Crohns Disease aka regional enteritis Overview of Presentation




- Slides: 23
Crohn’s Disease aka regional enteritis
Overview of Presentation General historical background information Description of the condition Management of the Disease Nutrition’s role in stabilizing the condition Conclusion Ethical dilemmas (M. D. vs Nutritional) Opinion for managing the disease What the audience should know
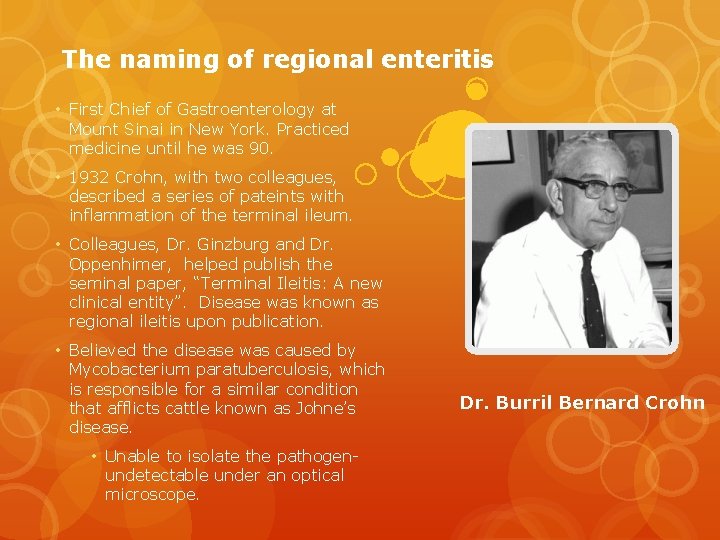
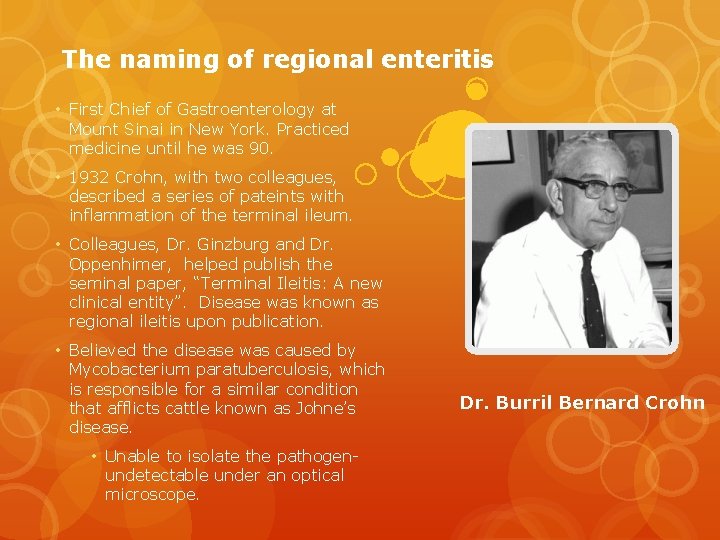
The naming of regional enteritis • First Chief of Gastroenterology at Mount Sinai in New York. Practiced medicine until he was 90. • 1932 Crohn, with two colleagues, described a series of pateints with inflammation of the terminal ileum. • Colleagues, Dr. Ginzburg and Dr. Oppenhimer, helped publish the seminal paper, “Terminal Ileitis: A new clinical entity”. Disease was known as regional ileitis upon publication. • Believed the disease was caused by Mycobacterium paratuberculosis, which is responsible for a similar condition that afflicts cattle known as Johne’s disease. • Unable to isolate the pathogenundetectable under an optical microscope. Dr. Burril Bernard Crohn
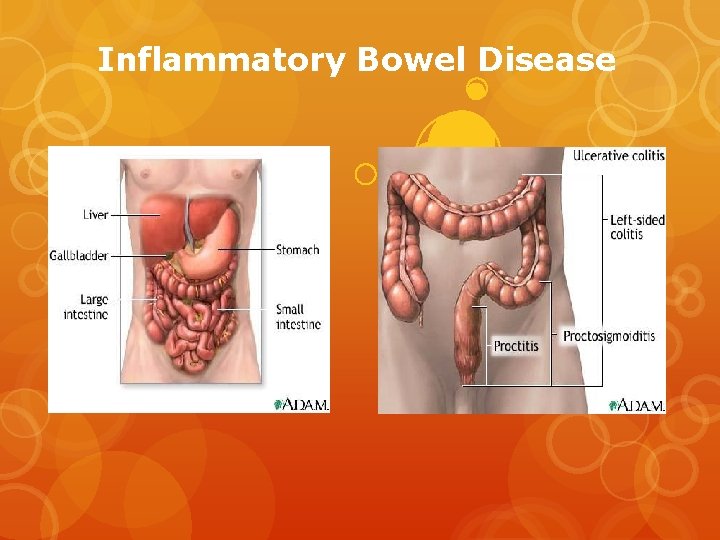
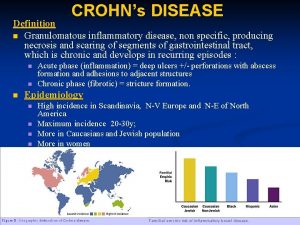
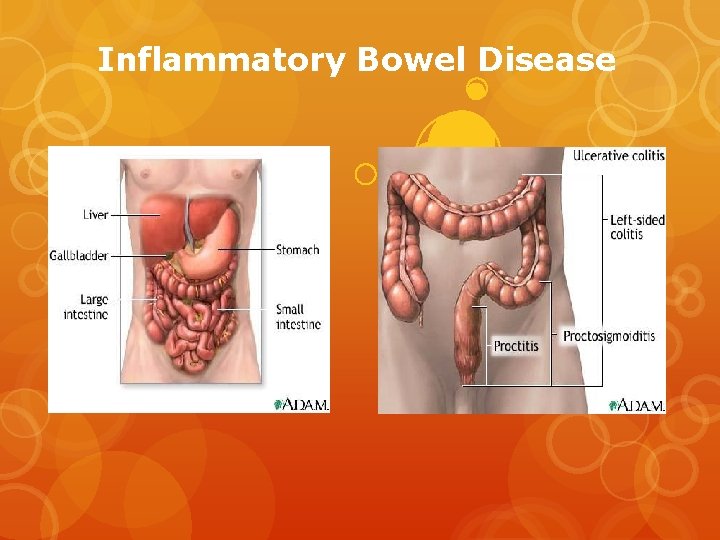
Inflammatory Bowel Disease

Behavioral Classification • Stricturing • Penetrating • Inflammatory
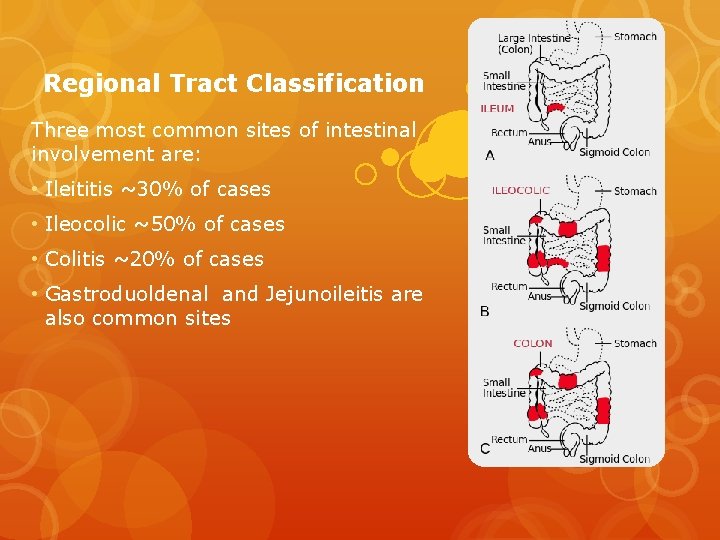
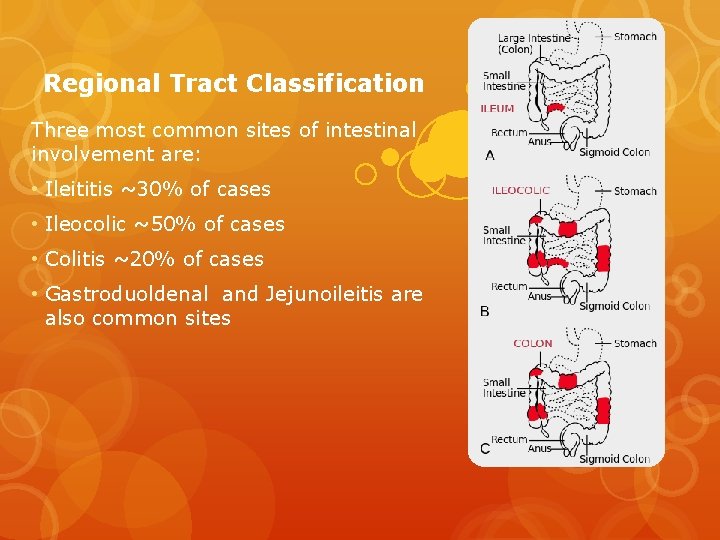
Regional Tract Classification Three most common sites of intestinal involvement are: • Ileititis ~30% of cases • Ileocolic ~50% of cases • Colitis ~20% of cases • Gastroduoldenal and Jejunoileitis are also common sites
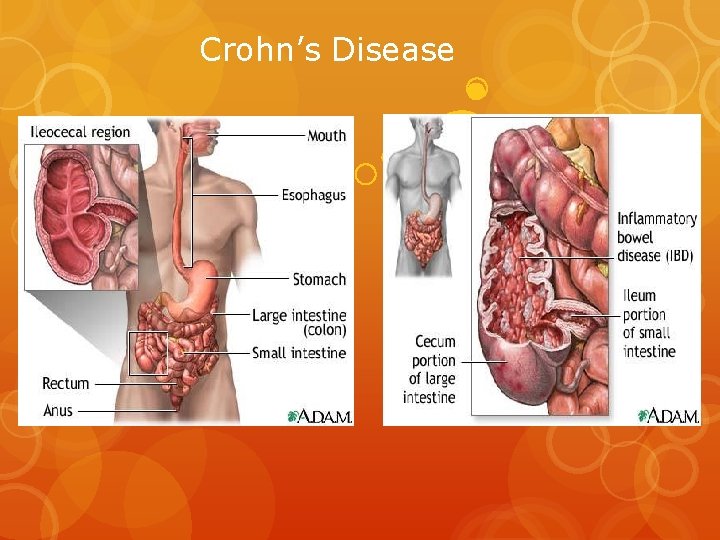
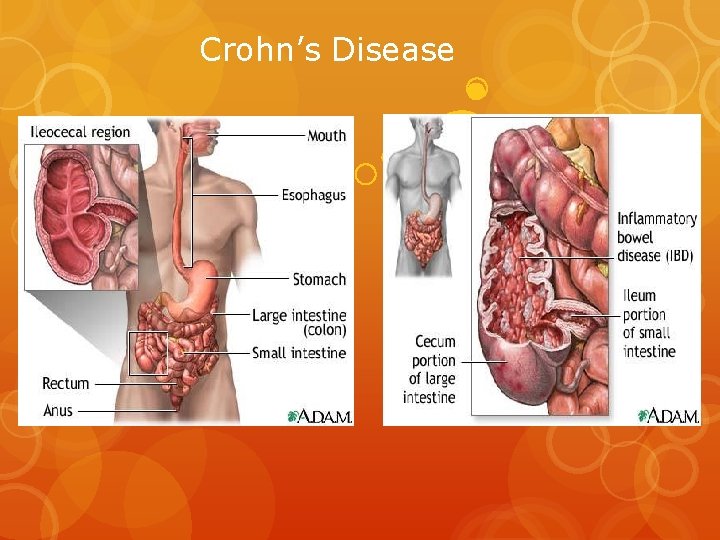
Crohn’s Disease
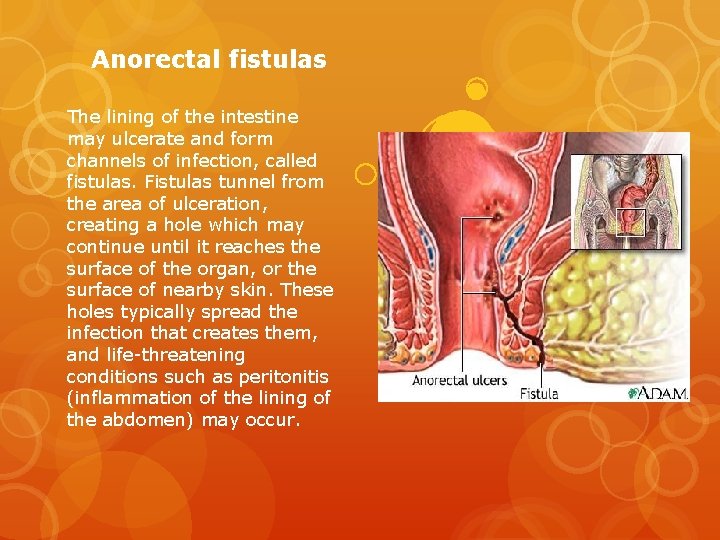
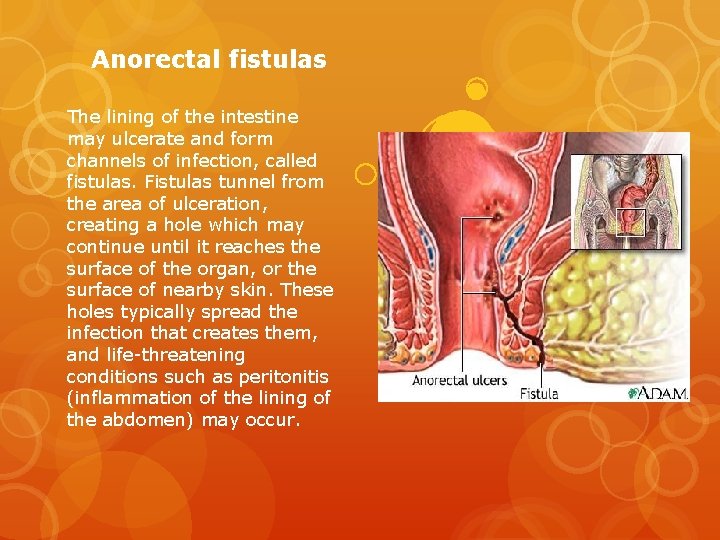
Anorectal fistulas The lining of the intestine may ulcerate and form channels of infection, called fistulas. Fistulas tunnel from the area of ulceration, creating a hole which may continue until it reaches the surface of the organ, or the surface of nearby skin. These holes typically spread the infection that creates them, and life-threatening conditions such as peritonitis (inflammation of the lining of the abdomen) may occur.
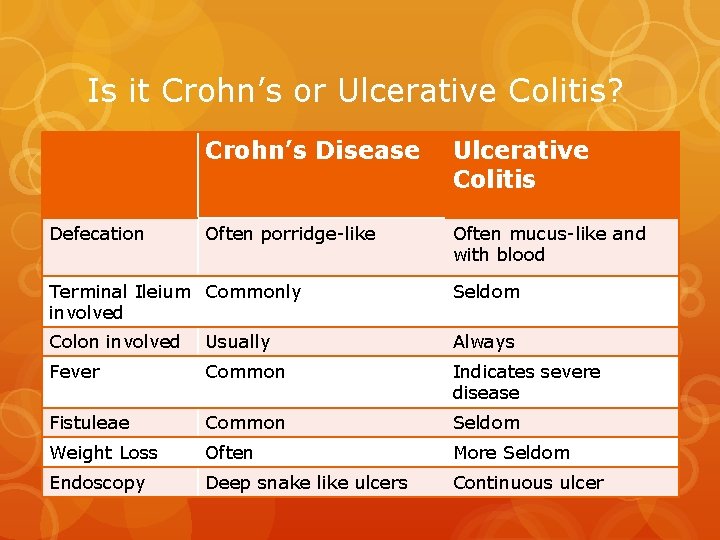
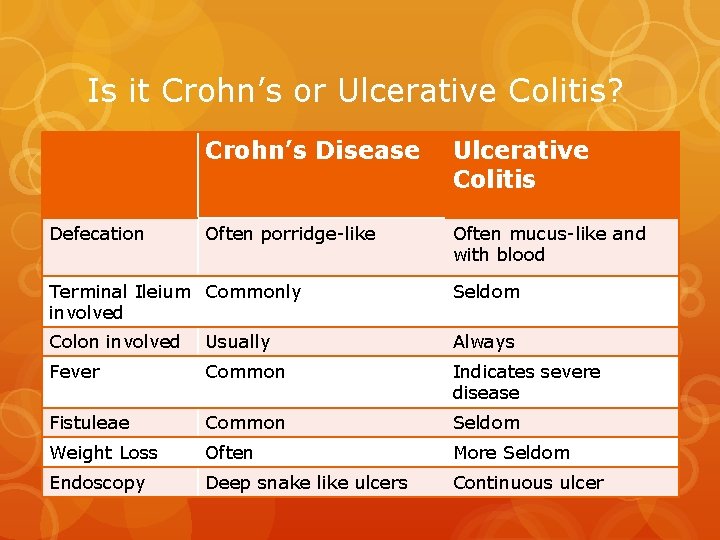
Is it Crohn’s or Ulcerative Colitis? Defecation Crohn’s Disease Ulcerative Colitis Often porridge-like Often mucus-like and with blood Terminal Ileium Commonly involved Seldom Colon involved Usually Always Fever Common Indicates severe disease Fistuleae Common Seldom Weight Loss Often More Seldom Endoscopy Deep snake like ulcers Continuous ulcer
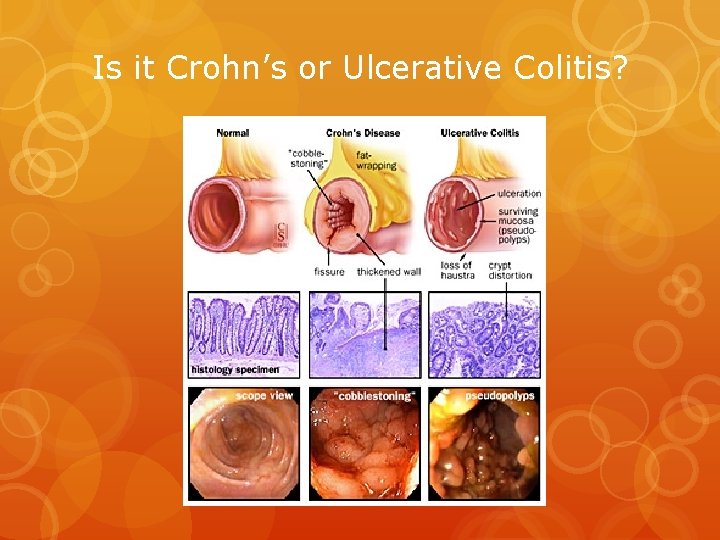
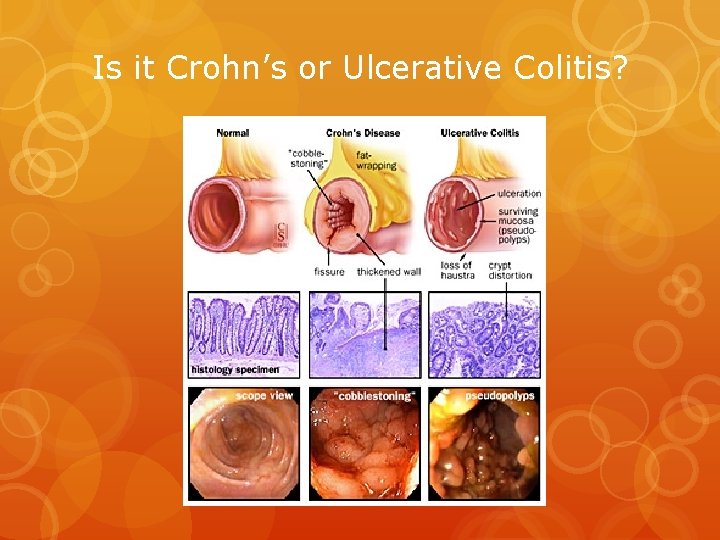
Is it Crohn’s or Ulcerative Colitis?

Symptoms Main symptoms include: Crampy abdominal pain Fever Fatigue Loss of appetite Pain with passing stool Diarrhea Weight loss Other symptoms may include: Constipation Eye inflammation Fistulas Joint pain and swelling Mouth ulcers Rectal bleeding Bloody stools Skin lumps or sores Swollen gums
What’s causing Crohn’s disease? Mycobacterium paratuberculosis Diet and stress Environmental stressors Autoimmune disorder
Who’s at risk for Crohn’s disease? Younger than 30 Elevated risk for whites and Eastern European Jewish descent A close relative diagnosed Smokers Live in an urban area Live in a northern climate Diet high in fat or refined foods
Bio-medical Interventions DIAGNOSIS Colonoscopy most effective at detection (70%) Endoscopy Blood tests MEDICATIONS Anti-inflammatory drugs Corticosteroids Antibiotics NUTRITION THERAPY Vitamin B-12 Iron Calcium Vitamin D
Bio-medical Interventions Surgery Strictureplasty Colon restructure Colectomy Treat symptoms Pros May lead to long-term remission Cons Disease often recurs
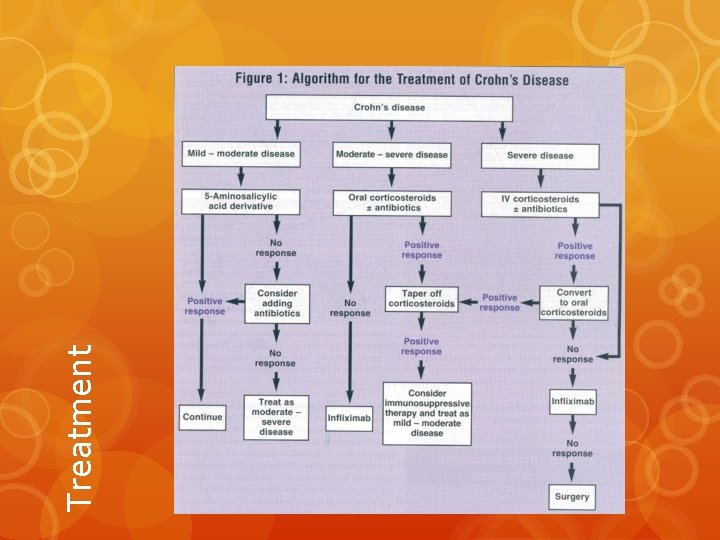
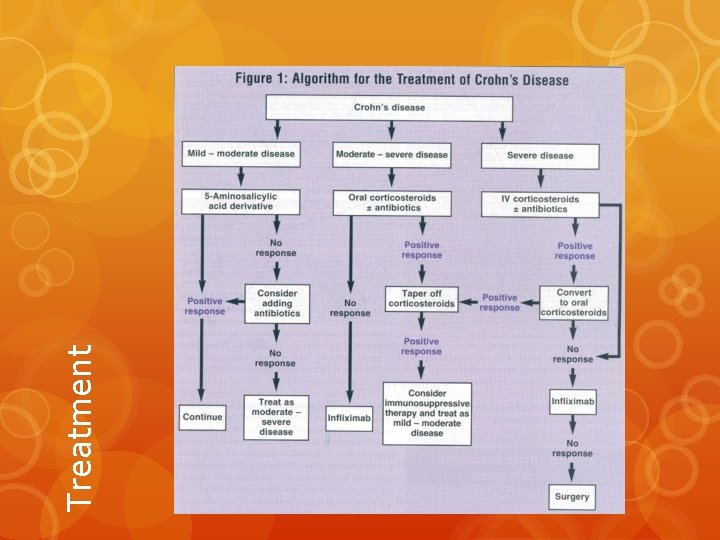
Treatment

Diet & Lifestyle Don’ts Exclusion Diets Food Journal Avoid gas inducing foods: High Fiber Do’s Drink lots of water Multi-vitamin and mineral Anti-inflammatory foods Fish oil Ginger Dairy Raw foods Stimulants Prebiotics Spicy Regular exercise High fat Stress-relief activities Stop smoking
Vitamin D o Qualitative research on 57 yr. old woman o Deficient while supplimenting o Tanning bed for 10 min. , 3 times a week for 6 months at Boston University Med. Center o Serum Vit D increase of 357% o Maintained adequate levels 6 months later o Hypovitaminosis D

Alternative Therapy Yoga Tai Chi Meditation Biofeedback Support Groups
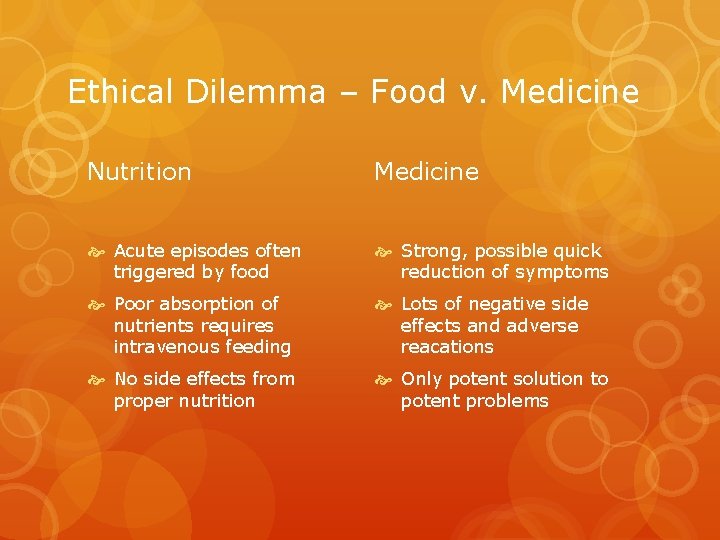
Ethical Dilemma – Food v. Medicine Nutrition Medicine Acute episodes often triggered by food Strong, possible quick reduction of symptoms Poor absorption of nutrients requires intravenous feeding Lots of negative side effects and adverse reacations No side effects from proper nutrition Only potent solution to potent problems
Conclussion Treatment requires a multi-faceted approach Support groups and experts necessary for proper education Beware of snake-oil and testimonials Get outside, get active, and gain control of your body
Need to know for the test How ulcerative colitis differs from Crohn’s disease. Nutritional guidelines for patients with Crohn’s disease. Most common areas affected by Crohn’s disease. What’s the lesser known name for Crohn’s disease. Possible causes of Crohn’s disease High risk categories Likelihood of contracting a IBD if family has been diagnosed.
The End
 Is crohns autoimmune
Is crohns autoimmune Enteritis acuta
Enteritis acuta Crohns disese
Crohns disese Chrons didease
Chrons didease Bharathi viswanathan
Bharathi viswanathan Areanna ai
Areanna ai Zabranjena vrata prezentacija
Zabranjena vrata prezentacija Bard actor
Bard actor Aka.ms/totalrewards
Aka.ms/totalrewards Akacatholic
Akacatholic Geneva metrics
Geneva metrics How to write a letter of interest for aka
How to write a letter of interest for aka Aka lut box
Aka lut box Httpaka.ms/remoteconnect
Httpaka.ms/remoteconnect Www.aka.msmyourpc
Www.aka.msmyourpc Http//aka
Http//aka Cutline vs caption
Cutline vs caption Aka sustentacular cells
Aka sustentacular cells Sigma epsilon omega
Sigma epsilon omega Alice porter murray
Alice porter murray åka skidor tjeckien
åka skidor tjeckien Tikkop meaning
Tikkop meaning Female pwo mask khan academy
Female pwo mask khan academy Aka bot
Aka bot