Creatine phosphate also called phosphocreatine the phosphorylated derivative
- Slides: 25
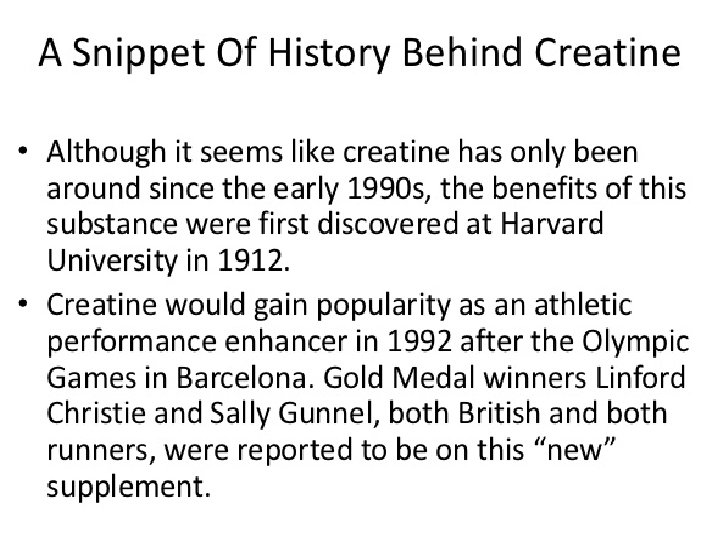
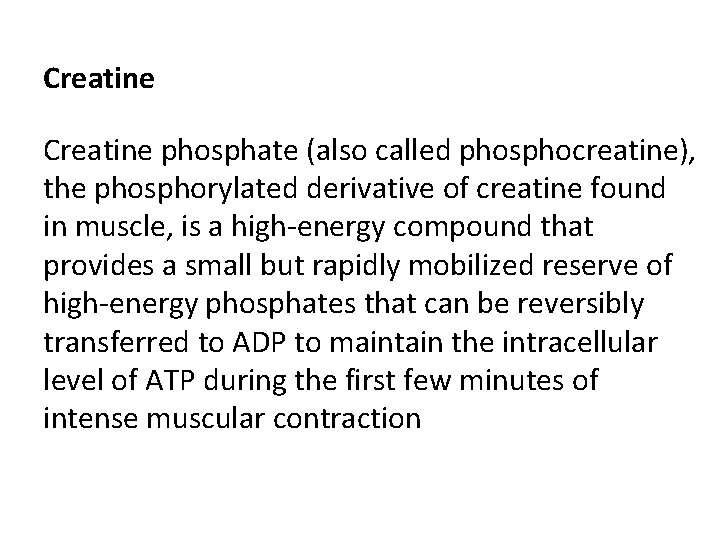
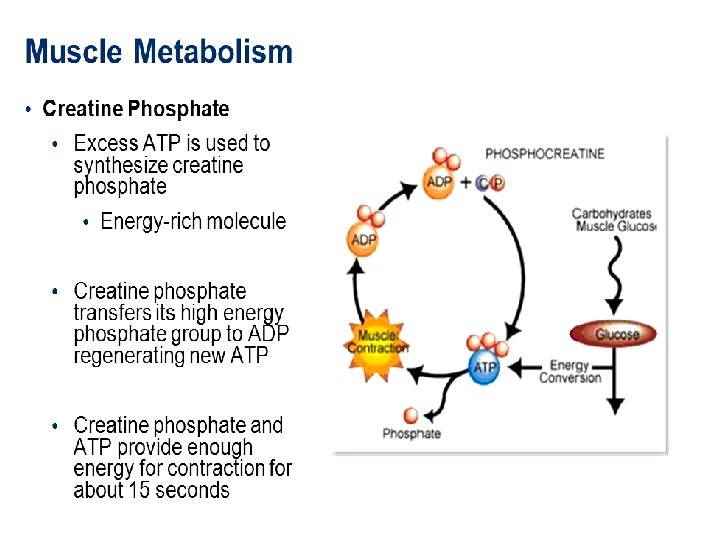
Creatine phosphate (also called phosphocreatine), the phosphorylated derivative of creatine found in muscle, is a high-energy compound that provides a small but rapidly mobilized reserve of high-energy phosphates that can be reversibly transferred to ADP to maintain the intracellular level of ATP during the first few minutes of intense muscular contraction
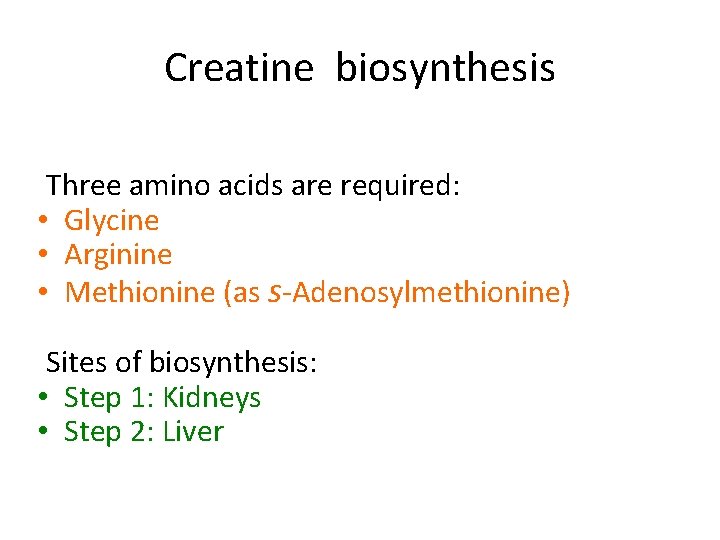
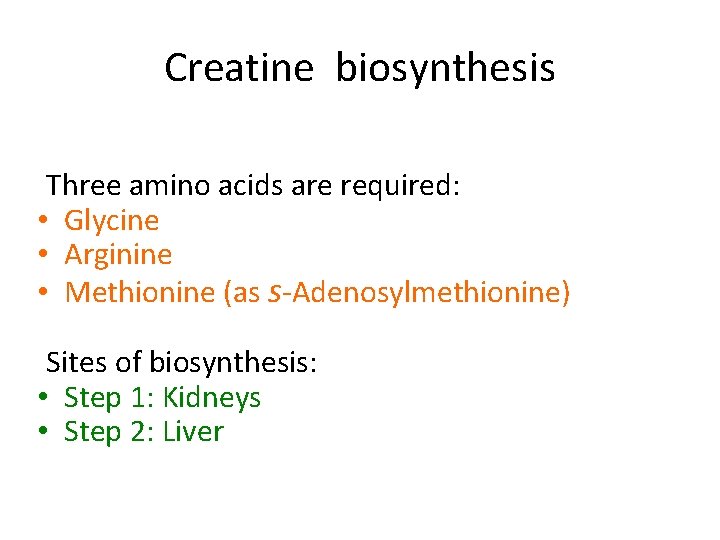
Creatine biosynthesis Three amino acids are required: • Glycine • Arginine • Methionine (as s-Adenosylmethionine) Sites of biosynthesis: • Step 1: Kidneys • Step 2: Liver
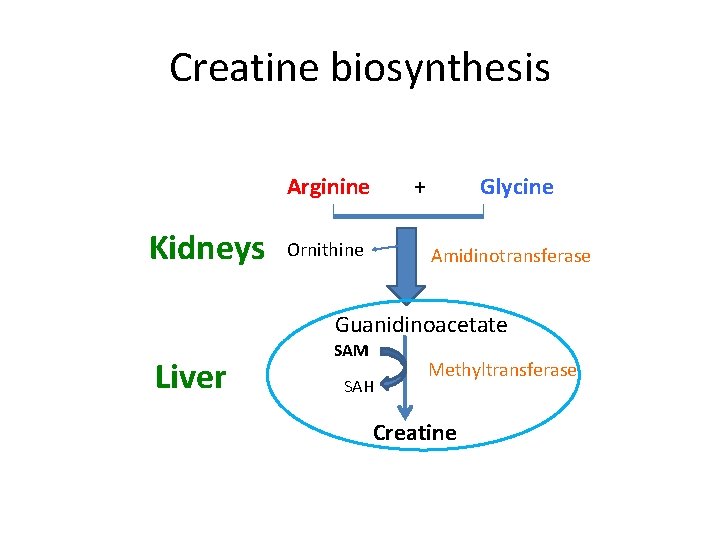
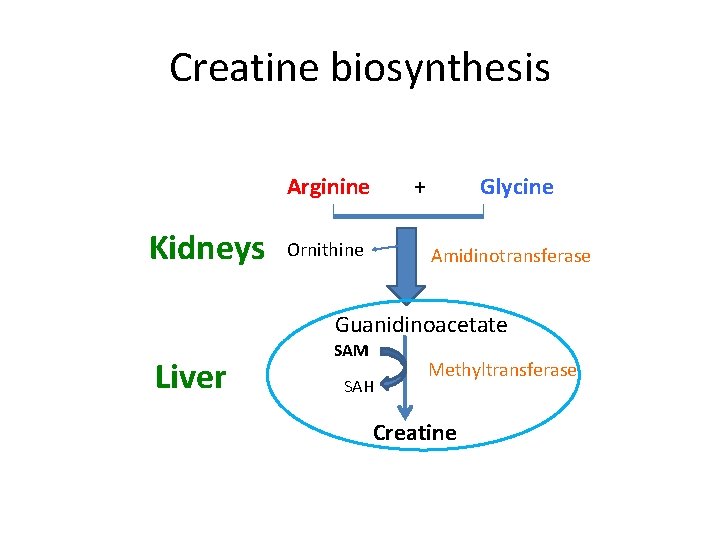
Creatine biosynthesis Arginine Kidneys + Ornithine Glycine Amidinotransferase Guanidinoacetate Liver SAM SAH Methyltransferase Creatine
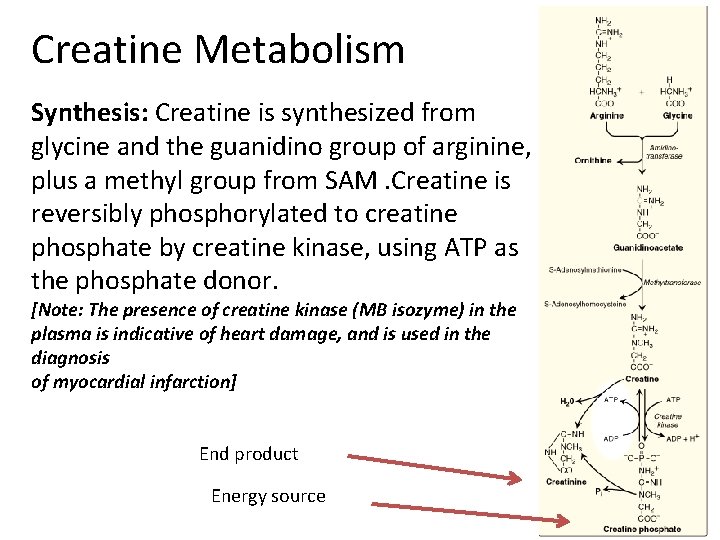
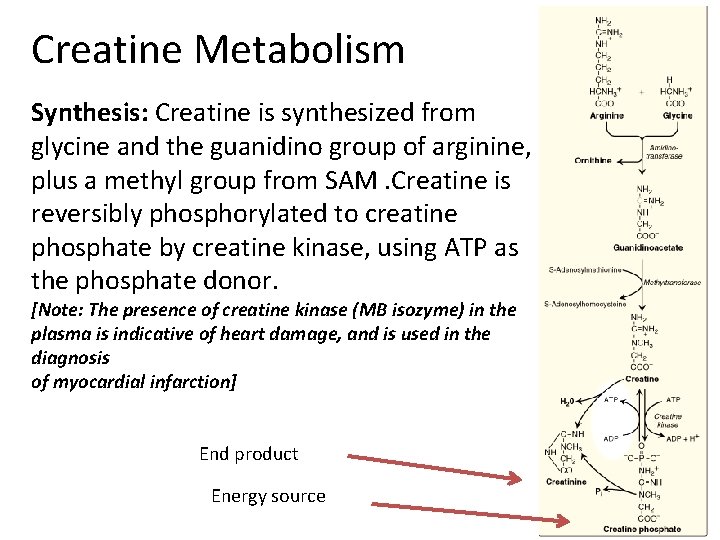
Creatine Metabolism Synthesis: Creatine is synthesized from glycine and the guanidino group of arginine, plus a methyl group from SAM. Creatine is reversibly phosphorylated to creatine phosphate by creatine kinase, using ATP as the phosphate donor. [Note: The presence of creatine kinase (MB isozyme) in the plasma is indicative of heart damage, and is used in the diagnosis of myocardial infarction] End product Energy source
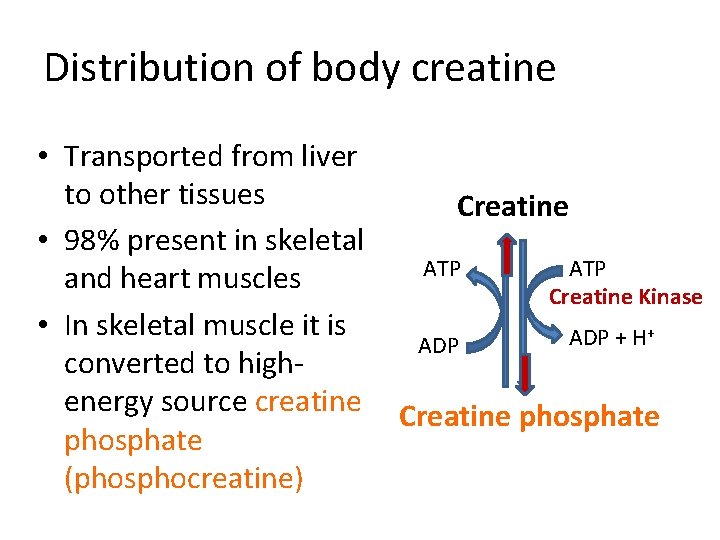
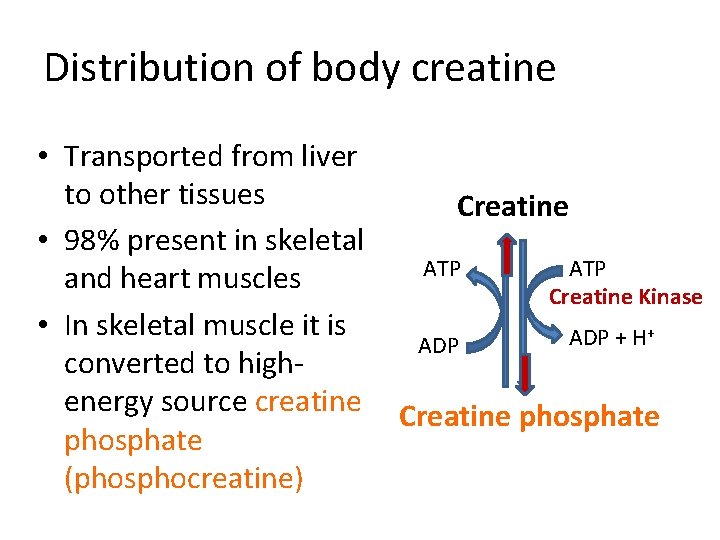
Distribution of body creatine • Transported from liver to other tissues • 98% present in skeletal and heart muscles • In skeletal muscle it is converted to highenergy source creatine phosphate (phosphocreatine) Creatine ATP ADP ATP Creatine Kinase ADP + H+ Creatine phosphate
Creatine phosphate • The amount of creatine phosphate in the body is proportional to the muscle mass
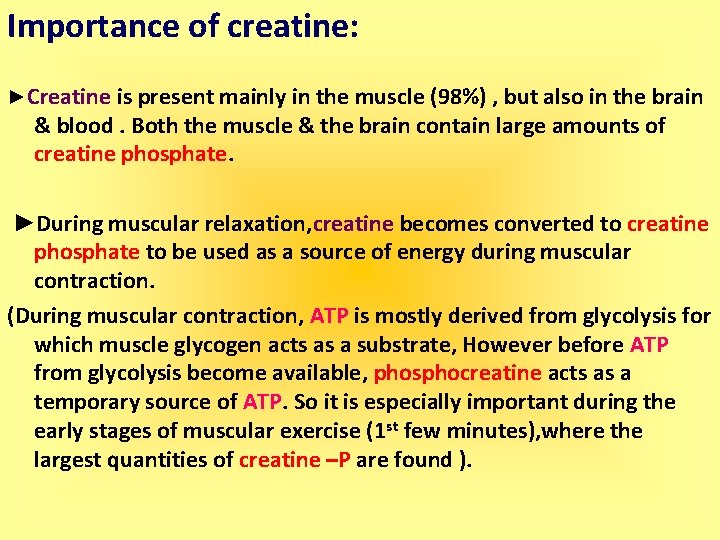
Importance of creatine: ►Creatine is present mainly in the muscle (98%) , but also in the brain & blood. Both the muscle & the brain contain large amounts of creatine phosphate. ►During muscular relaxation, creatine becomes converted to creatine phosphate to be used as a source of energy during muscular contraction. (During muscular contraction, ATP is mostly derived from glycolysis for which muscle glycogen acts as a substrate, However before ATP from glycolysis become available, phosphocreatine acts as a temporary source of ATP. So it is especially important during the early stages of muscular exercise (1 st few minutes), where the largest quantities of creatine –P are found ).
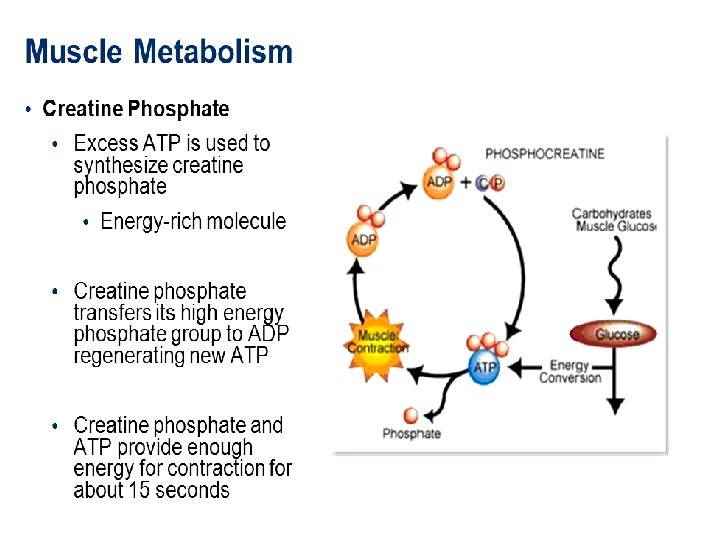
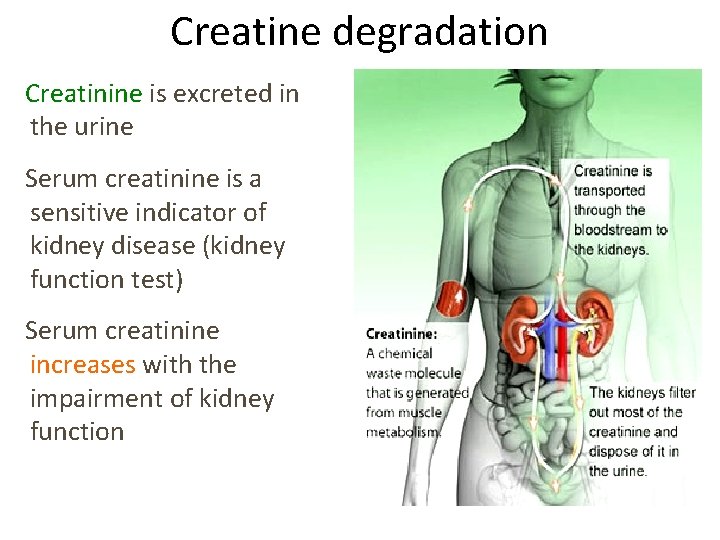
Degradation: Creatine and creatine phosphate spontaneously cyclize at a slow but constant rate to form creatinine, which is excreted in the urine. The amount of creatinine excreted is proportional to the total creatine phosphate content of the body, and thus can be used to estimate muscle mass. When muscle mass decreases for any reason (for example, from paralysis or muscular dystrophy), the creatinine content of the urine falls. In addition, any rise in blood creatinine is a sensitive indicator of kidney malfunction, because creatinine normally is rapidly removed from the blood and excreted. A typical adult male excretes about 15 mmol of creatinine per day.
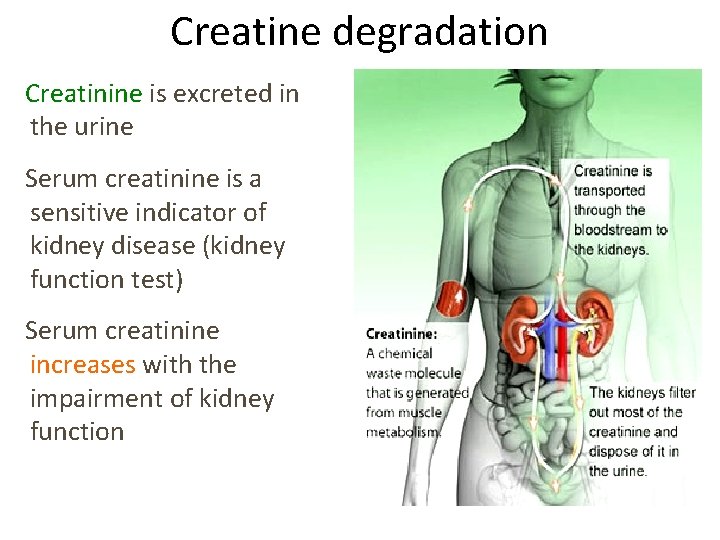
Creatine degradation Creatinine is excreted in the urine Serum creatinine is a sensitive indicator of kidney disease (kidney function test) Serum creatinine increases with the impairment of kidney function
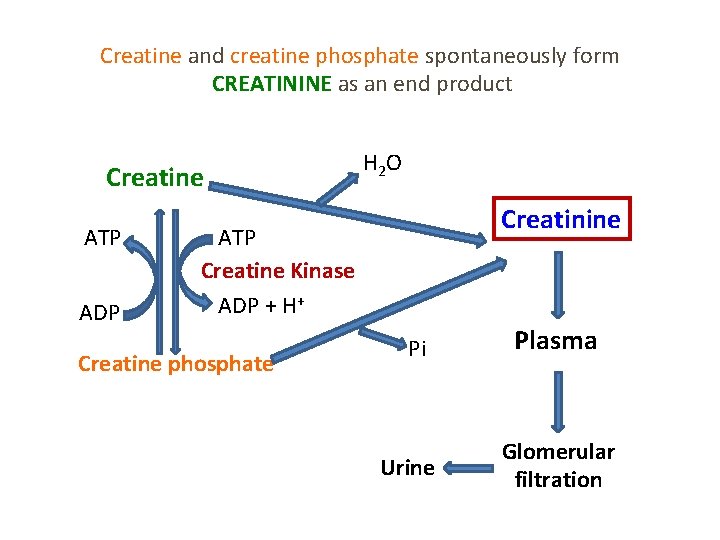
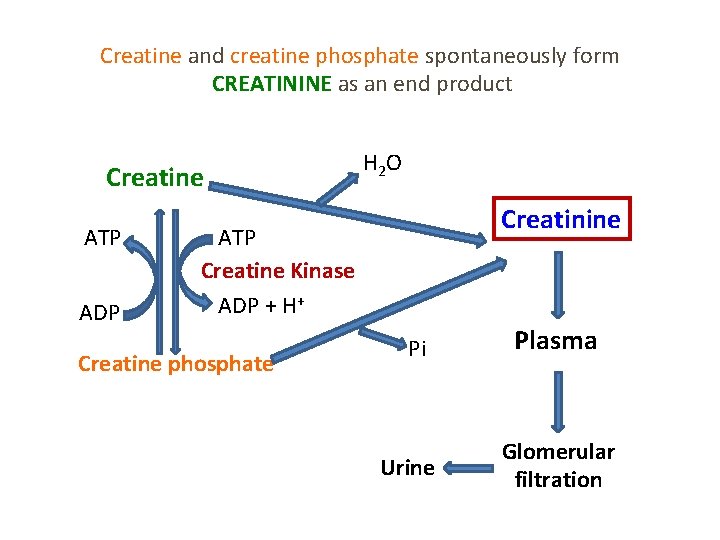
Creatine and creatine phosphate spontaneously form CREATININE as an end product Creatine ATP ADP H 2 O Creatinine ATP Creatine Kinase ADP + H+ Creatine phosphate Pi Urine Plasma Glomerular filtration
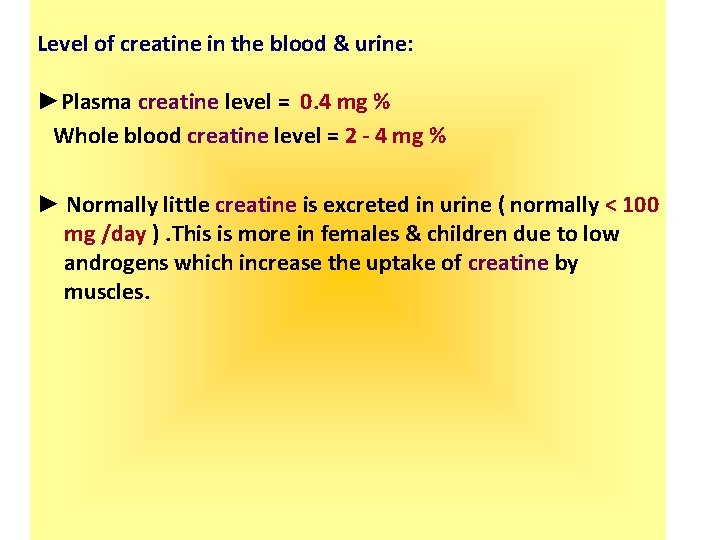
Level of creatine in the blood & urine: ►Plasma creatine level = 0. 4 mg % Whole blood creatine level = 2 - 4 mg % ► Normally little creatine is excreted in urine ( normally < 100 mg /day ). This is more in females & children due to low androgens which increase the uptake of creatine by muscles.
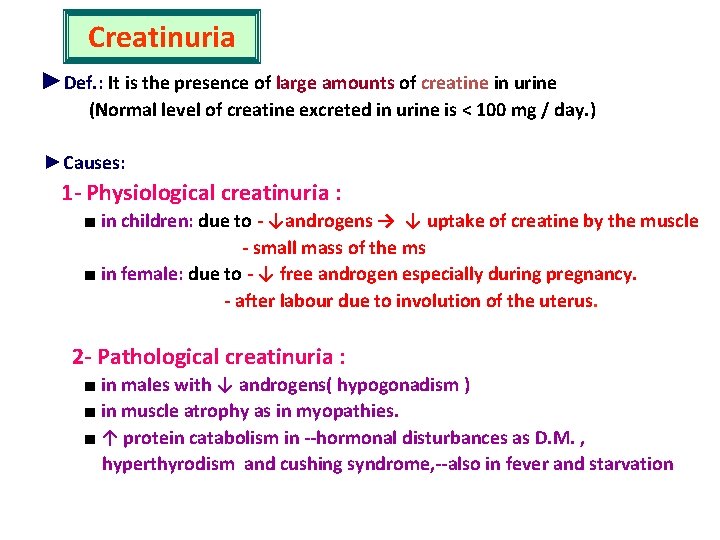
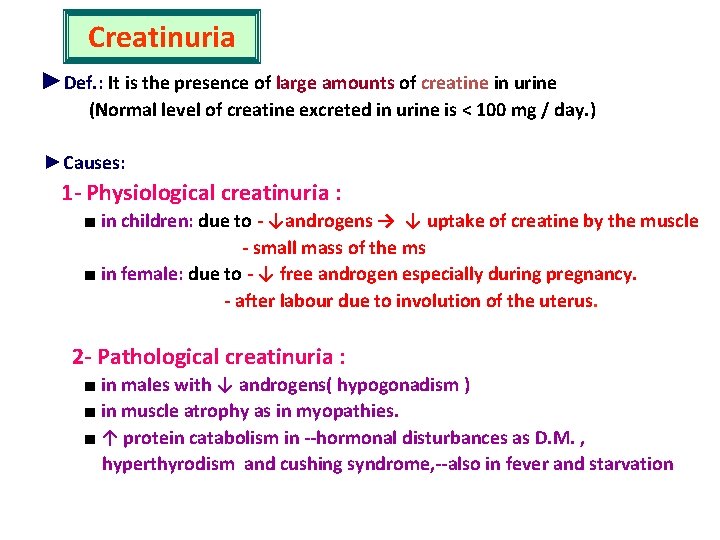
Creatinuria ►Def. : It is the presence of large amounts of creatine in urine (Normal level of creatine excreted in urine is < 100 mg / day. ) ►Causes: 1 - Physiological creatinuria : ■ in children: due to - ↓androgens → ↓ uptake of creatine by the muscle - small mass of the ms ■ in female: due to - ↓ free androgen especially during pregnancy. - after labour due to involution of the uterus. 2 - Pathological creatinuria : ■ in males with ↓ androgens( hypogonadism ) ■ in muscle atrophy as in myopathies. ■ ↑ protein catabolism in --hormonal disturbances as D. M. , hyperthyrodism and cushing syndrome, --also in fever and starvation
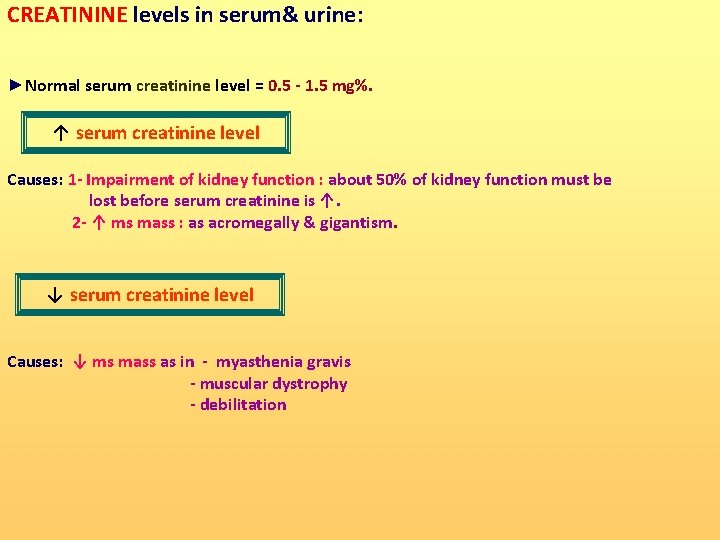
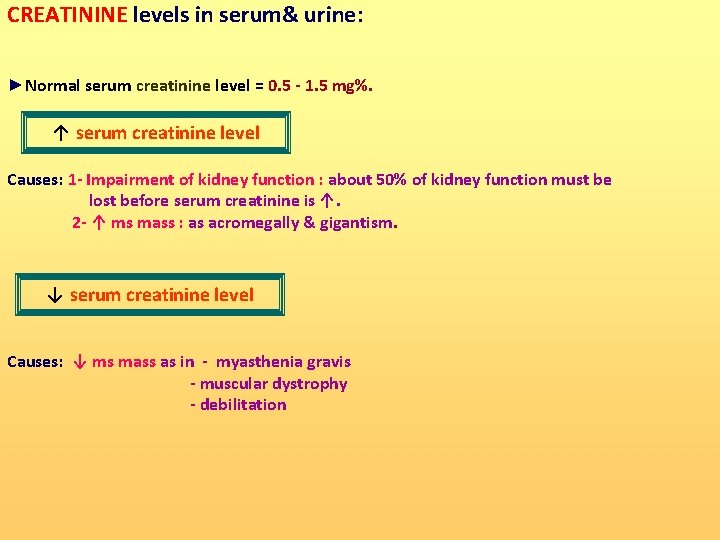
CREATININE levels in serum& urine: ►Normal serum creatinine level = 0. 5 - 1. 5 mg%. ↑ serum creatinine level Causes: 1 - Impairment of kidney function : about 50% of kidney function must be lost before serum creatinine is ↑. 2 - ↑ ms mass : as acromegally & gigantism. ↓ serum creatinine level Causes: ↓ ms mass as in - myasthenia gravis - muscular dystrophy - debilitation
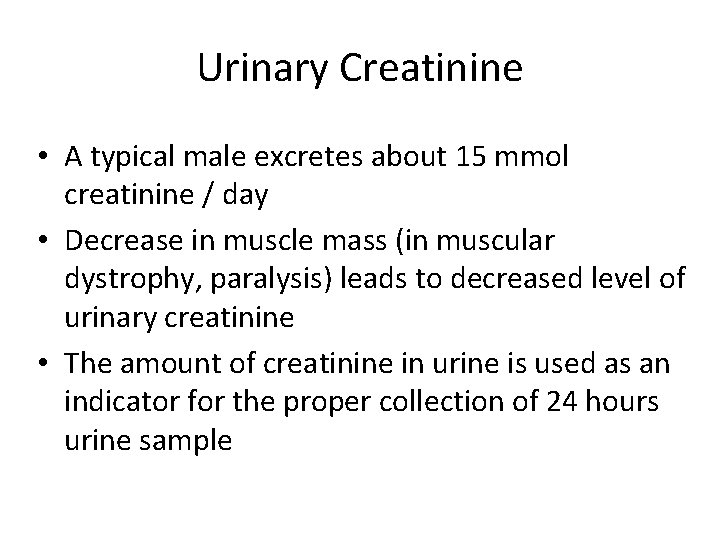
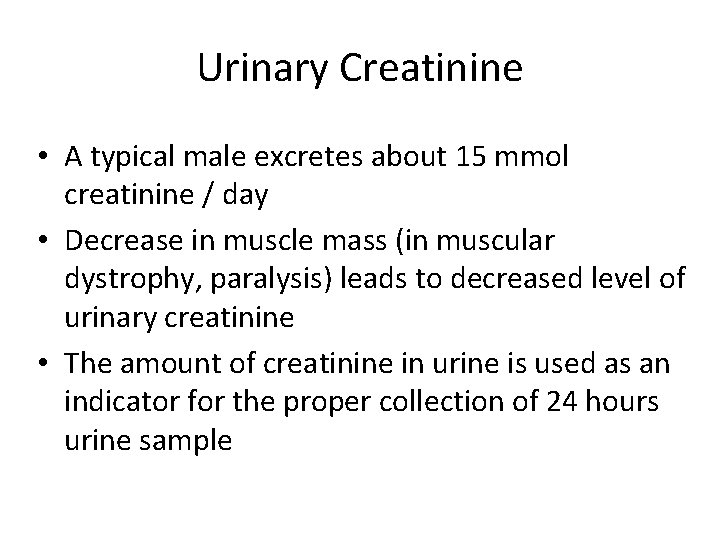
Urinary Creatinine • A typical male excretes about 15 mmol creatinine / day • Decrease in muscle mass (in muscular dystrophy, paralysis) leads to decreased level of urinary creatinine • The amount of creatinine in urine is used as an indicator for the proper collection of 24 hours urine sample
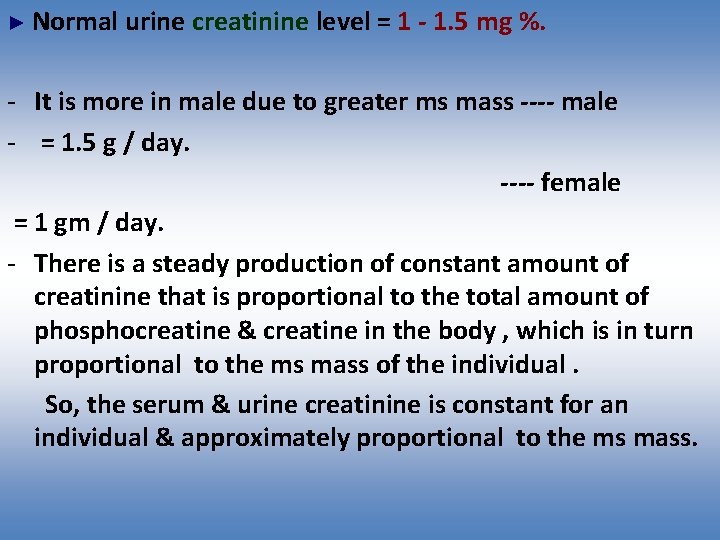
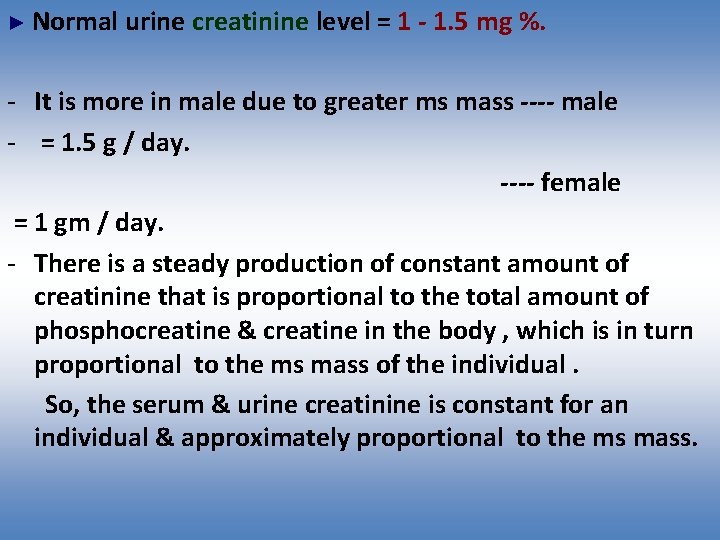
► Normal urine creatinine level = 1 - 1. 5 mg %. - It is more in male due to greater ms mass ---- male - = 1. 5 g / day. ---- female = 1 gm / day. - There is a steady production of constant amount of creatinine that is proportional to the total amount of phosphocreatine & creatine in the body , which is in turn proportional to the ms mass of the individual. So, the serum & urine creatinine is constant for an individual & approximately proportional to the ms mass.
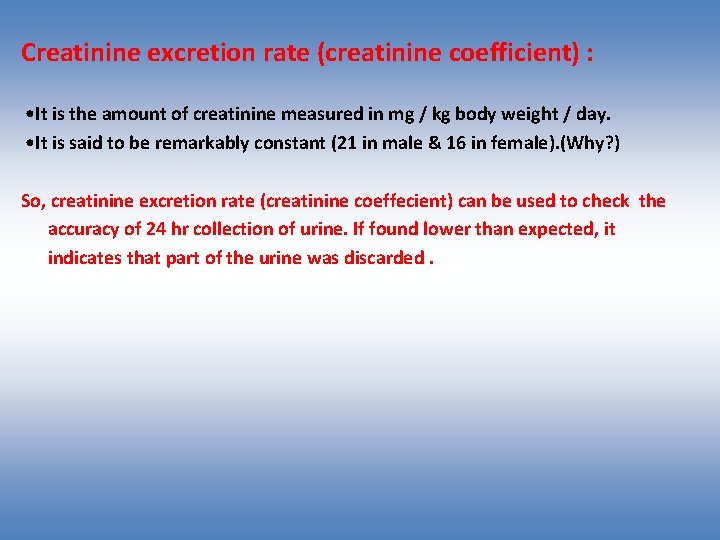
Creatinine excretion rate (creatinine coefficient) : • It is the amount of creatinine measured in mg / kg body weight / day. • It is said to be remarkably constant (21 in male & 16 in female). (Why? ) So, creatinine excretion rate (creatinine coeffecient) can be used to check the accuracy of 24 hr collection of urine. If found lower than expected, it indicates that part of the urine was discarded.
Creatinine clearance - The volume of serum or plasma that would be cleared of creatinine by one minute's excretion of urine. value that reflects the body's ability to excrete creatinine; it is used to diagnose and monitor renal function. - Urinary creatinine is 100% endogenous in origin i. e. not affected by diet being synthesized in the body & no diurnal variation. So it can be used for calculation of urinary output of substance amount of creatinine in urine.
Creatinine clearance ……. cont - Also creatinine is chiefly filtered by the kidney, though a small amount is actively secreted. There is little-to-no tubular reabsorption of creatinine. If the filtering of the kidney is deficient, blood levels rise. As a result, creatinine levels in blood and urine may be used to calculate the creatinine clearance (Cr. Cl), which reflects the glomerular filtration rate (GFR). The GFR is clinically important because it is a measurement of renal function. However, in cases of severe renal dysfunction, the creatinine clearance rate will be "overestimated" because the active secretion of creatinine will account for a larger fraction of the total creatinine cleared. Ketoacids, cimetidine and trimethoprim reduce creatinine tubular secretion and therefore increase the accuracy of the GFR estimate, particularly in severe renal dysfunction. (In the absence of secretion, creatinine behaves like inulin. )
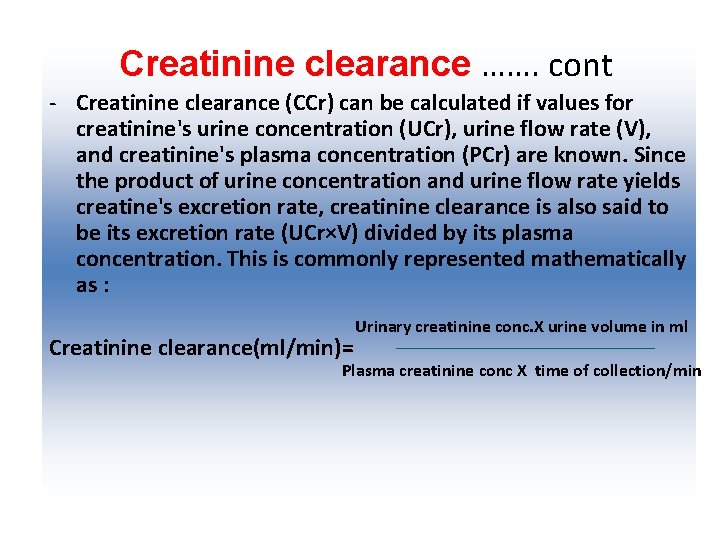
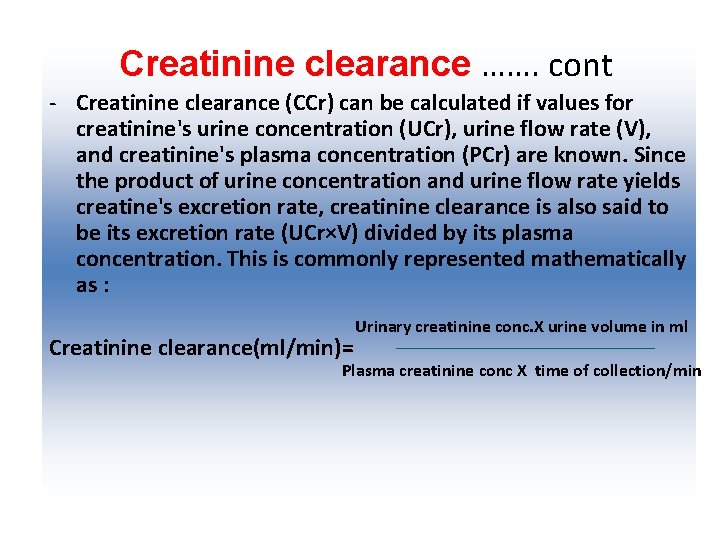
Creatinine clearance ……. cont - Creatinine clearance (CCr) can be calculated if values for creatinine's urine concentration (UCr), urine flow rate (V), and creatinine's plasma concentration (PCr) are known. Since the product of urine concentration and urine flow rate yields creatine's excretion rate, creatinine clearance is also said to be its excretion rate (UCr×V) divided by its plasma concentration. This is commonly represented mathematically as : Creatinine clearance(ml/min)= Urinary creatinine conc. X urine volume in ml Plasma creatinine conc X time of collection/min
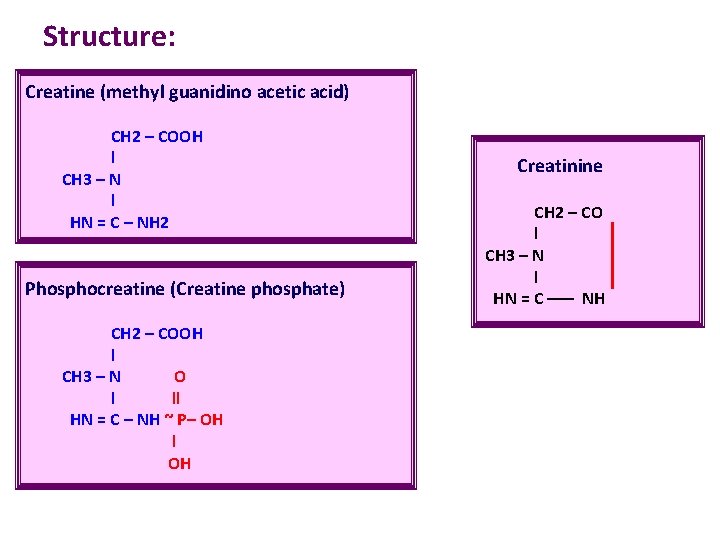
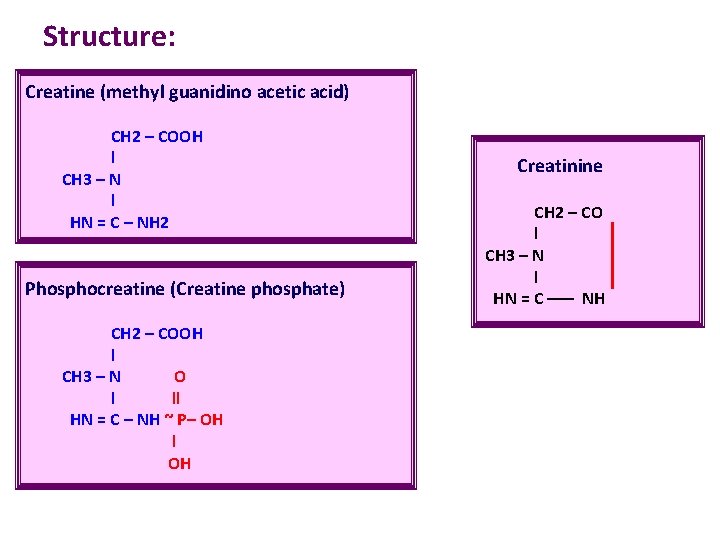
Structure: Creatine (methyl guanidino acetic acid) CH 2 – COOH l CH 3 – N l HN = C – NH 2 Phosphocreatine (Creatine phosphate) CH 2 – COOH l CH 3 – N O l ll HN = C – NH ~ P– OH l OH Creatinine CH 2 – CO l CH 3 – N l HN = C ––– NH
THANKS