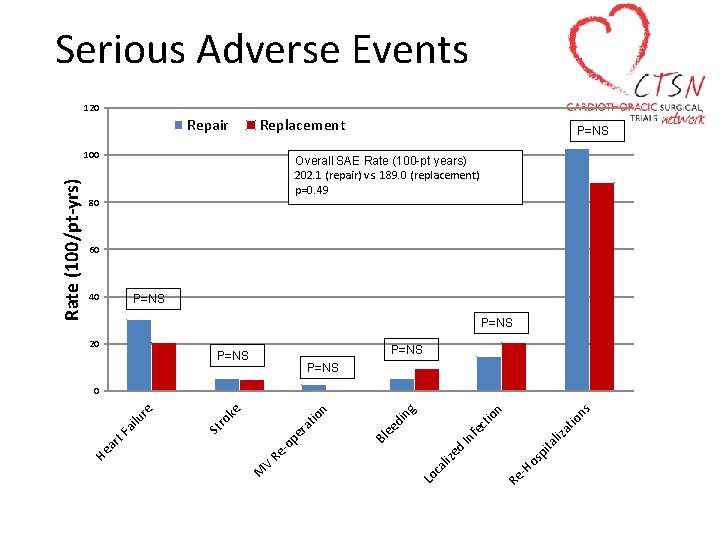
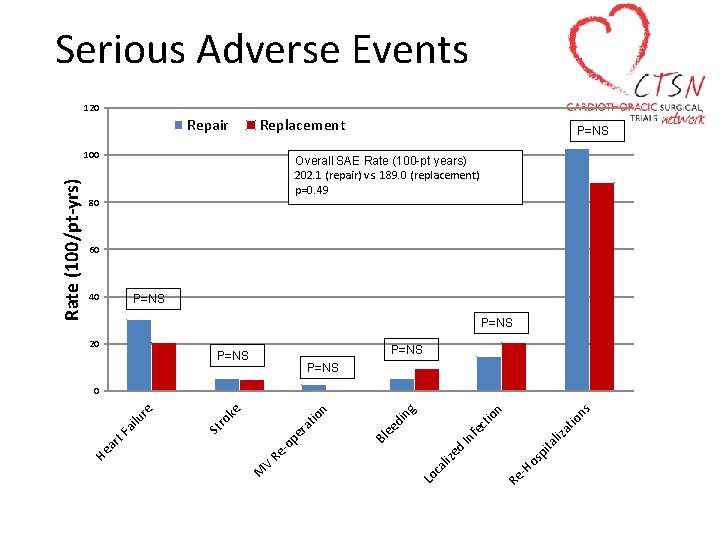
Serious Adverse Events 120 Repair Replacement Overall SAE Rate (100 -pt years) 202. 1 (repair) vs. 189. 0 (replacement) p=0. 49 80 60 40 P=NS 20 P=NS ns ita os p -H Re Lo ca liz ed In liz fe at io ct io n ng di ee pe r -o Re V M Bl at io n ro ke St ar t. F ai lu re 0 He Rate (100/pt-yrs) 100 P=NS
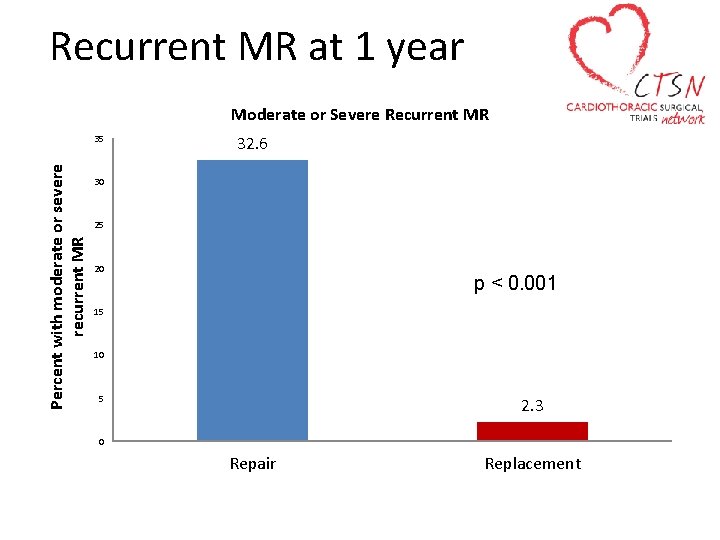
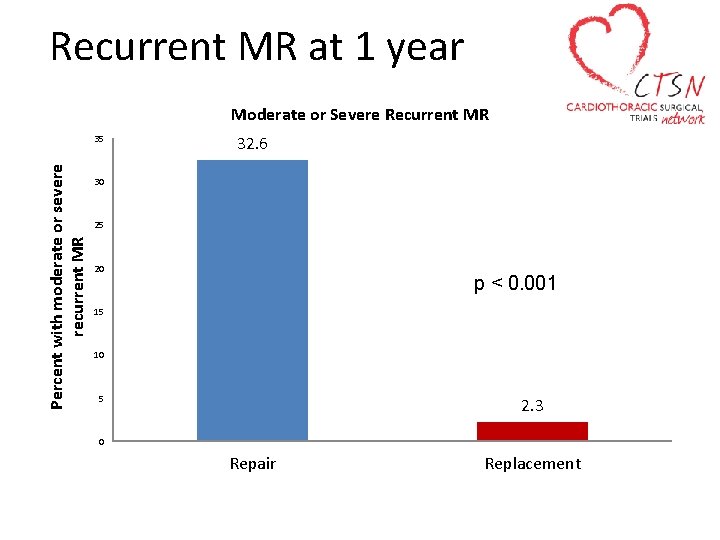
Recurrent MR at 1 year Moderate or Severe Recurrent MR Percent with moderate or severe recurrent MR 35 32. 6 30 25 20 p < 0. 001 15 10 5 2. 3 0 Repair Replacement
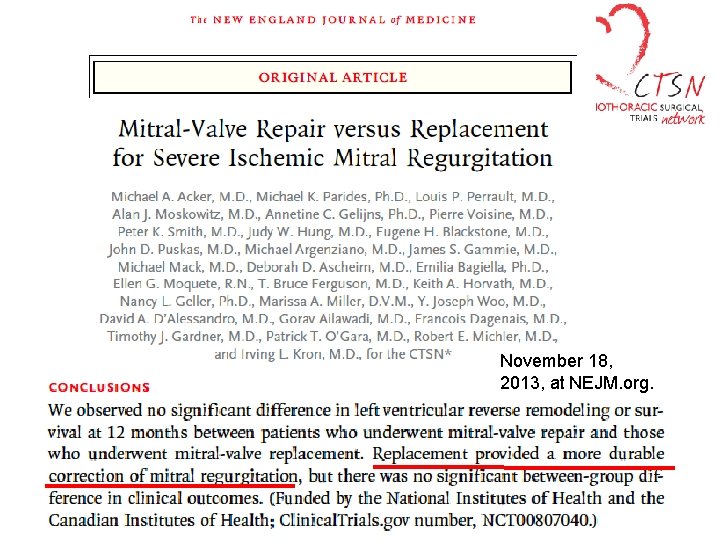
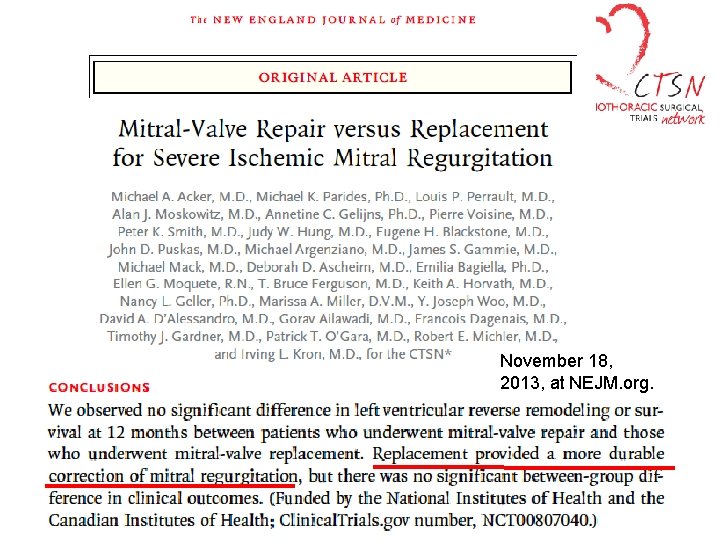
November 18, 2013, at NEJM. org.
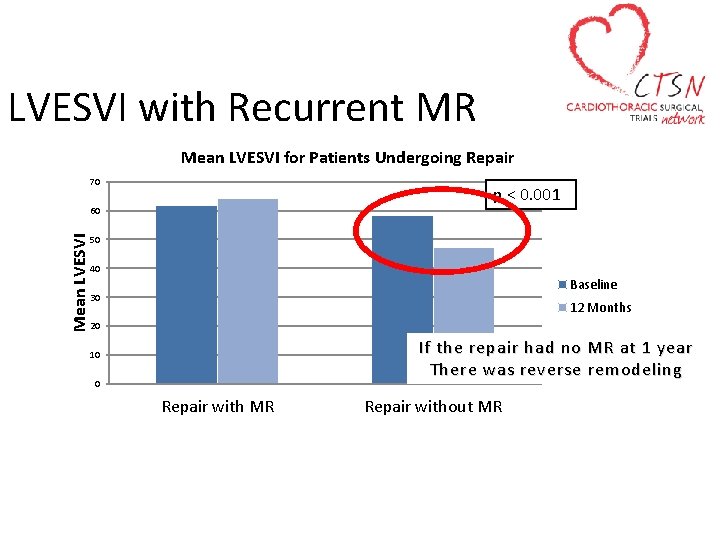
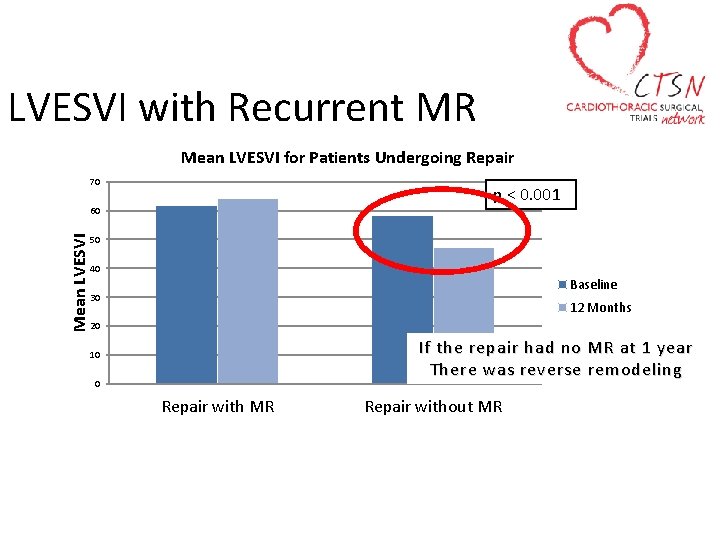
LVESVI with Recurrent MR Mean LVESVI for Patients Undergoing Repair 70 p < 0. 001 Mean LVESVI 60 50 40 Baseline 30 12 Months 20 If the repair had no MR at 1 year There was reverse remodeling 10 0 Repair with MR Repair without MR
• J Thorac Cardiovasc Surg 2015; 149: 752 -61)
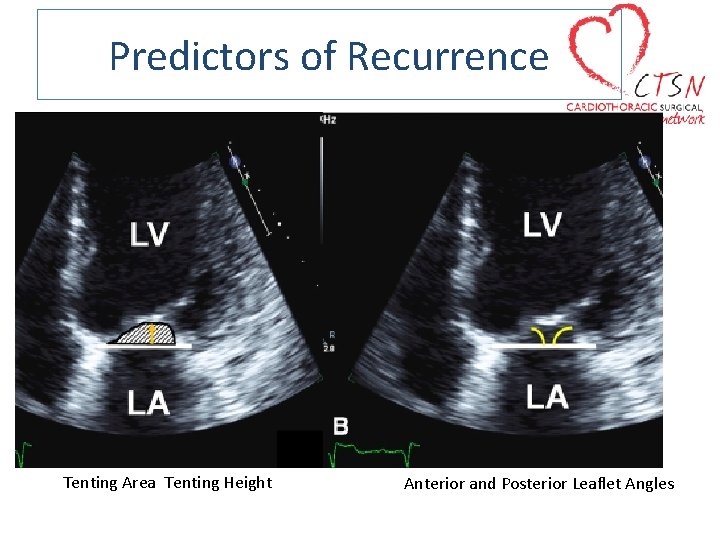
Predictors of Recurrence
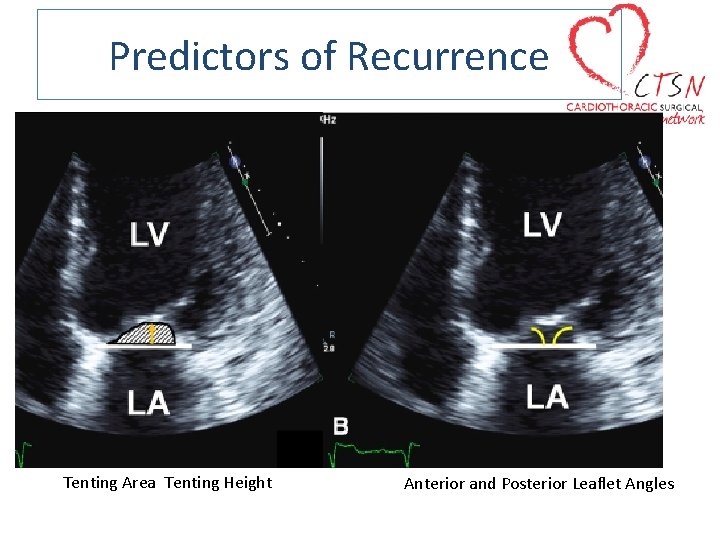
Predictors of Recurrence Tenting Area Tenting Height Anterior and Posterior Leaflet Angles
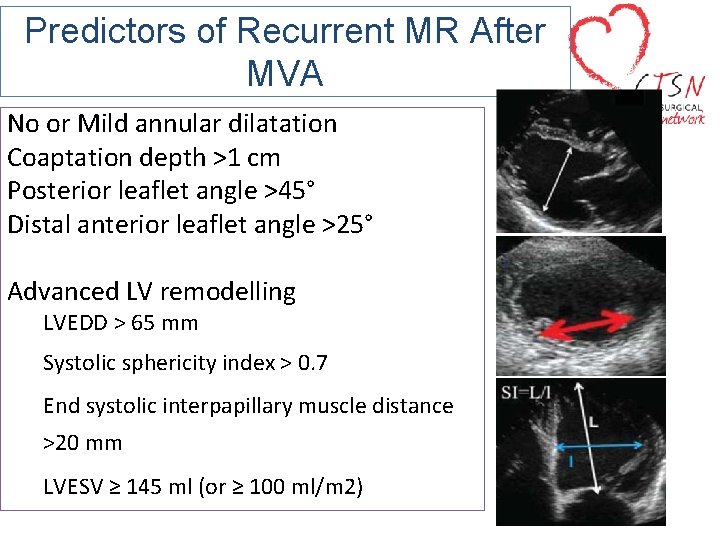
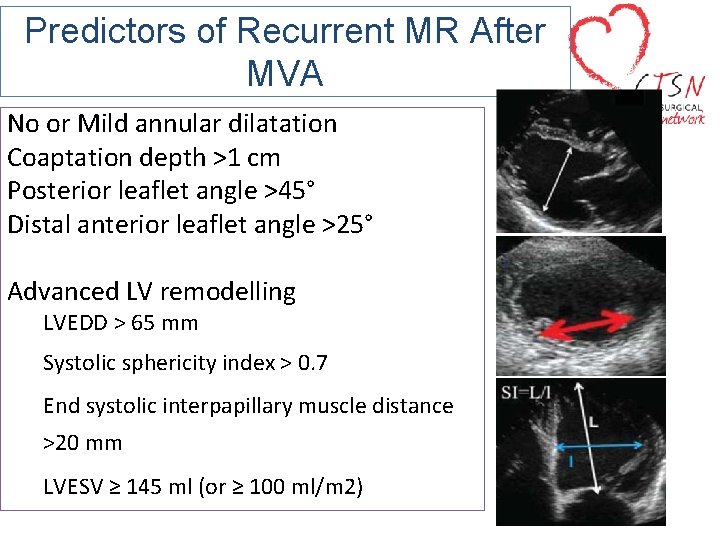
Predictors of Recurrent MR After MVA No or Mild annular dilatation Coaptation depth >1 cm Posterior leaflet angle >45° Distal anterior leaflet angle >25° Advanced LV remodelling LVEDD > 65 mm Systolic sphericity index > 0. 7 End systolic interpapillary muscle distance >20 mm LVESV ≥ 145 ml (or ≥ 100 ml/m 2)
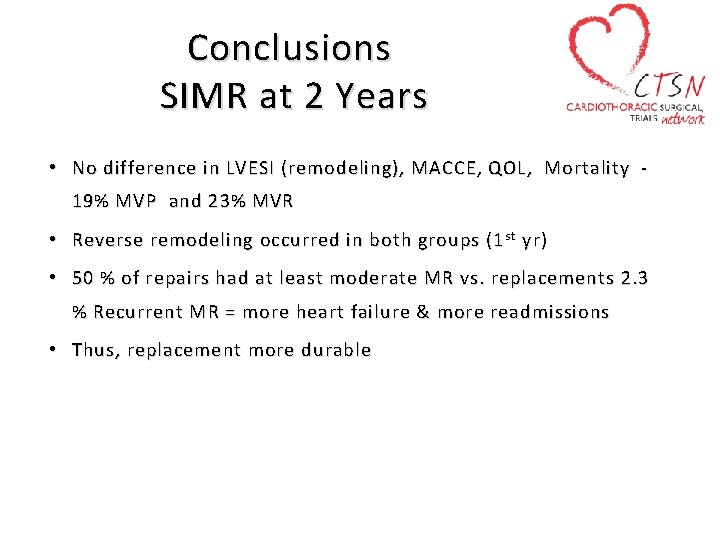
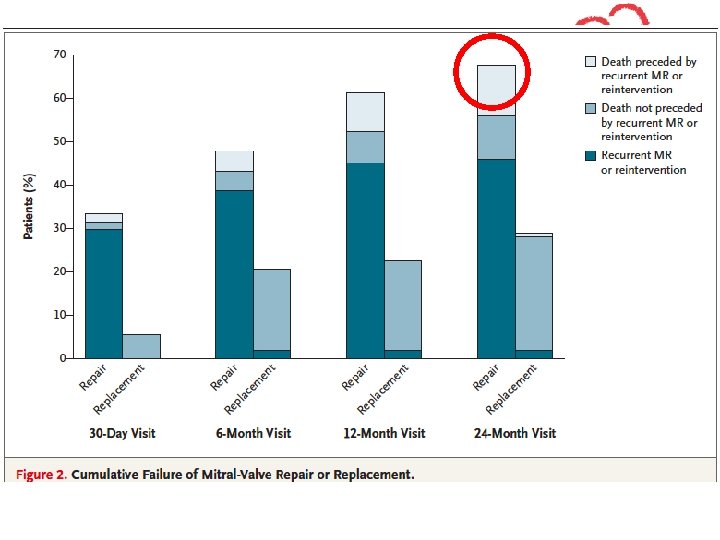
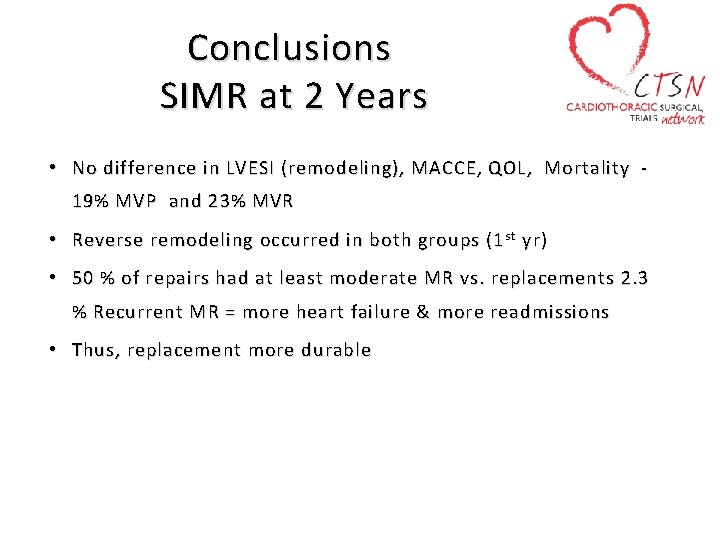
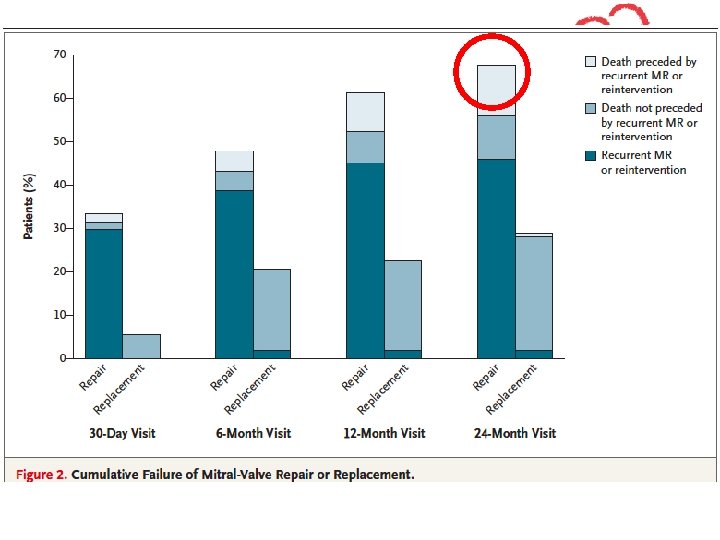
Conclusions SIMR at 2 Years • No difference in LVESI (remodeling), MACCE, QOL, Mortality 19% MVP and 23% MVR • Reverse remodeling occurred in both groups (1 st yr) • 50 % of repairs had at least moderate MR vs. replacements 2. 3 % Recurrent MR = more heart failure & more readmissions • Thus , replacement more durable
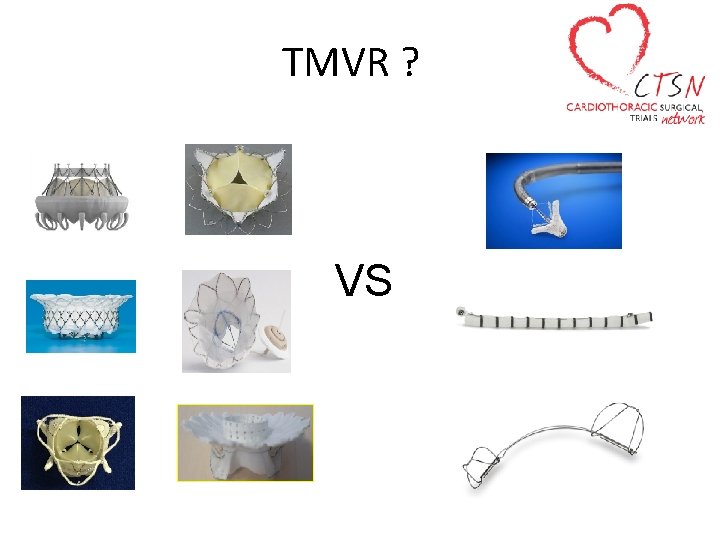
TMVR ? VS
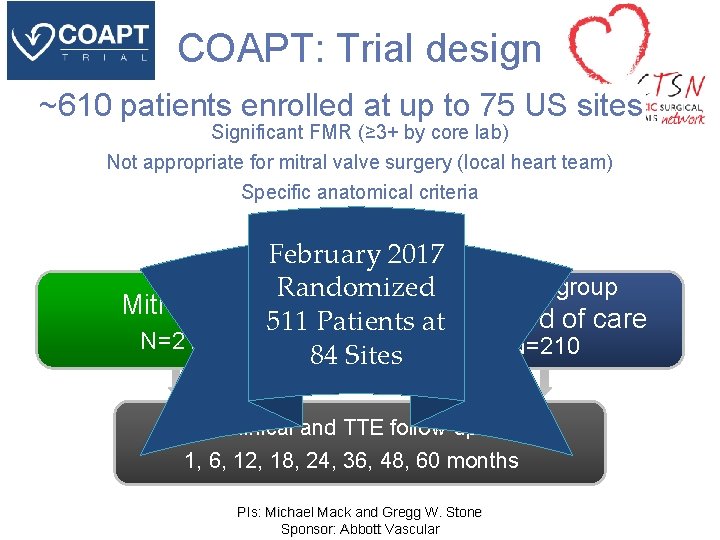
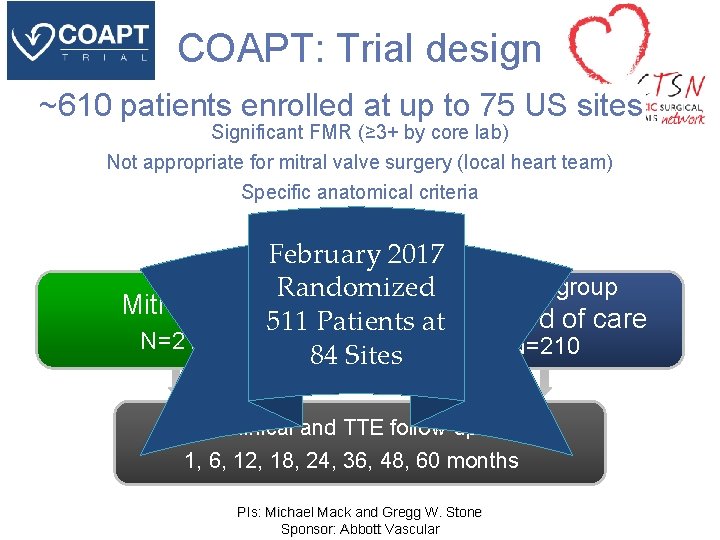
COAPT: Trial design ~610 patients enrolled at up to 75 US sites Significant FMR (≥ 3+ by core lab) Not appropriate for mitral valve surgery (local heart team) Specific anatomical criteria Randomize 1: 1 Mitra. Clip N=210 February 2017 Randomized Control group 511 Patients at. Standard of care N=210 84 Sites Clinical and TTE follow-up: 1, 6, 12, 18, 24, 36, 48, 60 months PIs: Michael Mack and Gregg W. Stone Sponsor: Abbott Vascular
Conclusions • The high incidence of recurrent MR at 2 years portends continued progression of ventricular remodeling. • A “no leak” repair in IMR (thus positive remodeling) should render better results than a replacement. • Expert echo imaging can predict a repair failure and guide surgeons’ selections. • Global dysfunction with apico-lateral displacement of papillary muscles portends a poor repair – due to leaflet tethering
Conclusions • A chord sparing MVR is better than a failed mitral repair • All viable ischemic myocardium must be revascularized • RCT` suggest that MVR no riskier than a MVP in SIMR • Method selection should be based on pathologic anatomy • Probably valid implications for transcatheter techniques • Wait on COAPT trial results to see if fixing the MR really helps survival or QOL (renal denervation? ? ? ).