Cryptococcosis Pathogenesis and immune response Dr Tihana Bicanic
Cryptococcosis: Pathogenesis and immune response Dr. Tihana Bicanic Reader and Consultant in Infectious Diseases Centre for Global Health, Institute of Infection and Immunity, St. George’s, University of London; St George's Hospital NHS Foundation Trust
Intended learning outcomes To understand the pathogenesis of cryptococcal meningitis To be aware of the host immune response to Cryptococcus
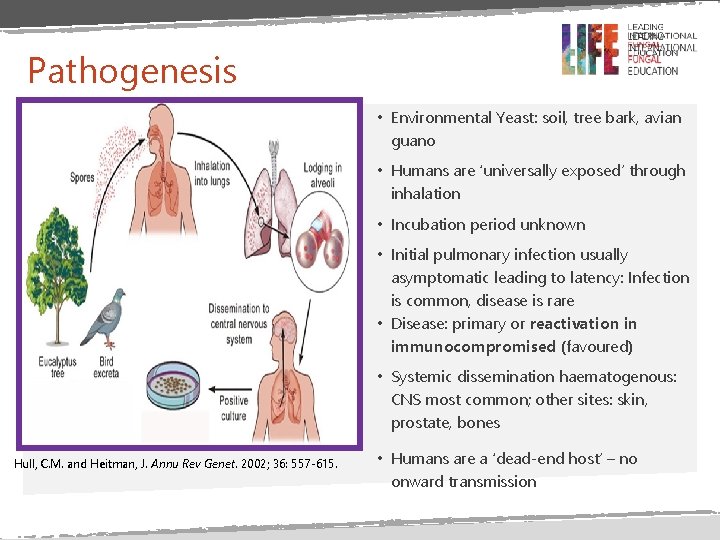
Pathogenesis • Environmental Yeast: soil, tree bark, avian guano • Humans are ‘universally exposed’ through inhalation • Incubation period unknown • Initial pulmonary infection usually asymptomatic leading to latency: Infection is common, disease is rare • Disease: primary or reactivation in immunocompromised (favoured) • Systemic dissemination haematogenous: CNS most common; other sites: skin, prostate, bones Hull, C. M. and Heitman, J. Annu Rev Genet. 2002; 36: 557 -615. • Humans are a ‘dead-end host’ – no onward transmission

Immune response and pathology Involves both innate and adaptive immunity • (Alveolar) macrophage main effector cell • Cryptococcus phagocytosed following opsonisation (Ab and complement) • T helper cells (CD 4+ T cells) activate: secrete Th 1 cytokines including IFN-γ • Granulomatous response (similar to TB) § Good=cryptococcoma (intracellular) § Bad (HIV+ CD 4<100)=disseminated (extracellular) infection • Cryptococci can survive, replicate within and be transmitted between macrophages- macrophages may be vehicle of dissemination to CNS

Summary • Cryptococcus is an environmental fungus to which we are all exposed via inhalation • Both the innate and adaptive arms of the immune system play a role in containing Cryptococcus. • Systemic dissemination occurs in patients who are immunocompromised. • CNS is the most frequent site for dissemination.

END
- Slides: 6