Crush Injuries and Rhabdomyolysis Dr M Mortazavi Nephrologist

Crush Injuries and Rhabdomyolysis Dr. M. Mortazavi Nephrologist

INTRODUCTION • Rhabdomyolysis is a syndrome characterized by muscle necrosis and the release of intracellular muscle constituents into the circulation. • The severity of illness ranges from asymptomatic elevations in serum muscle enzymes to life-threatening cases associated with extreme enzyme elevations, electrolyte imbalances, and acute renal failure
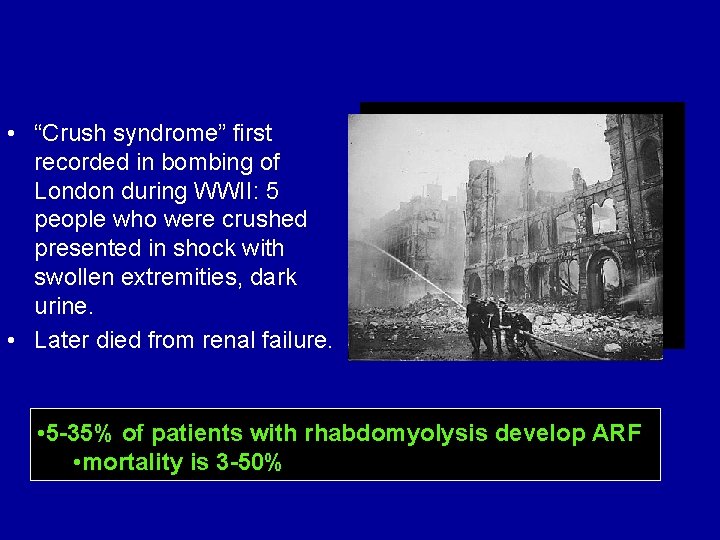
• “Crush syndrome” first recorded in bombing of London during WWII: 5 people who were crushed presented in shock with swollen extremities, dark urine. • Later died from renal failure. • 5 -35% of patients with rhabdomyolysis develop ARF • mortality is 3 -50%
Cause of Rhabdomyolysis • • Traumatic muscle injury Drugs and toxins Infections Genetic disorders Excessive muscle activity Ischemia Electrolyte and endocrine Immunologic disease
Pathophysiology of Rhabdomyolysis
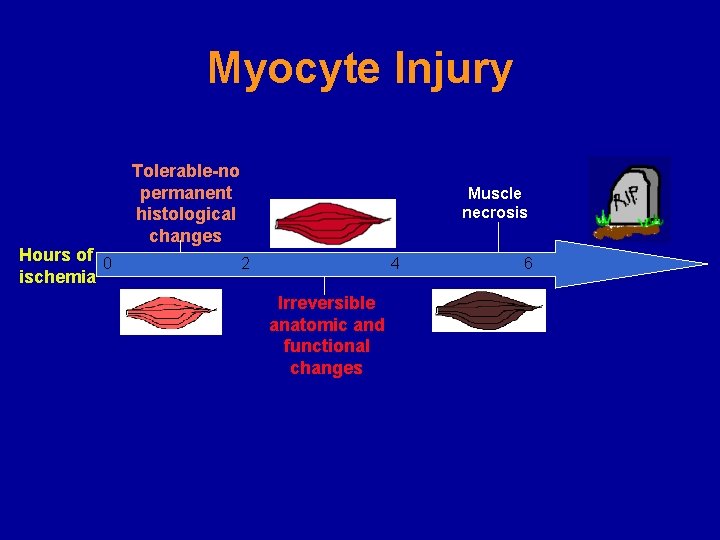
Myocyte Injury Tolerable-no permanent histological changes Muscle necrosis Hours of 0 2 4 6 ischemia Irreversible anatomic and functional changes
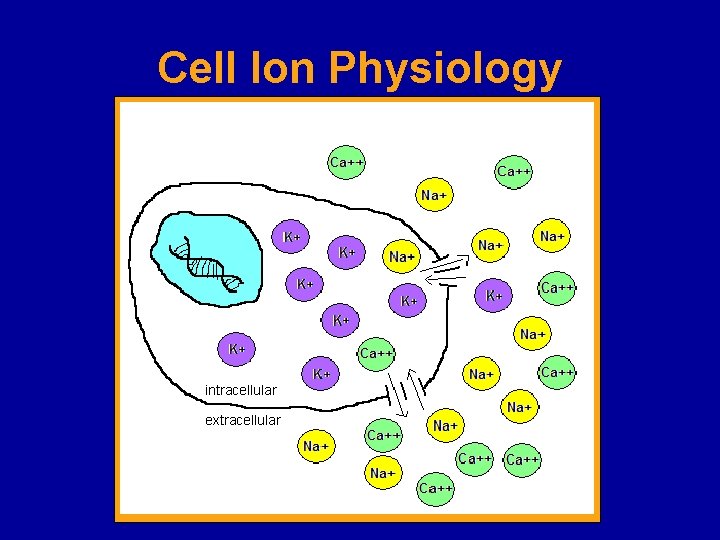
Cell Ion Physiology intracellular extracellular
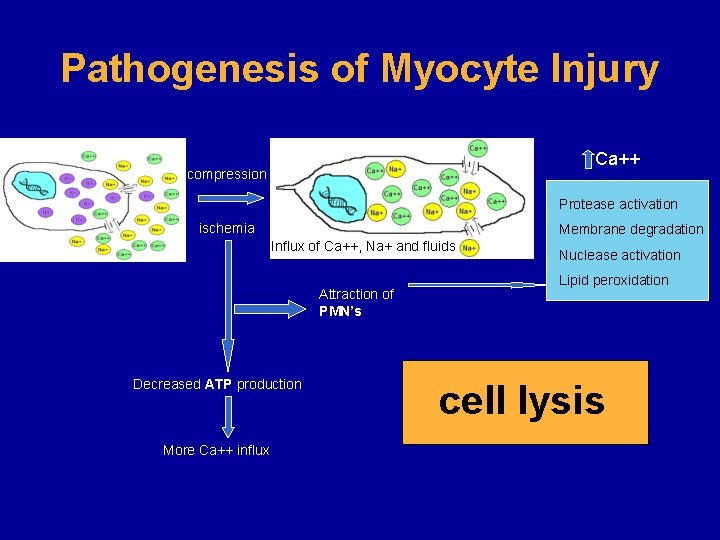
Pathogenesis of Myocyte Injury Ca++ compression Protease activation ischemia Membrane degradation Influx of Ca++, Na+ and fluids Attraction of PMN’s Decreased ATP production More Ca++ influx Nuclease activation Lipid peroxidation cell lysis
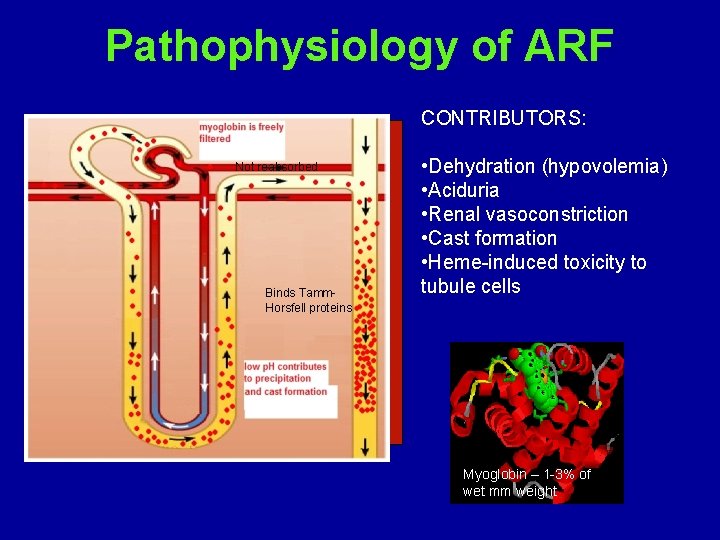
Pathophysiology of ARF CONTRIBUTORS: Not reabsorbed Binds Tamm. Horsfell proteins • Dehydration (hypovolemia) • Aciduria • Renal vasoconstriction • Cast formation • Heme-induced toxicity to tubule cells Myoglobin – 1 -3% of wet mm weight
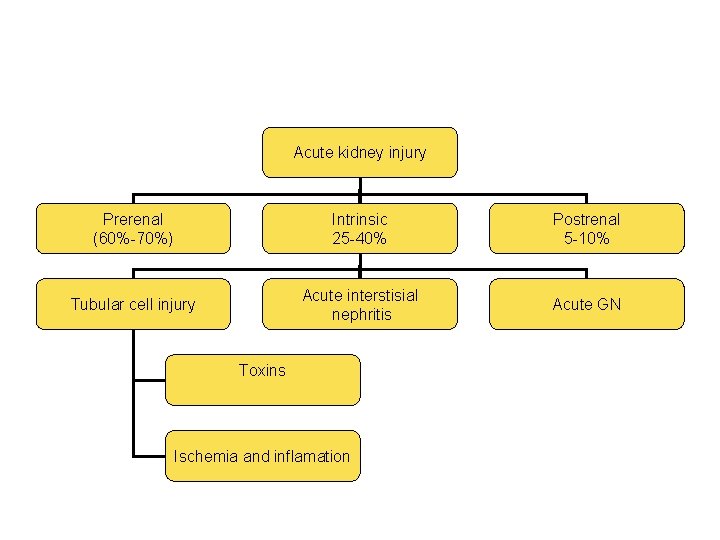
Acute kidney injury Prerenal (60%-70%) Intrinsic 25 -40% Postrenal 5 -10% Acute interstisial nephritis Acute GN Tubular cell injury Toxins Ischemia and inflamation
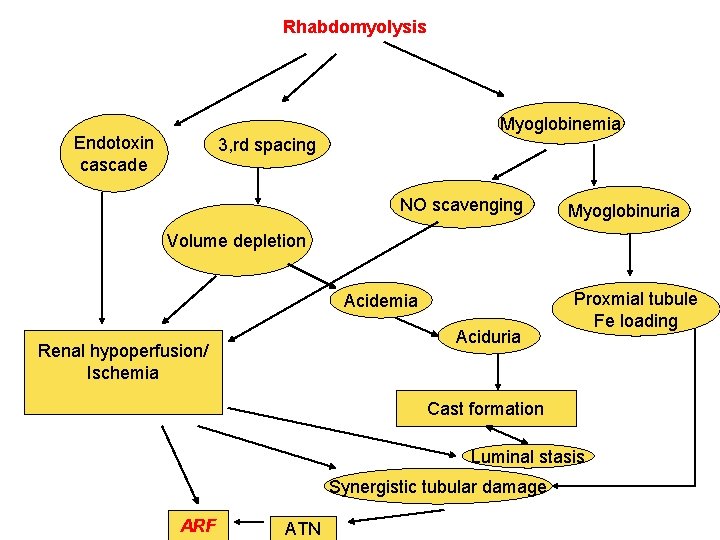
Rhabdomyolysis Myoglobinemia Endotoxin cascade 3, rd spacing NO scavenging Myoglobinuria Volume depletion Acidemia Aciduria Renal hypoperfusion/ Ischemia Proxmial tubule Fe loading Cast formation Luminal stasis Synergistic tubular damage ARF ATN

Diagnosis
CLINICAL MANIFESTATIONS AND DIAGNOSIS • The classic presentation of rhabdomyolysis includes myalgias, red to brown urine due to myoglobinuria, and elevated serum muscle enzymes (including creatine kinase)
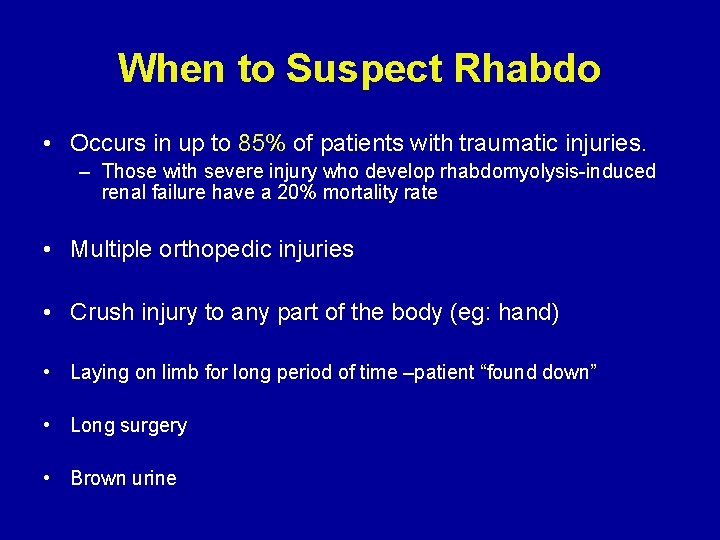
When to Suspect Rhabdo • Occurs in up to 85% of patients with traumatic injuries. – Those with severe injury who develop rhabdomyolysis-induced renal failure have a 20% mortality rate • Multiple orthopedic injuries • Crush injury to any part of the body (eg: hand) • Laying on limb for long period of time –patient “found down” • Long surgery • Brown urine
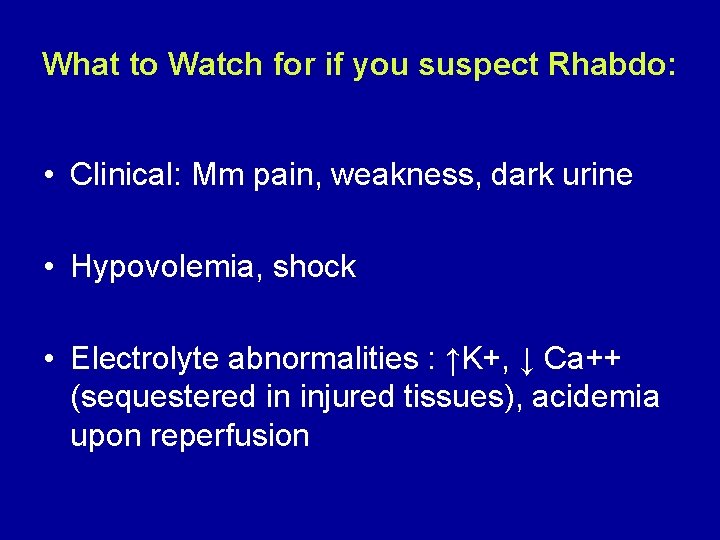
What to Watch for if you suspect Rhabdo: • Clinical: Mm pain, weakness, dark urine • Hypovolemia, shock • Electrolyte abnormalities : ↑K+, ↓ Ca++ (sequestered in injured tissues), acidemia upon reperfusion
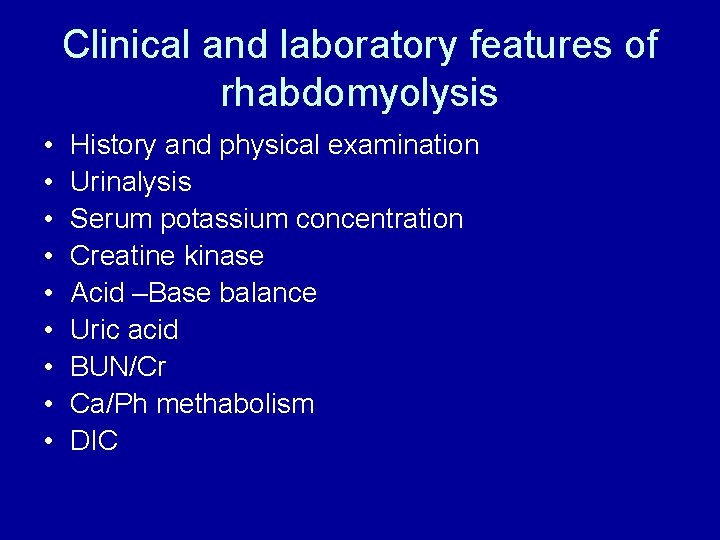
Clinical and laboratory features of rhabdomyolysis • • • History and physical examination Urinalysis Serum potassium concentration Creatine kinase Acid –Base balance Uric acid BUN/Cr Ca/Ph methabolism DIC
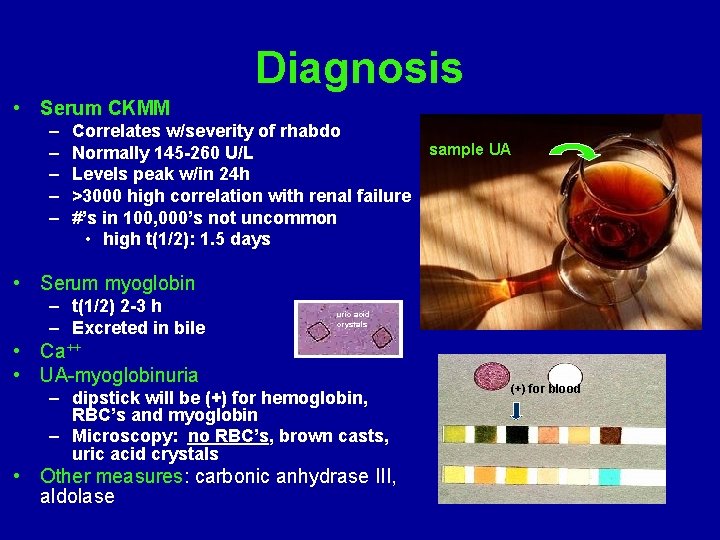
Diagnosis • Serum CKMM – – – Correlates w/severity of rhabdo Normally 145 -260 U/L Levels peak w/in 24 h >3000 high correlation with renal failure #’s in 100, 000’s not uncommon • high t(1/2): 1. 5 days sample UA • Serum myoglobin – t(1/2) 2 -3 h – Excreted in bile uric acid crystals • Ca++ • UA-myoglobinuria – dipstick will be (+) for hemoglobin, RBC’s and myoglobin – Microscopy: no RBC’s, brown casts, uric acid crystals • Other measures: carbonic anhydrase III, aldolase (+) for blood
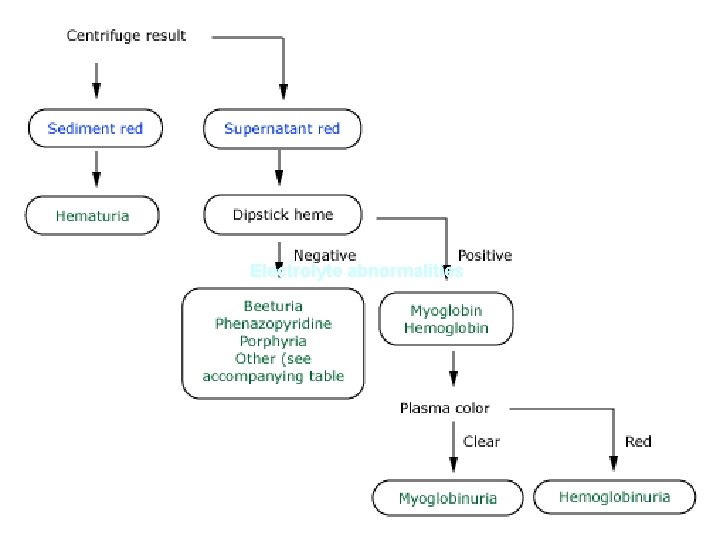
Approach to the patient with red or brown urine Electrolyte abnormalities
Muscle enzymes • The hallmark of rhabdomyolysis is an elevation in serum muscle enzymes. Serum CK levels may be massively elevated to above 100, 000 IU/L. • Elevations in serum aminotransferases are common and can cause confusion if attributed to liver disease.
Electrolyte abnormalities


Prevention and Treatment
MANAGEMENT • Plasma volume expansion with intravenous isotonic saline should be given as soon as possible, even while trying to establish the cause of the rhabdomyolysis. • Treatment of the underlying cause of the rhabdomyolysis.
• Monitoring with serial measurements of serum potassium, calcium, phosphate, and creatinine , CPK is recommended.
MANAGEMENT • The metabolic consequences of and renal functional impairment due to rhabdomyolysis should be anticipated, particularly potentially life-threatening hyperkalemia. • Hypocalcemia? Should be treated?
Early Treatment • FLUIDS – Begin early, even on the field • Damaged muscles attract a lot of fluid – Up to 10 L/day • Ideally NS with bicarb – prevents tubular precipitation – reduces risk of hyperkalemia from damaged mm – corrects academia • mannitol – renal vasodilator – free radical scavenger
Late Treatment • Dialysis – – intermitted preferred to continuous • Reduce use of anticoagulants in trauma patients

- Slides: 29