Cranial Nerves Tutor Information PULSE Preparation for Finals

- Slides: 24
Cranial Nerves: Tutor Information PULSE: Preparation for Finals Tutor name
Resource summary • Common OSCE questions/topics • Case-based additional information (Cases 1 – 3)
Common questions • Things you might pick up and questions you will get asked…
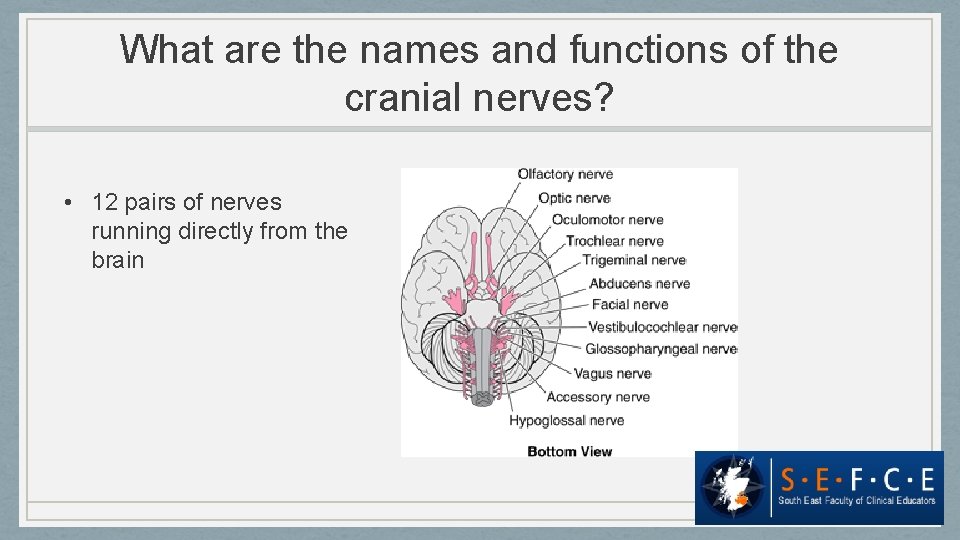
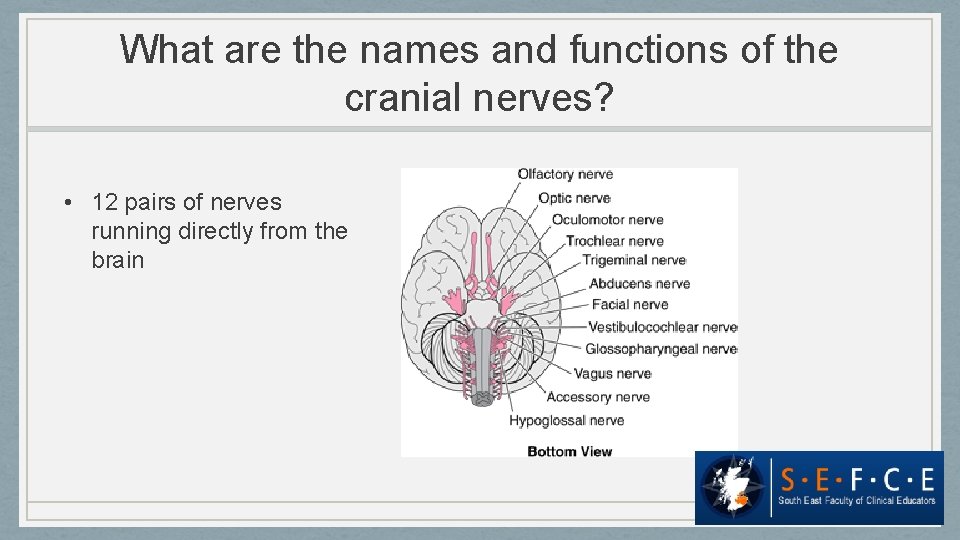
What are the names and functions of the cranial nerves? • 12 pairs of nerves running directly from the brain
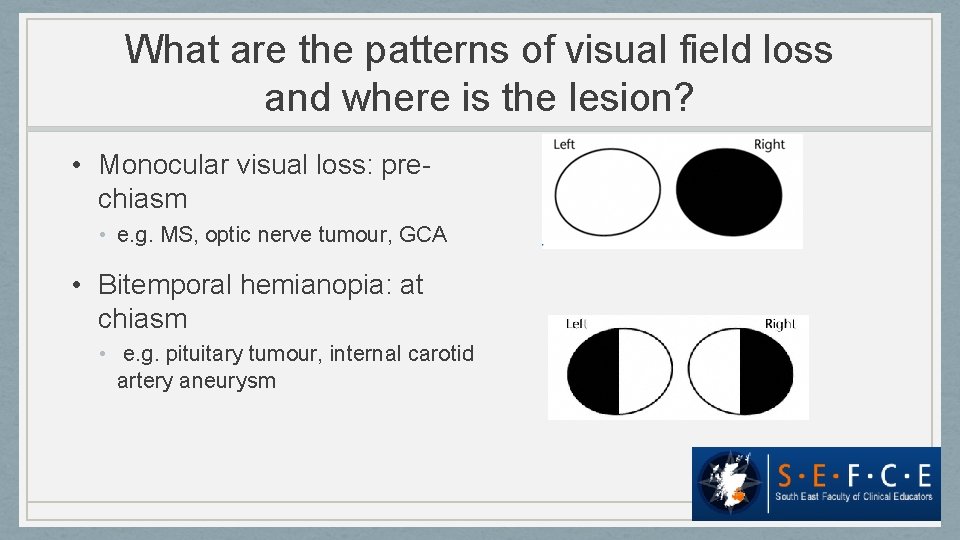
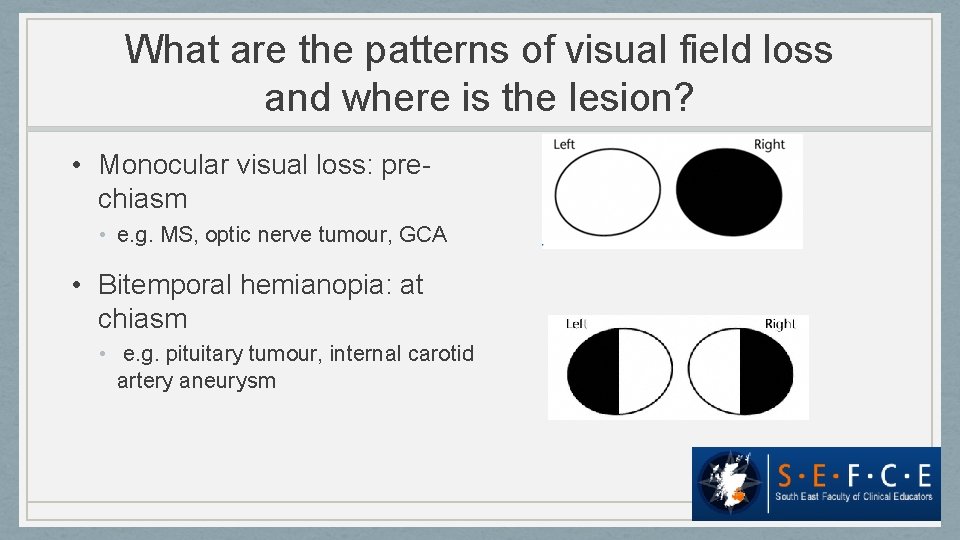
What are the patterns of visual field loss and where is the lesion? • Monocular visual loss: prechiasm • e. g. MS, optic nerve tumour, GCA • Bitemporal hemianopia: at chiasm • e. g. pituitary tumour, internal carotid artery aneurysm
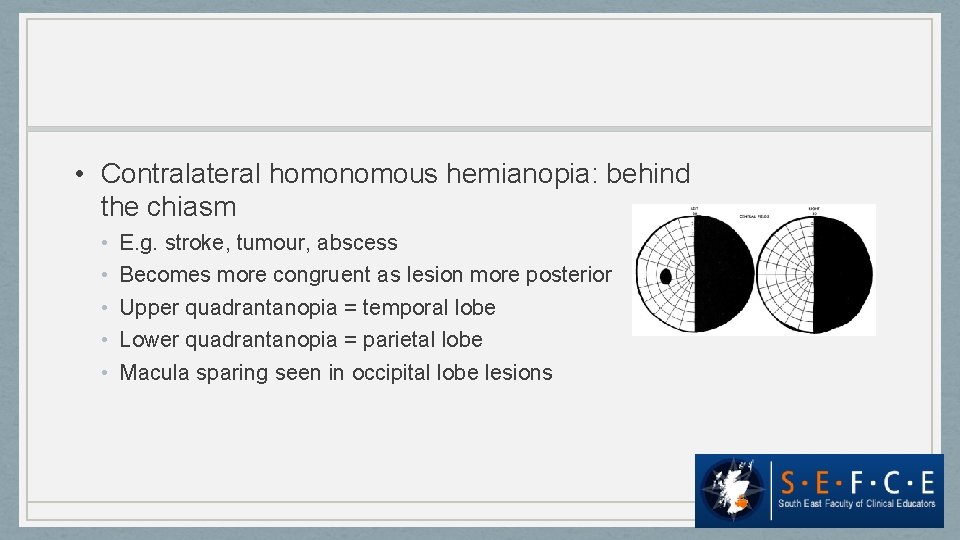
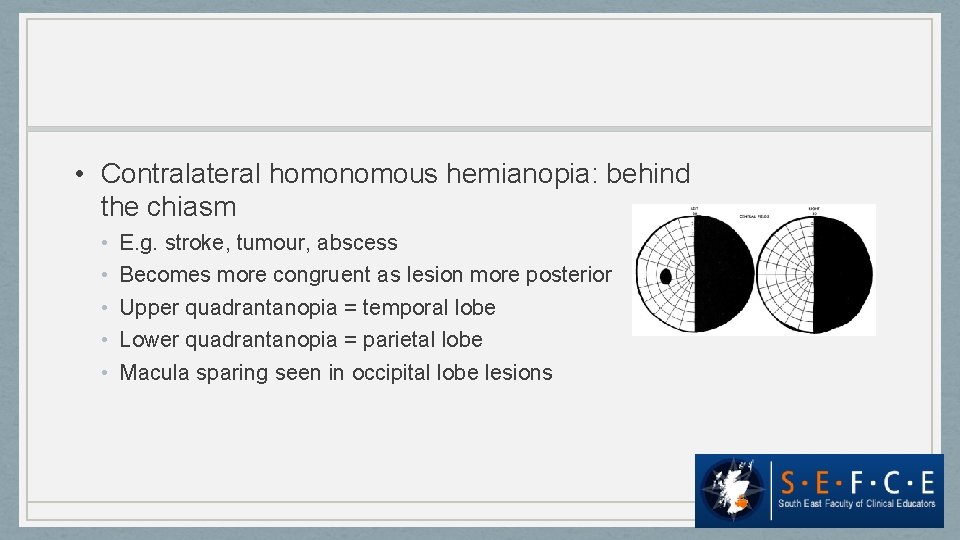
• Contralateral homonomous hemianopia: behind the chiasm • • • E. g. stroke, tumour, abscess Becomes more congruent as lesion more posterior Upper quadrantanopia = temporal lobe Lower quadrantanopia = parietal lobe Macula sparing seen in occipital lobe lesions
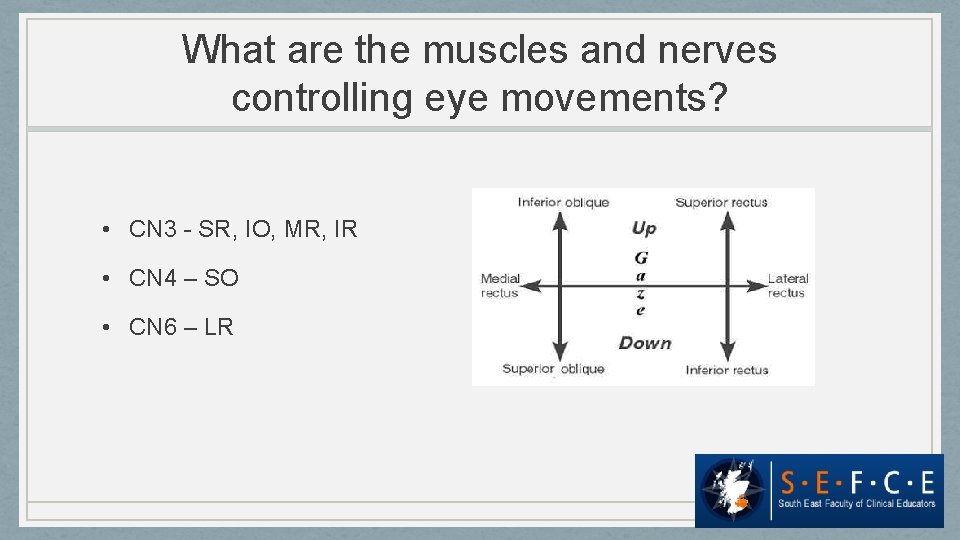
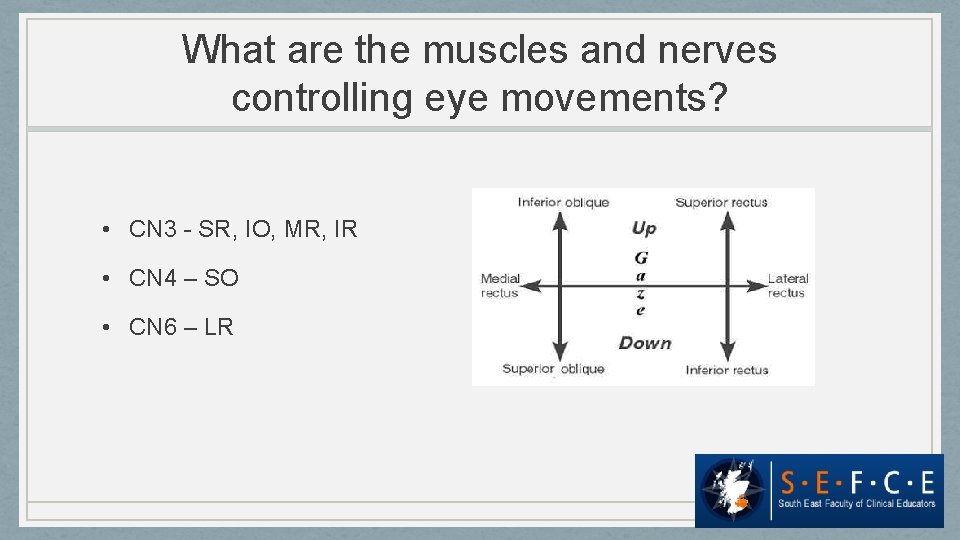
What are the muscles and nerves controlling eye movements? • CN 3 - SR, IO, MR, IR • CN 4 – SO • CN 6 – LR
Clinical signs
What are the causes and patterns of opthalmoplegia? • CN 3 palsy – down and out • Partial vs complete • CN 4 palsy - eye bobs up, may hold head squint (torticollis) • CN 6 palsy - esotropia • E. g. false localising sign • Maximum separation of the image is in the direction of the affected eye muscle; lateral image is the false one
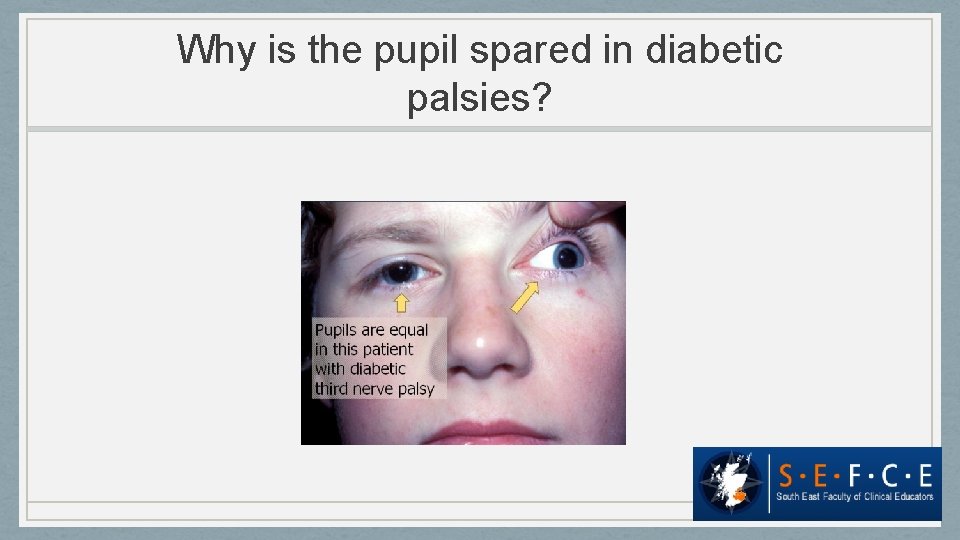
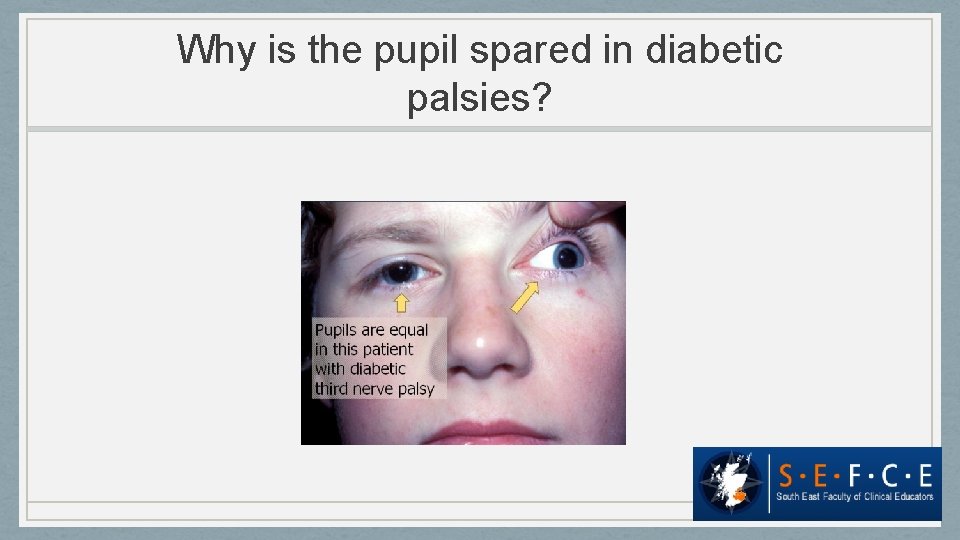
Why is the pupil spared in diabetic palsies?
What is a false localising sign? A misleading physical sign e. g. dilated pupil in raised ICP
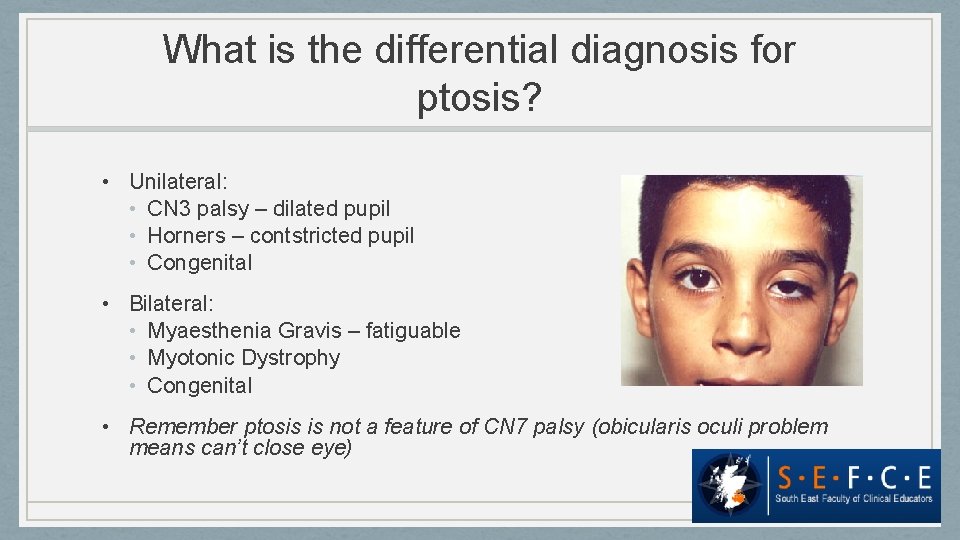
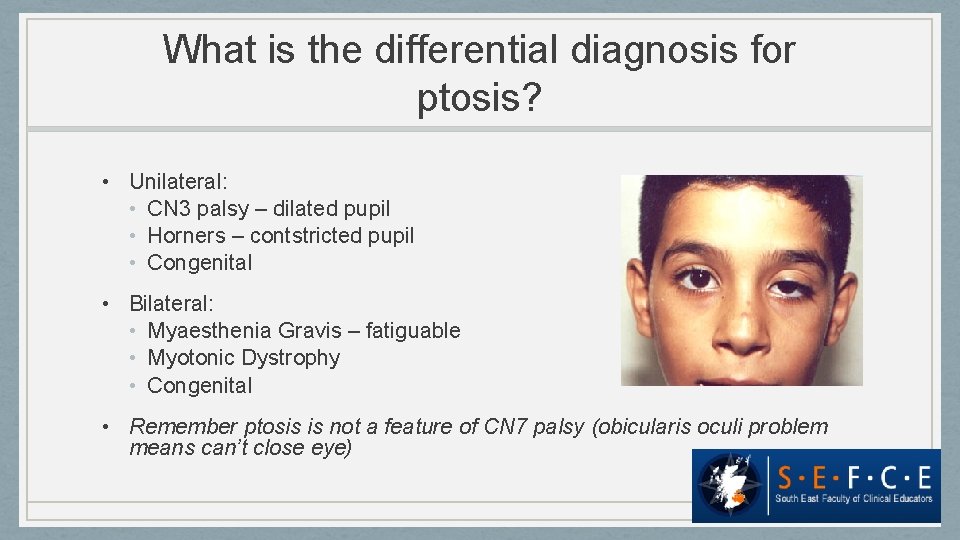
What is the differential diagnosis for ptosis? • Unilateral: • CN 3 palsy – dilated pupil • Horners – contstricted pupil • Congenital • Bilateral: • Myaesthenia Gravis – fatiguable • Myotonic Dystrophy • Congenital • Remember ptosis is not a feature of CN 7 palsy (obicularis oculi problem means can’t close eye)
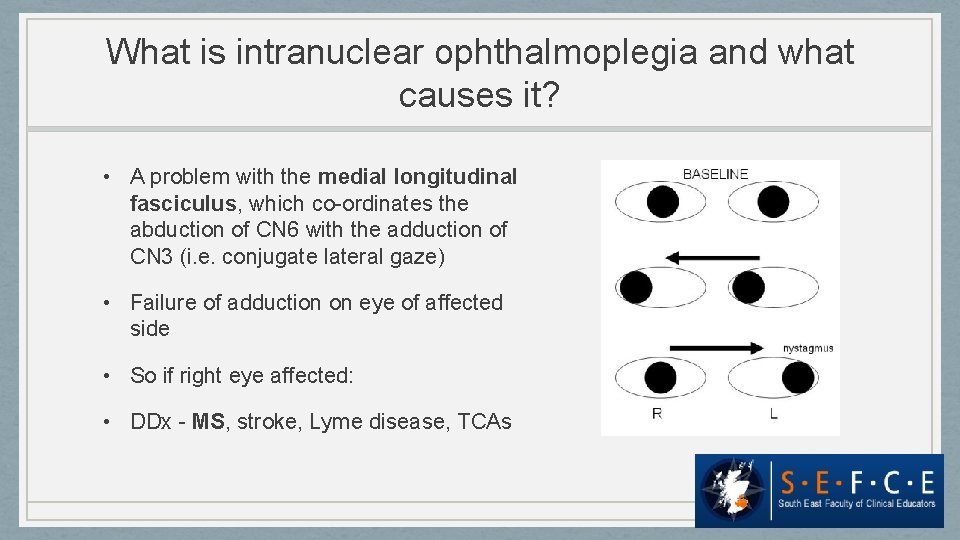
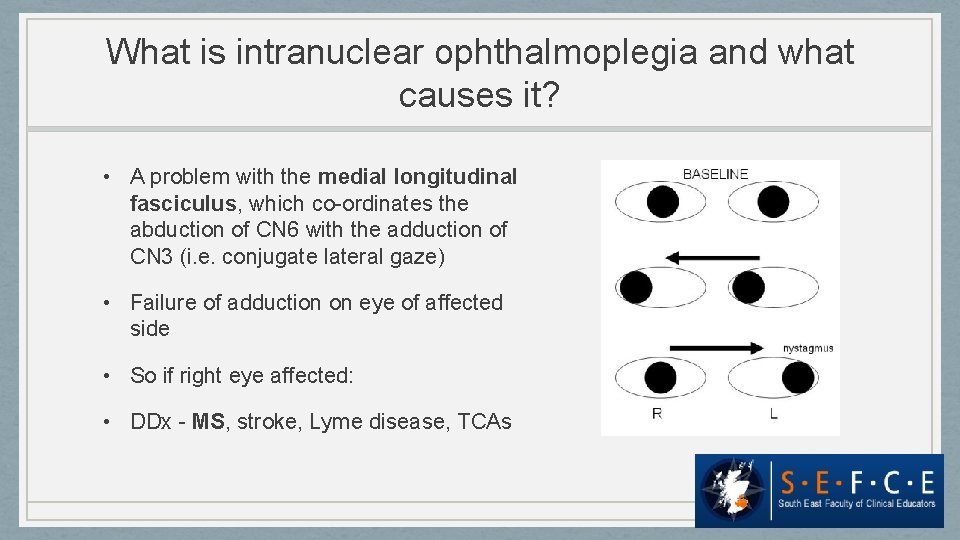
What is intranuclear ophthalmoplegia and what causes it? • A problem with the medial longitudinal fasciculus, which co-ordinates the abduction of CN 6 with the adduction of CN 3 (i. e. conjugate lateral gaze) • Failure of adduction on eye of affected side • So if right eye affected: • DDx - MS, stroke, Lyme disease, TCAs

What are the causes of a facial nerve palsy? • LMN: Bells, malignant parotid tumour, Ramsay Hunt, sarcoid, acoustic neuroma, brainstem infarct, DM • UMN: Stroke, tumour
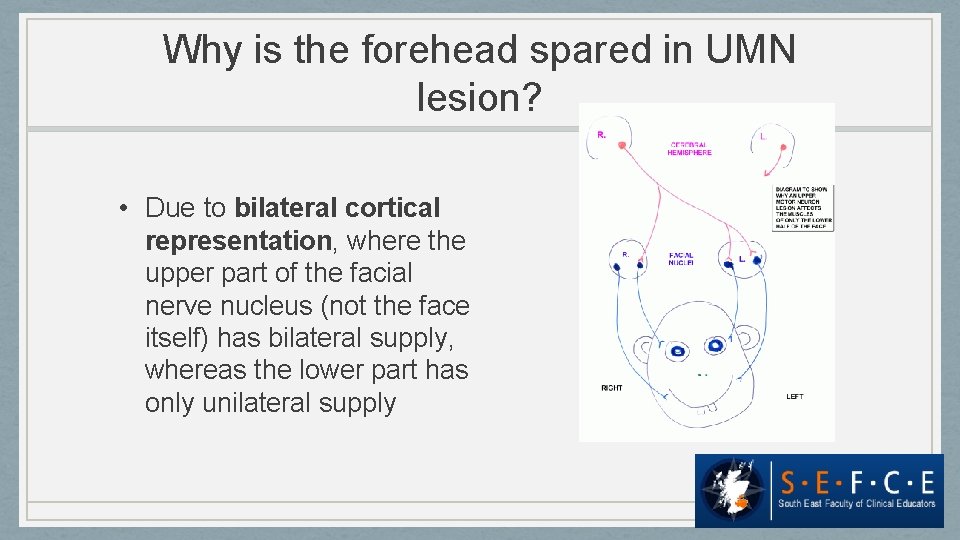
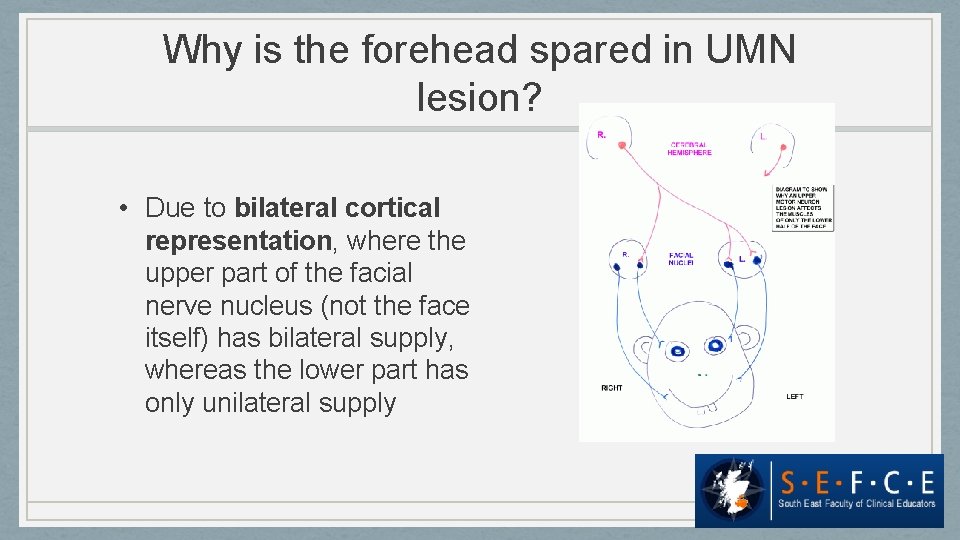
Why is the forehead spared in UMN lesion? • Due to bilateral cortical representation, where the upper part of the facial nerve nucleus (not the face itself) has bilateral supply, whereas the lower part has only unilateral supply
What are Rinne and Weber tests? • Unlikely you would have to perform this in finals but could certainly get asked about it! • Rinne - air v bone conduction at ear • Weber - put tuning fork on forehead • SNACRIP - in sensorineural loss or normal, air conduction > bone conduction, Rinne is positive.
What is the difference between bulbar and pseudobulbar palsy? • Both are impaired CN 9 -12, resulting in unilateral facial paralysis and problems with speech • Bulbar = LMN. Tongue fasciculates. • Pseudo = UMN. Tongue spastic. Associated with emotional lability.
What is the differential diagnosis of a cranial nerve palsy? Common differentials 1. Vascular – CVA/stroke (ischaemic/haemorrhagic), vasculitis 2. Inflammatory – demyelination (MS) 3. SOL – tumour, abscess, vascular, oedema, hydrocephalus 4. Infectious – viruses (HIV, CMV), bacteria (TB, Lyme, leprosy, syphilis), protozoal (toxoplasma) 5. Mononeuritis multiplex 1. 2. 3. 4. Metabolic – DM, amyloidosis Vasculitis – Wegener’s, PAN, SLE, RA Granulomatous – sarcoid, lyme, leprosy Malignancy – primary or secondary, SOL or paraneoplastic
Or… Lesions along the path of the nerve: • Central – within brain/brainstem • Intra-cranial – as the nerve passes out from the brain along the vault of the skull • Through the cranium – whichever foramen it pops out of • Extra-cranial – within the soft tissues of the orbit/face/neck/etc
Causes of cerebellopontine angle lesions? • Neoplastic • • Acoustic neuroma (vestibular schwannoma) Meningioma, cholesteatoma, haemangioblastoma Pontine glioma Nasopharyngeal carcinoma • Infective • Local mengingeal involvement, e. g. TB
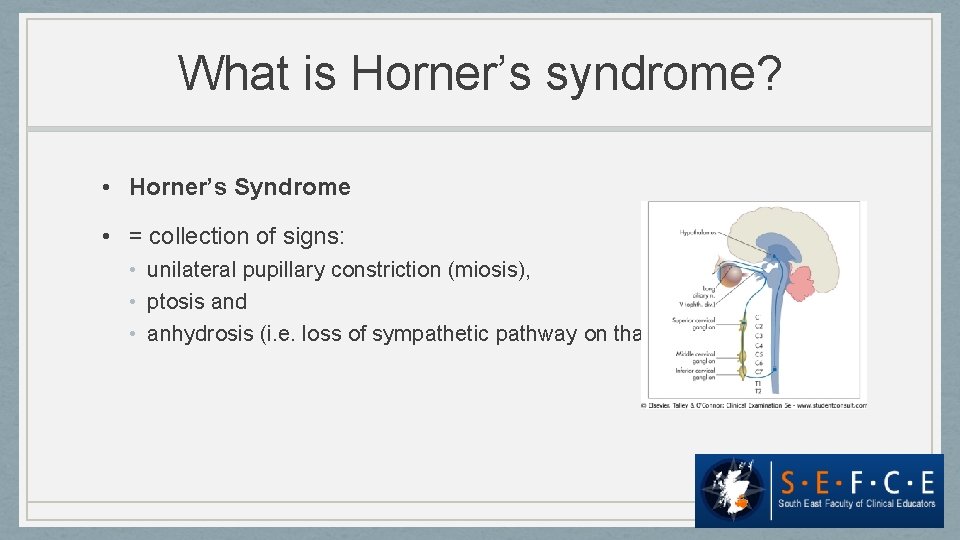
What is Horner’s syndrome? • Horner’s Syndrome • = collection of signs: • unilateral pupillary constriction (miosis), • ptosis and • anhydrosis (i. e. loss of sympathetic pathway on that side).
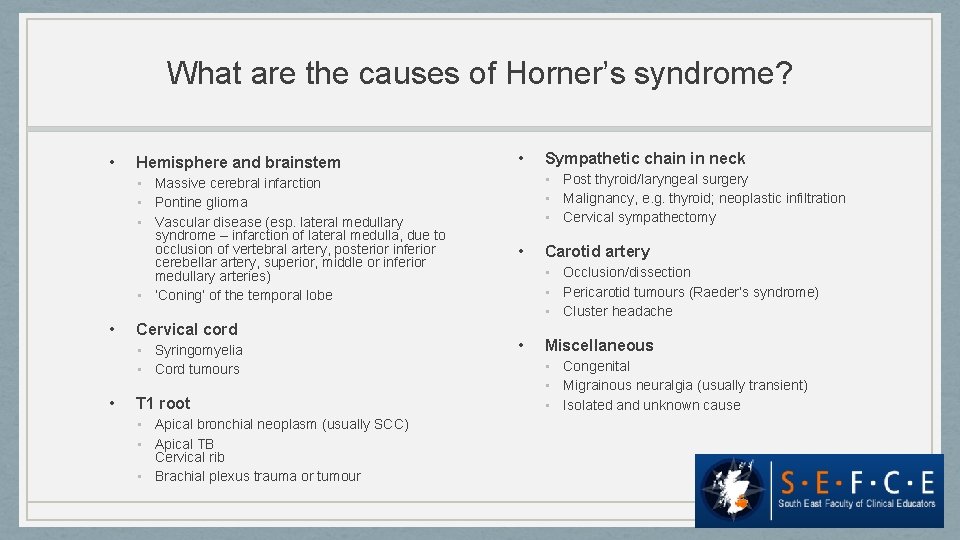
What are the causes of Horner’s syndrome? • Hemisphere and brainstem • Massive cerebral infarction • Pontine glioma • Vascular disease (esp. lateral medullary syndrome – infarction of lateral medulla, due to occlusion of vertebral artery, posterior inferior cerebellar artery, superior, middle or inferior medullary arteries) • ‘Coning’ of the temporal lobe • Cervical cord • Syringomyelia • Cord tumours • T 1 root • Apical bronchial neoplasm (usually SCC) • Apical TB Cervical rib • Brachial plexus trauma or tumour • Sympathetic chain in neck • Post thyroid/laryngeal surgery • Malignancy, e. g. thyroid; neoplastic infiltration • Cervical sympathectomy • Carotid artery • Occlusion/dissection • Pericarotid tumours (Raeder’s syndrome) • Cluster headache • Miscellaneous • Congenital • Migrainous neuralgia (usually transient) • Isolated and unknown cause
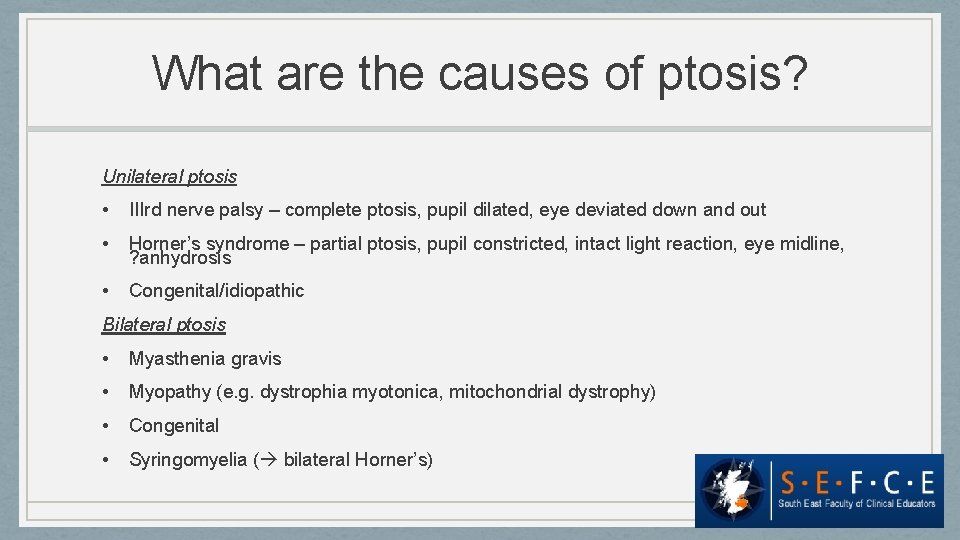
What are the causes of ptosis? Unilateral ptosis • IIIrd nerve palsy – complete ptosis, pupil dilated, eye deviated down and out • Horner’s syndrome – partial ptosis, pupil constricted, intact light reaction, eye midline, ? anhydrosis • Congenital/idiopathic Bilateral ptosis • Myasthenia gravis • Myopathy (e. g. dystrophia myotonica, mitochondrial dystrophy) • Congenital • Syringomyelia ( bilateral Horner’s)
• Case 1: visual field defect • Case 2: facial nerve palsy • Case 3: Horners Syndrome