CSA Examination Dr Faye Dannhauser Chigwell Medical Centre



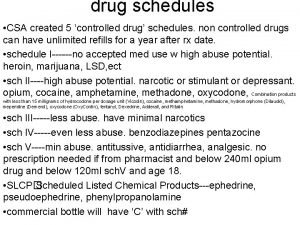
- Slides: 30
CSA Examination Dr Faye Dannhauser - Chigwell Medical Centre.
Format for CSA training session • • Introduction Statistics Marking schedules Group Work Feedback Benchmarking Top Tips
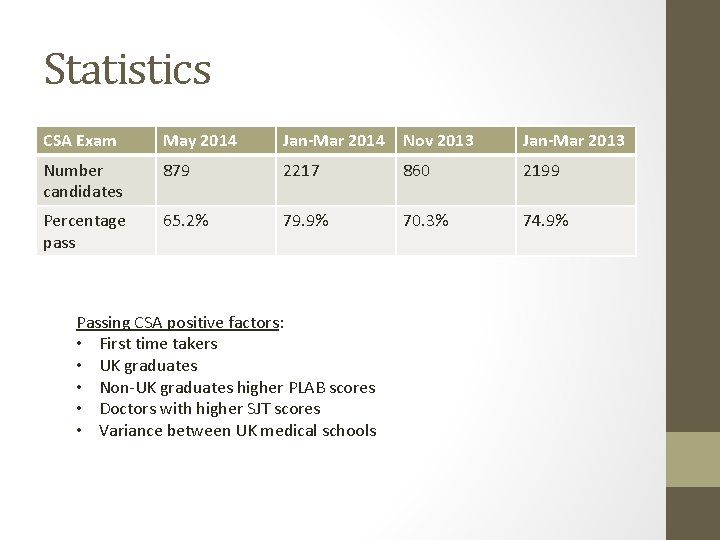
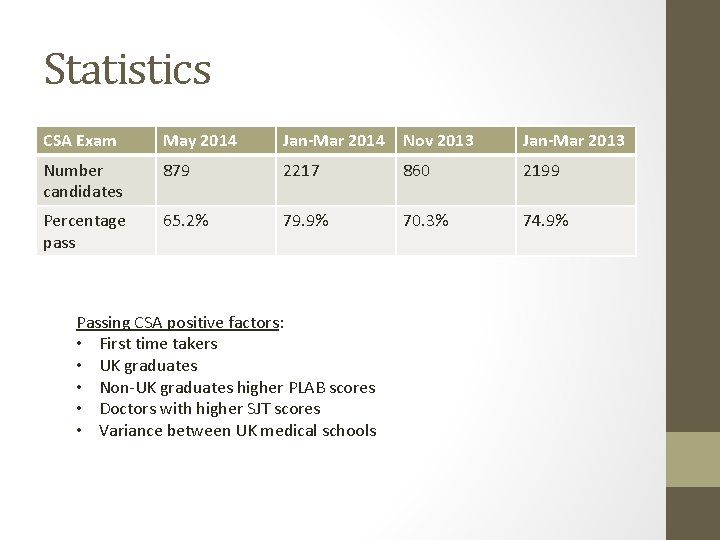
Statistics CSA Exam May 2014 Jan-Mar 2014 Nov 2013 Jan-Mar 2013 Number candidates 879 2217 860 2199 Percentage pass 65. 2% 79. 9% 70. 3% 74. 9% Passing CSA positive factors: • First time takers • UK graduates • Non-UK graduates higher PLAB scores • Doctors with higher SJT scores • Variance between UK medical schools
CSA Exam - logistics • • 13 cases (7 : 6) 10 mins per case Digital clock (counts up to 10 mins) 2 -3 mins between cases Extra visitors Desk equipment Furniture
Equipment to bring • • • BNF (no marking but you can tag pages) BNF for children Stethoscope Opthalmoscope Auroscope Thermometer Patella hammer Tape measure Peak flow meter and disposable mouth pieces (EU standard)
Cases • • • 600 cases Avoid labelling cases according to diagnosis Variable levels of challenge Examination Types: 1. Paediatric 2. Diversity case 3. Acute and chronic 4. Telephone triage or home visit cases
Why do candidates fail? • • No structure Doctor-centred Poor management plans – UK practice / specific to individual Lack of empathy Unable to see the issue or “nub of the case” Poor time keeping Poor examination techniques
Examination in the CSA • • Simple – level expected for a GP Specific – what parts relevant to that presentation Practice a time frame for different systems What is unlikely to be examined? Role players cue “what do you want to examine doctor” Practice verbalising what they are going to examine Prostheses / picture cards Examination findings – verbal and on cards
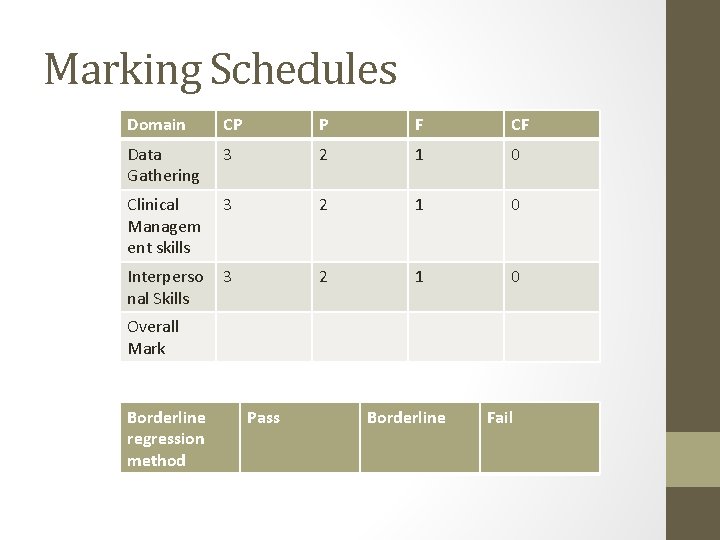
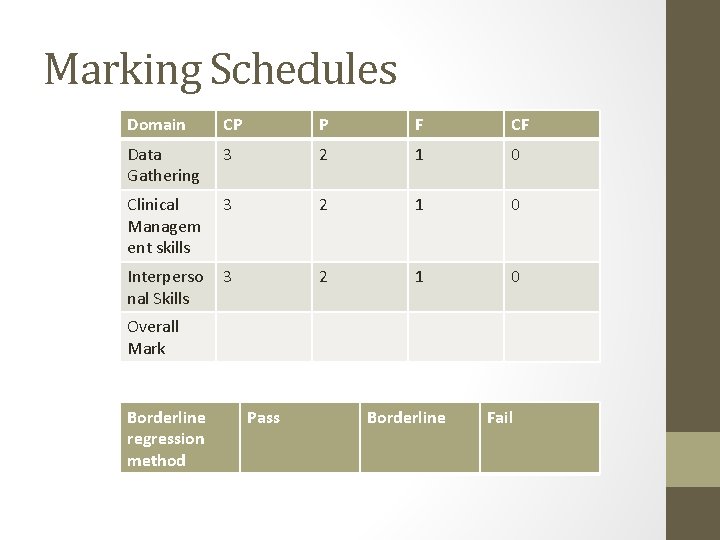
Marking Schedules Domain CP P F CF Data Gathering 3 2 1 0 Clinical Managem ent skills 3 2 1 0 Interperso nal Skills 3 2 1 0 Overall Mark Borderline regression method Pass Borderline Fail
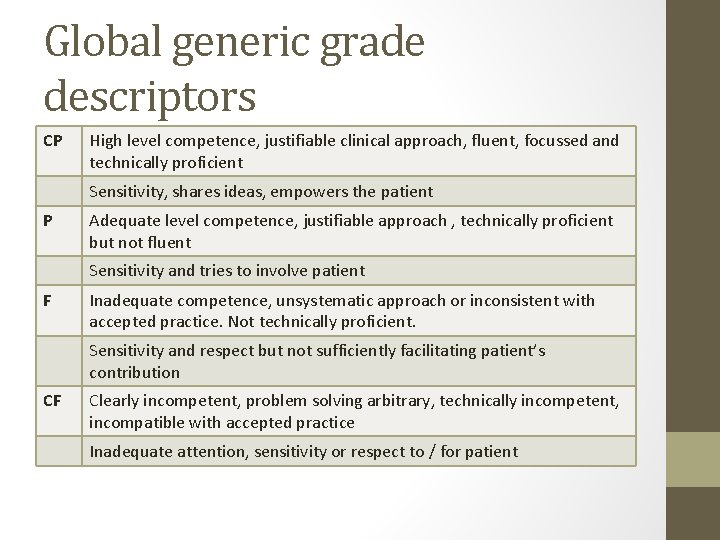
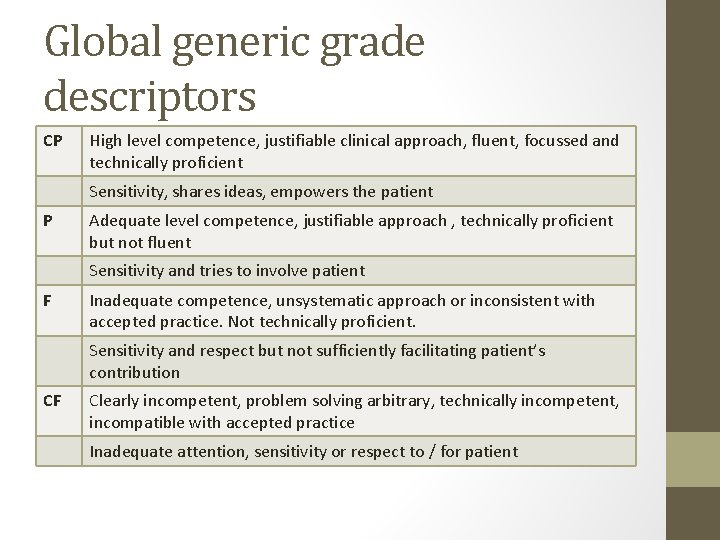
Global generic grade descriptors CP High level competence, justifiable clinical approach, fluent, focussed and technically proficient Sensitivity, shares ideas, empowers the patient P Adequate level competence, justifiable approach , technically proficient but not fluent Sensitivity and tries to involve patient F Inadequate competence, unsystematic approach or inconsistent with accepted practice. Not technically proficient. Sensitivity and respect but not sufficiently facilitating patient’s contribution CF Clearly incompetent, problem solving arbitrary, technically incompetent, incompatible with accepted practice Inadequate attention, sensitivity or respect to / for patient
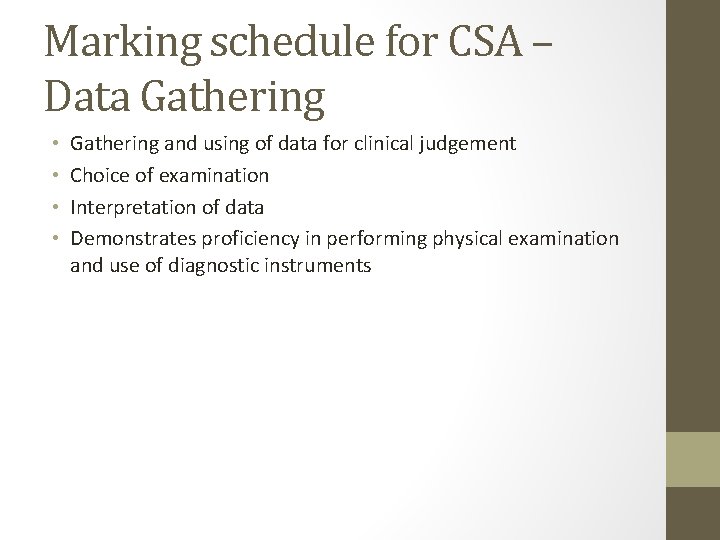
Marking schedule for CSA – Data Gathering • • Gathering and using of data for clinical judgement Choice of examination Interpretation of data Demonstrates proficiency in performing physical examination and use of diagnostic instruments
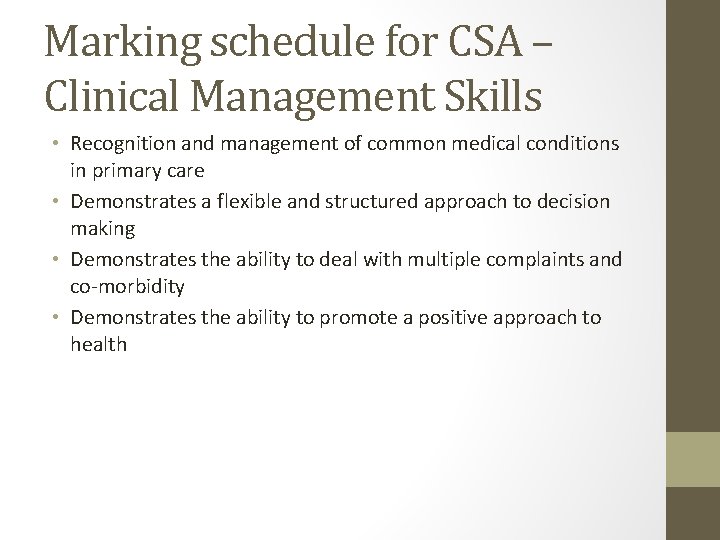
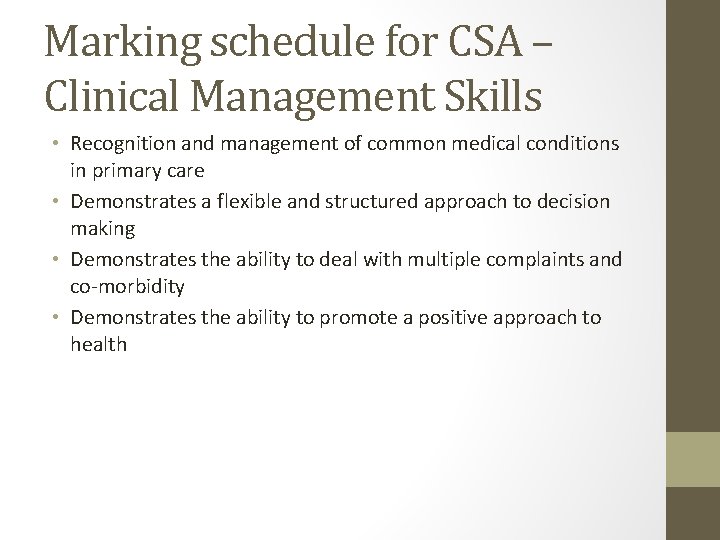
Marking schedule for CSA – Clinical Management Skills • Recognition and management of common medical conditions in primary care • Demonstrates a flexible and structured approach to decision making • Demonstrates the ability to deal with multiple complaints and co-morbidity • Demonstrates the ability to promote a positive approach to health
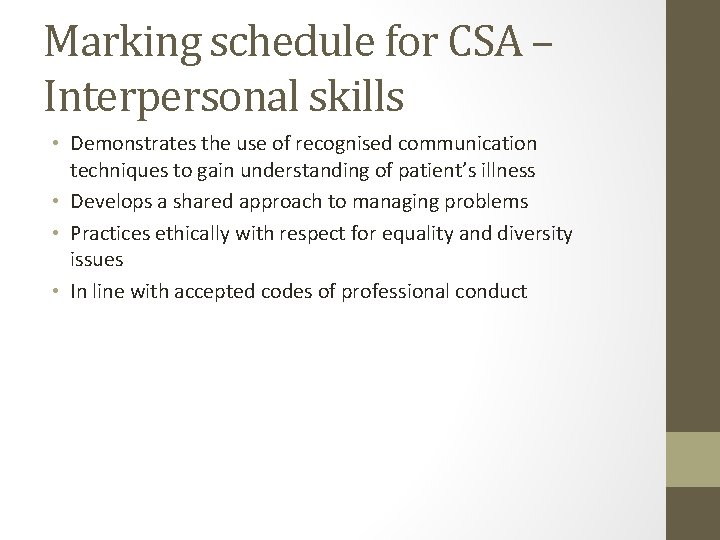
Marking schedule for CSA – Interpersonal skills • Demonstrates the use of recognised communication techniques to gain understanding of patient’s illness • Develops a shared approach to managing problems • Practices ethically with respect for equality and diversity issues • In line with accepted codes of professional conduct
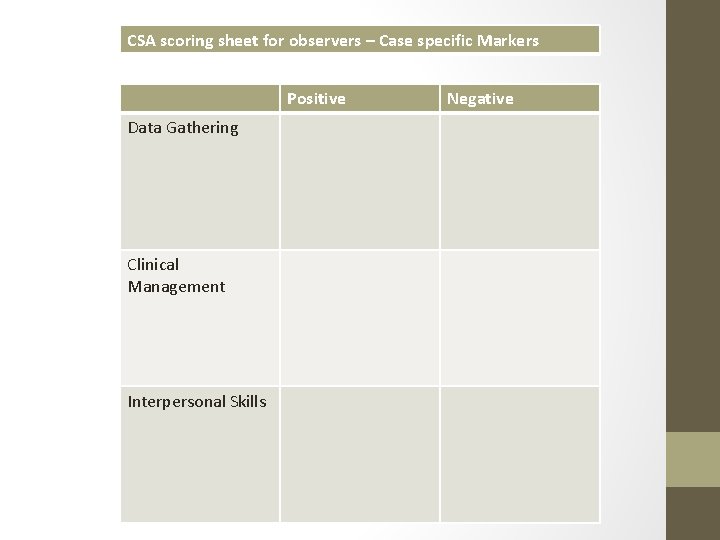
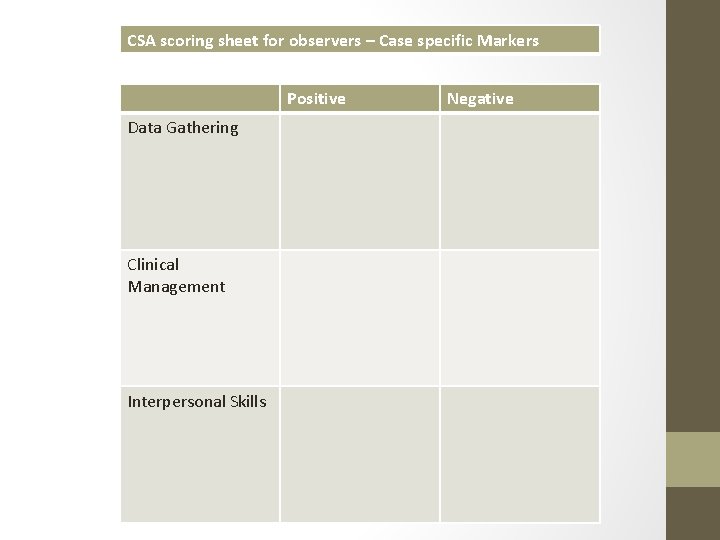
CSA scoring sheet for observers – Case specific Markers Positive Data Gathering Clinical Management Interpersonal Skills Negative
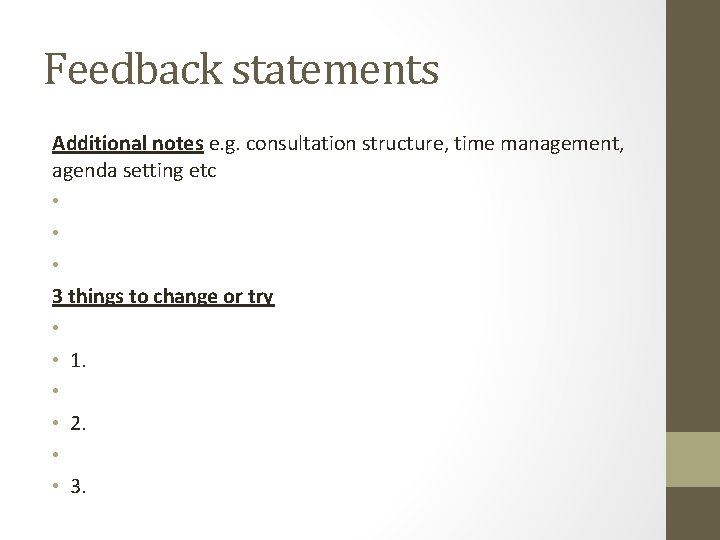
Feedback statements Additional notes e. g. consultation structure, time management, agenda setting etc • • • 3 things to change or try • • 1. • • 2. • • 3.
Dometic Violence case - DG • • Picks up cues Severity of injury Risk assessment Mental health history / symptoms Triggers Examination choice Safeguarding
DV case - CM • • • Correctly identifies high risk patient Supportive measures Safeguarding issues Adequate follow-up Emergency exit strategy
DV case - IPS • • • Respects confidentiality concerns Shows respect Non-judgmental Empowers patient Sensitively deals with safeguarding issue
Atrial fibrillation case - DG • • History relevant to presentation – Palpitations Red flags CVD risk factors Personal or family history of thyroid / CVD considered Psychosocial trigger factors relevant to the case Occupational factors that might be relevant to management Choice of examination Correct interpretation of ECG
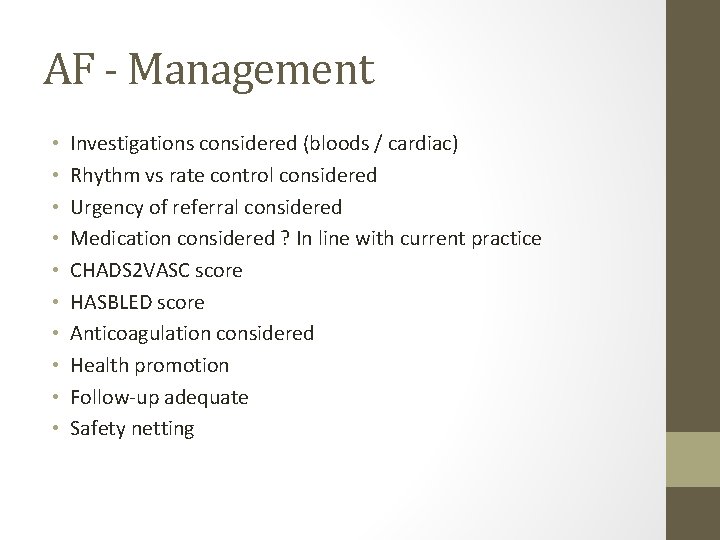
AF - Management • • • Investigations considered (bloods / cardiac) Rhythm vs rate control considered Urgency of referral considered Medication considered ? In line with current practice CHADS 2 VASC score HASBLED score Anticoagulation considered Health promotion Follow-up adequate Safety netting
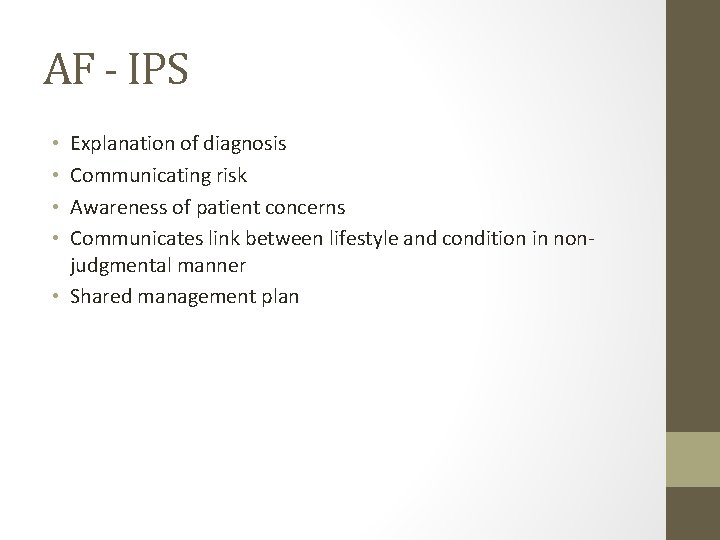
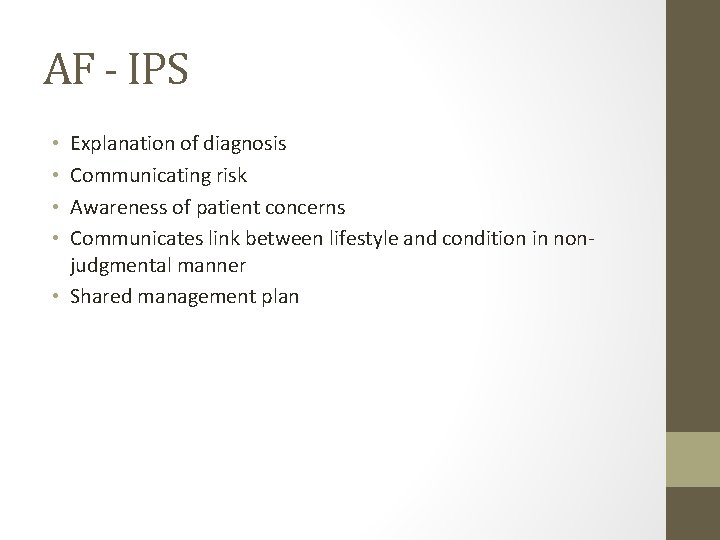
AF - IPS Explanation of diagnosis Communicating risk Awareness of patient concerns Communicates link between lifestyle and condition in nonjudgmental manner • Shared management plan • •

Erectile Dysfunction case - DG
ED case - CM
ED case - IPS
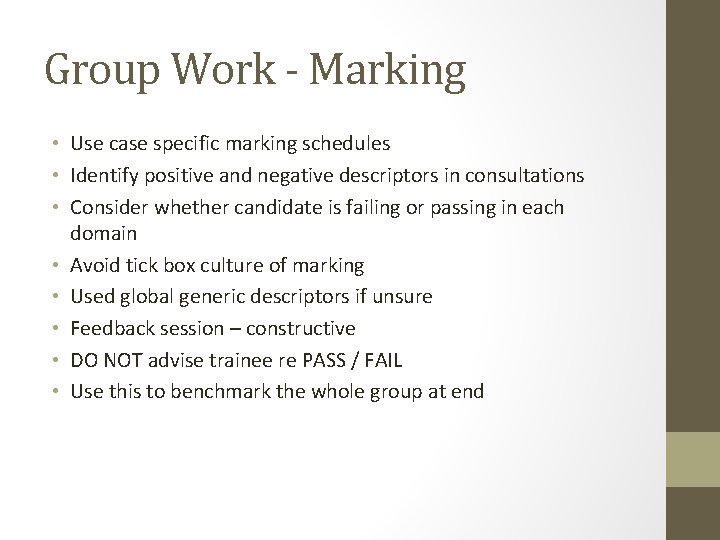
Group Work - Marking • Use case specific marking schedules • Identify positive and negative descriptors in consultations • Consider whether candidate is failing or passing in each domain • Avoid tick box culture of marking • Used global generic descriptors if unsure • Feedback session – constructive • DO NOT advise trainee re PASS / FAIL • Use this to benchmark the whole group at end


Effective Feedback Mary Conroy
How to give effective feedback • Give feedback only when asked to do so or when your offer is accepted. • Give feedback as soon after the event as possible. • Focus on the positive. • Feedback needs to be given privately wherever possible • Feedback needs to be part of the overall communication process and ‘developmental dialogue’. Use skills such as rapport or mirroring, developing respect and trust with the learner. • Stay in the ‘here and now’, don’t bring up old concerns or previous mistakes, unless this is to highlight a pattern of behaviours. • Focus on behaviours that can be changed, not personality traits. • Talk about and describe specific behaviours, giving examples where possible and do not evaluate or assume motives. • Use ‘I’ and give your experience of the behaviour (‘When you said…, I thought that you were…’). (descriptive)
How to give effective feedback • When giving negative feedback, suggest alternative behaviours. • Be sensitive to the impact of your message. • Encourage reflection…. (a) Did it go as planned? If not why not? (b) If you were doing it again what would you do the same next time and what would you do differently? Why? (c) How did you feel during the session? How would you feel about doing it again? (d) How do you think the patient felt? What makes you think that? (e) What did you learn from this session? • Be clear about what you are giving feedback on and link this to the learner’s overall professional development and/or intended programme outcomes. • Do not overload – identify two or three key messages that you summarise
CONSTRUCTIVE CONSIDERATE
 Chigwell medical centre
Chigwell medical centre Medical examination of the crucifixion
Medical examination of the crucifixion Fmek
Fmek Centroid engineering mechanics
Centroid engineering mechanics Gravity center
Gravity center Anette faye jacobsen
Anette faye jacobsen Afirmaciones teoricas de virginia henderson
Afirmaciones teoricas de virginia henderson Faye schulman photos
Faye schulman photos Marie-faye galarneau
Marie-faye galarneau Carmen faye mathes
Carmen faye mathes Faye dimassimo
Faye dimassimo Csa tw75
Csa tw75 Find the lateral area of a cone
Find the lateral area of a cone Csa 2010 login
Csa 2010 login Ap computer science recursion
Ap computer science recursion Csa feuerwehr
Csa feuerwehr Csa
Csa Csa viterbo
Csa viterbo Csa tracking system
Csa tracking system Rds.csa
Rds.csa Como buscar el autor de una imagen
Como buscar el autor de una imagen Schedule csa
Schedule csa Ria ia csa
Ria ia csa Csa notorious nine 2021
Csa notorious nine 2021 Csa vs usa
Csa vs usa Rcgp cot
Rcgp cot Csacash
Csacash Dg csa
Dg csa Csa basic thresholds
Csa basic thresholds C.s.a of cube
C.s.a of cube Contractor sourcing application
Contractor sourcing application