Criteria Led Discharge CLD Some examples Red 2

- Slides: 25
Criteria Led Discharge - CLD Some examples - #Red 2 Green #homefirst #end. PJparalysis “Patients time is the most important currency in health and social care” pete. gordon@nhs. net @Pete. Gordon 68 1
Why criteria led discharge - develop a compelling story • #Last 1000 days #Red 2 Green #end. PJparalysis • “Patient time is the greatest currency in health & social care” Prof Brian Dolan @Brianw. Dolan • 48% of people over 85 die within one year of hospital admission Imminence of death among hospital inpatients: Prevalent cohort study David Clark, Matthew Armstrong, Ananda Allan, Fiona Graham, Andrew Carnon and Christopher Isles, published online 17 March 2014 Palliat Med • 10 days in hospital (acute or community) leads to the equivalent of 10 years ageing in the muscles of people over 80 Gill et al (2004). studied the association between bed rest and functional decline over 18 months. They found a relationship between the amount of time spent in bed rest and the magnitude of functional decline in instrumental activities of daily living, mobility, physical activity, and social activity. Kortebein P, Symons TB, Ferrando A, et al. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci. 2008; 63: 1076– 1081. 2
#Red 2 Green days = giving patients back their time Criteria Led Discharge will help 3
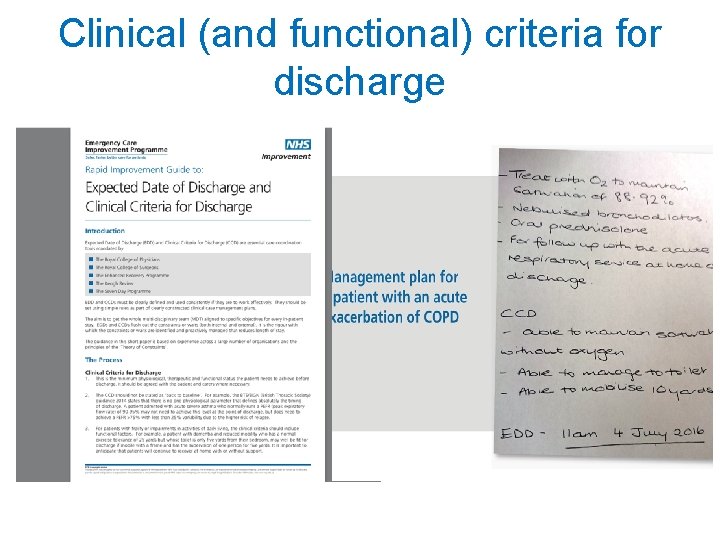
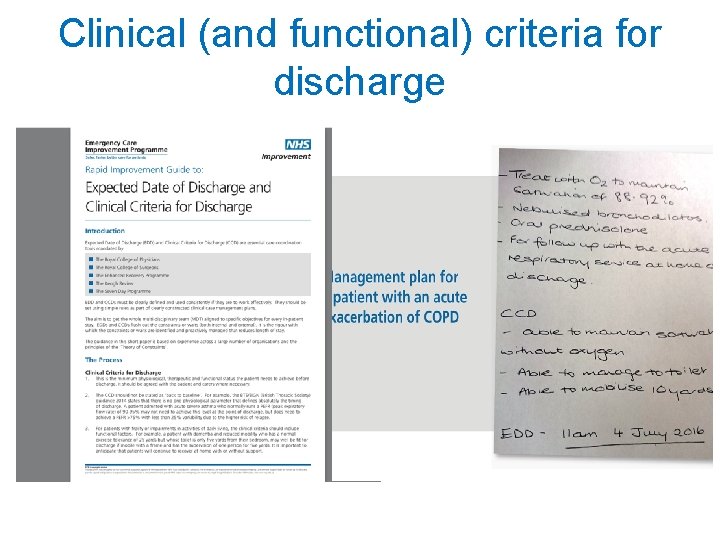
Clinical (and functional) criteria for discharge
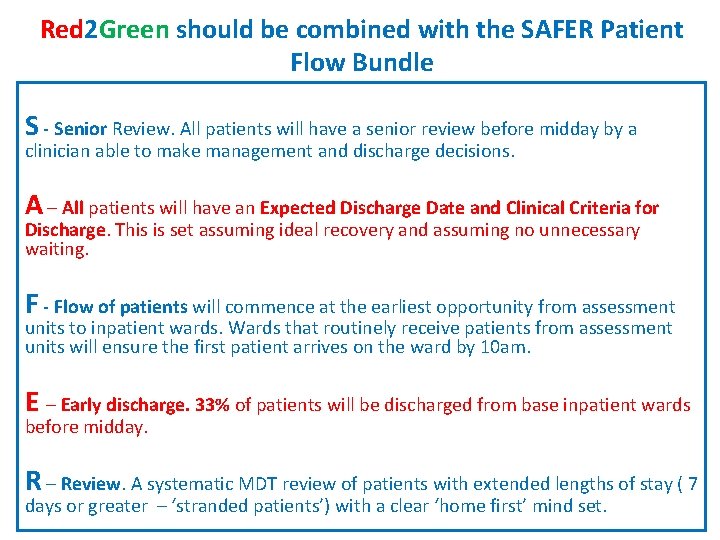
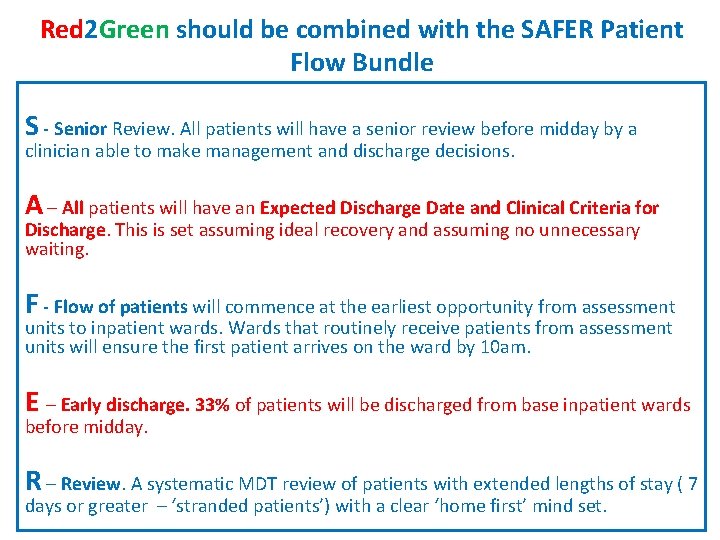
Red 2 Green should be combined with the SAFER Patient Flow Bundle S - Senior Review. All patients will have a senior review before midday by a clinician able to make management and discharge decisions. A – All patients will have an Expected Discharge Date and Clinical Criteria for Discharge. This is set assuming ideal recovery and assuming no unnecessary waiting. F - Flow of patients will commence at the earliest opportunity from assessment units to inpatient wards. Wards that routinely receive patients from assessment units will ensure the first patient arrives on the ward by 10 am. E – Early discharge. 33% of patients will be discharged from base inpatient wards before midday. R – Review. A systematic MDT review of patients with extended lengths of stay ( 7 days or greater – ‘stranded patients’) with a clear ‘home first’ mind set.
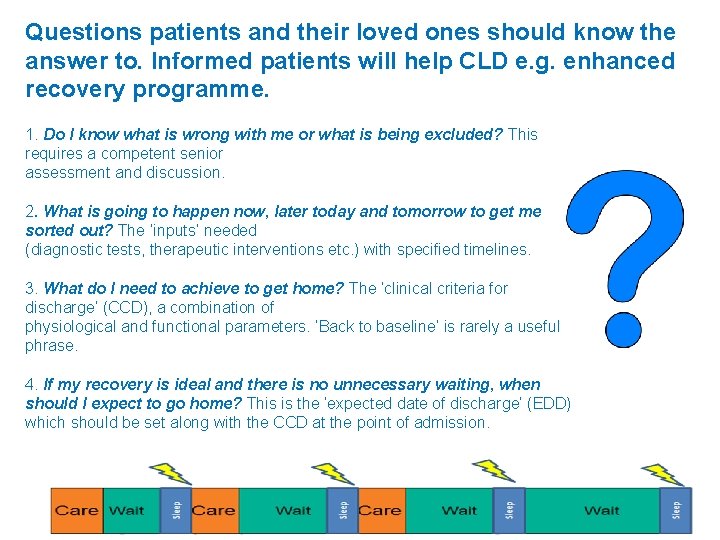
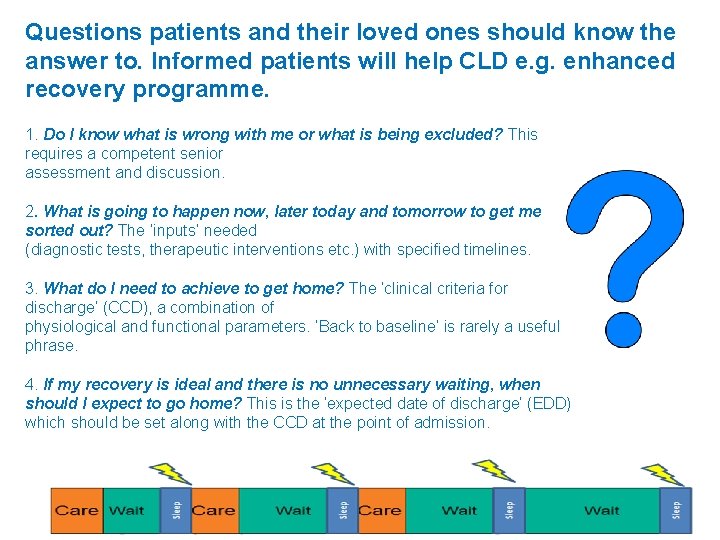
Questions patients and their loved ones should know the answer to. Informed patients will help CLD e. g. enhanced recovery programme. 1. Do I know what is wrong with me or what is being excluded? This requires a competent senior assessment and discussion. 2. What is going to happen now, later today and tomorrow to get me sorted out? The ‘inputs’ needed (diagnostic tests, therapeutic interventions etc. ) with specified timelines. 3. What do I need to achieve to get home? The ‘clinical criteria for discharge’ (CCD), a combination of physiological and functional parameters. ‘Back to baseline’ is rarely a useful phrase. 4. If my recovery is ideal and there is no unnecessary waiting, when should I expect to go home? This is the ‘expected date of discharge’ (EDD) which should be set along with the CCD at the point of admission. 6
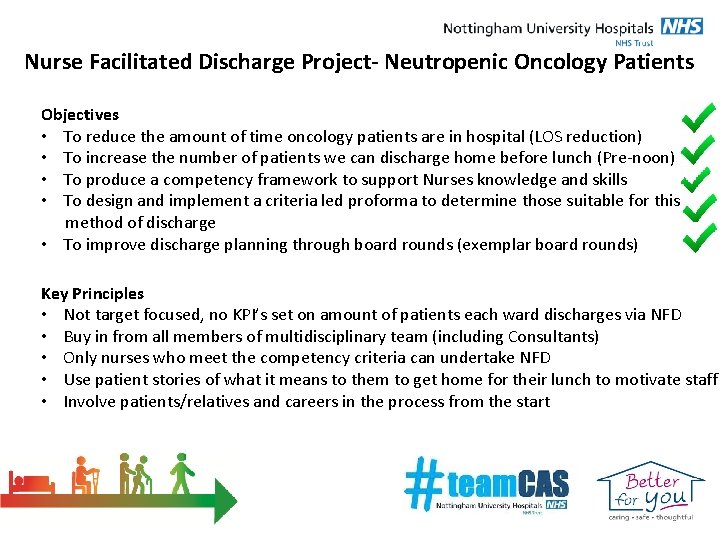
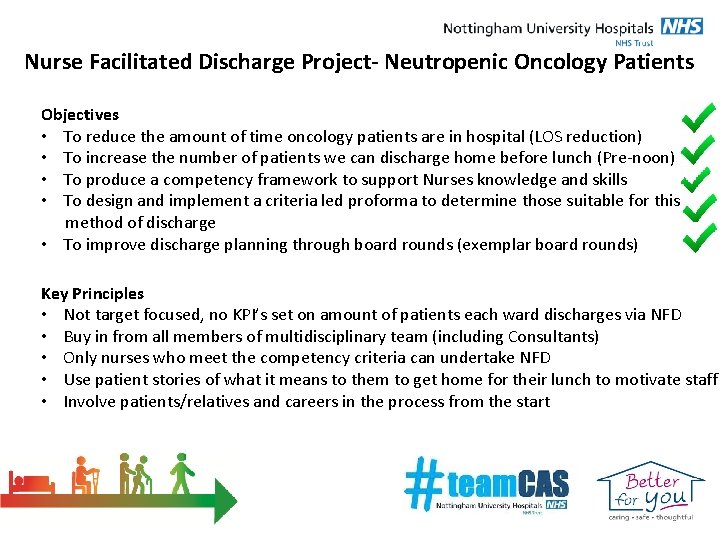
Nurse Facilitated Discharge Project- Neutropenic Oncology Patients Objectives • To reduce the amount of time oncology patients are in hospital (LOS reduction) • To increase the number of patients we can discharge home before lunch (Pre-noon) • To produce a competency framework to support Nurses knowledge and skills • To design and implement a criteria led proforma to determine those suitable for this method of discharge • To improve discharge planning through board rounds (exemplar board rounds) Key Principles • Not target focused, no KPI’s set on amount of patients each ward discharges via NFD • Buy in from all members of multidisciplinary team (including Consultants) • Only nurses who meet the competency criteria can undertake NFD • Use patient stories of what it means to them to get home for their lunch to motivate staff • Involve patients/relatives and careers in the process from the start
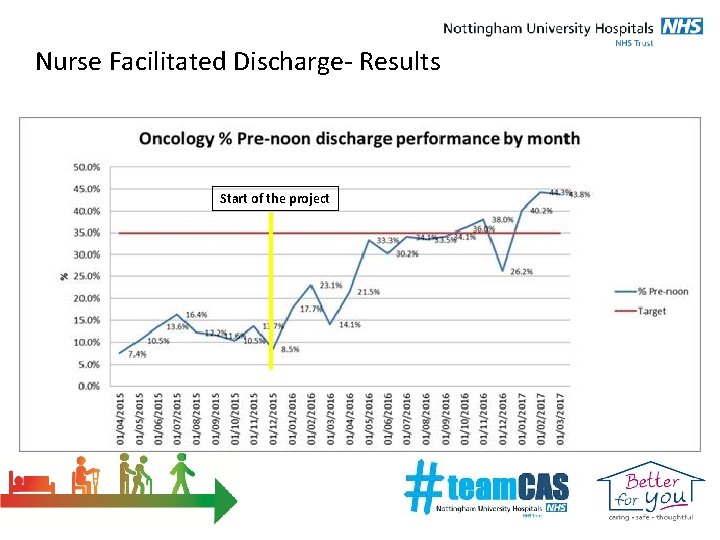
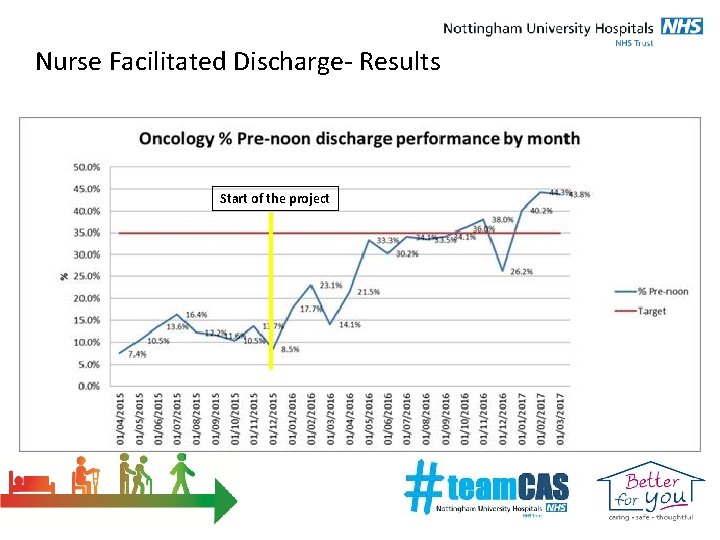
Nurse Facilitated Discharge- Results Start of the project
For further information please contact… Scott Purser- Deputy Divisional Nurse- scott. purser@nuh. nhs. uk Sharon Leighton- Project lead- sharon. leighton@nuh. nhs. uk Annie Walton- Matron Oncology- annie. walton@nuh. nhs. uk

+ Criteria led discharge South Warwickshire NHS Foundation Trust experience Dr Jyothi Nippani
+ Criteria Led Discharge n Supported by Director of Nursing n Standard operating policies ratified in the governance committees before being rolled out in specific areas n Well established on Day Surgery Unit where it is routine practice and delivered by qualified nurses n Also in 23 hour, Surgical wards, Urology, Gynaecology, Orthopaedic wards and some medical wards n Criteria for discharge are multidisciplinary and can be ANP led discharge on frail patients. n Clear instructions on when to escalate and seek advise
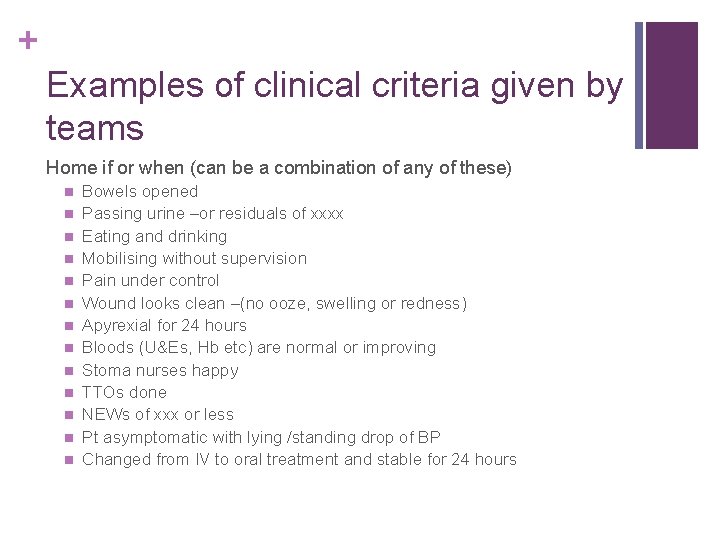
+ Examples of clinical criteria given by teams Home if or when (can be a combination of any of these) n n n n Bowels opened Passing urine –or residuals of xxxx Eating and drinking Mobilising without supervision Pain under control Wound looks clean –(no ooze, swelling or redness) Apyrexial for 24 hours Bloods (U&Es, Hb etc) are normal or improving Stoma nurses happy TTOs done NEWs of xxx or less Pt asymptomatic with lying /standing drop of BP Changed from IV to oral treatment and stable for 24 hours
+ Safety-netting methods used at discharge (varies with each team) n Verbal discharge advice given by nurse n Speciality advice leaflets given on what to expect and care at home n Access to a point of contact in the hospital for queries, advise and reassurance – (not to default to GP or ED) n Telephone calls to patient to check if they are OK after a GA n Nurses can access consultants /team out of hours for any queries n Nurses can book into urgent consultant OP slots/ hot clinics
+ Advantages n Patients can be discharged timely and earlier on in the morning n Nurses can plan the transport etc. accordingly n Patient flow is maximised n Frees up doctors
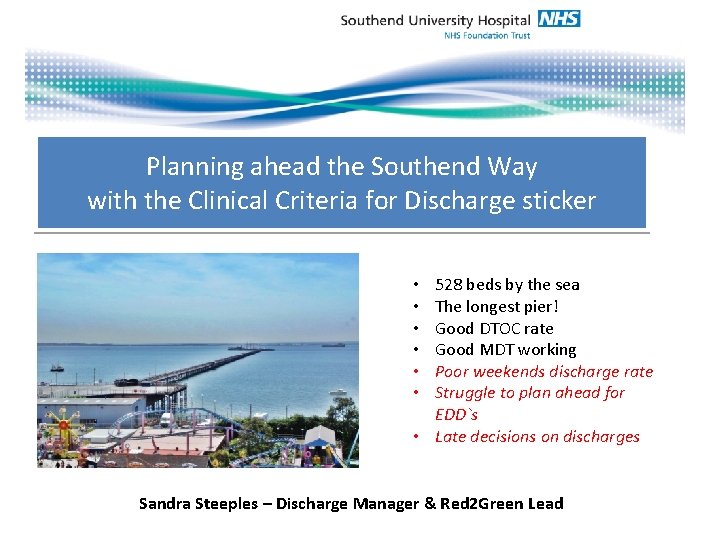
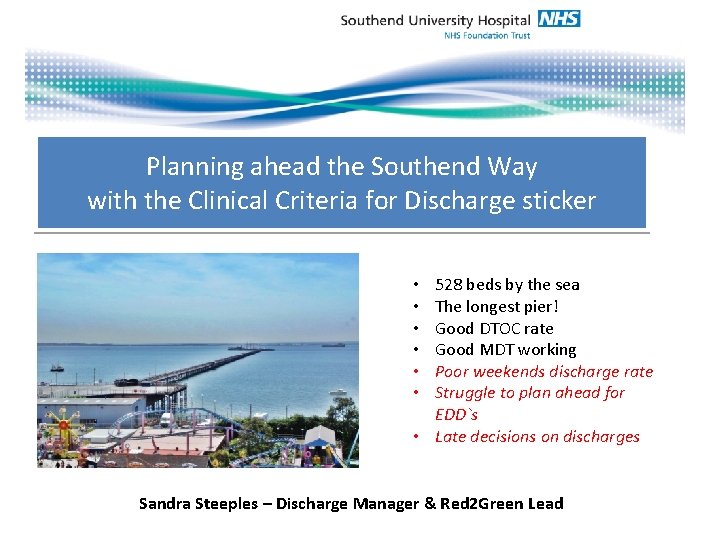
Planning ahead the Southend Way with the Clinical Criteria for Discharge sticker 528 beds by the sea The longest pier! Good DTOC rate Good MDT working Poor weekends discharge rate Struggle to plan ahead for EDD`s • Late decisions on discharges • • • Sandra Steeples – Discharge Manager & Red 2 Green Lead
Benefits of CCD • • • Many patients stay in hospital unnecessarily “waiting for something to happen”. This is often because there is no clear idea of what is needed to leave hospital. The senior Dr will know when the patient can go home – he / she just needs to share that knowledge! If the Dr documents clear clinical criteria for discharge, then discharge will happen! Patients benefit from improved care co-ordination Patients benefit from a good clinical plan with a timely planned discharge If the team understand what needs to happen to get a patient home, it is more likely to happen Benefits to the Trust • Real time accurate bed management • Improved patient flow through the organisation • Meaningful information for capacity and demand to be managed • Less complaints about delays • Happier patients
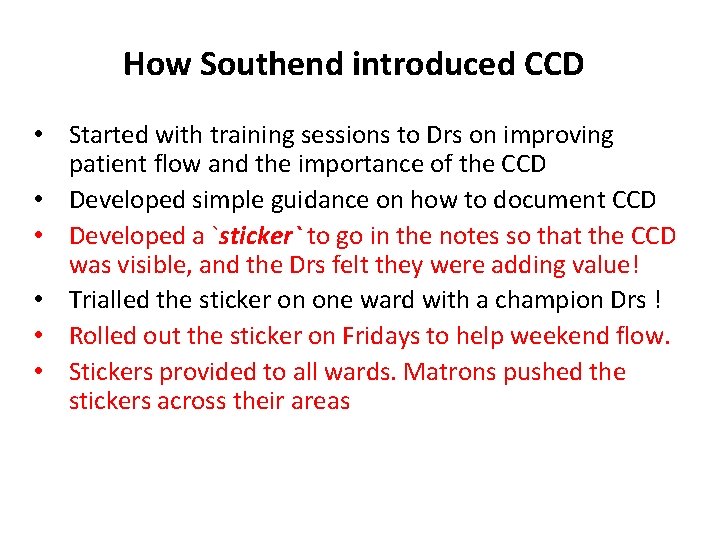
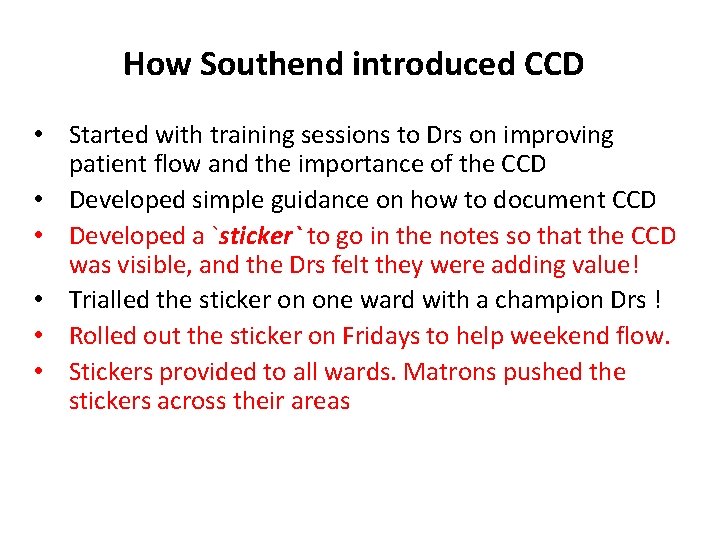
How Southend introduced CCD • Started with training sessions to Drs on improving patient flow and the importance of the CCD • Developed simple guidance on how to document CCD • Developed a `sticker` to go in the notes so that the CCD was visible, and the Drs felt they were adding value! • Trialled the sticker on one ward with a champion Drs ! • Rolled out the sticker on Fridays to help weekend flow. • Stickers provided to all wards. Matrons pushed the stickers across their areas
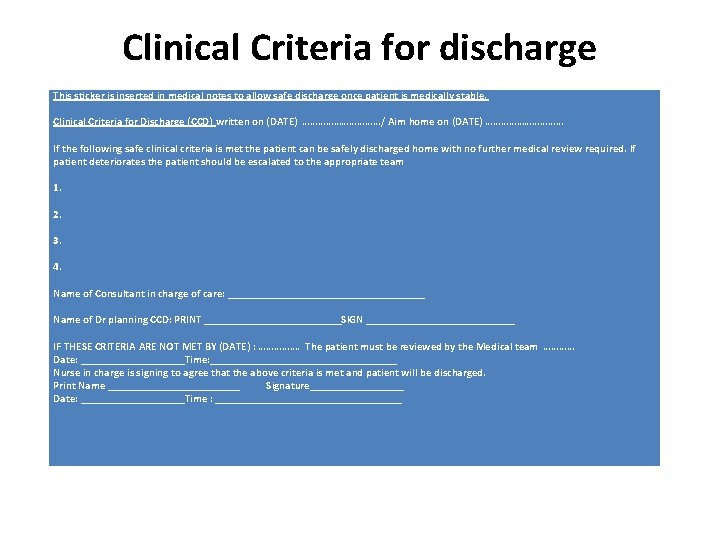
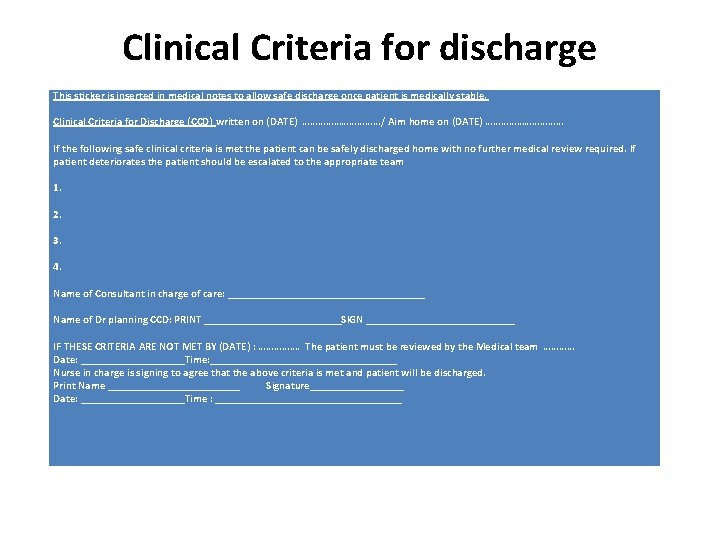
Clinical Criteria for discharge This sticker is inserted in medical notes to allow safe discharge once patient is medically stable. Clinical Criteria for Discharge (CCD) written on (DATE) ……………/ Aim home on (DATE) …………… If the following safe clinical criteria is met the patient can be safely discharged home with no further medical review required. If patient deteriorates the patient should be escalated to the appropriate team 1. 2. 3. 4. Name of Consultant in charge of care: __________________ Name of Dr planning CCD: PRINT _____________SIGN ______________ IF THESE CRITERIA ARE NOT MET BY (DATE) : ……………. The patient must be reviewed by the Medical team ………… Date: __________Time: _________________ Nurse in charge is signing to agree that the above criteria is met and patient will be discharged. Print Name ____________ Signature_________ Date: __________Time : _________________
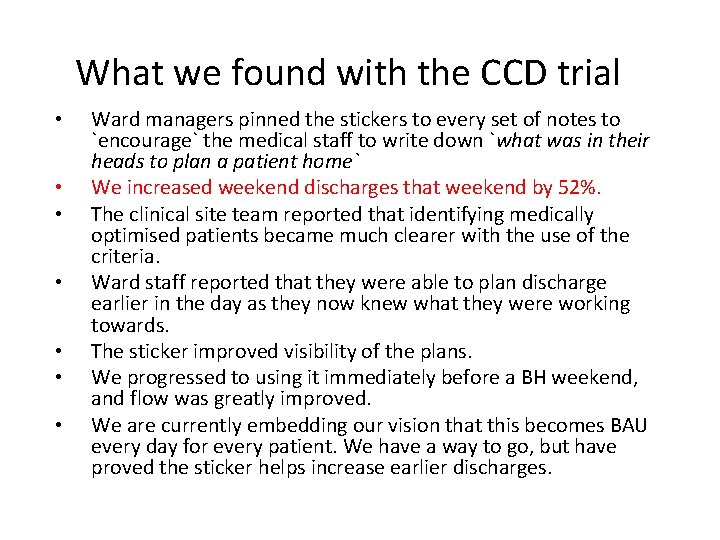
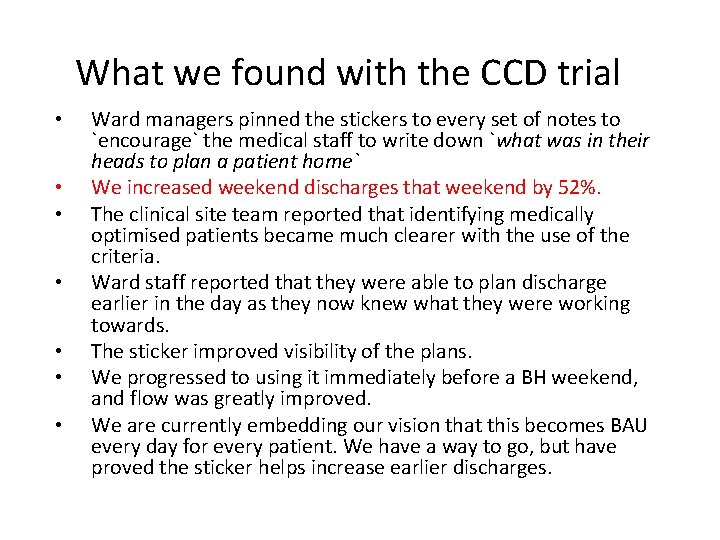
What we found with the CCD trial • • Ward managers pinned the stickers to every set of notes to `encourage` the medical staff to write down `what was in their heads to plan a patient home` We increased weekend discharges that weekend by 52%. The clinical site team reported that identifying medically optimised patients became much clearer with the use of the criteria. Ward staff reported that they were able to plan discharge earlier in the day as they now knew what they were working towards. The sticker improved visibility of the plans. We progressed to using it immediately before a BH weekend, and flow was greatly improved. We are currently embedding our vision that this becomes BAU every day for every patient. We have a way to go, but have proved the sticker helps increase earlier discharges.
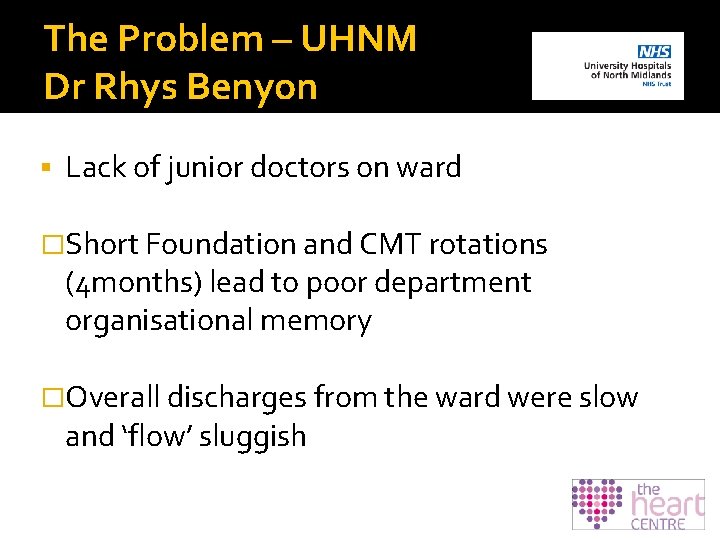
The Problem – UHNM Dr Rhys Benyon Lack of junior doctors on ward �Short Foundation and CMT rotations (4 months) lead to poor department organisational memory �Overall discharges from the ward were slow and ‘flow’ sluggish
UHNM solution � Cardiac nurse practitioners on the ward coordinating discharges and encouraging flow � Experienced senior nurses recruited from Cardiology wards – Average 15 yrs cardiology experience � 6 months course in generic health assessment � Prolonged specialty specific training program for 18 months with consultant mentor throughout � Prescribing course for allied health professionals
UHNM solution �Rigorous assessment process Nationally recognised cardiology specific masters program MINICEX’s as designed for SPR assessment Patient surveys 360 appraisal Team reviews
UHNM summary � The major gain will be when the cardiac nurse practitioners can complete the discharge letters and this requires them to have been through a nurse prescribing course. � 6 of them will complete this in September 2017 � Departmental view - we can no longer rely on the SHO grade. � 4 vacancies out of 10 slots has been the norm for the last 18 months. The deaneries simply cannot fill their slots. � We are going to try to move to a hybrid of specialist nurses and junior doctors in about equal numbers. � The feeling from everyone including the junior doctors is that this is a great success when we piloted it for shifts on the ward.
Summary / Key Points • Needs to be MDT • Involve patients – the 4 questions • Development of roles to ensure competency, merge boundaries – not just nurse led • Use multiple PDSAs & improvement measures (we are still poor at this) to prove the positive effect e. g. reduced LOS, earlier discharge time and reduced complaints • Use patient stories focussing on saving patients time • Link to the SAFER patient flow bundle and Red 2 Green days • Develop a proforma • Link to 7 day services – increase weekend discharge rates • Don’t aim for perfection – start somewhere You either believe you can or you can’t