CTG partogram Done by Areej ALHadidi CTG cardiotocograph
CTG & partogram Done by : Areej AL-Hadidi

CTG cardiotocograph it is sometimes called electronic fetal monitoring (EFM)
• The cardiotocograph (CTG) is a continuous tracing of the fetal heart rate used to assess fetal wellbeing, together with an assessment of uterine activity. • The CTG recording is obtained with the pregnant woman positioned comfortably in a left lateral or semi-recumbent position to avoid compression of the maternal vena cava. • Two external transducers are placed on the mother’s abdomen, each attached with a belt. • One transducer is a pressure-sensitive contraction tocodynometer (stretch gauge) that measures the pressure required to flatten a section of the abdominal wall. This correlates with the internal uterine pressure and indicates if there is any uterine activity (contractions). We put it against the fundus
• The second transducer uses ultrasound and the Doppler effect to detect motion of the fetal heart, and measures the interval between successive beats, thereby allowing a continuous assessment of fetal heart rate. We divide the fetus into 3 thirds and we put it against the nearest 1/3 to the head • Recordings are then made for at least 30 minutes with the output from the CTG machine producing two ‘lines’ traced onto a running piece of paper, one a tracing of fetal heart rate and a second a tracing of uterine activity. • The mother may be given a button to press to record any fetal movements that she has felt. • In addition, the CTG machine may record fetal movements detected via the tocodynometer.

• Fetal cardiac behaviour is regulated through the autonomic nervous system and by vasomotor, chemoceptor and baroreceptor mechanisms. • It depends on sympathetic and parasympathetic interactions • Pathological events, such as fetal hypoxia, modify these signals and hence cardiac response including variation in heart rate patterns, which can be detected and recorded in the CTG • The baseline fetal heart rate falls with advancing gestational age. Why? ? as a result of maturing fetal parasympathetic tone and, prior to term, 160 bpm is taken as the upper limit of normal.
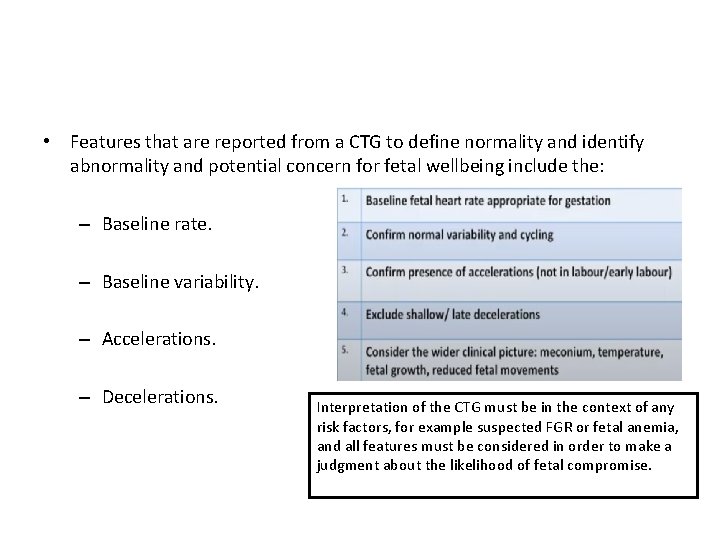
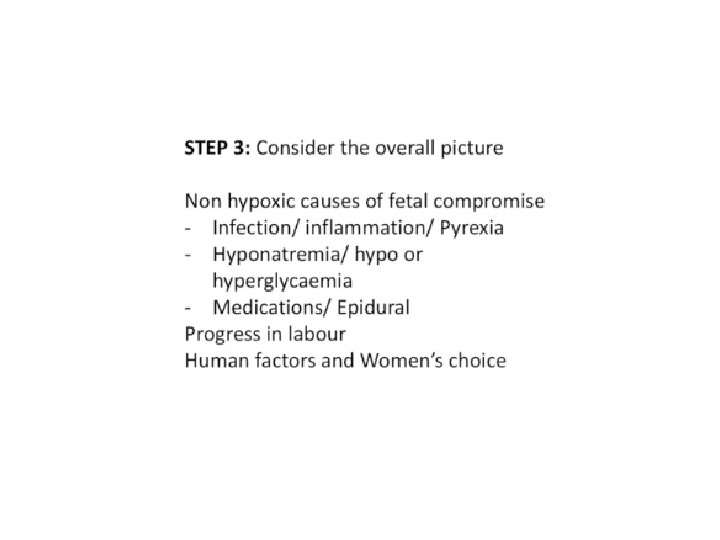
• Features that are reported from a CTG to define normality and identify abnormality and potential concern for fetal wellbeing include the: – Baseline rate. – Baseline variability. – Accelerations. – Decelerations. Interpretation of the CTG must be in the context of any risk factors, for example suspected FGR or fetal anemia, and all features must be considered in order to make a judgment about the likelihood of fetal compromise.
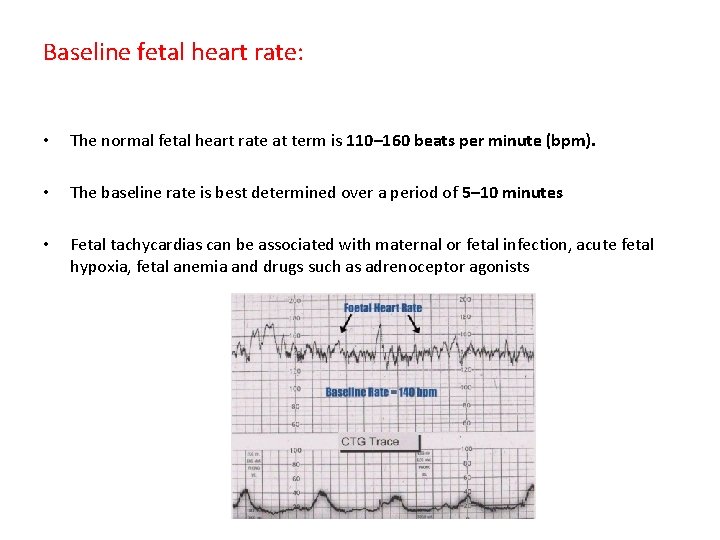
Baseline fetal heart rate: • The normal fetal heart rate at term is 110– 160 beats per minute (bpm). • The baseline rate is best determined over a period of 5– 10 minutes • Fetal tachycardias can be associated with maternal or fetal infection, acute fetal hypoxia, fetal anemia and drugs such as adrenoceptor agonists

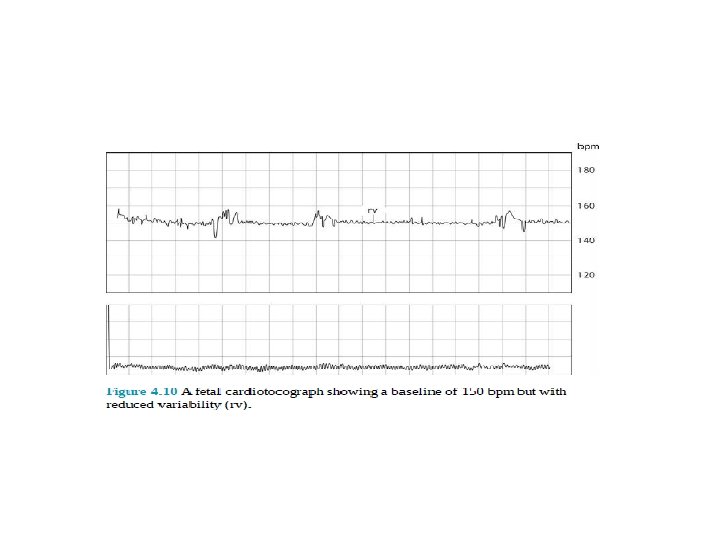
Baseline variability: • fluctuations in heart rate occurring between two and six times per minute. • 5 -15 (may be up to 25) up and down • Normal baseline variability reflects a normal fetal autonomic nervous system. • Abnormality called sinusoidal rhythm / loss of beat to beat variability(when it is less than 10 bpm )
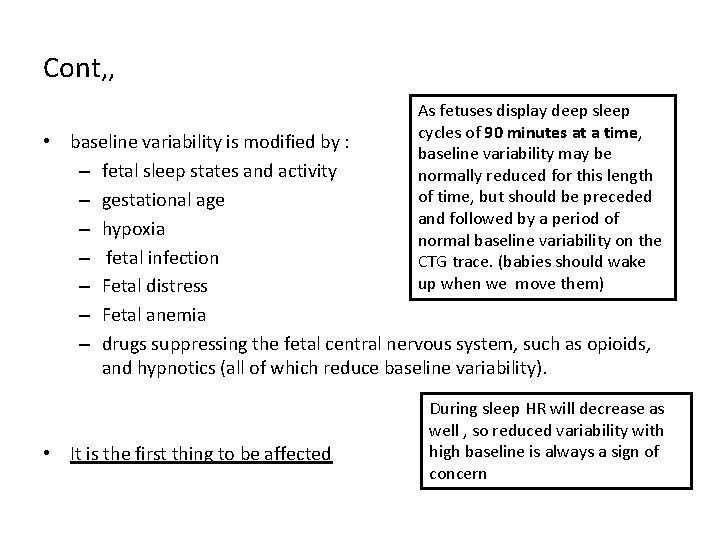
Cont, , As fetuses display deep sleep cycles of 90 minutes at a time, baseline variability may be normally reduced for this length of time, but should be preceded and followed by a period of normal baseline variability on the CTG trace. (babies should wake up when we move them) • baseline variability is modified by : – fetal sleep states and activity – gestational age – hypoxia – fetal infection – Fetal distress – Fetal anemia – drugs suppressing the fetal central nervous system, such as opioids, and hypnotics (all of which reduce baseline variability). • It is the first thing to be affected During sleep HR will decrease as well , so reduced variability with high baseline is always a sign of concern
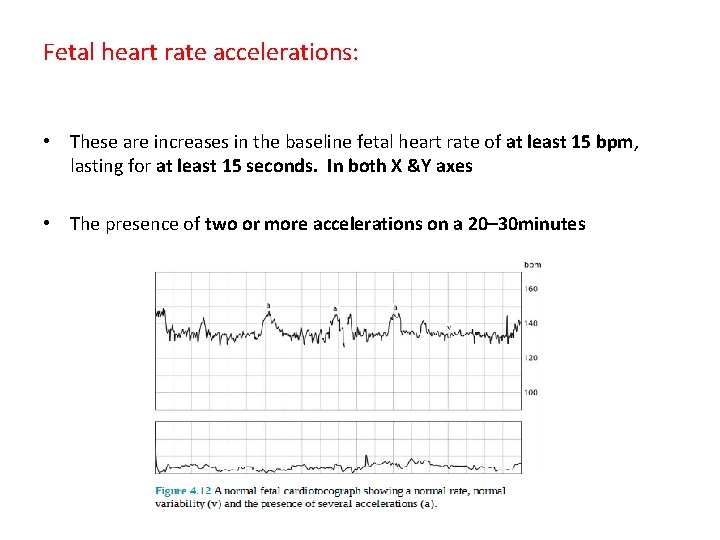
Fetal heart rate accelerations: • These are increases in the baseline fetal heart rate of at least 15 bpm, lasting for at least 15 seconds. In both X &Y axes • The presence of two or more accelerations on a 20– 30 minutes
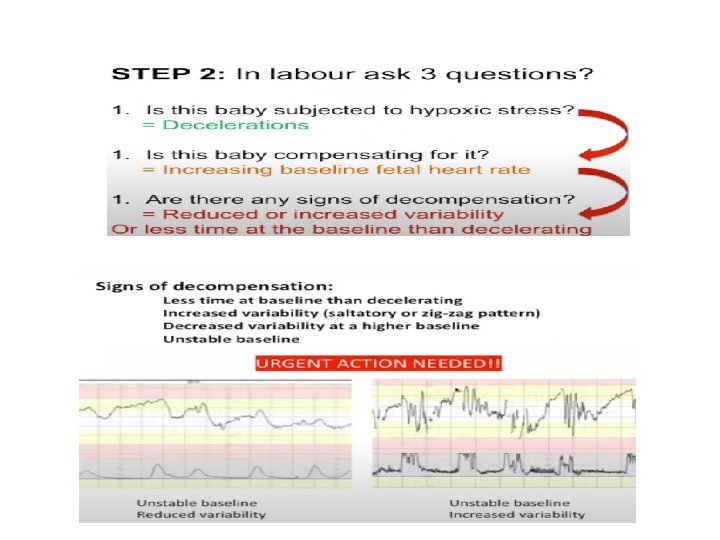
Fetal heart rate decelerations: • These are transient reductions in fetal heart rate of 15 bpm or more, lasting for more than 15 seconds. • Decelerations can be indicative of fetal hypoxia or umbilical cord compression. • There is a higher chance of fetal hypoxia being present if there additional abnormal features such as reduced variability or baseline tachycardia
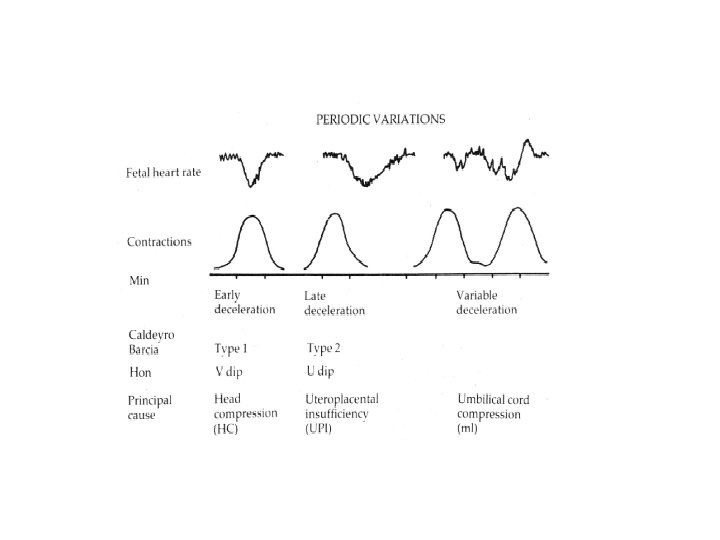
Cont , , • Early / type I / mirror image decelerations – They occur as a result of contractions and head compression – Benign but if persists >60 minutes (reassess) , >90 minutes (no adequate time to recover) – Reassure the mother • delayed/ late/ type II: – fetal distress • variable – Contractions are different in relation , size or duration – Cord compression – Just change the position of the mother
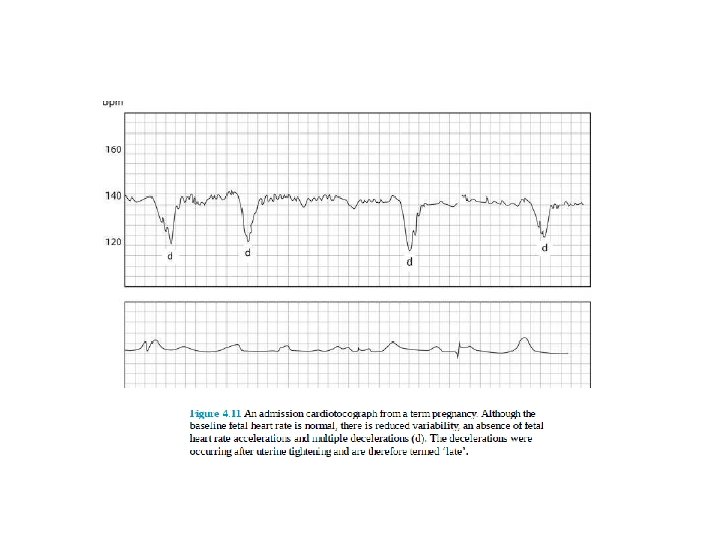
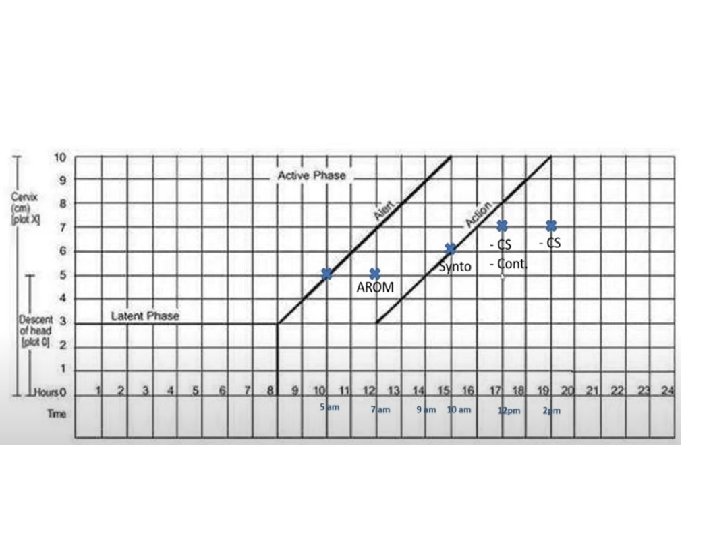
type II management: • Positional changes (left lateral to decrease the IVC compression) • Hydration with IV fluid • Leg elevation to correct maternal hypotension • Administer O 2 at 8 -10 L/min (face mask) • Analgesics • D/C oxytocin if infusing contractions compress blood flow • If persists >30 minutes measure fetal blood p. H – If normal close monitoring – Abnormal delivery • use instruments if the condition allow (forceps not vacuum because it needs time ) • CS if the cervix isn't fully dilated *Conditions in which early delivery or intervention is indicated : Late deceleration Loss of beat to beat variability
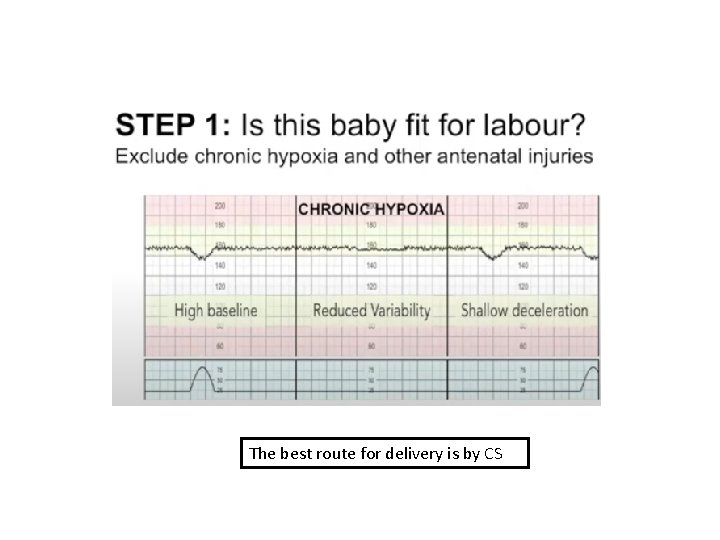
The best route for delivery is by CS
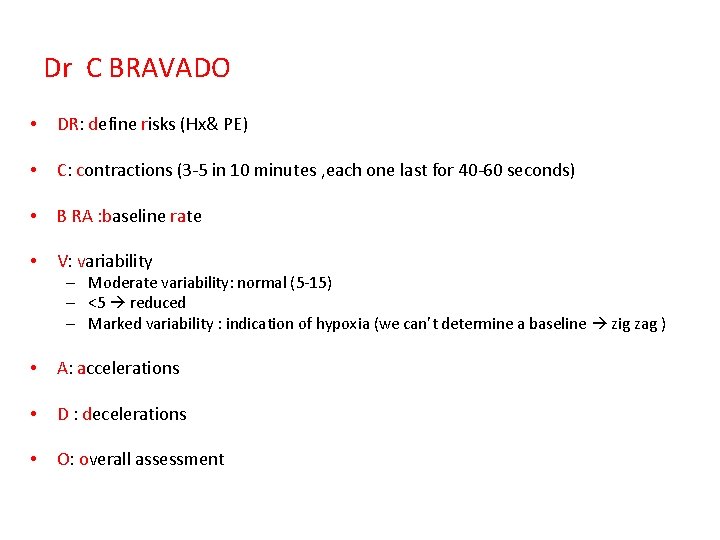
Dr C BRAVADO • DR: define risks (Hx& PE) • C: contractions (3 -5 in 10 minutes , each one last for 40 -60 seconds) • B RA : baseline rate • V: variability – Moderate variability: normal (5 -15) – <5 reduced – Marked variability : indication of hypoxia (we can’t determine a baseline zig zag ) • A: accelerations • D : decelerations • O: overall assessment
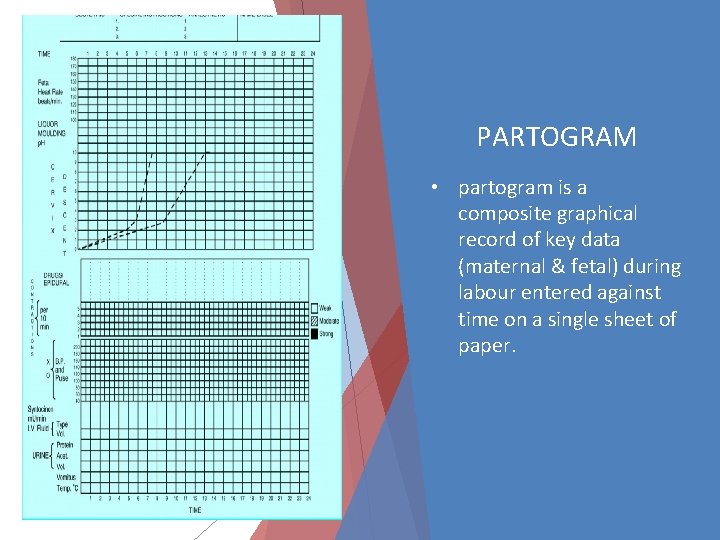
PARTOGRAM • partogram is a composite graphical record of key data (maternal & fetal) during labour entered against time on a single sheet of paper.
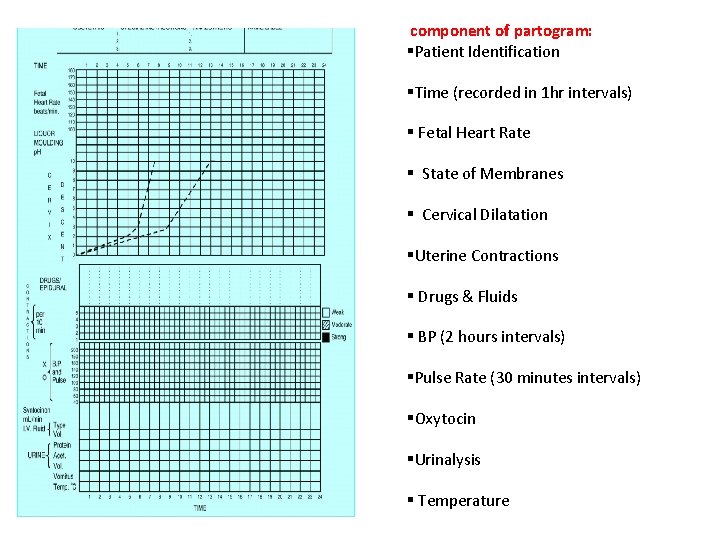
component of partogram: §Patient Identification §Time (recorded in 1 hr intervals) § Fetal Heart Rate § State of Membranes § Cervical Dilatation §Uterine Contractions § Drugs & Fluids § BP (2 hours intervals) §Pulse Rate (30 minutes intervals) §Oxytocin §Urinalysis § Temperature
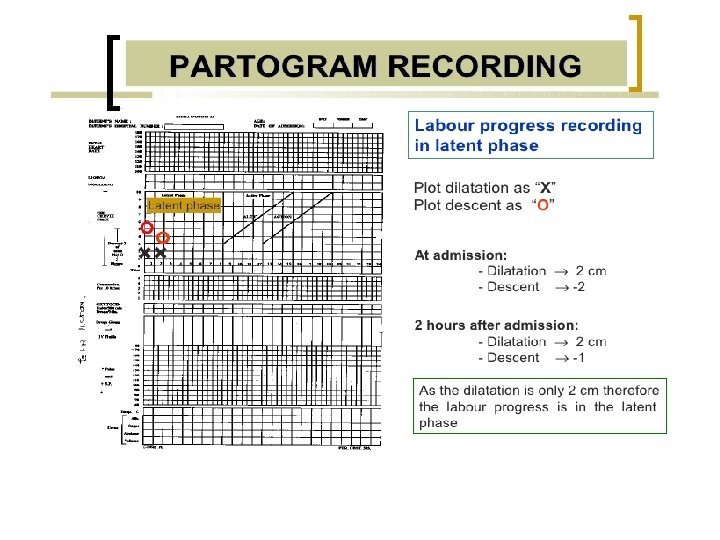

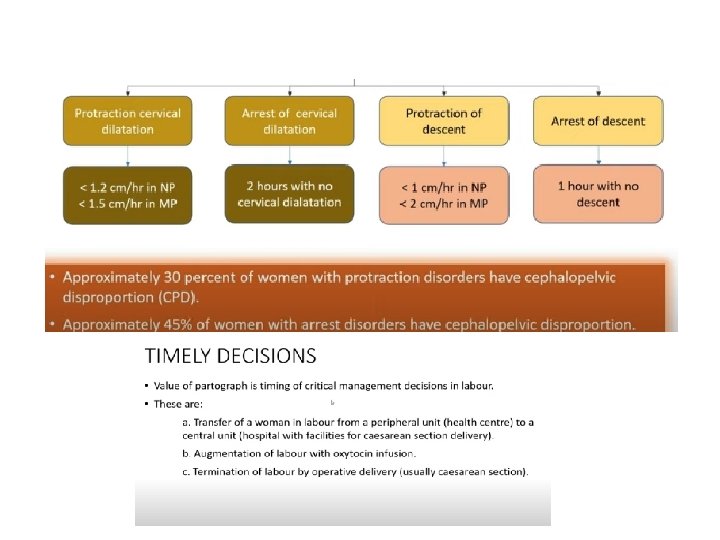
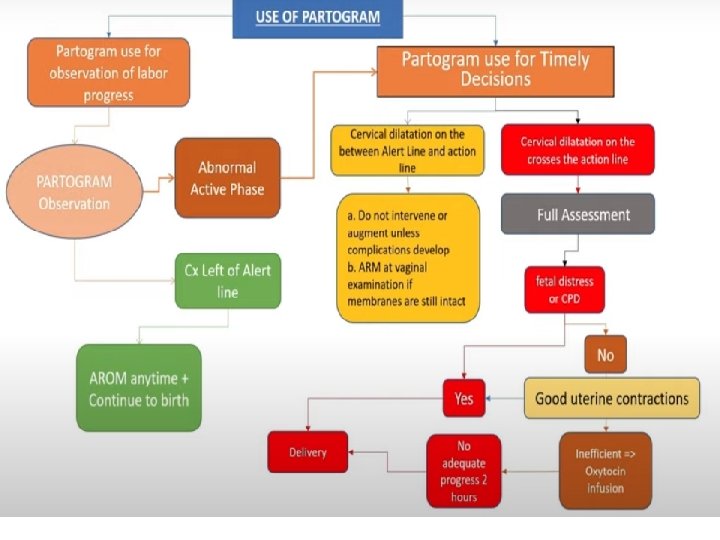
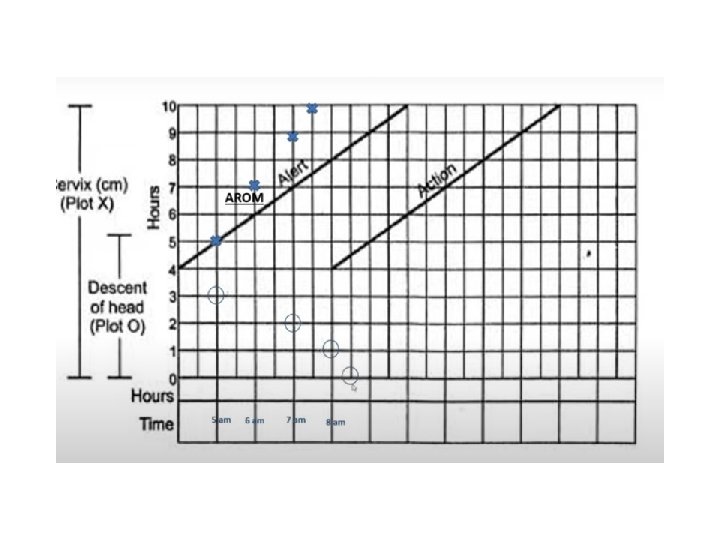
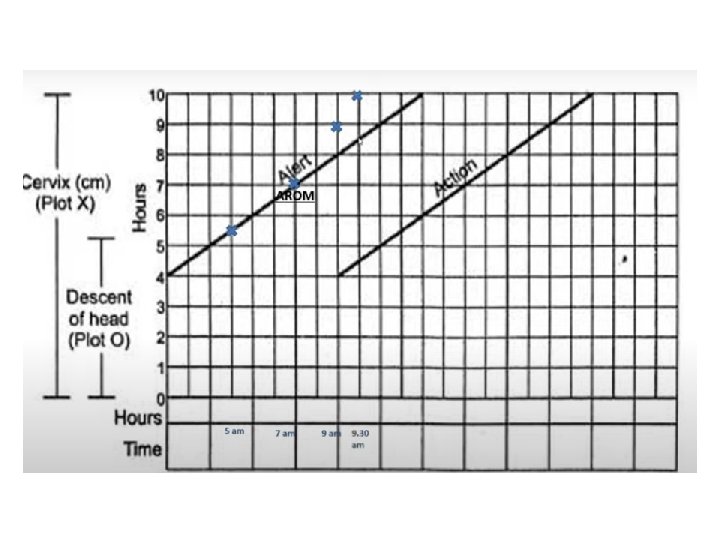
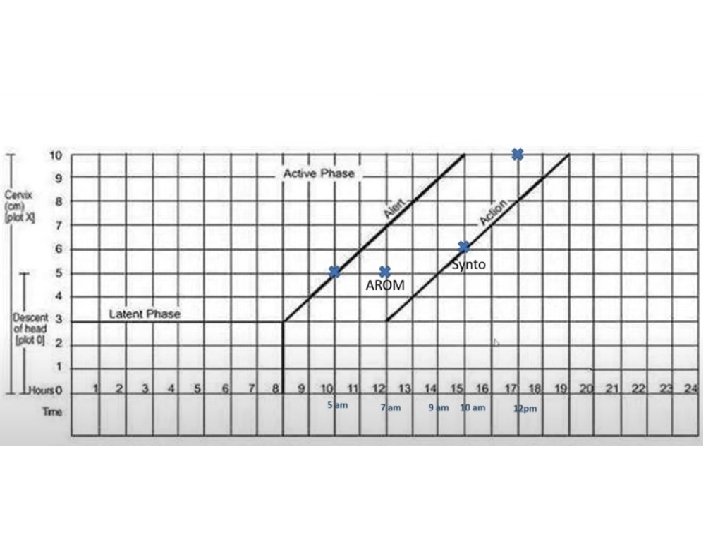
Cont, , • The Alert line starts at 4 cm of cervical dilatation and it travels diagonally upwards to the point of expected full dilatation (10 cm) at the rate of 1 cm per hour. • The action line is located 4 hours to the right of the alert line. • As slope is to the left side of the alert line everything is ok • Cervical dilatation represents the active phase • Descent represents the second stage
• It is used for: 1. record observations 2. plan and adjust management guidelines 3. indicate the appropriate timing of certain interventions can be incorporated • We remove the latent phase in the modified one. Why? ? – Latent phase is difficult to diagnose and assign its start which lead to early admission and intervention – Prolonged latent stage is relatively infrequent and doesn’t usually associated with poor perinatal outcomes
- Slides: 31